Abstract
Since 2017, Missouri has used federal funds to increase access to medication for opioid use disorder (OUD) within the State’s publicly-funded substance use specialty treatment system through a ‘Medication First’ approach. Results from a statewide assessment of the first year of State Targeted Response implementation showed increases and improvements in overall treatment admissions, medication utilization, and treatment retention in the first year of funding. The current manuscript, which focuses on the St. Louis region, the epicenter of Missouri’s overdose crisis, examines whether improvements were experienced equally among Black and White clients. Results from negative binomial regressions indicate that White individuals in St. Louis experienced larger increases in treatment admissions and utilization of medications for OUD than Black individuals, and Black clients were retained in treatment for shorter lengths of time than White clients. In Missouri, rates of drug overdose deaths are more than three times higher for Black people than White people. Racial inequities in OUD treatment utilization and retention must be intentionally targeted and corrected as one component of reducing this sizable disparity in fatalities.
The opioid overdose epidemic in the United States persists as a nationwide public health crisis despite recent increases in funding and public attention. Nationally, overdose deaths among Black Americans have outpaced deaths among White Americans since 2019.1 In Missouri, this has been the case since 2013, where the opioid overdose death rate among Black people is the third highest in the nation, behind only West Virginia and the District of Columbia.2,3 In 2021, the Missouri drug overdose death rate was 34.65 per 100,000 all persons whereas it was 78.34 per 100,000 among Black persons.4,5 The St. Louis metropolitan area is the epicenter of the overdose crisis statewide and drives Missouri’s racial inequities in overdose deaths. In 2021, 78% of deaths among Black individuals occurred in St. Louis City and County, which only account for 54% of Missouri’s Black population.6,7
These mortality data demonstrate the importance of assessing racial equity within opioid-related substance use disorder (SUD) services. The current study examines racial differences in the St. Louis region for outcomes of Missouri’s low-barrier ‘Medication First’ approach to opioid use disorder (OUD) treatment,8 aimed at improving access to and retention on medications for opioid use disorder (MOUD).
Racial Inequities in Substance Use Disorder Treatments
Nationally, significant inequities exist across the spectrum of SUD services. For example, despite overall increasing rates of buprenorphine prescribing, Black people are less likely to receive it than White people.9 Among pregnant women with OUD being treated with methadone, Black women have been found to receive lower doses than White women.10 Similar patterns exist for syringe access programs, which disproportionately advantage White clients.11 Treatment monitoring and accountability practices, like urine drug screens, contribute to the discharge of people of color at higher rates than White counterparts.12 Relatedly, multiple types and layers of stigma often have an inordinate negative impact on Black clients, which results in Black people making fewer attempts to access or complete treatment.13,14
Missouri’s Medication First Approach to Opioid Use Disorder
In 2017, the Missouri Department of Mental Health (MODMH) received funds from the Substance Abuse and Mental Health Services Administration (SAMHSA) to support integrated OUD prevention, treatment, and recovery initiatives. This funding came through the State Targeted Response to the Opioid Crisis (STR) mechanism and was followed by the State Opioid Response (SOR) in 2018. Twenty-five MODMH-affiliated SUD treatment programs received initial STR funding with a primary aim of increasing access to maintenance MOUD. Treatment agencies in the St. Louis region serving predominantly Black individuals were targeted for inclusion in STR.8,15
Missouri STR funding supported the development and implementation of the Medication First (MedFirst) approach to OUD treatment which is analogous to the Housing First model for chronic homelessness,8 and emphasizes low-barrier access to MOUD. Based on the observation that clients often discontinue buprenorphine or methadone therapy involuntarily due to high-barrier program requirements, which often leads to recurrences in use,16 the MedFirst approach prioritizes and protects client access to pharmacotherapy independent of participation in additional services. (For more detailed information on the MedFirst approach, see Winograd et al., 2019.8)
Early findings regarding the MedFirst approach were promising. When comparing statewide treatment episodes from the 12-month period prior to STR to treatment episodes during the first 12-months of STR implementation, results indicated: (a) increased use of MOUD, particularly buprenorphine, (b) increased retention rates at 1, 3, 6, and 9 months, (c) more rapid access to medication, (d) fewer hours of psychosocial services, and (e) decreased average monthly costs of treatment.15
The present study aims to investigate equity in access to, and retention within, MOUD treatment across racial groups before and during implementation of Missouri’s STR/SOR-funded MedFirst approach. We seek to answer the following research questions, all focused on the St. Louis region – the epicenter of Missouri’s overdose crisis – as opposed to the entire state:
What effect has STR/SOR’s MedFirst approach had on treatment admission across racial groups?
What effect has STR/SOR’s MedFirst had on medication utilization across racial groups?
What effect has STR/SOR’s MedFirst had on treatment retention across racial groups?
Methods
2.1. Data source
This study is a retrospective analysis using state-level billing records, inclusive of client-level diagnosis and demographic information. The authors analyzed data at the episode of care-level (EOC). The University of Missouri–St. Louis IRB approved this study to conduct secondary data analyses.
2.1.1. Sample inclusion and exclusion criteria
The authors included individuals with OUD listed as a primary diagnosis receiving services through publicly funded programs between July 1, 2016, and June 30, 2019, with claimed services updated by November 1, 2020, following delayed billing and reimbursement for services.
Study inclusion and exclusion criteria was similar to those detailed elsewhere,15 though inclusion criteria was in several ways: 1) EOCs among uninsured individuals with OUD enrolled in non-STR/SOR programs during concurrent timeframes were included to be compared to STR/SOR-funded EOCs, 2) there is an additional year of data, for a total of three fiscal years of comparison: the 2017 fiscal year (FY), the year prior to STR initiation, representing ‘treatment as usual’ (FY17); the first year of STR (FY18); and the second year of STR/beginning of SOR (FY19)1, 3) the initial 45-day gap in services signifying the end of EOCs was expanded to180-day gap based on feedback from STR/SOR-funded providers regarding how long breaks in services are treated, 4) EOCs were limited to those occurring in St. Louis City or County (not statewide), and 5) EOCs were excluded if the individual’s race was neither Black nor White due to sample size restrictions (n=163; 3.99%).
