Abstract
Background
The emergency department (ED) at the Veterans Affairs Greater Los Angeles Healthcare System (VAGLAHS) saw a decrease in the number of visits during the early stages of the COVID-19 pandemic. Little is known whether risk mitigation procedures may help reduce the spread of COVID-19 infections for veterans visiting the ED. Therefore, we reviewed patient visits to the ED for diagnoses other than COVID-19 to assess whether these patients had an increased COVID-19 positivity rate within 21 days of the initial visit.
Observations
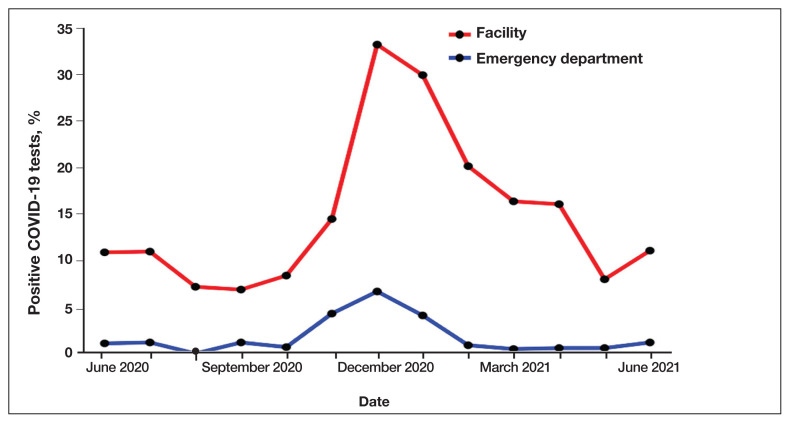
Risk mitigation procedures instituted by the VAGLAHS ED included a COVID-19 outdoor testing tent, immediate isolation of persons under investigation for COVID-19, disinfection protocols between high-risk patient encounters, dedicated training in donning and doffing personal protective equipment, implementation of 2-physician airway teams for COVID-19 intubations, use of electronic tablets to communicate with COVID-19 patients, and implementation of social distancing initiatives in the waiting room to minimize COVID-19 exposures. The average positivity rate at the VAGLAHS ED during this time frame was 0% to 6.7%, compared with 6.9% to 33.3% within the wider VAGLAHS.
Conclusions
Implementing risk mitigation procedures in the VAGLAHS ED helped minimize exposure and subsequent diagnosis of COVID-19 for veterans who visited the VAGLAHS ED for symptoms not associated with COVID-19 infection. Seeking acute medical care in the ED did not put patients at higher risk of contracting COVID-19.
At the onset of the COVID-19 pandemic, patient encounters with the health care system plummeted.1–3 The perceived increased risk of contracting COVID-19 while obtaining care was thought to be a contributing factor. In outpatient settings, one study noted a 63% decrease in visits to otolaryngology visits in Massachusetts, and another noted a 33% decrease in dental office visits at the onset of the pandemic in 2020 compared with the same time frame in 2019.2,4 Along with mask mandates and stay-at-home orders, various institutions sought to mitigate the spread of COVID-19 through different protocols, including the use of social distancing, limitation of visitors, and telehealth. Despite some of these measures, nosocomial infections were not uncommon. For example, one hospital in the United Kingdom reported that 15% of COVID-19 inpatient cases in a 6-week period in 2020 were probably or definitely hospital acquired. These patients had a 36% case fatality rate.5
Unlike outpatient treatment centers, however, the emergency department (ED) is mandated by the Emergency Medical Treatment and Labor Act to provide a medical screening examination and to stabilize emergency medical conditions to all patients presenting to the ED. Thus, high numbers of undifferentiated and symptomatic patients are forced to congregate in EDs, increasing the risk of transmission of COVID-19. This perception of increased risk led to a 42% decrease in ED visits during March and April 2020 at the onset of the COVID-19 pandemic.1 Correspondingly, there was a 20% decrease in code stroke activations at a hospital in Canada and a 38% decrease in ST-elevation myocardial infarction activations across 9 United States hospital systems.6,7
Limited studies have been conducted to date to determine whether contracting COVID-19 while in the ED is a risk. One retrospective case-control study evaluating 39 EDs in the US showed that ED colocation with known patients with COVID-19 was not associated with an increased risk of COVID-19 transmission.5 However, this study also recognized that infection control strategies widely varied by location and date.
In this study, we report the incidence of COVID-19 infections within 21 days after the initial visit for symptoms not associated with COVID-19 infection to the Veterans Affairs Greater Los Angeles Healthcare System (VAGLAHS) ED and compared it with that of COVID-19 infections for tests performed within the VAGLAHS.
Program Description
As a quality improvement measure, the VAGLAHS ED instituted multiple protocols to mitigate COVID-19 transmission. Social distancing was instituted in the waiting room to prevent the close congregation of patients, regardless of the reason for visit. A COVID-19 testing tent was located outdoors that was adjacent to the ED and staffed by a dedicated licensed independent practitioner and nurses during business hours. During COVID-19 infection surges, hours were extended to include evenings and weekends to decrease ED exposure of stable but symptomatic patients seeking testing. If patients were felt to require more care, they were referred to the ED.
