Abstract
Background
Three-dimensional-printed anatomical models (3DPAMs) appear to be a relevant tool due to their educational value and their feasibility. The objectives of this review were to describe and analyse the methods utilised for creating 3DPAMs used in teaching human anatomy and for evaluating its pedagogical contribution.
Methods
An electronic search was conducted on PubMed using the following terms: education, school, learning, teaching, learn, teach, educational, three-dimensional, 3D, 3-dimensional, printing, printed, print, anatomy, anatomical, anatomically, and anatomic. Data retrieved included study characteristics, model design, morphological evaluation, educational performance, advantages, and disadvantages.
Results
Of the 68 articles selected, the cephalic region was the most studied (33 articles); 51 articles mentioned bone printing. In 47 articles, the 3DPAM was designed from CT scans. Five printing processes were listed. Plastic and its derivatives were used in 48 studies. The cost per design ranged from 1.25 USD to 2800 USD. Thirty-seven studies compared 3DPAM to a reference model. Thirty-three articles investigated educational performance. The main advantages were visual and haptic qualities, effectiveness for teaching, reproducibility, customizability and manipulability, time savings, integration of functional anatomy, better mental rotation ability, knowledge retention, and educator/student satisfaction. The main disadvantages were related to the design: consistency, lack of detail or transparency, overly bright colours, long printing time, and high cost.
Conclusion
This systematic review demonstrates that 3DPAMs are feasible at a low cost and effective for teaching anatomy. More realistic models require access to more expensive 3D printing technologies and substantially longer design time, which would greatly increase the overall cost. Choosing an appropriate image acquisition modality is key. From a pedagogical viewpoint, 3DPAMs are effective tools for teaching anatomy, positively impacting the learning outcomes and satisfaction level. The pedagogical effectiveness of 3DPAMs seems to be best when they reproduce complex anatomical areas, and they are used by students early in their medical studies.
Keywords: Anatomy, Learning, Review, Teaching, 3D printing
Introduction
Practiced since Ancient Greece on animals, cadaver dissection is one of the main methods used to teach anatomy. Cadaveric dissection, carried out during hands-on training, supports the theoretical lessons given to medical students in universities and is currently considered the gold standard for learning anatomy [1–5]. However, there are many obstacles to using human cadaveric specimens, prompting a search for new pedagogical tools [6, 7]. Some of these new tools are extended reality, digital tools, and 3D printing. According to a recent literature review by Santos et al. [8] on the value of these new technologies for teaching anatomy, 3D printing appears to be one of the most relevant resources both in terms of its educational value to students and the feasibility of its implementation [4, 9, 10].
3D printing is not new. The first patents related to this technology date back to 1984: A Le Méhauté, O De Witte and JC André in France and 3 weeks later, C Hull in the USA. Since then, this technology has undergone continuous development, and its use has spread to numerous fields. For example, NASA printed the first object outside the planet Earth in 2014 [11]. The medical field has also appropriated this new tool, thus reinforcing the desire to develop personalized medicine [12].
Many authors have demonstrated the pedagogical benefits of using 3D-printed anatomical models (3DPAM) for medical education [10, 13–19]. When it comes to teaching human anatomy, non-pathological and anatomically normal models are required. Several reviews have studied pathological models or training models for a medical/surgical procedure [8, 20, 21]. With the intention of developing a hybrid teaching model for human anatomy that incorporates new tools such as 3D printing, we carried out a systematic review to describe and analyse how 3D-printed objects made for teaching of human anatomy are created and how students evaluate the pedagogical contribution of these 3D objects.
Materials and methods
This systematic review of the literature was conducted in June 2022 without time limitation using the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [22].
Eligibility criteria
Inclusion criteria were all research papers dealing with 3DPAM in anatomy teaching/learning. Literature reviews, letters, or articles studying pathological models, animal models, archaeological models, and medical/surgical training models were excluded. Only articles published in English were selected. Articles without available online abstracts were excluded. Articles dealing with several models – at least one of which was anatomically normal or had trivial pathology that did not alter the pedagogical value – were included.
Search strategy
A literature search was performed in the electronic PubMed database (National Library of Medicine, NCBI) to identify relevant studies published up to June 2022. The following search terms were used: education, school, learning, teaching, learn, teach, educational, three-dimensional, 3D, 3-dimensional, printing, printed, print, anatomy, anatomical, anatomically, and anatomic. A single query was carried out: (((education[Title/Abstract] OR school[Title/Abstract] OR learning[Title/Abstract] OR teaching[Title/Abstract] OR learn[Title/Abstract] OR teach[Title/Abstract] OR educational[Title/Abstract]) AND (three dimensional[Title] OR 3D[Title] OR 3 dimensional[Title])) AND (printing[Title] OR printed[Title] OR print[Title])) AND (anatomy[Title/Abstract] OR anatomical[Title/Abstract] OR anatomically[Title/Abstract] OR anatomic[Title/Abstract]). Additional articles were identified through a manual search in the PubMed database and by looking through the references of other scientific articles. No date restriction was applied but the “human” filter was used.
Study selection
All retrieved titles and abstracts were screened against the inclusion and exclusion criteria by two authors (EBR & AL), and any study that did not meet all the eligibility criteria were excluded. Full-text publications of the remaining studies were obtained and screened by three authors (EBR, EBE & AL). Any disagreement in the selection of articles was resolved, if necessary, by a fourth person (LT). Publications that met all the inclusion criteria were included in this review.
Data extraction
Data extraction was performed independently by two authors (EBR & AL) and supervised by a third (LT).
The extracted data consisted of:
- study characteristics: publication date, country of authors, type of study
- model design data: anatomical region, specific anatomical part, initial model used for 3D printing, acquisition method, segmentation and modelling software, type of 3D printer, type and number of materials, printing scale, colours, cost of printing
- morphological evaluation of the model: model used for comparison, medical evaluation by an expert/teacher, number of raters, type of evaluation
- pedagogical performance of the 3D model: student knowledge assessment, assessment methods, number of students, number of comparison groups, randomization of students, type of education/student
- advantages and disadvantages.
All data were extracted in predefined forms.
Results
Study selection
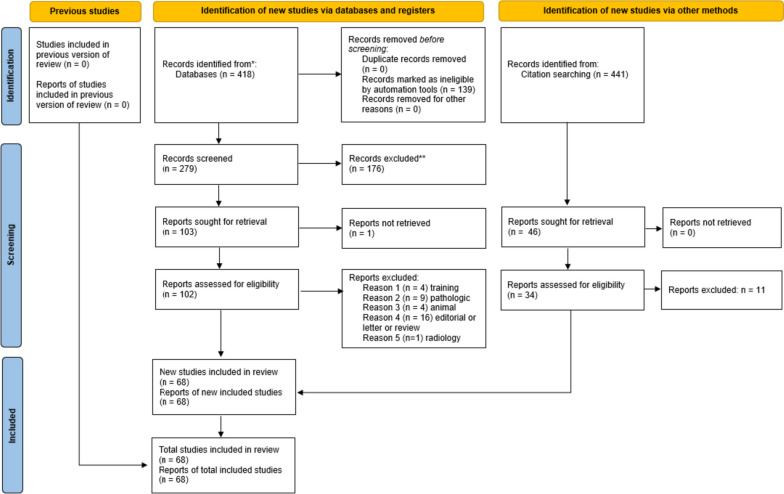
Four hundred eighteen studies were identified in the MEDLINE database; 139 articles were excluded by the “human” filter. After the title and abstract were analysed, 103 studies were selected for reading of the full text. Thirty-four articles were excluded because they were either pathological models (9 articles), medical/surgical training models (4 articles), animal models (4 articles), 3D radiology models (1 article) or were not original scientific papers (16 articles). A total of 68 articles were included in this review. Figure 1 summarizes the selection process with a flowchart.
Fig. 1.
Flow diagram summarizing the identification, screening and inclusion of articles for this systematic review
Study characteristics
All studies were published between 2014 and 2022, with the average year of publication being 2019. Of the 68 articles included, 33 (49%) studies were descriptive and experimental, 17 (25%) were purely experimental and 18 (26%) were purely descriptive. Among the 50 (73%) experimental studies, 21 (31%) used randomization. Only 34 studies (50%) included a statistical analysis. Table 1 summarizes the characteristics of each study included.
Table 1.
Summary of study characteristics
| Author (Year) | Country | Type of study | Design of study | Description | Use of statistical tools |
|---|---|---|---|---|---|
| Ben Awadh et al. (2022) [23] | United Kingdom | Experimental | Randomized comparative controlled | 3DPAM enhances novice learner interpretation of cross-sectional anatomy of the thorax | Y |
| Cercenelli et al. (2022) | Italy | Experimental and descriptive | Randomized | Educational tool evaluation combining 3DPAM and augmented reality | Y |
| Chandrasekaran et al. (2022) [24] | Singapore | Experimental | Randomized controlled cross-over | Validated instrument measuring students’ perceptions on plastinated and 3DPAM of the heart and the neck | Y |
| Hammerton et al. (2022) [25] | United Kingdom | Experimental | 3DPAM acceptation for assessment by students and educators | N | |
| Harmon et al. (2022) [26] | USA | Descriptive | 3DPAM for health science students | N | |
| Mogali et al. (2022) [27] | Singapore | Experimental | Randomized controlled cross-over | Effectiveness of 3DPAM compared to plastinated in learning cardiac and neck anatomy | Y |
| Saleh et al. (2022) | United Kingdom | Descriptive and experimental | Design of 3DPAM skull base, collaboration between clinicians and industry | N | |
| Tan et al. (2022) [28] | China | Descriptive and experimental | Full color 3DPAM of the head and the upper limb | N | |
| Bertolini et al. (2021) [29] | Italy | Descriptive and experimental | 3DPAM of the heart | N | |
| Krishnasamy et al. (2021) [30] | Malaysia | Descriptive and experimental | Heart 3DPAM rapid prototyping | N | |
| Mahrous et al. (2021) [31] | USA | Descriptive and experimental | Comparison of instructional technologies: natural teeth, 3DPAM et augmented reality | Y | |