2.1.2. Sample description
The included EOCs represent all individuals served through state-funded programs in St. Louis City or County during the years of interest (33.6% of the total statewide FY17 EOCs [of 2,732], 42.6% of total FY18 EOCs [of 3,530], and 37.2% of total FY19 EOCs [of 4,468]). EOCs in St. Louis City or County accounted for between 81% and 83% of EOCs specifically among Black individuals statewide across all three years (FY17: 388 of 471, 82.38%; FY18: 562 of 677, 83.01%; FY19: 583 of 721, 80.86%).
For the current study, comparison groups are based on fiscal year (FY17, FY18, and FY19) and STR/SOR funding (Pre-STR/SOR, STR/SOR, non-STR/SOR, and “Combined”). FY17 is the only group considered Pre-STR/SOR as it occurred before the funding and implementation of STR and is used as the primary comparison group for later time periods. Combined comparisons (inclusive of both STR/SOR-funded services and non-STR/SOR-funded services for the uninsured paid for through existing state and federal sources) evaluate changes across fiscal years to examine the overall impact of STR/SOR on OUD treatment delivery for the uninsured in the region over time (i.e., not broken out by STR/SOR vs. non-STR/SOR). Follow-up comparisons for FY18 and FY19 focus on EOCs within STR/SOR compared to each other and to Pre-STR/SOR to evaluate the differences between STR/SOR treatment and treatment delivery prior to the introduction of STR/SOR funding. (See Table 1 for comparison group definitions and descriptions.)
Table 1.
Treatment comparison groups by fiscal year and STR/SOR funding status
| Treatment Groups | |||
|---|---|---|---|
| Pre-STR/SOR | Non-STR/SOR | STR/SOR-Only Analysis | |
| STR/SOR | |||
| FY17 | FY17 Pre-STR/SOR (All OUD treatment for the uninsured prior to STR/SOR funding) | N/A – STR/SOR not yet funded or implemented | |
| FY18 | N/A – STR/SOR already funded and implemented | FY18 and FY19 - Non-STR/SOR (OUD treatment funded through existing state and federal sources for the uninsured, not STR/SOR and not necessarily with MedFirst intent) | FY18 and FY19 - STR/SOR (OUD treatment funded by STR/SOR in FY18 with MedFirst intent) |
| FY19 | |||
2.2. Outcome variables of interest
The primary outcome variables examined were treatment admissions, rates of MOUD utilization, and treatment retention.
Treatment admission is measured by counts of new EOCs initiated within that fiscal year and refers to the number of EOCs initiated (by race, MOUD status, grant year, etc.). An EOC is established when clients receive at least one billable service.
Medication utilization is a mutually exclusive categorical variable indicating whether an individual received buprenorphine, methadone, or naltrexone (or a combination of medications) at any point over the course of their EOC.
Treatment retention refers to the number of days a client is enrolled in treatment following the initiation of an EOC (i.e., the number of days between the first and last days of billed services). This number of days does not include the final 180 days without any services required before an EOC is considered closed if it was not previously closed by treatment agency staff.
2.3. Statistical Analyses
The research questions were analyzed using statistical approaches useful for count data. For each of our three research questions (i.e., regarding treatment admission, medication utilization, and treatment retention), we first examine STR/SOR and non-STR/SOR EOCs combined, then separately examined STR/SOR EOCs. First, to examine differences in treatment admission, we assessed differences in treatment episode initiation by race, fiscal year, and STR/SOR status using chi-square tests of independence. Second, medication utilization was analyzed using a chi-square test of independence to examine differences in MOUD use in new EOCs by race and fiscal year. All significant chi-square tests were followed up with an inspection of standardized residuals with a critical value of ±1.96 corrected for the number of cells.17 Third, to examine treatment retention, we used multivariate negative binomial regressions to analyze differences in treatment length across years and racial groups. Negative binomial regressions were used due to the outcome (days in treatment) being an overdispersed count variable. Four regressions models were estimated, first using the full sample of EOCs (Models 1 and 2), then using only STR/SOR EOCs (Models 3 and 4). Models 1 and 3 regressed Days in Treatment on Fiscal Year and Race; Model 2 regressed Days in Treatment on Fiscal Year, Race, MOUD utilization, and STR/SOR funding; and Model 4 regressed Days in Treatment on Fiscal year, Race, and MOUD utilization. Negative binomial regression parameters are reported as incident rate ratios (IRR), or exponentiated regression coefficients. Analyses were conducted for all EOCs available (i.e., through both STR/SOR and non-STR/SOR programs) to investigate the effect STR/SOR had on treatment among the uninsured in the St. Louis. All analyses were conducted in R version 4.2.1, and the{MASS} and {emmeans} packages for estimating negative binomial regressions and estimated marginal means.18–20
Results
Overall Sample
The total sample across all treatment groups over the three-year period included 3,920 treatment episodes. Approximately 23% (N=888) occurred in FY17, 37% (N=1,446) during FY18, and 40% (N=1,586) during FY19. During FY18 and FY19, enrollment in the STR/SOR program accounted for 727 (50%) and 974 (61%) of new EOCs, respectively. The total sample was 61% (n=2,387) White and 77% (n=3,049) male. Table 2 provides greater detail about the sample, while Figure 1 compares the racial breakdown of the treatment sample to equivalent racial proportions in the St. Louis region’s population and overdose deaths in 2017, 2018, and 2019.
Table 2.
