Abstract
Objectives:
The study aimed to evaluate the clinical and radiological results after endoscopic repair of gluteus medius muscle injuries and proposed an anatomical classification for the different injury classes.
Methods:
A retrospective case series, including patients who had undergone endoscopic repair of the hip abductor tendon. The surgical procedure was standardized. Magnetic resonance imaging (MRI) studies were analyzed, and the injuries were classified into three types: nontransfixing partial-extension (nTPE) tear, transfixing partial-extension (TPE) tear, and transfixing full-extension (TFE) tear. TPE and TFE were considered high-grade tears. The postoperative outcomes were as follows: duration of walking aid requirement, duration of physical therapy, time to return to daily activities, modified Harris Hip score (mHHS) and Nonarthritic Hip Score (NAHS) functional scores, pain visual analog scale (VAS), satisfaction, claudication, Trendelenburg test, and reoperation.
Results:
Sixteen patients were included (94% women; mean age 65 years), with a mean follow-up of 42 months (12-131, range). Out of the cases with preoperative exams available for analysis, four cases (31%) were nTPE, three (23%) TPE, and six (46%) TFE tears. Thus, 69% of the patients had high-grade injuries. These patients had a higher degree of fat infiltration (P = 0.034), but this was not correlated with inferior postoperative clinical or radiological results. One patient required reoperation due to a recurrent injury.
Conclusion:
Isolated extra-articular injuries to the tendons of the gluteus medius and minimus evolved satisfactorily after endoscopic repair. Due to the small number of cases, it was not possible to observe differences in outcomes between high-and low-grade injuries.
Key Words: Anatomical classification, Endocospic treatment, Tendon injuries
Introduction
Gluteus medius and minimus injuries, especially rupture injuries, are very common in women from the 4th-5th decade of life and usually produce greater trochanteric pain syndrome (GTPS). Initial conservative treatment is the first option and comprises physiotherapy, infiltrations, and shock wave therapy (SWT).1 Platelet-rich plasma (PRP) may be indicated in refractory cases and when performing open or endoscopic surgical procedures for ruptures.1
Endoscopic repair of torn tendons (gluteus medius and/or minimus) was initially described by Voos et al.2 Numerous researchers have reported good results following endoscopic treatment for both partial injuries3-5 and full-extension (transfixant/complete) gluteus medius tendon injuries,6-11 usually with short-and medium-term follow-up. Associated intra-articular injuries and the need for intra-articular approaches can change the clinical results. One study demonstrated that functional results were maintained with a mean time greater than five years with a survival rate of 92% when comparing patients with a minimum of five years of follow-up (mean two years).12
Few studies have compared the results of open and endoscopic techniques. In a systematic review, Chandrasekaran et al13 demonstrated that open treatment results in similar functional and pain outcomes, but endoscopic treatment leads to fewer complications; on the other hand, Maslaris et al14 reported similar results and suggested that open treatment should be applied for complex cases.
Concepts of repair of partial injuries originated from experience in shoulder surgery and were described by Domb et al.15 However, the association between injuries in this region and rotator cuff injuries in the shoulder is older, as described by Bunker et al16 and Kegan.17 Therefore, some authors refer to the gluteus medius and minimus tendons as the tendons of the hip rotator cuff. This association is also evident in the concept of muscle atrophy and fat degeneration described in the shoulder initially by Goutallier et al18 in computed tomography (CT) study and later by Gerber et al19 using Magnetic resonance imaging (MRI), which, as mentioned by Engelkem et al,20 was transferred to the hip based on the percentage of fat degeneration concerning integral muscle fibers and divided into four types/grades. Good inter-and intra-observer reproducibility was demonstrated in patients after hip arthroplasty20 and in patients after gluteal tendon repair.21 additionally, studies have shown the correlation between initial degrees of preoperative degeneration and superior functional results.21,22
Recent editorials by Ochiai23 and Lubowitz et al24 alerted general orthopedists and hip specialists who usually perform total joint replacements to the consistent and encouraging results of the endoscopic treatment of partial injuries. However, we believe substantial challenges remain for radiologists and orthopedists in characterizing partial extension injuries similar to shoulder partial articular supraspinatus tendon avulsion (PASTA) injuries. Nho et al25 described these injuries and proposed the term partial articular gluteus tendon avulsion (PAGTA) for those in the hip. Here, we propose an anatomical classification to encourage better characterization of these tears since the treatment strategies and results may differ.
