Abstract
Overcrowding in the Emergency department (ED) necessitates a major challenge in delivering high-quality care in acute settings. This study presents a novel approach to modeling the relationship between the day of the week, ED arrivals, chest pain (CP), and acute myocardial infarction (AMI) using regression analysis. We analyzed data from 2016 to 2019 across three platforms: a nationwide representative sample (NHAMCS), a federated data network (TriNetX), and a regional medical center. For the stated three outcomes, the number of patients in that category on each day of the week was calculated; these were then calculated separately for each year, as well as across all four years. In line with prior studies, this study demonstrates the highest percentage of ED arrival on Mondays and the lowest on the weekends. Similarly, chest pain was more prevalent on Mondays, with similar patterns for TriNetX and the regional medical center. Analyzing NHAMCS data demonstrated Wednesdays as the busiest day for AMI-related ED arrivals, although this observation was not statistically significant. This knowledge will better aid us in resource allocation and system awareness, paving a path toward better patient care, improving disease management, and reducing healthcare costs.
Keywords: Chest pain, Emergency department arrival, Acute myocardial infarction rates
1. Introduction
Emergency departments (EDs) are the gateway for patient flow into the hospital and play a crucial role in the chain of care. The goal of any emergency department is to provide high-quality medical treatment in an efficient environment wherein maximum productivity is achieved with minimal wasted effort and expense. Overcrowding in the ED is a major concern, negatively impacting patient satisfaction and the overall health system.1
Theory suggests that EDs become overcrowded as the result of input (demand), throughput (congestion and queuing within the ED), and output (resources needed to transition the patients to the next level of care) imbalance.2 Unless all components are available at the same time, ED overcrowding is inevitable, leading to delays in treatment. Yet, despite having conceptual knowledge of the cause, healthcare systems across the United States still face difficulty in combining knowledge with action. According to the CDC, approximately 50% of EDs across the U.S. face overcrowding.3
Over the past several years, researchers have become interested in patterns of ED arrival. Prior studies suggest emergency departments encounter a significantly higher volume of patients on Mondays, with the least volume on weekends.4,5
Among many others, chest pain (CP) is reported as one of the most common symptoms prompting patients to present to the ED.6 Though it may stem from less severe maladies, chest pain could signal that the patient is experiencing an acute myocardial infarction (AMI). Every 40 s in the U.S., one person suffers from an AMI.7
Previously several studies reported a relatively consistent circadian, septadian (day of the week), and seasonal pattern for the development of an AMI.8–10 It has been observed that there is an increased incidence of AMI in the morning compared to the night,11 in cold weather compared to hot, and a marked excess incidence on Mondays and a minimum on Saturdays.12
Although the exact etiology of these patterns remains unclear, several hypotheses have been proposed. Increased incidence of AMI in the mornings was previously attributed to surges in blood pressure and heart rate due to sudden activation of the sympathetic nervous system.13 Greater incidence of AMI in the cold months was attributed to increased inflammatory markers, such as C-reactive protein (CRP), vasoconstriction, and increased blood pressure.14
In 2005, the phenomenon of excess AMI on Mondays was re-examined and confirmed via a meta-analysis of 28 articles from 16 countries; however, the analysis also showed that the size of the Monday effect differs widely across populations.15 Employment-related stress, inactivity, overconsumption of alcoholic beverages, and registration error were speculated to be key factors.15 Given that this phenomenon varies across populations, additional studies from different geographic regions would help shed light on patterns of ED arrivals and cardiovascular events. In this study, we aim to re-examine day of the week variation for ED arrivals, CP, and AMI using data from the Nationwide Hospital Ambulatory Medical Care Survey (NHAMCS), TriNetX, and institutional data from a regional medical center (AAMC) from 2016 to 2019. Our goal is to assess the existence of meaningful patterns for the stated factors. If such patterns are uncovered, this knowledge will better aid us in resource allocation and system awareness, paving a path toward better patient care, improving disease management, and reducing healthcare costs.