Demographic, MOUD status, and retention information for the full sample, by treatment comparison group
| Pre-STR/SORa | STR/SORa | Non-STR/SORa | Combined | |
|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | |
| Sex | ||||
| Male | 661 (74%) | 1295 (76%) | 1029 (77%) | 2985 (76%) |
| Female | 227 (26%) | 406 (24%) | 300 (23%) | 933 (24%) |
| Race | ||||
| White | 500 (56%) | 1079 (63%) | 808 (61%) | 2387 (61%) |
| Black | 388 (44%) | 622 (37%) | 523 (39%) | 1533 (39%) |
| Received MOUD | 683 (77%) | 1508 (89%) | 866 (65%) | 3057 (78%) |
| M(SD) | M (SD) | M (SD) | M (SD) | |
| Age | 40.16 (9.43) | 39.15 (9.01) | 38.38 (9.37) | 39.12 (9.25) |
| Days in Treatment | 150.23 (169.17) | 213.51 (205.45) | 178.00 (185.93) | 187.12 (192.77) |
Note:
STR/SOR and Non-STR/SOR include FY18 and FY19, while Pre-STR/SOR includes FY17.
Figure 1.
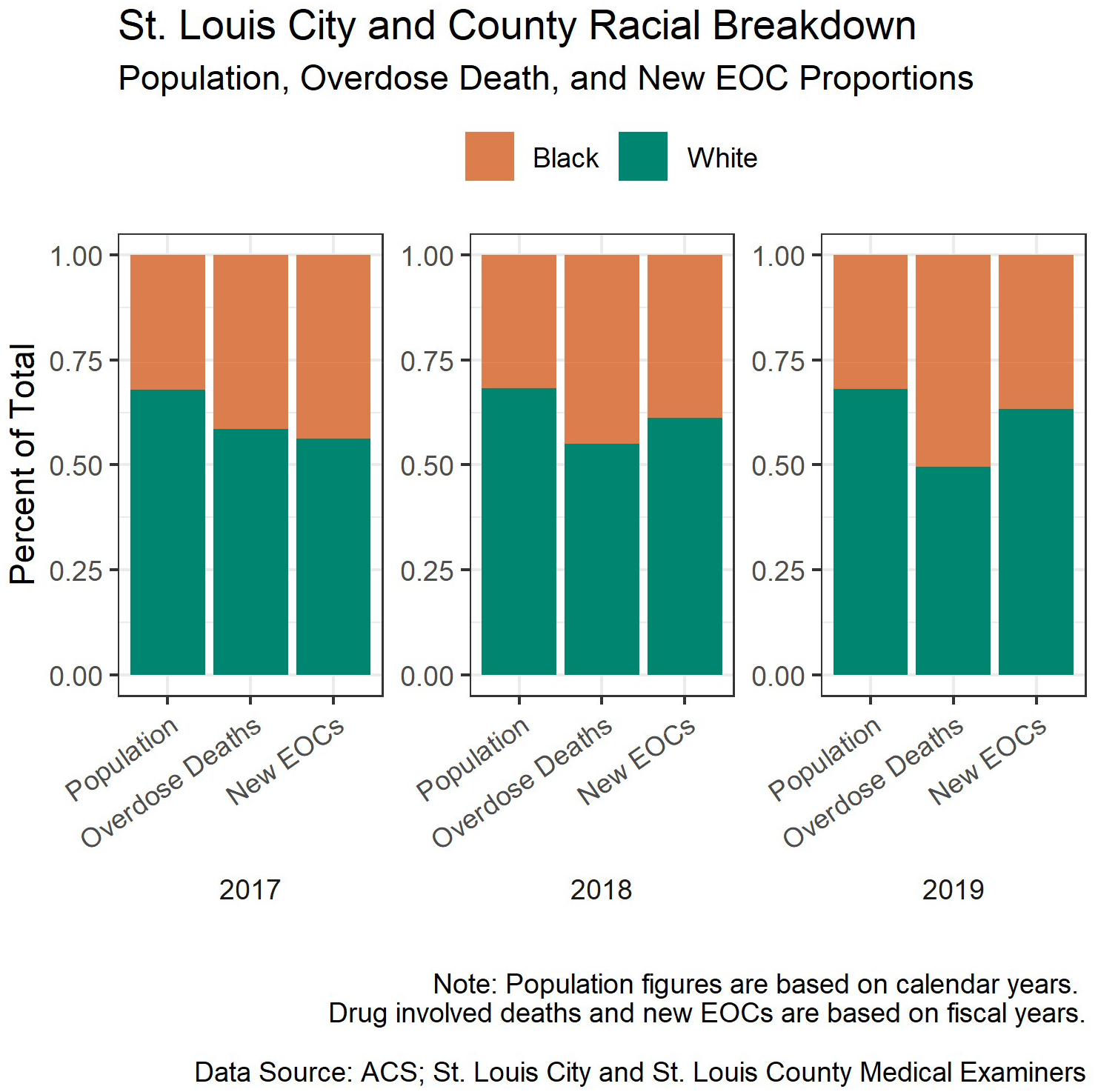
Annual comparisons of proportions of St. Louis region drug overdose deaths, resident populations, and new treatment episodes, by race
Treatment Admission
Combined Treatment Episodes
The chi-square test of the full sample indicated EOC initiation was dependent on fiscal year and racial group (χ2 (N=3,920, 2) = 11.55, p=.003; Cramer’s V=.05), with standardized residuals indicating an overrepresentation of White individuals compared to Black individuals with new EOCs in FY19 compared to FY17 (pre-STR), despite the absolute number of Black individuals receiving treatment continuing to increase in FY18 and FY19. The decreasing proportion of Black treatment episodes appears to be due to the greater increases in the number of EOCs among White individuals than among Black individuals. (See Table 3 for new EOC counts and significance tests and Figure 1 for the visualization of decreasing proportions of EOCs among Black clients.)
Table 3.
Counts and proportions of new episodes of care by fiscal year and race
| Combined Treatment Episodesa | STR/SOR Treatment Episodes | |||
|---|---|---|---|---|
| % Change | % Change | |||
| FY17 | ||||
| Black | 388 (44%) * | - | - | - |
| White | 500 (56%) * | - | - | - |
| FY18 | ||||
| Black | 562 (39%) | + 45% | 268 (37%) | - |
| White | 884 (61%) | + 77% | 459 (63%) | - |
| FY19 | ||||
| Black | 583 (37%) * | + 4% | 354 (36%) | + 32% |
| White | 1003 (63%) * | + 13% | 620 (64%) | + 35% |
Note:
FY17 is Pre-STR/SOR, while FY18 and FY19 include both new STR/SOR and Non-STR/SOR episodes of care;
Observed cell counts are significantly different from expected cell counts at the p = .05 level.
