Abstract
Background:
Acute abdomen in pregnancy (AAP) is defined as intensive abdominal pain lasting less than 24 hours that may require urgent surgery. It is a challenging situation to diagnose and manage, as it is associated with pain due to the normal anatomical and physiological changes that occur during pregnancy.
Objective:
Therefore, understanding these changes and their effect on almost every system, will help us appreciate the upcoming causes of AAP, mainly the non-obstetric surgical emergencies (e.g., appendicitis, cholecystitis).
Methods:
This article highlights the importance of the well-rounded care that should be offered to every pregnant patient presenting to any center with a Non-obstetric Acute Abdomen. The causes are discussed separately (for surgical pearls), laparoscopic approach and radiologic modality decision-making in pregnancy, which is an academic and a practice-based helpful summary.
Results and Discussion:
This article highlights the importance of the well-rounded care that should be offered to every pregnant patient presenting to any center with a Non-obstetric Acute Abdomen. The causes are discussed separately (for surgical pearls), laparoscopic approach and radiologic modality decision-making in pregnancy, which is an academic and a practice-based helpful summary. Results and Discussion: In addition, the sequence of ideas and language used in the article was based to help the reader understand the topic, rather than inform them about it. In addition, the utility of laparoscopy in pregnancy remains a concern due to the possible risk of injury to the fetus and fetal acidosis. Although, trials showed that laparoscopy was associated with less blood loss and a shorter hospital stay. Moreover, in some cases radiographic imaging is necessary, posing a diagnostic dilemma.
Conclusion:
AAP is a major concern that requires early interventions to pinpoint the cause and manage the patient, properly.
Keywords: acute abdomen, pregnancy, emergency, laparoscopy
1. BACKGROUND
Acute abdomen in pregnancy (AAP) is defined as intensive abdominal pain lasting less than 24 hours that may require urgent surgery. It is a challenging situation to diagnose and manage, as it is associated with pain due to the normal anatomical and physiological changes that occur during pregnancy (1, 2). AAP has been described as 5-10% of all emergency department cases, while non-obstetric acute abdomen that requires a surgical intervention represents about 0.5-2%, with more than 8000 necessitates emergent surgery per year (3, 4). Furthermore, the high prevalence of nausea, vomiting, and abdominal pain in the general obstetric population, and a general hesitancy to operate unreasonably (4).
2. OBJECTIVE
This article highlights the importance of the well-rounded care that should be offered to every pregnant patient presenting to any center with a Non-obstetric Acute Abdomen.
3. MATERIAL AND METHODS
This study will review the normal physiological and anatomical changes in pregnancy and summarize several non-obstetric conditions, including acute appendicitis, biliary diseases, cholangitis, acute pancreatitis, and intestinal obstruction, highlighting the diagnostic approach and treatment plan, then discuss the role of laparoscopy and radiological modalities in pregnancy.
4. RESULTS AND DISCUSSION
The sequence of ideas and language used in the article was based to help the reader understand the topic, rather than inform them about it.The causes are discussed separately (for surgical pearls), laparoscopic approach and radiologic modality decision-making in pregnancy, which is an academic and a practice-based helpful summary.
