Abstract
Background:
Telehealth and enabling services are promising approaches to address the intersecting challenges of chronic disease burden, a growing aging population, and poor access to care disproportionately affecting rural areas. Using potentially preventable hospitalizations (PPHs) as an indicator for health system efficiency and quality, this study examined the relationship between health information technology and hospital-provided enabling services on PPHs across rural, micropolitan, and metropolitan areas.
Methods:
We constructed a patient-, hospital-, community-, and state-level data set using the Medicare fee-for-service claims file and the Medicare Master Beneficiary Summary File, and the American Hospital Association Annual Survey. Logistic regressions were applied to examine associations between PPH and telehealth post-discharge, telehealth treatment, and telehealth post-discharge and enabling services.
Results:
Approximately 50% of rural and micropolitan residents (vs. 36% of urban residents) were treated in hospitals providing neither telehealth post-discharge services nor enabling services, and 7% (vs. 11% of urban residents) were treated in hospitals with both services. Telehealth post-discharge services were associated with significantly lower odds ratio (OR) of having any PPH due to acute (OR = 0.91, p < 0.001) and chronic conditions (OR = 0.94, p < 0.001). The ORs of having any PPH due to acute and chronic conditions were the least among beneficiaries who were treated in hospitals with both telehealth post-discharge and enabling services (OR = 0.56, p < 0.001, for acute conditions, and OR = 0.73, p < 0.001, for chronic conditions).
Conclusions:
Hospital use of post-discharge telehealth alongside enabling services may help provide timely access to care, improve care coordination, and reduce PPHs for older rural residents.
Keywords: telehealth, enabling services, potentially preventable hospitalizations, rural health disparities, telemedicine, telehealth
Introduction
Recent data from the U.S. Census show that more than one in every five (22.9%) older Americans live in rural areas, while from 1980 to 2016, the size of the older adult population in rural areas has grown more than those residing in urban areas during the same period (10.9–17.5% compared with 11.4–13.8%, respectively).1 Rural populations face unique health and aging challenges, where rural–urban and within-rural disparities are large, growing, and persistent.2,3 Several risk factors, including smoking, obesity, and physical inactivity, contribute to high needs of health care and public health services given rural–urban disparities in mortality rates due to conditions such as heart disease, stroke, and cancer.4
Potentially preventable hospitalizations (PPHs) are unplanned hospital admissions for certain acute illnesses or chronic conditions that might have been avoided by high-quality outpatient treatment and disease management in primary care settings.5 They can serve as potential markers of health system efficiency since the lack of access to health care and poor quality care can lead to increases in these types of hospitalizations.6 However, access and quality vary widely in rural and urban areas, where rural areas have greater shortages in health care services and providers7–9 and more barriers to telehealth adoption.10–13 This results in a higher incidence of health disparities in rural areas,14,15 which are home to larger proportions of older adults.16
Increased availability of telehealth services could potentially improve access to health services and disease management programs by eliminating transportation and travel challenges in rural areas.12,17 Telehealth services have increasingly become reimbursable by the Center for Medicare and Medicaid Services (CMS) and have been vastly expanded amidst the COVID-19 pandemic.18–20 In an average week before the COVID-19 public health emergency declaration, about 13,000 Medicare beneficiaries received services via telehealth, compared with about 1.7 million in late April 2020.20 While evidence shows rural beneficiaries utilizing less telehealth than urban beneficiaries,20 this could be due to lower telehealth adoption in rural areas.10
To address these disparities, access barriers, and other social determinants of health, many health centers provide “enabling services” that help patients access health care, such as transportation services and/or referrals to local social services agencies.21,22 When provided immediately post-hospital discharge, enabling services may help decrease preventable readmissions by connecting patients to primary care. Although research on enabling services is limited, they have been associated with improvements in health care access and patient satisfaction.21 These services are not systematically implemented across the nation because they have historically been inadequately funded by short-term grants and some insurance providers.22,23
Improvements in health information technology (HIT) and provision of enabling services are among several population health approaches that have shown promise in addressing the intersecting challenges of chronic disease burden, a growing aging population, and poor access to care in rural areas.21 There is growing evidence to support the important role that telehealth plays in reducing preventable hospitalizations.24 Hospitals provide critical health care resources for the aging and underserved patients. Care needs must be thoughtfully coordinated to prevent post-acute care utilization. Evidence demonstrating the effectiveness of the combination of telehealth and enabling services in the hospital setting is limited.
This study examines the relationship between HIT and hospital-provided enabling services on PPHs across rural, suburban, and metropolitan areas. We hypothesize that hospitals with capabilities to provide telehealth services post-discharge have lower rates of PPHs, and the combination of post-discharge telehealth capabilities and provision of enabling services is further related to lower odds of PPHs. This combination of services could reduce PPHs due to higher levels of patient engagement and improved care coordination as shown in outpatient safety net clinics.25 Finally, we hypothesize that the reductions of the likelihood of having PPH would be more substantial among patients residing in rural areas, who face more challenges in accessing high-quality care, compared with patients living in urban areas.
Methods
DATA
The main data sets used were the 100% inpatient Medicare fee-for-service (FFS) claims file for calendar year 2017 merged with the Medicare Master Beneficiary Summary File. We linked the CMS data with the American Community Survey (ACS) using beneficiaries' zip codes. CMS claims data were also linked to the 2017 American Hospital Association (AHA) Annual Survey, which tracks detailed measures of services hospitals provided (including the enabling services) and HIT functions hospital adopted. Hence, we constructed a patient-, hospital-, community-, and state-level data set, using a geographic identifier and the Medicare provider ID.
SAMPLE
Our sample included community-dwelling Medicare FFS beneficiaries, aged 65 years and older, with continuous enrollment in 2017 and who had at least one hospital visit in 2017. Elderly patients with Medicare Advantage or dual-eligible patients were not included. Our final sample size included 3,540,442 beneficiaries. Using the Core-Based Statistical Areas (CBSAs) in the AHA data, residents were divided into three geographical categories: rural (n = 155,288), suburban (n = 574,063), and urban (n = 2,531,601).26
MEASURES
The dependent variable was a PPH for any acute or chronic condition. Using the Prevention Quality Indicators (PQIs) developed by the Agency for Healthcare Research and Quality, ICD-10-CM diagnosis codes were used to identify conditions.27 Composite scores were generated for acute (PQI 91) and chronic (PQI 92) conditions.