2. Methods
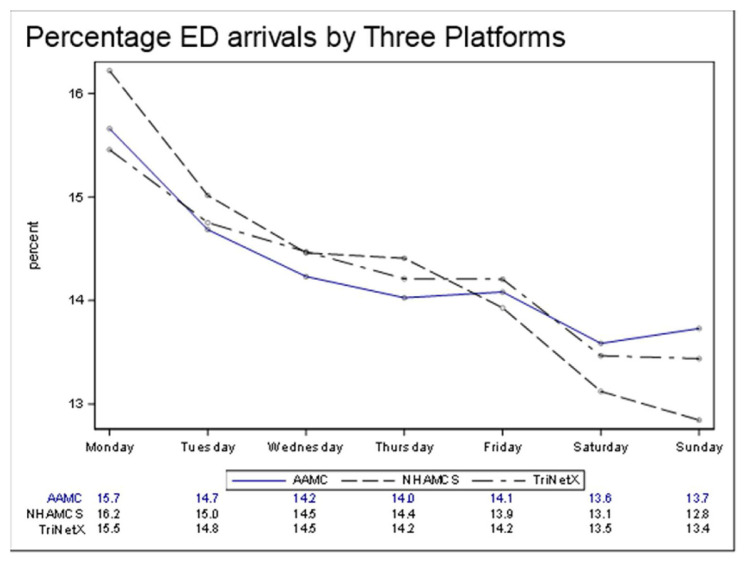
Data from 2016 to 2019 was analyzed across three platforms: a nationwide representative sample (NHAMCS), a federated data network (TriNetX), and a regional medical center. For each platform, we considered adults who were in any of the following categories: 1) patients arriving to the ED, 2) patients arriving to the ED who was diagnosed with chest pain (ICD10-R07.9), and 3) patients arriving at the ED with acute myocardial infarction (AMI ICD10-I21). For each of these three outcomes, the number of patients in that category on each day of the week was calculated; these were then calculated separately for each year, as well as across all four years. The totals were then expressed as a percentage; for example, at AAMC, 15.7% of all ED arrivals from 2016 to 2019 were presented on a Monday (see Fig. 1).
Fig. 1.
Regression analysis, with the outcome as the dependent variable, the R2 = 0.91 (p < 0.01). Demonstrating a downward trend in ED arrivals beginning on Monday and ending on Sunday across all three platforms.
NHAMCS is based on a national sample of visits to EDs in non-institutional general and short-stay hospitals (excluding federal, military, and Veterans Administration hospitals) and is collected using a three-stage probability sampling design. Each ED is randomly assigned to a four-week reporting period, during which a systematic random sample of visits is obtained, including the patient's reason for the visit and their diagnoses. Up to five (5) diagnoses may be reported per encounter. NHAMCS requires that data meet two reliability standards: the unweighted cell counts must be greater than 30, and the relative standard error must be less than 0.3. To meet these reliability standards, we used the latest four years of available NHAMCS data (2016–2019). To account for the complex sample design, Proc SurveyFreq (SAS 9.4, Cary, NC) was used to generate weighted totals and percentages, as well as standard errors.
AAMC is a 389-bed regional medical center with approximately 80,000 annual adult ED visits. Data from a separate pediatric ED were excluded from this study. TriNetX provides access to electronic medical records, including diagnoses and procedures, from approximately 17 million patients across 56 healthcare organizations. Because this study used only de-identified patient records and did not involve the collection, use, or transmittal of individually identifiable data, this study was exempted from Institutional Review Board approval. While TriNetX offers users the ability to summarize information using their graphical user interface, we received redacted data tables so that we could determine the day of the week for each of our outcomes of interest: 1) ED arrivals, 2) chest pain, and 3) acute myocardial infarction. The TriNetX data used in this study was collected on January 17, 2022.
Multiple regression analyses using Proc GLM were used for generating both individual and pooled estimates.
Limitations of the study regarding NHAMCS may include only five (5) diagnoses and exclude federal and military hospitals. Probably a consideration for future initiatives is to include the impact of urgent care centers which have increasingly been utilized by patients with emergent needs. Many other sociodemographic and economic factors, including proximity to health care facilities, may also be associated with outcome measures.
3. Results
Graphical and numeric values of ED arrivals according to the day of the week demonstrate Monday as the highest volume (AAMC 15.7%, NHAMCS 16.2% & TriNetX 15.5%). The amounts were aggregated across all four years (2016–2019) and are presented for each platform. The lowest percentages of ED arrivals occurred over the weekend (all three platforms less than 13.7%) displayed in Fig. 1.