Physiological and anatomical changes in pregnancy
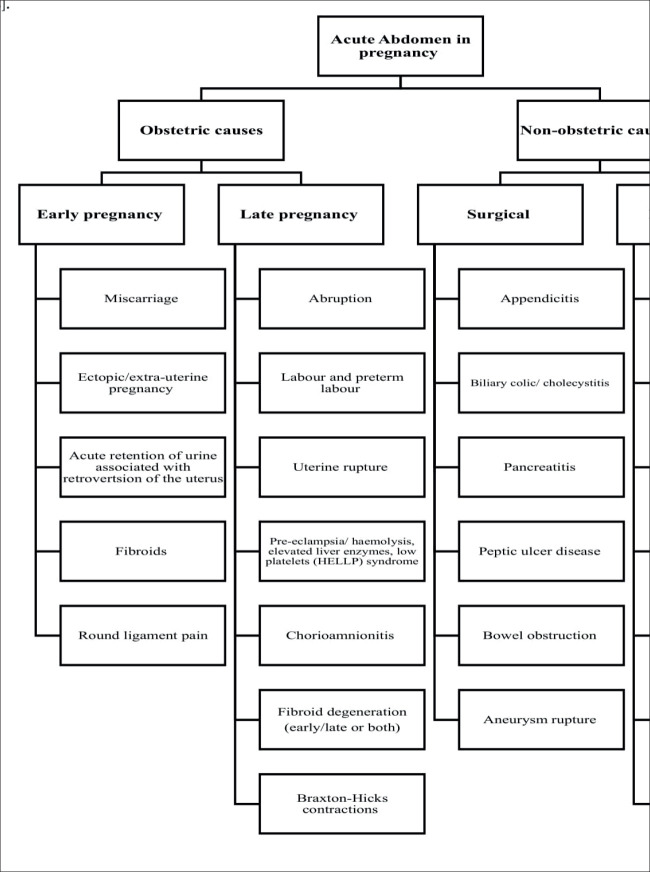
The metabolic demands of pregnancy require maternal adaption by physiological and anatomical changes. Therefore, understanding these changes and their effect on almost every system, including the cardiovascular, respiratory, renal, gastrointestinal, and hematologic systems will help us appreciate the upcoming causes of AAP, mainly the non-obstetric surgical emergencies (Figure 1) (5).
Figure 1. Causes of AAP (18).
Cardiovascular system
The heart is displaced more laterally and to the upper left of the chest by the effect of the gravid uterus’s progressive elevation of the diaphragm. In addition, the left ventricle muscle wall is enlarged to adapt to the increase in blood volume. Physiological changes in the heart include mild tachycardia, peripheral edema, jugular venous distention, and lateral displacement of the cardiac apex (6, 7).
Gastrointestinal system
The manifestations of heartburn, nausea, and vomiting are common during pregnancy. The decrease in gastric secretion PH, increases in the amount of secretion, and a reduction in the tone of the lower esophageal sphincter all contribute to heartburn. On the other hand, nausea and vomiting are also due to the decrease in the lower esophageal sphincter’s tone, which remains behind the progesterone actions (8).
Renal system
The kidneys throughout pregnancy are in a state of glomerular hyperfiltration, which lies behind the increase in the plasma volume, increased effective renal plasma flow (eRPF), and decreased renal plasma oncotic pressure. In the first trimester, the glomerular filtration rate (GFR) and eRPF increase, while in late pregnancy, the eRPF declines. However, GFR plateau declines from the second trimester and returns to normal in the postpartum period. Also, frequency and urgency are believed to be due to the changes in GFR and eRPF. Nevertheless, physical compression by the gravid uterus on the bladder has a role (9-11).
Hematological system
The basal metabolic rate increases during the third trimester by 20%. There exists a state of hyperinsulinism from hyperplasia of istle cells in the pancreas and peripheral insulin resistance. Moreover, the plasma volume in the first trimester increases by 15%, faster during the second trimester and continuing at a slower rate during the third trimester till it plateaus in the few weeks before delivery. This is essential as it considers a protective buffer to minimize the consequences of a large volume of blood loss during delivery (12-14).
Respiratory system
The high levels of serum progesterone induce a change in the threshold of the brain’s respiratory center, thus increasing the sensitivity to carbon dioxide. Additionally, progesterone results in the dilation of the respiratory airways, hyperemia, and edema of the mucosal surfaces causing nasal congestion and rhinitis during pregnancy, alongside the growth of the gravid uterus, the diaphragm is pushed upward, which decreases in the functional residual capacity. Hence, Dyspnea is common in pregnancy, especially in the third trimester, with a rate ranging from 50 to 70 % (15-17).