STR/SOR Treatment Episodes
A chi-square test using only STR/SOR enrollment counts in FY18 and FY19 (i.e., the first and second year of STR/SOR funding) showed STR/SOR EOC enrollment counts during these two years were not dependent on grant year or race (χ2 (N=1701, 1)=.05, p=.83; Cramer’s V=.005), with the same proportion of Black and White individuals being enrolled in treatment in both years, respectively. Comparing STR/SOR enrollment in FY18 and FY19 with pre-STR/SOR shows enrollment was based on grant year and race (χ2 (N=2589, 2) =12.502, p=.002; Cramer’s V=.07). Specifically, the number of Black individuals enrolled was smaller than expected in FY19 than FY17 (FY17: 388/888, 44%; FY19: 268/727, 37%), and the number of White individuals enrolled was larger than expected in FY18 compared to FY17 (FY17: 500/888, 56%; FY18: 620/974; 64%).
Medication Utilization
Combined Treatment Episodes
Treatment episodes in FY2018 included greater use of MOUD than those in FY2017 (see Figure 2), but this increase was dependent on race and fiscal year (χ2 (N=3,920, 6)=22.17, p=.001; Cramer’s V=.005). The number of EOCs for White clients receiving medication doubled following the implementation of STR in FY18 (FY17: 374/500; FY18: 712/884), while EOCs involving medication for Black clients increased 35% (FY17: 309/388; FY18: 419/562). Simultaneously, the number of EOCs for White clients who did not receive medication increased 37% (FY17: 126/500; FY18: 172/884) and EOCs with no medication for Black clients increased 81% (FY17: 79/388; FY18: 143/562). From FY18 to FY19, no significant changes in overall rates of medication use occurred.
Figure 2.
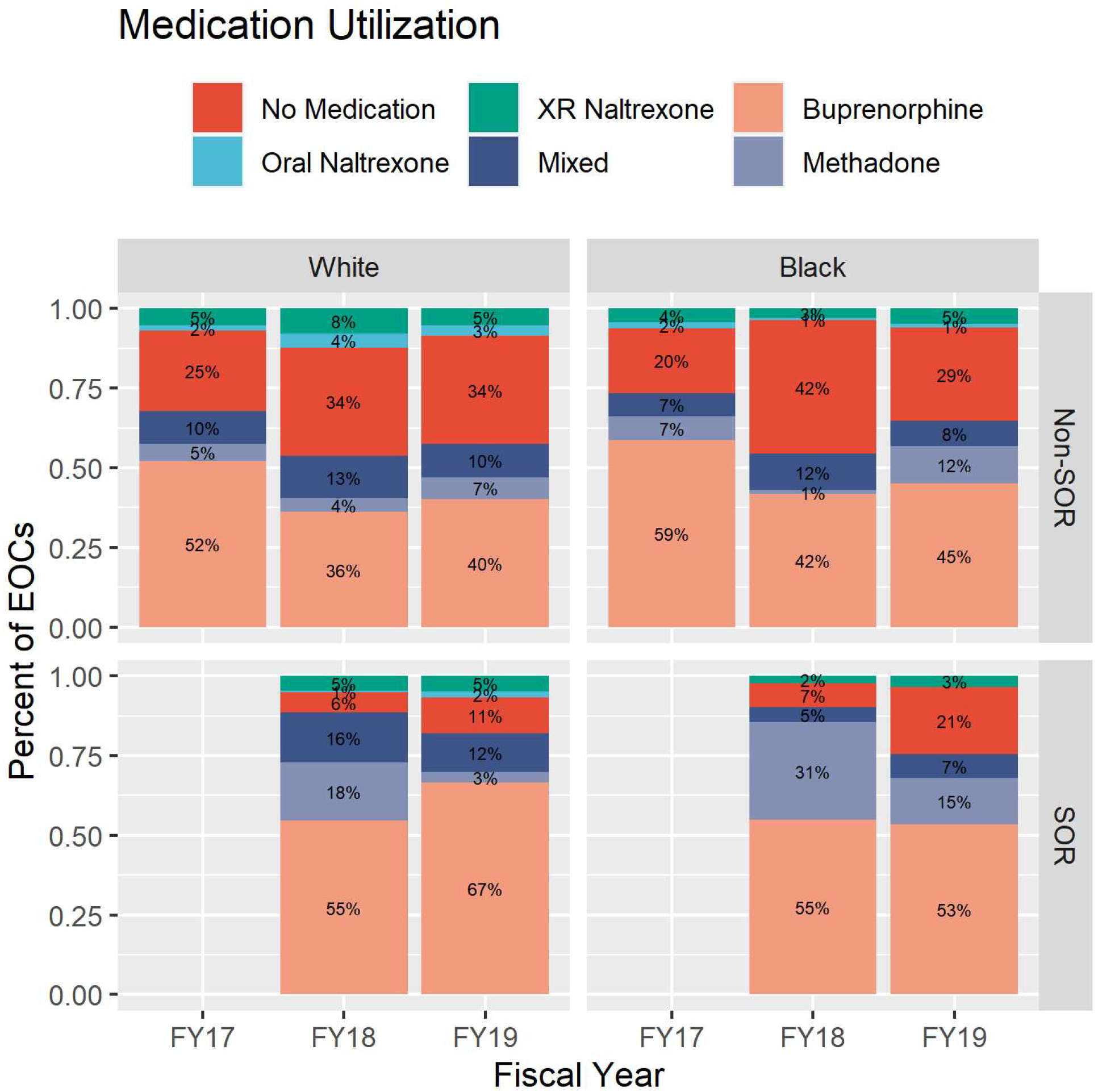
Medications Received by Race, STR/SOR participation, and Fiscal Year
STR/SOR Treatment Episodes
The proportion of EOCs involving MOUD was higher in STR/SOR EOCS than in FY17, prior to STR beginning (χ2 (N=1701, 3) = 30.89, p<.001; Cramer’s V=.14). Approximately 75% of EOCs among both Black and White clients involved MOUD in FY17, and this increased to more than 90% in FY18 for STR/SOR EOCs. In FY19, 88% of STR/SOR EOCs among White people involved MOUD, while the percentage fell to 78% for STR/SOR EOCs among Black clients. The proportion of STR/SOR EOCs involving MOUD for White clients fell 6% from FY18 to FY19 (FY18: 431/459, FY19: 550/620), while the proportion of STR/SOR EOCS involving MOUD for Black clients fell 15% (FY18: 248/268, FY19: 279/354). The total number of STR/SOR EOCs not including MOUD was similar for both Black and White clients in both FY18 (EOCs involving Black clients: 20; EOCs involving White clients: 28) and FY19 (EOCs involving Black clients: 75; EOCs involving White clients: 70). Thus, the difference in proportion can be attributable to the difference from FY18 to FY19 in the total number of new STR/SOR EOCs between Black and White clients receiving MOUD.
