Highlights
-
•
In urban counties, medicaid expansion was associated with a reduction in income-related buprenorphine (BUP) disparities.
-
•
In rural counties, there was no evidence of an association between medicaid expansion and income-related BUP disparities.
-
•
Future policies targeting low-income rural areas may be needed to achieve more equitable BUP access.
Keywords: Buprenorphine, Opioid use disorder, Medicaid expansion, Rural, Income, Disparities
Abstract
Background
Although use of buprenorphine for treating opioid use disorder increased over the past decade, buprenorphine utilization remains limited in lower-income and rural areas. We examine how the Affordable Care Act Medicaid expansion influenced buprenorphine initiation rates by county income and evaluate how associations differ by county rural-urban status.
Methods
This study used nationwide 2009–2018 IQVIA retail pharmacy data and a comparative interrupted time series framework–a hybrid framework combining regression discontinuity and difference-in-difference approaches. We used piecewise linear estimation to quantify changes in buprenorphine initiation rates before and after Medicaid expansion.
Results
The sample included observations from 376,704 county-months. We identified 5,227,340 new buprenorphine treatment episodes, with an average of 9.2 new buprenorphine episodes per month per 100,000 county residents. Among urban counties, those with the lowest median incomes experienced significantly larger increases in buprenorphine initiation rates associated with Medicaid expansion than counties with higher median incomes (5-year rates difference est=3525.3, se=1695.3, p = 0.04). However, among rural counties, there was no significant association between buprenorphine initiation rates and county median income after Medicaid expansion (5-year rates difference est=979.0, se=915.8, p = 0.29).
Conclusions
Medicaid expansion was associated with a reduction in income-related buprenorphine disparities in urban counties, but not in rural counties. To achieve more equitable buprenorphine access, future policies should target low-income rural areas.
1. Introduction
The U.S. opioid crisis continues its relentless evolution (Humphreys et al., 2022). In 2022 alone, around 80,000 Americans died of an opioid overdose (NCHS, 2023). Although methadone, buprenorphine, and extended-release naltrexone are effective medications for treating opioid use disorder (OUD), only 3 in 10 people who need treatment receive it (Ahrnsbrak et al., 2017). Buprenorphine, one of these FDA-approved medications to treat OUD, has been shown to decrease the likelihood of opioid overdose death by up to 50 % (Sordo et al., 2017). But despite recent growth in buprenorphine use (Olfson et al., 2020), not all populations have comparable access. Black individuals are less likely to receive buprenorphine than White individuals, and residents of rural counties and counties with lower median household income have lower rates of utilization than residents of urban counties and counties with higher median income, respectively (Andrilla et al., 2019; Hansen et al., 2016; Lister et al., 2020; Stein et al., 2018).
Low-income individuals and rural residents face numerous barriers to accessing buprenorphine treatment (Andrilla et al., 2019; Hansen et al., 2016; Lister et al., 2020). For example, buprenorphine treatment for a single patient may cost up to $6000 annually, a cost shared by patient and insurer (Jones et al., 2009; NIDA, 2021). As a result, buprenorphine treatment for OUD is often cost-prohibitive for the uninsured; and cost is a commonly cited barrier to OUD medication treatment (Hall et al., 2021). Rural communities often have substantial shortages of buprenorphine prescribers (Andrilla et al., 2019; Lister et al., 2020, 2020; Rosenblatt et al., 2015; Stein et al., 2018), often requiring rural residents to travel longer distances to access treatment than urban residents (Saloner et al., 2022). Lower-income communities also tend to have fewer buprenorphine providers than higher-income communities (Knudsen, 2015; Lister et al., 2020; Stein et al., 2015).
The federal Patient Protection and Affordable Care Act (ACA) of 2014 expanded Medicaid coverage for low-income families with incomes up to 138 % of the federal poverty level. Half of U.S. states chose to implement Medicaid expansion in January 2014. Studies suggest that expansion contributed to increased use of buprenorphine treatment among Medicaid populations in expansion states (Knudsen et al., 2022; Meinhofer and Witman, 2018; Olfson et al., 2021; Saloner et al., 2018; Sharp et al., 2018; Wen et al., 2017), although overall, some of these gains were offset by decreases in other populations (e.g., commercially insured, Medicare, uninsured) (Knudsen et al., 2022; Meinhofer and Witman, 2018; Olfson et al., 2021). Given that Medicaid expansion resulted in larger insurance coverage gains for lower-income groups (Courtemanche et al., 2019), Medicaid expansion may have increased buprenorphine utilization more for lower-income versus higher-income populations. This hypothesis has yet to be examined empirically.
Medicaid expansion also appears to have impacted health care coverage and utilization outcomes differently in rural and urban communities (Benitez and Seiber, 2018; Cole et al., 2018; Kaufman et al., 2016; Mandal, 2022). Medicaid expansion led to greater reductions in the likelihood that low-income rural residents were uninsured, compared with low-income urban residents (Benitez and Seiber, 2018; Mandal, 2022). Expansion was also associated with increased likelihood of routine medical check-ups and improved quality and increased volume of several types of health care services for rural, but not urban, residents (Cole et al., 2018; Mandal, 2022). Of particular relevance, Medicaid expansion was associated with substantial increases in the volume of visits for substance use treatment in rural, but not urban, settings (Cole et al., 2018).
However, we are unaware of studies examining how Medicaid expansion affected buprenorphine utilization by county income and assessing whether this effect differed in rural versus urban communities. To address this gap, we used ten years of national pharmacy data (2009–2018) to assess whether and to what extent Medicaid expansion is related to initiation of buprenorphine treatment, by county income and rurality. Given Medicaid expansion resulted in larger insurance coverage gains for lower-income individuals (Courtemanche et al., 2019), we hypothesized expansion would be associated with greater increases in buprenorphine utilization among counties with median household income in the lowest quartile. We also hypothesized Medicaid expansion would be associated with greater increases in buprenorphine initiation rates in lowest-income rural counties versus lowest-income urban counties, given insurance coverage gains attributable to Medicaid expansion were greater among low-income rural residents compared to low-income urban residents (Benitez and Seiber, 2018; Mandal, 2022).
2. Methods
2.1. Data
We used pharmacy claims from IQVIA Longitudinal Prescriptions Claims (IQVIA Real World Data – Longitudinal Prescriptions, 2006–2018) from 2008 to 2018. These de-identified data include information about the dispensed buprenorphine prescription (e.g., dose, days supply), payer, patient demographics (e.g., sex, age cohort), and prescriber (e.g., prescriber county, specialty), capturing approximately 74 % of prescriptions filled at retail pharmacies in 2006 increasing to approximately 92 % of prescriptions filled at retail pharmacies in 2018. The study was approved by the RAND IRB with a waiver of consent.
