Abstract
Many breast cancer survivors may be at increased risk for physical and psychological complications from cancer treatments. Research has shown that regular exercise can help ameliorate some of the lingering side effects of breast cancer treatments and improve health-related quality of life (HRQOL). Additionally, certain stress management techniques have helped increase HRQOL in breast cancer survivors. Few educational programs exist which address both the promotion of physical activity and use of mindfulness-based strategies to improve the health of breast cancer survivors. Community-based wellness workshops were designed to promote regular exercise and use of mindfulness-based techniques. There was an increase in physical activity and improvements on several HRQOL domains 1 month following the exercise workshops; although the results were not significant, they are encouraging.
Keywords: Breast cancer, Survivorship, Physical activity, Health-related quality of life, Wellness, Health education
Introduction
There are approximately 2.6 million breast cancer survivors in the USA. This represents the largest portion of the estimated 11.9 million cancer survivors in the USA [1]. Considering the one in eight lifetime chance of a breast cancer diagnosis and an overall 5-year breast cancer survival rate of 89.1% [2], the number of breast cancer survivors will continue to increase, leading to a large population of women with physiologic and psychological health care needs. Their unique health care needs are a result of both the cancer experience itself and the adverse effects from cancer treatments. In addition to the physical and psychological effects from the diagnosis and treatment, these women are at increased risk for recurrence; comorbidities such as weight gain, cardiovascular disease, diabetes, and osteoporosis; secondary malignancies; and premature death [3, 4]. Some breast cancer survivors may experience psychological side effects such as generalized anxiety, fear of recurrence, fear of death, and trouble concentrating [5]. Factors associated with reports of decreased quality of life in breast cancer survivors are impaired physical functioning, poor body image, a lack of social support, and inadequate coping strategies [6, 7]. There is limited information concerning the most effective way to address these needs in a comprehensive manner.
Over the past several years, there has been an accumulation of supportive evidence on the benefits of physical activity among cancer survivors. Exercise training among cancer survivors has been found to be safe and well tolerated. Additionally, exercise protects against weight gain; positively effects cardiorespiratory fitness; reduces fatigue, anxiety, and depression; and enhances overall quality of life [8, 9]. The role of post-diagnosis physical activity on breast cancer and overall mortality has been less clear, although a recent meta-analysis has provided support for the benefits of physical activity in breast cancer outcomes. Ibrahim and Al-Homaidh reported a 30% reduction in breast cancer mortality and a 41% decrease in all-cause mortality among women who engaged in physical activity post-diagnosis [10].
Considering the evidence on the benefits of certain lifestyle behaviors on cancer outcomes, the American Cancer Society (ACS) established nutrition and physical activity recommendations for cancer survivors, which include at least 150 min of moderate-intensity to vigorous physical activity per week, which is consistent with national public health guidelines for physical activity [11]. Despite these guidelines, a recent report revealed that only 37% of breast cancer survivors met the physical activity recommendations [12].
Equally important as leading an active lifestyle for breast cancer survivors is developing the coping skills needed to facilitate positive psychosocial well-being. Commonly reported psychological outcomes by breast cancer survivors include mood changes (e.g., sadness, worry, and frustration), existential concerns, fears about recurrence, and emotional distress related to role and family adjustments [13, 14]. Hodgkinson et al. reported on the supportive care needs of breast cancer survivors who were 2–10 years post-diagnosis. Results from the study revealed that anxiety rates were often equivalent to those reported by women within 3 months of a breast cancer diagnosis and among women with advanced stage disease. Additional findings from a recent meta-analysis addressing the relationship between stress-related psychosocial factors and cancer incidence and survival suggest that individuals with higher levels of distress and poor coping skills have poorer survival from breast cancer, as well as several other cancers [15]. Psycho-educational interventions can help women manage some of the distress that may persist well beyond the diagnosis of breast cancer, and it is possible that effective coping strategies may extend survival.
There is some preliminary support that community-based educational workshops may be effective in promoting positive physical and psychosocial behaviors among breast cancer survivors [16]. Therefore, our rationale for the development of community wellness workshops was to improve the physical and psychological well-being of breast cancer survivors, especially those who are considered to be traditionally underserved (i.e., ethnic minorities, under- or uninsured, and rural residents). The workshops focused on providing participants with the necessary knowledge, skills, and motivation to engage in regular physical activity and mindfulness-based practices to help facilitate positive emotions and alleviate stress, as well as provide them with community support and resources. Primary evaluation goals were to examine whether participants increased their physical activity and had improvements in perceived health-related quality of life as a result of the community wellness workshops. A secondary goal was to evaluate participant satisfaction with the workshops. Evaluation questions included: (1) Does participation in an educational wellness workshop impact the physical activity levels of breast cancer survivors?, (2) Does participation in an educational wellness workshop impact perceived health-related quality of life (HRQOL) of breast cancer survivors?, and (3) What is the level of participant satisfaction with the community wellness workshops?