Acute appendicitis
Acute appendicitis is the most common non-obstetric surgical pathology during pregnancy, occurring in about 1 in 500 to 1 in 635 pregnancies per year. In addition, it accounts for 65.6% of non-traumatic surgical emergencies in pregnancy, usually in the second trimester. However, the diagnosis is challenging as it has an atypical presentation and could be associated with normal pregnancy.
The anatomical and physiological changes secondary to pregnancy, alter the location of tenderness higher than usual and lateralized as the gravid uterus alternates the appendix’s anatomical position. Accordingly, the reported pain could be on the right upper quadrant in the third trimester, while in the second trimester, it will be at the level of the pelvic brim. In contrast, in the first trimester, it might remain at the right iliac fossa (19). On the other hand, a retrospective study disclosed that 90% of patients reported right lower quadrant pain, regardless of the trimester (4).
As clinical signs are variable, corresponding biological and radiological investigation are required. Unfortunately, the inflammatory markers (white blood count and C reactive protein) lack specificity, while first-line radiological investigation to be considered is abdominal ultrasound, has an estimated sensitivity of about 70% and a specificity of 83%. The diagnosis of appendicitis by ultrasound is by the presence of:
Increase appendix thickness (diameter > 6 mm and wall > 2 mm)
Inflamed immobile appendix
Incompressible appendix
Other indirect findings including (effusion in the right iliac fossa and Douglas heterogeneous collection in the right iliac fossa)
In case the ultrasound is inconclusive, an abdominal MRI remains the most reliable and accurate diagnostic method. Although the diagnosis can be a hurdle, treatment for acute appendicitis should not be delayed as it is associated with disastrous complications that affect both the mother and the fetus (20).
The treatment of acute appendicitis is surgical, and studies showed that conservative treatment only with antibiotics is associated with septic shock. According to recent studies, the laparoscopic approach is not preferred, and it is recommended for surgical exploration for the safety of the mother and the fetus. When laparotomy is picked, a transverse incision should be made where maximum pain is located and not essentially near the Mac Burney point. Also, a meta-analysis comparing laparoscopic appendectomy and open approach showed that the laparoscopic approach was associated with a higher fetal loss rate (19).
Biliary diseases
The second most common surgical procedure during pregnancy is cholecystectomy, with an incidence of 0.8% (21). Multiple risk factors are associated with biliary diseases include gender, obesity, number of pregnancies, and normal physiological changes during pregnancy (e.g mechanical, fetal compression causing dyspepsia). For instance, the prevalence of gallbladder diseases is higher in women 57.9%, compared with men 42.1%. While in obesity, the increase in the body mass index (BMI) during pregnancy became a strong predictor of gallbladder diseases (e.g Acute cholecystitis). Moreover, the risk is higher in multiparous ladies than nulliparous, with an incidence of 19% and 7%, respectively (22).
Cholelithiasis
Cholelithiasis is the presence of gallstones in the gallbladder; 0.2-2% of pregnant ladies have symptomatic cholelithiasis, while the majority are asymptomatic with an incidental discovery. In addition, high levels of estrogen and progesterone during pregnancy may cause biliary stasis (ie high progesterone levels reduce gall bladder emptying, while high estrogen levels lead to higher cholesterol secretion and bile saturation). Consequently, bile stasis with reduced bladder emptying leads to the formation of gallstones (21).
The symptoms of cholelithiasis during pregnancy are described as a sudden, constant, or aching pain in the right upper quadrant or the epigastric region that may radiate to the right shoulder or interscapular region. Eating precipitates symptoms, especially the intake of large or fatty meals. Hence, the sequelae in acute cholecystitis, cholangitis, and gallstone pancreatitis are possible uncommon complications with an incidence of 0.05%-0.8%. In the case of symptomatic cholelithiasis, the preferable management is laparoscopic cholecystectomy over conservative treatment with intravenous hydration, electrolyte correction, and bowel rest [21,22].