2.2. Variables
Buprenorphine Treatment Initiation Rate. The outcome was buprenorphine treatment initiation rate by county-month, operationalized as the monthly number of new buprenorphine episodes per 100,000 county residents. To create buprenorphine episodes, we identified individuals with one or more dispensed buprenorphine prescriptions between 2009 and 2018, using 2008 data to ensure episodes occurring in 2009 were new. Consistent with prior studies (Harrison et al., 2022; Stein et al., 2021, 2021), we defined episodes as starting with the date of the first observed fill of a prescription for a buprenorphine formulation with an FDA-approved indication for OUD treatment, after a 30-day period with no days’ supply from a previously dispensed buprenorphine prescription. The episode ended with the last days’ supply of buprenorphine for the last dispensed buprenorphine prescription, with no more than a 30-day gap in the patient having a supply of buprenorphine.
We aggregated buprenorphine episodes by county-month based on the episode's start date. We assigned the buprenorphine episode to the prescriber of the episode's first dispensed prescription, and we used the 5-digit Federal Information Processing Standards (FIPS) code of the episode's prescriber to determine the county in which the episode occurred. Annual county population estimates were obtained from the Census Bureau's American Community Survey (American Community Survey, 2006–2018). We calculated buprenorphine treatment initiation rates by dividing the number of new buprenorphine episodes each month by the county population and multiplying by 100,000.
County Characteristics. Using the Rural-Urban Continuum Codes (RUCC) from the Area Health Resources Files (AHRF) (Rural-Urban Continuum Codes, 2013), we categorized counties as “urban” (RUCC categories 1–3) or “rural” (RUCC categories 4–9) (Adu et al., 2019; Luo et al., 2021; Okwori et al., 2022; Owen et al., 2007). We also obtained median household income for each county from the AHRF; we derived the county proportion of non-Hispanic White residents from the American Community Survey (American Community Survey, 2006–2018). County fatal overdose rates were identified from the Centers for Disease Control and Prevention's multiple-cause-of-death mortality file (Multiple Cause of Death Data, 2006–2018). We relied on data from the Kaiser Family Foundation to identify each state's Medicaid expansion status (Status of State Action on the Medicaid Expansion Decision, 2021). We grouped county median household income, proportion of non-Hispanic White residents, and fatal overdose rates into time-variant quartiles.
2.3. Analytic approach
We first calculated descriptive statistics, including unadjusted rates of average buprenorphine treatment initiation overall and by county characteristics and year. We found little difference between county income quartiles 2–4 (higher-income counties), so in the remaining analyses, we grouped them and compared the result to county income quartile 1 (lowest-income counties).
We next examined if the association between Medicaid expansion and buprenorphine initiation rates differed by county income and urban-rural status. We conducted three multivariable regressions, using a comparative interrupted time series framework–a hybrid framework that combines regression discontinuity design and difference-in-difference approaches. The comparative interrupted time series models incorporate calendar time indicators (i.e., trends) similar to regression discontinuity design and compare trends from pre versus post periods similar to difference-in-difference designs (Perera et al., 2022). The first regression included interactions between calendar month, Medicaid expansion status, and binary county income status to examine whether the association between Medicaid expansion and rates of buprenorphine initiation differed by county income. To examine whether the association between Medicaid expansion, county income, and buprenorphine initiation rates differed in rural and urban communities, we re-calculated the first regression, stratified by rural-urban status. The second model included only urban counties; the third model included only rural counties.
All models included state fixed effects, and we calculated cluster robust standard errors to account for county-level serial correlation. Standard errors were clustered at the state level. Models also controlled for county proportion of non-Hispanic White residents and fatal overdose rates. In all models, the outcome variable was county-month rate of buprenorphine treatment initiation. Using January 2009 as the referent, our estimates reflect differences from the beginning of 2009, and estimates can be negative or positive. We divided the study timeline into two periods: 60 months before and 60 months after January 2014. We used piecewise linear estimation to quantify the 5-year change between pre- and post- periods, testing differences in area under the curve between the observed post-expansion lines versus the expected post-expansion lines for the county income groups.
Last, we conducted a sensitivity analysis. Although most expansion states adopted Medicaid expansion in 2014, some states (Pennsylvania, Indiana, Alaska, Montana, and Louisiana) implemented it between 2015 and 2018. In our main analyses, we grouped these “late adopters” with states that expanded Medicaid in 2014. The sensitivity analysis explored how model estimates changed when we excluded late adopters. We used SAS 9.4 for all analyses (SAS Institute Inc., Cary, NC, USA).
3. Results
3.1. Descriptive statistics
We identified 5227,340 new buprenorphine treatment episodes from 2009 through 2018, with an average monthly rate of buprenorphine treatment initiation per 100,000 county population of 9.2 (Table 1). Average rates increased steadily between 2009 and 2018. Rates were higher among counties in expansion states versus non-expansion states; urban counties versus rural counties; and counties in the lowest-income quartile versus counties in higher-income quartiles.
Table 1.
Unadjusted Buprenorphine Episode Initiation per 100,000 County Residents per Month, 2009–2018*.
| N (county-months) | Mean | 95 % Confidence Interval | |
|---|---|---|---|
| Total | 376,704 | 9.17 | (9.09, 9.25) |
| Medicaid Expansion Status | |||
| Expansion state | 179,652 | 11.31 | (11.17, 11.45) |
| Non-expansion state | 197,052 | 7.22 | (7.13, 7.31) |
| Median Household Income | |||
| Q1 (Lowest) | 93,900 | 10.95 | (10.71, 11.18) |
| Q2 | 94,260 | 8.72 | (8.56, 8.88) |
| Q3 | 94,332 | 7.49 | (7.38, 7.61) |
| Q4 (Highest) | 94,212 | 9.52 | (9.40, 9.63) |
| Rural-Urban Status | |||
| Urban | 139,824 | 12.01 | (11.89, 12.13) |
| Rural | 236,880 | 7.49 | (7.38, 7.60) |
| Percent non-Hispanic White | |||
| Q1 (Lowest) | 93,852 | 7.47 | (7.36, 7.56) |
| Q2 | 94,320 | 9.93 | (9.81, 10.06) |
| Q3 | 94,320 | 9.75 | (9.58, 9.93) |
| Q4 (Highest) | 94,212 | 9.52 | (9.29, 9.75) |
| Fatal Overdose Rate (1-Year Lag) | |||
| Q1 (Lowest) | 97,344 | 3.13 | (3.01, 3.25) |
| Q2 | 90,852 | 7.77 | (7.65, 7.89) |
| Q3 | 94,308 | 10.51 | (10.35, 10.67) |
| Q4 (Highest) | 94,200 | 15.42 | (15.19, 15.65) |
| Year | |||
| 2009 | 37,692 | 5.40 | (5.24, 5.56) |
| 2010 | 37,668 | 5.71 | (5.55, 5.87) |
| 2011 | 37,668 | 7.08 | (6.88, 7.27) |
| 2012 | 37,668 | 7.71 | (7.50, 7.92) |
| 2013 | 37,668 | 8.67 | (8.42, 8.91) |
| 2014 | 37,668 | 9.58 | (9.31, 9.84) |
| 2015 | 37,668 | 9.98 | (9.72, 10.24) |
| 2016 | 37,668 | 10.75 | (10.46, 11.05) |
| 2017 | 37,668 | 12.50 | (12.14, 12.85) |
| 2018 | 37,668 | 14.31 | (13.95, 14.67) |
Dispensed buprenorphine data derived from IQVIA Longitudinal Prescription Claims (LRx) between 2006 and 2018, which tracks individual's prescriptions over time. Longitudinal data derives from electronic data received from pharmacies, payers, software providers, and transactional clearinghouses.