Methods
Sample
Breast cancer survivors, and one of their co-survivors (e.g., spouse, daughter, friend), were invited to participate in the wellness workshops through word of mouth, flyers, emails, and news releases from partner organizations (i.e., local hospitals, community cancer centers, a community free clinic, local health departments, health clubs, and a Latina breast cancer support group). A total of 81 breast cancer survivors and18 co-survivors attended at least one of the workshops.
Procedures
Based on a community profile conducted by the NC Triangle Affiliate of Susan G. Komen for the Cure®, four North Carolina counties were selected for the workshops [17]. These counties were selected from among the13 affiliate counties because of high incidence or mortality rates, high rates of under- or uninsured women, and/or high rates of minority women with breast cancer compared to other counties. In order to achieve the goal of improving both physical and psychological quality of life among breast cancer survivors, we aimed to establish a network of collaborative partners in the four selected counties identified to be high-need areas for health education for breast cancer survivors. In partnership with the collaborative networks, the wellness workshop series were developed to meet the needs of breast cancer survivors in the designated counties. Figure 1 provides a diagram with the format and features pertinent to each of the five workshop series.
Fig. 1.
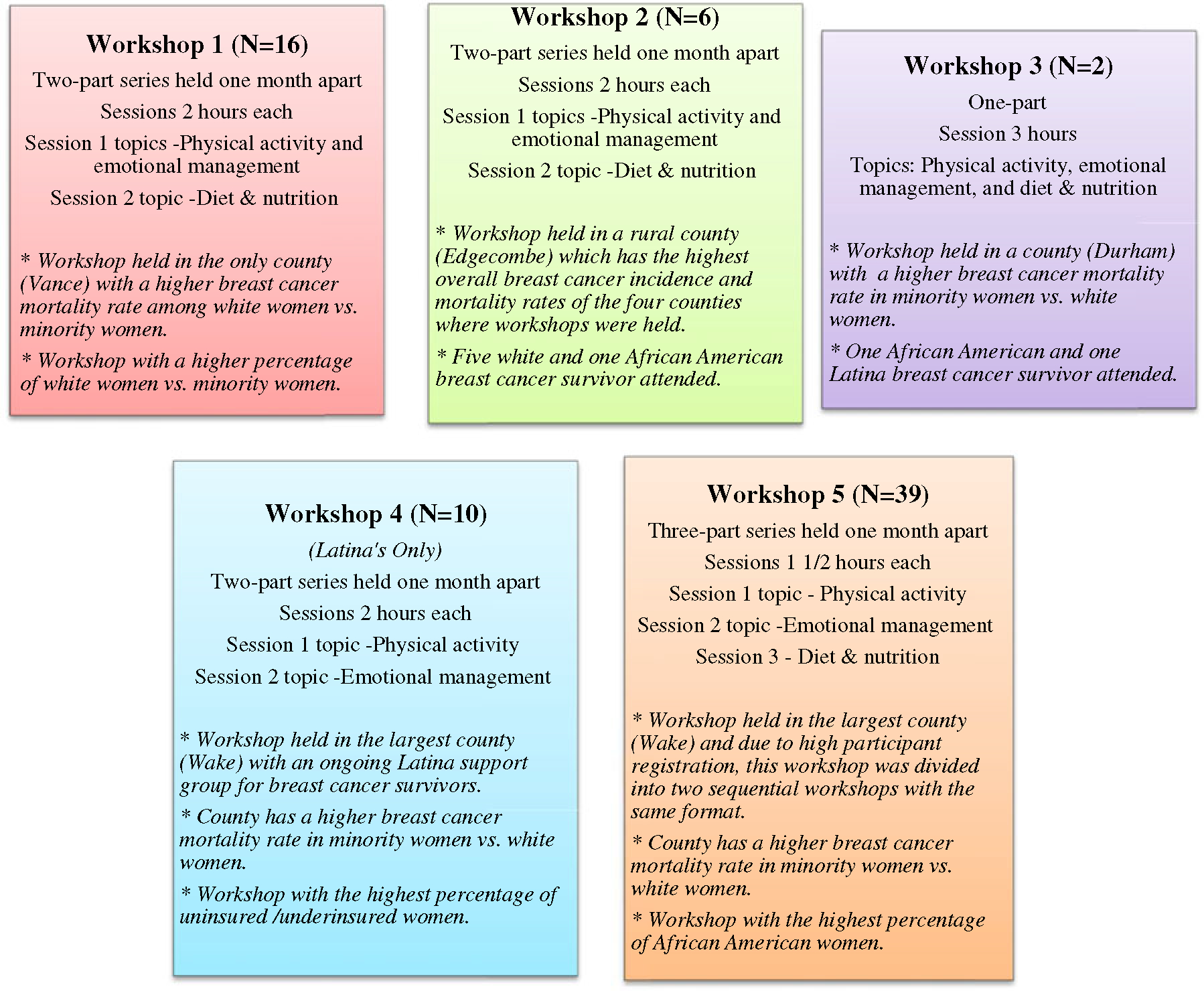
Diagram with the format and features of the five wellness workshops. Note: Co-survivors were also in attendance, but no demographic information was collected from them, and they are not included in the sample size for each workshop
Two separate workshop series were held in the largest county, one of which was developed specifically for a group of Latina women who were part of an ongoing breast cancer support group. All of the wellness workshops included information and interactive sessions on physical activity and emotional/stress management. The exercise portion of the curriculum provided an overview of the physical and psychosocial benefits of exercise, as well as instruction and guidance in safe and appropriate aerobic exercise, strength-training exercises, and stretching techniques. Latex resistance bands were used as a cost-effective form of muscular strengthening. The emotional self-management portion of the curriculum provided an overview of the mind–body connection and how emotions can impact health both negatively and positively. Participants also received instruction in HeartMath’s Quick Coherence® technique (QCT), which is a tool to refocus emotions and achieve a sense of synchronization within the autonomic nervous system [18]. The three-step technique begins by having individuals: (1) focus their breathing pattern around the area of the heart (heart focus), (2) breathe slowly and rhythmically (heart breathing), and (3) try to imagine an experience that created a positive emotion in the past (heart feeling). Individuals are encouraged to use the QCT in their daily life to engage in emotional self-regulation and stress management. Nutrition and weight management were additional topics selected for the curriculum by all but one of the collaborative partners. Therefore, these topics were also included into the workshop series for most counties, with the exception of the Latina group who recently attended a nutrition presentation. The nutrition portion of the curriculum provided a basic overview of the relationship between weight and breast cancer risk and the importance of good nutrition and calorie control on maintaining or