Abstract
Background/Aim
Hepatic encephalopathy (HE) is a significant complication of acute and chronic liver disease. It is crucial for nurses to have knowledge of encephalopathy symptoms to enable prompt and effective responses when caring for such patients. Therefore, this study aimed to evaluate nurses’ HE knowledge in Najran hospitals in Saudi Arabia.
Methods
This cross-sectional analytical study was conducted with nurses at the Najran Hospital in Najran City, Saudi Arabia. The sample size was determined using Epi-Calc 2000, resulting in a final sample of 125 nurses from intensive care units (ICU), cardiac surgical ICU and pediatric ICU, and they were selected by convenience sampling technique. Data were collected using a self-administered questionnaire, and 125 nurses participated in knowledge assessment. The data were coded and entered into SPSS version 21.0 for descriptive and inferential statistics. Information letters and consent forms were obtained from all the participants.
Results
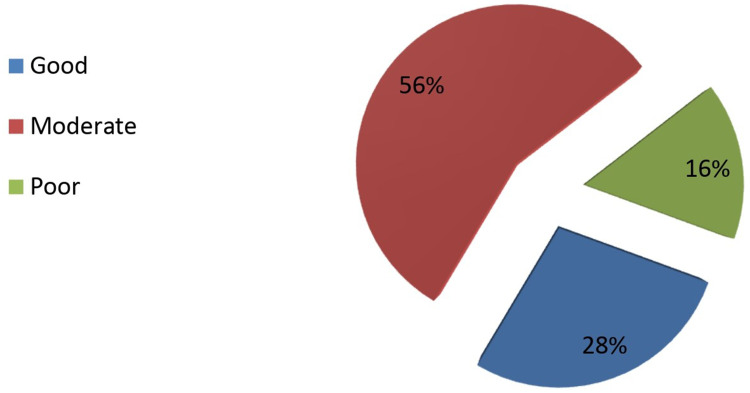
The majority of nurses (88.8%) were female, and 59.2% were married. The age range of participants was 20–30 years (50.4%). Approximately 36.8% had 4–6 years of work experience. The majority of the nurses (87.2%) held a bachelor’s degree. More than half (56%) of the nurses demonstrated moderate HE knowledge, whereas over a quarter (28%) exhibited good knowledge. There was a highly statistically significant association between marital status, level of education, nationality, and level of nurses’ knowledge regarding HE (P-value = 0.01, 0.02, and 0.02, respectively).
Conclusion
The study concludes that nurses in Najran hospitals have an adequate knowledge levels, ranging from moderate to good. This highlights the importance of tailored educational programs to enhance nurses’ understanding of HE symptoms and management. Furthermore, the marital status, education level, and nationality have significant association with nurses’ knowledge.
Keywords: hepatic encephalopathy, knowledge, Najran hospitals, nurses
Introduction
Hepatic encephalopathy (HE) stands as a substantial and intricate neurological complication arising from both acute and chronic liver diseases. It encompasses a range of neuropsychiatric abnormalities, varying from subtle cognitive deficits to severe manifestations, posing considerable challenges in patient care.1 The beginning is usually insidious and characterized by subtle and sometimes periodic changes in memory, cognition, associative higher intellectual functions, and altered personality.2
Nurses, positioned at the frontline of patient care, assume an indispensable role in the proactive identification and immediate intervention for HE.3 As the primary caregivers who maintain patient care, nurses are also responsible to observe the earliest signs of HE’s intricate neurological manifestations. Their daily interactions with patients foster an intimate understanding of their baseline cognitive and behavioral states, making them adept at detecting any deviations that could be indicative of HE deterioration.4,5
Nurses should be able to recognize the overdosing of some medications that metabolized in liver, because they may affect on pulmonary functions when used at higher doses. Bleeding in the digestive tract complicates further HE treatment, because proteins from the blood contribute to high levels of serum ammonia. Nurses should have the necessary work conditions and continuous education to enable effective and efficient care through nursing interventions and specific nursing care.6 Nurses need to know the symptoms of encephalopathy and, thus, be able to react promptly and adequately to taking care of such patients. HE can manifest acutely with a rapid deterioration of mental function leading to coma, with no previous symptomatology.7
Furthermore, nurses have the unique skills to provide holistic care that extends beyond medical management to the observation and diet of affected patients.8 Their expertise in building therapeutic association with patients and their families enables them to not only provide medical interventions but also offer emotional support and education.9–11 In the case of HE, where patients may experience confusion, altered consciousness, and mood changes, nurses’ empathetic communication can foster a sense of reassurance and facilitate patient cooperation in adhering to treatment plans.12,13
This study provides baseline information regarding nurses’ knowledge level in HE which is a critical aspect of cirrhosis management, including diet, over-the-counter medications, and important health maintenance activities, signs, and symptoms. Therefore, this study aimed to assess nurses’ HE knowledge levels in Najran hospitals, Saudi Arabia.