We created the key independent variables of hospital-based telehealth using the AHA data. Different measures were tested in the sensitivity analysis. We categorized the telehealth measures into two groups and created dichotomous variables: (1) telehealth post-discharge, which equaled 1 if a hospital adopted any remote patient monitoring: post-discharge and ongoing chronic care management, and 0 otherwise; and (2) telehealth treatment, which equaled 1 if a hospital adopted any telehealth consultation and office visits, Electronic Intensive Care Unit, stroke care, or psychiatric and addiction treatment.
Enabling services was defined as a program designed to help patients access health care services by offering any of the following: transportation services and/or referrals to local social services agencies. Hospitals reported whether or not enabling services were provided at their hospital (1 = “yes” or 0 = “no”). We were interested to study the continuous provision of services post-discharge (i.e., post-discharge + enabling services). Hence, we crossed tabulated these two measures and categorized hospitals into four groups: with or without telehealth post-discharge and/or enabling services.
Covariates included various characteristics at the patient, hospital, and community levels. The Medicare enrollment file was used to collect patient-level characteristics (age, sex, and race/ethnicity). A frailty index was created using the approach employed by Ouayogode et al.28 We also used definitions of chronic conditions provided by the CMS chronic conditions data warehouse29 and controlled for number of major chronic conditions beneficiaries had. Hospital-level characteristics included teaching status, ownership type, and bed size. Community-level characteristics included geography, percentage of the population in poverty, percentage of the African American population, percentage of the population with greater than high school education, and number of medical doctors per 1,000 residents.
ANALYSIS
We first presented characteristics of beneficiaries (and hospitals, communities) by rural and urban areas. More than 70% of the beneficiaries visited the same hospital. We created beneficiary hospital-level data to account for the situations where beneficiaries visited multiple hospitals and we adjusted for the weight of the number of hospitals in the regressions. Logistic regressions were applied to examine the associations between telehealth post-discharge, telehealth treatment, and telehealth post-discharge and enabling services with PPH for any acute or chronic condition. We also tested interactions between telehealth and rural/urban measures and controlled for state fixed effects. STATA15 MP4 was used for the analysis.
We implemented sensitivity analyses to test the robustness of the results. We applied the principal component and factor analysis.30 Two factors were predicted: (1) associated with telehealth treatment services and (2) associated with telehealth post-discharge services, when we set eigenvalue as 1. We also set eigenvalue as 0.8 in the factor analysis, using an overall telehealth measure. We also tested different model specifications using different geographic measures, including the area deprivation index.31 Results were similar and are available upon request. The study was approved by the University of Maryland Institutional Review Board.
Results
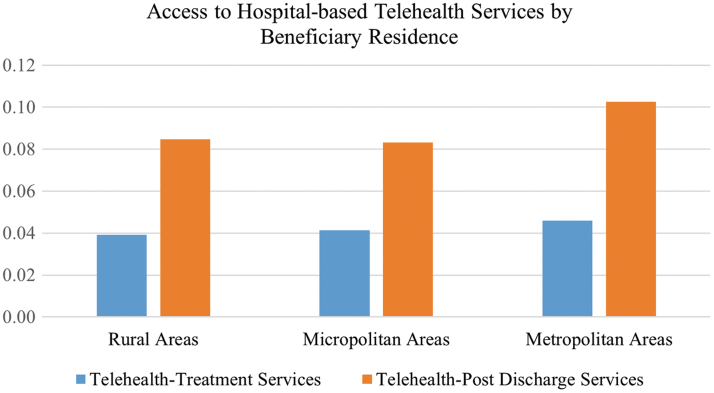
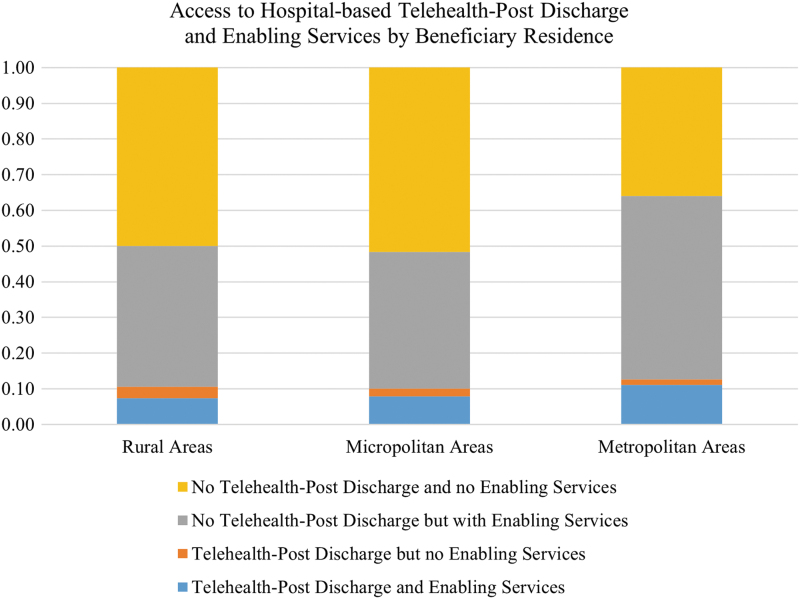
Approximately 8% (or 4%) of Medicare beneficiaries from rural and suburban areas who had any hospital stay in 2017 were treated in hospitals offering telehealth post-discharge services (or telehealth treatment services), compared with 10% (or 5%) of beneficiaries in urban areas, as shown in Figure 1. Figure 2 shows that ∼50% of rural and micropolitan residents (vs. 36% of urban residents) were treated in hospitals providing neither telehealth post-discharge services nor enabling services, and 7% (vs. 11% of urban residents) were treated in hospitals with both services.