| O’Brien et al. (2021) [32] | Canada | Experimental | Randomized controlled | Tracheo-bronchial 3DPAM to improve students understanding of segmentation anatomy | Y |
| Ruiz and Dhaher (2021) [33] | Italy and USA | Descriptive and experimental | Multi-color and multi-material 3DPAMs of knee joint | N | |
| Smillie et al. (2021) [34] | United Kingdom | Descriptive and experimental | Producing 3DPAM of hepatobiliary system from CT imaging data | N | |
| Vatankhah et al. (2021) [35] | Iran | Experimental | Randomized | 3DPAM for teaching orbital anatomy | Y |
| Weatherall et al. (2021) [36] | Australia | Descriptive | 3DPAM of pediatric airway models | N | |
| Abdulcadir et al. (2020) [37] | Switzerland | Descriptive and experimental | 3DPAM pelvic prototype to improve sexual anatomy and physiology | N | |
| Chae et al. (2020) [38] | USA | Descriptive and experimental | Comparison between 3DPAM and 3D scanned temporal bone models | Y | |
| Chedid et al. (2020) [39] | USA | Experimental | Randomized controlled cross-over | 3DPAM of the liver helps learner identify hepatic subsegments | Y |
| Chen et al. (2020) [40] | China | Experimental | Randomized comparative | 3DPAM improves residents’ understanding of gastrocolic trunk anatomy | Y |
| Damon et al. (2020) [41] | USA | Descriptive | Orientation planning of anatomical spine 3DPAM | N | |
| Hojo et al. (2020) [42] | Japan | Descriptive and experimental | Utility of pelvic 3DPAM for lymph node dissection | Y | |
| Javan et al. (2020) [43] | USA | Descriptive and experimental | 3D visualization of pterygopalatine fossa using 3DPAM, serious game and virtual reality | N | |
| Low et al. (2020) [44] | USA | Descriptive | Construction of frontal sinus 3DPAM | N | |
| Radzi et al. (2020) [45] | Singapore | Descriptive and experimental | Heart 3DPAM for learning anatomy | Y | |
| Tanner et al. (2020) [46] | USA | Descriptive and experimental | Randomized | Pterygopalatine 3DPAM enhances learning | Y |
| Tripodi et al. (2020) [47] | Australia | Descriptive | Impact of bones 3DPAM on first year students | Y | |
| Williams et al. (2020) [48] | United Kingdom | Descriptive | High fidelity retroperitoneal 3DPAM | N | |
| Backhouse al. (2019) [49] | Australia | Descriptive and experimental | 3DPAM enables active and personalized learning | Y | |
| Bartikian et al. (2019) [50] | Portugal | Descriptive and experimental | 3DPAM of head bones | N | |
| Cai et al. (2019) [51] | Singapore | Descriptive and experimental | Effects of knee joint 3DPAM in improving anatomical spatial knowledge | Y | |
| Hojo et al. (2019) [52] | Japan | Experimental | Randomized controlled | Utility of pelvic 3DPAM for lateral pelvic lymph node dissection education | Y |
| Kanagasuntheram et al. (2019) [53] | Singapore | Descriptive | Composite midcarpal joint 3DPAM | N | |
| Low et al. (2019) | USA | Descriptive and experimental | Randomized | Use of frontal sinus 3DPAM and 2D illustrations for resident education | Y |
| Shen et al. (2019) [54] | China | Descriptive | Process of skull 3DPAM for anatomy education | N | |
| Skrzat et al. (2019) [55] | Poland | Descriptive and experimental | Temporal bone 3DPAM for teaching gross anatomy | N | |
| Ugidos Lozano et al. (2019) [56] | Spain | Descriptive and experimental | Applicability of 3DPAM for students of health sciences | N | |
| Yi et al. (2019) [57] | China | Experimental | Randomized controlled | Ventricular system 3DPAM in anatomy education | Y |
| Young et al. (2019) | Australia | Descriptive | 3DPAM of archive human fetal material for teaching | N | |
| Zhang et al. (2019) [58] | China | Descriptive and experimental | 3DPAM for undergraduate medical students | Y | |
| Bannon et al. (2018) [59] | Scotland | Descriptive | Pterygopalatine fossa negative 3DPAM | N | |
| Casciato et al. (2018) [60] | USA | Descriptive | 3DPAM to enhance cross sectional anatomy instruction | N | |
| Garas et al. (2018) [61] | Australia | Experimental | 3DPAM as a tool for anatomy education | Y | |
| Mogali et al. (2018) [62] | Singapore | Descriptive and experimental | Evaluation by medical students of upper limb 3DPAM | Y | |
| Smith C.F et al. (2018) [63] | United Kingdom | Experimental | Randomized controlled | 3DPAM in undergraduate anatomy education | Y |
| Smith M.L et al. (2018) [64] | Ireland | Descriptive | 3DPAM for anatomy education | Y | |
| Suzuki et al. (2018) [65] | Japan | Descriptive | Transparent temporal bone and vestibulocochlear 3DPAM | N | |
| Ugidos Lozano et al. (2018) | Spain | Descriptive | Different digitalization techniques for 3DPAM | N | |
| Wu et al. (2018) [66] | China | Experimental | Randomized controlled | 3DPAM enhance teaching and learning bone spatial anatomy | Y |
| Zhang et al. (2018) [67] | China | Descriptive and experimental | Randomized | Paranasal sinus 3DPAM | Y |
| Bücking et al. (2017) [68] | United Kingdom | Descriptive | From medical imaging to 3DPAM | N | |
| Chen et al. (2017) [69] | China | Experimental | Randomized controlled | Role of skull 3DPAM in anatomy education | Y |
| Favier et al. (2017) [70] | France | Descriptive and experimental | Skull base 3DPAM for anatomical education and surgery simulation | N | |
| Javan et al. (2017) [71] | USA | Descriptive | Cranial nerves 3DPAM | N | |
| Kavanagh et al. (2017) | USA | Descriptive and experimental | Pediatric laryngeal simulator using 3DPAM | Y | |
| Legocki et al. (2017) [72] | USA | Descriptive and experimental | Maxillofacial skeletal 3DPAM for entry-level | N | |
| Lozano et al. (2017) [73] | Spain | Descriptive and experimental | Skull 3DPAM digitalization and prototyping | N | |
| Fasel et al. (2016) [74] | Switzerland | Descriptive and experimental | Adapting anatomy teaching to surgical trends with classical dissection, 3DPAM and medical imaging | Y | |
| Javan et al. (2016) [75] | USA | Descriptive | Understanding spatially complex anatomy with 3DPAM | N | |
| Kong et al. (2016) [76] | China | Experimental | Randomized controlled comparative | 3DPAM to improve teaching about hepatic segments to medical students | Y |
| Kong et al. (2016) [77] | China | Experimental | Randomized controlled | 3DPAM to improve teaching about hepatic segments to medical students | Y |
| Lim et al. (2016) [16] | Australia | Experimental | Randomized controlled | Comparison between 3DPAM and cadaveric dissection for learning cardiac extern anatomy | Y |
| O’Reilly et al. (2016) [78] | Dublin | Descriptive and experimental | Randomized | Fabrication and assessment of lower limb et femoral vessel 3DPAM | Y |
| Shah et al. (2016) [79] | USA | Descriptive and experimental | Skull base 3DPAM to teach anatomy to neurosurgery residents | N | |
| Adams et al. (2015) [80] | Australia | Descriptive and experimental | Orbital dissection 3DPAM reproduction for trainees in ophthalmology or optometry | N | |
| Cohen et al. (2015) [81] | USA | Descriptive and experimental | Creation of temporal bone 3DPAM | N | |
| Hochman et al. (2015) [82] | Canada | Descriptive and experimental | Randomized | Comparison between 3DPAM and virtual haptic temporal bone | Y |
| McMenamin al. (2014) [83] | Australia | Descriptive | Production of anatomical teaching resources using 3DPAM | N |
Abbreviations: 3DPAM 3D printed anatomical model, N no, Y yes
Model design data
Thirty-three articles (48%) studied the cephalic region, 19 (28%) the thoracic region, 17 (25%) the abdominopelvic region and 15 (22%) the limbs. Fifty-one articles (75%) mentioned 3D printing of bone as an anatomical model or within a multi-slice anatomical model.
Regarding the original model or file used for designing the 3DPAM, 23 articles (34%) mentioned the use of patient data, 20 articles (29%) the use of cadaver data, 17 articles (25%) the use of a database, and 7 studies (10%) did not disclose the origin of the file used.
In 47 studies (69%), the 3DPAMs were designed from CT scans, while 3 studies (4%) specified using micro-CT scans. In 7 articles (10%), the 3D objects were designed from optical scanners, in 4 articles (6%) from MRI and in 1 article (1%) from a camera and microscope. In 14 articles (21%), the origin of the source files for the design of the 3D model was not mentioned. The average spatial resolution was less than 0.5 mm for creating the 3D files. The best resolution was 30 µm [80] and the highest was 1.5 mm [32].
Sixty different software applications (segmentation, modelling, design, or printing) were used. Mimics (Materialise, Leuven, Belgium) was the most used (14 studies, 21%), followed by MeshMixer (Autodesk, San Rafael, CA) (13 studies, 19%), Geomagic (3D System, Morrisville, NC) (10 studies, 15%), 3D Slicer (Slicer Developer Orientation, Boston, MA) (9 studies, 13%), Blender (Blender Foundation, Amsterdam, The Netherlands) (8 studies, 12%) and CURA (Geldermalsen, The Netherlands) (7 studies, 10%).
Sixty-seven different printer models were mentioned with five printing processes. FDM (Fused Deposition Modelling) technology was used in 26 articles (38%), followed by material jetting in 13 articles (19%), then binder jetting (11 articles, 16%). Stereolithography (SLA) (5 articles, 7%) and selective laser sintering (SLS) (4 articles, 6%) were the least used technologies. The most used printer (7 articles, 10%) was the Connex 500 (Stratasys, Rehovot, Israel) [27, 30, 32, 36, 45, 62, 65].
When the material used to fabricate the 3DPAM was specified (51 articles, 75%), plastic and its derivatives were used in 48 (71%) studies. The main materials used were PLA (polylactic acid) (n = 20, 29%), resins (n = 9, 13%) and ABS (acrylonitrile butadiene styrene) (7 articles, 10%). Twenty-three articles (34%) studied 3DPAM made of several materials, 36 (53%) articles featured a 3DPAM made of only one material and 9 (13%) did not specify the material.
Twenty-nine articles (43%) mentioned the printing scale, which ranged from 0.25:1 to 2:1 and averaged 1:1. A 1:1 scale was used in 25 articles (37%). Twenty-eight 3DPAMs (41%) were composed of several colours and 9 (13%) were coloured after printing [43, 46, 49, 54, 58, 59, 65, 69, 75].
Thirty-four articles (50%) mentioned a cost. Nine articles (13%) mentioned the cost of the 3D printer and the raw materials. Printers ranged in price from 302 USD to 65,000 USD. The cost per model, when specified, ranged from 1.25 USD to 2800 USD; these extremes corresponded to a bone specimen [47] and a high-fidelity retroperitoneal model [48]. Table 2 summarizes the model design data for each included study.
Table 2.