Finally, there is controversy regarding the effectiveness of shoulder cuff tendon surgery to improve degeneration19,26,27 and prevent degeneration from progressing.28,29 However, no study has been conducted to compare the degree of preoperative muscle degeneration with the degree of postoperative gluteus medius muscle degeneration. The present study aimed to evaluate the functional and radiological results after endoscopic repair of gluteus medius muscle tears with a minimum follow-up of 12 months and propose an anatomical classification for the different injuries.
Materials and Methods
A retrospective, single-center case series study including patients submitted to surgical procedures between 2009 and 2021 and attended follow-up at the same location. This study was approved by the Ethics Committee for Research with Human Beings.
All surgeries were performed by the same two senior surgeons, one a hip surgeon and the other a knee and shoulder surgeon, with 20 years of experience in arthroscopy. The inclusion criteria were: patients submitted to endoscopic hip abductor tendon repair after at least six months of failed conservative care; no major hip arthrosis (G2, according to the Tonnis classification)30; no severe hip dysplasia (lateral center angle less than 20 degrees); and no previous surgeries on the same hip and/or previous conditions on the operated hip (fracture sequelae, epiphysiolysis and avascular necrosis). Cases with missing clinical follow-up were excluded from the analysis.
Surgical technique and operative tips
Patients underwent sedation in addition to spinal anesthesia. All were placed in horizontal dorsal decubitus and operated on the traction table. Traction table was used to treat a concomitant intra-articular symptomatic injury in only one patient. An accessory table, radioscopy, 30-degree optics, infusion pump, and radio frequency (VAPR, De Puy®) were used routinely, avoiding the use of adrenaline for older patients. The 1st arthroscopic portal was always made under radioscopic control. Four portals were used in a conformation of cardinal points (anterior, posterior, superior, and inferior, following the anatomical references shown in [Figure 1A].
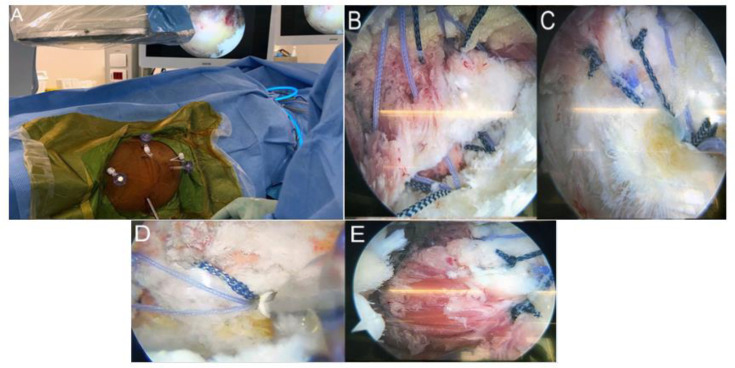
Figure 1.
Images of the arthroscopic repair of gluteal tendon injuries. (A) Four arthroscopic portals: anterior, posterior, superior, and inferior. (B-E) Arthroscopic images illustrating anchor placement using the double-row technique. (Color should be used for this figure)
With blunt dissection with the trocar, it is suggested to longitudinally transect the iliotibial tract, releasing adhesions with the bursa or the tendon itself that are present in some cases and improving visualization while working in the same space.
The 2nd and 3rd portals (posterior and anterior) are generated with an outside-in approach under an arthroscopic view, carefully selecting the best angle as these are the portals for the anchors in the first row; the superior portal is made last and is used only for handling the suture threads. The double-row anchor is usually inserted through the inferior portal. Importantly, as we always use cuff anchors (Healix advantage, De Puy®, 4.5-5.5 or Biorcorck screw, Artrhrex, 4.5-5.5 and Bioswivlock, 4.5, Arthrex®), the cannulas used for inserting anchors into the portals are shoulder cannulas for compatibility with the anchor cable, except for the upper cannula, which can be a hip canula. In all cases, we used shoulder tweezers to handle the tissues (Arthrex) and did not use loop tweezers. We performed the double-row technique in all cases [Figure 1B-E].