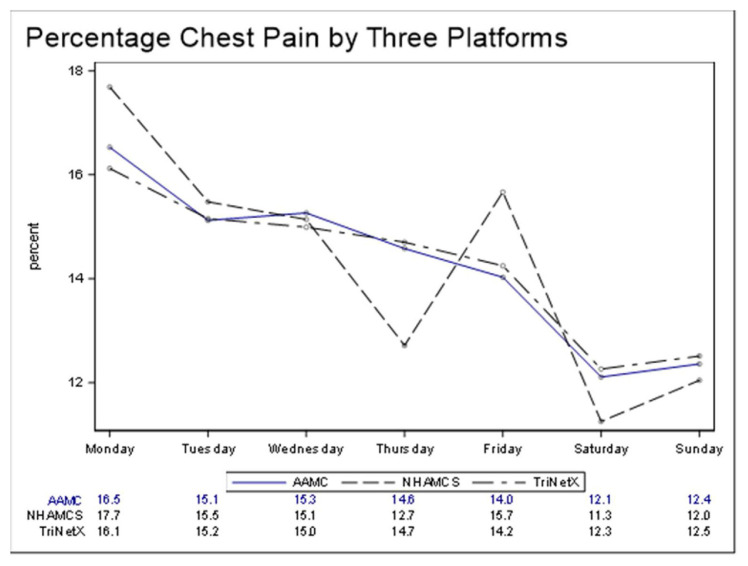
Patients experiencing chest pain according to the day of the week, Fig. 2 displays both graphical and numeric. The counts were aggregated across all four years (2016–2019) and are presented for each platform. As with ED arrivals, chest pain was more prevalent on Mondays, with TriNetX and AAMC displaying similar patterns. NHAMCS data exhibited greater variability, with a decrease on Thursdays and an increase on Fridays.
Fig. 2.
Beginning on Monday, there is a downward trend across days of the week for the outcome of chest pain. NHAMCS exhibits greater variability, with a decrease on Thursdays and an increase on Fridays.
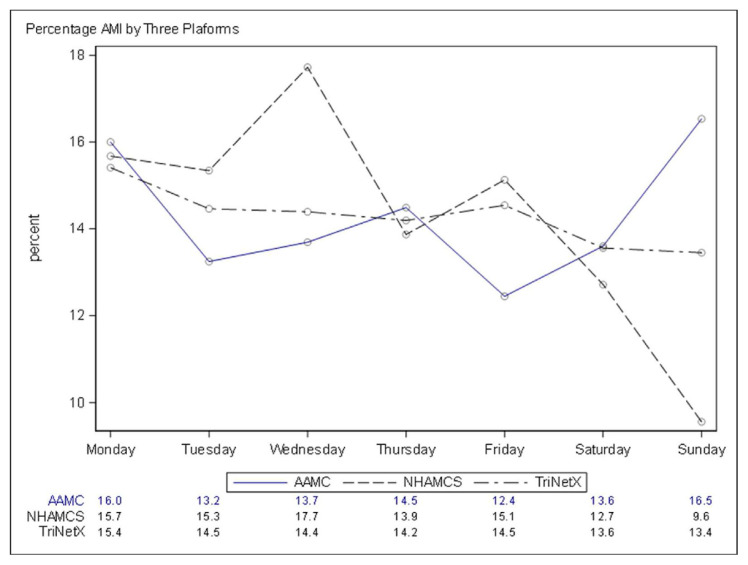
Patients experiencing acute myocardial infarction according to the day of the week in both graphical and numeric values are described in Fig. 3. The counts were aggregated across all four years (2016–2019) and are presented for each platform. TriNetX data displayed the least variability, with the largest percentage (15.4%) on Mondays and the smallest percentage (13.4%) on Sundays. AAMC displayed moderate variability compared to Tri-NetX. NHAMCS exhibited the most variability, with the largest percentage (17.7%) on Wednesdays and the smallest percentage (9.6%) on Sundays.
Fig. 3.
TriNetX data displayed the least variability, with the largest percentage (15.4%) on Mondays and the smallest percentage (13.4%) on Sundays. AAMC displayed moderate variability compared to TriNetX. NHAMCS exhibited the most variability, with the largest percentage (17.7%) on Wednesdays and the smallest percentage (9.6%) on Sundays.
Septadian patterns were assessed using multiple regression analysis with day of the week and platform as independent variables and one of the three outcomes (ED arrivals, chest pain, and AMI) as the dependent variable (Table 1). The results use data aggregated across all four years, as well as results where years are treated individually. Thus, the pooled results are based on 21 data points (three platforms and seven days of the week), while non-pooled results are based on 84 data points (three platforms, seven days of the week, and four years). The pooled and non-pooled results are similar: day of the week is statistically significant (with Mondays the highest and Sundays the lowest). The R2 is 0.91 and 0.86 for the pooled and non-pooled analysis, respectively. Moreover, the pattern of ED arrivals is consistent between TriNetX and our regional medical center, with NHAMCS having a significantly higher slope. Fig. 4 depicts this effect for the pooled results.