Summary of model design data
| Author (Year) | Anatomical human region | Precise anatomical part | Initial model | Modality of acquisition | Type of software | Type of printer | Type of material (number) | Printing scale | Colors (number) | Cost of printing |
|---|---|---|---|---|---|---|---|---|---|---|
| Ben Awadh et al. (2022) [23] | Thorax | Heart | Patient and database | CT | 3D Slicer, Blender, ideaMaker | FDM | NS | NS | N | NS |
| Cercenelli et al. (2022) [84] | Head | Dry skull, orbit | Cadaver | CT | D2P, Meshmixer | SLA | NS | NS | NS | NS |
| Chandrasekaran et al. (2022) [24] | Neck and thorax | Heart and neck | NS | NS | NS | NS | NS | N | NS | |
| Hammerton et al. (2022) [25] | Thorax | Heart | Public database | NS | NS | NS | NS | NS | N | NS |
| Harmon et al. (2022) [26] | Upper and lower-limbs, pelvis, thorax | Bones | Public database | CT | In Vesalius, Meshmixer, Blender, Cura, 3D Slicer | FDM | NS | NS | NS | 1.88 USD per model |
| Mogali et al. (2022) [27] | Thorax and neck | Full hearts, cross-section of the heart, coronary trees | Cadaver (plastinated human prosections) | CT | 3D slicer, Materialise Magics | MJ | Photopolymers and translucent elastomers resins (Vero Yellow), Tango Plus and VeroMagenta | 1 and 0.95 | Y | 6, 310, 319, 715 and 1,960 USD per model |
| Saleh et al. (2022) | Head | Temporal bone | Anonymized DICOM data | CT | Blender, MeshMixer, GrabCAD | MJ | Vero and Tango rigid and elastic polymers | 1.4 | Y | 1300 GBP |
| Tan et al. (2022) [28] | Head, upper-limb | Skull, brain, face, hand muscles, blood vessels, nerves and deep structures | Database from frozen cadaver | optical | Maya | MJ | Hard and flexible | 1 | Y | NS |
| Bertolini et al. (2021) [29] | Thorax | Heart | Patient | CT | Mimics, 3-Matic (Materialise), Preform 3.3 (Formlabs), ScanStudio 2.0, CloudCompare (GPL) | SLA | Rigid and elastic resin | NS | N | NS |
| Krishnasamy et al. (2021) [30] | Thorax | Heart | Patient | CT | BioModroid | MJ and BJ | Rigid polymer, plastic and wax | 1 | N | NS |
| Mahrous et al. (2021) [31] | Head | Teeth | NS | NS | SLA | NS | 1 | N | NS | |
| O’Brien et al. (2021) [32] | Thorax | Tracheobronchial tree | Patient | CT | 3-Matic Medical | MJ | Vero clear | NS | N | NS |
| Ruiz and Dhaher (2021) [33] | Lower-limb | Knee joint | Previous study.stl file | NS | GrabCAD Print, Materialise 3-Matic (Materialise), SolidWorks, (Dassault), Rhinoceros 3D (Robert McNeel & Associates) | MJ | Agilus30, Tango and Digital ABS | NS | Y | NS |
| Smillie et al. (2021) [34] | Abdomen | Hepatobiliary system with stomach and duodenum | Database | Contrast enhanced CT | Simpleware ScanIP, Meshmixer, Blender, GrabCAD | MJ | VeroMagenta, VeroYellow, VeroCyan | NS | Y | 1.343 GBP for raw plastic |
| Vatankhah et al. (2021) [35] | Head | Orbit | Patient | CT | NS | NS | NS | N | NS | |
| Weatherall et al. (2021) [36] | Thorax | Airway with bone pieces | 21-month-old patient and adult woman archived | CT | Avizo Lite, Geomagic studio 2014, Rhinoceros | BJ, MJ and SLA | White Version 3 resin, Flexible version 2 resin, VeroPure White, Tango Plus, Tango Black Polymers photopolymers, silicone elements | NS | Y | NS |
| Abdulcadir et al. (2020) [37] | Pelvis | Female pelvis with bone pieces | Patient | CT and MRI | Vitrea Vital Version 6.7.6 Canon, Kerne b40d, 3D Organ Segmentation (Vitrea), PrusaSlicer Version 2.0 (Slic3r), Blender | FDM | PLA | 1 and 0.5 | Y | NS |
| Chae et al. (2020) [38] | Head | Temporal bone | Cadaver | 3D scan and micro-CT | Meshlab, iNtellect Cranial Navigation system, blender, 3D printer | SLA | resin | 1 | N | 25 000 USD (optic scan), 200 USD (micro-CT), 3350 USD (SLA printer), 7 USD per model (resin) |
| Chedid et al. (2020) [39] | Abdomen | Liver segments | NS | CT | NS | NS | NS | Y | NS | |
| Chen et al. (2020) [40] | Abdomen | Gastro-colic trunk | Patients | CT angiography | Advantage Workstation GE Medical System, Geomagic studio 2014 modelling software | NS | Thermoplastic urethane and resin | 1 | Y | NS |
| Damon et al. (2020) [41] | Vertebral column | Lumbosacral vertebrae | Database | NS | 3D Slicer | FDM | ABS | NS | N | NS |
| Hojo et al. (2020) [42] | Pelvis | Pelvic lymph nodes with bone pieces | Patient | CT | Meshmixer version 3.5 | FDM | PLA | NS | Y | 15 USD |
| Javan et al. (2020) [43] | Head | Pterygopalatine fossa | Database | CT | Materialize InPrint, Autodesk 3D Studio Max 2018, Adobe Flash, iMaterialise.com | NS | PA and disk magnet | NS | AP | 200 USD |
| Low et al. (2020) [44] | Head | Frontal sinus | Database | CT | Mimics, 3-matic (Materialise) | BJ | Gypsum powder | NS | Y | 75.75 USD |
| Radzi et al. (2020) [45] | Thorax | Heart | Plastinated heart | CT | 3D slicer, Materialise magics', Objet studio' | MJ | NS | 1 | Y | 411 and 1639.7 Singapour dollar |
| Tanner et al. (2020) [46] | Head | Pterygopalatine fossa | Database | NS | FDM | PLA | NS | AP | NS | |
| Tripodi et al. (2020) [47] | Upper-limb | Bones pieces | NS | NS | FlashPrint MeshMixer | FDM | PLA | 0.25 | N | 635 USD (printer), 1.25 USD per model (filament) |
| Williams et al. (2020) [48] | Abdomen | Retroperitoneum with bone pieces | Patient | CT and MRI | Simpleware ScanIP, Meshmixer, Blender, GrabCAD | MJ | VeroMagenta, VeroYellow, VeroWhite | 1 | Y | 2223.02£ |
| Backhouse et al. (2019) [49] | Head | Orbit with bone pieces | Cadaver bone piece | 3D scan | DAVID Laserscanner Pro Edition v4 | NS | ABS | 0.85 | AP | 2 USD per model, 5000 to 8000 USD (printer) |
| Bartikian et al. (2019) [50] | Head | Bone pieces | Cadaver bone piece | CT | 3D Slicer, Craft-ware, Z-suite | FDM | PLA and ABS | NS | N | NS |
| Cai et al. (2019) [51] | Lower-limb | Knee joint | Patient | CT | InVesalius, Artec Studio, Rhino | SLS | PA EOS | 1 | N | 90 USD per set |
| Hojo et al. (2019) [52] | Pelvis | Lateral pelvic lymph nodes with bone pieces | Patient | CT | Osirix MD Viewer, MeshMixer | FDM | NS | 1 | Y | NS |
| Kanagasuntheram et al. (2019) [53] | Upper-limb | Midcarpal joint | Patient | CT | Leios2 (Evatronix SA), Rhinoceros version 5 | SLS | PA EOS and stainless steel with bronze | 1 | Y | 150 USD per model (material) |
| Low et al. (2019) | Head | Frontal sinus | Patient | CT | Mimics (Materialise) | BJ | NS | NS | Y | NS |
| Shen et al. (2019) [54] | Head | Skull | Patient | CT | Mimics 17.0, Geomagic Studio (13.0), Autodesk Mudbox, MeshMixer | FDM | PLA | NS | AP | 14 USD per model (material) and 500 USD (printer) |
| Skrzat et al. (2019) [55] | Head | Temporal bone | Cadaver bone piece | CT | In Vesalius, MeshLab | FDM | PLA and polyvinyl alcohol filament | 1 | N | NS |
| NSgidos Lozano et al (2019) | Head, thorax, small bones | Skull, small bones, vertebrae, thorax | NS | Laser scan | Geomagic | FDM | PLA | NS | N | NS |
| Yi et al. (2019) [57] | Head | Ventricular system with bone pieces | Patient | CT | PolyJet Studio 3DP | MJ | PLA and photocurable resin | NS | N | 30 USD (material), “very expensive” printer |
| Young et al. (2019) [85] | Human gestational specimens | Week 4 to week 21 | Fixed human embryonic and fetal specimens | CT | Mimics, version 17 (Materialise, Leuven, Belgium) 3D Coat, version 4.7.06 (Pilgway, Kiev, Ukraine), Stratasys 3D printing software PolyJet Studio, | BJ | gypsum-like plaster and binders, TangoPlus, VeroMagenta, yellow and cyan | 1 | Y | 30 AUD USD (week 9 print) to 215 AUD USD (week 21 print) |
| Zhang et al. (2019) [58] | Head, neck, thorax, abdomen, pelvis, reproductive organ, lower-limb | Uterus, vagina, bladder, urethra, skin, cerebellum, brain stem, bone pieces, eyeball, optic nerve, liver, kidney, lung, penis | Database | Camera and microscope | Amira | FDM and SLA | PLA and photosensitive resin | NS | AP | NS |
| Bannon et al. (2018) [59] | Head | Pterygopalatine fossa | Database | NS | 3D slicer, Meshmixer, Blender (open source), Slic3r Prusa Edition (G-code conversion) | FDM | PLA | 1 and 2 | AP | 0.13£ (Scotland) |
| Casciato et al. (2018) [60] | Lower-limb | Right leg | Cadaver | NS | Microsoft PowerPoint, Selva3D, CURA | FDM | PLA | NS | N | 304 USD (full cost) including 2.13 USD (filament) and printer |
| Garas et al. (2018) [61] | Trunk | Heart, shoulder, tight | NS | NS | NS | NS | NS | NS | Y | NS |
| Mogali et al. (2018) [62] | Upper-limb | Left upper-limb | Cadaver (plastinated) | CT | 3D Doctor (Able Software) | MJ | soft elastomers and rigid plastic | NS | Y | 390 USD |
| Smith et al. (2018) [64] | Thorax, musculo-skeletal | Respiratory system, musculo-skeletal system | Cadaver | CT | Materialize Mimics v15.0, MakerWare | FDM | ABS | From 0.4 to 1 | N | NS |
| Smith et al. (2018) [63] | Head and neck | Posterior triangle of the neck, laryngeal model, intrinsic muscles of the larynx and vocal folds, bone pieces | Database | NS | MeshMixer, CURA LulzBot | FDM | PLA and FilaFlex | NS | Y | 4077 USD (printer); 26 USD (FilaFlex), 40 USD (PLA). 144 to 387 USD per model |
| Suzuki et al. (2018) [65] | Head | Temporal bone, vestibulocochlear organ | Cadaver | CT | Synapse Vincent (Fujifilm) | MJ | Ultraviolet transparent curing resin | 0.66 | AP | NS |
| Ugidos Lozano et al. (2018) | Head and arm | Bone pieces | Cadaveric bone | CT and laser scan | 3D slicer, Artec studio 3D, Geomagic Design X 3D, CURA | FDM | PLA | 1 | N | NS |
| Wu et al. (2018) [66] | Spine, pelvis, upper and lower-limbs | Bone pieces | Patient | CT | Mimics 16.0 | NS | NS | NS | NS | 6 to 10.50 USD (spine and limbs) to 90 USD (pelvis) |
| Zhang et al. (2018) [67] | Head | Sinus-skull base | Patient | CT | Mimics, Cura version 15.02 | FDM | PLA | 1 | N | 3 USD |
| Bücking et al. (2017) [68] | Thorax and abdomen | Ribs, lung, liver | Database | NS | Mimics, Simpleware, Freesurfer, Seg3D, 3D Slicer, MeshMixer, Cura, InVesalius, ITK Snap, Osirix Lite, Horos, ImageJ | FDM | PLA | NS | N | 16£ (lung), 25£ (ribs), 10£ (liver) |
| Chen S. et al. (2017) [69] | Head | Skull | Cadaveric bone | CT | Mimics, Geomagic, 3ds Max, MeshMixer | FDM | PLA | NS | AP | 500 USD (printer) and 14 USD (material) |
| Favier et al. (2017) [70] | Head | Bone pieces | Cadavers | CT and micro-CT | Medical Image Segmentation Tool, Meshlab | MJ and BJ and SLS and FDM | Multicolor plaster, resin, PA, polycarbonate, composite powder | 1 | N | 155 USD (computer), 275 USD (Multicolor), 880 USD (resin), 298 USD (PA) |