Choledocholithiasis
Choledocholithiasis is defined as the presence of gall stone in the common bile duct. It happens only in 10% to 15% of patients with gallstones. Complicated choledocholithiasis is an indication of endoscopic retrograde cholangiopancreatography (ERCP), and it is considered safe and effective with the possibility to reduce fetal radiation exposure by using a lead shield and depreciation of the radiation dosage. Choledocholithiasis can be treated by laparoscopic cholecystectomy after ERCP with sphincterotomy, and it is considered safe. A study showed that laparoscopic cholecystectomy and ERCP were associated with a lower incidence of postpartum biliary symptoms than conservative management in complicated gallstone disease. Yet only 1 in 1200 pregnancies with choledocholithiasis requires intervention (21, 22).
Ascending cholangitis
Ascending cholangitis is inflammation or infection of the common bile duct secondary to obstruction. The signs and symptoms of ascending cholangitis during pregnancy are described as the Charcot triad, which is composed of right upper quadrant pain, fever, and jaundice, and these symptoms and signs are present in 70% of patients (22). These complications can lead to preterm labor in 20% of the cases and fetal loss. In addition, ascending cholangitis specifically poses a 10% chance of spontaneous abortion (21). The Tokyo guidelines for the diagnosis of Ascending cholangitis are substantially more sensitive. In addition, investigations are the same as in the case of non-pregnant females, including ultrasound, Magnetic resonance cholangiopancreatography (MRCP), and liver function test that shows an obstructive jaundice pattern (24).
In general population the treatment of acute cholangitis focuses on the main etiologic factors of the disease (ie biliary infection and obstruction). The principles of treatment consists of systemic antibiotic therapy, biliary drainage procedures and supportive care. Hence, when cholangitis is suspected empirical antibiotic should be administered to all patients as soon as possible. The currently preferred treatment method for pregnant patients with ascending cholangitis accompanied with choledocholithiasis is endoscopic treatment if the facility and a surgeon’s expertise are available with minimal risk of radiation to the fetus and the possibility of conscious sedation or general anesthesia for safety concerns. In addition, Maternal-fetal monitoring is used under the obstetrician’s supervision during the surgery.
The percutaneous transhepatic cholangiography (PTC) with drainage (PTCD) can be done when ERCP is either not accessible or failed, in the case of a second trimester and early third-trimester laparoscopic common bile duct exploration have been described, however, cholecystectomy is offered during the same hospitalization regardless of the technique utilized to clear the duct (23-26).
Acute pancreatitis
Acute pancreatitis affects 1 in 1000 to 5000 pregnancies on average, and most frequently, it affects women in their third trimester or right after giving birth. Cholelithiasis is the most common cause of pregnancy-related acute pancreatitis, which accounts for more than 65% of cases, followed by ethanol use and hyperlipidemia (4, 27). The typical presentation is an acute, dull aching, rapidly worsening pain in the epigastrium that radiates to the back and is resistant to standard doses of analgesics and usually improves by leaning forward. Moreover, the patient may experience nausea or vomiting, often associated with anorexia and fever (24, 27, 28). Two out of the following three characteristics are necessary for the diagnosis of acute pancreatitis (29):
Abdominal pain that is consistent with acute pancreatitis. Serum lipase activity (or amylase activity) is at least three times higher than the upper limit of normal.
Characteristic findings of acute pancreatitis on contrast-enhanced computed tomography (CECT), less frequently magnetic resonance imaging (MRI), or transabdominal ultrasonography.
The acute course of acute pancreatitis in pregnancy may lead to pancreatic necrosis, abscess, multi-organ failure, and other negative maternal and fetal outcomes. Organ failure and the absence of regional or systemic consequences are characteristics of mild acute pancreatitis (MAP). In contrast, the occurrence of temporary organ failure or local or systemic consequences without the presence of chronic organ failure (less than 48 hours) characterizes moderately severe acute pancreatitis (MSAP). On the other hand, persistent organ failure (more than or equal 48 hours) is a defining feature of severe acute pancreatitis (SAP) (27, 29).