Fig. 1.
Access to hospital-based telehealth services by beneficiary residence. Our sample included community-dwelling Medicare fee-for-services beneficiaries, aged 65 years and older, with continuous enrollment in 2017 and who had at least one hospital visit in 2017. Elderly patients with Medicare Advantage or dual-eligible patients were not included. Telehealth post-discharge was a binary measure indicating whether a hospital adopted any remote patient monitoring: post-discharge; and remote patient monitoring: ongoing chronic care management. Telehealth treatment was a binary measure indicating whether a hospital adopted any telehealth consultation and office visits, Electronic Intensive Care Unit, stroke care, or psychiatric and addiction treatment. T-tests were also implemented to compare the differences of telehealth treatment and telehealth post-discharge by beneficiary residence, using metropolitan areas as the reference group. All differences were statistically significant at 95% confidence interval.
Fig. 2.
Access to hospital-based telehealth post-discharge and enabling services by beneficiary residence. Enabling services (the AHA definition): “A program that is designed to help the patient access health care services by offering any of the following linguistic services, transportation services, and/or referrals to local social services agencies.” T-tests were also implemented to compare the differences of adopting none, either, or both telehealth post-discharge and enabling services by hospital locations, using metropolitan areas as the reference group. All differences were statistically significant at 95% confidence interval. AHA, American Hospital Association.
Table 1 presents the comparisons of population characteristics by rurality. The likelihoods of having any PPH due to acute and chronic conditions were relatively higher in rural and micropolitan areas (0.09 vs. 0.07, p < 0.001, for PPH for acute conditions, and 0.13 vs. 0.12, p < 0.001, for PPH for chronic conditions), compared with the rates for beneficiaries living in urban areas. Compared with residents in urban areas, rural and suburban residents were less likely to be aged 85+ years, White, and fragile. They were also less likely to be treated in teaching hospitals, hospitals with bed size >200, and more likely to be treated in government-owned hospitals. Compared with urban counterparts, they were more likely to live in neighborhoods with lower rates of high school degrees, low rates of Black residents, higher poverty rates, and lower per physician to resident ratios.
Table 1.
Characteristics of Beneficiaries, Hospitals, and Communities by Beneficiary Residence
| TOTAL |
METROPOLITAN AREAS |
RURAL AREAS |
MICROPOLITAN AREAS |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
N = 3,260,952
|
N = 2,531,601
|
N = 155,288
|
N = 574,063
|
|||||||
| MEAN | SD | MEAN | SD | MEAN | SD | p | MEAN | SD | p | |
| Telehealth treatment services | 0.04 | 0.21 | 0.05 | 0.21 | 0.04 | 0.19 | <0.001 | 0.04 | 0.20 | <0.001 |
| Telehealth post-discharge services | 0.10 | 0.30 | 0.10 | 0.30 | 0.08 | 0.28 | <0.001 | 0.08 | 0.28 | <0.001 |
| No telehealth post-discharge and no enabling services | 0.39 | 0.49 | 0.36 | 0.48 | 0.50 | 0.50 | <0.001 | 0.52 | 0.50 | <0.001 |
| Telehealth post-discharge but no enabling services | 0.02 | 0.13 | 0.02 | 0.13 | 0.03 | 0.17 | <0.001 | 0.02 | 0.15 | <0.001 |
| No telehealth post-discharge but with enabling services | 0.48 | 0.50 | 0.51 | 0.50 | 0.40 | 0.49 | <0.001 | 0.38 | 0.49 | <0.001 |
| Telehealth post-discharge and enabling services | 0.10 | 0.30 | 0.11 | 0.31 | 0.07 | 0.26 | <0.001 | 0.08 | 0.27 | <0.001 |
| BENEFICIARY CHARACTERISTICS | ||||||||||
| Any PPH for acute conditions | 0.08 | 0.27 | 0.08 | 0.27 | 0.09 | 0.29 | <0.001 | 0.09 | 0.28 | <0.001 |
| Any PPH for chronic conditions | 0.13 | 0.33 | 0.12 | 0.33 | 0.13 | 0.34 | <0.001 | 0.13 | 0.34 | <0.001 |
| Age, years | ||||||||||
| 65–74 | 0.49 | 0.50 | 0.49 | 0.50 | 0.50 | 0.50 | <0.001 | 0.50 | 0.50 | <0.001 |
| 75–84 | 0.35 | 0.48 | 0.34 | 0.47 | 0.35 | 0.48 | <0.001 | 0.35 | 0.48 | <0.001 |
| 85 and older | 0.16 | 0.37 | 0.17 | 0.37 | 0.14 | 0.35 | <0.001 | 0.14 | 0.35 | <0.001 |
| Sex | ||||||||||
| Male | 0.49 | 0.50 | 0.51 | 0.50 | 0.52 | 0.50 | <0.001 | 0.50 | 0.50 | <0.001 |
| Female | 0.51 | 0.50 | 0.51 | 0.50 | 0.48 | 0.50 | <0.001 | 0.50 | 0.50 | <0.001 |
| Race and ethnicity | ||||||||||
| White | 0.86 | 0.34 | 0.85 | 0.36 | 0.88 | 0.32 | <0.001 | 0.91 | 0.28 | <0.001 |