| Javan et al. (2017) [71] | Head | Cranial nerve, brainstem, skull | Patient | NS | Materialise Mimics, Adobe Photoshop, Osirix Lite, Autodesk 3D Studio Max | NS | PA | 1.2 | N | 120 USD |
| Kavanagh et al. (2017) | Neck and thorax | Larynx and trachea | NS | CT | SolidWorks (Dassault Systèmes) | FDM | PLA, ABS, HIPS | NS | N | 1.75 USD to 4.66 USD per model |
| Legocki et al. (2017) [72] | Head | Skull, mandible and maxilla | Patient | CT | Osirix, MeshLab | FDM | PLA and thermoplastic | 1 | N | 1000 USD including 90.85 to 91.65 USD per model and 2 × 22.5 USD per hour and excluding 3598 USD for printer and software |
| Lozano et al. (2017) [73] | Head | Skull | Cadaver | 3D scan | Geomagic design 3D, Repetier-Host, CURA (Ultimaker trading house) | FDM | PLA | 1 | N | “Low cost” |
| Fasel et al. (2016) [74] | Head, neck, thorax, abdomen and pelvis | Isthmus of the thyroid, diaphragm and aorta | Cadaver | CT | Osirix, Mimics 14.12 | BJ | NS | 1 | N | NS |
| Javan et al. (2016) [75] | Head, thorax, abdomen and pelvis | Liver, lung, prostate, coronary arteries, circle of Willis | Database | MRI | Autodesk 3D Studio Max, Osirix lite, Slicer | NS | PA | NS | AP | 40 to 100 USD per model |
| Kong et al. (2016) [76] | Abdomen | Liver | Cadaver | CT | Mimics, Geomagic, Zedit 3.21 (3D system) | Ink-jet 3DP | composite powder, curing agent, transparent jelly wax | NS | Y | 600 USD per model |
| Kong et al. (2016) [77] | Abdomen | Liver | Patient | CT | 3DV system, Zedit 3.21 | Ink-jet 3DP | composite powder, curing agent | NS | Y | NS |
| Lim et al. (2016) [16] | Thorax | Heart | Cadaver (prosection) | CT | Avizo Lite, 3D coat version | BJ | NS | 1 | Y | NS |
| O’Reilly et al. (2016) [78] | Lower-limb | Bone, tendon, muscles | Database | NS | MeshLab, version 1.3.3, Tinkercad (Autodesk Inc., San Francisco, CA), Z EditTM Pro, (3D Systems Corp., Rock Hill, SC) | BJ | Composite powder and silicone | 0.5 and 0.33 | Y | NS |
| Shah et al. (2016) [79] | Head | Sphenoid sinus | Patient | MRI and CT | NC (3-D printing system) | NS | Thermoplastic | NS | N | NS |
| Adams et al. (2015) | Head | Orbit with bone pieces | Cadaver | Laser scan | Artec studio Version9.0, 3D Coat (PILGWAY, Ukraine), Geomagic (3D systems, USA) | BJ | Composite powder and powdered plastic | 1 | Y | NS |
| Cohen et al. (2015) [81] | Head | Temporal bone | Patient | CT | ITK-SNAP | FDM | ABS | NS | Y | 27.61 to 42.02 USD |
| Hochman et al. (2015) [82] | Head | Temporal bone | Cadaver | Micro-CT | Mimics 14.0, Geomagic | NS | remnant material, binding agent | NS | Y | NS |
| McMenamin et al. (2014) [83] | Upper-limb | Wrist and hand | Cadaver (prosection) | CT | Avizo Lite, 3D coat version | BJ | NS | 1 | Y | 65 000 USD (printer), 8000 USD (software), 400 USD per hour (CT), 5000 USD (computer), 0.55 USD per cc (consumables) and 40,000 USD (technical staff) |
Abbreviations: AP A posteriori, BJ Binder jetting, ABS Acrylonitrile butadiene styrene, CT Computed tomography, FDM Fused deposition modelling, GBP Great Britain Pound, HIPS High impact polystyrene, micro-CT Micro-computed tomography, MJ Material jetting, MRI Magnetic Resonance Imaging, N No, NS Not specified, PA Polyamide, PLA Polylactic acid, SLA Stereolithography, USD United States dollars, Y Yes
Morphological evaluation of 3D models
Thirty-seven studies (54%) compared the 3DAPM to a reference model. Among these studies, the most common comparator was a reference anatomical model, which was used in 14 articles (38%), a plastinated specimen in 6 articles (16%), virtual reality in 6 articles (16%), CT-scan imaging in 5 articles (14%), another 3DPAM in 3 articles (8%), a serious game in 1 article (3%), radiographs in 1 article (3%), a business model in 1 article (3%), and augmented reality in 1 article (3%). Thirty-four (50%) studies rated the 3DPAM. Fifteen (48%) studies specified the raters’ experience (Table 3). The 3DPAM was evaluated by surgeons or attending physicians in 7 studies (47%), anatomy experts in 6 studies (40%), students in 3 studies (20%), teachers (without specifying the discipline) in 3 studies (20%) and another rater in 1 article (7%). The average number of raters was 14 (minimum 2, maximum 30). The morphology of the 3DPAM was evaluated qualitatively in 33 studies (49%) and quantitatively in 10 studies (15%). Among the 33 studies using a qualitative assessment, 16 studies used a purely descriptive assessment (48%), 9 studies used tests/scores/surveys (27%) and 8 studies used a Likert scale (24%). Table 3 summarizes the morphological evaluation of the models in each included study.
Table 3.
Summary of how the morphology of the 3D models was evaluated
| Author (Year) | Model used for comparison | Qualification of evaluator (number) | Type of evaluation |
|---|---|---|---|
| Ben Awadh et al. (2022) [23] | 2D images | NS | NS |
| Cercenelli et al. (2022) [84] | 3DPAM and VR versus 2D images | NS | NS |
| Chandrasekaran et al. (2022) [24] | Plastinated | NS | NS |
| Hammerton et al. (2022) [25] | NS | Anatomy senior (2) and educators (11) | Qualitative |
| Mogali et al. (2022) [27] | Plastinated | NS | NS |
| Saleh et al. (2022) | NS | Authors (5) | Qualitative |
| Tan et al. (2022) [28] | Cadaver and digital | Anatomist (5) and surgeons (3) | Qualitative and quantitative |
| Bertolini et al. (2021) [29] | CT images | Authors (3) | Qualitative and quantitative |
| Krishnasamy et al. (2021) [30] | NS | Surgeons, cardiologists, radiologists, surgical registrars (30) | Survey |
| Mahrous et al. (2021) [31] | Natural tooth, 3D AR and VR | NS | NS |
| O’Brien et al. (2021) [32] | 2D images | NS | NS |
| Ruiz et al. (2021) [33] | NS | Authors (2) | Quantitative |
| Weatherall et al. (2021) [36] | NS | Authors (6) | Qualitative |
| Abducaldir et al. (2020) | 2D diagrams | Expert researchers (30) | Semi-structure interview |
| Chae et al. (2020) [38] | Cadaver (temporal bone), optic scanner and micro-CT images | Authors (8) | Quantitative |
| Chedid et al. (2020) [39] | 2D images | NS | NS |
| Chen et al. (2020) [40] | 2D images | NS | NS |
| Damon et al. (2020) [41] | Same model with and without initial rotation | NS | NS |
| Hojo et al. (2020) [6] | 3D VR and CT images | Surgeons (30) | Likert and Adachi classification |
| Javan et al. (2020) [43] | Serious gaming and VR | NS | NS |
| Low et al. (2020) [44] | NS | Authors (4) | Qualitative |
| Radzi et al. (2020) [45] | Plastinated | NS | NS |
| Tanner et al. (2020) [46] | Cadaver (half-skull) | NS | NS |
| Bartikian et al. (2019) [50] | Same model with different printer | Authors (4) | Qualitative |
| Cai et al. (2019) [51] | Cadaver (knee skeleton) | Experts in human anatomy (2) | Qualitative |
| Low et al. (2019) | 2D images | NS | NS |
| Shen et al. (2019) [54] | Cadaver (skull) (other study) | NS | NS |
| Skrzat et al. (2019) [55] | Cadaver | Authors (4) | Qualitative |
| Ugidos Lozano et al. (2019) [56] | 2D images and cadaver (bones) | NS | NS |
| Yi et al. (2019) [57] | NS | Professor of anatomy (2) and professor of surgery (2) | Likert |
| Zhang et al. (2019) [58] | NS | Experienced teachers (5) | Scores |
| Casciato et al. (2018) [60] | NS | Authors (3) | Quantitative |
| Garas et al. (2018) [61] | Cadaver and plastinated | NS | NS |
| Mogali et al. (2018) [62] | Plastinated | Students (15) | Qualitative |
| Smith et al. (2018) [64] | Cadaver (teacher) and 2D images (students) | Teachers (6) | Survey |
| Smith et al. (2018) [64] | NS | Authors (2) | Qualitative |
| Suzuki et al. (2018) [65] | NS | Authors (9) | Qualitative |
| Ugidos Lozano et al. (2018) | NS | Authors (6) | Qualitative |
| Wu et al. (2018) [66] | Radiographics | NS | NS |
| Zhang et al. (2018) [67] | CT images | Senior doctors (9) | Survey and Likert |
| Chen et al. (2017) [69] | 2D images and cadaver | Students (26) | Likert |
| Favier et al. (2017) [70] | Cadaver | Authors (9) | Quantitative |
| Javan et al. (2017) [71] | NS | Authors (3) | Qualitative and descriptive |
| Kavanagh et al. (2017) | NS | Authors (6) | Quantitative and Likert |
| Legocki et al. (2017) [72] | Commercial model | Authors (3) | Quantitative and qualitative |
| Fasel et al. (2016) [74] | CT images and cadaver (dissection) | Students (12) | Quantitative |
| Khong et al. (2016) | 3 different 3DPAM and 2D images | Anatomy teachers (4) and consultants of surgery (2) | Likert |
| Khong et al. (2016) | 3D VR and 2D images | Anatomy teachers (4) and consultants of surgery (2) | Likert |
| O’Reilly et al. (2016) [78] | Cadaver | NS | NS |
| Shah et al. (2016) [79] | 2D images | NS | NS |
| Adams et al. (2015) [80] | NS | Authors (6) | Satisfaction |
| Cohen et al. (2015) [81] | NS | Authors (2) | Qualitative |
| Hochman et al. (2015) [82] | 3D VR | NS | NS |
| McMenamin et al. (2014) [83] | Plastinated | Authors (4) | Descriptive |
Abbreviations: 3DPAM 3D printed anatomical model, AR Augmented reality, CT Computed tomography, NS Not specified, VR Virtual reality
Pedagogical performance of 3D models
Thirty-three (48%) articles investigated and compared the pedagogical performance of 3DPAMs in students. Among these studies, 23 (70%) articles evaluated student satisfaction, 17 (51%) used a Likert scale and 6 (18%) used other methods. Twenty-two articles (67%) evaluated student learning through a knowledge check, 10 (30%) of which administered pre- and/or post-tests. Eleven studies (33%) used multiple-choice questions and quizzes to assess students' knowledge and 5 (15%) used image labelling/anatomical identification. An average of 76 students participated per study (minimum 8, maximum 319). Twenty-four studies (72%) had comparison groups, 20 (60%) of which applied randomization. Conversely, 1 study (3%) randomized the anatomical models to assign them to 10 different students. On average, 2.6 groups were compared (minimum 2, maximum 10). Twenty-three studies (70%) involved medical students, of which 14 (42%) included first-year students. Six (18%) studies involved residents, 4 (12%) dental students, and 3 (9%) science students. Six studies (18%) implemented and evaluated self-directing learning with the 3DPAM. Table 4 summarizes how the pedagogical performance of 3DPAMs was evaluated in each included study.
Table 4.