These are managed similarly to non-pregnant women; the medical management includes nil per oral, fluid, electrolyte resuscitation, nasogastric aspiration, and painkiller usage, and an intensive care unit is ideal setting for managing these patients (4, 24, 27). A quick (laparoscopic vs open) cholecystectomy should be carried out if the identified etiology of acute pancreatitis was a biliary cause due to the high recurrence rate of symptoms related to gallstones, as previously mentioned for choledocholithiasis (23).
Intestinal obstruction
Acute intestinal obstruction is the third most frequent non-obstetric abdominal emergency, accounting for 1 in 1500 pregnancies. The most common cause of intestinal obstruction during pregnancy is adhesions and found in 60%–70% of cases. Adhesions typically result from prior abdominal procedures, such as a previous cesarean section. Moreover, there are other less frequent causes include volvulus, intussusception, hernia, neoplasm, and appendicitis. The 16th to 20th week, the 36th week, and the early puerperium are typically the three periods where intestinal obstructions are most likely to occur in pregnancy (4, 27).
Furthermore, it is challenging to assess abdominal distention and visible peristalsis due to the growing uterus. It is characterized by general non-specific abdominal colicky pain 98%, nausea and vomiting 82%, and total constipation 30%. The bowel sounds may initially be hyperperistaltic and then gradually become hypoperistaltic, which is a worrying sign that strangulation is about to commence (which is an ominous sign that might denote the onset of strangulation). Ideally, MRI should be the test of choice during pregnancy. If MRI is unavailable, a supine abdominal x-ray should be done. However, it can be challenging to identify dilated bowel loops because of the superimposed images of the fetal skeleton. Furthermore, the choice should be made after weighing the benefits and risks, as it should be used with caution during the period of organogenesis (24, 27).
Most patients improve with conservative management, including bowel rest, intravenous hydration, and nasogastric decompression under strict supervision. If conservative therapy fails and there are indications like impending bowel strangulation or symptoms of fetal distress, immediate surgical intervention is required (4, 24, 27).
The role of laparoscopy in pregnancy
Laparoscopy is broadly utilized to diagnose and treat gynecological and general surgical conditions. In comparison, non-obstetric abdominal surgery during pregnancy is rare and occurs in 1-2/1000 pregnancies. The surgery is preferred to be done in the early second trimester as it is associated with a lower risk of miscarriage and preterm birth compared to the first and third trimesters, respectively. Laparoscopy in pregnancy remains a concern due to the possible risk of injury to the fetus, decreased blood supply to the uterus from carbon dioxide pneumoperitoneum, and fetal acidosis. Although a randomized trial showed that laparoscopy was associated with less blood loss, shorter hospital stays, and less postoperative pain compared to laparotomy (23-25).
In the case of early pregnancy, the approach is by a trocar, 5cm higher than the upper part of the uterus. Also, the trocar can be inserted at the palmer point, which is 3 cm below the left costal margin in the midclavicular line. In the case of a pregnant lady in the late second trimester and beyond, an open incision, either vertical or over the point of maximal tenderness, is used rather than the classical approach as it is considered technically difficult, with a carbon dioxide insufflation up to 12 mm Hg (considered safe). The requirement for continuous fetal monitoring after operating on a woman with a viable fetus of over 24 gestational weeks remains unclear. However, in the case of a pre-viable fetus, a simple ultrasound providing cardiac activity before and after the operation is necessary (24).