Methods
Study Design
This is a cross-sectional analytical study which was conducted to assess nurses’ knowledge toward HE in Najran hospitals, Najran, Saudi Arabia.
Study Setting
This study was conducted at Najran hospitals (King Khalid Hospital, Najran General Hospital and Najran University Hospital) that provide primary, secondary, and tertiary healthcare services. The nurses working in intensive care units (ICU), cardiac surgical ICU and pediatric ICU were included as they provide direct care for patients with HE.
Study Population
This study was conducted among nurses work at the Najran hospitals (King Khalid Hospital, Najran General Hospital and Najran University Hospital) at the period of data collection. Registered nurses with previous experience in the field of ICU, cardiac surgical ICU and pediatric ICU were included in this study. The nursing students or nurses’ managers were excluded from the study.
Sampling and Sample Size
A convenience sampling technique was used to include nurses working in the three Najran hospitals (King Khalid Hospital, Najran General Hospital and Najran University Hospital); the sample size was determined through the use of the EpiCalc program 2000, taking into consideration the following: precision (5%) and 95% confidence level. The final sample size calculated was 125 nurses working at the targeted departments.
Data Collection
The data was collected using a survey consisting of two parts: part I: demographic characteristics of nurses (11 questions); part II: knowledge toward HE which consists of causes, signs, medication, complications, and nursing care of HE (24 questions). The levels of knowledge were classified as follows: good level of the nurses’ knowledge who got 76%–100%, moderate knowledge 50–75% and poor knowledge 0%–49%. The questionnaire was distributed to nurses working in the hospitals at the time of data collection. The survey was distributed online to nurses in the hospitals’ units through WhatsApp while visiting the department. They were voluntarily responded to the invitation by 100% completion rate.
Data Collection Tool
The knowledge questionnaire was adopted from one previous study conducted by Ramachandran et al, 2020.14 The tool was tested on 15 nurses from Aseer region to assess its validity and reliability. The questionnaire was reviewed by two faculty members and a statistician to ensure accuracy and measurability. Cronbach’s alpha was 0.84 more that the acceptable level. The Content Validity Index (CVI) value of the tool was reviewed by experts, solidifying the tool’s relevance and appropriateness for measuring HE knowledge among targeted nurses.
Data Analysis
Data were analyzed using SPSS version 24. Descriptive analysis was performed for the demographic variables, and characteristics. The inferential test as Chi-square was used to test any association between knowledge levels with demographic characteristics of nurses.
Results
Table 1 provides a comprehensive overview of the demographic attributes of nurses operating within three prominent hospitals in Najran, namely King Khalid Hospital, Najran General Hospital, and University Hospital. The nurses work in the units including ICU, cardiac surgical ICU, and pediatric ICU. The nurses’ age distribution was between 20 and 50 years, and a notable portion (59%) were married, reflecting potential work-life equilibrium challenges. All nurses held a university education (100%), predominantly possessing bachelor’s degrees (87.2%) in nursing, highlighting their specialized training. The international composition of the nursing staff is evident, with 75% being non-Saudi nationals. While 27% received limited training in HE courses, 48.8% reported adherence to hospital policies in HE patient care.
Table 1.
