Abstract
We explored temporal trends and geographic variations in United States of America (US) mortality rates from smoking and firearms from 1999 to 2019. To do so, we used the publicly available Centers for Disease Control and Prevention (CDC) Wide Ranging Online Data for Epidemiologic Research (WONDER) with Multiple Cause of Death files from 1999 to 2019. Using age-specific rates and ArcGIS Pro Advanced software for Optimized Hot Spot Analyses from Esri, we generated maps of statistically significant spatial clusters with 90-99% confidence intervals with the Getis-Ord Gi* statistic for mortality from smoking-related causes and firearms.
These data show temporal trends and geographic variations in mortality from smoking and firearms in the US. Smoking and firearm-related mortality from assault and suicide increased throughout the US and clustered in the Southeast. Firearm-related suicide also clustered in the continental West and Alaska. These descriptive data generate many hypotheses which are testable in analytic epidemiologic studies designed a priori to do so. The trends suggest smoking and firearm-related causes pose particular challenges to the Southeast and firearms also to the West and Alaska. These data may aid clinicians and public health authorities to implement evidence-based smoking avoidance and cessation programs as well as address firearm mortality, with particular attention to the areas of highest risks. As has been the case with cigarettes, individual behavior changes as well as societal changes are likely to be needed to achieve decreases in premature mortality.
Keywords: epidemiology, tobacco use, firearms, mortality, geographic mapping, Southeastern United States, Preventive Medicine
Introduction
Mortality in the United States of America (US) is related, in large part, to potentially avoidable legal exposures including cigarettes and firearms. In 2021 in the US, there were >3.4 million total deaths1 with >480,000 attributable to tobacco2,3 and more than 40,000 to firearms,4 both legal exposures.2,5
Despite remarkable declines in prevalence rates among US adults, cigarettes remain the leading avoidable cause of preventable, premature US mortality.5 Cigarettes, obesity, and physical inactivity are major contributors to the rise in deaths from cardiovascular disease from 5 to 1 worldwide.6 Additionally, smoking is related to premature death due to a number of common and fatal cancers. The relationship of cigarettes with premature deaths from cancer is generally due to duration of exposure, whereas that to deaths from cardiovascular disease is primarily associated with amount currently smoked.7 In combatting this mortality, it has been noted that mortality rates fall quickly from cardiovascular disease6, and, due to the higher prevalence, quitting avoids more premature deaths from cardiovascular disease than cancer.8 Worldwide, tobacco is exported to developing countries at alarming rates with preventable deaths from smoking increasing and accounting for more than 7 million deaths each year.9
In 2020,4 of the 24,576 recorded deaths due to homicide, 79% were firearm-related (19,384), and of the 45,979 reported deaths due to suicide, 53% were firearm-related (24,292) with a total of 45,222 firearm-related deaths including those which were accidental or unknown.4 These contributions additionally involve accidental discharges, related not to intent, but rather a failure to observe safety protocols for the proper handling of firearms. The mortality rate due to firearm-related injuries in the US is higher than most developed countries. Additionally, from 1999 to 2017, there were 38,942 firearm-related deaths that disproportionately affected Black men and US children aged 5-18 years of age.10 Further, firearms are now the leading cause of years of potential life lost from trauma, overtaking motor vehicle crashes, an increase largely driven by increasing rates of suicides.11 Ultimately, during the US epidemic of the COVID-19 pandemic, many potentially avoidable causes of death increased and firearm-related homicides reached their highest rate since 1994. 2,4
In a previous peer-reviewed publication, we found temporal trends and geographic variations in US mortality from opioids, another potentially avoidable cause of premature mortality.12 The results showed a changing landscape of mortality from 1999-2016 with the major hot spots of mortality being primarily located in the Southeast and Appalachia.12 The availability of the CDC Wide-Ranging Data for Epidemiologic Research (WONDER) and the Multiple Cause of Death files afforded us a unique opportunity to explore whether there are temporal trends and geographic variations in US mortality rates from smoking-related causes and firearm-related mortality associated with both suicide and assault. Such descriptive data could formulate important hypotheses and help target interventions in addressing these causes of premature mortality.13
