Abstract
The aim of this study is to determine the functioning of adults with autism spectrum disorders (ASDs) diagnosed in childhood and depression and burnout levels among their parents. A total of 261 adults with ASDs and their parents were recruited for the study. Both parents completed the Beck Depression and Maslach Burnout Inventories and reported the functioning of their adult offspring with ASDs. Only 5.4 % of our sample reported “good” or “very good” outcomes. The most common psychiatric comorbidities were intellectual disabilities and attention-deficit/hyperactivity disorder. Maternal burnout and depression scores were significantly elevated compared to those of fathers. There is an undeniable urgent need for more research to identify the needs of adults and families suffering from ASD. Modifications for those with ASD may have to be made for support in workplaces, achieving driving licenses, using public transportation and attendance at tertiary education.
Keywords: Adulthood, ASD, Autism, Burnout, Parents
1. Introduction
Autism spectrum disorder (ASD) is a neurodevelopmental disorder that presents with communication and social impairments, limited interests/repetitive actions, and problems with sensory integration [1]. Although genetic factors are important, the symptoms are thought to arise from a complex interplay of genetic, epigenetic, and environmental factors [2]. The latest estimates of prevalence suggest that ASD may affect one out of every forty children in the USA [3], with a male-to-female ratio of 2.5:1, while the global prevalence of ASD may be 0.4 % (95 % CI = 0.3–0.5), with a slightly greater (i.e., 0.7 %) prevalence among highly industrialized countries [4]. The neurodevelopmental, life-long nature of ASD along with associated symptoms and functional consequences are increasingly being recognized [5].
The transition from adolescence to adulthood is difficult for neurotypical youth and their family members. However, for individuals with ASD and their families, this transition may be more complicated and stressful [6]. As children age, parents’ concerns focus on the future, and issues of guardianship, education, day services/employment, independent living, transition planning, health and safety, social outlets and financial security come to the forefront [6,7]. Those concerns and related stress/anxiety levels may especially be pronounced among mothers with lower education and those with male/older children with ASD [[6], [7], [8]]. Parental concerns about the independent living of their children with ASD and their future well-being increase as they grow into adulthood, affecting their mental health. Studies addressing parents of adults with ASD found that behavior problems, psychiatric morbidity, gender of the child with diagnosis, poor physical health, and social impairments were associated with reduced quality of life, problems in intrafamilial relationships, and elevated symptoms of depression and anxiety among parents as well as children [9]. The risk for psychopathology among parents may continue to be elevated even when their adult offspring with autism have achieved independent living skills [10].
Parenting a child with ASD involves considerable stress, which may lead to parental burnout involving chronic mental and physical exhaustion [11]. Elevated levels of stress and burnout among parents may adversely affect couples’ relationships, parenting practices, behavior problems in offspring with ASD and the mental health of all family members [11]. Supporting this position, recent meta-analyses reported that anxiety and depression were common among parents of children with ASD, with median rates of 33.0 % and 31.0 %, respectively [12,13]. Depressive symptoms may be especially elevated among mothers [13]. Studies conducted in Turkey supported that parents of children with ASD had elevated levels of burnout and depression, while no study has been conducted to date on depression and burnout levels among parents of Turkish adults with ASD [14].
Although the functional outcomes of children diagnosed with ASD in childhood have improved somewhat since early reports, these adults still display impaired functioning, especially in vocational and independent living domains. Additionally, most of the available studies were conducted on western samples [[15], [16], [17]]. Available studies mostly used Rutter/Howlin criteria to classify functioning in adulthood according to occupation, friendship, and independent living domains ([18], Table 1).
Table 1.
Rutter/Howlin criteria for functional outcome of autism spectrum disorder in adulthood [18].
| Score | Occupation | Friendship | Independence | Outcome | Total Quantitative Scorea |
|---|---|---|---|---|---|
| 0 | employed/self-employed | ≥1 close friendships of good quality (mutual sharing of confidences and a range of activities undertaken together) | living independently | “Very Good”, high level of independence, including some friends and a job | 0–2 |
| 1 | volunteer work/job training/low-pay scheme | ≥1 friends but of poorer quality (restricted range of interests undertaken together) | semisheltered accommodation/at home with a high degree of autonomy | “Good”, in work, but requires some daily living support; some friends/acquaintances | 3–4 |
| 2 | Supported/sheltered employment | no specific friendships, seeks contact with others in group situations | living with parents, with limited autonomy | “Fair”, some independence, requires support/supervision but does not need residential support. No close friends, some acquaintances | 5–7 |
| 3 | special center//no occupation | no friends, no joint activities | residential accommodation with some autonomy | “Poor”, specialist residential support/high level of support across domains, no friends outside of residence | 8–10 |
| 4 | – | – | specialist residential accommodation, little- no autonomy | “Very Poor”, high-level hospital care, no friends, no autonomy | ≥11 |
| 5 | – | – | hospital care/at home (due to lack of alternative accommodation) | – | – |
Sum of occupation, friendship, and independence domains.
According to studies, 50.0–60.0 % of individuals diagnosed with ASD in childhood have poor or very poor outcomes in adulthood [[15], [16], [17]]. In a meta-analysis of 18 studies comprising 1199 individuals, 49.3 % of the participants were reported to have a poor outcome, with the sole predictive variable being IQ in adulthood ([15], Table 2).
Table 2.
Results of studies on functional outcome of autism spectrum disorder in adulthood using Rutter-Howlin criteria (modified from 15).
| Study Author | Year | N | Mean Age (yrs) | Diagnosis | Rate of “Good”/“very good” outcome (%) |
|---|---|---|---|---|---|
| Gillberg & Steffenberg | 1987 | 23 | 19.8 | IA | 4.3 |
| Kobayashi et al. | 1992 | 197 | 21.8 | IA | 26.9 |
| Larssen & Mouridsen | 1997 | 18 | 37.8 | ASD | 27.8 |
| Engstrom et al. | 2003 | 16 | 31.4 | ASD | 12.5 |
| Billstedt et al. | 2005 | 108 | 25.5 | IA (n = 73), ASD (n = 35) | 0.0 for both |
| Cederlund et al. | 2008 | 70 | 24.5 | IA | 0.0 |
| Eaves & Ho | 2008 | 47 | 24.0 | ASD | 21.3 |
| Esbensen et al. | 2010 | 70 | 37.7 | ASD | 10.0 |
| Gillespie- Lynch et al. | 2012 | 20 | 26.6 | IA | 30.0 |
| Chamak & Bonniau | 2016 | 76 | - | - | 30.3 |
| Moss et al. | 2017 | 52 | 47.9 | IA | 9.6 |
| Otsuka et al. | 2017 | 41 | 27.7 | ASD | 39.0 |
| Helles et al. | 2017 | 50 | 29.9 | ASD | 36.0 |
| Jónsdóttir et al. | 2018 | 15 | 21.9 | IA | 33.3 |
| Farley et al. | 2018 | 151 | 35.5 | IA | 19.9 |
| Mason et al. | 2019 | 69 | 61.5 | ASD | 20.4 |
| Sevaslidou et al. | 2019 | 53 | 19.4 | - | 41.5 |
| Pickles et al. | 2020 | 123 | 26.1 | ASD | 47.5 |
Yrs: years, IA: infantile autism/childhood autism, ASD: autism spectrum disorder, -: not reported.
Simonoff and colleagues reported that from adolescence to early adulthood, the IQ points of children with ASD increased, while ASD symptoms remained unchanged. According to their results, attendance at mainstream education settings was associated with reduced autism symptoms [16]. On the other hand, Pickles and colleagues found that adult functional outcomes of children with ASD could be predicted by childhood IQ and symptom severities in childhood [15]. McCauley and colleagues [19] found that criteria for positive outcomes in adulthood may be affected by the cognitive ability of those with ASD. According to their results, positive adult outcomes for those with less ability may involve daily living skills above the 8-year-old level with regular activities/social contacts outside the family, while more cognitively able adults may live independently with a paid vocation and at least one friend. The sole predictor of those positive outcomes was verbal IQ. The results of those studies were affected by study periods and sites and criteria used to define functional outcomes along with the availability of social support and services [15]. Adult functional outcomes in autism may also be affected by age at diagnosis, early language skills and ASD symptom severity [[15], [16], [17], [18], [19]]. Despite the importance of discerning functional outcomes among adults with ASD, no studies have been conducted among samples from Turkey.
Studies on adults with ASD from Turkey are limited, although interest in their functional outcomes, comorbidities and parenting burden is increasing [20]. Kucuk and colleagues evaluated 21 patients with ASD with an average age of 20.9 years (range = 16.0–36.0) and an IQ ≥ 50 and found that the symptoms of 20.0 % of the patients improved during puberty, with 4.8 % developing psychotic disorders [21]. Gormez evaluated parenting burden among 101 Turkish adults with intellectual disabilities (IDs), of whom 31.7 % also had ASD [22]. In the study, elevated caregiving burden was associated with ASD, behavioral problems, and caregivers’ higher education level. Gormez and colleagues also evaluated a large group (n = 771) of adults with IDs and reported that 50.1 % had psychiatric symptoms, while the rate of challenging behaviors was 36.4 %. Challenging behaviors were predicted by the presence of ASD, and 64.7 % reported barriers to receiving appropriate care [23]. None of those studies evaluated functional outcomes with operationally defined criteria, and all were limited to single centers.