Table 1.
General linear model effects.
| Outcomes | Group (ref = TriNetX) | Day of Week * Group | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||
| R2 | Intercept | Day of Week | AAMC | NHAMCS | AAMC | NHAMCS | ||
| ED Arrivals | Pooled | 0.91 | 15.2 | −0.32 | −0.08 | 0.59 | 0.02 | −0.19 |
| p-value | p < 0.01 | p < 0.01 | p 0.77 | p 0.05 | p 0.72 | p 0.02 | ||
| ED Arrivals | Separate | 0.86 | 15.2 | −0.31 | −0.06 | 0.61 | 0.02 | −0.2 |
| p-value | p < 0.01 | p < 0.01 | p 0.67 | p < 0.01 | p 0.61 | p < 0.01 | ||
| Chest Pain | Pooled | 0.78 | 16.1 | −0.62 | 0.25 | 0.8 | −0.09 | −0.27 |
| p-value | p < 0.01 | p < 0.01 | p 0.77 | p 0.38 | p 0.73 | p 0.29 | ||
| Chest Pain | Separate | 0.61 | 16.1 | −0.61 | 0.25 | 0.92 | −0.08 | −0.31 |
| p-value | p < 0.01 | p < 0.01 | p 0.67 | p 0.13 | p 0.62 | p 0.07 | ||
| AMI | Pooled | 0.47 | 15.2 | −0.27 | −0.92 | 1.99 | 0.3 | −0.66 |
| p-value | p < 0.01 | p 0.33 | p 0.51 | p 0.16 | p 0.42 | p 0.10 | ||
Pooled df = 5,20; Separate df = 5,83
Fig. 4.
Regression model based on Table 1 Pooled Results for ED arrivals.
The outcome variable of chest pain also displayed significant day of the week variation (with Mondays the highest), the R2 was lower at 0.78 and 0.61 for the pooled and non-pooled analysis, respectively. Considering the third outcome measure, AMI revealed a significant R2 of 0.47 for pooled results. Because NHAMCS requires at least 30 records for each data point, we could not produce reliable NHAMCS estimates of AMI by day of the week and year; therefore, only pooled results for AMI are presented. No significant effect was found for AMI by either day of the week or platform.
4. Discussion
Our study demonstrates that in all three platforms, the highest percentages of ED arrivals occur on Mondays. There was a consistent downward trend throughout the week, with the lowest ED arrivals reported on weekends.
This observation could be partly due to the fresh start effect. According to prior studies “Temporal Landmarks Motivate Aspirational Behavior”,16 the beginning of a new year, new month, or new week is thought to provide a mental construct that helps people to dissociate from their past imperfections and start the new calendar cycle with a fresh and health-orientated mindset.16 In 2014, Dai et al. noticed that people tend to take health-related initiatives more seriously at the beginning of a new calendar cycle.16 They realized that the number of internet searches for the word “diet,” as well as the number of gym visits, increased on Mondays.16
Due to this phenomenon, we speculate that overall healthcare utilization increases on Monday simply in an attempt for many to live healthier. The adoption of this mindset at the beginning of the week could be fueled by a few theories.
Many people have a tendency to indulge and make poor health-related choices over the weekend, such as binge drinking or consuming foods that conflict with their dietary restrictions. This may add to their previously described sense of imperfection, prompting them to schedule a checkup immediately afterward to mentally disassociate themselves from self-destructive behavior.
In this case, where the decision to seek medical oversight is made in such a short time (over the weekend), scheduling an appointment with a regular primary care provider may not be feasible, leading to the utilization of the emergency department as an alternative. Additionally, weekend indulgences may increase the risk of injury or illness in anything from an alcohol-related motor vehicle accident to a gout flare-up after a heavy meal.
Socialization during the weekend may also raise health awareness for an individual. For example, a person being visited by a family member might be asked if they have lost weight or be told that they look unwell. This may prompt them to take action on the following Monday.
Every day, a large portion of ED visits are classified as non-urgent encounters.17,18 For a non-life-threatening malady, patients are often less likely to trade in a peaceful weekend for a long wait in an ED waiting room. If lower volume over the weekends is in fact, due to patients’ deliberate planning, then the Monday excess phenomenon could be a repercussion of lower weekend volume.