| Black | 0.07 | 0.25 | 0.07 | 0.26 | 0.06 | 0.24 | <0.001 | 0.04 | 0.19 | <0.001 |
| Hispanic | 0.03 | 0.18 | 0.04 | 0.19 | 0.02 | 0.16 | <0.001 | 0.02 | 0.14 | <0.001 |
| Asian | 0.01 | 0.11 | 0.02 | 0.12 | 0.00 | 0.07 | <0.001 | 0.00 | 0.06 | <0.001 |
| Native | 0.01 | 0.07 | 0.00 | 0.05 | 0.02 | 0.12 | <0.001 | 0.01 | 0.11 | <0.001 |
| Unknown | 0.01 | 0.11 | 0.01 | 0.11 | 0.01 | 0.10 | <0.001 | 0.01 | 0.10 | <0.001 |
| Other race | 0.01 | 0.08 | 0.01 | 0.08 | 0.00 | 0.06 | <0.001 | 0.00 | 0.06 | <0.001 |
| Health conditions | ||||||||||
| Frailty index | 0.45 | 0.50 | 0.44 | 0.50 | 0.46 | 0.50 | <0.001 | 0.48 | 0.50 | <0.001 |
| No. of major chronic conditions | 2.76 | 1.32 | 2.76 | 1.32 | 2.71 | 1.34 | <0.001 | 2.77 | 1.33 | <0.001 |
| Hospital characteristics | ||||||||||
| Teaching | 0.18 | 0.38 | 0.20 | 0.40 | 0.12 | 0.32 | <0.001 | 0.12 | 0.32 | <0.001 |
| For-profit | 0.17 | 0.38 | 0.18 | 0.38 | 0.17 | 0.38 | <0.001 | 0.16 | 0.37 | <0.001 |
| Non-for-profit | 0.73 | 0.45 | 0.74 | 0.44 | 0.67 | 0.47 | <0.001 | 0.68 | 0.46 | <0.001 |
| Government | 0.10 | 0.30 | 0.08 | 0.28 | 0.16 | 0.36 | <0.001 | 0.16 | 0.36 | <0.001 |
| Bed size ≤50 | 0.06 | 0.24 | 0.04 | 0.19 | 0.14 | 0.34 | <0.001 | 0.15 | 0.35 | <0.001 |
| Bed size 50–200 | 0.26 | 0.44 | 0.23 | 0.42 | 0.29 | 0.45 | <0.001 | 0.35 | 0.48 | <0.001 |
| Bed size ≥200 | 0.68 | 0.47 | 0.73 | 0.44 | 0.57 | 0.49 | <0.001 | 0.51 | 0.50 | <0.001 |
| Community characteristics | ||||||||||
| % Population with high school degrees | 88.89 | 7.31 | 89.59 | 7.22 | 85.93 | 7.29 | <0.001 | 86.33 | 7.01 | <0.001 |
| % Population living in poverty | 13.18 | 8.02 | 12.27 | 7.84 | 16.56 | 8.71 | <0.001 | 16.59 | 7.59 | <0.001 |
| % Black population | 10.51 | 16.13 | 11.32 | 16.57 | 7.36 | 14.90 | <0.001 | 7.55 | 13.81 | <0.001 |
| % MD per 1,000 resident | 0.71 | 0.32 | 0.77 | 0.30 | 0.35 | 0.33 | <0.001 | 0.55 | 0.26 | <0.001 |
Data source: The main data sets used were the 100% inpatient Medicare FFS claims file for calendar year 2017 merged with the Medicare Master Beneficiary Summary File. We linked the CMS data with the ACS using beneficiaries' zip codes. CMS claims data were also linked to the 2017 AHA Annual Survey, which tracks detailed measures of services hospitals provided (including the enabling services) and HIT functions hospital adopted. Our sample included community-dwelling Medicare FFS beneficiaries, aged 65 years and older, with continuous enrollment in 2017 and who had at least one hospital visit in 2017. Elderly patients with Medicare Advantage or dual-eligible patients were not included. Any PPH for acute conditions: the measure was created according to the PQI 91 acute composite—PQI composite of acute conditions including dehydration, bacterial pneumonia, or urinary tract infection. Any PPH for chronic conditions: the measure was created according to the PQI 92 chronic composite—PQI composite of chronic conditions including diabetes with short-term complications, diabetes with long-term complications, uncontrolled diabetes without complications, diabetes with lower extremity amputation, chronic obstructive pulmonary disease, asthma, hypertension, or heart failure without a cardiac procedure. Number of diseases: depression, AMI, asthma, heart failure, COPD, diabetes, hyperlipidemia, and hypertension.
ACS, American Community Survey; AHA, American Hospital Association; AMI, Acute Myocardial Infarction; COPD, Chronic Obstructive Pulmonary Disease; FFS, fee-for-service; HIT, health information technology; PPH, potentially preventable hospitalization; PQI, Prevention Quality Indicators; SD, standard deviation.
Table 2 presents the regression results. Model 1 presents results of unit regression, only controlling for rural and micropolitan areas, with metropolitan areas as the reference group. Results showed that the rates of having any PPH for acute conditions were higher among patients residing in rural and micropolitan areas (odds ratio [OR] = 1.16, p < 0.001, for rural areas, OR = 1.12, p < 0.001, for micropolitan areas, with metropolitan areas as the reference group). The rates of having any PPH for chronic conditions were higher in rural and micropolitan areas (OR = 1.02, p < 0.05, for rural areas, OR = 1.06, p < 0.001, for micropolitan areas, with metropolitan areas as the reference group). Model 2 presents the results controlling for all the covariates presented in Table 1, and the interaction terms between hospital-based telehealth services with rural and micropolitan areas.
Table 2.