3.2. Association between medicaid expansion and buprenorphine initiation rates by county income
We first examined the association between Medicaid expansion and buprenorphine initiation trends differed by county income. Table 2 shows the estimated differences between observed and expected buprenorphine initiation trends for counties in the lowest-income and higher-income quartiles after policy implementation. Among counties in higher-income quartiles, we observed 89.9 more buprenorphine episodes initiated per 100,000 residents over the 5-year, post-policy implementation period than expected (se: 274.5; p = 0.74), based on pre-policy implementation trends. In contrast, among counties in the lowest-income quartile, we observed 1984.2 more buprenorphine episodes initiated per 100,000 residents over the 5-year, post-policy implementation period than expected (se: 993.4, p = 0.05).
Table 2.
Piecewise Linear Estimation Estimates for Models 1–3.
| Average County Income, Quartile | Jan 2009 - Dec 2013 |
Jan 2014 - Dec 2018 |
Difference between Pre and Post Periods |
||||
|---|---|---|---|---|---|---|---|
| Est. | SE | Est. | SE | Est. | SE | p | |
| MODEL 1: ALL COUNTIES | |||||||
| Lowest-Income (Q1) | |||||||
| Observed | 166.9 | 129.0 | 2479.5 | 1132.7 | 2312.5 | 1072.6 | 0.036 |
| Expected | n/a | n/a | 495.3 | 382.7 | 328.3 | 253.7 | 0.202 |
| Observed - Expected | 1984.2 | 993.4 | 0.051* | ||||
| Higher-Income (Q2–4) | |||||||
| Observed | −7.8 | 38.8 | 66.6 | 286.3 | 74.4 | 277.1 | 0.789 |
| Expected | n/a | n/a | −23.2 | 115.1 | −15.4 | 76.3 | 0.841 |
| Observed - Expected | 89.8 | 274.5 | 0.745 | ||||
| MODEL 2: URBAN COUNTIES ONLY | |||||||
| Lowest-Income (Q1) | |||||||
| Observed | 66.8 | 170.1 | 3723.5 | 1970.6 | 3656.7 | 1867.1 | 0.056 |
| Expected | n/a | n/a | 198.2 | 504.7 | 131.4 | 334.7 | 0.696 |
| Observed - Expected | 3525.3 | 1695.3 | 0.043⁎⁎ | ||||
| Higher-Income (Q2–4) | |||||||
| Observed | −4.5 | 41.0 | −15.6 | 294.5 | −11.1 | 283.3 | 0.969 |
| Expected | n/a | n/a | −13.3 | 121.7 | −8.8 | 80.7 | 0.913 |
| Observed - Expected | −2.3 | 278.1 | 0.994 | ||||
| MODEL 3: RURAL COUNTIES ONLY | |||||||
| Lowest-Income (Q1) | |||||||
| Observed | 214.1 | 189.1 | 1614.3 | 1332.5 | 1400.2 | 1178.7 | 0.241 |
| Expected | n/a | n/a | 635.3 | 561.1 | 421.2 | 372.0 | 0.263 |
| Observed - Expected | 979.0 | 915.8 | 0.291 | ||||
| Higher-Income (Q2–4) | |||||||
| Observed | −69.1 | 66.0 | 561.8 | 483.3 | 630.9 | 490.2 | 0.205 |
| Expected | n/a | n/a | −136.0 | 129.8 | 0.300 | ||
| Observed - Expected | 767.0 | 528.2 | 0.153 | ||||
p < 0.05,.
p < 0.10
Note: Models control for county proportion of non-Hispanic White residents and fatal overdose rates. Dispensed buprenorphine data derived from IQVIA Longitudinal Prescription Claims (LRx) between 2006 and 2018, which tracks individual's prescriptions over time. Longitudinal data derives from electronic data received from pharmacies, payers, software providers, and transactional clearinghouses.
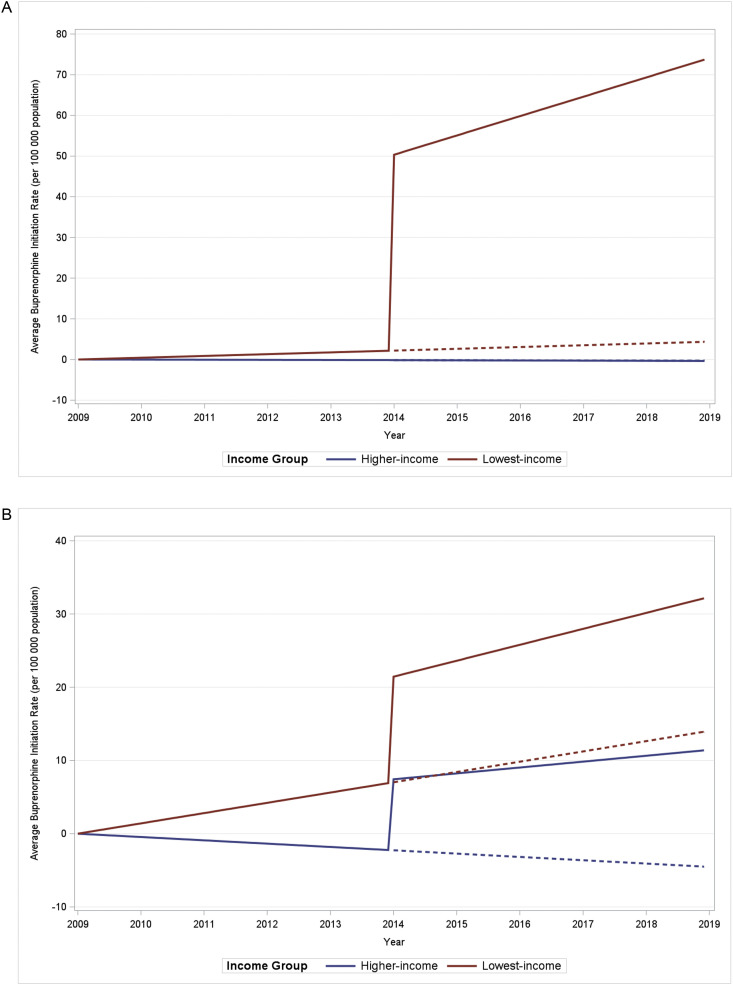
Fig. 1 illustrates the association between Medicaid expansion and buprenorphine initiation rates by county income, controlling for proportion of non-Hispanic White residents and fatal overdose rate. Compared to January 2009 model estimates, the difference in average buprenorphine initiation rates between counties in expansion states versus non-expansion states increased instantaneously and sharply after January 2014 (i.e., Medicaid expansion implementation) and also at a faster pace among counties in the lowest-income quartile, compared to counties in higher-income quartiles.
Fig. 1.