A true medical emergency is time sensitive. If an illness could be held over to a desired day of the week (in this case, Mondays) with no adverse consequences, there is a higher likelihood of this illness being a non-life-threatening condition. If this theory is true, then Monday ED visitors are expected to be less sick. One way to assess this theory is to look at the variability of inpatient admission rate by day of the week. People with less serious illnesses are less likely to be admitted to the inpatient wards. Hence a lower percentage of inpatient admissions following an ED visit is expected for Mondays. We could not explore this idea further due to resource limitations.
This theory should be approached very carefully as there is a potential risk of underestimating the severity of an illness. In fact, one study demonstrated that patients who are denied ED care during their initial encounter experience higher rates of subsequent hospitalization.19
On the contrary, if a patient deliberately underestimates symptoms of a severe illness to avoid hospitalization over the weekend, a higher percentage of inpatient admissions is expected on the following Monday. This is only true, however, if the patient does not succumb to their illness prior to the ED presentation.
Additionally, the lower volume of patients over the weekend could be explained by the widespread fear of the “weekend effect. “This effect has been described as a higher mortality rate for patients admitted over the weekend compared to those admitted on weekdays.20
This data demonstrates little variability across years for any given day (except for Saturday). From 2016 to 2019, there was a trend of Saturday ED arrivals decreasing by approximately 0.4 percent each year. This might be due to the increased use of urgent care centers, as the statistics from the Urgent Care Association website (gathered by the year of urgent care usage) shows an upward trend during the years of our study.
Similar to our finding with ED arrivals, chest pain was more prevalent on Mondays, with very similar patterns for TriNetX and our regional medical center.
Chest pain is a generic symptom with a broad range of differential diagnosis. Chest pain could be a manifestation of a benign condition, such as acid reflux, or it could be the harbinger of a life-threatening condition, such as angina and myocardial infarction. A high index of suspicion is always required to identify cardiac etiologies since pain arising from heart disease could be highly variable in its characteristics.21
Chest pain is one of the most common chief complaints in the emergency department.22–24; thus, it is not unexpected that there would be an increased prevalence of such a complaint on an ED's busiest day.
Certain weekend activities may involve a sudden shift in one's diet and lifestyle, which can inherently promote cardiac and non-cardiac chest pain. Organizations such as the Centers for Disease Control (CDC) and the American Heart Association (AHA) are making ongoing efforts to promote awareness of the preceding signs and symptoms of AMI.25 Therefore, we believe that many patients take symptoms of chest pain seriously and act upon it in a timely fashion.
For the outcome of chest pain, more variability was displayed for NHAMCS, with a decrease on Thursdays and an increase on Fridays. We speculate that as the work week comes to an end, with deadlines looming, an individual can become more stressed and may ignore any health-related red flags. These individuals may then compensate by increasing their work hours, causing them to be less focused on their physical and mental well-being. This rushed attempt to accomplish their tasks can heighten anxiety levels. This scenario resembles the Venturi effect; in this case, pressure builds due to high anxiety levels from heavy workloads and impending time constraints, and pressure is released upon completion of work the following day. This effect was first described in the 18th century by an Italian physicist, Giovanni Battista Venturi, in the context of fluid dynamics.26
For the diagnosis of AMI, analysis of TriNetX data displayed the least day-of-the-week variability, with the largest percentages occurring on Mondays and the smallest on Sundays. Our regional medical center displayed moderate variability compared to TriNetX. For NHAMCS data, Wednesdays appear to overtake Mondays as the busiest day for AMI-related ED arrivals, although this result is not statistically significant.