Rates of Potentially Preventable Hospitalizations by Beneficiary Residence and Hospital-Based Telehealth Treatment and Telehealth Post-Discharge Services
| |
ANY PPH FOR ACUTE CONDITIONS |
ANY PPH FOR CHRONIC CONDITIONS |
||||||
|---|---|---|---|---|---|---|---|---|
| MODEL 1 | OR | 95% CI | p | OR | 95% CI | p | ||
| Metropolitan areas | Reference | Reference | ||||||
| Rural areas | 1.16 | 1.14 | 1.18 | <0.001 | 1.02 | 1.00 | 1.03 | 0.04 |
| Micropolitan areas | 1.12 | 1.11 | 1.13 | <0.001 | 1.06 | 1.05 | 1.07 | <0.001 |
| MODEL 2: FULL MODEL | OR | 95% CI | p | OR | 95% CI | p | ||
|---|---|---|---|---|---|---|---|---|
| Rural areas |
1.08 |
1.05 |
1.11 |
<0.001 |
0.95 |
0.93 |
0.97 |
<0.001 |
| Micropolitan areas |
1.00 |
0.99 |
1.02 |
0.48 |
0.96 |
0.94 |
0.97 |
<0.001 |
| Telehealth: post-discharge services |
0.91 |
0.90 |
0.93 |
<0.001 |
0.94 |
0.93 |
0.96 |
<0.001 |
| Telehealth: post-discharge services × rural areas |
0.71 |
0.65 |
0.78 |
<0.001 |
0.83 |
0.76 |
0.89 |
<0.001 |
| Telehealth: post-discharge services × micropolitan areas |
0.80 |
0.76 |
0.84 |
<0.001 |
0.85 |
0.82 |
0.88 |
<0.001 |
| Telehealth: treatment services |
0.97 |
0.94 |
0.99 |
0.01 |
1.01 |
0.99 |
1.04 |
0.25 |
| Telehealth: treatment services × rural areas |
0.91 |
0.79 |
1.04 |
0.17 |
0.88 |
0.78 |
0.99 |
0.04 |
| Telehealth: treatment services × micropolitan areas | 0.84 | 0.79 | 0.90 | <0.001 | 0.90 | 0.86 | 0.95 | <0.001 |
Data source: The main data sets used were the 100% inpatient Medicare FFS claims file for calendar year 2017 merged with the Medicare Master Beneficiary Summary File. We linked the CMS data with the ACS using beneficiaries' zip codes. CMS claims data were also linked to the 2017 AHA Annual Survey, which tracks detailed measures of services hospitals provided (including the enabling services) and HIT functions hospital adopted. Our sample included community-dwelling Medicare FFS beneficiaries, aged 65 years and older, with continuous enrollment in 2017 and who had at least one hospital visit in 2017. Elderly patients with Medicare Advantage or dual-eligible patients were not included. Our final sample size included 3,540,442 beneficiaries. Using the CBSAs in AHA data, residents were divided into three geographical categories: rural (n = 155,288), suburban (n = 574,063), and urban (n = 2,531,601). Model 1 presents results of unit regression, only controlling for rural and micropolitan areas, with metropolitan areas as the reference group. Model 2 presented the results controlling for the covariates presented in Table 1.
CBSA, Core-Based Statistical Area; CI, confidence interval; OR, odds ratio.
Results showed that telehealth post-discharge services were associated with significantly lower OR of having any PPH due to acute (OR = 0.91, p < 0.001) and chronic conditions (OR = 0.94, p < 0.001). The interaction terms of rural and telehealth post-discharge services were significantly lower (OR = 0.91, p < 0.001, for PPH due to acute conditions, and OR = 0.83, p < 0.001, for PPH due to chronic conditions). Telehealth treatment services were associated with a significant reduction of PPH due to acute conditions (OR = 0.97, p = 0.01), but not chronic conditions (OR = 1.01, p = 0.25). The interaction terms of telehealth treatment services and rural (OR = 0.91, p = 0.17, for PPH due to acute conditions, and OR = 0.88, p = 0.04, for PPH due to chronic conditions) and micropolitan areas (OR = 0.84, p < 0.001, for PPH due to acute conditions, and OR = 0.90, p < 0.001, for PPH due to chronic conditions) were also associated with lower PPH rates.
Table 3 presents the results of the combined hospital-based telehealth post-discharge services and hospital provision of enabling services. The ORs of having any PPH due to acute and chronic conditions were the least among beneficiaries who were treated in hospitals with both telehealth post-discharge and enabling services (OR = 0.56, p < 0.001, for PPH due to acute conditions, and OR = 0.73, p < 0.001, for PPH due to chronic conditions). ORs of interaction terms of hospitals with both telehealth post-discharge and enabling services were also the least in both regressions of PPHs, compared with ORs of having either telehealth post-discharge or enabling services, or neither of these two services.
Table 3.
Rates of Potentially Preventable Hospitalizations by Beneficiary Residence and Hospital-Based Telehealth Post-Discharge and Enabling Services
| FULL MODEL | ANY PPH FOR ACUTE CONDITIONS |
ANY PPH FOR CHRONIC CONDITIONS |
||||||
|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | |||
| Metropolitan areas | Reference | Reference | ||||||
| Rural areas | 1.18 | 1.15 | 1.23 | <0.001 | 1.00 | 0.97 | 1.04 | 0.80 |
| Micropolitan areas | 1.07 | 1.05 | 1.09 | <0.001 | 1.01 | 0.99 | 1.02 | 0.37 |
| No telehealth post-discharge and no enabling services | Reference | Reference | ||||||
| Telehealth post-discharge but no enabling services | 0.87 | 0.83 | 0.91 | <0.001 | 0.97 | 0.93 | 1.01 | 0.11 |
| No telehealth post-discharge but with enabling services | 0.99 | 0.97 | 1.00 | 0.03 | 1.00 | 0.99 | 1.01 | 0.49 |
| Telehealth post-discharge and enabling services | 0.89 | 0.88 | 0.91 | <0.001 | 0.93 | 0.91 | 0.94 | <0.001 |
| Telehealth post-discharge but no enabling services × rural area | 0.79 | 0.68 | 0.91 | <0.001 | 0.84 | 0.74 | 0.95 | 0.01 |
| No telehealth post-discharge but with enabling services × rural area | 0.70 | 0.66 | 0.74 | <0.001 | 0.81 | 0.77 | 0.85 | <0.001 |
| Telehealth post-discharge and enabling services × rural area | 0.56 | 0.50 | 0.64 | <0.001 | 0.73 | 0.66 | 0.80 | <0.001 |
| Telehealth post-discharge but no enabling services × micropolitan areas | 0.87 | 0.80 | 0.95 | <0.001 | 0.85 | 0.78 | 0.91 | <0.001 |
| No telehealth post-discharge but with enabling services × micropolitan areas | 0.79 | 0.77 | 0.82 | <0.001 | 0.82 | 0.80 | 0.84 | <0.001 |
| Telehealth post-discharge and enabling services × micropolitan areas | 0.69 | 0.65 | 0.73 | <0.001 | 0.78 | 0.74 | 0.81 | <0.001 |
Data source: The main data sets used were the 100% inpatient Medicare FFS claims file for calendar year 2017 merged with the Medicare Master Beneficiary Summary File. We linked the CMS data with the ACS using beneficiaries' zip codes. CMS claims data were also linked to the 2017 AHA Annual Survey, which tracks detailed measures of services hospitals provided (including the enabling services) and HIT functions hospital adopted. Our sample included community-dwelling Medicare FFS beneficiaries, aged 65 years and older, with continuous enrollment in 2017 and who had at least one hospital visit in 2017. Elderly patients with Medicare Advantage or dual-eligible patients were not included. Our final sample size included 3,540,442 beneficiaries. Using the CBSAs in AHA data, residents were divided into three geographical categories: rural (n = 155,288), suburban (n = 574,063), and urban (n = 2,531,601). All the models (full model) controlled for the covariates presented in Table 1.