Demographic Characteristics of Nurses from Three Hospitals in Najran City (N = 125)
| Demographic Characteristics | Frequency | Percentage |
|---|---|---|
| Hospitals | ||
|
100 | 80 |
|
20 | 16 |
|
5 | 4 |
| Department name | ||
|
55 | 44 |
|
31 | 24.8 |
|
39 | 31.2 |
| Gender | ||
|
14 | 11.2 |
|
111 | 88.8 |
| Marital status | ||
|
51 | 40.8 |
|
74 | 59.2 |
| Age (year) | ||
|
63 | 50.4 |
|
43 | 34.4 |
|
16 | 12.8 |
|
3 | 2.4 |
| Working experience (year) | ||
|
32 | 25.6 |
|
46 | 36.8 |
|
22 | 17.6 |
|
25 | 20 |
| Level of education | ||
|
11 | 8.8 |
|
109 | 87.2 |
|
5 | 4 |
| Nationality | ||
|
30 | 24 |
|
95 | 76 |
| Training course about HE | ||
|
27 | 24 |
|
98 | 76 |
| Written policy in caring for HE patients | ||
|
61 | 48.8 |
|
64 | 51.2 |
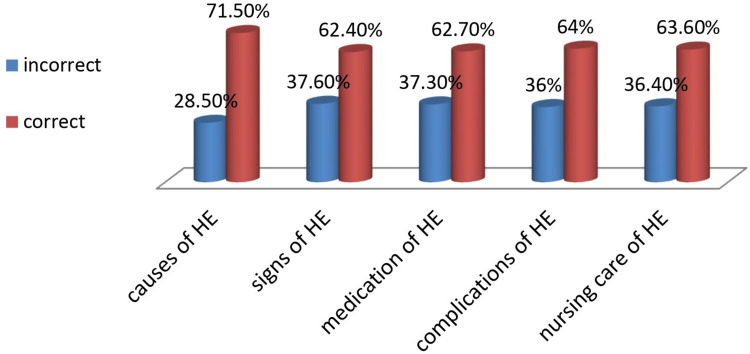
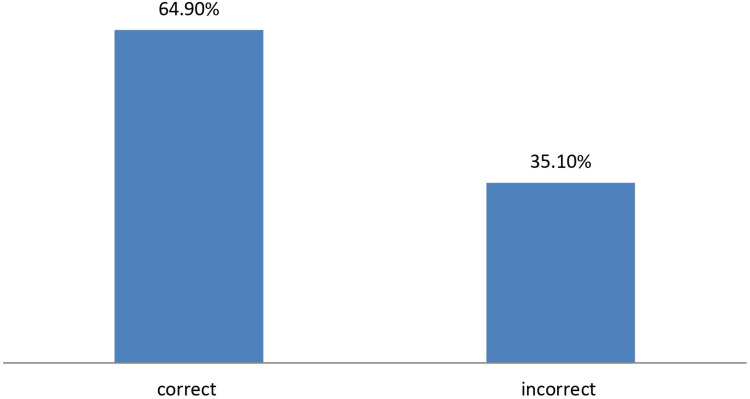
In Table 2, an insightful depiction of nurses’ comprehension regarding the stages of HE disease is presented. Around two-thirds of nurses exhibited awareness of the disease itself (71.5%), showcasing a foundational grasp of the concept. Over half of the nurses demonstrated recognition of disease-specific signs (62.4%), indicating a substantial understanding of clinical indicators. Furthermore, a similar percentage displayed knowledge about the medications employed in HE management. Impressively, 64% of nurses showcased awareness of potential complications that could arise if the disease is left undetected and untreated, underlining a comprehensive understanding. Cumulatively, the nurses’ collective knowledge regarding HE disease stages was positive, with 64.9% demonstrating accurate comprehension, underscoring their adeptness in this critical aspect of patient care.
Table 2.