As previously described, certain weekend activities can precipitate cardiac events. An AMI can in turn promote the development of fatal tachyar-rhythmias such as ventricular fibrillation (VF).27,28
Post–MI arrhythmias are the leading cause of sudden cardiac death (SCD) following an AMI.29,30 These may occur at any time, from minutes or days (acute) to months or years after the event (subacute and chronic, respectively).31–33 Polymorphic ventricular tachycardia and VF are the most common causes of out-of-hospital sudden death (SCD) following an ischemic event.34,35 Possibly a portion of the patients who develop an extensive AMI over the weekend may never reach the hospital, as they have already succumbed to the illness due to an acute and lethal arrhythmia. The remainder of AMI survivors (likely those with a less extensive myocardial injury) and typical angina will likely present to the ED on the following Monday, which could again explain the high prevalence of chest pain on Mondays. Although chest pain is the most common symptom of MI,36 up to 80% of patients with transient cardiac ischemia never experience chest pain. This is known as silent ischemia, where the commonly known signs and symptoms of an MI are absent.37 Thus, a portion of MI sufferers never experience any chest pain and therefore, never seek medical care. There is an area of concern for such patients, particularly in the setting of a non-ST segment elevation MI (NSTEMI). The ECG interpretation is often contextualized, and these patients’ symptoms may not be taken seriously when ST-segment elevation is not present.38
It has been observed that out of all patients who present to the ED with the chief complaint of chest pain, 31% were found to have acute coronary syndrome. 39 Additionally, nonspecific chest discomfort is one of the most common causes of treat-and-release ED visits.40
We postulate that this subgroup of patients is perhaps those who return to the emergency department with full-blown myocardial infarction or recurrent MI after being released following the initial encounter. Moreover, despite the multidisciplinary efforts of various health organizations to raise awareness for MI,25 societal and demographic knowledge gaps are still present.41 Suboptimal insight into the disease process may play a significant role in patients’ delayed presentation, leading to an undesirable outcome immediately or within the next few days.
Our observation demonstrated a higher rate of ED utilization and CP diagnosis at the beginning of the week. Future studies can evaluate the severity of illness in the patient population by septadian patterns addressing inpatient admission status. This information can improve system awareness and resource allocation with better preparedness and potentially prevent ED overcrowding. Our data at the time of extraction and analysis is limited to pre-SARS-CoV-2 pandemic time. Future initiatives may consider if differences exist in the outcome measures for pre and post-SARS-CoV-2 pandemic time frames.
Footnotes
Conflict of interest
The authors report no conflict of interests.
References
- 1. Salway R, Valenzuela R, Shoenberger J, Mallon W, Viccellio A. Emergency department (ed) overcrowding: evidence-based answers to frequently asked questions. Rev Méd Clín Las Cond. 2017;28(2):213–219. doi: 10.1016/j.rmclc.2017.04.008. [DOI] [Google Scholar]
- 2. Toloo G, Fitzgerald G, Aitken P, Chu K, Ting J, Tippett V. Emergency health services: demand & service delivery models-monograph 1: literature Review and activity trends. 2011 doi: 10.13140/2.1.3944.2889. [DOI] [Google Scholar]
- 3. Burt CW, McCaig LF. Staffing, capacity, and ambulance diversion in emergency departments: United States, 2003–04. Adv Data. 2006;376:1–23. [PubMed] [Google Scholar]
- 4. Karpman M, Menon N, Turcotte J. Polynomial modeling of emergency department arrivals: an analysis of local and national utilization patterns. J Emerg Manag. 2021;19(2):189–196. doi: 10.5055/jem.0569. [DOI] [PubMed] [Google Scholar]
- 5. Asplin BR, Magid DJ, Rhodes KV, Solberg LI, Lurie N, Camargo CA. A conceptual model of emergency department crowding. Ann Emerg Med. 2003;42(2):173–180. doi: 10.1067/mem.2003.302. [DOI] [PubMed] [Google Scholar]
- 6. Bhuiya FA, Pitts SR, McCaig LF. Emergency department visits for chest pain and abdominal pain: United States, 1999–2008. NCHS Data Brief. 2010;43:1–8. [PubMed] [Google Scholar]