Our patient with partial injuries had high-grade injuries; that is, almost full-thickness (transfixing) injuries. Therefore, we completed the injury and performed the double-row technique with two more superior anchors and another knotless anchor. Osteophytes were evaluated by imaging in all cases, and intraoperative resection with a bur blade or acromionizer (De Puy® or Arthrex®) was performed in some cases.
Postoperative management
Patients used a walker for approximately six to eight weeks, did not use pads/braces, and started physiotherapy from the first week, initially for pain and edema control. Later, physiotherapy aimed to gain a wider range of motion and enhanced core control.
Data collection and outcomes
The following preoperative data were collected: symptoms, previous treatments, pain level on a visual analog scale (VAS, 0-10), claudication, and Trendelenburg test. The postoperative outcomes collected and analyzed were as follows: duration of use of external walking support, duration of physiotherapy treatment, time to return to daily activities, and clinical outcomes at the last visit: modified Harris hip score (mHHS) and nonarthritic hip score (NAHS) scores, visual analog scale (VAS) for pain, satisfaction (0-10), presence of claudication and Trendelenburg test. In addition, data regarding the need for reoperation was also collected and analyzed.
The MRIs were evaluated before (baseline) and after surgery (postoperative follow-up). The exams were performed in 1.5 Tesla MRI Scanners with fast spin-echo (FSE) T1 and T2 sequences with fat saturation, multiplanar sections, and patients in the supine position. The tendon and muscles of the gluteus medius and minimus evaluated were atrophy and fat infiltration into muscles was evaluated using the FSE T1 sequence, and fat infiltration was graded according to a 5-point semiquantitative scale described by Goutallier et al18 that was modified for the hip20,21 (Grade 0: normal; Grade 1: some traces of fat; Grade 2: less than 50% fat; Grade 3: both fat and muscle; Grade 4: more fat than muscle).
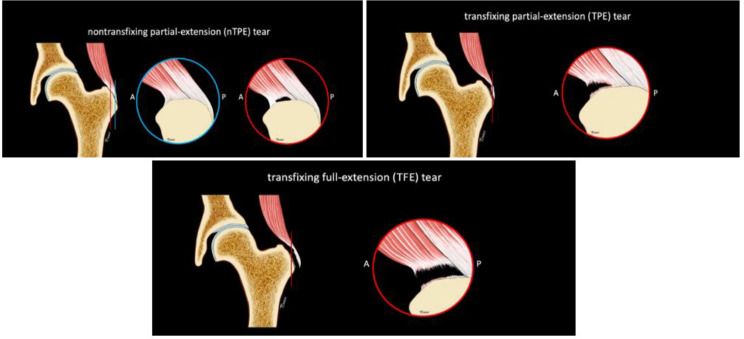
The tendon insertion was analyzed to define the tendon tear/injury magnitude. The authors created a tear classification system based on transfixation and injury extension [Figures 2 and 3] as follows: i) nontransfixing partial-extension (nTPE tear); ii) transfixing partial-extension (TPE tear); and transfixing full-extension-disinsertion (TFE tear). TPT and TFE tears were considered high-grade injuries in the subgroup analysis.
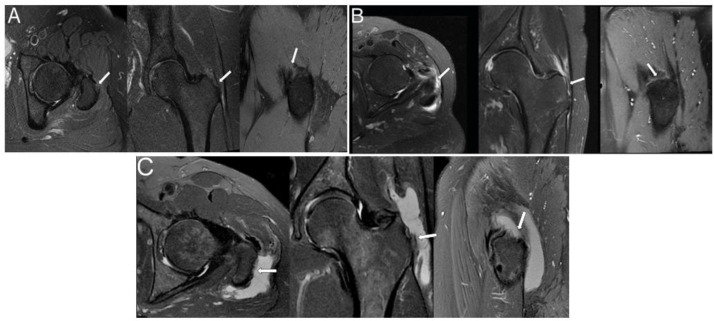
Figure 2.
Different types of gluteal tendon injuries in axial (left), coronal (center) and sagittal (right). (A) Nontransfixing partial-extension (nTPE) tear (low-grade); (B) transfixing partial-extension (TPE) tear (high-grade); (C) transfixing full-extension (TFE) tear (high-grade)
Figure 3.