Discussion
The expansion of telehealth during the pandemic underscores its importance to increasing health care access, although more work remains to further increase access particularly in rural areas.32 Recent study suggested the potential to apply hospital-based telehealth services among the aging population with dementia, a high-risk and high-cost population.33 Our study further demonstrated a connection between hospital telehealth adoption and reduced PPH especially for all the aging rural residents. Hospital use of telehealth post-treatment and for ongoing chronic care management may help provide timely access to care and improve care coordination. The recently released CMS final Physician Fee Schedule Payment Policies keeps certain telehealth provisions in place through 2023,34 but additional congressional action will be needed to ensure that telehealth expansions from COVID-19 become permanent.32,35
Our study also showed a lower likelihood of PPH (for both acute and chronic conditions) when a hospital reported provision of enabling services alongside post-discharge telehealth. This finding underscores the important role that enabling services can play in helping to address the needs of vulnerable populations. Enabling services are a hallmark of community health centers; nationally, the number of health centers employing staff to provide enabling services grew by 30% between 2010 and 2019.36 Enabling services are not directly reimbursed by CMS unless provided as a part of reimbursable care coordination services and provided by a billable service provider.
There are likely contextual differences between enabling services provided in hospitals compared with those provided in primary care settings; future studies should examine these differences to better understand the mechanisms by which enabling services contribute to improved health outcomes post-hospitalization. In the shift toward value-based care, an improved understanding of the role of enabling services will be needed as more primary care offices become affiliated with hospitals and larger health systems.
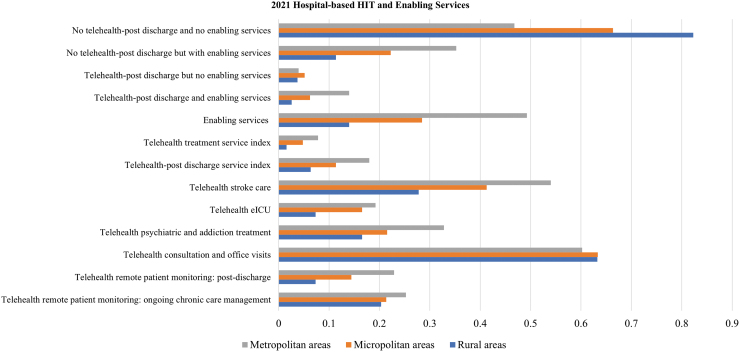
Finally, we would like to note that similar patterns were observed in 2021, during/post the COVID-19 pandemic. Although we were not able to link hospital-based HIT and enabling services with 2021 due to the availability of the CMS 2021 data, we produced evidence of hospital-based HIT using the recently released 2021 AHA annual survey (Fig. 3). More than 82% of hospitals in rural areas reported neither telehealth post-discharge services nor enabling services, compared with 47% of hospitals in metropolitan areas. The adoption of digital health care likely will play a more critical role after the COVID-19 pandemic. The results of our study suggest the importance of focusing on the digital divide between urban and rural hospitals.
Fig. 3.
2021 Hospital-based HIT and enabling services. Author's analysis using the 2021 AHA Annual Survey. General medical and surgical hospitals were included. (1) Telehealth post-discharge service index, which equaled 1 if a hospital adopted any remote patient monitoring: post-discharge and ongoing chronic care management, and 0 otherwise; and (2) telehealth treatment index, which equaled 1 if a hospital adopted any telehealth consultation and office visits, Electronic Intensive Care Unit, stroke care, or psychiatric and addiction treatment. Enabling services (the AHA definition): “A program that is designed to help the patient access health care services by offering any of the following linguistic services, transportation services, and/or referrals to local social services agencies.” HIT, health information technology.
Myriad factors contribute to PPH in general and in rural contexts among the elderly,37 including use of rural health clinics,38 access to specialists,39 and other structural, patient-related, and geographic variations.40–42 As constructed, the linked data set used in this study is unable to fully examine the complexity of factors contributing to PPH in the rural elderly population; thus, our study has several limitations. First, our sample is limited to the community-dwelling Medicare FFS population. Future studies may examine the role of telehealth in the post-acute care settings (e.g., long-term care hospitals, inpatient rehabilitation facilities, skilled nursing facilities, and home health agencies).
Second, telehealth and enabling services were only coded as yes if they were provided directly by the hospital, which does not necessarily indicate patients' actual use of these services. We implemented an intent-to-treat analysis assuming that patients had equal opportunities to access such services if they were admitted into the same hospitals. Third, using claims data, we were unable to capture more specific measures on beneficiaries' socioeconomic status, such as education or income, that might be associated with the likelihood of having PPHs. Finally, our analysis was cross-sectional. Our study identified association between having PPH and availability of hospital-telehealth and enabling services. Future research may use longitudinal data to estimate causality.
Conclusions
Our findings demonstrated that the combination of post-discharge telehealth capability and enabling services was associated with the lowest odds of PPHs for any acute conditions, especially for rural residents. Notably, compared with residents of other areas (metropolitan and micropolitan) and compared with telehealth capability or enabling services alone, it was the combination of these in rural areas that showed the largest effect on any PPHs for both acute and chronic conditions in those aged 65 years and older. Future research can further explore the specific mechanisms by which post-discharge telehealth and enabling services combine in the rural hospital setting to improve care management in the outpatient or home-based settings. The larger effect in rural areas compared with micropolitan and metropolitan areas may suggest that rural areas stand to benefit most from these strategies given disproportionate health care access challenges related to transportation and fewer health care providers per capita.