Overall Knowledge About of HE (N = 125)
| Items | Incorrect | Correct | Total | |||
|---|---|---|---|---|---|---|
| Frequency | Percentage | Frequency | Percentage | Frequency | Percentage | |
| Total of knowledge about causes of HE. | 214 | 28.5% | 536 | 71.5 | 750 | 100 |
| Total of knowledge about signs of HE. | 235 | 37.6 | 390 | 62.4 | 625 | 100 |
| Total of knowledge about medication of HE | 140 | 37.3% | 235 | 62.7% | 375 | 100% |
| Total of Knowledge about complications of HE | 135 | 36% | 240 | 64% | 375 | 100% |
| Total of knowledge about nursing care of HE | 591 | 36.4% | 1034 | 63.6% | 1625 | 100 |
| Total of knowledge | 1315 | 35.1% | 2435 | 64.9 | 3750 | 100 |
Figure 1 shows that all nurses have knowledge regarding HE disease in all stages from causes (71.5% a correct answer, while 28.5 in correct answers). About 62.4% had correct answers to the signs of disease, but 37.6% have correct answers. The same result about the importance of medications 62.7% has correct answers but 37.3% have incorrect answers. Lastly, nearly two thirds of participants were knowledgeable about HE disease (65%). Figure 2 explores knowledge of nurses about caring of HE patients from the hospitals (N = 125). Figure 3 shows the overall nurses’ knowledge regarding HE. It is shown that most of nurses are knowledgeable about caring of HE patients.
Figure 1.
The nurses’ knowledge on causes, signs, complications and nursing care of HE.
Figure 2.
Level of nurses’ knowledge on HE.
Figure 3.
Overall of nurses’ knowledge on HE.
Table 3 provides the association between demographic characteristics of nurses and their proficiency in comprehending HE. Meanwhile, no notable variations emerged based on hospital affiliations or gender. However, the association between knowledge and HE-specific training courses was not statistically significant. Age and years of experience did not yield significant correlations with HE knowledge levels. A significant association was reported between knowledge levels with marital status and education level. Married nurses and those holding bachelor’s degrees showed higher levels of knowledge.
Table 3.
Association Between Demographics and Characteristics of the Participants Nurses and Level of Knowledge Toward HE (N = 125)
| Demographic Data | Level of Knowledge | P-value | ||
|---|---|---|---|---|
| Good | Moderate | Poor | ||
| Hospitals | ||||
|
29 | 53 | 18 | 0.54 |
|
4 | 14 | 2 | |
|
2 | 3 | 0 | |
| Gender | ||||
|
4 | 9 | 1 | 0.61 |
|
31 | 61 | 19 | |
| Marital status | ||||
|
16 | 42 | 16 | 0.01* |
|
19 | 28 | 4 | |
| Age (years) | ||||
|
14 | 39 | 10 | 0.22 |
|
13 | 23 | 7 | |
|
8 | 5 | 3 | |
|
0 | 3 | 0 | |
| Working experience (years) | ||||
|
10 | 20 | 2 | 0.37 |
|
9 | 27 | 10 | |
|
6 | 12 | 4 | |
|
10 | 11 | 4 | |
| Level of education | ||||
|
2 | 6 | 3 | 0.02* |
|
32 | 60 | 17 | |
|
1 | 4 | 0 | |
| Nationality | ||||
|
5 | 16 | 12 | 0.02* |
|
30 | 54 | 8 | |
| Training course about HE | ||||
|
9 | 16 | 2 | 0.36 |
|
26 | 54 | 18 | |
| Written policy in caring for HE patients | ||||
|
21 | 34 | 6 | 0.10 |
|
14 | 36 | 14 | |
Note: *Significant.
Discussion
The nurses work in Najran hospitals (King Khalid Hospital, Najran General Hospital, and University Hospital) participated in the study, and their age distribution was between 20 and 50 years, which is consistent with many studies conducted on nurses in Saudi hospitals15 and other countries;16 furthermore, a notable portion (59%) were married, reflecting potential work-life equilibrium challenges.
This study examined nurses’ knowledge regarding HE in Najran hospitals, Saudi Arabia. The findings of this study showed that the participants demonstrated a good level of knowledge regarding the HE. These findings are consistent with the findings of other studies conducted on nurses17,18 that demonstrated that the majority of nurses had good knowledge about liver and HE.