Treatment Retention
Combined Treatment Episodes
Results from the negative binomial regression model showed a significant association for both race and program year with number of days in treatment. Estimated marginal means are calculated based on the identified model and provided in estimated days in treatment. Model 1 indicates that, compared to FY17 (M=149 days, 95% CI 137, 162), all clients remained in treatment longer in both FY18 (M=206 days, 95% CI [192, 220]; IRR=1.38, 95% CI 1.24, 1.53) and FY19 (M=182, 95% CI 171, 194; IRR=1.22, 95% CI 1.10, 1.35). Over this period, Black clients (M=164, 95% CI 154, 175) were retained in treatment for fewer days than White clients (M=192, 95% CI 182, 202; IRR=.85, 95% CI 0.79, 0.93). When adjusting for funding through STR/SOR and the use of MOUD with Model 2, Black clients (M=131, 95% CI 122, 140) were still retained in treatment for fewer days than White clients (M=148, 95% CI 139,157; IRR=.88, 95% CI .82, .96). Table 4 provides additional details about model results.
Table 4.
Retention (days in treatment) negative binomial regression coefficients by fiscal year, race, MOUD status, and STR/SOR program status
| Days in Treatment | Combined Treatment Episodes | STR/SOR Treatment Episodes | ||
|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | Model 4 | |
| IRR (95% CI) | IRR (95% CI) | IRR (95% CI) | IRR (95% CI) | |
| Fiscal Year | ||||
| FY17 (refa) | 1.00 | 1.00 | ||
| FY18 (refa) | 1.38 (1.24, 1.53)* | 1.31 (1.17, 1.47)* | 1.00 | 1.00 |
| FY19 | 1.22 (1.10, 1.35)* | 1.15 (1.03, 1.29)* | 0.85 (0.75, 0.96)* | 0.92 (0.81, 1.03) |
| Race | ||||
| White (ref) | 1.00 | 1.00 | 1.00 | 1.00 |
| Black | 0.85 (0.79, 0.93)* | 0.88 (0.82, 0.96)* | 0.85 (0.75, 0.96)* | 0.91 (0.80, 1.03) |
| MOUD | ||||
| Not Received (ref) | 1.00 | 1.00 | ||
| Received | 2.13 (1.93, 2.35)* | 3.70 (3.04, 4.46)* | ||
| Program | ||||
| Non-STR/SOR (ref) | 1.00 | |||
| STR/SOR | 1.01 (0.92, 1.11) | |||
Note. IRR – Incidence Risk Ratio; CI – Confidence Interval; Models 1 and 3: Days in Treatment regressed on Fiscal Year and Race; Model 2: Days in Treatment regressed on Fiscal Year, Race, MOUD utilization, and STR/SOR funding; Model 4: Days in Treatment regressed on Fiscal year, Race, and MOUD utilization. Model 1 and 2 uses the full sample, Models 3 and 4 use the STR/SOR-only portion of the sample;
For combined treatment episodes, FY17 serves as the reference category. For STR/SOR-only analyses, FY18 serves as the reference category.
STR/SOR Treatment Episodes
Results from the negative binomial regression model showed a significant association between the number of days in treatment and both race and program year for the sample of STR/SOR EOCs. Model 3 indicates that, compared to FY18 (M=226, 95% CI 215, 250), clients initiated in FY19 remained in treatment for less time (M=192, 95% CI 177, 208; IRR=0.85, 95% CI 0.75, 0.96). Across this period, Black clients (M=187, 95% CI 169, 206) remained in treatment for fewer days (IRR=.85, 95% CI 0.75, 0.96) than White clients (M=232, 95% CI 169, 206). When adjusting for the use of MOUD in Model 4, Black clients (M=114, 95% CI 101, 128) remained in treatment for a similar number of days as White clients (M=125, 95% CI 113, 140; IRR=.91, 95% CI 0.80, 1.03).
Discussion
Despite indications the STR/SOR-funded, low-barrier MedFirst approach has increased OUD treatment access and retention statewide,15 the current study provides the first investigation of the effect of STR/SOR implementation on racial inequities within specialty SUD treatment settings. We focused specifically on the St. Louis region, the epicenter of Missouri’s overdose crisis and the driving source of the state’s racial inequities in fatal overdose rates. Following the implementation of STR/SOR, treatment admissions across the region increased in number for both Black and White individuals, with an overall growth in treatment episodes of 63%. However, compared to the year prior to implementation, fewer Black individuals were enrolled in STR/SOR-funded treatment than would have been anticipated (both by their representation in treatment in FY17, as well as their representation in overdose deaths, see Figure 1). Prior to STR/SOR beginning, the proportion of St. Louis treatment episodes involving MOUD was 75%, already much higher than the national average.21–23 Even with this high proportion, in the two years following the rollout of STR/SOR there was a further increase in MOUD treatment (both the number of episodes and the proportion of total episodes involving some form of MOUD, which increased to 90% overall) for both Black and White clients, but this increase in access appears to have disproportionately benefited White clients. Specifically, the increase in MOUD access was larger for White individuals, plus the proportion of Black clients receiving MOUD decreased in FY19 (while staying level for White clients). Treatment retention improved broadly following the initiation of STR/SOR, with clients remaining in treatment longer than those served prior to STR/SOR, though retention length regressed in FY19. Despite this overall increase in treatment retention, Black clients were generally not retained as long as White clients in the combined sample. Within STR/SOR programs, though, treatment retention was similar when controlling for whether clients received MOUD.