Methods
Sources of Data:
We used publicly available data administered by the Office of Analysis, Epidemiology and Health Promotion of the National Center for Health Statistics, of the United States Centers for Disease Control and Prevention (CDC) on its WONDER website.14 Rates used in these descriptions were obtained from the Multiple Cause of Death files from 1999 to 2019 for all ages from birth to 85 and over. Multiple Cause files were used, in part, to reduce underestimation of attributable mortality from these conditions. This data presents age-adjusted rates for US counties and larger geographic units. The three time periods of equal duration were selected (1999-2005, 2006-2012, 2013-2019) to organize a significant number of counties with data deemed reliable for analysis. The National Center for Health Statistics considers the data reliable if at least 20 deaths were recorded within the county being reported. Death certificates are issued to identify decedents who are legal residents of the US with the certificates estimated to capture 99% of all such deaths among legal residents.15 The time period was selected due to the transition to the 10th revision of the International Classification of Diseases (ICD-10) for mortality reporting in death certificates in 1999.16 A list of ICD-10 Codes used in these descriptions is included in the Supplemental Material (Appendix A). Smoking-related causes of death were those identified as such by the US Surgeon General. 2,5
Measures/Statistical Analysis:
As was used previously in the study of temporal trends of geographic variation in mortality due to opioids, we utilized cluster “hot spot” analyses to explore temporal geographic trends.12 Analysis of the age-adjusted rates was conducted using the ArcGIS Pro Advanced software through Esri.17 Optimized Hot Spot Analysis was conducted, generating a map of statistically significant spatial clusters of high values, hot spots, using the Getis-Ord Gi* statistic. Additionally, the optimization features aggregate incident data, implement the appropriate scale of analysis, and correct for spatial dependence and multiple testing. Geospatial maps of hot spots with 90-99% confidence were generated for three legal but lethal exposures (mortality from smoking-related diseases, mortality from firearm-related suicide, and mortality from firearm-related assault) across three time periods (1999-2005, 2006-2012, 2013-2019).2,17 Overlapping maps with all three exposures were generated for each of the time periods displaying hot spots; however, complete maps displaying confidence levels of both hot and cold spots are presented in the Supplemental Material.
This original research was classified as exempt by the Institutional Review Board.
Results
These data demonstrate significantly higher rates of mortality from smoking-related causes, firearm-related assault, and firearm-related suicide in the Southeast compared to the US overall. As regards cigarettes, mortality rates decreased from 1999-2019. For firearms, mortality rate ratios increased by 16% overall and 20% in the Southeast from 1999-2019 (Table 1).
Table 1.
Age-Adjusted US Mortality Rates and Mortality Rate Ratio from Smoking-Related and Firearm-Related Assault and Suicide Mortality per 100,000 Population in the United States of America and Southeast Region 1999 and 2019a
| 1999 | 2019 | Mortality Rate ratio |
||
|---|---|---|---|---|
| Smoking-Related Causes | Overall | 963.7 (962.1, 965.3) |
613.4 (612.4-614.5) |
0.64 |
| Southeast b | 997,1 (993.8, 1000.4) |
653.3 (651.2, 655.4) |
0.66 | |
| Firearm-Related Assault and Suicide | Overall | 9.8 (9.7, 9.9) |
11.4 (11.3, 11.5) |
1.16 |
| Southeast b | 12.7 (12.5, 13.0) |
15.3 (15.0, 15.5) |
1.20 | |
Centers for Disease Control and Prevention, National Center for Health Statistics. National Vital Statistics System, Mortality 1999-2020 on CDC WONDER Online Database, released in 2021. Data are from the Multiple Cause of Death Files from 1999-2019, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program. Accessed at http://wonder.cdc.gov/mcd-icd10.html on Aug 4, 2022.
In this analysis, we included the states of Alabama, Arkansas, Florida, Georgia, Kentucky, Louisiana, Mississippi, North Carolina, South Carolina, Tennessee, Virginia and West Virginia.