Specialized Child and Adolescent Psychiatry Departments in Turkey have been in operation since 1990, and children initially diagnosed with ASD have been getting older [24,25]. However, until now, no study has concentrated on how Turkish early adults diagnosed with ASD in their childhood function and the problems experienced by their parents. Therefore, the goals of this study were to evaluate the sociodemographic features and functional outcomes of Turkish early adults with ASD diagnosed in childhood, to determine predictors of favorable functional outcomes according to the Rutter/Howlin criteria and to assess self-reported burnout and depression levels among their parents.
2. Methods
2.1. Study centers and sampling
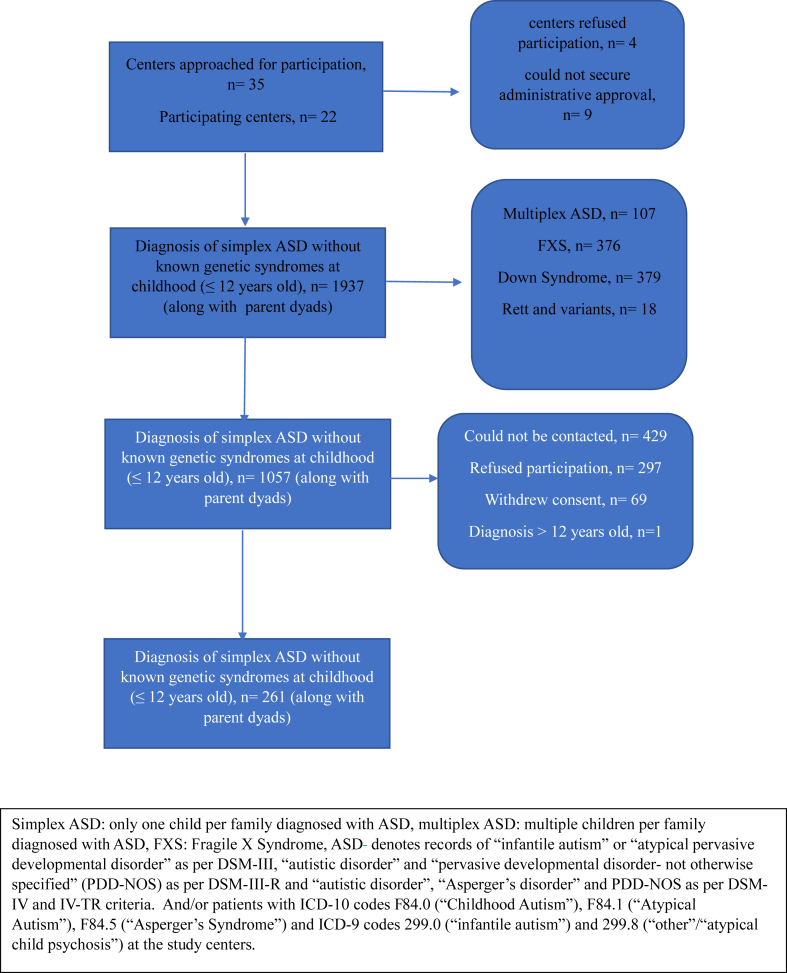
This research was performed in the Child and Adolescent Psychiatry Departments from different geographical regions of Turkey. The diagnoses of the included patients at the time of the study were ascertained through clinical interviews by psychiatrists following them at the time as per DSM-5 [1]. The study flowchart according to the STROBE criteria is illustrated in Fig. 1 [26]. Informed consent was obtained from parents of early adults/late adolescents with ASD as well as verbal individuals with ASD to be included in the study. Patients with epilepsy and psychiatric or other neurodevelopmental comorbidities were included, and the effects of those confounders were controlled for in the analyses.
Fig. 1.
Flowchart of the study to evaluate functional outcome and parent-reported depression/burnout symptoms of Turkish early adults with ASD diagnosed in childhood.
3. Ethics
The study was conducted in accordance with the Declaration of Helsinki and local laws and regulations. The study protocol was approved by the IRB of Gaziantep University (No:2019/234).
3.1. Study measures and tools
-
1.
Sociodemographic form
This form was established by the authors for this study and included a questionnaire for both parents that collected information about demographics about the patient and themselves. The questions tapped education status/level, occupation, age of diagnosis of ASD in offspring, history of psychopathology requiring treatment and symptoms observed in the early adult/late adolescent patients with ASD, developmental milestones, comorbidities (including epilepsy), and past medical history of patients with ASD.
-
2.
Beck Depression Inventory (BDI)
The BDI was developed by Beck in 1961 to evaluate symptoms of depression, and a reliability and validity study for the inventory in Turkish was conducted previously [27,28]. It includes 21 Likert-type items evaluating motivational, cognitive, somatic, social, and vegetative symptoms of depression. Previous studies on parents of children with disabilities, including ASD, supported its reliability and validity [14,29]. Parents of adults with ASD completed the BDI in the current study. Cronbach's alpha for the present sample was 0.79. Seventeen was taken as the cutoff score for clinically significant depressive symptoms, as suggested in the Turkish reliability and validity study of the BDI [28].
-
3.
Maslach Burnout Inventory (MBI)
The MBI, a 22-item Likert-type scale, was developed by Maslach and Jackson to evaluate self-reported symptoms of burnout [30]. It consists of three subscales (emotional exhaustion, depersonalization, and personal accomplishment). The MBI was initially translated into Turkish and validated by Ergin [31]. It was later used to evaluate burnout among parents of children with disabilities [32]. In the study by Duygun and Sezgin, factor analysis revealed that a two-factor model was more appropriate for parents and explained 35.6 % of the variance. Accordingly, the items from the depersonalization subscale of the MBI were subsumed under emotional exhaustion, with the personal accomplishment items remaining the same [32]. We used the two-factor solution in our study. Mothers and fathers of adults with ASD completed the MBI in the current study. Cronbach's alpha for the present sample was 0.74.
4. Determination of functional outcome
A composite measure of overall social functioning in our sample was calculated according to previous studies and Rutter/Howlin criteria [18]. Parents' and currently following clinicians’ reports on education, employment, and independence along with medical records were scored and summed to form individual scores for occupation, friendships, and independent living (Table 1). Composite ratings were controlled by the first three authors, and ambiguous cases (n = 26, 10.0 %) were classified by adjudication.
4.1. Study procedure
Early adults (≥18 years, henceforth termed “adults” for ease of use) diagnosed with ASD were identified by hospital charts. The clinicians completed the sociodemographic form, while mothers and fathers of individuals with ASD completed the BDI and MBI for themselves.
4.2. Statistics
As no previous study evaluated the functioning of Turkish adults with ASD and due to the exploratory nature of the current study, no calculations were conducted to determine the sample size. Data were entered into a database prepared with Statistical Program for Social Sciences (SPSS™, IBM Inc., Armonk, NY) Version 22.0 and analyzed with SPSS. Nominal data were summarized as counts and frequencies, while quantitative data were summarized as the means and standard deviations or medians and interquartile ranges (IQRs) depending on normality and outliers. Comparisons between groups were conducted with chi-square tests for nominal variables. Yates', Fisher's, and likelihood ratio corrections were used as appropriate. Bivariate correlations were evaluated using Spearman correlation analyses. Bivariate comparisons of quantitative variables between independent and dependent groups were conducted with t tests. Predictors of “good”/“very good” functioning in adulthood were evaluated with logistic regression (enter method). P was set at 0.05 (two-tailed). Bonferroni- Holm correction for controlling familywise error was used in bivariate analyses of associated factors for parental depression and burnout (denoted by p’, Gaetano, J. (2018). Holm‒Bonferroni sequential correction: An Excel calculator (1.3) [Microsoft Excel workbook]. Retrieved from:https://www.researchgate.net/publication/322568540_HolmBonferroni_sequential_correction_An_Excel_calculator_13). Effect sizes for significant findings were also reported.
5. Results
The sociodemographic characteristics of Turkish adults with ASD and their parents are illustrated in Table 2. The median age at diagnosis of ASD was 36.0 (IQR = 24.0, Range = 6.0–144.0) months, while the median age for starting special education was 40.0 (IQR = 30.0, Range = 12.0–216.0) months among adults with ASD. The median time for special education was 15.0 (IQR = 5.0, Range = 1.0–33.0) years. More than half (n = 191, 73.2 %) were receiving some sort of special education, which consisted of daily living skills/academic support for those with an education of primary school or lower (n = 95, 74.2 %) and academic support/vocational skills for those with an education level of high school (n = 96, 75.0 %). None of the study participants with a university education (n = 5) were receiving special education at the time of the study.