Our results are consistent with nationally representative data and evidence from other regions demonstrating racial inequities in various aspects of OUD treatment services. Critically, though there is substantial research documenting the existence of racial inequities in SUD treatment,24–26 the current findings reveal increases in inequities following the influx of federal funding to address the opioid overdose crisis in 2017. To our knowledge, this growing inequity has only been documented in one recent study using nationally representative pharmacy claims. Based on over 11 million buprenorphine prescriptions issued between 2006 and 2020, Dong et al. found evidence of decreased retention on buprenorphine among Black patients despite increased retention among White patients since 2017.27 In the present study, though we did not find evidence of decreased treatment access or retention among Black individuals within STR/SOR, the relative increases in access and retention for White individuals were large enough to create racial inequities that had not existed prior to this funding being established. Taken together, the current results in St. Louis coupled with these recent national findings suggest new monies to address the opioid overdose crisis were more effective at reaching and engaging White people who use opioids than their Black counterparts.
To effectively reduce the prevalence of OUD and overdose among Black individuals, systemic changes improving equitable access to and retention in treatment, including but not limited to increasing MOUD, are overdue. National research suggests both individual provider factors and structural determinants of heath contribute to current inequities, including biased prescribing practices, geographic inequities in treatment locations and differential insurance coverage.28,29 However, as noted by Jordan and colleagues,24 “no scientific consensus has emerged as to which determinants are most influential… what extent they matter, or which level matters most” (p.11). Below, we discuss factors that may help explain the current findings in St. Louis.
Potential factors contributing to racial inequities in treatment access and retention
Racial inequities in improvements in treatment admissions and retention may be caused or exacerbated differential implementation of MedFirst principles, substance use resource deserts and broader environmental barriers in predominantly Black neighborhoods, and the lack of culturally affirming options for Black people seeking OUD treatment in St. Louis.
Differential fidelity to the MedFirst approach could, for example, manifest in clinical decisions about discharging clients due to treatment “infractions” (testing positive for illicit drug use, repeated missed visits, etc.). This practice is discouraged under MedFirst principles yet national research suggests it is common in SUD treatment settings.30–33 Because providers are more likely to discharge Black clients for these infractions12 and to require Black clients to undergo urine drug screens in general,12,34 it is possible Black clients in STR/SOR have not been afforded the same “low-barrier” MedFirst leniencies afforded to White clients.
Another potential contributor to racial inequities in treatment access and retention is the lack of substance use treatment and recovery resources operating in the predominantly Black neighborhoods of North St. Louis City and County (i.e., “resource deserts”). Many parts of North St. Louis suffer from decades of disinvestment, redlining and racial covenants, and segregation35 across health and business sectors, with behavioral health (and SUD treatment specifically) being no exception. Additionally, the public transportation system in St. Louis is inadequate and unreliable.36 For individuals from resource-poor areas who needed or sought publicly funded OUD treatment, they simply may not have been willing or able to travel to and from treatment appointments (sometimes requiring more than two hours on busses, each way) to reach an STR/SOR-funded program. Though providing free transportation (in the form of bus tickets or metro passes) is allowable and encouraged through STR/SOR, this form of assistance is insufficient for many and only 9% of treatment episodes during FY18 and FY19 included at least one billing for transportation. In lieu of immediately establishing new, brick and mortar SUD treatment programs in under-resourced, high need areas, funding mobile services and service linkages delivered in Black neighborhoods can be hepful.37 The latter is crucial to building cultural trust and disrupting the legacy of racial segregation that has required Black clients to travel out of their home context, where they may experience more comfort and cultural congruence, into unfamiliar contexts to receive the standard of care.38 Beyond travel and transportation barriers, a multitude of systemic and environmental factors undoubtedly synergize to contribute to the racial inequities documented here. High rates of poverty, homelessness, incarceration, unemployment, over-policing, and gun violence, coupled with low funding for education and the low rates of redevelopment and repopulation persist in North St. Louis, combine to serve as powerful treatment barriers.39
Relatedly, traditional SUD treatment services lack intentional implementation of culturally responsive strategies that address the environmental obstacles described above and deeply resonate with the individuals being served. Specifically, approaches that include faith-based interventions,40 matching Black clients with Black clinicians, education about adaptive relational supports in clients’ own communities, recovery support services that address structural barriers29 and provide recognition, affirmation, and mitigation of “healthy mistrust” of MOUD based on historical and current examples of mistreatment of Black clients in healthcare and substance use treatment settings41,42 have demonstrated promise and should be expanded.
Limitations and Future Directions
This study has several limitations. First, the state-level claims database used to measure treatment enrollment and services provides reliable information about services billed to the state, but lacks details about individuals’ unique experiences, quality of life, and well-being, as well as their perceptions of the treatment itself. The data also only include services billed to state funding streams supporting those without insurance, meaning services paid for through private insurance or Medicaid, or services funded through other sources (e.g., fundraising, individual grants) could have been provided but not reflected in this data. Second, though metrics such as treatment retention are often used as a proxy for clinical outcomes,43 this is not ideal, and future research should integrate other data sources, including qualitative data and narratives about peoples’ experiences navigating SUD treatment,44 including a focus on the intersection of racism and drug user stigma. Third, because this study is based on observational data, we cannot rule out the possibility of these findings – both the overall improvements in MOUD utilization and retention and the introduction of racial inequities in those same metrics – occurring without the influx of opioid-focused STR/SOR funding and Missouri’s implementation of the MedFirst approach.