On the other hand, this is inconsistent with the study conducted by Sohal et al, 2021, who reported a gap in level of nurses’ knowledge toward HE care.19 Additionally, the findings showed that an affirmative positive demonstrated a moderate level of knowledge regarding the medication of HE between the participants, as well as international studies regarding current vision on diagnosis and comprehensive care in HE.20 They showed in their extensive search that nurses had good knowledge of the different types of treatment. In addition, Sohal et al,19 identified areas of improvement in nursing knowledge regarding HE management, found in the largest survey that has been performed to identify inpatient nursing knowledge regarding HE management. Although most nurses are able to recognize worsening, HE symptoms, many are unaware that ammonia is the culprit toxin. Nearly 70% of nurses wanted to up titrate lactulose without adding rifaximin in the cases of decreased bowel movements, which shows that knowledge regarding the combination therapy can be improved.
This study revealed significant statistical differences in the association between the demographic characteristics of the nurses and their level of knowledge toward HE, especially marital status, level of education, and nationality. This could be justified by the fact that the nurses received appropriate education during their study at the college. This finding is similar to Ahmed’s (2018) study nurses’ ability to care for patients with HE, which showed that the level of education of nurses who had graduated from nursing institutes as a factor influencing their level of knowledge.21 However, these levels of knowledge in Saudi Arabia are expected when compared to the total government expenses of the health care and educational delivery system and the training programs the nurses received.
However, while the study reveals valuable insights, it also bears certain limitations. The cross-sectional design restricts the ability to establish causality. Moreover, relying on self-reported knowledge might introduce response bias, and the inclusion of only Najran hospitals limits the generalizability to other regions. Despite these limitations, the analysis sheds light on the intricate interplay between demographic attributes and HE knowledge among nurses, offering directions for targeted educational interventions and policy enhancements.
Conclusion
In conclusion, this study revealed an adequate knowledge levels among the nurses in Najran hospitals, ranging from moderate to good. This highlights the importance of tailored educational programs to enhance nurses’ understanding of HE symptoms and management. Furthermore, the marital status, education level, and nationality have significant association with nurses’ knowledge. These insights emphasize the need for targeted interventions that consider these factors to effectively improve HE-related patient care.
Acknowledgments
The authors are thankful to the Deanship of Scientific Research at Najran University for funding this work under the Research Priorities and Najran Research Funding Program. Grant code (NU/NAR/MRC/11/8).
Funding Statement
The project was funded by the Ministry of Education and the Deanship of Scientific Research at Najran University, Saudi Arabia, for funding the project: Najran Research Funding program. Grant code (NU/NAR/MRC/11/8).
Data Sharing Statement
The datasets generated and analyzed during this study are not publicly available because of data privacy but are available from the corresponding author upon reasonable request.
Ethics Approval and Consent to Participate
Ethical approval was obtained from the Health Affairs in Najran (Nurses’ Knowledge Regarding HE in Najran hospitals in Najran City-KSA. Reference No.:443-437-32417-DS). The project was primarily approved by the Research Ethics Committee, Najran University, with approval number 443-437-32417-DS on 30 December 2022. The nurses provided agreement and written consents before their participation in this study.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Rose CF, Amodio P, Bajaj JS, et al. Hepatic encephalopathy: novel insights into classification, pathophysiology and therapy. J Hepatol. 2020;73(6):1526–1547. doi: 10.1016/j.jhep.2020.07.013 [DOI] [PubMed] [Google Scholar]