Classification of the tendon tear based on transfixation and extension. (Top) Nontransfixing partial-extension (nTPE) tear (low-grade); (middle) transfixing partial-extension (TPE) tear (high-grade); (bottom) transfixing full-extension (TFE) tear (high-grade). A= anterior; P=posterior. (Color should be used for this figure)
Initially, a descriptive analysis of the collected data was performed. The outcome variables were not normally distributed, and the hypotheses were tested by nonparametric tests. The means between two groups were compared using the Mann–Whitney U test, Kruskal–Wallis test was used for three groups, and Wilcoxon's test was used for paired groups. Kendall's tau-b test for correlation between numerical variables and Spearman's test for correlation between numerical and ordinal variables were applied. The significance level was adopted at 95%, and the tests were performed using SPSS software.
Results
Sixteen cases were treated, met inclusion criteria, and were included in this case series. The descriptive data of this series are shown in [Table 1].
Table 1.
Preoperative demographic and clinical data
| Data | |
|---|---|
| Patients | 16 |
| Female sex | 15 (94%) |
| Age (years old) | 65 (52; 73) |
| VAS pain (0-10) | 9 (8; 10) |
| Positive Trendelenburg sing | 6 (38%) |
| Claudication | 9 (56%) |
| Duration of symptoms (months) | 12 (7; 23) |
Data are shown as absolute numbers and percentages (%) or as median and quartiles (Q1; Q3). VAS: visual analog scale
No intraoperative complications were observed. Fourteen patients had preoperative MRI available for analysis (88%). One patient had calcareous tendinopathy of the gluteus medius and was not considered for the tear type analysis. The analyzed cases were classified according to the classification described in the methods section: six (46%) TFE tears, three (23%) TPE tears, and four (31%) nTPE tears. Nine cases of TFE and TPE tears comprised the high-grade group (69%). Most of the cases presented an isolated injury of the gluteus medius tendon (10; 77%), while three cases (23%) showed a combined rupture of the tendons of the gluteus medius and minimus.
The high-grade cases had a higher degree of fat infiltration than the nTPE cases [Table 2], both in the preoperative MRI (P = 0.003) and postoperative MRI (P = 0.029). There was no postoperative increase or decrease in the Goutalier score at a mean of seven months (2.5 to 10 months range). The analysis of fat degeneration did not show differences based on the tendons involved (minimum, medium, or both) (P = 0.209; [Table 2]).
Table 2.
Analysis of the relationship between fat degeneration and tear type
| n | Goutalier preop | |
|---|---|---|
| Low-grade tear | 4 | 0.5 (0; 1) |
| High-grade tear | 9 | 1.5 (1.5; 2) |
| P value | 0.034* | |
| MED tendon | 10 | 1.5 (1; 2) |
| MED + MIN tendons | 3 | 1.0 (0; 2) |
| P value | 0.209 |
Data are shown as median and quartiles (Q1; Q3). n: number of cases. MED: gluteus medius tendon. MIN: gluteus minimus tendon. * Statistically significant (P < 0.05)
Clinical outcomes were collected during the postoperative period, and scores were collected at the last visit, with a median follow-up time of 24 months (3-131 minimum-maximum and Q3:62-Q1:23). The data obtained are shown in [Table 3].
Table 3.
Postoperative clinical outcomes
| Outcomes | |
|---|---|
| Walking aid (months) | 2 (2; 4) |
| Return to daily activities (months) | 2 (2; 6) |
| Physiotherapy (months) | 5,5 (3;13) |
| VAS pain (0-10) | 2 (0; 3) |
| mHHS score | 97 (94; 97) |
| NAHS score | 94 (83; 99) |
| Claudication | 0 (0%) |
| Satisfaction (0-10) | 10 (8; 10) |
Data are shown as absolute numbers and percentages (%) or as median and quartiles (Q1; Q3).
VAS: visual analog scale. MHHS: modified Harris hip score; NAHS: nonarthritic hip score
To evaluate the relationships between clinical or radiological factors and either better or worse clinical outcomes, the preoperative variables (Trendelenburg sign, claudication, duration of symptoms, VAS pain, Goutalier grades and tear grades) were tested versus the postoperative outcomes (VAS pain, mHHS, NAHS and satisfaction). All these tests demonstrated the absence of statistical significance, as shown in [Table 4].
Table 4.