Over half of the adults with ASD had current (n = 137, 52.5 %) or lifetime (n = 147, 56.3 %) comorbid neurodevelopmental/psychiatric disorders. Current and lifetime comorbid diagnoses are listed in Table 3. Most adults with ASD (n = 189, 72.7 %) were receiving psychopharmacological treatment while enrolled in the study. Twenty-eight (14.8 %) continued the medication prescribed by their child/adolescent psychiatrist without being followed up by any psychiatrist. The most commonly used agents were antipsychotics (n = 165, 63.2 %), mood stabilizers/antiepileptics (n = 49, 18.8 %) and antidepressants (n = 29, 11.1 %). Eighty-four adults with ASD (32.2 %) had chronic physical disorders requiring treatment. The most common of these disorders were epilepsy (n = 50, 19.2 %), obesity (n = 9, 3.5 %) and autoimmune thyroiditis (n = 4, 1.5 %). Ninety-four participants (36.0 %) were admitted to the hospital at least once, mostly for physical disorders (n = 87, 92.6 %), while the rest (7.4 %) were admitted for psychiatric emergencies. Parents of thirty-seven adults (14.2 %) previously sought complementary and alternative treatment methods (CAM). The most common methods were hyperbaric oxygen therapy (n = 16, 44.4 %), dietary modifications (n = 6, 16.7 %) and hippotherapy (n = 4, 11.1 %). The current functioning of adults with ASD is illustrated in Table 4, and variables associated with “good”/“very good” functioning are illustrated in Table 5. In bivariate analyses, lifetime/current ID comorbidity, receiving vocational support, living in an intact family with both parents, having a mother with a higher level of education and maternal participation in work out of home were associated with “good”/“very good” functional outcomes, albeit with some remaining at trend levels.
Table 3.
Sociodemographic characteristics of Turkish adults with ASD and their parents.
| Mean (S.D.) or n (%) |
||
|---|---|---|
| Age of offspring with ASD (years) | 21.4 (2.9) | |
| Gender of offspring with ASD | Male | 225 (86.2) |
| Female | 36 (13.8) | |
| Maternal age (years) | 47.8 (5.7) | |
| Paternal age (years) | 52.3 (6.6) | |
| Maternal education | Primary school or lower | 131 (50.4) |
| High school | 62 (23.8) | |
| University or higher | 67 (25.8) | |
| Maternal vocation | Housewife | 189 (72.7) |
| Civil servant | 33 (12.7) | |
| Worker | 5 (1.9) | |
| Artisan | 11 (4.2) | |
| Retired | 22 (8.5) | |
| Paternal education | Primary school or lower | 91 (36.4) |
| High school | 68 (27.2) | |
| University or higher | 91 (36.4) | |
| Paternal vocation | Jobless | 6 (2.3) |
| Civil servant | 64 (24.5) | |
| Worker | 36 (13.8) | |
| Artisan | 96 (36.8) | |
| Retired | 59 (22.6) | |
| Maternal chronic medical disorder | 81 (34.1) | |
| Maternal psychopathology requiring treatmenta | 47 (17.9) | |
| Paternal chronic medical disorder | 62 (25.0) | |
| Paternal psychopathology requiring treatmenta | 15 (6.0) | |
| Family status | Intact/nuclear | 217 (83.5) |
| Separated/divorced | 31 (11.9) | |
| Widowed | 12 (4.6) | |
Major depression was the most common diagnosis (n = 35, 74.5% of mothers and n = 10, 66.7% of fathers).
Table 4.
Current and lifetime comorbid neurodevelopmental/psychiatric diagnoses of Turkish adults with ASDs during their participation in the study.
| Diagnosis, n (%) | Lifetime (n = 147) | Current (n = 137) |
|---|---|---|
| Intellectual disabilities | 91 (34.9) | 77 (29.5) |
| ADHD | 52 (35.4) | 42 (30.7) |
| DBD | 9 (3.4) | 19 (13.9) |
| OCD | 6 (2.3) | 7 (2.7) |
| MDD | 4 (1.5) | 6 (2.3) |
| Bipolar disorders | 3 (1.1) | 2 (0.8) |
| Anxiety disorders | 2 (0.8) | 4 (1.5) |
| Sleep disorders | 1 (0.4) | 0 (0.0) |
ADHD: attention deficit/hyperactivity disorder, DBD: disruptive behavior disorders, OCD: obsessive compulsive disorder, MDD: major depressive disorder.
Table 5.
Clinical features and current daily functioning of Turkish adults with ASD.
| Mean (S.D.) or n (%) |
||
|---|---|---|
| Current level of functional speech | None |
80 (30.7) |
| Single words |
40 (15.3) |
|
| ≤2 Word strings |
29 (11.1) |
|
| Complete sentences with at least 3 words | 112 (42.9) | |
| Age at emergence of functional speech (months) | 54.0 (36.0) | |
| Highest academic grade completed | Primary school or lower | 127 (48.8) |
| High school | 127 (48.8) | |
| University or higher | 5 (2.4) | |
| Achievement of continence | 233 (89.3) | |
| Age at emergence of continence (months) | 48.0 (36.0) | |
| Able to self-groom | 120 (46.0) | |
| Able to shop alone | 56 (21.5) | |
| Able to use public transport alone | 29 (11.1) | |
| Able to travel between cities alone | 16 (6.1) | |
| Able to use telephone for some communicationa | 74 (28.4) | |
| Has social media account | 57 (21.8) | |
| Able to drive/has driver's permit | 3 (1.1) | |
| Attended compulsory military service | 0 (0.0) | |
| Has peer circle to socialize ≥3 h/week | 37 (14.2) | |
| Ever had romantic affair | 9 (3.4) | |
| Ever worked for pay* | 24 (9.2) | |
| Ever mutilated self | 68 (26.1) | |
| Ever attempted suicide | 6 (2.3) | |
| Ever harmed another** | 99 (37.9) | |
| Inappropriate social behavior (touching, masturbating) | 45 (17.2) | |
| History of hospitalization | 93 (35.6) | |
| Nicotine/alcohol use | 1 (0.4) | |
| Involvement in legal proceedings*** | 9 (3.4) | |
| Able to attend national examinations for high-school/university entry | 27 (10.3) | |
| Functional outcome according to Rutter/Howlin criteria | Very good | 7 (2.7) |
| Good | 7 (2.7) | |
| Fair | 20 (7.7) | |
| Poor | 31 (11.9) | |
| Very poor | 196 (75.1) | |
including speech/messaging, *Median duration of work was 12.0 (IQR = 21, Min. = 1.0-Max. = 48.0) months, **due to rage attacks, ***due to social communication problems and restricted interests.
Logistic regression was used to evaluate predictors of “good” or “very good outcome” in the sample, and variables found to be significantly associated in bivariate analyses were entered as predictors. Due to the significant association between diagnosis of ID in childhood and adulthood (χ 2 = 6.5, p = 0.011, McNemar test), we used ID in childhood as the sole predictor to prevent multicollinearity (Table 6). ID in childhood by itself increased the risk of lower functioning in adulthood (p = 0.06, O.R. = 7.5, 95 % CI for O.R. = 1.0–57.9), while receiving vocational support in adulthood reduced it (p = 0.08, O.R. = 0.4, 95 % CI for O.R. = 0.1–1.1), although at trend levels for both. Intact family and maternal higher education had no significant effect on outcome. Having a mother working out of home was the sole significant predictor of reduced risk of lower functioning in adulthood. Although it was statistically significant and fit the data (Hosmer‒Lemeshow χ 2 [6] = 1.7, p = 0.95), as a whole, the model did not improve the classification of “good”/“very good” functioning in adulthood (94.6 % classification at baseline and at the end of the analysis, Table 6).
Table 6.
Variables associated with “good”/“very good” (n = 14) daily functioning of Turkish adults with ASD according to Rutter/Howlin criteria.
| Variable | N, % | χ 2/dF | pa | Effect size** | |
|---|---|---|---|---|---|
| ID in childhood | 1 (7.1) | 5.0/1 | 0.04 | 0.14 | |
| ID in adulthood | 1 (7.1) | 3.6/1 | 0.07 | 0.12 | |
| Age at diagnosis | ≤4 yrs. | 12 (85.7) | 0.48/2 | 0.79 | 0.03 |
| 5–8 yrs. | 2 (14.3) | ||||
| ≥9 yrs. | 0 (0.0) | ||||
| Age at onset of special education | ≤4 yrs. | 10 (76.9) | 1.7/2 | 0.43 | 0.06 |
| 5–8 yrs. | 3 (23.1) | ||||
| ≥9 yrs. | 0 (0.0) | ||||
| Receiving vocational support | 7 (50.0) | 2.9/1 | 0.09 | 0.13 | |
| Comorbid diagnosis in childhood | 7 (50.0) | 0.2/1 | 0.78 | 0.03 | |
| Comorbid diagnosis in adulthood | 5 (35.7) | 1.7/1 | 0.27 | 0.08 | |
| Comorbid epilepsy | 1 (7.1) | 1.4/1 | 0.48 | 0.07 | |
| Receiving psychiatrist follow-up | 8 (57.1) | 0.1/1 | 0.94 | 0.02 | |
| Intact family | 14 (100.0) | 5.2/2 | 0.07 | 0.11 | |
| Maternal education | Primary or lower | 4 (28.6) | 5.0/2 | 0.08 | 0.15 |
| High school | 7 (50.0) | ||||
| University or higher | 3 (21.4) | ||||
| Mother working | 7 (50.0) | 7.1/1 | 0.01 | 0.19 | |
| Maternal organic disorder | 5 (35.7) | 0.0/1 | 1.00 | 0.01 | |
| Maternal psychopathology | 3 (21.4) | 0.1/1 | 0.72 | 0.02 | |
| Paternal education | Primary or lower | 3 (21.4) | 1.6/2 | 0.45 | 0.08 |
| High school | 5 (35.7) | ||||
| University or higher | 6 (42.9) | ||||
| Father working | 12 (85.7) | 0.89/1 | 0.53 | 0.06 | |
| Paternal organic disorder | 5 (35.7) | 0.89/1 | 0.35 | 0.06 | |
| Paternal psychopathology | 0 (0.0) | – | – | – | |
Chi square test (with Fisher's exact test, Yates' correction and likelihood ratio tests as needed), **Phi for 2 X 2 and Cramer's V for larger tables, ID: intellectual disability.