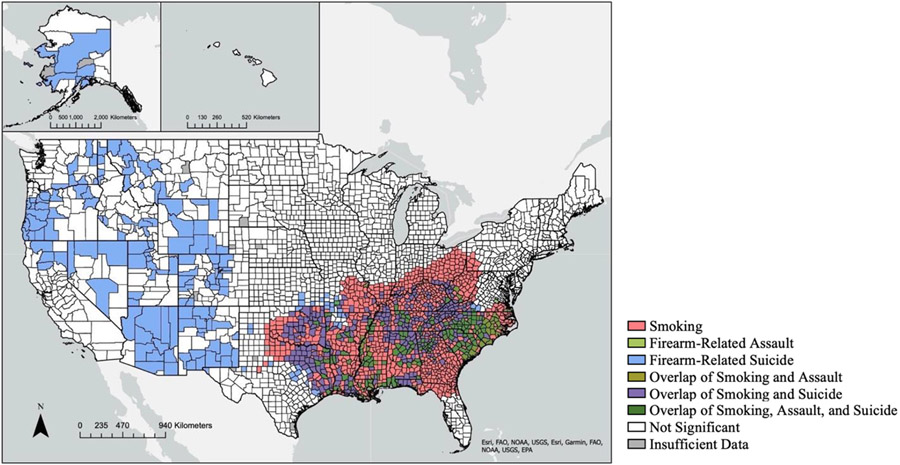
Smoking and Firearm-Related Mortality: 1999-2005
For smoking-related causes of mortality, 1268 counties were identified as hot spots primarily in the Southeast extending up the Appalachian corridor. The 20 states with the highest rates were: Alabama, Arkansas, Florida, Georgia, Illinois, Indiana, Kentucky, Louisiana, Maryland, Mississippi, Missouri, North Carolina, Ohio, Oklahoma, Pennsylvania, South Carolina, Tennessee, Texas, Virginia, and West Virginia. The single county with the highest rate in the US, however, was in South Dakota with 2229.5 deaths per 100,000 individuals (95% Confidence Interval = 1999.9, 2459.1). The corresponding cold spots were primarily located in southern Florida and the Northeast.
For firearm-related assault mortality, 190 counties were identified as hot spots within a single region in the Southeast. A total of 15 states contained hot spots for firearm-related mortality including: Alabama, Arkansas, Florida, Georgia, Kentucky, Louisiana, Mississippi, Missouri, North Carolina, Oklahoma, South Carolina, Tennessee, Texas, Virginia, and West Virginia. The county with the highest rate among hot spot counties was in Louisiana with 35.9 deaths per 100,000 individuals (33.9, 37.8). The hot spot in Florida was restricted to two northern counties. In contrast, cold spots were located primarily in the Northeast as well as in California and Oregon.
For firearm-related suicide mortality, there were 602 counties identified as part of hot spots primarily in the Southeast and the West as well as Alaska. The 31 states with counties identified as hot spots for firearm-related suicide mortality included: Alabama, Alaska, Arizona, Arkansas, California, Colorado, Florida, Georgia, Idaho, Illinois, Indiana, Kansas, Kentucky, Louisiana, Mississippi, Missouri, Montana, Nevada, New Mexico, North Carolina, Ohio, Oklahoma, Oregon, South Carolina, Tennessee, Texas, Utah, Virginia, Washington, West Virginia and Wyoming. The county with the highest rate among hot spot counties was in Alaska with 55.5 deaths per 100,000 individuals (39.1, 76.4). Cold spots were apparent, in particular, in the Northeast (Figure 1).
Figure 1. Hot Spot Analysis of Age-Adjusted Mortality Rates in the United States from Smoking, Firearm-Related Suicide, and Firearm-Related Assault from 1999-2005.
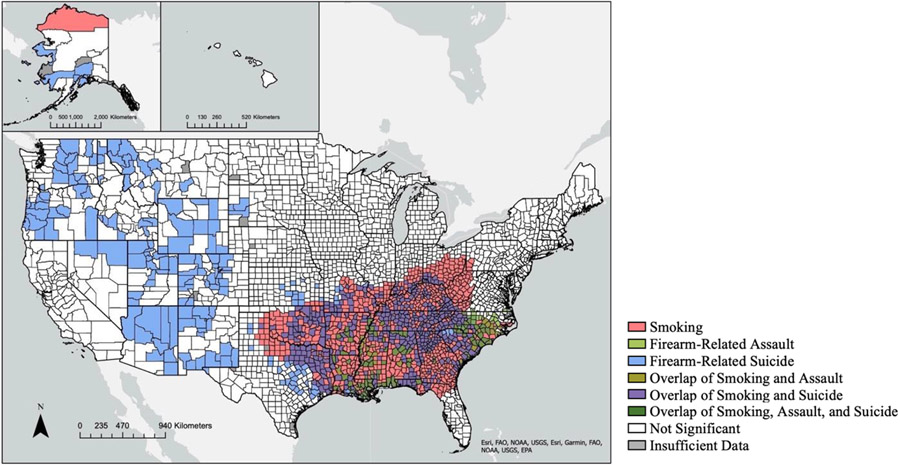
Smoking and Firearm-Related Mortality: 2006-2012
For smoking-related causes of mortality, 1194 counties were apparent as hot spots, primarily in the Southeast with the overall distributions minimally changed in comparison to 1999-2005. A total of 21 states contained hot spots, namely: Alabama, Alaska, Arkansas, Florida, Georgia, Illinois, Indiana, Kansas, Kentucky, Louisiana, Mississippi, Missouri, North Carolina, Ohio, Oklahoma, Pennsylvania, South Carolina, Tennessee, Texas, Virginia, and West Virginia. Maryland no longer contained any hot spot counties while Alaska and Kansas were newly included in the hot spots. The county with the highest rate was in Kentucky with 1861.3 deaths per 100,000 individuals (1777.9, 1944.7). The overall distributions were virtually unchanged from 1999-2005 with the exception of the northern portions of North Carolina shifted from being classified as hot spots to being non-significantly elevated.