Comparison of different preoperative presentations with clinical outcomes in the last follow-up
| n | VAS pain | mHHS | NAHS | Satisfaction | |
|---|---|---|---|---|---|
| Trendelenburg - | 10 | 2 (1; 2) | 97 (94; 97) | 99 (94; 99) | 10 (7; 10) |
| Trendelenburg + | 6 | 1 (0; 3) | 96 (94; 97) | 88 (82; 94) | 10 (10; 10) |
| P value | 0.396 | 0.607 | 0.088 | 0.562 | |
| Claudication - | 7 | 2 (0; 6) | 96 (91; 97) | 96 (94; 99) | 10 (6; 10) |
| Claudication + | 9 | 1 (0; 2) | 97 (94; 97) | 97 (82; 99) | 10 (10; 10) |
| P value | 0.456 | 0.776 | 0.995 | 0.471 | |
| Duration of symptoms | 16 | -0,119 | 0.012 | -0.010 | -0.167 |
| P value | 0.570 | 0.956 | 0.960 | 0.434 | |
| Low-grade tear | 4 | 1 (0; 6) | 97 (97; 97) | 94 (94; 99) | 9 (7; 10) |
| High-grade tear | 9 | 2 (0; 2) | 97 (94; 97) | 98 (94; 99) | 10 (9; 10) |
| P value | 1.000 | 0.352 | 1.000 | 0.724 | |
| MED tear | 10 | 2 (0; 6) | 97 (94; 97) | 94 (94; 99) | 10 (7; 10) |
| MED + MIN tear | 3 | 2 (1; 2) | 97 (97; 97) | 99 (99; 99) | 9 (6; 10) |
| P value | 0.503 | 0.471 | 0.188 | 0.499 | |
| Goutalier score | 14 | 0.119 | -0.013 | 0.037 | -0.077 |
| P value | 0.699 | 0.966 | 0.906 | 0.793 |
Median and quartiles (Q1; Q3) are shown for the Trendelenburg and rupture subgroups, and correlation coefficients between the Goutalier scores and clinical outcomes are shown. n: number of cases. MED: gluteus medius tendon. MIN: gluteus minimus tendon. VAS: visual analog scale; mHHS: modified Harris hip score; NAHS: nonarthritic hip score
Discussion
Several studies have demonstrated good results after using arthroscopic techniques to repair partial and/or complete injuries of the tendons of the gluteus medius and minimus.3-11 Despite the absence of comparative and randomized studies comparing endoscopic and open techniques,13,14 showing similar results, fewer complications were observed with the endoscopic technique in the first study and suggested that open surgery should be performed for more complex surgeries. The authors of the current work suggest reserving the open technique for cases of gluteal tendon rupture after arthroplasty and more complex injuries, consistent with that indicated by Maslaris et al.14 For partial or complete tears, we always performed the same osteophyte debridement technique and fixation of the injuries with a double-row technique, always using a lower anchor.
The present work covers a more reasonable follow-up time than previous studies.1,31 The authors believe that the best indications are for isolated cases of extra-articular injuries with little or no intra-articular damage. However, other researchers have frequently combined joint and extra-articular injuries in their analyses, which, in our view, influences the results of using endoscopic surgery to repair the gluteal tendon.9,12
An isolated gluteus medius injury was the most prevalent injury in all previous series and was also found in our series.8,11,22 We did not find statistically significant differences in the outcomes in the subgroup analysis. Technically, the gluteus minimus tendon approach adds complexity to the procedure since, in addition to being more anterior, the gluteus minimus tendon is more medialized and deeper. In our first patient, we placed an isolated anchor for minimus tendon repair. Still, in the other patients, we ended up including repairs to the medius's tendons and the minimus in one of the anchors. Another important and constant feature of the injuries in our series and the literature is the much more significant incidence of the involvement of the gluteus anterior bundle compared to its more robust posterior bundle.