All Counties: Association Between ACA Medicaid Expansion and Buprenorphine Initiation Rates by County Income. This figure illustrates the first regression model, estimating the association between Medicaid expansion and buprenorphine initiation rates by county income, controlling for county proportion of non-Hispanic white residents and fatal overdose rate. Results show relative changes from the referent period (January 2009) by Medicaid expansion status. Solid lines are predictions using our model. Dashed lines are predictions using our model as if no policy was implemented. Dispensed buprenorphine data derived from 2006 to 2018 IQVIA Longitudinal Prescription Claims (LRx).
3.3. Association between medicaid expansion and buprenorphine initiation rates by county income in urban counties
In the second regression, we examined how the association between Medicaid expansion and buprenorphine initiation trends differed by county income in urban counties. The difference in average initiation rates between counties in expansion states versus non-expansion states increased instantaneously and sharply after Medicaid expansion. The increase occurred at a faster pace among counties in the lowest-income quartile, compared to counties in higher-income quartiles (Fig. 2A), and the gap between observed and expected buprenorphine initiation rates was larger in the lowest-income urban counties, compared to all lowest-income counties (Fig. 1).
Fig. 2.
A. Urban Counties: Association Between ACA Medicaid Expansion and Buprenorphine Initiation Rates by County Income. Caption: This figure illustrates the second regression model, estimating the association between Medicaid expansion and buprenorphine initiation rates by county income in urban counties, controlling for county proportion of non-Hispanic White residents and fatal overdose rate. Results show relative changes from the referent period (January 2009) by Medicaid expansion status. Solid lines are predictions using our model. Dashed lines are predictions using our model as if no policy was implemented. Dispensed buprenorphine data derived from 2006 to 2018 IQVIA Longitudinal Prescription Claims (LRx).
B. Rural Counties: Association Between ACA Medicaid Expansion and Buprenorphine Initiation Rates by County Income. This figure illustrates the third regression model, estimating the association between Medicaid expansion and buprenorphine initiation rates by county income in rural counties, controlling for county proportion of non-Hispanic White residents and fatal overdose rate. Results show relative changes from the referent period (January 2009) by Medicaid expansion status. Solid lines are predictions using our model. Dashed lines are predictions using our model as if no policy was implemented. Dispensed buprenorphine data derived from 2006 to 2018 IQVIA Longitudinal Prescription Claims (LRx).
Among urban counties in higher-income quartiles, we observed 2.3 fewer buprenorphine episodes initiated per 100,000 residents over the 5-year, post-policy implementation period than expected (se: 278.1; p>0.99). Among urban counties in the lowest-income quartile, we observed 3525.3 more buprenorphine episodes initiated per 100,000 residents over the 5-year, post-policy implementation period than expected based on pre-policy implementation trends (se: 1695.3, p = 0.04).
3.4. Association between medicaid expansion and buprenorphine initiation rates by county income in rural counties
The third model examined how the association between Medicaid expansion and buprenorphine initiation trends differed by county income only in rural counties. The difference in average buprenorphine initiation rates between counties in expansion states versus non-expansion states increased at a similar pace after Medicaid expansion among counties in the lowest-income quartile, compared to counties in higher-income quartiles (Fig. 2B). Also, the gap between observed and expected buprenorphine initiation rates in lowest-income rural counties was smaller, not statistically significant, and similar in size to that of higher-income rural counties.
Among rural counties in higher income quartiles, we observed 767.0 more buprenorphine episodes initiated per 100,000 residents over the 5-year, post-policy implementation period than expected (se: 528.2; p = 0.15). Among rural counties in the lowest-income quartile, we observed 979.0 more buprenorphine episodes initiated per 100,000 residents over the 5-year, post-policy implementation period than expected based on pre-policy implementation trends (se: 915.8, p = 0.29).
3.5. Sensitivity analysis
The sensitivity analysis explored whether findings were sensitive to excluding “late adopters” (i.e., states that implemented Medicaid expansion between 2015 and 2018). Table 3 shows the results of this analysis for both urban and rural counties, urban counties only, and rural counties only. In general, these analyses suggest that Medicaid expansion had stronger effects on buprenorphine initiation rates among states that expanded Medicaid in 2014, compared to effects found in the main analysis, which included “late adopters” in expansion states. The sensitivity analysis also showed significant effects of Medicaid expansion on buprenorphine initiation rates (including both rural and urban counties). Specifically, among counties in the lowest-income quartile, we observed 2703.1 more buprenorphine episodes initiated per 100,000 residents over the 5-year, post-policy implementation period than expected, based on pre-policy implementation trends (se: 1062.8, p = 0.01).
Table 3.
Sensitivity Analysis (Excluding Late Adopters) Piecewise Linear Estimation Estimates.
| Average County Income, Quartile | Jan 2009 - Dec 2013 |
Jan 2014 - Dec 2018 |
Difference between Pre and Post Periods |
||||
|---|---|---|---|---|---|---|---|
| Est. | SE | Est. | SE | Est. | SE | p | |
| SENSITIVITY ANALYSIS A: ALL COUNTIES | |||||||
| Lowest-Income (Q1) | |||||||
| Observed | 161.8 | 159.5 | 3183.1 | 1281.3 | 3021.3 | 1191.3 | 0.015 |
| Expected | n/a | n/a | 480.0 | 473.2 | 318.2 | 313.7 | 0.316 |
| Observed - Expected | 2703.1 | 1062.8 | 0.015⁎⁎ | ||||
| Higher-Income (Q2–4) | |||||||
| Observed | −24.9 | 39.6 | −21.0 | 300.1 | 3.9 | 291.5 | 0.990 |
| Expected | n/a | n/a | −73.9 | 117.6 | −49.0 | 78.0 | 0.533 |
| Observed - Expected | 52.9 | 290.2 | 0.856 | ||||
| SENSITIVITY ANALYSIS B: URBAN COUNTIES ONLY | |||||||
| Lowest-Income (Q1) | |||||||
| Observed | 60.0 | 230.0 | 4587.2 | 2479.2 | 4527.2 | 2302.8 | 0.056 |
| Expected | n/a | n/a | 178.1 | 682.4 | 118.1 | 452.4 | 0.795 |
| Observed - Expected | 4409.1 | 1988.0 | 0.032⁎⁎ | ||||
| Higher-Income (Q2–4) | |||||||
| Observed | −30.2 | 40.5 | −114.0 | 303.9 | −83.8 | 292.3 | 0.776 |
| Expected | n/a | n/a | −89.7 | 120.1 | −59.4 | 79.6 | 0.459 |
| Observed - Expected | −24.4 | 285.4 | 0.932 | ||||
| SENSITIVITY ANALYSIS C: RURAL COUNTIES ONLY | |||||||
| Lowest-Income (Q1) | |||||||
| Observed | 188.5 | 220.6 | 2300.3 | 1467.2 | 2111.9 | 1267.3 | 0.103 |
| Expected | n/a | n/a | 559.3 | 654.6 | 370.8 | 434.0 | 0.398 |
| Observed - Expected | 1741.1 | 902.6 | 0.061* | ||||
| Higher-Income (Q2–4) | |||||||
| Observed | −54.4 | 82.9 | 641.5 | 552.8 | 695.9 | 570.0 | 0.229 |
| Expected | n/a | n/a | −161.5 | 246.1 | −107.1 | 163.1 | 0.515 |
| Observed - Expected | 803.0 | 634.8 | 0.213 | ||||
p < 0.05,.
p < 0.10
Note: Models control for county proportion of non-Hispanic White residents and fatal overdose rates. Dispensed buprenorphine data derived from IQVIA Longitudinal Prescription Claims (LRx) between 2006 and 2018, which tracks individual's prescriptions over time. Longitudinal data derives from electronic data received from pharmacies, payers, software providers, and transactional clearinghouses.