Conclusion
The overdose crisis is disproportionately affecting Black communities across the United States. Despite a significant need for effective substance use services, Black people who use drugs often experience substantial barriers to entering and maintaining treatment and recovery. In Missouri, the Medication First approach was developed and disseminated through STR/SOR funding with the intention of broadly reducing structural barriers to MOUD treatment to enable all people coming from a variety of life circumstances maintain their care. We found that despite these efforts, STR/SOR funding fueled racial inequities in OUD treatment access and retention in the St. Louis region, with proportionally larger enrollment and increases in MOUD among White clients than Black clients, and shorter treatment retention of Black clients than White clients. Critically, treatment initiatives aimed to better serve people with OUD must prioritize racial equity in the planning and implementation phases or risk introducing or worsening racial inequities.
Footnotes
the first billable service for the FY19 EOCs fell between July 1, 2018, and June 30, 2019
References
- 1.Centers for Disease Control and Prevention. Drug overdose deaths rise, disparities widen. CDC. https://www.cdc.gov/vitalsigns/overdose-death-disparities/index.html [Google Scholar]
- 2.Banks DE, Carpenter RW, Wood CA, Winograd RP. Commentary on Furr-Holden et al. : As opioid overdose deaths accelerate among Black Americans, COVID-19 widens inequities-a critical need to invest in community-based approaches. Addiction. 2021;116(3):686–687. doi: 10.1111/add.15362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Opioid Overdose Deaths by Race/Ethnicity. KFF. Published May 9, 2022. Accessed September 19, 2022. https://www.kff.org/other/state-indicator/opioid-overdose-deaths-by-raceethnicity/ [Google Scholar]
- 4.Missouri Department of Health & Senior Services. Drug overdose dashboard - Fatal overdoses. Accessed December 22, 2022. https://health.mo.gov/data/opioids/
- 5.U.S. Census Bureau. ACS DEMOGRAPHIC AND HOUSING ESTIMATES.; 2021. Accessed December 22, 2022. https://data.census.gov/table?g=0400000US29&tid=ACSDP1Y2021.DP05
- 6.Missouri Overdose Information. MIMH Addiction Science. Published April 2022. Accessed May 16, 2022. https://www.mimhaddisci.org/missouri-overdose-data
- 7.Saint Louis County Department of Public Health. Substance-Involved Deaths St. Louis County, Missouri. Saint Louis Department of Public Health; 2021. Accessed December 22, 2022. https://stlouiscountymo.gov/st-louis-county-departments/public-health/health-data-and-statistics/chronic-disease-reports/drug-overdose/drug-overdose-deaths-2020/ [Google Scholar]
- 8.Winograd RP, Presnall N, Stringfellow E, et al. The case for a medication first approach to the treatment of opioid use disorder. The American Journal of Drug and Alcohol Abuse. 2019;45(4):333–340. doi: 10.1080/00952990.2019.1605372 [DOI] [PubMed] [Google Scholar]
- 9.Lagisetty PA, Ross R, Bohnert ASB. Buprenorphine treatment divide by race/ethnicity and payment. JAMA Psychiatry. 2019;76(9):879–986. doi: 10.1001/jamapsychiatry.2018.3000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rosenthal E, Short V, Cruz Y, Barber C, Roman A, Hand DJ. Racial inequity in methadone dose at delivery in pregnant women with opioid use disorder. Journal of Substance Abuse Treatment. 2021;131. doi: 10.1016/j.jsat.2021.108454 [DOI] [PubMed] [Google Scholar]
- 11.Paquette CE, Syvertsen JL, Pollini RA. Stigma at every turn: Health services experiences among people who inject drugs. International Journal of Drug Policy. 2018;57:104–110. doi: 10.1016/J.DRUGPO.2018.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gaither JR, Gordon K, Crystal S, et al. Racial disparities in discontinuation of long-term opioid therapy following illicit drug use among black and white patients. Drug and Alcohol Dependence. 2018;192:371–376. doi: 10.1016/j.drugalcdep.2018.05.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mennis J, Stahler G. Racial and ethnic disparities in outpatient substance use disorder Treatment episode completion for different substances. Journal of Substance Abuse Treatment. 2016;63:25–33. doi: 10.1016/j.jsat.2015.12.007 [DOI] [PubMed] [Google Scholar]
- 14.Myers B, Fakier N, Louw J. Stigma, treatment beliefs, and substance abuse treatment use in historically disadvantaged communities. African Journal of Psychiatry. 2009;12(3). doi: 10.4314/ajpsy.v12i3.48497 [DOI] [PubMed] [Google Scholar]
- 15.Winograd RP, Wood CA, Stringfellow EJ, et al. Implementation and evaluation of Missouri’s Medication First treatment approach for opioid use disorder in publicly-funded substance use treatment programs. Journal of Substance Abuse Treatment. Published online 2019. doi: 10.1016/j.jsat.2019.06.015 [DOI] [PubMed] [Google Scholar]
- 16.Bentzley BS, Barth KS, Back SE, Book SW. Discontinuation of buprenorphine maintenance therapy: Perspectives and outcomes. Journal of Substance Abuse Treatment. 2015;52:48–57. doi: 10.1016/j.jsat.2014.12.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Delucchi KL. On the Use and Misuse of Chi-Square. University of California, Berkeley; 1993. Accessed December 22, 2022. https://files.eric.ed.gov/fulltext/ED204399.pdf [Google Scholar]
- 18.R Core Team. R: A language and environment for statistical computing. Published online 2022. Accessed December 2, 2022. https://www.r-project.org/
- 19.Venables WN, Ripley BD. Modern Applied Statistics with S. Fourth. Springer, New York; 2002. [Google Scholar]
- 20.Lenth R emmeans: Estimated Marginal Means, aka Least-Squares Means. Published online 2022. https://CRAN.R-project.org/package=emmeans
- 21.Jones A, Honermann B, Sharp A, Millett G. Where multiple modes Of medication-assisted treatment are available. Health Affairs. https://www.healthaffairs.org/do/10.1377/forefront.20180104.835958/full/. Published January 9, 2018. Accessed December 22, 2022. [Google Scholar]