achieving a healthy weight. Practical tips were provided by nutrition experts in the different counties on how to select healthy food options for improvement in overall health and well-being. The informational lectures were followed by cooking demonstrations and tastings where participants could sample healthy foods and receive recipes to take home. Each participant received a wellness workbook which included the following: copies of the presentation slides, exercise photos, exercise logs, tips on how to overcome exercise barriers, description of the Quick Coherence® technique, and tips and tracking tools for goals. Workbooks also included a list of literature and web resources related to health, wellness, breast cancer, and survivorship. Additionally, all participants were given a pedometer and were encouraged to increase daily physical activity with a goal of reaching 10,000 steps per day and exercising at least 150 min a week.
The design of each of the workshop series was slightly different to accommodate the needs in each community. Three of the five community partners requested a two-part workshop series with 2-h workshops held 1 month apart; one group requested a three-part workshop series with 90-min workshops held 2 weeks apart, and one community group elected a single 3-h workshop. Community partners served as hosts for each of the workshops.
Only breast cancer survivors were asked to complete the physical activity and quality of life questionnaires, which was done prior to the beginning of the content at the first workshop and again 1 month later if they were in attendance at both workshops. We were not able to collect this information in the county where we held only one workshop. All participants, breast cancer survivors and co-survivors, were asked to complete the workshop satisfaction questionnaires.
Measures
Sociodemographics
Only breast cancer participants were asked to complete an anonymous sociodemographic information form. Data were collected to obtain information on the following: age range, race, education, employment, income, insurance status, marital status, area of residence (i.e., city, suburban, or rural), and whether they were in active treatment or had completed breast cancer treatments.
Physical Activity
Physical activity was measured both at baseline and 1 month after the exercise workshop using the short form of the International Physical Activity Questionnaire (IPAQ). The seven-item self-administered questionnaire is designed to assess physical activity over the past 7 days in adults aged 18–65 years. The IPAQ has undergone extensive reliability and validity testing and has been found to have acceptable psychometric properties [19]. Typical correlation coefficients for reliability were 0.80 and were highest when tested in populations within the USA. Continuous scores calculated and expressed as metabolic equivalent minutes (METs) per week (MET-minutes/week) were determined. METs are used as a practical way to express intensity and energy expenditure of physical activity relative to resting metabolic rate, which can also be compared between individuals of varying body weights. Values for walking METs are determined using the following formula (3.3×walking minutes×walking days); moderate METs (4.0×moderate-intensity activity minutes×moderate days); and vigorous METs (8.0×vigorous-intensity activity minutes×vigorous days). Total METs were calculated by summing walking METs, moderate-intensity METs, and vigorous-intensity METs. Total physical activity in minutes per week were calculated to determine if participants met the ACS guidelines of at least 150 min of moderate to vigorous physical activity a week.