Disclosure Statement
No competing financial interests exist.
Funding Information
This study is supported by the National Institute on Aging (R01AG62315) and the National Institute on Minority Health and Health Disparities (R01MD011523). Additionally, the Robert Wood Johnson Foundation's Health Policy Research Scholars program supported D.B. None of the funding bodies played a role in the design of the study, data collection, analysis, interpretation, article writing, or the decision to submit this article for publication.
References
- 1. Smith AS, Trevelyan E. The Older Population in Rural America: 2012–2016. American Community Survey Reports. Published online September 2019:21. Available from: https://www.census.gov/content/dam/Census/library/publications/2019/acs/acs-41.pdf [Last accessed: November 9, 2022]. [Google Scholar]
- 2. Jensen L, Monnat SM, Green JJ, et al. Rural population health and aging: Toward a Multilevel and Multidimensional Research Agenda for the 2020s. Am J Public Health 2020;110(9):1328–1331; doi: 10.2105/AJPH.2020.305782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. James W, Cossman J, Wolf JK. Persistence of death in the United States: The remarkably different mortality patterns between America's Heartland and Dixieland. Demogr Res 2018;39:897–910. [Google Scholar]
- 4. Knudson A, Meit M, Tanenbaum E, et al. Exploring Rural and Urban Mortality Differences. Rural Health Reform Policy Research Center. Published online March 2016:47. Available from: https://ruralhealth.und.edu/projects/health-reform-policy-research-center/pdf/technical-notes-exploring-rural-urban-mortality-differences.pdf [Last accessed: July 15, 2022]. [Google Scholar]
- 5. Moy E, Chang E, Barrett M, Centers for Disease Control & Prevention (CDC). Potentially preventable hospitalizations—United States, 2001–2009. MMWR Suppl 2013;62(3):139–143. [PubMed] [Google Scholar]
- 6. Torio CM, Andrews RM. Geographic Variation in Potentially Preventable Hospitalizations for Acute and Chronic Conditions, 2005–2011. 2014 Sep. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2006. Feb–. Statistical Brief #178. PMID: . [Google Scholar]
- 7. Caldwell JT, Ford CL, Wallace SP, et al. Intersection of living in a rural versus urban area and race/ethnicity in explaining access to health care in the United States. Am J Public Health 2016;106(8):1463–1469; doi: 10.2105/AJPH.2016.303212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Probst J, Eberth JM, Crouch E. Structural urbanism contributes to poorer health outcomes for rural America. Health Aff (Millwood) 2019;38(12):1976–1984; doi: 10.1377/hlthaff.2019.00914 [DOI] [PubMed] [Google Scholar]
- 9. Gao Y, Nocon RS, Gunter KE, et al. Characteristics associated with patient-centered medical home capability in Health Centers: A cross-sectional analysis. J Gen Intern Med 2016;31(9):1041–1051; doi: 10.1007/s11606-016-3729-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chen J, Amaize A, Barath D. Evaluating telehealth adoption and related barriers among hospitals located in rural and urban areas. J Rural Health 2021;37(45):801–811; doi: 10.1111/jrh.12534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Heisey-Grove DM. Variation in rural health information technology adoption and use. Health Aff (Millwood) 2016;35(2):365–370; doi: 10.1377/hlthaff.2015.0861 [DOI] [PubMed] [Google Scholar]
- 12. Rural Health Information Hub. Telehealth Use in Rural Healthcare. Available from: https://www.ruralhealthinfo.org/topics/telehealth [Last accessed: November 9, 2022].
- 13. Mack D, Zhang S, Douglas M, et al. Disparities in primary care EHR adoption rates. J Health Care Poor Underserved 2016;27(1):327–338; doi: 10.1353/hpu.2016.0016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Cross SH, Califf RM, Warraich HJ. Rural-Urban Disparity in Mortality in the US From 1999 to 2019. JAMA. 2021;325(22):2312–2314; doi: 10.1001/jama.2021.5334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rural Health Information Hub. Rural Health Disparities. Available from: https://www.ruralhealthinfo.org/topics/rural-health-disparities [Last accessed: November 9, 2022].
- 16. Parker K, Horowitz J, Brown A, et al. Demographic and Economic Trends in Urban, Suburban and Rural Communities. In: What Unites and Divides Urban, Suburban and Rural Communities. Pew Research Center; 2018. Available from: https://www.pewresearch.org/social-trends/2018/05/22/demographic-and-economic-trends-in-urban-suburban-and-rural-communities/ [Last accessed: February 5, 2023].
- 17. Rush KL, Singh S, Seaton CL, et al. Telehealth use for enhancing the health of rural older adults: A systematic mixed studies review. Gerontologist 2022;62(10):e564–e577; doi: 10.1093/geront/gnab141 [DOI] [PubMed] [Google Scholar]
- 18. H.R. 34, 114th Congress. 21st Century Cures Act; 2016. Available from: https://www.congress.gov/bill/114th-congress/house-bill/34/text [Last accessed: November 9, 2022].
- 19. Center for Connected Health Policy. Telehealth Policy Barriers. Public Health Institute; 2019. Available from: https://cdn.cchpca.org/files/2019-02/TELEHEALTH%20POLICY%20BARRIERS%202019%20FINAL.pdf [Last accessed: November 9, 2022].
- 20. Verma S. Early Impact of CMS Expansion of Medicare Telehealth During COVID-19. Health Affairs Blog. Available from: https://www.healthaffairs.org/do/10.1377/forefront.20200715.454789/ [Last accessed: November 9, 2022].