- 7.AHA. 2019 heart disease and stroke statistics. American college of cardiology; [Accessed April 21, 2022]. https://www.acc.org/latest-in-cardiology/ten-points-to-remember/2019/02/15/14/39/http%3a%2f%2fwww.acc.org%2flatest-in-cardiology%2ften-points-to-remember%2f2019%2f02%2f15%2f14%2f39%2faha-2019-heart-disease-and-stroke-statistics . [Google Scholar]
- 8. Collart P, Coppieters Y, Godin I, Levêque A. Day-of-the-week variations in myocardial infarction onset over a 27-year period: the importance of age and other risk factors. Am J Emerg Med. 2014;32(6):558–562. doi: 10.1016/j.ajem.2014.02.012. [DOI] [PubMed] [Google Scholar]
- 9. Spielberg C, Falkenhahn D, Willich SN, Wegscheider K, Völler H. Circadian, day-of-week, and seasonal variability in myocardial infarction: comparison between working and retired patients. Am Heart J. 1996;132(3):579–585. doi: 10.1016/s0002-8703(96)90241-0. [DOI] [PubMed] [Google Scholar]
- 10. Witte DR, Grobbee DE, Bots ML, Hoes AW. A meta-analysis of excess cardiac mortality on Monday. Eur J Epidemiol. 2005;20(5):401–406. doi: 10.1007/s10654-004-8783-6. [DOI] [PubMed] [Google Scholar]
- 11. Selvi Y, Smolensky MH, Boysan M, et al. Role of patient chronotype on circadian pattern of myocardial infarction: a pilot study. Chronobiol Int. 2011;28(4):371–377. doi: 10.3109/07420528.2011.559605. [DOI] [PubMed] [Google Scholar]
- 12. Manfredini R, Manfredini F, Boari B, et al. Seasonal and weekly patterns of hospital admissions for nonfatal and fatal myocardial infarction. Am J Emerg Med. 2009;27(9):1097–1103. doi: 10.1016/j.ajem.2008.08.009. [DOI] [PubMed] [Google Scholar]
- 13. Muller JE. Circadian variation in cardiovascular events. Am J Hypertens. 1999;12(2 Pt 2):35S–42S. doi: 10.1016/s0895-7061(98)00278-7. [DOI] [PubMed] [Google Scholar]
- 14. Donaldson K, Stone V, Seaton A, MacNee W. Ambient particle inhalation and the cardiovascular system: potential mechanisms. Environ Health Perspect. 2001;109(Suppl 4):523–527. doi: 10.1289/ehp.01109s4523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Barnett A, Dobson A. Excess in cardiovascular events on Mondays: a meta-analysis and prospective study. J Epidemiol Community Health. 2005;59(2):109–114. doi: 10.1136/jech.2003.019489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Dai H, Milkman KL, Riis J. The fresh start effect: temporal Landmarks motivate aspirational behavior. Manag Sci. 2014;60(10):2563–2582. doi: 10.1287/mnsc.2014.1901. [DOI] [Google Scholar]
- 17. Dinh MM, Russell SB, Bein KJ, et al. Statewide retrospective study of low acuity emergency presentations in New South Wales, Australia: who, what, where and why? BMJ Open. 2016;6(5):e010964. doi: 10.1136/bmjopen-2015-010964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Uscher-Pines L, Pines J, Kellermann A, Gillen E, Mehrotra A. Deciding to visit the emergency department for non-urgent conditions: a systematic Review of the literature. Am J Manag Care. 2013;19(1):47–59. [PMC free article] [PubMed] [Google Scholar]
- 19. Lowe RA, Bindman AB, Ulrich SK, et al. Refusing care to emergency department of patients: evaluation of published triage guidelines. Ann Emerg Med. 1994;23(2):286–293. doi: 10.1016/s0196-0644(94)70042-7. [DOI] [PubMed] [Google Scholar]
- 20. Pauls LA, Johnson-Paben R, McGready J, Murphy JD, Pronovost PJ, Wu CL. The weekend effect in hospitalized patients: a meta-analysis. J Hosp Med. 2017;12(9):760–766. doi: 10.12788/jhm.2815. [DOI] [PubMed] [Google Scholar]
- 21. Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: a report of the American college of cardiology/American heart association joint committee on clinical practice guidelines. Circulation. 2021;144(22):e368–e454. doi: 10.1161/CIR.0000000000001029. [DOI] [PubMed] [Google Scholar]
- 22. Hardy M, Cho A, Stavig A, et al. Understanding frequent emergency department use among primary care patients. Popul Health Manag. 2018;21(1):24–31. doi: 10.1089/pop.2017.0030. [DOI] [PubMed] [Google Scholar]
- 23. Pitts SR, Niska RW, Xu J, Burt CW. National hospital ambulatory medical care Survey: 2006 emergency department summary. Natl Health Stat Report. 2008;7:1–38. [PubMed] [Google Scholar]