Health-Related Quality of Life
The Centers for Disease Control’s HRQOL instrument was used to measure participant’s health-related quality of life at baseline and from 2 to 4 weeks following the emotional and stress management portion of the workshop series. The instrument is widely used and has well-established reliability and validity [20]. The instrument is comprised of a four-item Healthy Days Core Module, a five-item Activity Limitations Module, and a five-item Healthy Days Symptoms Module [21]. The core module and healthy day’s symptoms module were used for pre- and post-evaluation purposes.
Question 1 of the core module is a global self-perceived health item where individuals indicate if they perceive their general health to be excellent, very good, good, fair, or poor. Higher scores indicate worse perceived general health. This item is followed by two questions that measure the number of days in the past 30 days that physical and mental health was not good. The two questions are combined to determine the “overall unhealthy days.” If the summary of unhealthy days is greater than 30, a maximum score of 30 is assigned. The five-item healthy days symptoms module asks the number of days in the last 30 days that an individual felt the following: (1) pain, (2) depression, (3) anxiety, (4) sleeplessness, and (5) energy. Higher scores on items 1–4 indicate worse health, while lower scores on item 5 indicate worse health. Scores ranged from 0 to 30.
Workshop Evaluations
All participants (i.e., breast cancer survivors and their co-survivors) were asked to complete anonymous workshop evaluations at the end of each workshop. Evaluation responses were based on 5-point Likert scales, for example: not likely=1 to very likely=5 and strongly disagree=1 to strongly agree=5. An additional section allowed for open-ended responses addressing what participants liked and disliked most about the workshops.
Statistical Analyses
Descriptive statistics were used to generate frequencies and percentages for sociodemographic characteristics of the breast cancer survivor workshop participants, as well as for determining the percentage of women who were meeting ACS guidelines for physical activity. Paired-sample t tests were conducted to examine whether total MET-minutes/week of physical activity (i.e., moderate activity, vigorous, activity, and walking) increased as a result of the exercise presentation and demonstration. A Wilcoxon signed-rank test was used to determine whether there was a change in the number of participants who met the ACS guidelines for engaging in at least 150 min of moderate to vigorous physical activity a week from baseline to follow-up. Participants were categorized as meeting or not meeting the physical activity guidelines. Paired-sample t tests were also used to examine whether changes occurred in self-rated health, number of physically healthy and mentally healthy days, overall unhealthy days, and number of days individuals experienced each of the five symptoms, as a result of the emotional/stress management interactive presentation.
Results
Sociodemographics
Of the 81 breast cancer survivors who participated in at least one of the workshops, 73 completed the sociodemographic questionnaire (see Table 1). Over 50% of the women were among minority racial groups with African American women comprising the highest percentage followed by Latina/Hispanic women. Most women were married, 45 years of age or older, and unemployed. Over 25% of the women had less than or equal to a high school education, and roughly 17% were uninsured or had Medicaid. The majority of women resided in cities or suburbs compared to 26% who resided in rural areas. Approximately 75% of the women had completed breast cancer treatments.
Table 1.
Sociodemographic characteristics of breast cancer survivors participating in the wellness workshops (N = 73)
| Characteristics | N (%) |
|---|---|
|
| |
| Race ethnicity | |
| Caucasian | 31 (42.5) |
| African American | 23 (31.5) |
| Hispanic/Latina | 11 (15.1) |
| Asian | 1 (1.4) |
| Native American | 1 (1.4) |
| Other | 1 (1.4) |
| Age | |
| 25–34 | 4 (5.5) |
| 35–44 | 5 (6.8) |
| 45–54 | 22 (30.1) |
| 55–64 | 20 (27.4) |
| 65–74 | 12 (16.4) |
| ≥75 | 5 (6.8) |
| Education | |
| Less than high school | 2 (2.7) |
| High school/GED | 18 (24.7) |
| Some college | 16 (21.9) |
| Associate’s/bachelor’s degree | 23 (31.5) |
| Graduate/professional degree | 9 (12.3) |
| Employment | |
| Full time | 25 (34.2) |
| Part time | 7 (9.6) |
| Retired | 23 (31.5) |
| Unemployed | 12 (16.5) |
| Self-employed | 1 (1.4) |
| Insurance | |
| Private | 37 (50.7) |
| Medicare | 6 (8.2) |
| Private plus Medicare | 11 (15.1) |
| Medicaid | 5 (6.8) |
| Uninsured | 8 (11.0) |
| Marital status | |
| Married | 45 (61.6) |
| Divorced/separated | 16 (13.7) |
| Single | 5 (6.8) |
| Unmarried living with partner | 3 (4.1) |
| Widowed | 5 (6.8) |
| Area of residence | |
| City | 30 (41.1) |
| Suburban | 15 (20.5) |
| Rural | 19 (26.0) |
| Cancer status | |
| Completed treatment | 49 (67.1) |
| In active treatment | 19 (26.0) |
Not all variables add up to 100% due to missing values, which ranged from 6.8% (most variables) to 12.3% (area of residence)
Physical Activity
The majority of workshop participants, for whom we had baseline data (N=64), did not meet the ACS guidelines of engaging in at least 150 min of moderate to vigorous physical activity per week (72%) compared to those who did meet the guidelines (28%). There was no significant increase in total MET-minutes/week of physical activity 1 month following the exercise workshop: t(38)=−0.278, p=0.783. However, the mean was slightly higher on the post-intervention questionnaire (pre-test M=2,085 vs. post-test M=2,185 MET-min/week). As a result of some participants’ not attending each session, pre- and post-test IPAQ data could not be compared for all participants. A Wilcoxon signed-rank test showed that the exercise workshop did not elicit a statistically significant increase in the number of participants meeting the physical activity guidelines (Z=−1.897, p=0.056); however, the result was positive in that there was a higher number of participants meeting the guidelines after the workshop compared to the baseline measures. An additional Wilcoxon analysis was conducted on data only from those women who had completed treatments (omitting data from women in active treatment), and no appreciable differences were found in significance testing.