We believe, however, that gluteus tendon tears should be better characterized, and injuries cannot be divided into complete or partial injuries. Instead, we suggest better representing the thickness of the injury (transfixing or not transfixing) and its extension (partial or full-extension). Therefore, we proposed an anatomical classification system by dividing the tears about both aspects/ dimensions into nTPE, TPE, or TFP. nTPE, could, in theory, be of the joint component (PAGTA) or bursal component; however, in our series and our experience, we did not find injuries only on the bursal face. We believe, therefore, that partial injury should be better characterized and, as noted in an editorial in the journal Arthroscopy in 2020,24 that general orthopedists and hip specialists should better monitor these partial tendon tears since recent studies demonstrate excellent treatment results despite the absence of randomized controlled trials comparing methods with conservative treatments and biological techniques such as PRP and SWT.
Regarding the fatty degeneration of the gluteus muscle, we believe that MRI should include images up to the pelvis, not just the hip itself, to achieve a better analysis. Unlike some studies in the literature that correlate lower degrees of degeneration with better clinical outcomes,8,11,22 we did not observe any correlation between the scores analyzed and the degree of fatty degeneration, but this could be due to the reduced sample size. Furthermore, we believe that volumetric MRI sequences help better detect and characterize the tears and the tendon itself because the small gap between the slices reduces the chance of skipping small injuries. Also, these sequences allow for reconstructing images in all planes enabling a better understanding of the injury morphology.
We were the first to analyze potential fatty degeneration reversal after repair, although the results did not reveal a statistically significant difference, and the postoperative MRI collection times varied widely. There is also great controversy regarding the reversal of degeneration in the shoulder after repair,19,26,27 with some studies demonstrating that repair at least prevents the progression of muscle degeneration.28,29 In addition, there is great variation in the methods and the follow-up time for these assessments. We believe that the community should be aware of this matter and aim to standardize approaches in the future.
As for limitations of the study, this is a retrospective case series without a formal comparative analysis, and no preoperative clinical scores were included. In addition, the small sample size limited the subgroup analysis, and not all cases received a full pre-or postoperative MRI study. For the assessment of fatty degeneration, the number of cases (postoperative MRI) was reduced, and there were variations in postoperative MRI times.
However, we believe this is a relevant study because we used the same surgical technique performed by the same surgeons for all patients, and the follow-up time produced interesting findings. Furthermore, MRI followed well-established techniques and were always evaluated by two experienced radiologists. In addition, this is the first comparison of pre-and postoperative degrees of muscle degeneration in the hip. Finally, this study highlights the difficulty of optimizing the characterization of these tears. Thus, we proposed a comprehensive classification system to address this issue.
Conclusion
In conclusion, cases of isolated extra-articular tears of the gluteus tendons presented good clinical results with a mean follow-up time of 42 months. However, possibly due to the small number of cases, no differences were found in clinical and radiological outcomes between high-grade and low-grade tears.
Acknowledgment
We thank Rodrigo Tonan for the illustration of Figure designed especially for use in this publication.