Summary of how the pedagogical performance of 3D models was evaluated
| Author (Year) | Knowledge assessment | Knowledge assessment method | Number of student / Number of comparison groups | Randomization | Type of education/student | Satisfaction evaluation | Satisfaction assessment method |
|---|---|---|---|---|---|---|---|
| Ben Awadh et al. (2022) [23] | Y | Pre and posttest (cross-section images labelling questionnaire and mental rotation test) | 319 / 2 | N | 1st year medical students | Y | Likert |
| Cercenelli et al. (2022) [84] | Y | MCQ and practical task | 62/2 | Y | second-year medical students | Y | Likert |
| Chandrasekaran et al. (2022) [24] | N | NS | 96/2 | Y | 1st year medical students | Y | Likert |
| Hammerton et al. (2022) [25] | N | NS | 84 / x | N | 1st year medical students | Y | Likert (semi-structured interview) |
| Harmon D.J. et al. (2022) [26] | N | NS | 80 / x | N | 2nd year doctors, 1st year medical and dental students | Y | Qualitative |
| Mogali et al. (2022) [27] | Y | Qualtrics software pre-test (MCQ) | 63 / 2 | Y | 1st year medical students | N | |
| Mahrous et al. (2021) [31] | N | NS | 70 / x | N | Dental students | Y | Survey |
| O’Brien et al. (2021) [32] | Y | MCQ (structure identification on cross-sectional images) immediate and delayed test | 31 / 2 | Y | 1st year medical students | N | |
| Vatankhah et al. (2021) [35] | Y | Pre and post-test MCQ | 13 / 2 | Y | 1st and 2nd year residents | N | |
| Chedid et al. (2020) [39] | Y | Test questions | 116 / 2 | Y | Gastro-enterology, radiology and general surgery departments | N | |
| Chen et al. (2020) [40] | Y | Pre and post-test | 47 / 2 | Y | Residents | Y | Questionnaire |
| Radzi et al. (2020) [45] | N | NS | 58 / x | N | 1st year medical students | Y | Likert |
| Tanner et al. (2020) [46] | Y | Quiz with pre and post test | 123 / 2 | Y | Junior and sophomores in medical education, premedecine undergraduate, graduate students of Master of Biomedical Science and 1st year medical students, dental and physicians’ students | Y | NS |
| Tripodi et al. (2020) [47] | N | NS | 111 / x | N | 1st year osteopathy students | Y | Likert and long answer survey |
| Backhouse et al. (2019) [49] | N | NS | 81 / x | N | 1st year students in ocular anatomy unit bachelor or vision sciences and master of optometry | Y | Likert |
| Cai et al. (2019) [51] | Y | MCQ | 35 / 2 | Y | 1st year medical students | N | |
| Hojo et al. (2019) [52] | Y | Short and long tests | 102 / 2 | Y | Medical students, residents and one colorectal surgeon | Y | Likert |
| Low et al. (2019) | Y | Pre and post-tests | 41 / 2 | Y | Residents (radiology and ENT) | N | |
| Ugidos Lozano et al. (2019) [56] | N | NS | 280 / x | N | Physiotherapy, medicine, nursing, occupational therapy and dentistry students of Health Sciences | Y | Likert |
| Yi et al. (2019) [57] | Y | Pre and post-tests (theorical and practical questions) | 60 / 3 | Y | 2nd year medical students | Y | Likert |
| Zhang et al. (2019) [58] | Y | Reports | 30 / 10 | Y | 5 year medical students | Y | Likert |
| Garas et al. (2018) [61] | Y | 9 questions test (identify pinned structures) | 23 / 2 | N | 1st year health sciences and 3rd year Human Biology Preclinical students | Y | Likert |
| Mogali Et al. (2018) | N | NS | 15 / x | N | 2nd year medical students | Y | Likert |
| Smith et al. (2018) [63] | Y | Test questions | 127 / 2 | Y | 1st year medical students | Y | Key themes from focus group |
| Wu et al. (2018) [66] | Y | Questions | 90 / 2 | Y | Medical students completed anatomy courses | Y | Likert |
| Chen et al. (2017) [69] | Y | MCQ and labelled structures to be recognized | 79 / 3 | Y | 3rd year medical students | Y | Likert |
| Fasel et al. (2016) [74] | N | NS | 12 / x | N | Undergraduate medical students | Y | Scale 1 to 6 |
| Kong et al. (2016) [77] | Y | Quiz | 92 / 4 | Y | 1st year medical students | N | |
| Kong et al. (2016) [77] | Y | Quiz | 61 / 3 | Y | 1st year medical students | N | |
| Lim et al. (2016) [16] | Y | MCQ and labelled structures to be recognized pre and post-tests | 53 / 3 | Y | 1st year medical students | N | |
| O’Reilly et al. (2016) [78] | Y | Quizdom System pre and post-test | 22 / 2 | Y | Graduate entry medicine year 1 class | Y | Likert |
| Shah et al. (2016) [79] | Y | Labelled structures to be recognized | 8 / 2 | N | Neurosurgery residents (junior and senior) | N | |
| Hochman et al. (2015) [82] | N | NS | 10 / 10 | Y | Residents | Y | Likert |
Abbreviations: ENT Ear nose throat, MCQ Multiple choice question, N No, NS Not specified, Y Yes
Advantages and disadvantages
The main advantages reported by the authors using 3DPAM as a pedagogical tool for teaching normal human anatomy were the visual and haptic characteristics, including authenticity [55, 67], precision [44, 50, 72, 85], variability of consistencies [34, 45, 48, 64], colours and transparency [28, 45], solidness [24, 56, 73], effectiveness for education [16, 32, 35, 39, 52, 57, 63, 69, 79], cost [27, 41, 44, 45, 48, 51, 60, 64, 80, 81, 83], reproducibility [80], possibility of improvement or personalization [28, 30, 36, 45, 48, 51, 53, 59, 61, 67, 80], possibility of manipulation by the students [30, 49], time savings for teaching [61, 80], ease of storage [61], possibility of integrating functional anatomy or creating a specific design [51, 53, 67], rapid design for bone models [81], possibility of co-creation and taking the model home [49, 60, 71], improvement in mental rotation ability [23] and knowledge retention [32], and positive effect on educators [25, 63] as well as student satisfaction [25, 45, 46, 52, 52, 57, 63, 66, 69, 84].
The main drawbacks were related to design: stiffness [80], consistency [28, 62], lack of detail or transparency [28, 30, 34, 45, 48, 62, 64, 81], overly bright colours [45], and fragility [71]. Other drawbacks were the loss of information [30, 76], long time needed for image segmentation [36, 52, 57, 58, 74], printing time [57, 63, 66, 67], lack of anatomical variability [25] and the high cost [48].
Discussion
This systematic review summarizes 68 articles published over 9 years, highlighting the scientific community’s interest in 3DPAM as a pedagogical tool for teaching normal human anatomy. Every anatomical region has been studied and printed in 3D. Among these articles, 37 compared the 3DPAM to another model and 33 evaluated the pedagogical relevance of the 3DPAM for students.
Given the differences in the design of studies on 3D printing in anatomy, we did not feel it was appropriate to carry out a meta-analysis. A meta-analysis published in 2020 focused mainly on post-training tests of anatomical knowledge, without analysing the technical and technological aspects of the design and manufacture of 3DPAMs [10].
Model design data
The cephalic region was the most studied, probably because its anatomical complexity makes it difficult for students to picture this anatomical region in 3D space, compared to the limbs or trunk. CT scan was by far the most used image acquisition modality. This modality is widely available, especially in healthcare facilities, but its spatial resolution is limited, and its soft-tissue contrast is low. These limitations make CT scan unsuitable for segmentation and modelling of the nervous system for example. On the other hand, CT scan was preferred for the segmentation/modelling of bone tissue; the bone/soft tissue contrast facilitates these steps before 3D printing of an anatomical model. Micro-CT, on the other hand, was cited as the reference technology in terms of spatial resolution for the acquisition of bone tissue images [70]. An optical scanner or MRI can also be used for image acquisition. Higher resolution prevents the smoothing of bone surfaces and preserves the subtleties of the anatomy [59]. The choice of models also influences the spatial resolution; for example, plastinated models have lower resolution [45]. A graphic designer was needed when creating highly customized 3D models, which increases the cost (25 to 150 USD per hour of work) [43]. Obtaining a good quality.STL file was not sufficient to produce a good quality anatomical model. The printing parameters such as the orientation of the anatomical model on the printing plate must be defined [29]. Some authors suggested that advanced printing technologies such as SLS should be used whenever possible to improve the 3DPAM’s accuracy [38]. The help of a professional was required to make the 3DPAM; the most requested professionals were an engineer [72], radiologist, [75] graphic designer, [43] and anatomist [25, 28, 51, 57, 76, 77].
Segmentation and modelling software are important factors for obtaining an accurate anatomical model, but the price of these software packages and their complexity hinder their use. Some studies compared the use of different software packages and printing technologies, highlighting the advantages and disadvantages of each [68]. In addition to modelling software, printing software is required that is compatible with the chosen printer; some authors preferred to use online 3D printing [75]. If enough 3D objects will be printed, the investment may be financially profitable [72].
Plastic was by far the most used material. It is the material of choice for 3DPAM due to its large range of textures and colours. Several authors praised its high strength compared to traditional cadaveric or plastinated models [24, 56, 73]. Some plastics even have flexural or tensile properties. For example, the Filaflex used with FDM technology can stretch up to 700%. For some authors, it is the material of choice for reproducing muscles, tendons and ligaments [63]. On the other hand, two studies raised questions about the direction of the fibres as printed. Indeed, the direction of the muscle fibres is critical when modelling a muscle, along with its insertions, innervation and function [33].
Surprisingly, few studies mentioned the printing scale. Since many consider a 1:1 scale as standard, the authors may have decided not to mention it. The possibility of enlargement has not been explored much despite its benefit for directed teaching in large groups, especially given the increasing number of students per class where the actual size of the model is an important element. Of course, a full-size scale makes it easier to locate the various anatomical elements and to transpose it to patients, which probably explains why this scale is often used.
Among the multiple printers available on the market, those that provide high-definition printing in colour and in several materials – thus several textures – using PolyJet technology (material jetting or binder jetting) cost between 20,000 and 250,000 + dollars (https://www.aniwaa.com/). This high cost likely restricts the diffusion of 3DPAMs in medical schools. In addition to the price of buying a printer, the materials needed for material jetting cost more than those used for SLA or FDM printers [68]. The price of SLA or FDM printers is also more manageable, ranging from 576 to 4999 € in the articles listed in this review. According to Tripodi and colleagues, bone parts could be printed for 1.25 USD each [47]. Eleven studies concluded that 3D printing costs less than plastinated or commercial models [24, 27, 41, 44, 45, 48, 51, 60, 63, 80, 81, 83]. Furthermore, these commercial models are intended for patient information and do not have sufficient detail to be used for teaching anatomy [80]. These commercial models were considered inferior to 3DPAMs [44]. It is important to note that – in addition to the printing technology used – the final cost is also proportional to the scale and thus the final size of the 3DPAM [48]. For these reasons, the preferred scale was full size [37].
Morphological evaluation of 3D models
Only one study compared a 3DPAM to a commercially available anatomical model [72]. Cadaveric specimens were the most used comparator for 3DPAM. Despite its drawbacks, the cadaveric model remains a valuable tool for teaching anatomy. A distinction needs to be made between cadaveric dissection, prosections and dry bones. Two studies found that 3DPAMs were significantly more effective than plastinated prosections based on learning tests [16, 27]. A single study compared one hour of learning using a 3DPAM (lower limb) with one hour of dissection on the same anatomical area [78]. There was no significant difference between the two teaching methods. It is likely that few studies have been done on this topic because this comparison is difficult to set up. Dissection by students is a time-consuming task to prepare for. Several dozens of hours of dissection are sometimes necessary, depending on the dissection subjects. A third comparison can be made with dry bones. The studies by Cai and Smith found significantly better test results for the groups who used 3DPAM [51, 63]. Chen and colleagues specified that students who used the 3D model were better at recognizing structures (skull) but that there was no difference in MCQ results [69]. Finally, Tanner and colleagues demonstrated better post-test results for the group using a 3DPAM of the pterygopalatine fossa [46]. This literature review identified other new teaching tools. Among the most common were augmented reality, virtual reality, and serious gaming [43]. According to Mahrous and colleagues, the anatomical model preference depends on the number of video game hours played by the student [31]. On the other hand, the main pitfall of new tools in anatomy education is haptic feedback, especially for virtual-only tools [48].
Pedagogical performance of 3D models
A knowledge pre-test was used in most studies evaluating new 3DPAMs. These pre-tests help to avoid assessment bias. Some authors excluded all students who scored above average on the pre-test before conducting their experimental study [40]. Among the assessment biases, Garas and colleagues cited the colouring of the models but also the choice of volunteers among the student classes [61]. Staining makes anatomical structures easier to identify. Chen and colleagues imposed strict experimental conditions, with no initial intergroup differences and as much blinding as possible [69]. Lim and colleagues suggest avoiding assessment bias by having the post-test assessment prepared by a third person [16]. Some of the studies used Likert scales to assess the 3DPAM’s appropriateness. This tool is suitable for evaluating satisfaction but nevertheless has important biases that one must be aware of [86].