Health-Related Quality of Life
No significant differences from baseline to final scores were found on any of the HRQOL items; however, there were decreases in the number of days that mental health was rated as not good (M=9.30 vs. 3.21 days), the number of days that pain interfered with daily activities (M=7.23 vs. 5.68 days), and the number of days not getting enough sleep or rest (M=10.45 vs. 5.40) (See Table 2). Considering the possibility that those women in active cancer treatment may have lower HRQOL scores, we also analyzed the data only for those women who had completed treatment, and significance testing was unchanged. Of the 41 women that contributed data to the HRQOL analysis, 15 were in active treatment. Due to the participants’ lack of attendance at each workshop, we were unable to collect both pre- and post-HRQOL data on all participants.
Table 2.
Changes in health-related quality of life of breast cancer participants from baseline to post-evaluation
| N | M (SD) | t | df | Sig. | |||
|---|---|---|---|---|---|---|---|
|
| |||||||
| Healthy days | General health | Pre | 41 | 2.46 (0.83) | 0.227 | 40 | 0.82 |
| Post | 41 | 2.43 (0.80) | |||||
| Physical health | Pre | 37 | 8.02 (18.1) | −0.440 | 36 | 0.66 | |
| Post | 37 | 9.32 (18.6) | |||||
| Mental health | Pre | 37 | 9.30 (19.1) | 1.92 | 32 | 0.064 | |
| Post | 33 | 3.21 (4.9) | |||||
| Sum healthy days | Pre | 27 | 7.96 (9.4) | −1.08 | 26 | 0.287 | |
| Post | 27 | 9.88 (10.9) | |||||
| Symptom days | Pain | Pre | 38 | 7.23 (18.0) | 0.419 | 37 | 0.678 |
| Post | 38 | 5.68 (14.3) | |||||
| Sad | Pre | 32 | 7.21 (19.0) | −0.226 | 31 | 0.823 | |
| Post | 32 | 7.85 (19.4) | |||||
| Worried | Pre | 35 | 6.94 (18.8) | −0.370 | 34 | 0.714 | |
| Post | 35 | 8.22 (18.4) | |||||
| Sleepless | Pre | 35 | 10.45 (18.8) | 1.57 | 34 | 0.126 | |
| Post | 35 | 5.40 (7.4) | |||||
| Energy | Pre | 36 | 21.8 (24.6) | 1.40 | 35 | 0.170 | |
| Post | 36 | 16.6 (18.1) | |||||
A lower score indicates better health in all categories except energy where higher scores indicate better health
Workshop Evaluations
Written evaluations were distributed after each workshop. In most counties, attendance was highest at the first session of each workshop series. The majority of participants indicated that they would very likely use the information and skills they learned through the workshops to increase their daily physical activity and emotional well-being, as well as improve their nutrition. Additionally, most participants indicated that they strongly agreed that each of the workshops provided a positive experience for them (see Table 3). The majority of participants, 81% (N=75), were able to correctly identify three benefits of regular exercise. Participant responses included both physical and psychological benefits such as: “increase energy,” “muscle tone,” “flexibility,” “heart health,” “weight loss,” “reduce blood pressure,” “decrease cholesterol,” “improve sleep,” “relieve tension,” “fight depression,” “improve mood,” “mental concentration,” and “better body image.” Comments in response to what participants liked most about the workshops included the following: “Provided knowledge of what I can do to help myself,” “Motivated speakers made me excited about exercise program,” “Can understand the importance of exercising,” “It was both practical & theoretical,” “It shows how easy it is to perform physical exercise,” “Relaxed & open seminars. Food was great!” “Practical information presented in an interesting way,” “The heart math activity was great, practical and easy to both implement & share,” and “The most important thing is that I was reminded to focus on positive thinking and positive emotions every day.” Participant comments about what they liked least about the workshop series were the following: “That I have limitations that make some of the exercises difficult/impossible,” “It ran a bit long,” “It was at night,” and “The briefness of sessions—wish there were more.”