- 24. Goodacre S, Cross E, Arnold J, Angelini K, Capewell S, Nicholl J. The health care burden of acute chest pain. Heart. 2005;91(2):229–230. doi: 10.1136/hrt.2003.027599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Fang J. Awareness of heart attack symptoms and response among adults — United States, 2008–2014 and 2017. MMWR Morb Mortal Wkly Rep. 2019;68 doi: 10.15585/mmwr.mm6805a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Venturi effect. Wikipedia; 2022. [Accessed May 30, 2022]. https://en.wikipedia.org/w/index.php?title=Venturi_effect&oldid=1087666226 . [Google Scholar]
- 27. Henkel DM, Witt BJ, Gersh BJ, et al. Ventricular arrhythmias after acute myocardial infarction: a 20-year community study. Am Heart J. 2006;151(4):806–812. doi: 10.1016/j.ahj.2005.05.015. [DOI] [PubMed] [Google Scholar]
- 28. Khairy P, Thibault B, Talajic M, et al. Prognostic significance of ventricular arrhythmias post-myocardial infarction. Can J Cardiol. 2003;19(12):1393–1404. [PubMed] [Google Scholar]
- 29. Zipes DP, Wellens HJ. Sudden cardiac death. Circulation. 1998;98(21):2334–2351. doi: 10.1161/01.cir.98.21.2334. [DOI] [PubMed] [Google Scholar]
- 30. Savard P, Rouleau JL, Ferguson J, et al. Risk stratification after myocardial infarction using signal-averaged electrocardiographic criteria adjusted for sex, age, and myocardial infarction location. Circulation. 1997;96(1):202–213. doi: 10.1161/01.cir.96.1.202. [DOI] [PubMed] [Google Scholar]
- 31. Al-Khatib SM, Stebbins AL, Califf RM, et al. Sustained ventricular arrhythmias and mortality among patients with acute myocardial infarction: results from the GUSTO-III trial. Am Heart J. 2003;145(3):515–521. doi: 10.1067/mhj.2003.170. [DOI] [PubMed] [Google Scholar]
- 32. Mont L, Cinca J, Blanch P, et al. Predisposing factors and prognostic value of sustained monomorphic ventricular tachycardia in the early phase of acute myocardial infarction. J Am Coll Cardiol. 1996;28(7):1670–1676. doi: 10.1016/S0735-1097(96)00383-X. [DOI] [PubMed] [Google Scholar]
- 33. Askari AT, Shishehbor MH, Kaminski MA, et al. The association between early ventricular arrhythmias, renin-angiotensin-aldosterone system antagonism, and mortality in patients with ST-segment-elevation myocardial infarction: insights from Global Use of Strategies to Open coronary arteries (GUSTO) V. Am Heart J. 2009;158(2):238–243. doi: 10.1016/j.ahj.2009.05.023. [DOI] [PubMed] [Google Scholar]
- 34. Koplan BA, Stevenson WG. Ventricular tachycardia and sudden cardiac death. Mayo Clin Proc. 2009;84(3):289–297. doi: 10.4065/84.3.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Pogwizd SM, Corr PB. Mechanisms underlying the development of ventricular fibrillation during early myocardial ischemia. Circ Res. 1990;66(3):672–695. doi: 10.1161/01.res.66.3.672. [DOI] [PubMed] [Google Scholar]
- 36. Malik MA, Alam Khan S, Safdar S, Taseer IUH. Chest Pain as a presenting complaint in patients with acute myocardial infarction (AMI) Pakistan J Med Sci. 2013;29(2):565–568. doi: 10.12669/pjms.292.2921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gul Z, Makaryus AN. Stat-Pearls. StatPearls Publishing; 2022. [Accessed May 30, 2022]. Silent myocardial ischemia. http://www.ncbi.nlm.nih.gov/books/NBK536915/ [PubMed] [Google Scholar]
- 38. Zdzienicka J, Siudak Z, Zawiślak B, et al. Patients with non-ST-elevation myocardial infarction and without chest pain are treated less aggressively and experience higher in-hospital mortality. Kardiol Pol. 2007;65(7):769–775. discussion 776–777. [PubMed] [Google Scholar]
- 39. Fruergaard P, Launbjerg J, Hesse B, et al. The diagnoses of patients admitted with acute chest pain but without myocardial infarction. Eur Heart J. 1996;17(7):1028–1034. doi: 10.1093/oxfordjournals.eurheartj.a014998. [DOI] [PubMed] [Google Scholar]
- 40.Weiss AJ, Wier LM, Stocks C, Blanchard J. Healthcare cost and utilization project (HCUP) statistical briefs. Agency for Healthcare Research and Quality (US); 2006. [Accessed April 21, 2022]. Overview of emergency department visits in the United States, 2011: statistical brief #174. http://www.ncbi.nlm.nih.gov/books/NBK235856/ [PubMed] [Google Scholar]
- 41. Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart disease and stroke statistics—2017 update: a report from the American heart association. Circulation. 2017;135(10):e146–e603. doi: 10.1161/CIR.0000000000000485. [DOI] [PMC free article] [PubMed] [Google Scholar]