Maternal BDI and MBI-emotional exhaustion scores were significantly elevated compared to paternal scores (11.7 ± 8.9 vs. 9.1 ± 9.0, p = 0.001, 95 % CI = 1.0–3.6 and 16.4 ± 9.8 vs. 13.0 ± 8.9, p = 0.000, 95 % CI = 1.5–4.5, respectively). However, maternal (8.3 ± 6.3) and paternal (9.4 ± 7.7) MBI personal accomplishment scores did not differ significantly (p = 0.261, 95 % CI = − 1.7–0.5; t-test for paired samples). The effects of lifetime vs. current ID/comorbid psychopathology, epilepsy, and current “good”/“very good” functioning of offspring with ASD on depression and burnout levels of parent dyads are illustrated in Table 7.
Table 7.
Predictors of “good”/“very good” (n = 14) daily functioning among Turkish adults with ASD according to Rutter/Howlin criteria.
| Variable | Odds Ratio | p | 95% CI for Odds Ratio | Nagelkerke R2 |
|---|---|---|---|---|
| ID in childhood | 6.8 | 0.07 | 0.9–54.5 | 0.07 |
| Receiving vocational support | 0.5 | 0.18 | 0.1–1.4 | 0.10 |
| Intact family | 0.0 | 1.00 | 0.0–0.0 | 0.16 |
| Maternal education (high school or higher) | 1.0 | 0.98 | 0.3–3.4 | 0.17 |
| Mother working | 0.2 | 0.01 | 0.1–0.7 | 0.23 |
ID: intellectual disability, CI: confidence Interval.
Mothers with current and lifetime comorbidity of ID and other neurodevelopmental/psychiatric disorders in offspring with ASD had significantly elevated levels of depressive symptoms (see Table 8). Additionally, mothers with current and lifetime comorbidity of ID and current comorbidity of other neurodevelopmental/psychiatric disorders in offspring with ASD had significantly elevated burnout levels. On the other hand, no significant effect emerged for paternal depressive symptoms. Paternal burnout was significantly elevated among those with current ID and other neurodevelopmental/psychiatric disorder comorbidities in offspring with ASD. Lifetime comorbidity of ID and presence of “good”/“very good” functioning in adulthood affected paternal burnout only at trend levels (Table 7).
Table 8.
Effects of lifetime/current intellectual disability, comorbid psychopathology, epilepsy, and current “good”/“very good” functioning of Turkish adults with ASD on depression and burnout levels of their parents.
| Mean (S.D.) | Mothers |
Fathers |
||||
|---|---|---|---|---|---|---|
| BDI | ||||||
| Yes | No | p | Yes | No | p | |
| ID in childhood of offspring with ASD | 13.4 (8.7) | 10.7 (8.9) | 0.03 | 10.1 (8.8) | 9.1 (8.6) | 0.35 |
| ID in adulthood of offspring with ASD | 13.7 (8.8) | 10.8 (8.8) | 0.02 | 10.5 (8.8) | 9.1 (8.6) | 0.27 |
| Comorbid dx. In childhood of offspring with ASD | 12.7 (9.0) | 10.2 (8.6) | 0.03 | 9.9 (9.3) | 8.7 (8.2) | 0.26 |
| Comorbid dx. In adulthood of offspring with ASD | 13.0 (8.7) | 10.2 (8.9) | 0.02 | 10.2 (8.5) | 9.4 (8.3) | 0.20 |
| Epilepsy in offspring with ASD | 13.7 (9.4) | 11.2 (8.7) | 0.10 | 8.8 (7.4) | 9.3 (9.2) | 0.86 |
| “Good”/“very good” functioning of offspring with ASD |
12.6 (10.6) |
11.7 (8.7) |
0.64 |
13.6 (8.9) |
9.2 (8.5) |
0.90 |
| MBI- Total | ||||||
| Yes | No | p | Yes | No | p | |
| ID in childhood of offspring with ASD | 27.2 (12.4) | 23.0 (13.0) | 0.02 | 25.1 (12.6) | 20.8 (13.1) | 0.05 |
| ID in adulthood of offspring with ASD | 28.1 (11.8) | 23.0 (13.0) | 0.01 | 26.7 (12.4) | 20.5 (12.9) | 0.01 |
| Comorbid dx. In childhood of offspring with ASD | 25.6 (12.9) | 23.1 (12.8) | 0.14 | 23.7 (13.2) | 20.6 (12.7) | 0.14 |
| Comorbid dx. In adulthood of offspring with ASD | 26.6 (12.1) | 22.1 (13.4) | 0.01 | 24.8 (13.2) | 20.2 (12.6) | 0.03 |
| Epilepsy in offspring with ASD | 27.0 (12.9) | 24.0 (12.9) | 0.17 | 22.3 (12.8) | 22.3 (13.1) | 0.99 |
| “Good”/“very good” functioning of offspring with ASD | 20.9 (16.1) | 24.7 (12.7) | 0.28 | 17.5 (16.5) | 22.8 (12.5) | 0.09 |
ASD: Autism Spectrum Disorder, S.D.: Standard Deviation, BDI: Beck Depression Inventory, ID: Intellectual Disability, dx.: diagnosis, MBI: Maslach Burnout Inventory.
When a cutoff score of 17 or higher was taken as a measure of “clinically significant depressive symptoms” as proposed previously [28], 22.9 % of mothers (n = 60) and 10.7 % of fathers (n = 28) were found to have significant depressive symptoms. Clinically significant depression symptoms in mothers were related to incontinence according to the bivariate analysis (χ2 = 8.4, p = 0.00, Phi = 0.19, p’ = 0.01), lack of spare time for themselves and their spouses (χ2 = 22.8, p = 0.00, Phi = 0.31, p’ = 0.00), and clinically significant depressive symptoms in fathers (χ2 = 5.9, p = 0.02, Phi = 0.16, p’ = 0.03). Mothers of minimally verbal adults also tended to report clinically significant depressive symptoms (χ2 = 3.0, p = 0.08, Cramer's v = 0.15, p’ = 0.08). Clinically significant depressive symptoms in fathers were significantly associated with a lack of education of their children (χ2 = 8.1, p = 0.00, Cramer's V = 0.19, p’ = 0.01), a history of hospitalization of their child (χ2 = 6.4, p = 0.01, Phi = 0.16, p’ = 0.02) and clinically significant depression symptoms among their wives (χ2 = 5.9, p = 0.02, Phi = 0.16, p’ = 0.02).
6. Discussion
This multicenter, cross-sectional study aimed to evaluate functional outcomes among Turkish early adults with ASD and depressive symptoms and burnout levels of their parents. Most of the early adults with ASD had “poor”/“very poor” outcomes according to the Rutter-Howlin criteria, while only 5.4 % had “good”/“very good” outcomes. Bivariate analyses revealed that lifetime/current ID comorbidity was negatively associated, while receiving vocational support, living in an intact family with both parents, having a mother with a higher level of education and maternal participation in work out of home were positively associated with “good”/“very good” functional outcomes among those with ASD, albeit with some remaining at trend levels. In logistic regression analyses, maternal participation in work out of home was the sole significant predictor of reduced risk of poor functioning in adulthood, with comorbidity of ID in childhood remaining at the trend level. More than one-fifth of mothers and one-tenth of fathers reported clinically significant depressive symptoms. Maternal and paternal depressive symptoms were significantly associated with each other. Incontinence, mutism, and the necessity of close supervision of offspring with ASD were significantly associated with maternal depressive symptoms, while paternal symptoms were associated with lack of educational attainment in offspring and a history of hospitalization among the children. Mothers were significantly more depressed and reported greater emotional exhaustion than fathers. Current and lifetime ID and other neurodevelopmental/psychiatric disorder comorbidities affected maternal depression and burnout levels, while only current comorbidities affected paternal burnout.