For firearm-related assault, 131 counties were identified as hot spots, continuing to be located predominantly in the Southeast with minimal changes. The 10 states that contained hot spots for firearm-related mortality included Alabama, Arkansas, Florida, Georgia, Louisiana, Mississippi, North Carolina, South Carolina, Tennessee, and Virginia. Kentucky, Missouri, Oklahoma, Texas, and West Virginia no longer contained hot spot counties. The county with the highest rate continued to be in Louisiana with an increase to 43.6 deaths per 100,000 individuals (40.9, 46.3). The hot spot in the Southeast still excluded most of Florida, and the hot spot as a whole saw a general consolidation of hot areas within West Virginia and a decrease in the number of counties in Virginia.
For firearm-related suicide, 693 counties were included as hot spots, especially in the Southeast and the West as seen previously with minimal changes to the hot spot patterns. Overall, 29 states contained hot spots for firearm-related suicide mortality, namely: Alabama, Alaska, Arizona, Arkansas, Colorado, Florida, Georgia, Idaho, Illinois, Indiana, Kansas, Kentucky, Louisiana, Mississippi, Missouri, Montana, Nevada, New Mexico, North Carolina, Ohio, Oklahoma, Oregon, South Carolina, South Dakota, Tennessee, Texas, Virginia, Washington, and Wyoming. South Dakota developed a portion of the hot spot and California, Utah, and West Virginia no longer contained hot spot counties. The county with the highest rate among hot spot counties was in Alaska with 44.7 deaths per 100,000 individuals (28.4, 67.1). While the patterns were mostly unchanged, a strengthening of the confidence in the northern border of the southeastern hot spot was observed with consolidation of the western hot spot (Figure 2).
Figure 2. Hot Spot Analysis of Age-Adjusted Mortality Rates in the United States from Smoking, Firearm-Related Suicide, and Firearm-Related Assault from 2006-2012.
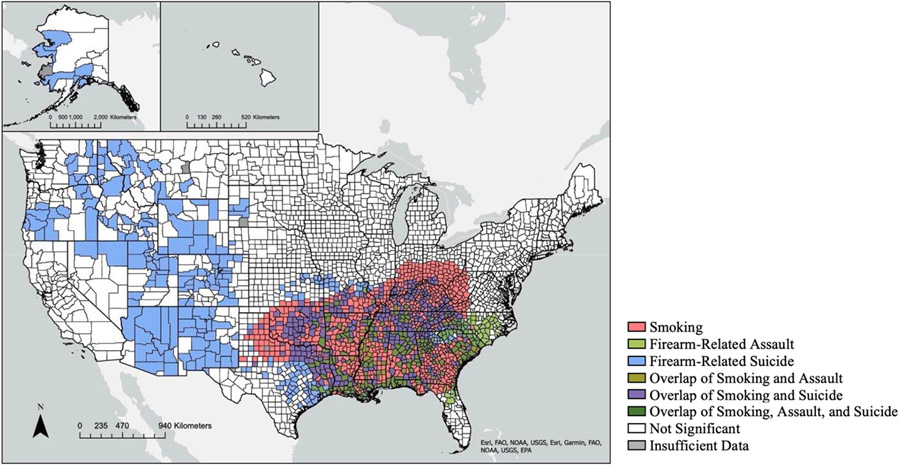
Smoking and Firearm-Related Mortality: 2013-2019
For smoking-related mortality, 1135 counties were apparent in the hot spot region primarily in the Southeast with some southern expansion noted. The same 20 states exhibited hot spots from 2013-2019 that did so in 2006-2012. The county with the highest rate was in South Dakota with 2047.3 deaths per 100,000 individuals (1635.3, 2531.5). The hot spot patterns remained in Southeast, but the majority of North Carolina continued its trend with the non-significant pattern expanding further south and into South Carolina. The additional small hot spot in northern Alaska was also no longer present in this time period, and more specifically, the state of Texas experienced an expansion of its hot spot as well.