Patients with specific symptoms noted during triage, such as those associated with COVID-19 diagnosis, respiratory infections, fever, and/or myalgias, were isolated in their own patient room. Electronic tablets were used for persons under investigation and patients with COVID-19 to communicate with family and/or medical staff who did not need to enter the patient’s room. Two-hour disinfection protocols were instituted for high-risk patients who were moved during the course of their treatment (ie, transfer to another bed for admission or discharge). All staff was specifically trained in personal protective equipment (PPE) donning and doffing, and 2-physician airway teams were implemented to ensure proper PPE use and safe COVID-19 intubations.
COVID-19 INFECTIONS
Electronic health records of patients who visited the VAGLAHS ED for symptoms not related to COVID-19 were reviewed from June 1, 2020, to June 30, 2021, to determine whether these patients had an increased incidence of confirmed COVID-19 infection within 21 days of the index ED visit. Patients with upper respiratory infection symptoms, such as cough, fever, chills, sore throat, changes to taste or smell, or a confirmed COVID-19 infection on the initial visit were excluded. Patients were considered to have had an ED-acquired COVID-19 infection if they had a positive test within 21 days of visiting the ED for a symptom not related to COVID-19. We report the overall average positivity rate by month of COVID-19 infections 21 days post-ED visit for visits for symptoms not related to COVID-19.
A total of 8708 patients who came to the ED with symptoms not associated with COVID-19 infection and had a COVID-19 test within 21 days of the ED visit met the inclusion criteria. The overall average positivity rate at the VAGLAHS ED for symptoms not associated with COVID-19 infection was 1.1% from June 1, 2020, to June 30, 2021. The positivity rate by month ranged from 0% to 6.7% for this period (Figure). We overlaid these data with the overall positivity rate by month for veterans in the VAGLAHS catchment area who were tested for COVID-19 at the US Department of Veterans Affairs (VA) to show that veterans who visited the ED did not appear to have an increased incidence of COVID-19 following an ED visit.
FIGURE.
Veterans Affairs Greater Los Angeles Healthcare System COVID-19 Infection Rates
DISCUSSION
Implementing COVID-19 mitigation measures in the VAGLAHS ED helped minimize exposure and subsequent infection of COVID-19 for veterans who visited the VAGLAHS ED with symptoms not associated with COVID-19 infection. Contextualizing this with the overall average monthly positivity rate of veterans in the VAGLAHS catchment area (10.9%) or Los Angeles County (7.9%) between June 1, 2020, to June 30, 2021, veterans who visited the VAGLAHS ED for symptoms not associated with COVID-19 infection were less likely to test positive for COVID-19 within 21 days (1.1%), suggesting that the extensive measures taken at the VAGLAHS ED were effective.8
Many health care systems in the US and abroad have experimented with different transmission mitigation strategies in the ED. These tactics have included careful resource allocation when PPE shortages occur, incorporation of airway teams with appropriate safety measures to reduce nosocomial spread to health care workers, and use of a cohorting plan to separate persons under investigation and patients with COVID-19 from other patients.9–15 Additionally, forward screening areas were incorporated similar to the COVID-19 tent that was instituted at the VAGLAHS ED to manage patients who were referred to the ED for COVID-19 testing during the beginning of the pandemic, which prevented symptomatic patients from congregating with asymptomatic patients.14,15
Encouragingly, some of these studies reported no cases of nosocomial transmission in the ED.11,13 In a separate study, 14 clusters of COVID-19 cases were identified at one VA health care system in which nosocomial transmission was suspected, including one in the ED.16 Using contact tracing, no patients and 9 employees were found to have contracted COVID-19 in that cluster. Overall, among all clusters examined within the health care system, either by contact tracing or by whole-genome sequencing, the authors found that transmission from health care personnel to patients was rare. Despite different methodologies, we also similarly found that ED patients in our VA facility were unlikely to become infected with COVID-19.
While the low incidence of positive COVID-19 tests cannot be attributed to any one method, our data provide a working blueprint for enhanced ED precautions in future surges of COVID-19 or other airborne diseases, including that of future pandemics.
Limitations
Notably, although the VA is the largest health care system in the US, a considerable number of veterans may present to non-VA EDs to seek care, and thus their data are not included here; these veterans may live farther from a VA facility or experience higher barriers to care than veterans who exclusively or almost exclusively seek care within the VA. As a result, we are unable to account for COVID-19 tests completed outside the VA. Moreover, the wild type SARS-CoV-2 virus was dominant during the time frame chosen for this assessment, and data may not be generalizable to other variants (eg, omicron) that are known to be more highly transmissible.17 Lastly, although our observation was performed at a single VA ED and may not apply to other facilities, especially in light of different mitigation strategies, our findings still provide support for approaches to minimizing patient and staff exposure to COVID-19 in ED settings.