Conflict of interest:
None
Funding:
None
References
- 1.Zhu MF, Musson DS, Cornish J, Young SW, Munro JT. Hip abductor tendon tears: where are we now? Hip Int. 2020;30(5):500–512. doi: 10.1177/1120700020922522. [DOI] [PubMed] [Google Scholar]
- 2.Voos JE, Rudzki JR, Shindle MK, Martin H, Kelly BT. Arthroscopic Anatomy and Surgical Techniques for Peritrochanteric Space Disorders in the Hip. Arthroscopy. 2007;23(11):1246.e1–5. doi: 10.1016/j.arthro.2006.12.014. [DOI] [PubMed] [Google Scholar]
- 3.Coulomb R, Essig J, Mares O, Asencio G, Kouyoumdjian P, May O. Clinical results of endoscopic treatment without repair for partial thickness gluteal tears. Orthop Traumatol Surg Res. 2016;102(3):391–5. doi: 10.1016/j.otsr.2016.01.007. [DOI] [PubMed] [Google Scholar]
- 4.Hartigan DE, Perets I, Ho SW, Walsh JP, Yuen LC, Domb BG. Endoscopic Repair of Partial-Thickness Undersurface Tears of the Abductor Tendon: Clinical Outcomes with Minimum 2-Year Follow-up. Arthroscopy. 2018;34(4):1193–1199. doi: 10.1016/j.arthro.2017.10.022. [DOI] [PubMed] [Google Scholar]
- 5.D'Addona A, Rocca F Della, Carrella D, et al. Effectiveness of endoscopic trans-tendineous repair for partial-thickness tears of medius gluteus: A systematic review of literature. J Hum Sport Exerc. 2020;15:S770–S780. [Google Scholar]
- 6.Lübbeke A, Kampfen S, Stern R, Hoffmeyer P. Results of surgical repair of abductor avulsion after primary total hip arthroplasty. J Arthroplasty. 2008;23(5):694–8. doi: 10.1016/j.arth.2007.08.018. [DOI] [PubMed] [Google Scholar]
- 7.Domb BG, Botser I, Giordano BD. Outcomes of endoscopic gluteus medius repair with minimum 2-year follow-up. Am J Sports Med. 2013;41(5):988–97. doi: 10.1177/0363546513481575. [DOI] [PubMed] [Google Scholar]
- 8.Makridis KG, Lequesne M, Bard H, Djian P. Clinical and MRI results in 67 patients operated for gluteus medius and minimus tendon tears with a median follow-up of 4 6 years. Orthop Traumatol Surg Res. 2014;100(8):849–53. doi: 10.1016/j.otsr.2014.08.004. [DOI] [PubMed] [Google Scholar]
- 9.Chandrasekaran S, Gui C, Hutchinson MR, Lodhia P, Suarez-Ahedo C, Domb BG. Outcomes of Endoscopic Gluteus Medius Repair: Study of Thirty-four Patients with Minimum Two-Year Follow-up. J Bone Joint Surg Am. 2015;97(16):1340–7. doi: 10.2106/JBJS.N.01229. [DOI] [PubMed] [Google Scholar]
- 10.Kirby D, Fried JW, Bloom DA, Buchalter D, Youm T. Clinical Outcomes after Endoscopic Repair of Gluteus Medius Tendon Tear Using a Knotless Technique with a 2-Year Minimum Follow-Up. Arthroscopy. 2020;36(11):2849–55. doi: 10.1016/j.arthro.2020.07.022. [DOI] [PubMed] [Google Scholar]
- 11.Nazal MR, Abraham PF, Conaway WK, et al. Endoscopic Repair of Full-Thickness Gluteus Medius and Minimus Tears-Prospective Study with a Minimum 2-Year Follow-Up. Arthroscopy. 2020;36(8):2160–9. doi: 10.1016/j.arthro.2020.04.025. [DOI] [PubMed] [Google Scholar]
- 12.Perets I, Mansor Y, Yuen LC, Chen AW, Chaharbakhshi EO, Domb BG. Endoscopic Gluteus Medius Repair with Concomitant Arthroscopy for Labral Tears: A Case Series with Minimum 5-Year Outcomes. Arthroscopy. 2017;33(12):2159–67. doi: 10.1016/j.arthro.2017.06.032. [DOI] [PubMed] [Google Scholar]
- 13.Chandrasekaran S, Lodhia P, Gui C, Vemula SP, Martin TJ, Domb BG. Outcomes of Open Versus Endoscopic Repair of Abductor Muscle Tears of the Hip: A Systematic Review. Arthroscopy. 2015;31(10):2057–67. doi: 10.1016/j.arthro.2015.03.042. [DOI] [PubMed] [Google Scholar]
- 14.Maslaris A, Vail TP, Zhang AL, Patel R, Jäger M, Bini SA. Equivalent Mid-Term Results of Open vs Endoscopic Gluteal Tendon Tear Repair Using Suture Anchors in Forty-Five Patients. J Arthroplasty. 2020;35(6):S352–8. doi: 10.1016/j.arth.2020.03.013. [DOI] [PubMed] [Google Scholar]