- 22.Nosyk B, Anglin MD, Brissette S, et al. A call for evidence-based medical treatment of opioid dependence in the United States and Canada. Health Affairs. 2013;32(8):1462–1469. doi: 10.1377/hlthaff.2012.0846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mauro P, Gutkind S, Annunziato E. Use of medication for opioid use disorder among US adolescents and adults with need for opioid treatment, 2019. JAMA Netw Open. 2022;5(3). doi: 10.1001/jamanetworkopen.2022.3821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jordan A, Mathis M, Haeny AM, Funaro M, Paltin D, Ransome Y. An evaluation of opioid use in black communities: A rapid review of the literature. Harvard Review of Psychiatry. 2021;29(2):108–130. doi: 10.1097/HRP.0000000000000285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sahker E, Pro G, Sakata M, Furukawa T. Substance use improvement depends on Race/Ethnicity: Outpatient treatment disparities observed in a large US national sample. Drug & Alcohol Dependence. 2020;231. doi: 10.1016/j.drugalcdep.2020.108087 [DOI] [PubMed] [Google Scholar]
- 26.Windsor LC, Jemal A, Alessi E. Cognitive behavioral therapy: A meta-analysis of race and substance use outcomes. Cultural Diversity and Ethnic Minority Psychology. 2015;21(2):300–313. doi: 10.1037/a0037929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dong H, Stringfellow EJ, Russell A. Racial and ethnic disparities in buprenorphine treatment duration in the US. JAMA Psychiatry. doi: 10.1001/jamapsychiatry.2022.3673 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sadler RC, Hippensteel CL, Nelson V, Greene-Moton E, Furr-Holden D. Community-engaged development of a GIS-based healthfulness index to shape health equity solutions. Social Science & Medicine. 2019;1982(227):63–75. doi: 10.1016/j.socscimed.2018.07.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stevens-Watkins D Opioid-related overdose deaths among African Americans: Implications for research, practice and policy. Drug and Alcohol Review. 2020;39(7):857–861. doi: 10.1111/dar.13058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Williams I, Bonner E. Patient termination as the ultimate failure of addiction treatment: Reframing administrative discharge as clinical abandonment. Journal of Social Work Values and Ethics. 2020;17(1):35–46. [Google Scholar]
- 31.Condon T, Jacobs P, Tai B, Pintello D, Miner L, Elcano J. Patient relapse in the context of drug abuse treatment. Journal of Addiction Medicine. 2011;5(3):157–162. doi: 10.1097/adm.0b013e31820497ae [DOI] [PubMed] [Google Scholar]
- 32.Andraka-Christou B, Totaram R, Nguyen T. Comprehensive analysis of discharge reasons from methadone outpatient treatment programs. The American Journal on Addictions. 2022;31(6):508–516. doi: 10.1111/ajad.13326 [DOI] [PubMed] [Google Scholar]
- 33.Chang JS, Chiu J, Gruber V, Sorensen JL. Fair hearing outcomes of patients recommended discharge from methadone maintenance. Journal of Substance Abuse Treatment. 2017;83:68–72. doi: 10.1016/j.jsat.2017.07.011 [DOI] [PubMed] [Google Scholar]
- 34.Becker WC, Meghani S, Tetrault JM, Fiellin DA. Racial/ethnic differences in report of drug testing practices at the workplace level in the U.S. American Journal on Addictions. 2014;23(4):357–362. doi: 10.1111/j.1521-0391.2013.12109.x [DOI] [PubMed] [Google Scholar]
- 35.Goodman M, Gilbert K. Divided Cities Lead to Differences in Health. Washington University in St. Louis; 2013:1–6. Accessed December 23, 2022. https://forthesakeofall.files.wordpress.com/2013/11/policy-brief-4.pdf [Google Scholar]
- 36.Sanchez T. Poverty, policy, and public transportation. Transportation Research Part A: Policy and Practice. 2008;42(5):833–841. doi: 10.1016/j.tra.2008.01.011 [DOI] [Google Scholar]
- 37.Hall G, Neighbors C, Iheoma J, et al. Mobile opioid agonist treatment and public funding expands treatment for disenfranchised opioid-dependent individuals. Journal of Substance Abuse Treatment. 2014;46(4):511–515. doi: 10.1016/j.jsat.2013.11.002 [DOI] [PubMed] [Google Scholar]
- 38.Goedel WC, Shapiro A, Cerdá M. Association of racial/ethnic segregation with treatment capacity for opioid use disorder in counties in the United States. JAMA Network Open. 2020;3(4). doi: 10.1001/jamanetworkopen.2020.3711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Banks DE, Duello A, Paschke ME, Grigsby SR, Winograd RP. Identifying drivers of increasing opioid overdose deaths among black individuals: a qualitative model drawing on experience of peers and community health workers. Harm Reduction Journal. 2023;20(1):5. doi: 10.1186/s12954-023-00734-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.James K, Jordan A. The opioid crisis in black communities. The Journal of Law, Medicine, & Ethics. 2018;46(2). doi: 10.1177/1073110518782949 [DOI] [PubMed] [Google Scholar]
- 41.Eversman M “We want a living solution”: views of harm reduction programs in black US Communities. Journal of Ethnicity in Substance Abuse. 2015;14(2):187–207. doi: 10.1080/15332640.2014.976803 [DOI] [PubMed] [Google Scholar]
- 42.Hargons CN, Miller-Roenigk BD, Malone NJ, Mizelle DL, Atkinson JD, Stevens-Watkins DJ. “Can we get a Black rehabilitation center”? Factors impacting the treatment experiences of Black people who use opioids. Journal of Substance Abuse Treatment. Published online May 21, 2022:108805. doi: 10.1016/j.jsat.2022.108805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hser YI, Evans E, Huang D, et al. Long-term outcomes after randomization to buprenorphine/naloxone versus methadone in a multi-site trial. Addiction (Abingdon, England). 2016;111(4):695–705. doi: 10.1111/add.13238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mark T, Goode LS, McMurtrie G, Weinstein L, Perry. Improving research on racial disparities in access to medications to treat opioid use disorders. Journal of Addiction Medicine. Published online October 26, 2022. doi: 10.1097/ADM.0000000000001104 [DOI] [PubMed] [Google Scholar]