Available studies mostly using Rutter-Howlin criteria to evaluate functional outcomes of ASD in adulthood have reported that those outcomes improved somewhat compared to earlier reports [[15], [16], [17], [18], [19],33,34]. Despite this observation, at least half of individuals diagnosed with ASD in childhood may have “poor”/“very poor” adult outcomes [[15], [16], [17]], while rates of “good”/very good” outcomes may display greater variability (i.e., between 3.0 and 48.0 %). This variability may be due to the use of differing criteria for functioning, sampling methods, study centers, enrollment of participants with IDs and the presence of social support [[15], [16], [17], [18], [19],33,34]. Additionally, most studies on functional outcomes among those with ASD are conducted on Western samples, and the external validity of those results should be tested considering the variation in CAP resources in different settings [11,24,25,35,36]. There are no studies from Turkey on functional outcomes in adulthood of children diagnosed with ASD, and the rate of “good”/“very good” functioning in our sample is at the lower end of those reported for Western samples [[15], [16], [17], [18], [19],33,34]. To increase representativeness, we enrolled participants from 22 centers corresponding to all seven geographic regions of Turkey (Mediterranean, n = 5; Aegean, n = 4; Marmara, n = 2; Central/Eastern/Southeastern Anatolia, n = 3 for each; Black Sea, n = 2), although not according to population density. It is known that the Marmara, Aegean, and Mediterranean regions of Turkey had higher human development indices along with greater populations, possibly biasing our results [37]. Additionally, our results may be biased due to dependence on clinical records, and future studies from Turkey may enroll larger samples of adults with ASD from both sexes, reflecting urban/rural population distributions and using both clinical and community samples to evaluate functioning. Last, longitudinal studies suggest that functioning may improve as participants with ASD age, and this, along with the lower mean age of our sample compared to those reported in previous studies, may be a source of discrepancy (Table 2, [[15], [16], [17]].
Previous studies suggest that IQ measured either in childhood or adulthood may predict adult functioning among patients with ASD and that verbal IQ may be especially important in this regard. Age at diagnosis, early language skills, severity of ASD symptoms at baseline and attendance at mainstream education settings emerged as other predictors of adult functioning [[15], [16], [17], [18], [19]]. Our results partially support those findings, and in bivariate analyses, lifetime/current ID comorbidity was negatively associated, while receiving vocational support, living in an intact family with both parents, having a mother with a higher level of education and maternal participation in work out of home were positively associated with “good”/“very good” functional outcomes among those with ASD. However, in logistic regression analyses, maternal participation in work out of home was the sole significant predictor of reduced risk of poor functioning in adulthood, with comorbidity of ID in childhood remaining at the trend level.
Studies suggest that financial problems are among the main reasons for stress among parents of children with ASD, while the diagnosis of ASD also increases the risk of unemployment among parents [38,39]. Having working parents may reduce the financial burden on families of children with ASD and enable them to access health/educational services [40,41]. Supporting this view, Kilincaslan and colleagues found that elevated speech skills and higher monthly household income were associated with increased daily living skills among their sample with ASD [41]. In previous studies from Turkey, higher maternal education levels were also found to be related to increased participation in the workforce [42]. Maternal participation in work may also be associated with a greater perception of self-efficacy, more sensitive parenting, lower levels of depression and greater knowledge of typical and atypical child development [43,44]. This may also affect mothers’ interactions with their children [45]. On the other hand, separation/divorce may compound the financial problems of parents looking after children with ASD and may limit access to services and treatments [46]. Alternatively, maternal participation in work may also increase conflicts due to demands from work and familial obligations [47]. Because of complex, bidirectional relationships between family status, maternal participation in work, family status, socioeconomic level and other related constructs and the cross-sectional nature of our study, we could not discern the direction of causality on adult functioning of offspring with ASD. Future studies may use longitudinal designs to dissect the relationships between those constructs and establish causality.
Studies conducted to date support the importance of IQ, measured in childhood and/or in adulthood, in adult functioning of those with ASD [[15], [16], [17], [18], [19]]. Earlier studies suggest that an overall IQ of 50, or alternatively a performance IQ of 70 and a verbal IQ of 50, may differentiate those with “fair” or better outcomes in adulthood from “poor”/“very poor” outcomes [15]. Although IQ scores correlate positively and significantly with adult outcomes, high IQ by itself does not guarantee a better prognosis. Additionally, although IQ levels remain stable at the group level, they may vary with time among individuals. Pickles and colleagues [16] suggest that IQ may be protective only for the poorest outcomes without a guarantee of a good outcome. Recent studies suggest that verbal IQ may be more important in this regard and that other factors, such as social support or severity of autism symptoms, may moderate its effects on functioning [[15], [16], [17], [18], [19]]. Supporting those results, we found that lifetime/current ID comorbidity was negatively associated with “good”/“very good” outcomes and that ID in childhood predicted worse functioning in adulthood at a trend level. Despite the importance of discerning functional outcomes among adults with ASD who were diagnosed in childhood, there are no studies conducted on samples from Turkey, and our results should be replicated with further studies. Due to dependence on clinical records, we could not evaluate the effects of verbal IQ level and symptom severity at baseline on adult functioning of cases with ASD. We also did not evaluate adult participants with ASD with formal intelligence tests and reliable and valid measures of psychopathology and social functioning, which may be used in further studies.
Caring for a child with ASD from the time of diagnosis onward is a demanding process requiring a balance of parenting roles. Parents also act as cotherapists for their children while educating relatives, schools, and teachers on the nature of ASD, advocate for their children's rights and, with the transition to adulthood, must address problems such as guardianship, higher education, social/romantic relationships of their children, financial security, independent living, and housing [7]. Those obligations lead them to experience elevated levels of stress and burnout. Mothers of children with ASD are the primary caregivers experiencing elevated stress, which may contribute to the development of maternal psychopathology [14,22,23,29]. Accordingly, past studies reported that mothers of children with ASD experience elevated burden and depression in comparison to fathers, and there may exist bidirectional spillover effects between parent dyads [[10], [11], [12], [13], [14],48,49]. Parents with lower education, those living with male/older children with ASD without functional speech, and the presence of behavioral problems/psychiatric comorbidity/physical disorders in offspring with ASD were found to have elevated stress, depressive symptoms, and burnout in previous studies [[9], [10], [11], [12], [13], [14],38,41]. Supporting those views, self-reported depression and burnout levels in our study were also significantly elevated in mothers compared to fathers. Maternal and paternal depressive symptoms were significantly associated with each other. Lack of self-grooming skills and speech of offspring with ASD were significantly associated with maternal depressive symptoms, while paternal symptoms were associated with lack of educational attainment in offspring and a history of hospitalization among the children. Current and lifetime ID and other neurodevelopmental/psychiatric disorder comorbidities affected maternal depression and burnout levels, while only current comorbidities affected paternal burnout. The discrepancy between mothers and fathers may be due to differing responses to the diagnosis of autism in their children [[47], [48], [49], [50]]. Previous studies on Turkish parents of children with ASD reported that fathers tended to withdraw from the family, interact with their child less and focus more on the financial aspects of caring for their children and family, while mothers take over the role of caring for the child as well as other family members. Turkish mothers and fathers may also differ in expectations of academic achievement from their children [44,50,51]. Our results should be deemed preliminary, and correlates and predictors of depression, parenting stress and burnout among fathers and mothers of children diagnosed with ASD should be evaluated with further studies using longitudinal designs and evaluating those constructs across multiple time points.
Recent studies suggest that approximately one-fifth to more than one-third of parents with children who were diagnosed with ASD may report clinically significant depressive symptoms [[10], [11], [12], [13], [14]]. Our results support and extend the results of previous studies and may suggest that parenting stress, burnout and depression may continue over the long term for parents of Turkish children with ASD. Further studies on Turkish samples with ASD and their parents as they age may be required to evaluate the temporal change rates of clinically significant depressive symptoms among parents.
Tertiary education and finding employment may be especially challenging for those with ASD [7,[15], [16], [17], [18], [19]]. Our results are consistent with those studies and may underline the importance of lifelong educational and vocational support for adults with ASD. Further studies should evaluate predictors of gainful employment among this sample. Counseling services, vocational training and support and coordination of services across schools, families, and potential employers for young adults and adults with ASD should be established as soon as possible in developing countries, including Turkey [7,[20], [21], [22], [23], [24], [25]]. An additional indicator of successful functioning in adulthood is independent living, which includes separation from the family of origin and becoming socially active in the community. However, studies show that most adults with ASD continue to live with their parents and never leave home [[15], [16], [17], [18], [19]]. Consistent with previous studies, most of our sample lived with their families. Transportation is another major problem for adults with ASD. Mobility provides a certain level of independence for young people to travel, access to health care, and attend group activities, although special modifications may have to be made to overcome sensory difficulties [[52], [53], [54]]. Underlining the importance of independent mobility and barriers to achieving it, approximately one percent of our sample could obtain their driver's license, and less than one-tenth could travel between cities by using buses/planes. Driving instructors and courses may be informed of neurodevelopmental disorders, including ASD, and appropriate modifications to the licensing process may be required to address the needs of Turkish adults with ASD. Staff working at intercity bus/train/airplane services may also be educated on the needs of adults with ASD as well as the importance of sensory problems in adapting to travel. Social relations, including friendships, protect mental health among people, including adults with ASD. However, adults with autism experience significant difficulties in establishing and maintaining friendships and romantic relationships due to their symptoms [[15], [16], [17], [18], [19]]. Our results are in accordance with those previous reports, and we found that parents of just over one-tenth of our sample reported that their children had friends, and less than five percent experienced romantic relationships. Considering the result that less than one tenth of our sample had ever worked for pay, vocational support for Turkish adults with ASD may have to be introduced.