For firearm-related assault, 254 counties had hot spots in the Southeast with some expansion of the region. Hot spots were located in 13 states including Alabama, Arkansas, Florida, Georgia, Kentucky, Louisiana, Mississippi, Missouri, North Carolina, Oklahoma, South Carolina, Tennessee, and Texas. Virginia no longer included hot spot counties; however, the county with the highest rate was located in Virginia with 38 deaths per 100,000 individuals (29.8, 47.8). The hot spot in the Southeast expanded further south into Florida and further northwest.
For firearm-related suicide, 764 counties were identified as hot spots with a major region still observed in the Southeast with minimal changes. A total of 30 states contained hot spots including: Alabama, Alaska, Arizona, Arkansas, Colorado, Florida, Georgia, Idaho, Illinois, Indiana, Kansas, Kentucky, Louisiana, Mississippi, Missouri, Montana, Nevada, New Mexico, North Carolina, Ohio, Oklahoma, Oregon, South Carolina, South Dakota, Tennessee, Texas, Utah, Virginia, Washington, and Wyoming. The county with the highest rate among hot spot counties was located in Alaska with 56.2 deaths per 100,000 individuals (36.4, 83) (Figure 3).
Figure 3. Hot Spot Analysis of Age-Adjusted Mortality Rates in the United States from Smoking, Firearm-Related Suicide, and Firearm-Related Assault from 2013-2019.
All three measures – smoking, firearm-related assault, and firearm-related suicide – clustered in the southeastern US. States with hot spots of all three measures including the states of Florida, Alabama, Georgia, South Carolina, North Carolina, Mississippi, Louisiana, Arkansas, Texas, Oklahoma, Missouri, Kentucky, Virginia, and West Virginia. The largest number of overlapping counties were located in the states of North and South Carolina. This contrasts with the Western US where there was no overlap and hot spots were located solely for firearm-related suicide.
Discussion
Legal but lethal exposures such as cigarettes and firearms are among the leading avoidable causes of premature death in the US. These data show geographically distinct areas of the highest rates of mortality from smoking related deaths as well as firearms, including both assault and suicide in addition to opposite trends of overall mortality rates. These patterns persisted over the course of the two decades of the observation period.
Both smoking and firearm-related mortality rates remain higher in the Southeast compared to the entirety of the US with the patterns largely unchanged over the two decades of observation. From 1999 to 2019, firearm assault-related and suicide-related mortality increased 16% in the US and 25% in the Southeast. This is in comparison to smoking-related mortality for which rates have decreased significantly over the course of the last 20 years but clusters of increased mortality persist in the Southeast.
The patterns of smoking-related and firearm-related mortality are consistent with those observed in previous studies, including the identification of 7 of the 10 top ranked states for smoking-related cancers.18 The hot spot for smoking-related mortality is located in the Southeast into Appalachia. The Southeast historically has been known for agriculture including growing tobacco, which may have been contributory; however, this hypothesis would need to be tested in analytic studies designed a priori to do so. As previously mentioned, smoking cessation significantly reduces risks of CVD beginning in a matter of months, and reaching those of lifelong non-smokers within a few years, even among older adults. The observations between immediacy of benefits of cessation on cardiovascular disease and delayed on cancer7,19 are compatible with the observations concerning the state of North Carolina, which gradually transitioned from being a hot spot to non-significant during this last decade. In 2009, the state of North Carolina passed the Smoke Free Restaurants and Bars Law, which banned smoking in enclosed areas of restaurants and bars.20 Since then significant declines in active and second-hand smoke have been reported. For example, there have been significant declines in cigarette use among middle and high school students which, more recently, may be beginning to be mitigated by the expanded use of e-cigarettes and vaping.20 These and similar evidence-based interventions have indicated the potential for mitigation of mortality in these epidemics.
Looking further at the long-term effects of efforts in smoking decline, often related to cancer as described above, and possible geographic areas in which slower declines may have impacted improvements, the National Health Interview Survey data demonstrated from 1965 to 2017 a prevalence decrease of 36.2% among men and 21.9% among women with the highest prevalence of former smokers noted in 1985 for men and 1991 for women.21 These trends varied by race and socioeconomic status as well, which could impact geographic changes within the reports issued throughout the period since 1965.22,23,24 Additional data from the US Behavioral Risk Factor Surveillance System, the largest continuously conducted health survey system in the world, describes a progression in the decades preceding the present study with declines in smoking being unequally represented.25 The greatest declines in a period studied between 1984 and 1992 were described in Arizona, California, the District of Columbia, Georgia, Hawaii, Idaho, Iowa, Maryland, Montana, Nebraska, New Mexico, and Utah to less than 20%; however, it is additionally important to note the increased prevalence of smokeless tobacco use in southern states as noted in this data.24 This slower decline in tobacco use prevalence, persisting well into the 1980s and early 1990s, could explain a part of why this area in particular was a consistent hot spot.