Table 3.
Community wellness workshop evaluations
| Evaluation question/statement | N | Mean and SD (scales ranged from 1 to 5)a |
|---|---|---|
|
| ||
| Please indicate how likely or unlikely you are to... | ||
| Use the information and skills you learned to increase your daily physical activity? | 76 | 4.88 (0.68) |
| Use the information and skills you learned to increase your emotional well-being? | 61 | 4.50 (0.60) |
| Use the information and skills you learned to improve your nutrition? | 46 | 4.72 (0.46) |
| Please indicate how much you agree or disagree with the following statements: | ||
| The exercise portion of the workshop was a positive experience for me. | 75 | 4.77 (0.75) |
| The emotional management portion of the workshop was a positive experience for me. | 60 | 4.50 (0.61) |
| The diet and nutrition portion of the workshop was a positive experience for me. | 45 | 4.91 (0.29) |
Scales ranged from 1 = not likely/strongly disagree to 5 = very likely/strongly agree. Evaluations obtained from breast cancer survivors and their co-survivors who attended
Discussion
Among the breast cancer survivors participating in the workshops, the percentage meeting national guidelines for physical activity (≥150 min/week of moderate to vigorous activity) is lower (28%) compared to other breast cancer survivors (37.1%) and to women in the general US population (47%) [12, 22]. Our population was comprised of a higher percentage of ethnic minorities, 51% compared to approximately 21% in the study by Blanchard et al. [12], and it is known that African American and Hispanic breast cancer survivors report lower levels of physical activity [23, 24]. This may in part help explain the lower percentage of workshop participants who met national physical activity guidelines, although data were not analyzed separately on race/ethnicity.
While there were no statistically significant improvements in physical activity 1 month following the exercise component of the workshops, there were positive changes reflecting that some participants increased their weekly frequency of exercise and went from not meeting physical activity guidelines (≥150 min of physical activity/week) prior to the workshop to engaging in 150 min or more of physical activity a month after the workshop. It may not be a realistic expectation that one exercise workshop can overturn long-standing barriers that constrain survivors from exercising 150 min/week 4 weeks following the workshop, but the fact that the findings revealed some positive changes in physical activity levels is promising. Participants were also encouraged to gradually increase their physical activity to a level of comfort and ability, as safety was a primary concern. Therefore, increasing physical activity to 150 min a week was a longer-term goal for most women.
Improvements in several dimensions of the HRQOL measure occurred following the workshops on exercise and emotional management techniques, although none of the changes were statistically significant. The HRQOL dimensions that improved were as follows: mental health, pain, sleep, energy, and being worried. Studies have shown that regular physical exercise and the use of some psychological techniques (e.g., cognitive and behavior therapy, relaxation training, counseling, and psychosocial education) are associated with decreased fatigue, less depression and anxiety, and overall improvements in HRQOL [24, 25]. Therefore, the incorporation of easy-to-use and accessible interventions such as the QCT® that encourage positive emotions and stress reduction can be a valuable addition to wellness workshops. There is an increasing body of evidence to suggest that facilitating positive emotions and helping individuals adequately deal with lingering negative emotions such as anxiety, stress, and helplessness can improve immune function and improve psychosocial and physiological resilience [26]. These techniques may be particularly effective if combined with the promotion of physical activity for breast cancer survivors.
Smith et al. [24] found a positive relationship between higher quality of life and meeting national public health recommendations for physical activity among both black and white breast cancer survivors, but not among Hispanic breast cancer survivors. Findings from the meta-analysis by Duijts et al. [25] revealed statistically significant improvements in fatigue, stress, depression, and anxiety as a result of various behavioral and psychosocial interventions with breast cancer patients and survivors. Additionally, physical activity was found to be significantly related to improvements in fatigue, depression, body image, and HRQOL. Although relationships between physical activity and HRQOL were not examined from the data on the workshop participants, some of the post-assessment HRQOL measures, along with the post-assessment IPAQ scores, improved after the workshops.
Overall, our findings are encouraging, and it is possible that the workshops had a positive impact on the physical activity behaviors and HRQOL among some of the participants, although direct inferences about any relationships cannot be determined. Additionally, the incorporation of the QCT® into the workshops may have been beneficial to those participants who practiced the technique after the completion of the workshop series. However, practice of the technique was not assessed as a component of the workshop evaluation. Strategies that encourage positive emotions and stress reduction may be particularly effective when combined with physical activity interventions and therefore warrant further study.
Limitations
A few limitations that must be taken into consideration include the use of self-report for the physical activity assessments, participant attrition after the first workshop in each series, and the lack of a longer-term follow-up to assess both physical activity and HRQOL. Due to the fact that many women we had collected baseline data on (N=73) did not return for the second workshop, we were unable to obtain follow-up data on physical activity and HRQOL, which limited our sample size for comparative analyses on these measures. An additional limitation is that relationships between sociodemographic factors, physical activity, and HRQOL were not examined.