- 21. Yue D, Pourat N, Chen X, et al. Enabling services improve access to care, preventive services, and satisfaction among health center patients. Health Aff (Millwood) 2019;38(9):1468–1474; doi: 10.1377/hlthaff.2018.05228 [DOI] [PubMed] [Google Scholar]
- 22. Weir R, Proser M. Highlighting the Role of Enabling Services at Community Health Centers: Collecting Data to Support Service Expansion & Enhanced Funding, The Enabling Services Accountability Project. National Association of Community Health Centers and Association of Asian Pacific Community Health Organizations; 2010. Available from: https://www.nachc.org/wp-content/uploads/2015/06/EnablingServicesReport.pdf [Last accessed: February 5, 2023].
- 23. Wells R, Punekar RS, Vasey J. Why do some health centers provide more enabling services than others? J Health Care Poor Underserved 2009;20(2):507–523. [DOI] [PubMed] [Google Scholar]
- 24. McLean S, Sheikh A, Cresswell K, et al. The impact of telehealthcare on the quality and safety of care: A systematic overview. PLoS ONE 2013;8(8):e71238; doi: 10.1371/journal.pone.0071238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kranz A, Dalton S, Damberg C, et al. Using health IT to coordinate care and improve quality in Safety Net Clinics. Jt Comm J Qual Patient Saf 2018;44(12):731–740; doi: 10.1016/j.jcjq.2018.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. U.S. Health Resources & Services Administration. Defining Rural Population. Available from: https://www.hrsa.gov/rural-health/about-us/what-is-rural#:~:text=We%20define%20the%20following%20areas,of%20at%20least%20400%20sq [Last accessed: November 9, 2022].
- 27. Agency for Healthcare Research and Quality. Prevention Quality Indicators Overview. Available from: https://qualityindicators.ahrq.gov/measures/pqi_resources [Last accessed: November 9, 2022].
- 28. Ouayogode MH, Mainor AJ, Meara E, et al. Association between care management and outcomes among patients with complex needs in Medicare Accountable Care Organizations. JAMA Netw Open 2019;2(7):e196939; doi: 10.1001/jamanetworkopen.2019.6939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Condition Categories—Chronic Conditions Data Warehouse. Available from: https://www2.ccwdata.org/web/guest/condition-categories [Last accessed: November 9, 2022].
- 30. Ford JK, MacCALLUM RC, Tait M. The application of exploratory factor analysis in applied psychology: A critical review and analysis. Pers Psychol 1986;39(2):291–314; doi: 10.1111/j.1744-6570.1986.tb00583.x [DOI] [Google Scholar]
- 31. Kind AJH, Buckingham WR. Making neighborhood-disadvantage metrics accessible—The neighborhood atlas. N Engl J Med 2018;378(26):2456–2458; doi: 10.1056/NEJMp1802313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Fact Sheet: Biden Administration Takes Steps to Address COVID-19 in Rural America and Build Rural Health Back Better. The White House. Published August 13, 2021. Available from: https://www.whitehouse.gov/briefing-room/statements-releases/2021/08/13/fact-sheet-biden-administration-takes-steps-to-address-covid-19-in-rural-america-and-build-rural-health-back-better/ [Last accessed: November 9, 2022].
- 33. Wang N, Buchongo P, Chen J. Rural and urban disparities in potentially preventable hospitalizations among US patients with Alzheimer's disease and related dementias: Evidence of hospital-based telehealth and enabling services. Prev Med 2022;163:107223; doi: 10.1016/j.ypmed.2022.107223 [DOI] [PubMed] [Google Scholar]
- 34. Federal Register: Medicare Program; CY 2022 Payment Policies Under the Physician Fee Schedule and Other Changes to Part B Payment Policies; Medicare Shared Savings Program Requirements; Provider Enrollment Regulation Updates; and Provider and Supplier Prepayment and Post-Payment Medical Review Requirements. Available from: https://www.federalregister.gov/documents/2021/11/19/2021-23972/medicare-program-cy-2022-payment-policies-under-the-physician-fee-schedule-and-other-changes-to-part [Last accessed: November 9, 2022].
- 35. Williams R. H.R.341—117th Congress (2021–2022): Ensuring Telehealth Expansion Act of 2021. Published February 2, 2021. Available from: https://www.congress.gov/bill/117th-congress/house-bill/341 [Last accessed: November 9, 2022].
- 36. 2022 Community Health Center Chartbook. NACHC. Available from: https://www.nachc.org/research-and-data/research-fact-sheets-and-infographics/2021-community-health-center-chartbook/ [Last accessed: November 9, 2022].
- 37. Culler SD, Parchman ML, Przybylski M. Factors related to potentially preventable hospitalizations among the elderly. Med Care 1998;36(6):804–817. [DOI] [PubMed] [Google Scholar]
- 38. Wright B, Potter AJ, Trivedi AN, et al. The relationship between rural health clinic use and potentially preventable hospitalizations and emergency department visits among medicare beneficiaries. J Rural Health 2018;34(4):423–430; doi: 10.1111/jrh.12253 [DOI] [PubMed] [Google Scholar]
- 39. Johnston KJ, Wen H, Joynt Maddox KE. Lack of access to specialists associated with mortality and preventable hospitalizations of rural medicare beneficiaries. Health Aff 2019;38(12):1993–2002; doi: 10.1377/hlthaff.2019.00838 [DOI] [PubMed] [Google Scholar]
- 40. Characteristics and Costs of Potentially Preventable Inpatient Stays, 2017. #259. Available from: https://www.hcup-us.ahrq.gov/reports/statbriefs/sb259-Potentially-Preventable-Hospitalizations-2017.jsp [Last accessed: November 9, 2022]. [PubMed]
- 41. Weiss AJ, Jiang HJ. Geographic Variation in Potentially Preventable Inpatient Stays for Chronic Health Conditions, 2016. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Agency for Healthcare Research and Quality (US); 2006. Available from: https://www.ncbi.nlm.nih.gov/books/NBK563793/ [Last accessed: November 9, 2022]. [PubMed]
- 42. Steiner CA, Barrett ML, Weiss AJ, Andrews RM. Trends and Projections in Hospital Stays for Adults With Multiple Chronic Conditions, 2003–2014. 2014. Nov. In: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2006 Feb–. Statistical Brief #183. PMID: .25558764 [Google Scholar]