The hot spots for firearm-related mortality due to assault persisted in the Southeast and suicide in both the Southeast and the West. These data on firearm-related mortality add further support to the patterns observed in previous studies.4 Over time, one important change in the maps of firearm-related mortality, with regard specifically to firearm-related assault, is the expansion of the hot spot in Northern Florida to include locations further south into Central Florida. Data from the CDC show an increase in firearm-related mortality in metropolitan areas of Central Florida including Orlando, Kissimmee, and Sanford.26 This contrasts with geographic variations in Florida in smoking-related mortality in which the North is a hot spot and the South a cold spot. Potential explanations for this geographic separation of the state of Florida would be speculative without further analyses; however, they could be related to differences in socioeconomic makeup and migration from areas typically identified as cold spots such as the northeast. Further points of note as limitations for the study is the reduced access of firearm-related data in comparison to smoking-related data. While the efforts for improvement in smoking-related mortality have been well documented since the 1960s, this data is less consistently available for firearms. The reasons behind this are speculative; however, may be in part related to prior limitations from public policy on research related to gun control in the US passed in 1996 known as the Dickey Amendment. Research has grown significantly regarding the impacts of firearm-related mortality in recent years.27
For firearm-related suicide, the hot spot in the West persisted over time. With respect to geographic variations in mortality from firearms, low rates of homicide and suicide have been in New England and the highest rates in the Southeast as well as low homicide and high suicide rates in the Northwest.26 It is speculative whether these findings are related to higher levels of gun owners in the Southeast.2 In addition, the Southeast accounts for more than 60% of US gun thefts.28,29 Prior studies have had inconsistent and at times, contradictory results regarding permissive and restrictive strategies for firearms including studies examining child access prevention laws, stand your ground laws, minimum age to carry, and right-to-carry laws, which have been seen to be sensitive to changes in methods and could be biased by a number of factors.30,31 As these present data are descriptive, all speculations about interventions and policies would require direct testing in analytic studies designed a priori to do so.13,32 It would be premature at this stage for this study to draw firm conclusions; however, future studies of this issue could include more objective studies designed for hypothesis testing and further examination in hypothesis-generating observational studies of socioeconomic, cultural, and political makeups in hot spot mapping. It is also of interest to compare these findings to those previously reported about opioids. Specifically, the increasing epidemic of deaths from opioids also had major impacts in the Southeast and Appalachia.12
Conclusions
Smoking and firearms are among the leading causes of avoidable death in the US. Due to the large array of common and serious diseases due to cigarettes, despite marked declines in prevalence, smoking remains the leading cause of preventable death in the US. These data generate many hypotheses which are testable in analytic epidemiologic studies designed a priori to do so. Cigarettes and firearms pose particular clinical and public health challenges to the southeastern US and firearms to the western US and Alaska. Ultimately, the ability to achieve smoking cessation may be dependent on a better understanding of regional differences. A better understanding of these differences could improve generalizability and understanding outside of the United States These data may aid clinicians and public health authorities to implement interventions in areas of highest risk such as geographically targeted evidence-based cigarette cessation programs. Further, firearm-related mortality increases in the Southeast highlight similarities with cigarette use in that region; however, obtaining analytic study data are necessary to create the best evidence-based practices.
In summary, these descriptive data generate numerous hypotheses requiring testing in analytic epidemiological studies. In the meanwhile, these observed temporal trends and geographic variations may be useful to guide public policies to combat these epidemics of premature and avoidable mortality in the US.
Supplementary Material
Highlights.
Over 20 years, smoking and firearm-related mortality has increased nationwide.
Mortality from smoking and firearm-related mortality clustered in the Southeast.
The descriptive data generates hypotheses testable in analytic epidemiologic studies.
This may aid clinicians or public health officials to create evidence-based programs.
Both individual behavior changes as well as societal changes are likely to be needed.
Funding:
This work was supported by the National Institutes of Health [grant numbers R01 DA044015, 5R01GM114665].