4. Discussion
We examined the extent to which Medicaid expansion influenced buprenorphine initiation trends stratified by county income, including in rural versus urban counties. Among urban counties, Medicaid expansion was associated with significant increases in buprenorphine initiation rates in lowest-income urban counties, but not in higher-income urban counties. In contrast, among rural counties, we saw no evidence that Medicaid expansion was associated with a significant increase in buprenorphine rates in lower-income or higher income rural counties.
Low-income communities have historically had lower rates of buprenorphine use than higher-income communities (Hansen et al., 2016; Lister et al., 2020), and the increases in buprenorphine initiation rates associated with Medicaid expansion in lowest-income counties suggest that Medicaid expansion may have reduced income-related disparities in buprenorphine access. Prior research on whether Medicaid expansion reduced economic disparities in health care utilization is mixed: some studies found that expansion reduced economic disparities for routine medical check-ups (Kino and Kawachi, 2018) and post-injury rehabilitation services (Akande et al., 2018), but not for cancer screenings (Kino and Kawachi, 2018) or dental visits (Kino and Kawachi, 2018).
Effects of Medicaid expansion were stronger in our analysis that excluded late adopter expansion states, perhaps because late adopters had less time during the observation period to realize the benefits of expansion. Since the end of our observation period in 2018, seven more states have expanded Medicaid (Status of State Action on the Medicaid Expansion Decision, 2021). However, twelve states still have not implemented Medicaid expansion as of 2022, including five states – Florida, North Carolina, Tennessee, South Carolina, and Georgia – that accounted for nearly 20 % of opioid overdose deaths in the United States in 2020 (KFF, 2022). Medicaid expansion in these states might particularly benefit individuals with OUD by increasing buprenorphine treatment rates among residents of low-income counties.
Contrary to our hypothesis, we found that rural lowest-income counties had much smaller increases in buprenorphine initiation rates associated with Medicaid expansion than urban lowest-income counties, consistent with the results of a prior study examining how Medicaid expansion affected physician visits in rural versus urban counties (Benitez and Seiber, 2018). The authors attributed the lack of Medicaid expansion's impact in rural settings to health professional shortages (Benitez and Seiber, 2018). Historically, rural counties have had fewer prescribers who had applied to be able to prescribe buprenorphine for OUD. Thus compared to urban counties, these counties have less buprenorphine treatment capacity (Ghertner, 2019).
Passage of the Consolidated Appropriations Act of 2023 abolished the X-waiver, allowing any clinician who can prescribe controlled substances to prescribe buprenorphine (ASAM, 2023). As a result, Medicaid expansion could impact buprenorphine rates differently in the future, although the effect of allowing any DEA registered clinician to prescribe buprenorphine may still be muted by the shortage of physicians and other prescribing clinicians in rural areas (Andrilla et al., 2019; Lister et al., 2020, 2020; Rosenblatt et al., 2015; Stein et al., 2018). Relatedly, the Comprehensive Addiction and Recovery Act (CARA) of 2016 authorized nurse practitioners (NPs) and physician assistants (PAs) to prescribe buprenorphine (Barnett et al., 2019). After passage of CARA, NPs and PAs played a major role in increasing buprenorphine treatment capacity in rural areas (Barnett et al., 2019). Considering the evolving role of NPs and PAs in buprenorphine treatment, we may have observed different effects if our observation period extended beyond 2018. Nonetheless, at least during our analytic time period, it seems plausible that limited buprenorphine treatment capacity may have attenuated gains in buprenorphine initiation rates associated with Medicaid expansion in rural counties.
More targeted and nuanced policies may be necessary to realize the full potential of Medicaid expansion for increasing access to buprenorphine in rural counties. Future research should explore whether abolishing the X-waiver affects rural-urban disparities in buprenorphine use. Other potential policy responses could include federal grants to encourage buprenorphine treatment provision in rural primary care clinics and substance use treatment centers, as well as educational interventions, training grants, and loan repayment programs to incentivize rural clinicians to prescribe buprenorphine. Buprenorphine treatment capacity could also be increased in rural communities through telehealth (Hughes et al., 2021; Weintraub et al., 2018) depending on federal and state policies regarding telehealth following the expiration of the COVID-19 public health emergency (Andraka-Christou, 2021). In addition, the impact of Medicaid expansion on buprenorphine use depends on whether local buprenorphine providers accept Medicaid, but many buprenorphine providers do not accept Medicaid patients (Knudsen and Studts, 2019; Patrick et al., 2020). Hence, efforts to encourage buprenorphine providers to accept Medicaid patients may also be needed, especially in rural areas.
Furthermore, a substantial number of pharmacies do not stock buprenorphine, particularly in rural areas (Major et al., 2023; Ostrach et al., 2022). Many pharmacists do not perceive buprenorphine as an effective OUD treatment; have held misperceptions about DEA limits on buprenorphine dispensing; and exhibit stigma toward people who use drugs (Major et al., 2023; Ostrach et al., 2022). Secret shopper data showed that approximately 30 % of rural pharmacies would not fill buprenorphine prescriptions or refused to disclose buprenorphine availability over the phone (Kazerouni et al., 2021). Thus, even if buprenorphine treatment capacity increases in rural areas, individuals still may face challenges in obtaining buprenorphine. Pharmacists and pharmacy staff, especially in rural areas, would benefit from training and education about buprenorphine efficacy, regulatory constraints, and stigma reduction (Major et al., 2023).
It is also possible that rural community residents have lower demand for or interest in buprenorphine treatment, despite Medicaid expansion reducing cost barriers. Rural residents may prefer abstinence-based treatment, believing that buprenorphine “trades one addiction for another” (Richard et al., 2020). Culturally-competent educational interventions addressing misconceptions about OUD and buprenorphine should be targeted toward rural areas. For example, the Implementing Technology and Medication Assisted Treatment Team Training in Rural Colorado (IT MATTTRs) study collaborated with rural community members to develop an effective intervention tailored for rural communities that increased awareness and promoted positive attitudes toward buprenorphine treatment (Curcija et al., 2022).
Remaining cost barriers (e.g., co-payments, deductibles) may also disproportionately impact rural communities, as rural populations often have lower incomes than urban populations (Jones, 2010; Lister et al., 2020), and reducing patient cost sharing (i.e., out-of-pocket costs for patients with medical insurance) for buprenorphine treatment could particularly benefit rural patients (Kino and Kawachi, 2018). Future research should examine the impact of policies designed to decrease financial barriers to buprenorphine treatment, such as eliminating copayment requirements and requiring SUD treatment facilities to accept income-based sliding scale payments (Andraka-Christou et al., 2022). These policies may have effects similar to Medicaid expansion and could potentially further reduce income-related buprenorphine disparities.