CONCLUSIONS
Implementation of COVID-19 mitigation measures in the VAGLAHS ED may have minimized exposure to COVID-19 for veterans who visited the VAGLAHS ED for symptoms not associated with COVID-19 and did not put one at higher risk of contracting COVID-19. Taken together, our data suggest that patients should not avoid seeking emergency care out of fear of contracting COVID-19 if EDs have adequately instituted mitigation techniques.
Footnotes
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies.
Ethics and consent
This project was reviewed by the Veterans Affairs Greater Los Angeles Institutional Review Board and was determined to be nonresearch.
Author disclosures
The authors report no actual or potential conflicts of interest or outside sources of funding with regard to this article.
References
- 1.Hartnett KP, Kite-Powell A, DeVies J, et al. National Syndromic Surveillance Program Community of Practice. Impact of the COVID-19 pandemic on emergency department visits—United States, January 1, 2019–May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(23):699–704. doi: 10.15585/mmwr.mm6923e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fan T, Workman AD, Miller LE, et al. The impact of COVID-19 on otolaryngology community practice in Massachusetts. Otolaryngol Head Neck Surg. 2021;165(3):424–430. doi: 10.1177/0194599820983732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baum A, Kaboli PJ, Schwartz MD. Reduced in-person and increased telehealth outpatient visits during the COVID-19 pandemic. Ann Intern Med. 2021;174(1):129–131. doi: 10.7326/M20-3026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kranz AM, Chen A, Gahlon G, Stein BD. 2020 trends in dental office visits during the COVID-19 pandemic. J Am Dent Assoc. 2021;152(7):535–541e1. doi: 10.1016/j.adaj.2021.02.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ridgway JP, Robicsek AA. Risk of coronavirus disease 2019 (COVID-19) acquisition among emergency department patients: a retrospective case control study. Infect Control Hosp Epidemiol. 2021;42(1):105–107. doi: 10.1017/ice.2020.1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bres Bullrich M, Fridman S, Mandzia JL, et al. COVID-19: stroke admissions, emergency department visits, and prevention clinic referrals. Can J Neurol Sci. 2020;47(5):693–696. doi: 10.1017/cjn.2020.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Garcia S, Albaghdadi MS, Meraj PM, et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75(22):2871–2872. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.LA County COVID-19 Surveillance Dashboard. [Accessed July 25, 2022]. https://covid19.lacounty.gov/dashboards .
- 9.Wallace DW, Burleson SL, Heimann MA, et al. An adapted emergency department triage algorithm for the COVID-19 pandemic. J Am Coll Emerg Physicians Open. 2020;1:1374–1379. doi: 10.1002/emp2.12210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Montrief T, Ramzy M, Long B, Gottlieb M, Hercz D. COVID-19 respiratory support in the emergency department setting. Am Journal Emerg Med. 2020;38(10):2160–2168. doi: 10.1016/j.ajem.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alqahtani F, Alanazi M, Alassaf W, et al. Preventing SARS-CoV-2 transmission in the emergency department by implementing a separate pathway for patients with respiratory conditions. J Complement Integr Med. 2022;19(2):383–388. doi: 10.1515/jcim-2020-0422. [DOI] [PubMed] [Google Scholar]
- 12.Odorizzi S, Clark E, Nemnom MJ, et al. Flow impacts of hot/cold zone infection control procedures during the COVID-19 pandemic in the emergency department. CJEM. 2022;24(4):390–396. doi: 10.1007/s43678-022-00278-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wee LE, Fua TP, Chua YY, et al. Containing COVID-19 in the emergency department: the role of improved case detection and segregation of suspect cases. Acad Emerg Med. 2020;27(5):379–387. doi: 10.1111/acem.13984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tan RMR, Ong GYK, Chong SL, Ganapathy S, Tyebally A, Lee KP. Dynamic adaptation to COVID-19 in a Singapore paediatric emergency department. Emerg Med J. 2020;37(5):252–254. doi: 10.1136/emermed-2020-20963. [DOI] [PubMed] [Google Scholar]
- 15.Quah LJJ, Tan BKK, Fua TP, et al. Reorganising the emergency department to manage the COVID-19 outbreak. Int J Emerg Med. 2020;13(1):32. doi: 10.1186/s12245-020-00294-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jinadatha C, Jones LD, Choi H, et al. Transmission of SARS-CoV-2 in inpatient and outpatient settings in a Veterans Affairs health care system. Open Forum Infect Dis. 2021;8(8):ofab328. doi: 10.1093/ofid/ofab328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Riediker M, Briceno-Ayala L, Ichihara G, et al. Higher viral load and infectivity increase risk of aerosol transmission for Delta and Omicron variants of SARS-CoV-2. Swiss Med Wkly. 2022;152:w30133. doi: 10.4414/smw.2022.w30133. [DOI] [PubMed] [Google Scholar]