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: The authors have no conflicts of interest to report
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Disclosure of Financial Support: Ms. Palumbo, Dr. Levine, and Dr. Robishaw have no disclosures. Dr. Hennekens reports that he serves as an independent scientist in an advisory role to investigators and sponsors as Chair or Member of Data and Safety Monitoring Boards for Amgen, British Heart Foundation, Cadila, Canadian Institutes of Health Research, DalCor, and Regeneron; to the United States (U.S.) Food and Drug Administration, and UpToDate; receives royalties for authorship or editorship of 3 textbooks and as co-inventor on patents for inflammatory markers and cardiovascular disease that are held by Brigham and Women’s Hospital; has an investment management relationship with the West-Bacon Group within SunTrust Investment Services, which has discretionary investment authority; does not own any common or preferred stock in any pharmaceutical or medical device company.
Proprietary Statement: The authors report no commercial or proprietary interest in any equipment mentioned in the submitted article.
This research was classified as exempt by the Institutional Review Board of the Baylor College of Medicine.
CRediT Author Statement
Sarah A. Palumbo: Conceptualization, Methodology, Software, Formal Analysis, Writing – Original Draft, Writing – Review and Editing. Robert S. Levine: Conceptualization, Methodology, Data Curation, Writing – Review and Editing. Janet D. Robishaw: Conceptualization, Supervision, Funding Acquisition, Writing – Review and Editing. Charles H. Hennekens: Conceptualization, Methodology, Supervision, Writing – Review and Editing
Dr. Palumbo, Professor Levine, and Professor Robishaw have no disclosures. Professor Hennekens reports that he serves as an independent scientist in an advisory role to investigators and sponsors as Chair of Data Monitoring Committees for Amgen and UBC, the Collaborative Institutional Training Initiative (CITI), the United States Food and Drug Administration, and UpToDate; additionally, receiving royalties for authorship or editorship of 3 textbooks and as co-inventor on patents for inflammatory markers and cardiovascular disease that are held by Brigham and Women’s Hospital. Professor Hennekens additionally has an investment management relationship with the West-Bacon Group within SunTrust Investment Services, which has discretionary investment authority, and does not own any common or preferred stock in any pharmaceutical or medical device company. The authors report no commercial or proprietary interest in any equipment mentioned in the submitted article.
References
- 1.Ahmad FB, Cisewski JA, Anderson RN. Provisional Mortality Data — United States, 2021. MMWR Morb Mortal Wkly Rep. 2022;71(17):597–600. doi: 10.15585/mmwr.mm7117e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention (CDC). Wide-Ranging Online Data for Epidemiologic Research (WONDER). National Center for Health Statistics; 2020. Accessed August 4, 2022. http://wonder.cdc.gov [Google Scholar]
- 3.Office on Smoking and Health, National Center for Chronic Disease Prevention and Health Promotion. Burden of Cigarette Use in the U.S Centers for Disease Control and Prevention; 2022. [Google Scholar]
- 4.Kegler SR, Simon TR, Zwald ML, et al. Vital Signs: Changes in Firearm Homicide and Suicide Rates — United States, 2019–2020. MMWR Morb Mortal Wkly Rep. 2022;71(19). doi: 10.15585/mmwr.mm7119e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Centers for Disease Control and Prevention (US); 2014. Accessed March 31, 2019. http://www.ncbi.nlm.nih.gov/books/NBK179276/ [PubMed] [Google Scholar]
- 6.Caldwell M, Martinez L, Foster JG, Sherling D, Hennekens CH. Prospects for the Primary Prevention of Myocardial Infarction and Stroke. J Cardiovasc Pharmacol Ther. 2019;24(3):207–214. doi: 10.1177/1074248418817344 [DOI] [PubMed] [Google Scholar]
- 7.LaCroix AZ, Lang J, Scherr P, et al. Smoking and mortality among older men and women in three communities. N Engl J Med. 1991;324(23):1619–1625. doi: 10.1056/NEJM199106063242303 [DOI] [PubMed] [Google Scholar]
- 8.Hennekens CH. In Their Own Words: Recipients of the Alton Ochsner Award Relating Tobacco and Disease Discuss Their Work. Ochsner J. 2017;17(3):270–272.29089862 [Google Scholar]
- 9.World Health Organization. WHO Report on the Global Tobacco Epidemic, 2017. World Health Organization; 2017. [Google Scholar]