It is well known that physical activity measures, such as the IPAQ, may lead to self-report bias. However, it would have been impractical to objectively assess physical activity as a part of community educational wellness workshops. The second limitation was the lack of participant attendance after the initial workshop in the series. Participants were required to register in advance of the workshop series in each of the communities, and at the time of registration, they were informed that attendance was expected at each session within the series. However, there was a drop in attendance after the first workshop session in all but one of the communities, which led to smaller sample sizes for conducting statistical analyses on the pre- and post-assessments of physical activity and HRQOL. This limited the ability to assess the impact of the workshops on participants’ physical activity and on their HRQOL. Third, no long-term follow-up assessments on physical activity or HRQOL were conducted. Therefore, we were unable to determine whether physical activity patterns and HRQOL changed over a longer time frame following the workshops. Concerns were raised about participant burden, so follow-up phone calls or mailed assessments were not included as part of the evaluation process. Finally, it would have been valuable to examine whether any specific sociodemographic factors were related to physical activity behavior and HRQOL to help determine which subgroups may have the highest need for future wellness workshops.
Conclusions
In the long term, it is expected that the wellness workshops will contribute to the establishment of healthy lifestyle behaviors among the breast cancer participants and their co-survivors in the four counties, which may ultimately lead to improvements in quality of life and possibly reductions in mortality. The content of the workshops complemented and reinforced public health initiatives focused on cancer survivors, such as the report from the Institute of Medicine entitled, “From Cancer Patient to Cancer Survivor: Lost in Transition,” which recommends that health care providers and health educators encourage the adoption of healthy lifestyle behaviors among cancer survivors to improve overall health and quality of life [5].
As more data emerge regarding the relationships between regular physical activity, the use of stress-reducing techniques, and better health outcomes among breast cancer survivors, it will become increasingly important to develop educational programs which encompass both mind and body approaches to improve health outcomes among diverse groups of breast cancer survivors, especially for women who are traditionally underserved (i.e., ethnic minorities, under- and uninsured, and rural residents). Cancer care clinicians and educators may have to design tailored programs to better meet the needs of breast cancer survivors from populations that may have very different health beliefs and barriers towards the engagement in exercise and/or emotional management techniques for improving health after a breast cancer diagnosis.
Acknowledgments
The authors would like to acknowledge Lineberger Comprehensive Cancer Center and the Department of Exercise and Sport Science at the University of North Carolina at Chapel Hill, as well as the Petro Kuylnich Foundation and the NC Triangle Affiliate of Susan G. Komen for the Cure® for their support of the Get REAL & HEEL after-care breast cancer program. We would also like to thank all of the community partners for their dedication and efforts and especially the individuals who participated in the educational sessions.
Contributor Information
D. Spector, Department of Nutrition, Gillings School of Global Public Health, and the Department of Exercise and Sport Science, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, USA
C. Battaglini, Department of Exercise and Sport Science, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, USA Get REAL & HEEL Breast Cancer Program, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, USA.
A. Alsobrooks, Get REAL & HEEL Breast Cancer Program, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, USA
J. Owen, Get REAL & HEEL Breast Cancer Program, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, USA
D. Groff, Department of Exercise and Sport Science, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, USA Get REAL & HEEL Breast Cancer Program, University of North Carolina at Chapel Hill, Chapel Hill, NC 27599, USA.