- 15.Domb BG, Nasser RM, Botser IB. Partial-thickness tears of the gluteus medius: rationale and technique for trans-tendinous endoscopic repair. Arthroscopy. 2010;26(12):1697–705. doi: 10.1016/j.arthro.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 16.Bunker TD, Esler CN, Leach WJ. Rotator-cuff tear of the hip. J Bone Joint Surg Br. 1997;79(4):618–20. doi: 10.1302/0301-620x.79b4.7033. [DOI] [PubMed] [Google Scholar]
- 17.Kegan 2nd A. Rotator cuff tears of the hip. Clin Orthop Relat Res. 1999;368:135–40. [PubMed] [Google Scholar]
- 18.Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994;304:78–83. [PubMed] [Google Scholar]
- 19.Gerber C, Schneeberger AG, Hoppeler H, Meyer DC. Correlation of atrophy and fatty infiltration on strength and integrity of rotator cuff repairs: a study in thirteen patients. J shoulder Elb Surg. 2007;16(6):691–6. doi: 10.1016/j.jse.2007.02.122. [DOI] [PubMed] [Google Scholar]
- 20.Engelken F, Wassilew GI, Köhlitz T, Brockhaus S, Hamm B, Perka C. Assessment of Fatty Degeneration of the Gluteal Muscles in Patients With THA Using MRI: Reliability and Accuracy of the Goutallier and Quartile Classification Systems. J Arthroplasty. 2014;29(1):149–53. doi: 10.1016/j.arth.2013.04.045. [DOI] [PubMed] [Google Scholar]
- 21.Bogunovic L, Lee SX, Haro MS, et al. Application of the Goutallier/Fuchs Rotator Cuff Classification to the Evaluation of Hip Abductor Tendon Tears and the Clinical Correlation with Outcome after Repair. Arthrosc J Arthrosc Relat Surg. 2015;31(11):2145–51. doi: 10.1016/j.arthro.2015.04.101. [DOI] [PubMed] [Google Scholar]
- 22.Thaunat M, Clowez G, Desseaux A, et al. Influence of Muscle Fatty Degeneration on Functional Outcomes after Endoscopic Gluteus Medius Repair. Arthroscopy. 2018;34(6):1816–24. doi: 10.1016/j.arthro.2018.01.005. [DOI] [PubMed] [Google Scholar]
- 23.Ochiai D. Editorial Commentary: Treatment of Partial Thickness Undersurface Abductor Tears of the Hip: Like Backwards a Bike Riding. Arthroscopy. 2018;34(4):1200–1. doi: 10.1016/j.arthro.2017.11.024. [DOI] [PubMed] [Google Scholar]
- 24.Lubowitz JH, Brand JC, Rossi MJ. Hip Gluteus Medius and Minimus Endoscopic Treatment Results in Patient Satisfaction. Arthroscopy. 2020;36(11):2775–6. doi: 10.1016/j.arthro.2020.09.030. [DOI] [PubMed] [Google Scholar]
- 25.Nho SJ, Grzybowski JS, Bogunovic L, et al. Diagnosis, Evaluation, and Endoscopic Repair of Partial Articular Gluteus Tendon Avulsion. Arthrosc Tech. 2016;5(3):e425–31. doi: 10.1016/j.eats.2016.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gerber C, Meyer DC, Frey E, et al. Neer Award 2007: Reversion of structural muscle changes caused by chronic rotator cuff tears using continuous musculotendinous traction An experimental study in sheep. J shoulder Elb Surg. 2009;18(2):163–71. doi: 10.1016/j.jse.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 27.Chaudhury S, Dines JS, Delos D, Warren RF, Voigt C, Rodeo SA. Role of fatty infiltration in the pathophysiology and outcomes of rotator cuff tears. Arthritis Care Res (Hoboken). 2012;64(1):76–82. doi: 10.1002/acr.20552. [DOI] [PubMed] [Google Scholar]
- 28.Kuzel BR, Grindel S, Papandrea R, Ziegler D. Fatty infiltration and rotator cuff atrophy. J Am Acad Orthop Surg. 2013;21(10):613–23. doi: 10.5435/JAAOS-21-10-613. [DOI] [PubMed] [Google Scholar]
- 29.Melis B, Nemoz C, Walch G. Muscle fatty infiltration in rotator cuff tears: descriptive analysis of 1688 cases. Orthop Traumatol Surg Res. 2009;95(5):319–24. doi: 10.1016/j.otsr.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 30.Busse J, Gasteiger W, Tönnis D. [A new method for roentgenologic evaluation of the hip joint--the hip factor] Arch Orthop Unfallchir. 1972;72(1):1–9. doi: 10.1007/BF00415854. [DOI] [PubMed] [Google Scholar]
- 31.Kenanidis E, Kyriakopoulos G, Kaila R, Christofilopoulos P. Lesions of the abductors in the hip. EFORT open Rev. 2020;5(8):464–76. doi: 10.1302/2058-5241.5.190094. [DOI] [PMC free article] [PubMed] [Google Scholar]