- 2.Milovanovic T, Pantic I, Velickovic J, et al. Bacteremia in patients with liver cirrhosis in the era of increasing antimicrobial resistance: single-center epidemiology. J Infect Dev Ctries. 2021;15(12):1883–1890. doi: 10.3855/jidc.14508 [DOI] [PubMed] [Google Scholar]
- 3.Künzler‐Heule P, Beckmann S, Mahrer‐Imhof R, Semela D, Händler‐Schuster D. Being an informal caregiver for a relative with liver cirrhosis and overt hepatic encephalopathy: a phenomenological study. J Clin Nurs. 2016;25(17–18):2559–2568. doi: 10.1111/jocn.13298 [DOI] [PubMed] [Google Scholar]
- 4.KAftSot L. KASL clinical practice guidelines for liver cirrhosis: varices, hepatic encephalopathy, and related complications. Clin Mol Hepatol. 2020;26(2):83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shrestha D, Rathi S, Grover S, et al. Factors affecting psychological burden on the informal caregiver of patients with cirrhosis: looking beyond the patient. J Clin Exp Hepatol. 2020;10(1):9–16. doi: 10.1016/j.jceh.2019.06.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rice J, Dodge JL, Bambha KM, et al. Neutrophil-to-lymphocyte ratio associates independently with mortality in hospitalized patients with cirrhosis. Clin Gastroenterol Hepatol. 2018;16(11):1786–91. e1. doi: 10.1016/j.cgh.2018.04.045 [DOI] [PubMed] [Google Scholar]
- 7.Tapper EB, Kanwal F, Asrani SK, et al. Patient‐reported outcomes in cirrhosis: a scoping review of the literature. Hepatology. 2018;67(6):2375–2383. doi: 10.1002/hep.29756 [DOI] [PubMed] [Google Scholar]
- 8.de Campos AP, Levoy K, Pandey S, et al. Integrating palliative care into nursing care. Am J Nurs. 2022;122(11):40. doi: 10.1097/01.NAJ.0000897124.77291.7d [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Munkombwe WM, Petersson K, Elgán C. Nurses’ experiences of providing nonpharmacological pain management in palliative care: a qualitative study. J Clin Nurs. 2020;29(9–10):1643–1652. doi: 10.1111/jocn.15232 [DOI] [PubMed] [Google Scholar]
- 10.McQueen A. Nurse–patient relationships and partnership in hospital care. J Clin Nurs. 2000;9(5):723–731. doi: 10.1046/j.1365-2702.2000.00424.x [DOI] [Google Scholar]
- 11.Legg MJ. What is psychosocial care and how can nurses better provide it to adult oncology patients. Aust J Adv Nurs. 2011;28(3):61–67. [Google Scholar]
- 12.Bajaj JS, Gentili A, Wade JB, Godschalk M. Specific challenges in geriatric cirrhosis and hepatic encephalopathy. Clin Gastroenterol Hepatol. 2022;20(8):S20–S9. doi: 10.1016/j.cgh.2022.04.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vlaisavljevic Z, Rankovic I. Specific nursing care rendered in hepatic encephalopathy: contemporary review and new clinical insights. J Nurs Care. 2015;4(264):2167–1168.1000264. [Google Scholar]
- 14.Ramachandran J, Woodman RJ, Muller KR, et al. Validation of knowledge questionnaire for patients with liver cirrhosis. Clin Gastroenterol Hepatol. 2020;18(8):1867–73. e1. doi: 10.1016/j.cgh.2019.11.045 [DOI] [PubMed] [Google Scholar]
- 15.Ahmed WAM. Anxiety and related symptoms among critical care nurses in Albaha, Kingdom of Saudi Arabia. AIMS Med Sci. 2015;2(4):303–309. doi: 10.3934/medsci.2015.4.303 [DOI] [Google Scholar]
- 16.Ahmed WAM, Eltayeb M, Abd-Elsalam NA-E. Invasive haemodynamic monitoring at critical care units in Sudan: assessment of nurses’ performance. J Health Specialties. 2016;4(3):196. doi: 10.4103/2468-6360.186493 [DOI] [Google Scholar]
- 17.Eldosokey AAE, Mohammed HAB Effect of educational guideline on nurses’ knowledge regarding patients with minimal hepatic encephalopathy Mansoura Nursing Journal. 2017;8(1):111–126. doi: 10.21608/mnj.2017.176414 [DOI] [Google Scholar]
- 18.Bager P. The assessment and care of patients with hepatic encephalopathy. Br J Nurs. 2017;26(13):724–729. doi: 10.12968/bjon.2017.26.13.724 [DOI] [PubMed] [Google Scholar]
- 19.Sohal A, Green V, Sandhu S, Roytman M. Identifying areas of improvement in nursing knowledge regarding hepatic encephalopathy management. J Community Hosp Intern Med Perspect. 2021;11(5):722–726. doi: 10.1080/20009666.2021.1954784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Miela RJ, Cubała WJ, Jakuszkowiak-Wojten K, Mazurkiewicz DW. Pharmacotherapy of alcohol use disorder. A review of current literature. Biol Psychiatry Psychopharmacol. 2018;20(1):2. [Google Scholar]
- 21.Ahmed EA Nurses’ performance regarding management of patients with Hepatic encephalopathy. 2018.