6.1. Limitations
This study is not without limitations. First, most of the participants could not be contacted/enrolled in the study, and their medical records were incomplete, preventing us from evaluating the effects of baseline IQ subscales, adaptive functioning, ASD symptom severity and effects of specific symptoms. Parents of more impaired adults may refuse participation outright, withdraw their consent or may have moved to other addresses, introducing selection bias to our results. Dependence on clinical records may be another source of bias. Second, we did not evaluate adults with ASD with clinical interviews and depended on the reports of psychiatrists following them for comorbid diagnoses. Further studies may evaluate adults with ASD via specialized instruments (e.g., the PAS-ADD) and use formal intelligence tests to evaluate IQ in adulthood. Third, we evaluated depression and caregiving burden among parents with self-reports, and there is a possibility of recall and bias in reporting as well as shared method variance. Structured interviews and scales (e.g., Zarit Caregiving Burden Interview, Hamilton Depression Rating Scale, etc.) may provide greater objectivity in evaluating those constructs. Fourth, we depended on parents’ own reports for their psychopathologies and medical disorders requiring treatment, and those reports may also be subject to bias. Fifth, rather than depending on the MBI adapted previously for parents of youth with ASD, we may have used a more direct measure of parental burnout, such as the Parental Burnout Assessment [55]. Last, rather than using discrete questions tapping social participation, we could have used a psychometric scale to evaluate social competence among adults with ASD (e.g., Ref. [56]). Nevertheless, our study is the first to evaluate functioning among a large sample of adults with ASD from Turkey along with depression and burnout levels among their parents. Our data may contribute to the literature on adult outcomes of ASD, as most of the available data are from Western countries.
7. Conclusion
The transition to adulthood is very difficult for individuals with ASD and their families. Similar to the status of education services in other countries, many services that were offered as children are limited or no longer available for adults with ASD in Turkey, and there are no structured supports easing the transition to adult services [7]. Even in countries with structured support to ease the transition to adult services, young adults with ASD may be socially isolated and lack participation in the community [7]. Lack of education among health care workers for ASD in adulthood may present barriers to receiving help. This may lead to embitterment among parents and adults with ASD [7]. Our results support the urgent need for a structured transition plan for families of adults with ASD as well as those adults for adult mental health services such as those in other countries (e.g., STEPS, [57]). Modifications for those with ASD may have to be made for support in workplaces, achieving driving licenses, using public transportation and attendance at tertiary education. Our study may be a tentative first step in this direction, and the results of our study group should be replicated with a nationwide survey.
CRediT authorship contribution statement
Meryem Ozlem Kutuk: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Supervision, Writing – original draft, Writing – review & editing. Ali Evren Tufan: Conceptualization, Data curation, Formal analysis, Supervision, Writing – original draft, Writing – review & editing. Fethiye Kilicaslan: Conceptualization, Data curation, Formal analysis, Writing – original draft, Writing – review & editing. Pınar Vural: Data curation, Investigation, Supervision, Validation. Cem Gokcen: Formal analysis, Supervision, Validation. Sevay Alsen Guney: Data curation, Formal analysis. Bahtim Kutuk: Data curation, Formal analysis. Gonca Ozyurt: Data curation, Formal analysis. Neslihan Inal: Data curation, Formal analysis. Tuba Mutluer: Data curation, Formal analysis. Eren Yavuz Acikalin: Data curation, Formal analysis. Fadime Hande Ozer: Data curation, Formal analysis. Esma Nur Pamuk: Data curation, Formal analysis. Seyma Celikcan Yesilmese: Data curation, Formal analysis. Mehmet Karadag: Data curation, Formal analysis. Zehra Hangul: Data curation, Formal analysis. Cilem Bilginer: Data curation, Formal analysis. Nilfer Sahin: Data curation, Formal analysis. Oznur Bilac: Data curation, Formal analysis. Hasan Kandemir: Data curation, Formal analysis. Eyup Sabri Ercan: Data curation, Formal analysis, Methodology, Supervision. Tugba Eseroglu Soylemez: Data curation, Formal analysis. Sadettin Burak Acikel: Data curation, Formal analysis. Gulen Guler Aksu: Data curation, Formal analysis. Pelin Dag: Data curation, Formal analysis. Fevziye Toros: Data curation, Formal analysis. Caner Mutlu: Data curation, Formal analysis. Omer Kardas: Data curation, Formal analysis. Burcu Kardas: Data curation, Formal analysis. Suleyman Kizildag: Data curation, Formal analysis. Esra Demirci: Data curation, Formal analysis. Sevgi Ozmen: Data curation, Formal analysis. Leyla Sevicin: Data curation, Formal analysis. Yuksel Sumeyra Karagoz: Data curation, Formal analysis. Umit Isik: Data curation, Formal analysis. Evrim Aktepe: Data curation, Formal analysis. Hatice Altun: Data curation, Formal analysis. Çigdem Yektas: Data curation, Formal analysis. Berna Polat Tuysuz: Data curation, Formal analysis. Ahmet Buber: Data curation, Formal analysis. Mehmet Akif Cansiz: Data curation, Formal analysis. Hakan Ogutlu: Data curation, Formal analysis. Safak Eray: Data curation, Formal analysis. Hande Ayraler Taner: Data curation, Formal analysis, Supervision. Ebru Altintas: Data curation, Formal analysis, Methodology, Supervision. Ozgur Kutuk: Conceptualization, Data curation, Formal analysis, Supervision, Writing – original draft, Writing – review & editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
All the authors gratefully acknowledge Burcu Gonul who is the Clinical Nurse Specialist (CNS) of the Department of Child and Adolescent Psychiatry at Dr. Turgut Noyan Medical and Research Center for her support for the overall coordination of the whole study. We thank all patients and their families that participated in the study.
Contributor Information
Meryem Ozlem Kutuk, Email: drozlemina@gmail.com.
Ali Evren Tufan, Email: tevrenus@yahoo.com.
Fethiye Kilicaslan, Email: fethiyeklcaslan@gmail.com.
Pınar Vural, Email: apvural@gmail.com.
Cem Gokcen, Email: drcem78@hotmail.com.
Sevay Alsen Guney, Email: sevayalsen@gmail.com.
Bahtim Kutuk, Email: bahtimkutuk_ege@hotmail.com.
Gonca Ozyurt, Email: goncaenginozyurt@gmail.com.
Neslihan Inal, Email: neslihanemir@hotmail.com.
Tuba Mutluer, Email: tubamutluer@gmail.com.
Eren Yavuz Acikalin, Email: eacikalin15@ku.edu.tr.
Fadime Hande Ozer, Email: fhandeozer@gmail.com.
Esma Nur Pamuk, Email: pskesmapamuk@gmail.com.
Seyma Celikcan Yesilmese, Email: seymacelikcan@gmail.com.
Mehmet Karadag, Email: karadagm@gantep.edu.tr.
Zehra Hangul, Email: zehratopal86@gmail.com.
Cilem Bilginer, Email: cilemcolak@yahoo.com.
Nilfer Sahin, Email: nilfersahin@hotmail.com.
Oznur Bilac, Email: oznurbilac@gmail.com.
Hasan Kandemir, Email: kandemirhsn@yahoo.com.
Eyup Sabri Ercan, Email: eyup.sabri.ercan@ege.edu.tr.
Tugba Eseroglu Soylemez, Email: tugbaeseroglu@gmail.com.
Sadettin Burak Acikel, Email: acikel42@gmail.com.
Gulen Guler Aksu, Email: dr.gulen@hotmail.com.
Pelin Dag, Email: drpelindag@yahoo.com.
Fevziye Toros, Email: fevziyetoros@gmail.com.
Caner Mutlu, Email: canerrmutluu@yahoo.com.
Omer Kardas, Email: kardasomer@gmail.com.
Burcu Kardas, Email: burcu-atar@hotmail.com.
Suleyman Kizildag, Email: suleyman.kizildag_7@hotmail.com.
Esra Demirci, Email: esra_z_d_r@hotmail.com.
Sevgi Ozmen, Email: drsevgiozmen@gmail.com.
Leyla Sevicin, Email: sevicinleyla@gmail.com.
Yuksel Sumeyra Karagoz, Email: drsumeyrakaragoz@yahoo.com.
Umit Isik, Email: crsumt@gmail.com.
Evrim Aktepe, Email: e_aktepe@yahoo.com.
Hatice Altun, Email: drhaticealtun@gmail.com.
Çigdem Yektas, Email: drcigdemyektas@hotmail.com.
Berna Polat Tuysuz, Email: bernatalop@gmail.com.
Ahmet Buber, Email: ahmetbuber@gmail.com.
Mehmet Akif Cansiz, Email: makifcansiz@gmail.com.
Hakan Ogutlu, Email: hogutlu@gmail.com.
Safak Eray, Email: drsafakeray@gmail.com.
Hande Ayraler Taner, Email: h_ayraler@hotmail.com.
Ebru Altintas, Email: yurdagulebru@hotmail.com.
Ozgur Kutuk, Email: ozgurkutuk@gmail.com.