Our findings must be considered within the context of the study's limitations. First, the data included only aggregate county-level information; we lack individual level information on household income and urban-rural status. Although county-level analyses are preferable to state-level analyses by allowing for important county-level covariates, and while we sought to control for the need for OUD treatment by including county fatal overdose rates in our models, there may be important within-county individual-level variation, particularly regarding OUD diagnoses and severity. Although we are unable to account for heterogeneity within counties, the associations between treatment rates and Medicaid expansion at the county level provide important information for policymakers. Second, we did not have access to county-level data on Medicaid enrollment or buprenorphine treatment capacity, which could play a role in the observed associations or lack thereof. Third, we restricted our analyses to buprenorphine formulations indicated for OUD treatment, but cannot identify off-label use of those formulations. Fourth, over the period we examined, the IQVIA data captured an increasing number of dispensed retail pharmacy prescriptions; we do not know if or how our results were impacted by this change in percentage of prescriptions captured by IQVIA over time. Fifth, we used a dichotomous urban-rural variable created from the US Department of Agriculture RUC codes, and we do not know to what extent alternative approaches to considering the urbanicity or population density of communities might influence our results. Lastly, our analyses focus solely on buprenorphine utilization and do not examine trends in methadone or naltrexone utilization. Future research should focus on increasing access to methadone, in addition to buprenorphine, as some research suggests methadone may be associated with greater retention in treatment than buprenorphine (Degenhardt et al., 2023; Mattick et al., 2014).
5. Conclusion
Despite these limitations, our findings suggest that Medicaid expansion reduced pre-existing income disparities in buprenorphine access in urban areas, but it did not appear to influence income disparities in buprenorphine access in rural counties. To achieve more equitable buprenorphine access, future policies should target low-income rural areas.
Funding
This work was supported by the National Institute on Drug Abuse [P50DA046351 and R01DA048500].
Role of funding source
Nothing declared.
Contributors
Olivia K. Golan, Flora Sheng, Andrew W. Dick, Mark Sorbero, Daniel J. Whitaker, Barbara Andraka-Christou, Therese Pigott, Adam J. Gordon, Bradley D. Stein
CRediT authorship contribution statement
Olivia K. Golan: Conceptualization, Methodology, Formal analysis, Investigation, Writing – original draft, Project administration. Flora Sheng: Methodology, Formal analysis, Investigation, Writing – review & editing. Andrew W. Dick: Methodology, Formal analysis, Investigation, Writing – review & editing, Supervision. Mark Sorbero: Methodology, Formal analysis, Investigation, Writing – review & editing, Supervision. Daniel J. Whitaker: Conceptualization, Methodology, Investigation, Writing – review & editing, Supervision. Barbara Andraka-Christou: Conceptualization, Investigation, Writing – review & editing, Supervision. Therese Pigott: Conceptualization, Methodology, Investigation, Writing – review & editing, Supervision. Adam J. Gordon: Investigation, Writing – review & editing. Bradley D. Stein: Conceptualization, Methodology, Investigation, Resources, Writing – review & editing, Supervision.
Declaration of Competing Interest
No conflict declared.
Acknowledgements
This manuscript was prepared with support from the National Institute on Drug Abuse P50DA046351 (Stein) and R01DA048500 (Stein).
References
- Adu A., Brown S.V., Asaolu I., Sanderson W. Understanding suicide in pregnant and postpartum women, using the National Violent Death Reporting System data: are there differences in rural and urban status? Open J. Obstet. Gynecol. 2019;9(5):547–565. [Google Scholar]
- Ahrnsbrak, R., Bose, J., Hedden, S., Lipari, R., & Park-Lee, E. (2017). Key substance use and mental health indicators in the United States: results from the 2016 National Survey on Drug Use and Health (HHS Publication No. SMA 17-5044, NSDUH Series H-52). https://www.samhsa.gov/data/.
- Akande M., Minneci P.C., Deans K.J., Xiang H., Chisolm D.J., Cooper J.N. Effects of medicaid expansion on disparities in trauma care and outcomes in young adults. J. Surg. Res. 2018;228:42–53. doi: 10.1016/j.jss.2018.02.058. [DOI] [PubMed] [Google Scholar]
- American Community Survey. (2006-2018). https://www.census.gov/programs-surveys/acs.
- Andraka-Christou B. Addressing racial and ethnic disparities in the use of medications for opioid use disorder. Health Aff. (Millwood) 2021;40(6):920–927. doi: 10.1377/hlthaff.2020.02261. [DOI] [PubMed] [Google Scholar]
- Andraka-Christou B., Saloner B., Gordon A.J., Totaram R., Randall-Kosich O., Golan M., Stein B.D. Laws for expanding access to medications for opioid use disorder: a legal analysis of 16 states & Washington DC. Am. J. Drug Alcohol Abuse. 2022:1–12. doi: 10.1080/00952990.2022.2082301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrilla C.H.A., Moore T.E., Patterson D.G., Larson E.H. Geographic distribution of providers with a DEA waiver to prescribe buprenorphine for the treatment of opioid use disorder: a 5-Year update. J. Rural Health. 2019;35(1):108–112. doi: 10.1111/jrh.12307. [DOI] [PubMed] [Google Scholar]
- American Society of Addiction Medicine (ASAM). (2023). Consolidated Appropriations Act, 2023. https://www.asam.org/advocacy/practice-resources/buprenorphine-management#:∼:text=Consolidated%20Appropriations%20Act%2C%202023&text=There%20are%20no%20longer%20any,opioid%20use%20disorder%20with%20buprenorphine.