The educational relevance of 3DPAMs was evaluated mostly in medical students, including first-year students in 14 of the 33 studies identified. In their pilot study, Wilk and colleagues reported that medical students felt 3D printing should be incorporated into their learning of anatomy [87]. Eighty-seven percent of students surveyed in the Cercenelli study felt that their second year was the best time to use 3DPAMs [84]. Results from Tanner and colleagues also showed that students were better if they had never studied the area [46]. These data suggest that the first years of medical school are the best time to incorporate 3DPAMs into the teaching of anatomy. Ye's meta-analysis corroborates this idea [18]. Of the 27 articles included in their study, there was a significant difference in test results in favour of 3DPAMs versus conventional models for medical students but not for residents.
3DPAMs were effective as pedagogical tools in terms of achievement, [16, 35, 39, 52, 57, 63, 69, 79] long-term knowledge retention [32] and student satisfaction [25, 45, 46, 52, 57, 63, 66, 69, 84]. Expert panels have also been found these models useful [37, 42, 49, 81, 82] and two studies highlighted teacher satisfaction with 3DPAMs [25, 63]. Among all resources, Backhouse and colleagues judged 3D printing to be the best alternative to conventional anatomical models [49]. In their first meta-analysis, Ye and colleagues affirm that the post-test results of students who received instruction incorporating 3DPAMs were better than those who received instruction in 2D or on a cadaver [10]. However, they did not differentiate the 3DPAMs by their complexity but simply as heart, nervous system and abdomen. In seven studies, 3DPAMs were not superior to other models based on the knowledge tests given to students [32, 66, 69, 77, 78, 84]. In their meta-analysis, Salazar and colleagues conclude that the use of 3DPAMs specifically improves the understanding of complex anatomical structures [17]. This concept is consistent with a letter to the editor by Chytas [88]. Certain anatomical areas that are considered less complex would not require the use of 3DPAMs, while more complex anatomical areas such as the neck or nervous system would be a reasonable choices for 3DPAMs. This notion probably explains why some 3DPAMs have not been judged superior to conventional models, especially since the model's effectiveness seems to be better when the student has no knowledge in the field. Consequently, a simple model, presented to students who already have some knowledge of the subject (advanced medical students or residents), would be useless for improving student results.
Advantages and disadvantages
Of all the educational benefits listed, 11 studies highlighted the visual or tactile qualities of their models, [27, 34, 44, 45, 48, 50, 55, 63, 67, 72, 85] while 3 studies emphasized the strength and durability (33, 50–52, 63,79,85,86). Other advantages were that the students could manipulate the structures, the teacher could save time, they were easier to preserve than a cadaver, the design could be completed in less than 24 h, it could be used as a home study tool and it could be used to teach large groups [30, 49, 60, 61, 80, 81]. The 3D printing of multiple copies for teaching anatomy in large groups, make the 3D printing of models more cost-effective [26]. Using 3DPAMs increased mental rotation ability [23], and improved interpretation of cross-sectional imaging [23, 32]. Two studies found that students exposed to 3DPAMs were more attracted to surgery [40, 74]. Metal connectors can be incorporated to produce the motion needed to study functional anatomy [51, 53] or to print the model with a page-turning design [67].
3D printing made it possible to create adjustable anatomical models by improving certain aspects during the modelling stage, [48, 80] creating a suitable base, [59] merging multiple models, [36] using transparency, (49) colour, [45] or making certain internal structures visible [30]. Tripodi and colleagues used modelling clay to supplement their 3D printed bone models, highlighting the value of co-creating the model as a teaching tool [47]. In 9 studies, colour was applied after printing, [43, 46, 49, 54, 58, 59, 65, 69, 75] but only once by the students [49]. Unfortunately, that study did not assess the pedagogical quality of the model or the teaching sequence. This is something to take into consideration in the context of anatomy education, since the benefits of hybrid learning and co-creation [89] are well known. In response to growing promotions, self-learning has been implemented several times to evaluate models [24, 26, 27, 32, 46, 69, 82].
One study considered the colours of the plastic materials too bright, [45] another that the model was too fragile, [71] and two others pointed out the lack of anatomical variability when a single model was designed [25, 45]. Seven studies concluded that the anatomical detail was insufficient in their 3DPAM [28, 34, 45, 48, 62, 63, 81].
The segmentation and modelling time was considered very long and the cost very high (about 2000 USD) for more elaborate anatomical models of large and complex regions such as the retroperitoneum or the cervical region [27, 48]. In their study, Hojo and colleagues specified that it took 40 h to create their pelvic anatomical model [42]. The longest segmentation time was 380 h in the study by Weatherall and colleagues where several models were merged to make a finished paediatric airway model [36]. Segmentation and printing time was considered a drawback in nine studies [36, 42, 57, 58, 74]. However, 12 studies criticized the physical properties of their model, particularly its consistency, [28, 62] lack of transparency, [30] fragility and unicolor nature, [71] absence of soft tissues [66] or lack of detail [28, 34, 45, 48, 62, 63, 81]. These drawbacks could likely have been overcome with more segmentation or modelling time. Loss of acquisition-related information was an issue for three teams [30, 74, 77]. Patient data was used in which the iodinated contrast agent did not provide an optimal view of the blood vessels due to dose limitations [74]. The injected cadaveric model appears to be an ideal approach, freeing itself from the “as low as reasonably achievable” principle and limitations in the dose of contrast agent injected.
Limitations
Unfortunately, many articles did not mention certain key features of their 3DPAM. Less than half of the articles specified whether their 3DPAM was coloured or not. The printing scale was not consistently reported (43% of articles) and only 34% of articles mentioned the use of multiple materials. These printing parameters are crucial because they influence the 3DPAM’s pedagogical properties. Most of the articles did not provide enough information about the complexity of obtaining the 3DPAM (design time, qualifications of people, cost of software, cost of printing, etc.). This information is essential and must be taken into consideration before thinking about starting a project to develop a new 3DPAM.
Conclusions
This systematic review demonstrates that the design and 3D printing of a normal anatomical model is feasible at a low cost, particularly by using FDM or SLA printers and inexpensive single-color plastic materials. These basic models can nevertheless be improved by adding colour, or adding structures made of various materials. More realistic models – printed with several materials of different colours and textures to reproduce the haptic qualities of the reference cadaveric model as closely as possible – require access to more expensive 3D printing technologies and substantially longer design time. This would greatly increase the overall cost. No matter the chosen printing process, selecting the appropriate imaging modality is key to successful 3DPAMs. The higher the spatial resolution, the more the model will match reality and be usable at advanced levels of study. From a pedagogical point of view, 3DPAMs are effective tools for teaching anatomy, as evidenced by knowledge tests carried out with students and by the students’ satisfaction. The pedagogical effectiveness of 3DPAMs seems to be best when they reproduce complex anatomical areas, and they are used by students early in their medical studies.
Acknowledgements
The authors wish to thank the Laboratoire d’Anatomie de l’UFR Santé de Besançon for making this study possible. The authors acknowledge the editorial assistance provided by Joanne Archambault, PhD.
Authors’ contributions
Eléonore Brumpt: conceptualization, methodology, formal analysis, investigation, data curation, writing original draft. Eugénie Bertin: formal analysis, investigation, resources. Laurent Tatu: conceptualization, validation, investigation, formal analysis, supervision. Aurélien Louvrier: conceptualization, methodology, formal analysis, investigation, writing original draft, supervision. All authors read and approved the final manuscript.
Authors’ information
- ELEONORE BRUMPT MD, MSc is a medical doctor (radiologist), anatomy teacher and a second-year PhD student in the Doctoral School Environment-Health at the Bourgogne Franche-Comté University.
- EUGENIE BERTIN MD, MSc is a medical doctor (maxillofacial surgery) and anatomy teacher assistant at the Bourgogne Franche-Comté University.
- LAURENT TATU MD, PhD is a medical professor (neurology) and the Head of the Besançon Medical Faculty Anatomy Laboratory at the Bourgogne Franche-Comté University.
- AURELIEN LOUVRIER MD, PhD is a medical doctor (maxillofacial surgery) and the Head of the Besançon Medical 3D Printing Laboratory at the Bourgogne Franche-Comté University.
Funding
This project has been performed thanks to the RITM-BFC program (contract ANR-17-NCUN-0003).
Availability of data and materials
The datasets generated and/or analysed for the current study are not publicly available due to the language barrier but are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Drake RL, Lowrie DJ, Prewitt CM. Survey of gross anatomy, microscopic anatomy, neuroscience, and embryology courses in medical school curricula in the United States. Anat Rec. 2002;269(2):118–122. doi: 10.1002/ar.10079. [DOI] [PubMed] [Google Scholar]
- 2.Ghosh SK. Cadaveric dissection as an educational tool for anatomical sciences in the 21st century: Dissection as an Educational Tool. Anat Sci Educ. 2017;10(3):286–299. doi: 10.1002/ase.1649. [DOI] [PubMed] [Google Scholar]
- 3.Sugand K, Abrahams P, Khurana A. The anatomy of anatomy: A review for its modernization. Anat Sci Educ. 2010;NA-NA. [DOI] [PubMed]
- 4.Estai M, Bunt S. Best teaching practices in anatomy education: A critical review. Ann Anat - Anat Anz. 2016;208:151–157. doi: 10.1016/j.aanat.2016.02.010. [DOI] [PubMed] [Google Scholar]
- 5.Aziz MA, Mckenzie JC, Wilson JS, Cowie RJ, Ayeni SA, Dunn BK. The human cadaver in the age of biomedical informatics. Anat Rec. 2002;269(1):20–32. doi: 10.1002/ar.10046. [DOI] [PubMed] [Google Scholar]