References
- 1.National Cancer Institute (2011) Cancer survivorship research, estimated US cancer prevalence counts: who are our cancer survivors in the U.S At: http://cancercontrol.cancer.gov/ocs/prevalence/index.html. Accessed 25 August 2011
- 2.Howlader N, Noone AM, Krapcho M, Neyman N, Aminou R, Waldron W, Altekruse SF, Kosary CL, Ruhl J, Tatalovich Z, Cho H, Mariotto A, Eisner MP, Lewis DR, Chen HS, Feuer EJ, Cronin KA, Edwards BK (eds) (2011) SEER cancer statistics review, 1975–2008, National Cancer Institute. Bethesda, MD. At: http://seer.cancer.gov/csr/1975_2008/. Accessed 25 August 2011 [Google Scholar]
- 3.Brines J, Gradishar W (1997) Primary care issues for the breast cancer survivor. Compr Ther 23:605–611 [PubMed] [Google Scholar]
- 4.Hewitt M, Rowland JH, Yancik R (2003) Cancer survivors in the United States: age, health, and disability. J Gerontol Ser A Biol Sci Med Sci 58:82–91 [DOI] [PubMed] [Google Scholar]
- 5.Hewitt M, Greenfield S, Stovall EL, Institute of Medicine and National Research Council (2005) From cancer patient to cancer survivor: lost in transition. National Academies Press, Washington [Google Scholar]
- 6.Avis NE, Crawford S, Manuel J (2005) Quality of life among younger women with breast cancer. J Clin Oncol 23:3322–3330 [DOI] [PubMed] [Google Scholar]
- 7.Mandelblatt J, Ueiredo M, Cullen J (2003) Outcomes and quality of life following breast cancer treatment in older women: when, why, how much, and what do women want? Health Qual Life Outcomes 1:45–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Demark-Wahnefried W, Jones LW (2008) Promoting a healthy lifestyle among cancer survivors. Hematol Oncol Clin N Am 22:319–342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rock CL, Demark-Wahnefried W (2002) Can lifestyle modification increase survival in women diagnosed with breast cancer? J Nutr 132(Suppl, 11):3504–3507 [DOI] [PubMed] [Google Scholar]
- 10.Ibrahim EM, Al-Homaidh A (2010) Physical activity and survival after breast cancer diagnosis: meta-analysis of published studies. Medical Oncology. At: http://www.springerlink.com.libproxy.lib.unc.edu/content/g570w876754u7261/. Accessed 10 June 2011 [DOI] [PubMed]
- 11.Doyle C, Kushi L, Byers T, Courneya KS, Demark-Wahnefried W, Grant B et al. (2006) Nutrition and physical activity during and after cancer treatment: an American Cancer Society guide to informed choices. CA Cancer J Clin 56:323–353 [DOI] [PubMed] [Google Scholar]
- 12.Blanchard CM, Courneya KS, Stein K (2008) Cancer survivors’ adherence to lifestyle behavior recommendations and associations with health-related quality of life: results from the American Cancer Society’s SCS-II. J Clin Oncol 26:2198–2204 [DOI] [PubMed] [Google Scholar]
- 13.Hodgkinson K, Butow P, Hunt GE, Pendlebury S, Hobbs KM, Wain G (2007) Breast cancer survivors’ supportive care needs 2–10 years after diagnosis. Support Care Cancer 15:515–523 [DOI] [PubMed] [Google Scholar]
- 14.Knobf MT (2007) Psychological responses in breast cancer survivors. Semin Oncol Nurs 23:71–83 [DOI] [PubMed] [Google Scholar]
- 15.Chida Y, Hamer M, Wardle J, Steptoe A (2008) Do stress-related psychosocial factors contribute to cancer incidence and survival? Nat Clin Pract Oncol 5:466–475 [DOI] [PubMed] [Google Scholar]
- 16.Alsobrooks A, Owen J, Groff D, Battaglini C, Evans E, Brustad R (2010) Promoting physical and psychosocial health behavior changes in breast cancer survivors through a community-based workshop: process and impact evaluation. Am J Recreat Ther 9:39–46 [Google Scholar]
- 17.Barrett N (2009) Susan G. Komen for the Cure, NC Triangle community health profile, 2009. At: http://www.komennctriangle.org/assets/grants-documents/2009-community-profile.pdf. Accessed 5 June 2010
- 18.Childre D, Rozman D (2005) Transforming stress: the HeartMath® solution for relieving worry, fatigue, and tension. New Harbinger Publications, Oakland [Google Scholar]
- 19.Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE et al. (2003) International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 35:1381–1395 [DOI] [PubMed] [Google Scholar]
- 20.Hagerty MR, Cummins R, Ferriss A, Land K, Michalos A, Peterson M et al. (2001) Quality of life indexes for national policy: review and agenda for research. Soc Indic Res 55:1–96 [Google Scholar]
- 21.Centers for Disease Control and Prevention (2000) Measuring healthy days. CDC, Atlanta [Google Scholar]
- 22.Centers for Disease Control (2010) U.S. physical activity statistics. At: http://apps.nccd.cdc.gov/PASurveillance. Accessed 9 December 2011
- 23.Hong S, Bardwell WA, Natarajam L, Flatt SW, Rock CL, Newman VA et al. (2007) Correlates of physical activity level in breast cancer survivors participating in the Women’s Healthy Eating and Living (WHEL) Study. Breast Cancer Res Treat 101:225–232 [DOI] [PubMed] [Google Scholar]
- 24.Smith AW, Alfano CM, Reeve BB, Irwin ML, Bernstein L, Baumgartner K et al. (2009) Race/ethnicity, physical activity, and quality of life in breast cancer survivors. Cancer Epidemiol Biomark Prev 18:656–663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Duijts SFA, Faber MM, Oldenburg HSA, van Beurden M, Aaronson NK (2011) Effectiveness of behavioral techniques and physical exercise on psychosocial functioning and health-related quality of life in breast cancer patients and survivors—a meta-analysis. Psychooncology 20:115–126 [DOI] [PubMed] [Google Scholar]
- 26.Servan-Schreiber D (2008) Anti-cancer: a new way of life. Penguin Group, New York [Google Scholar]