- Barnett M.L., Lee D., Frank R.G. In rural areas, buprenorphine waiver adoption since 2017 driven by nurse practitioners and physician assistants. Health Aff. 2019;38(12):2048–2056. doi: 10.1377/hlthaff.2019.00859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benitez J.A., Seiber E.E. US health care reform and rural america: results from the ACA's Medicaid expansions. J. Rural Health. 2018;34(2):213–222. doi: 10.1111/jrh.12284. [DOI] [PubMed] [Google Scholar]
- Cole M.B., Wright B., Wilson I.B., Galarraga O., Trivedi A.N. Medicaid expansion and community health centers: care quality and service use increased for rural patients. Health Aff. (Millwood) 2018;37(6):900–907. doi: 10.1377/hlthaff.2017.1542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Courtemanche C., Marton J., Ukert B., Yelowitz A., Zapata D., Fazlul I. The three-year impact of the affordable care act on disparities in insurance coverage. Health Serv. Res. 2019;54(Suppl 1):307–316. doi: 10.1111/1475-6773.13077. Suppl 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curcija K., Zittleman L., Fisher M., Nease D.E., Jr., Dickinson L.M., de la Cerda D., Sutter C., Ancona J., Rank J., Westfall J.M. Does a rural community-based intervention improve knowledge and attitudes of opioid use disorder and medication-assisted treatment? A report from the IT MATTTRs Study. J. Rural Health. 2022;38(1):120–128. doi: 10.1111/jrh.12545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenhardt L., Clark B., Macpherson G., Leppan O., Nielsen S., Zahra E., Larance B., Kimber J., Martino-Burke D., Hickman M. Buprenorphine versus methadone for the treatment of opioid dependence: a systematic review and meta-analysis of randomised and observational studies. Lancet Psychiatry. 2023 doi: 10.1016/S2215-0366(23)00095-0. [DOI] [PubMed] [Google Scholar]
- Ghertner R. US trends in the supply of providers with a waiver to prescribe buprenorphine for opioid use disorder in 2016 and 2018. Drug Alcohol Depend. 2019;204 doi: 10.1016/j.drugalcdep.2019.06.029. [DOI] [PubMed] [Google Scholar]
- Hall N.Y., Le L., Majmudar I., Mihalopoulos C. Barriers to accessing opioid substitution treatment for opioid use disorder: a systematic review from the client perspective. Drug Alcohol Depend. 2021;221 doi: 10.1016/j.drugalcdep.2021.108651. [DOI] [PubMed] [Google Scholar]
- Hansen H., Siegel C., Wanderling J., DiRocco D. Buprenorphine and methadone treatment for opioid dependence by income, ethnicity and race of neighborhoods in New York City. Drug Alcohol Depend. 2016;164:14–21. doi: 10.1016/j.drugalcdep.2016.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harrison J.M., Kerber R., Andraka-Christou B., Sorbero M., Stein B.D. State policies and buprenorphine prescribing by nurse practitioners and physician assistants. Med. Care Res. Rev. 2022;79(6):789–797. doi: 10.1177/10775587221086489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes P.M., Verrastro G., Fusco C.W., Wilson C.G., Ostrach B. An examination of telehealth policy impacts on initial rural opioid use disorder treatment patterns during the COVID-19 pandemic. J. Rural Health. 2021;37(3):467–472. doi: 10.1111/jrh.12570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphreys K., Shover C.L., Andrews C.M., Bohnert A.S.B., Brandeau M.L., Caulkins J.P., Chen J.H., Cuellar M.F., Hurd Y.L., Juurlink D.N., Koh H.K., Krebs E.E., Lembke A., Mackey S.C., Larrimore Ouellette L., Suffoletto B., Timko C. Responding to the opioid crisis in North America and beyond: recommendations of the Stanford-Lancet Commission. Lancet. 2022;399(10324):555–604. doi: 10.1016/S0140-6736(21)02252-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IQVIA Real World Data – Longitudinal Prescriptions. (2006-2018). https://www.iqvia.com/solutions/real-world-evidence/real-world-data-and-insights.
- Jones C.A. DIANE Publishing; 2010. Health Status and Health Care Access of Farm and Rural Populations. [Google Scholar]
- Jones E.S., Moore B.A., Sindelar J.L., O'Connor P.G., Schottenfeld R.S., Fiellin D.A. Cost analysis of clinic and office-based treatment of opioid dependence: results with methadone and buprenorphine in clinically stable patients. Drug Alcohol Depend. 2009;99(1–3):132–140. doi: 10.1016/j.drugalcdep.2008.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaiser Family Foundation (KFF). (2022). KFF analysis of Centers for Disease Control and Prevention (CDC), National Center for Health Statistics. Multiple Cause of Death 1999-2020 on CDC WONDER Online Database. https://www.kff.org/other/state-indicator/opioid-overdose-deaths-by-raceethnicity/?dataView=0¤tTimeframe=0&sortModel=%7B%22colId%22:%22Total%22,%22sort%22:%22desc%22%7D.
- Kaufman B.G., Reiter K.L., Pink G.H., Holmes G.M. Medicaid expansion affects rural and urban hospitals differently. Health Aff. (Millwood) 2016;35(9):1665–1672. doi: 10.1377/hlthaff.2016.0357. [DOI] [PubMed] [Google Scholar]
- Kazerouni N.J., Irwin A.N., Levander X.A., Geddes J., Johnston K., Gostanian C.J., Mayfield B.S., Montgomery B.T., Graalum D.C., Hartung D.M. Pharmacy-related buprenorphine access barriers: an audit of pharmacies in counties with a high opioid overdose burden. Drug Alcohol Depend. 2021;224 doi: 10.1016/j.drugalcdep.2021.108729. [DOI] [PubMed] [Google Scholar]
- Kino S., Kawachi I. The impact of ACA Medicaid expansion on socioeconomic inequality in health care services utilization. PLoS One. 2018;13(12) doi: 10.1371/journal.pone.0209935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knudsen H.K. The supply of physicians waivered to prescribe buprenorphine for opioid use disorders in the United States: a state-level analysis. J. Stud. Alcohol Drugs. 2015;76(4):644–654. doi: 10.15288/jsad.2015.76.644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knudsen H.K., Hartman J., Walsh S.L. The effect of Medicaid expansion on state-level utilization of buprenorphine for opioid use disorder in the United States. Drug Alcohol Depend. 2022;232 doi: 10.1016/j.drugalcdep.2022.109336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knudsen H.K., Studts J.L. Physicians as mediators of health policy: acceptance of Medicaid in the context of buprenorphine treatment. J. Behav. Health Serv. Res. 2019;46(1):151–163. doi: 10.1007/s11414-018-9629-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lister J.J., Weaver A., Ellis J.D., Himle J.A., Ledgerwood D.M. A systematic review of rural-specific barriers to medication treatment for opioid use disorder in the United States. Am. J. Drug Alcohol Abuse. 2020;46(3):273–288. doi: 10.1080/00952990.2019.1694536. [DOI] [PubMed] [Google Scholar]
- Lister J.J., Weaver A., Ellis J.D., Molfenter T., Ledgerwood D.M., Himle J.A. Shortages of medication-assisted treatment for opioid use disorder in underserved Michigan counties: examining the influence of urbanicity and income level. J. Health Care Poor Underserved. 2020;31(3):1291–1307. doi: 10.1353/hpu.2020.0095. [DOI] [PubMed] [Google Scholar]
- Luo H., Wu Q., Bell R.A., Wright W., Quandt S.A., Basu R., Moss M.E. Rural-urban differences in dental service utilization and dental service procedures received among US adults: results from the 2016 Medical Expenditure Panel Survey. J. Rural Health. 2021;37(3):655–666. doi: 10.1111/jrh.12500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Major E.G., Wilson C.G., Carpenter D.M., Harless J.C., Marley G.T., Ostrach B. Factors in rural community buprenorphine dispensing. Exploratory Res. Clin. Soc. Pharmacy. 2023;9 doi: 10.1016/j.rcsop.2022.100204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandal B. Rural–urban differences in health care access and utilization under the Medicaid expansion. Appl. Econ. Perspect Policy. 2022;44(2):702–721. [Google Scholar]
- Mattick R., Breen C., Kimber J., Davoli M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Systematic Rev. 2014 doi: 10.1002/14651858.CD002207.pub4. [DOI] [PubMed] [Google Scholar]
- Meinhofer A., Witman A.E. The role of health insurance on treatment for opioid use disorders: evidence from the Affordable Care Act Medicaid expansion. J. Health Econ. 2018;60:177–197. doi: 10.1016/j.jhealeco.2018.06.004. [DOI] [PubMed] [Google Scholar]
- Multiple Cause of Death Data. (2006-2018). https://wonder.cdc.gov/mcd.html.