Radiological issues in the pregnant patient
Pregnancy-related maternal illness is not rare; in some cases, radiographic imaging is necessary for accurate diagnosis and treatment. The most suitable imaging modality to use while managing pregnant women is a typical diagnostic dilemma. The impact of ionizing radiation on the developing fetus is the main issue concerning imaging during pregnancy. Similar to imaging for the general population, the basic rule for imaging during pregnancy is that radiation exposure should be kept as low as reasonably achievable (ALARA). The effects of radiation exposure on fetuses are primarily inferred from observations rather than rigorous scientific studies (e.g animal studies, Chernobyl victims). Although the American College of Obstetricians and Gynecologists claims that exposure of less than 5 rads has not been linked to an increase in fetal malformations or pregnancy loss, clinically, the fetal dose that should be of concern for teratogenesis is likely to be in the range of 10–20 rads. The treating clinician’s expert recommendations should serve as the foundation for the practice decision regarding the best imaging modality for pregnancy (Table 1) (4, 30).
Table 1. Radiological modalities and their clinical considerations (30).
| Modality | Clinical consideration |
|---|---|
| Plain films | The fetus does not get a considerable radiation dosage from a single plain radiograph. The estimated radiation exposure to the fetus can range from (0.001 mGy to 10 mGy). The radiograph of the lumbar spine provides the highest radiation exposure, with a maximum fetal radiation dosage of (10 mGy). |
| Computed Tomography (CT) | The CT exposes fetuses to a huge amount of radiation, with the CT pelvis exposing the fetus to the most radiation at (50 mGy). |
| Magnetic Resonance (MRI) & Magnetic resonance cholangiopancreatography (MRCP) | The MRI/MRCP are becoming a valuable tool to assess the abdomen in pregnant women as it produces diagnostic pictures using a magnetic field rather than ionizing radiation. |
| Ultrasonography | Ultrasound does not produce ionizing radiation, which is helpful in detecting appendicitis, cholecystitis, and free fluid following abdominal trauma. |
| Endoscopic retrograde cholangiopancreatography (ERCP) | The radiation exposure can be significantly decreased to a level below 5 rads, in which patients are exposed to radiation doses ranging from (0.04 to 0.18 rads) during ERCP in many series, with no immediate adverse effects on the pregnancy or the newborns. |
| Fluoroscopy | It has been observed that radiation exposure and fluoroscopy time are clearly correlated. To reduce exposure, precautions including lead shielding, increasing the space between the patient and the X-ray source, and reducing fluoroscopy sessions are advised. |
5. CONCLUSION
AAP is a common surgical presentation that requires a set of skills in the evaluation and management of such patients. The difficulties lie in the differentiation between physiological changes and pathological manifestations (e.g acute appendicitis), which doctors worldwide need to be familiar with, as a gravid abdomen’s organs are displaced from their usual anatomical site. In addition, laparoscopy’s prominent role in pregnancy depends upon the case, gestational age, and the presence or absence of complications. Therefore, recent advancements in radiological and endoscopic approaches are helpful in the diagnostic and therapeutic processes. However, due to the use of ionizing radiation and the presence of different modalities (e.g Ultrasound), the necessity of using these tools as they still pose the typical risk of teratogenicity is still questionable during pregnancy.
Authors contribution:
All authors were involved in all steps of preparation this article. Final proofreading was made by the first author.
Conflict of interest:
None declared.
Financial support and sponsorship:
Nil.