- 6.Papa V, Vaccarezza M. Teaching Anatomy in the XXI Century: New Aspects and Pitfalls. Sci World J. 2013;2013:1–5. doi: 10.1155/2013/310348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yiasemidou M, Gkaragkani E, Glassman D, Biyani CS. Cadaveric simulation: a review of reviews. Ir J Med Sci. 2018;187(3):827–833. doi: 10.1007/s11845-017-1704-y. [DOI] [PubMed] [Google Scholar]
- 8.Santos VA, Barreira MP, Saad KR. Technological resources for teaching and learning about human anatomy in the medical course: Systematic review of literature. Anat Sci Educ. 2022;15(2):403–419. doi: 10.1002/ase.2142. [DOI] [PubMed] [Google Scholar]
- 9.Erolin C. Interactive 3D Digital Models for Anatomy and Medical Education. In: Rea PM, editor. Biomedical Visualisation [Internet]. Cham: Springer International Publishing; 2019 [retrieved 3 March 2023]. p. 1‑16. (Advances in Experimental Medicine and Biology; vol. 1138). Available on: http://link.springer.com/10.1007/978-3-030-14227-8_1 [DOI] [PubMed]
- 10.Ye Z, Dun A, Jiang H, Nie C, Zhao S, Wang T, et al. The role of 3D printed models in the teaching of human anatomy: a systematic review and meta-analysis. BMC Med Educ. 2020;20(1):335. doi: 10.1186/s12909-020-02242-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Witze A. NASA to send 3D printer into space. Nature. 2014;513(7517):156–156. doi: 10.1038/513156a. [DOI] [PubMed] [Google Scholar]
- 12.Snyder TJ, Andrews M, Weislogel M, Moeck P, Stone-Sundberg J, Birkes D, et al. 3D Systems’ Technology Overview and New Applications in Manufacturing, Engineering, Science, and Education. 3D Print Addit Manuf. 2014;1(3):169‑76. [DOI] [PMC free article] [PubMed]
- 13.Valverde I. Three-dimensional printed cardiac models: applications in the field of medical education, cardiovascular surgery, and structural heart interventions. Rev Esp Cardiol Engl Ed. 2017;70(4):282–291. doi: 10.1016/j.recesp.2016.09.043. [DOI] [PubMed] [Google Scholar]
- 14.Chytas D, Johnson EO, Piagkou M, Tsakotos G, Babis GC, Nikolaou VS, et al. Three-dimensional printing in anatomy teaching: current evidence. Surg Radiol Anat. 2020;42(7):835–841. doi: 10.1007/s00276-020-02470-2. [DOI] [PubMed] [Google Scholar]
- 15.Keenan ID, ben Awadh A. Integrating 3D Visualisation Technologies in Undergraduate Anatomy Education. In: Rea PM, editor. Biomedical Visualisation [Internet]. Cham: Springer International Publishing; 2019 [retrieved 3 March 2023]. p. 39‑53. (Advances in Experimental Medicine and Biology; vol. 1120). Available on: http://link.springer.com/10.1007/978-3-030-06070-1_4 [DOI] [PubMed]
- 16.Lim KHA, Loo ZY, Goldie SJ, Adams JW, McMenamin PG. Use of 3D printed models in medical education: A randomized control trial comparing 3D prints versus cadaveric materials for learning external cardiac anatomy: Use of 3D Prints in Medical Education. Anat Sci Educ. 2016;9(3):213–221. doi: 10.1002/ase.1573. [DOI] [PubMed] [Google Scholar]
- 17.Salazar D, Thompson M, Rosen A, Zuniga J. Using 3D printing to improve student education of complex anatomy: A systematic review and meta-analysis. Med Sci Educ. 2022;32(5):1209–1218. doi: 10.1007/s40670-022-01595-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ye Z, Jiang H, Bai S, Wang T, Yang D, Hou H, et al. Meta-analyzing the efficacy of 3D printed models in anatomy education. Front Bioeng Biotechnol. 2023;11:1117555. doi: 10.3389/fbioe.2023.1117555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fleming C, Sadaghiani MS, Stellon MA, Javan R. Effectiveness of three-dimensionally printed models in anatomy education for medical students and resident physicians: Systematic review and meta-analysis. J Am Coll Radiol. 2020;17(10):1220–1229. doi: 10.1016/j.jacr.2020.05.030. [DOI] [PubMed] [Google Scholar]
- 20.Leung G, Pickett AT, Bartellas M, Milin A, Bromwich M, Shorr R, et al. Systematic review and meta-analysis of 3D-printing in otolaryngology education. Int J Pediatr Otorhinolaryngol. 2022;155:111083. doi: 10.1016/j.ijporl.2022.111083. [DOI] [PubMed] [Google Scholar]
- 21.Lau I, Sun Z. Three-dimensional printing in congenital heart disease: A systematic review. J Med Radiat Sci. 2018;65(3):226–236. doi: 10.1002/jmrs.268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, The PRISMA, et al. statement: an updated guideline for reporting systematic reviews. BMJ. 2020;2021:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ben Awadh A, Clark J, Clowry G, Keenan ID. Multimodal three-dimensional visualization enhances novice learner interpretation of basic cross-sectional anatomy. Anat Sci Educ. 2022;15(1):127–142. doi: 10.1002/ase.2045. [DOI] [PubMed] [Google Scholar]
- 24.Chandrasekaran R, Radzi S, Kai PZ, Rajalingam P, Rotgans J, Mogali SR. A validated instrument measuring students’ perceptions on plastinated and three-dimensional printed anatomy tools. Anat Sci Educ. 2022;15(5):850–862. doi: 10.1002/ase.2147. [DOI] [PubMed] [Google Scholar]
- 25.Hammerton C, Yip SWL, Manobharath N, Myers G, Sturrock A. Are 3D printed models acceptable in assessment? Clin Teach. 2022;19(3):221–228. doi: 10.1111/tct.13477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Harmon DJ, Klein BA, Im C, Romero D. Development and implementation of a three-dimensional (3D) printing elective course for health science students. Anat Sci Educ. 2022;15(3):620–627. doi: 10.1002/ase.2133. [DOI] [PubMed] [Google Scholar]
- 27.Mogali SR, Chandrasekaran R, Radzi S, Peh ZK, Tan GJS, Rajalingam P, et al. Investigating the effectiveness of three-dimensionally printed anatomical models compared with plastinated human specimens in learning cardiac and neck anatomy: A randomized crossover study. Anat Sci Educ. 2022;15(6):1007–1017. doi: 10.1002/ase.2128. [DOI] [PubMed] [Google Scholar]
- 28.Tan L, Wang Z, Jiang H, Han B, Tang J, Kang C, et al. Full color 3D printing of anatomical models. Clin Anat. 2022;35(5):598–608. doi: 10.1002/ca.23875. [DOI] [PubMed] [Google Scholar]
- 29.Bertolini M, Rossoni M, Colombo G. Operative workflow from CT to 3D printing of the heart: opportunities and challenges. Bioengineering. 2021;8(10):130. doi: 10.3390/bioengineering8100130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Krishnasamy S, Mokhtar RAR, Singh R, Sivallingam S, Aziz YFA, Mathaneswaran V. 3D Rapid Prototyping Heart Model Validation for Teaching and Training — A Pilot Project in a Teaching Institution. Braz J Cardiovasc Surg [Internet]. 2021 [retrieved 3 March 2023];36(5). Available on: https://cdn.publisher.gn1.link/bjcvs.org/pdf/v36n5a18.pdf [DOI] [PMC free article] [PubMed]
- 31.Mahrous A, Elgreatly A, Qian F, Schneider GB. A comparison of pre-clinical instructional technologies: Natural teeth, 3D models, 3D printing, and augmented reality. J Dent Educ. 2021;85(11):1795–1801. doi: 10.1002/jdd.12736. [DOI] [PubMed] [Google Scholar]
- 32.O’Brien C, Souza CA, Sheikh A, Miguel O, Wood T. Use of tracheobronchial tree 3-dimensional printed model: does it improve trainees’ understanding of segmentation anatomy? A prospective study. 3D Print Med. 2021;7(1):2. [DOI] [PMC free article] [PubMed]
- 33.Ruiz OG, Dhaher Y. Multi-color and Multi-Material 3D Printing of Knee Joint models. 3D Print Med. 2021;7(1):12. [DOI] [PMC free article] [PubMed]
- 34.Smillie R, Williams M, Richard M, Cosker T. Producing three-dimensional printed models of the hepatobiliary system from computed tomography imaging data. Ann R Coll Surg Engl. 2021;103(1):41–46. doi: 10.1308/rcsann.2020.0191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vatankhah R, Emadzadeh A, Nekooei S, Tafaghodi Yousefi B, Khadem Rezaiyan M, Karimi Moonaghi H, et al. 3D Printed Models for Teaching Orbital Anatomy, Anomalies and Fractures. J Ophthalmic Vis Res [Internet]. 25 oct 2021 [retrieved 3 March 2023]; Available on: https://knepublishing.com/index.php/JOVR/article/view/9751 [DOI] [PMC free article] [PubMed]
- 36.Weatherall AD, Rogerson MD, Quayle MR, Cooper MG, McMenamin PG, Adams JW. A Novel 3-dimensional printing fabrication approach for the production of pediatric airway models. Anesth Analg. 2021;133(5):1251–1259. doi: 10.1213/ANE.0000000000005260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Abdulcadir J, Dewaele R, Firmenich N, Remuinan J, Petignat P, Botsikas D, et al. In Vivo imaging-based 3-dimensional pelvic prototype models to improve education regarding sexual anatomy and physiology. J Sex Med. 2020;17(9):1590–1602. doi: 10.1016/j.jsxm.2020.05.025. [DOI] [PubMed] [Google Scholar]
- 38.Chae R, Sharon JD, Kournoutas I, Ovunc SS, Wang M, Abla AA, et al. Replicating skull base anatomy with 3D technologies: A comparative study using 3D-scanned and 3D-printed models of the temporal bone. Otol Neurotol. 2020;41(3):e392–403. doi: 10.1097/MAO.0000000000002524. [DOI] [PubMed] [Google Scholar]
- 39.Chedid VG, Kamath AA, M. Knudsen J, Frimannsdottir K, Yost KJ, R. Geske J, et al. Three-Dimensional-Printed Liver Model Helps Learners Identify Hepatic Subsegments: A Randomized-Controlled Cross-Over Trial. Am J Gastroenterol. 2020;115(11):1906‑10. [DOI] [PubMed]
- 40.Chen Y, Qian C, Shen R, Wu D, Bian L, Qu H, et al. 3D printing technology improves medical interns’ understanding of anatomy of gastrocolic trunk. J Surg Educ. 2020;77(5):1279–1284. doi: 10.1016/j.jsurg.2020.02.031. [DOI] [PubMed] [Google Scholar]
- 41.Damon A, Clifton W, Valero-Moreno F, Nottmeier E. Orientation Planning in the Fused Deposition Modeling 3D Printing of Anatomical Spine Models. Cureus [Internet]. 23 Feb 2020 [retrieved 3 March 2023]; Available on: https://www.cureus.com/articles/28416-orientation-planning-in-the-fused-deposition-modeling-3d-printing-of-anatomical-spine-models [DOI] [PMC free article] [PubMed]
- 42.Hojo D, Murono K, Nozawa H, Kawai K, Hata K, Tanaka T, et al. Utility of a three-dimensional printed pelvic model for lateral pelvic lymph node dissection. Int J Colorectal Dis. 2020;35(5):905–910. doi: 10.1007/s00384-020-03534-w. [DOI] [PubMed] [Google Scholar]
- 43.Javan R, Rao A, Jeun BS, Herur-Raman A, Singh N, Heidari P. From CT to 3D printed models, serious gaming, and virtual reality: framework for educational 3D visualization of complex anatomical spaces from within—the pterygopalatine fossa. J Digit Imaging. 2020;33(3):776–791. doi: 10.1007/s10278-019-00315-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Low CM, Choby G, Viozzi M, Morris JM. Construction of three-dimensional printed anatomic models for frontal sinus education. Neuroradiol J. 2020;33(1):80–84. doi: 10.1177/1971400919849781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Radzi S, Tan HKJ, Tan GJS, Yeong WY, Ferenczi MA, Low-Beer N, et al. Development of a three-dimensional printed heart from computed tomography images of a plastinated specimen for learning anatomy. Anat Cell Biol. 2020;53(1):48–57. doi: 10.5115/acb.19.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tanner JA, Jethwa B, Jackson J, Bartanuszova M, King TS, Bhattacharya A, et al. A Three-dimensional print model of the pterygopalatine fossa significantly enhances the learning experience. Anat Sci Educ. 2020;13(5):568–580. doi: 10.1002/ase.1942. [DOI] [PubMed] [Google Scholar]