- National Center for Health Statistics (NCHS) Centers for Disease Control and Prevention; 2023. Provisional Data Shows U.S. Drug Overdose Deaths Top 100,000 in 2022.https://blogs.cdc.gov/nchs/2023/05/18/7365/ Retrieved September 20, 2023 from. [Google Scholar]
- National Institute on Drug Abuse (NIDA). (2021). How much does opioid treatment cost? Retrieved April 1 from https://nida.nih.gov/publications/research-reports/medications-to-treat-opioid-addiction/how-much-does-opioid-treatment-cost.
- Okwori G., Hale N., Smith M., Beatty K.E. Geographic differences in contraception provision and utilization among federally funded family planning clinics in South Carolina and Alabama. J. Rural Health. 2022;38(3):639–649. doi: 10.1111/jrh.12612. [DOI] [PubMed] [Google Scholar]
- Olfson M., Zhang V.S., King M., Mojtabai R. Changes in buprenorphine treatment after Medicaid expansion. Psychiatr. Serv. 2021;72(6):633–640. doi: 10.1176/appi.ps.202000491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olfson M., Zhang V.S., Schoenbaum M., King M. Trends in buprenorphine treatment in the United States, 2009-2018. JAMA. 2020;323(3):276–277. doi: 10.1001/jama.2019.18913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ostrach B., Potter R., Wilson C.G., Carpenter D. Ensuring buprenorphine access in rural community pharmacies to prevent overdoses. J. Am. Pharm. Assoc. 2022;62(2):588–597. doi: 10.1016/j.japh.2021.10.002. e582. [DOI] [PubMed] [Google Scholar]
- Owen J.A., Conaway M.R., Bailey B.A., Hayden G.F. Predicting rural practice using different definitions to classify medical school applicants as having a rural upbringing. J. Rural Health. 2007;23(2):133–140. doi: 10.1111/j.1748-0361.2007.00080.x. [DOI] [PubMed] [Google Scholar]
- Patrick S.W., Richards M.R., Dupont W.D., McNeer E., Buntin M.B., Martin P.R., Davis M.M., Davis C.S., Hartmann K.E., Leech A.A. Association of pregnancy and insurance status with treatment access for opioid use disorder. JAMA Network Open. 2020;3(8) doi: 10.1001/jamanetworkopen.2020.13456. e2013456-e2013456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perera U.G.E., Dick A.W., Chastain A.M., Stone P.W., Shang J. The effects of home health value-based purchasing on home health care quality in for-profit and nonprofit agencies: a comparative interrupted time-series analysis, 2012–2018. Medical Care Res. Review. 2022;79(3):414–427. doi: 10.1177/10775587211049628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richard E.L., Schalkoff C.A., Piscalko H.M., Brook D.L., Sibley A.L., Lancaster K.E., Miller W.C., Go V.F. You are not clean until you're not on anything”: perceptions of medication-assisted treatment in rural Appalachia. Int J Drug Policy. 2020;85 doi: 10.1016/j.drugpo.2020.102704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenblatt R.A., Andrilla C.H., Catlin M., Larson E.H. Geographic and specialty distribution of US physicians trained to treat opioid use disorder. Ann. Fam. Med. 2015;13(1):23–26. doi: 10.1370/afm.1735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rural-Urban Continuum Codes. (2013). https://www.ers.usda.gov/data-products/rural-urban-continuum-codes.aspx.
- Saloner B., Landis R.K., Jayakrishnan R., Stein B.D., Barry C.L. A bridge too far? Distance to waivered physicians and utilization of buprenorphine treatment for opioid use disorder in West Virginia Medicaid. Subst. Abus. 2022;43(1):682–690. doi: 10.1080/08897077.2021.1986882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saloner B., Levin J., Chang H.Y., Jones C., Alexander G.C. Changes in buprenorphine-naloxone and opioid pain reliever prescriptions after the Affordable Care Act Medicaid expansion. JAMA Netw Open. 2018;1(4) doi: 10.1001/jamanetworkopen.2018.1588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharp A., Jones A., Sherwood J., Kutsa O., Honermann B., Millett G. Impact of Medicaid expansion on access to opioid analgesic medications and medication-assisted treatment. Am. J. Public Health. 2018;108(5):642–648. doi: 10.2105/AJPH.2018.304338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sordo L., Barrio G., Bravo M.J., Indave B.I., Degenhardt L., Wiessing L., Ferri M., Pastor-Barriuso R. Mortality risk during and after opioid substitution treatment: systematic review and meta-analysis of cohort studies. BMJ. 2017;357:j1550. doi: 10.1136/bmj.j1550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Status of State Action on the Medicaid Expansion Decision. (2021). Kaiser Family Foundation. Retrieved June 8 from https://www.kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D.
- Stein B.D., Dick A.W., Sorbero M., Gordon A.J., Burns R.M., Leslie D.L., Liccardo Pacula R. A population-based examination of trends and disparities in medication treatment for opioid use disorders among Medicaid enrollees A population-based examination of trends and disparities in medication treatment for opioid use disorders among Medicaid enrollees. Subst. Abus. 2018;39(4):419–425. doi: 10.1080/08897077.2018.1449166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein B.D., Gordon A.J., Dick A.W., Burns R.M., Pacula R.L., Farmer C.M., Leslie D.L., Sorbero M. Supply of buprenorphine waivered physicians: the influence of state policies. J. Subst. Abuse Treat. 2015;48(1):104–111. doi: 10.1016/j.jsat.2014.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein B.D., Jones C.M., Smart R., Sheng F., Sorbero M. Patient, prescriber, and community factors associated with filled naloxone prescriptions among patients receiving buprenorphine 2017-18. Drug Alcohol Depend. 2021;221 doi: 10.1016/j.drugalcdep.2021.108569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein B.D., Smart R., Jones C.M., Sheng F., Powell D., Sorbero M. Individual and community factors associated with naloxone co-prescribing among long-term opioid patients: a retrospective analysis. J. Gen. Intern. Med. 2021;36(10):2952–2957. doi: 10.1007/s11606-020-06577-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weintraub E., Greenblatt A.D., Chang J., Himelhoch S., Welsh C. Expanding access to buprenorphine treatment in rural areas with the use of telemedicine. Am. J. Addict. 2018;27(8):612–617. doi: 10.1111/ajad.12805. [DOI] [PubMed] [Google Scholar]
- Wen H., Hockenberry J.M., Borders T.F., Druss B.G. Impact of Medicaid expansion on Medicaid-covered utilization of buprenorphine for opioid use disorder treatment. Med. Care. 2017;55(4):336–341. doi: 10.1097/mlr.0000000000000703. [DOI] [PubMed] [Google Scholar]