REFERENCES
- 1.Zachariah SK, Fenn M, Jacob K, Arthungal SA, Zachariah SA. Management of acute abdomen in pregnancy: current perspectives. International journal of women’s health. 2019 Feb;8:119–134. doi: 10.2147/IJWH.S151501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mahmood T, Ventura CS, Messinis I, Mukhopadhyay S, editors. Cambridge University Press; 2021. Dec 2, The EBCOG Postgraduate Textbook of Obstetrics & Gynaecology: Obstetrics & Maternal-fetal Medicine. [Google Scholar]
- 3.Abhirami GR, Sathyavani C, Patil RN. Acute abdomen in pregnancy: a case series on clinical presentation and diagnostic dilemma. International Journal of Reproduction, Contraception, Obstetrics and Gynecology. 2021 Feb 1;10(2):742–747. [Google Scholar]
- 4.Skubic JJ, Salim A. Emergency general surgery in pregnancy. Trauma surgery & acute care open. 2017 Nov 1;2(1):e000125. doi: 10.1136/tsaco-2017-000125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kazma JM, van den Anker J, Allegaert K, Dallmann A, Ahmadzia HK. Anatomical and physiological alterations of pregnancy. Journal of pharmacokinetics and pharmacodynamics. 2020 Aug;47(4):271–285. doi: 10.1007/s10928-020-09677-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kametas NA, McAuliffe F, Hancock J, Chambers J, Nicolaides KH. Maternal left ventricular mass and diastolic function during pregnancy. Ultrasound in Obstetrics and Gynecology: The Official Journal of the International Society of Ultrasound in Obstetrics and Gynecology. 2001 Nov;18(5):460–466. doi: 10.1046/j.0960-7692.2001.00573.x. [DOI] [PubMed] [Google Scholar]
- 7.Davies GA, Herbert WN. Assessment and management of cardiac disease in pregnancy. Journal of Obstetrics and Gynaecology Canada. 2007 Apr 1;29(4):331–336. doi: 10.1016/S1701-2163(16)32432-X. [DOI] [PubMed] [Google Scholar]
- 8.Richter JE. The management of heartburn in pregnancy. Alimentary pharmacology & therapeutics. 2005 Nov;22(9):749–757. doi: 10.1111/j.1365-2036.2005.02654.x. [DOI] [PubMed] [Google Scholar]
- 9.Conrad KP, Davison JM. The renal circulation in normal pregnancy and preeclampsia: is there a place for relaxin? American Journal of Physiology-Renal Physiology. 2014 May 15; doi: 10.1152/ajprenal.00042.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Danielson LA, Conrad KP. Acute blockade of nitric oxide synthase inhibits renal vasodilation and hyperfiltration during pregnancy in chronically instrumented conscious rats. The Journal of clinical investigation. 1995 Jul 1;96(1):482–490. doi: 10.1172/JCI118059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dunlop W. Serial changes in renal haemodynamics during normal human pregnancy. BJOG: An International Journal of Obstetrics & Gynaecology. 1981 Jan;88(1):1–9. doi: 10.1111/j.1471-0528.1981.tb00929.x. [DOI] [PubMed] [Google Scholar]
- 12.Bernstein IM, Ziegler W, Badger GJ. Plasma volume expansion in early pregnancy. Obstetrics & Gynecology. 2001 May 1;97(5):669–672. doi: 10.1016/s0029-7844(00)01222-9. [DOI] [PubMed] [Google Scholar]
- 13.Lund CJ, Donovan JC. Blood volume during pregnancy: significance of plasma and red cell volumes. American journal of obstetrics and gynecology. 1967 Jun 1;98(3):393–403. [PubMed] [Google Scholar]
- 14.Goonewardene M, Shehata M, Hamad A. Anaemia in pregnancy. Best practice & research Clinical obstetrics & gynaecology. 2012 Feb 1;26(1):3–24. doi: 10.1016/j.bpobgyn.2011.10.010. [DOI] [PubMed] [Google Scholar]