- 47.Tripodi N, Kelly K, Husaric M, Wospil R, Fleischmann M, Johnston S, et al. The impact of three-dimensional printed anatomical models on first-year student engagement in a block mode delivery. Anat Sci Educ. 2020;13(6):769–777. doi: 10.1002/ase.1958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Williams MA, Smillie RW, Richard M, Cosker TDA. Producing 3D printed high-fidelity retroperitoneal models from in vivo patient data: The Oxford Method. J Anat. 2020;237(6):1177–1184. doi: 10.1111/joa.13278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Backhouse S, Taylor D, Armitage JA. Is this mine to keep? Three-dimensional printing enables active, personalized learning in anatomy. Anat Sci Educ. 2019;12(5):518–528. doi: 10.1002/ase.1840. [DOI] [PubMed] [Google Scholar]
- 50.Bartikian M, Ferreira A, Gonçalves-Ferreira A, Neto LL. 3D printing anatomical models of head bones. Surg Radiol Anat. 2019;41(10):1205–1209. doi: 10.1007/s00276-018-2148-4. [DOI] [PubMed] [Google Scholar]
- 51.Cai B, Rajendran K, Bay BH, Lee J, Yen C. The effects of a functional three-dimensional (3D) printed knee joint simulator in improving anatomical spatial knowledge. Anat Sci Educ. 2019;12(6):610–618. doi: 10.1002/ase.1847. [DOI] [PubMed] [Google Scholar]
- 52.Hojo D, Murono K, Nozawa H, Kawai K, Hata K, Tanaka T, et al. Utility of a Three-Dimensional Printed Pelvic Model for Lateral Pelvic Lymph Node Dissection Education: A Randomized Controlled Trial. J Am Coll Surg. 2019;229(6):552–559e3. [DOI] [PubMed]
- 53.Kanagasuntheram R, Geh NKT, Yen CC, Dheen ST, Bay BH. A composite 3D printed model of the midcarpal joint. Anat Sci Int. 2019;94(1):158–162. doi: 10.1007/s12565-018-0469-3. [DOI] [PubMed] [Google Scholar]
- 54.Shen Z, Yao Y, Xie Y, Guo C, Shang X, Dong X, et al. The process of 3D printed skull models for anatomy education. Comput Assist Surg. 2019;24(sup1):121–130. doi: 10.1080/24699322.2018.1560101. [DOI] [PubMed] [Google Scholar]
- 55.Skrzat J, Zdilla MJ, Brzegowy P, Hołda M. 3 D printed replica of the human temporal bone intended for teaching gross anatomy. Folia Med Cracov. 2019;59(3):23–30. [PubMed] [Google Scholar]
- 56.Ugidos Lozano MT, Haro FB, Ruggiero A, Manzoor S, Juanes Méndez JA. Evaluation of the applicability of 3d models as perceived by the students of health sciences. J Med Syst. 2019;43(5):108. doi: 10.1007/s10916-019-1238-0. [DOI] [PubMed] [Google Scholar]
- 57.Yi X, Ding C, Xu H, Huang T, Kang D, Wang D. Three-dimensional printed models in anatomy education of the ventricular system: a randomized controlled study. World Neurosurg. 2019;125:e891–901. doi: 10.1016/j.wneu.2019.01.204. [DOI] [PubMed] [Google Scholar]
- 58.Zhang X, Xu Z, Tan L, Li Y, Liu L, Chen N, et al. Application of three-dimensional reconstruction and printing as an elective course for undergraduate medical students: an exploratory trial. Surg Radiol Anat. 2019;41(10):1193–1204. doi: 10.1007/s00276-019-02248-1. [DOI] [PubMed] [Google Scholar]
- 59.Bannon R, Parihar S, Skarparis Y, Varsou O, Cezayirli E. 3D printing the pterygopalatine fossa: a negative space model of a complex structure. Surg Radiol Anat. 2018;40(2):185–191. doi: 10.1007/s00276-017-1916-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Casciato DJ, Builes NA, Singh BN. Using three-dimensional printing to enhance cross-sectional anatomy instruction. J Am Podiatr Med Assoc. 2018;108(4):304–310. doi: 10.7547/16-137. [DOI] [PubMed] [Google Scholar]
- 61.Garas M, Vaccarezza M, Newland G, McVay-Doornbusch K, Hasani J. 3D-Printed specimens as a valuable tool in anatomy education: A pilot study. Ann Anat - Anat Anz. 2018;219:57–64. doi: 10.1016/j.aanat.2018.05.006. [DOI] [PubMed] [Google Scholar]
- 62.Mogali SR, Yeong WY, Tan HKJ, Tan GJS, Abrahams PH, Zary N, et al. Evaluation by medical students of the educational value of multi-material and multi-colored three-dimensional printed models of the upper limb for anatomical education: 3D Printed Upper Limb in Anatomical Education. Anat Sci Educ. 2018;11(1):54–64. doi: 10.1002/ase.1703. [DOI] [PubMed] [Google Scholar]
- 63.Smith CF, Tollemache N, Covill D, Johnston M. Take away body parts! An investigation into the use of 3D-printed anatomical models in undergraduate anatomy education. Anat Sci Educ. 2018;11(1):44–53. doi: 10.1002/ase.1718. [DOI] [PubMed] [Google Scholar]
- 64.Smith ML, Jones JFX. Dual-extrusion 3D printing of anatomical models for education: Two Materials 3D Printing in Anatomy. Anat Sci Educ. 2018;11(1):65–72. doi: 10.1002/ase.1730. [DOI] [PubMed] [Google Scholar]
- 65.Suzuki R, Taniguchi N, Uchida F, Ishizawa A, Kanatsu Y, Zhou M, et al. Transparent model of temporal bone and vestibulocochlear organ made by 3D printing. Anat Sci Int. 2018;93(1):154–159. doi: 10.1007/s12565-017-0417-7. [DOI] [PubMed] [Google Scholar]
- 66.Wu AM, Wang K, Wang JS, Chen CH, Yang XD, Ni WF, et al. The addition of 3D printed models to enhance the teaching and learning of bone spatial anatomy and fractures for undergraduate students: a randomized controlled study. Ann Transl Med. 2018;6(20):403–403. doi: 10.21037/atm.2018.09.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Zhang XD, Li ZH, Wu ZS, Lin W, Lin WJ, Lin JC, et al. A novel three-dimensional-printed paranasal sinus–skull base anatomical model. Eur Arch Otorhinolaryngol. 2018;275(8):2045–2049. doi: 10.1007/s00405-018-5051-z. [DOI] [PubMed] [Google Scholar]
- 68.Bücking TM, Hill ER, Robertson JL, Maneas E, Plumb AA, Nikitichev DI. From medical imaging data to 3D printed anatomical models. Chen HCI, éditeur. PLOS ONE. 2017;12(5):e0178540. [DOI] [PMC free article] [PubMed]
- 69.Chen S, Pan Z, Wu Y, Gu Z, Li M, Liang Z, et al. The role of three-dimensional printed models of skull in anatomy education: a randomized controlled trail. Sci Rep. 2017;7(1):575. doi: 10.1038/s41598-017-00647-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Favier V, Zemiti N, Caravaca Mora O, Subsol G, Captier G, Lebrun R, et al. Geometric and mechanical evaluation of 3D-printing materials for skull base anatomical education and endoscopic surgery simulation – A first step to create reliable customized simulators. Cavallo LM, editor. PLOS ONE. 2017;12(12):e0189486. [DOI] [PMC free article] [PubMed]
- 71.Javan R, Davidson D, Javan A. Nerves of steel: a low-cost method for 3D printing the cranial nerves. J Digit Imaging. 2017;30(5):576–583. doi: 10.1007/s10278-017-9951-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Legocki AT, Duffy-Peter A, Scott AR. Benefits and limitations of entry-level 3-dimensional printing of maxillofacial skeletal models. JAMA Otolaryngol Neck Surg. 2017;143(4):389. doi: 10.1001/jamaoto.2016.3673. [DOI] [PubMed] [Google Scholar]
- 73.Lozano MTU, Haro FB, Diaz CM, Manzoor S, Ugidos GF, Mendez JAJ. 3D digitization and prototyping of the skull for practical use in the teaching of human anatomy. J Med Syst. 2017;41(5):83. doi: 10.1007/s10916-017-0728-1. [DOI] [PubMed] [Google Scholar]
- 74.Fasel JHD, Aguiar D, Kiss-Bodolay D, Montet X, Kalangos A, Stimec BV, et al. Adapting anatomy teaching to surgical trends: a combination of classical dissection, medical imaging, and 3D-printing technologies. Surg Radiol Anat. 2016;38(3):361–367. doi: 10.1007/s00276-015-1588-3. [DOI] [PubMed] [Google Scholar]
- 75.Javan R, Herrin D, Tangestanipoor A. Understanding spatially complex segmental and branch anatomy using 3D printing. Acad Radiol. 2016;23(9):1183–1189. doi: 10.1016/j.acra.2016.04.010. [DOI] [PubMed] [Google Scholar]
- 76.Kong X, Nie L, Zhang H, Wang Z, Ye Q, Tang L, et al. Do three-dimensional visualization and three-dimensional printing improve hepatic segment anatomy teaching? A randomized controlled study. J Surg Educ. 2016;73(2):264–269. doi: 10.1016/j.jsurg.2015.10.002. [DOI] [PubMed] [Google Scholar]
- 77.Kong X, Nie L, Zhang H, Wang Z, Ye Q, Tang L, et al. Do 3D printing models improve anatomical teaching about hepatic segments to medical students? A randomized controlled study. World J Surg. 2016;40(8):1969–1976. doi: 10.1007/s00268-016-3541-y. [DOI] [PubMed] [Google Scholar]
- 78.O’Reilly MK, Reese S, Herlihy T, Geoghegan T, Cantwell CP, Feeney RNM, et al. Fabrication and assessment of 3D printed anatomical models of the lower limb for anatomical teaching and femoral vessel access training in medicine: Subject Specific 3D-Printed Anatomy. Anat Sci Educ. 2016;9(1):71–79. doi: 10.1002/ase.1538. [DOI] [PubMed] [Google Scholar]
- 79.Shah KJ, Peterson JC, Beahm DD, Camarata PJ, Chamoun RB. Three-dimensional printed model used to teach skull base anatomy through a transsphenoidal approach for neurosurgery residents. Oper Neurosurg. 2016;12(4):326–329. doi: 10.1227/NEU.0000000000001127. [DOI] [PubMed] [Google Scholar]
- 80.Adams JW, Paxton L, Dawes K, Burlak K, Quayle M, McMenamin PG. 3D printed reproductions of orbital dissections: a novel mode of visualising anatomy for trainees in ophthalmology or optometry. Br J Ophthalmol. 2015;99(9):1162–1167. doi: 10.1136/bjophthalmol-2014-306189. [DOI] [PubMed] [Google Scholar]
- 81.Cohen J, Reyes SA. Creation of a 3D printed temporal bone model from clinical CT data. Am J Otolaryngol. 2015;36(5):619–624. doi: 10.1016/j.amjoto.2015.02.012. [DOI] [PubMed] [Google Scholar]
- 82.Hochman JB, Rhodes C, Kraut J, Pisa J, Unger B. End user comparison of anatomically matched 3-dimensional printed and virtual haptic temporal bone simulation: a pilot study. Otolaryngol Neck Surg. 2015;153(2):263–268. doi: 10.1177/0194599815586756. [DOI] [PubMed] [Google Scholar]
- 83.McMenamin PG, Quayle MR, McHenry CR, Adams JW. The production of anatomical teaching resources using three-dimensional (3D) printing technology: 3D Printing in Anatomy Education. Anat Sci Educ. 2014;7(6):479–486. doi: 10.1002/ase.1475. [DOI] [PubMed] [Google Scholar]
- 84.Cercenelli L, De Stefano A, Billi AM, Ruggeri A, Marcelli E, Marchetti C, et al. AEducaAR, anatomical education in augmented reality: A pilot experience of an innovative educational tool combining AR technology and 3D printing. Int J Environ Res Public Health. 2022;19(3):1024. doi: 10.3390/ijerph19031024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Young JC, Quayle MR, Adams JW, Bertram JF, McMenamin PG. Three-dimensional printing of archived human fetal material for teaching purposes: 3D printed human gestational replicas. Anat Sci Educ. 2019;12(1):90–96. doi: 10.1002/ase.1805. [DOI] [PubMed] [Google Scholar]
- 86.Jebb AT, Ng V, Tay L. A review of key likert scale development advances: 1995–2019. Front Psychol. 2021;12:637547. doi: 10.3389/fpsyg.2021.637547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Wilk R, Likus W, Hudecki A, Syguła M, Różycka-Nechoritis A, Nechoritis K. What would you like to print? Students’ opinions on the use of 3D printing technology in medicine. Miller AC, éditeur. PLOS ONE. 2020;15(4):e0230851. [DOI] [PMC free article] [PubMed]
- 88.Chytas D, Salmas M, Demesticha T, Troupis T. Three-dimensional printing in anatomy education: Is it similarly useful for teaching of all anatomical regions and structures? Anat Sci Educ. 2023;16(1):5–6. doi: 10.1002/ase.2216. [DOI] [PubMed] [Google Scholar]
- 89.Könings KD, Mordang S, Smeenk F, Stassen L, Ramani S. Learner involvement in the co-creation of teaching and learning: AMEE Guide No. 138. Med Teach. 2021;43(8):924‑36. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analysed for the current study are not publicly available due to the language barrier but are available from the corresponding author upon reasonable request.