References
- 1.(APA) American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. fifth ed. American Psychiatric Publishing; Arlington; VA: 2013. (DSM-5) [Google Scholar]
- 2.Veenstra-VanderWeele J., O'Reilly K.C., Dennis M.Y., Uribe-Salazar J.M., Amaral D.G. Translational Neuroscience approaches to understanding autism. Am. J. Psychiatr. 2023;180:265–276. doi: 10.1176/appi.ajp.20230153. [DOI] [PubMed] [Google Scholar]
- 3.Xu G., Strathearn L., Liu B., O'Brien M., Kopelman T.G., Zhu J., Snetselaar L.G., Bao W. Prevalence and treatment patterns of autism spectrum disorder in the United States, 2016. JAMA Pediatr. 2019;173:153–159. doi: 10.1001/jamapediatrics.2018.4208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Olusanya B.O., Smythe T., Ogbo F.A., Nair M.K.C., Scher M., Davis A.C. Global prevalence of developmental disabilities in children and adolescents: a systematic umbrella review. Front. Public Health. 2023;11 doi: 10.3389/fpubh.2023.1122009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Scattoni M.L., Micai M., Ciaramella A., Salvitti T., Fulceri F., Fatta L.M., Poustka L., Diehm R., Iskrov G., Stefanov R., Guillon Q., Rogé B., Staines A., Sweeney M.R., Boilson A.M., Leósdóttir T., Saemundsen E., Moilanen I., Ebeling H., Yliherva A., Gissler M., Parviainen T., Tani P., Kawa R., Vicente A., Rasga C., Budişteanu M., Dale I., Povey C., Flores N., Jenaro C., Monroy M.L., Primo P.G., Charman T., Cramer S., Warberg C.K., Canal-Bedia R., Posada M., Schendel D. Real-world experiences in autistic adult diagnostic services and post-diagnostic support and alignment with services guidelines: results from the ASDEU study. J. Autism Dev. Disord. 2021;51:4129–4146. doi: 10.1007/s10803-021-04873-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maurice V., Russet F., Scocco P., McNicholas F., Santosh P., Singh S.P., Street C., Purper-Ouakil D. Transition from child and adolescent mental health care to adult services for young people with Attention-Deficit/Hyperactivity Disorder (ADHD) or Autism Spectrum Disorder (ASD) in Europe: barriers and recommendations. Encephale. 2022;48:555–559. doi: 10.1016/j.encep.2022.01.012. [DOI] [PubMed] [Google Scholar]
- 7.Elster N., Parsi K. Transitioning from adolescence to adulthood with autism spectrum disorder: an overview of planning and legal issues. Psychiatr. Clin. 2020;43:723–733. doi: 10.1016/j.psc.2020.08.008. [DOI] [PubMed] [Google Scholar]
- 8.Bujnowska A.M., Rodriguez C., Garcia T., Areces D., V Marsh N. Parenting and future anxiety: the impact of having a child with developmental disabilities. Int. J. Environ. Res. Publ. Health. 2019;16 doi: 10.3390/ijerph16040668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Burke M., Heller T. Individual, parent and social-environmental correlates of caregiving experiences among parents of adults with autism spectrum disorder. J. Intellect. Disabil. Res. 2016;60:401–411. doi: 10.1111/jir.12271. [DOI] [PubMed] [Google Scholar]
- 10.Hoyle J.N., Laditka J.N., Laditka S.B. Mental health risks of parents of children with developmental disabilities: a nationally representative study in the United States. Disabil Health J. 2021;14 doi: 10.1016/j.dhjo.2020.101020. [DOI] [PubMed] [Google Scholar]
- 11.Alnazly E.K., Abojedi A. Psychological distress and perceived burden in caregivers of persons with autism spectrum disorder. Psychiatr. Care. 2019;55:501–508. doi: 10.1111/ppc.12356. [DOI] [PubMed] [Google Scholar]
- 12.Schnabel A., Youssef G.J., Hallford D.J., Hartley E.J., McGillivray J.A., Stewart M., Forbes D., Austin D.W. Psychopathology in parents of children with autism spectrum disorder: a systematic review and meta-analysis of prevalence. Autism. 2020;24:26–40. doi: 10.1177/1362361319844636. [DOI] [PubMed] [Google Scholar]
- 13.Bispo-Torres A.C., Lucena R., Tavares-Rodrigues I.C., Barouh J.L., Lins-Silva D.H., Dorea-Bandeira I., Souza L.S., Faria-Guimarães D., Tolentino A., Miranda-Scippa Â., Hermens D.F., Sampaio A.S., Quarantini L.C., Glozier N., Hickie I.B., Bandeira I.D. Psychopathological symptoms in parents and siblings of people on the autism spectrum: a systematic review and meta-analysis. Psychiatr. Res. 2023;323 doi: 10.1016/j.psychres.2023.115145. [DOI] [PubMed] [Google Scholar]
- 14.Kutuk M.O., Tufan A.E., Kilicaslan F., Guler G., Celik F., Altintas E., Gokcen C., Karadag M., Yektas C., Mutluer T., Kandemir H., Buber A., Topal Z., Acikbas U., Giray A., Kutuk O. High depression symptoms and burnout levels among parents of children with autism spectrum disorders: a multi-center, cross-sectional, case-control study. J. Autism Dev. Disord. 2021 doi: 10.1007/s10803-021-04874-4. [DOI] [PubMed] [Google Scholar]
- 15.Mason D., Capp S.J., Stewart G.R., Kempton M.J., Glaser K., Howlin P., Happé F. A meta-analysis of outcome studies of autistic adults: quantifying effect size, quality, and meta-regression. J. Autism Dev. Disord. 2021;51:3165–3179. doi: 10.1007/s10803-020-04763-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pickles A., McCauley J.B., Pepa L.A., Huerta M., Lord C. The adult outcome of children referred for autism: typology and prediction from childhood. JCPP (J. Child Psychol. Psychiatry) 2020;61:760–767. doi: 10.1111/jcpp.13180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Simonoff E., Kent R., Stringer D., Lord C., Briskman J., Lukito S., Pickles A., Charman T., Baird G. Trajectories in symptoms of autism and cognitive ability in autism from childhood to adult life: findings from a longitudinal epidemiological cohort. J. Am. Acad. Child Adolesc. Psychiatry. 2020;59:1342–1352. doi: 10.1016/j.jaac.2019.11.020. [DOI] [PubMed] [Google Scholar]
- 18.Howlin P., Goode S., Hutton J., Rutter M. Adult outcome for children with autism. JCPP (J. Child Psychol. Psychiatry) 2004;45:212–229. doi: 10.1111/j.1469-7610.2004.00215.x. [DOI] [PubMed] [Google Scholar]
- 19.McCauley J.B., Pickles A., Huerta M., Lord C. Defining positive outcomes in more and less cognitively able autistic adults. Autism Res. 2020;13:1548–1560. doi: 10.1002/aur.2359. [DOI] [PubMed] [Google Scholar]
- 20.Atbasoglu E.C. Autism spectrum disorder as an initial diagnosis in adults. Noro Psikiyatr Ars. 2020;57:1–2. doi: 10.29399/npa.25050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kücük A., Maner F., Ceylan M.E. Autism spectrum disorders among adolescents and adults and comparison with schizophrenia. The European Research Journal. 2019;5:962–968. doi: 10.18621/eurjç441214. [DOI] [Google Scholar]
- 22.Gormez A. Family caregiving burden of adults with intellectual disability and associated factors. Anat. Clin. 2017;22:169–176. doi: 10.21673/anadoluklin.327742. [DOI] [Google Scholar]
- 23.Gormez A., Kurtulmus A., Ince Z., Torun P., Uysal O., Citak S. Psychiatric symptoms, challenging behaviour and utilization of psychiatric services among adults with intellectual disabilities in Turkey. J. Appl. Res. Intellect. Disabil. 2020;33:1038–1048. doi: 10.1111/jar.12726. [DOI] [PubMed] [Google Scholar]
- 24.Barrett E., Jacobs B., Klasen H., Herguner S., Agnafors S., Banjac V., Bezborodovs N., Cini E., Hamann C., Huscsava M.M., Kostadinova M., Kramar Y., Maravic V.M., McGrath J., Molteni S., Moron-Nozaleda M.G., Mudra S., Nikolova G., Vorkas K.P., Prata A.T., Revet A., Joseph J.R., Serbak R., Tomac A., Van den Steene H., Xylouris G., Zielinska A., Hebebrand J. The child and adolescent psychiatry: study of training in Europe (CAP-STATE) Eur Child Adolesc Psychiatry. 2020;29:11–27. doi: 10.1007/s00787-019-01416-3. [DOI] [PubMed] [Google Scholar]
- 25.Clausen C.E., Bazaid K., Azeem M.W., Abdelrahim F., Elgawad A.A.A., Alamiri B., AlAnsari A.M., Alhamzawi A., Al Mai A.M., Bakhiet A.M., Bashtawi M., Cuhadaroglu F., Hedar M., Holdar M., Jabr S., Jafri A.S., Jumaian A., Moussa S., Osman A.H., Razjouyan K., Yanes E., Guerrero A., Skokauskas N. A.P. in the M.E. Consortium on Academic Child, Child and adolescent psychiatry training and services in the Middle East region: a current status assessment. Eur Child Adolesc Psychiatry. 2020;29:51–61. doi: 10.1007/s00787-019-01360-2. [DOI] [PubMed] [Google Scholar]