- 15.Jensen D, Duffin J, Lam YM, Webb KA, Simpson JA, Davies GA, Wolfe LA, O’Donnell DE. Physiological mechanisms of hyperventilation during human pregnancy. Respiratory physiology & neurobiology. 2008 Mar 20;161(1):76–86. doi: 10.1016/j.resp.2008.01.001. Lyons HA, Antonio R. The sensitivity of the respiratory center in pregnancy and after the administration of progesterone. Transactions of the Association of American Physicians. 1959 Jan 1; 72: 173-180. [DOI] [PubMed] [Google Scholar]
- 16.Tenholder CM, South-Paul MJ. Dyspnea in pregnancy. Chest. 1989 Aug 1;96(2):381–388. doi: 10.1378/chest.96.2.381. [DOI] [PubMed] [Google Scholar]
- 17.Woodhead N, Nkwam O, Caddick V, Morad S, Mylvaganam S. Surgical causes of acute abdominal pain in pregnancy. The Obstetrician & Gynaecologist. 2019 Jan;21(1):27–35. [Google Scholar]
- 18.Mejri A, Arfaoui K, Trigui E. Acute appendicitis in pregnant women: A Tunisian center experience. Medicine. 2022 Jul 7;101(29) doi: 10.1097/MD.0000000000028574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ball E, Waters N, Cooper N, Talati C, Mallick R, Rabas S, Mukherjee A, Ranjan YS, Thaha M, Doodia R, Keedwell R. Evidence-based guideline on laparoscopy in pregnancy: commissioned by the British Society for Gynaecological Endoscopy (BSGE) endorsed by the Royal College of Obstetricians & Gynaecologists (RCOG) Facts, views & vision in ObGyn. 2019 Mar;11(1):5. [PMC free article] [PubMed] [Google Scholar]
- 20.Arkenbosch JH, van Ruler O, de Vries AC. Non-obstetric surgery in pregnancy (including bowel surgery and gallbladder surgery) Best Practice & Research Clinical Gastroenterology. 2020 Feb 1;44:101669. doi: 10.1016/j.bpg.2020.101669. [DOI] [PubMed] [Google Scholar]
- 21.Brown KE, Hirshberg JS, Conner SN. Gallbladder and biliary disease in pregnancy. Clinical Obstetrics and Gynecology. 2020 Mar 1;63(1):211–225. doi: 10.1097/GRF.0000000000000496. [DOI] [PubMed] [Google Scholar]
- 22.Mukherjee R, Samanta S. Surgical emergencies in pregnancy in the era of modern diagnostics and treatment. Taiwanese Journal of Obstetrics and Gynecology. 2019 Mar 1;58(2):177–182. doi: 10.1016/j.tjog.2019.01.001. [DOI] [PubMed] [Google Scholar]
- 23.Pearl JP, Price RR, Tonkin AE. Guidelines for the use of laparoscopy during pregnancy. 2017. URL: www.sages.org/publications/guidelines/guidelines-for-diagnosis-treatment-and-use-of-laparoscopy-for-surgical-problems-during-pregnancy.2018 . [DOI] [PubMed]
- 24.Hot S, Eğin S, Gökçek B, Yeşiltaş M, Karakaş DÖ. Acute biliary pancreatitis during pregnancy and in the post-delivery period. Ulus Travma Acil Cerrahi Derg. 2019 May 1;25(3):253–258. doi: 10.14744/tjtes.2019.03846. [DOI] [PubMed] [Google Scholar]
- 25.Mosler P. Management of acute cholangitis. Gastroenterology & hepatology. 2011 Feb;7(2):121. [PMC free article] [PubMed] [Google Scholar]
- 26.Zachariah SK, Fenn M, Jacob K, Arthungal SA, Zachariah SA. Management of acute abdomen in pregnancy: current perspectives. International journal of women’s health. 2019 Feb;8:119–134. doi: 10.2147/IJWH.S151501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ayati S, Pourali L, Mohammadzadeh Vatanchi A, Saeedi E, Hasanzadeh E. Acute pancreatitis during pregnancy: A case report. The Iranian Journal of Obstetrics, Gynecology and Infertility. 2020 May 21;23(3):99–104. [Google Scholar]
- 28.Zhang T, Wang G, Cao Z, Huang W, Xiao H, Wei H, Lu J, Liu R, Yin C. Acute pancreatitis in pregnancy: a 10-year, multi-center, retrospective study in Beijing. BMC pregnancy and childbirth. 2022 Dec;22(1):1–9. doi: 10.1186/s12884-022-04742-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yoon I, Slesinger TL. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022. Radiation Exposure In Pregnancy. [PubMed] [Google Scholar]