- 26.von Elm E., Altman D.G., Egger M., Pocock S.J., Gøtzsche P.C., Vandenbroucke J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J. Clin. Epidemiol. 2008;61:344–349. doi: 10.1016/j.jclinepi.2007.11.008. [DOI] [PubMed] [Google Scholar]
- 27.Beck T A., Steer A R., Carbin G M. Psychometric properties of the Beck depression inventory: twenty-five years of evaluation. Clin. Psychol. Rev. 1988;8:77–100. 10.1016/0272-7358(88)90050-5. [Google Scholar]
- 28.Hisli N. Reliability and validity of the Turkish version of Beck Depression Inventory among college students. Turkish Journal of Psychology. 1989;7:3–13. [Google Scholar]
- 29.Baykal S., Karakurt M.N., Cakir M., Karabekiroglu K. An examination of the relations between symptom distributions in children diagnosed with autism and caregiver burden, anxiety and depression levels. Community Ment. Health J. 2019;55:311–317. doi: 10.1007/s10597-018-0343-8. [DOI] [PubMed] [Google Scholar]
- 30.Maslach C., Jackson S.E. The measurement of experienced burnout. J. Organ. Behav. 1981;2:99–113. [Google Scholar]
- 31.Ergin C. Ankara: VII. National Psychology Congress. 1993. Burnout in doctor and nurses and adaptation of Maslach burnout inventory; pp. 143–144. [Google Scholar]
- 32.Duygun T., Sezgin N. The effects of stress symptoms, coping styles and perceived social support on burnout level of mentally handicapped and healthy children's mothers. Turkish Journal of Psychology. 2003;18:37–52. [Google Scholar]
- 33.Gray K.M., Keating C.M., Taffe J.R., V Brereton A., Einfeld S.L., Reardon T.C., Tonge B.J. Adult outcomes in autism: community inclusion and living skills. J. Autism Dev. Disord. 2014;44:3006–3015. doi: 10.1007/s10803-014-2159-x. [DOI] [PubMed] [Google Scholar]
- 34.Steinhausen H.C., Mohr Jensen C., Lauritsen M.B. A systematic review and meta-analysis of the long-term overall outcome of autism spectrum disorders in adolescence and adulthood. Acta Psychiatr. Scand. 2016;133:445–452. doi: 10.1111/acps.12559. [DOI] [PubMed] [Google Scholar]
- 35.Imran N., Azeem M.W. Comprehensive Guide to Autism. Springer; New York, New York, NY: 2014. Autism spectrum disorders: perspective from Pakistan; pp. 2483–2496. [DOI] [Google Scholar]
- 36.Mupaku W.M., van Breda A.D., Kelly B. Transitioning to adulthood from residential childcare during COVID‐19: experiences of young people with intellectual disabilities and/or autism spectrum disorder in South Africa. Br. J. Learn. Disabil. 2021;49:341–351. doi: 10.1111/bld.12409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Şeker M., Bakış Ç., Dizeci B. Foundation for Human Development.; İstanbul: 2018. Human Development Index- Districts (HDI-D) 2017: Transitioning from Consumer to Human. [Google Scholar]
- 38.Faden S.Y., Merdad N., Faden Y.A. Parents of children with neurodevelopmental disorders: a mixed methods approach to understanding quality of life, stress, and perceived social support. Cureus. 2023 doi: 10.7759/cureus.37356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lynch F.L., Bulkley J.E., Varga A., Crawford P., Croen L.A., Daida Y.G., Fombonne E., Hatch B., Massolo M., Dickerson J.F. The impact of autism spectrum disorder on parent employment: results from the <scp>r‐Kids</scp> study. Autism Res. 2023;16:642–652. doi: 10.1002/aur.2882. [DOI] [PubMed] [Google Scholar]
- 40.Caner A., Karaoğlan D., Yaşar G. Utilization of health-care services by young children: the aftermath of the Turkish Health Transformation Program. Int J Health Plann Manage. 2018;33:596–613. doi: 10.1002/hpm.2504. [DOI] [PubMed] [Google Scholar]
- 41.Kilincaslan A., Kocas S., Bozkurt S., Kaya I., Derin S., Aydin R. Daily living skills in children with autism spectrum disorder and intellectual disability: a comparative study from Turkey. Res. Dev. Disabil. 2019;85:187–196. doi: 10.1016/j.ridd.2018.12.005. [DOI] [PubMed] [Google Scholar]
- 42.Güneş P.M. The role of maternal education in child health: evidence from a compulsory schooling law. Econ. Educ. Rev. 2015;47:1–16. doi: 10.1016/j.econedurev.2015.02.008. [DOI] [Google Scholar]
- 43.Uyanık Balat G. Okul öncesi dönemde çocuğu olan annelerin özyeterlilik ve depresyon düzeylerinin incelenmesi. Int. J. Hum. Sci./Uluslararası İnsan Bilimleri Dergisi. 2014:661–677. doi: 10.14687/ijhs.v11i2.2972. [DOI] [Google Scholar]
- 44.Güven Baysal Ş., Gümüş Doğan D., Kortay S., Arslan F.N., Demirkıran Öztürk Y., Yağın F.H. Parenting knowledge of child development in Turkish mothers and fathers. Trends in Pediatrics. 2023;4:109–119. doi: 10.59213/TP.2023.51523. [DOI] [Google Scholar]
- 45.Diken I.H. Turkish mothers' self‐efficacy beliefs and styles of interactions with their children with language delays. Early Child. Dev. Care. 2009;179:425–436. doi: 10.1080/03004430701200478. [DOI] [Google Scholar]
- 46.Papadopoulos A., Siafaka V., Tsapara A., Tafiadis D., Kotsis K., Skapinakis P., Tzoufi M. Measuring parental stress, illness perceptions, coping and quality of life in families of children newly diagnosed with autism spectrum disorder. BJPsych Open. 2023;9:e84. doi: 10.1192/bjo.2023.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rfat M., Koçak O., Uzun B. Global Social Welfare; 2023. Parenting Challenges in Families of Children with a Diagnosis of Autism Spectrum Disorder: A Qualitative Research Study in Istanbul. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hartley S.L., Papp L.M., Bolt D. Spillover of marital interactions and parenting stress in families of children with autism spectrum disorder. J. Clin. Child Adolesc. Psychol. 2018;47:S88. doi: 10.1080/15374416.2016.1152552. –S99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cetinbakis G., Bastug G., Ozel-Kizil E.T. Factors contributing to higher caregiving burden in Turkish mothers of children with autism spectrum disorders. Int. J. Dev. Disabil. 2020;66:46–53. doi: 10.1080/20473869.2018.1478630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Arslan S., Diken Ö. Examination of interactional behaviours between Turkish fathers and their children with autism spectrum disorder. International Journal of Early Childhood Special Education. 2020 doi: 10.20489/intjecse.702082. [DOI] [Google Scholar]
- 51.Sunar D. In: Autonomy and Dependence in Family: Turkey and Sweden in Critical Perspective. Özdalga E., Liljestrom R., editors. Swedish Research Institute; İstanbul: 2003. Change and continuity in the Turkish middle class family; pp. 217–238. [Google Scholar]
- 52.Kersten M., Coxon K., Lee H., Wilson N.J. Independent community mobility and driving experiences of adults on the autism spectrum: a scoping review. Am. J. Occup. Ther. 2020;74 doi: 10.5014/ajot.2020.040311. 7405205140pp.1–7405205140p.17. [DOI] [PubMed] [Google Scholar]
- 53.Afif I.Y., Farkhan M., Kurdi O., Maula M.I., Ammarullah M.I., Setiyana B., Jamari J., Winarni T.I. Effect of short-term deep-pressure portable seat on behavioral and biological stress in children with autism spectrum disorders: a pilot study. Bioengineering. 2022;9:48. doi: 10.3390/bioengineering9020048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Afif I.Y., Manik A.R., Munthe K., Maula M.I., Ammarullah M.I., Jamari J., Winarni T.I. Physiological effect of deep pressure in reducing anxiety of children with ASD during traveling: a public transportation setting. Bioengineering. 2022;9:157. doi: 10.3390/bioengineering9040157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Roskam I., Brianda M.-E., Mikolajczak M. A step forward in the conceptualization and measurement of parental burnout: the parental burnout assessment (PBA) Front. Psychol. 2018;9 doi: 10.3389/fpsyg.2018.00758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.McConkey R., Walsh J. An index of social competence for use in determining the service needs of mentally handicapped adults. J. Ment. Defic. Res. 1982;26:47–61. doi: 10.1111/j.1365-2788.1982.tb00128.x. [DOI] [PubMed] [Google Scholar]
- 57.White S.W., Elias R., Capriola-Hall N.N., Smith I.C., Conner C.M., Asselin S.B., Howlin P., Getzel E.E., Mazefsky C.A. Development of a college transition and support Program for students with autism spectrum disorder. J. Autism Dev. Disord. 2017;47:3072–3078. doi: 10.1007/s10803-017-3236-8. [DOI] [PMC free article] [PubMed] [Google Scholar]