- 10.Rubenstein A, Wood SK, Levine RS, Hennekens CH. Alarming Trends in Mortality from Firearms Among United States Schoolchildren. The American Journal of Medicine. Published online March 2019. doi: 10.1016/j.amjmed.2019.02.012 [DOI] [PubMed] [Google Scholar]
- 11.Klein J, Prabhakaran K, Latifi R, Rhee P. Firearms: the leading cause of years of potential life lost. Trauma Surg Acute Care Open. 2022;7(1):e000766. doi: 10.1136/tsaco-2021-000766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Palumbo SA, Hennekens CH, Robishaw JD, Levine RS. Temporal Trends and Geographic Variations in Mortality Rates from Prescription Opioids: Lessons from Florida and West Virginia. Southern Medical Journal. 2020;113(3):140–145. doi: 10.14423/SMJ.0000000000001074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hennekens CH, Buring JE. Epidemiology in Medicine. 1st ed. (Mayrent SL, ed.). Little, Brown; 1987. [Google Scholar]
- 14.United States Department of Health and Human Services (US DHHS), Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS). Multiple Cause of Death 1999-2019 on CDC WONDER Online Database. Data Are Compiled from Data Provided by the 57 Vital Statistics Jurisdictions through the Vital Statistics Cooperative Program. [Google Scholar]
- 15.Centers for Disease Control and Prevention (CDC). Mortality Data from the National Vital Statistics System. 1989;38(8):119–123. [PubMed] [Google Scholar]
- 16.National Center for Health Statistics (NCHS). International Classification of Diseases,Tenth Revision (ICD-10). cdc.gov. [Google Scholar]
- 17.Esri. Optimized Hot Spot Analysis. ArcMap. Published 2018. Accessed December 1, 2018. http://desktop.arcgis.com/en/arcmap/10.3/tools/spatial-statistics-toolbox/optimized-hot-spot-analysis.htm [Google Scholar]
- 18.Lortet-Tieulent J, Goding Sauer A, Siegel RL, et al. State-Level Cancer Mortality Attributable to Cigarette Smoking in the United States. JAMA Internal Medicine. 2016;176(12):1792. doi: 10.1001/jamainternmed.2016.6530 [DOI] [PubMed] [Google Scholar]
- 19.Office of the Surgeon General (US), Office on Smoking and Health (US). The Health Consequences of Smoking: A Report of the Surgeon General. Centers for Disease Control and Prevention (US); 2004. Accessed March 31, 2019. http://www.ncbi.nlm.nih.gov/books/NBK44695/ [PubMed] [Google Scholar]
- 20.Herndon S, Martin J, Patel T, Staples AH, Swetlick J. The Impact of Smoke-Free Legislation on Population Health in North Carolina. North Carolina Medical Journal. 2014;75(6):422–428. doi: 10.18043/ncm.75.6.422 [DOI] [PubMed] [Google Scholar]
- 21.United States Public Health Service Office of the Surgeon General, National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. Chapter 2, Patterns of Smoking Cessation Among U.S. Adults, Young Adults, and Youth. In: Smoking Cessation: A Report of the Surgeon General. US Department of Health and Human Services; 2020. [Google Scholar]
- 22.Ahmed PI, Gleeson GA. Changes in cigarette smoking habits between 1955 and 1966. Vital Health Stat 10. 1970;10(59):1–33. [PubMed] [Google Scholar]
- 23.Bonham GS, Leaverton PE. Use habits among adults of cigarettes, coffee, aspirin, and sleeping pills. Vital Health Stat 10. 1979;(131):1–48. [PubMed] [Google Scholar]
- 24.Giovino GA, Schooley MW, Zhu BP, et al. Surveillance for selected tobacco-use behaviors--United States, 1900-1994. MMWR CDC Surveill Summ. 1994;43(3):1–43. [PubMed] [Google Scholar]
- 25.National Center for Chronic Disease Prevention and Health Promotion, Division of Population Health. Behavioral Risk Factor Surveillance System. [Google Scholar]
- 26.Wintemute GJ. The Epidemiology of Firearm Violence in the Twenty-First Century United States. Annual Review of Public Health. 2015;36(1):5–19. doi: 10.1146/annurev-publhealth-031914-122535 [DOI] [PubMed] [Google Scholar]
- 27.Rostron A. The Dickey Amendment on Federal Funding for Research on Gun Violence: A Legal Dissection. Am J Public Health. 2018;108(7):865–867. doi: 10.2105/AJPH.2018.304450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hemenway D, Azrael D, Miller M. Whose guns are stolen? The epidemiology of Gun theft victims. Inj Epidemiol. 2017;4( 1):11. doi: 10.1186/s40621-017-0109-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Langton L. Firearms Stolen during Household Burglaries and Other Property Crimes, 2005–2010. US DOJ: Bureau of Justice Statistics; 2012. [Google Scholar]
- 30.Schell TL, Cefalu M, Griffin BA, Smart R, Morral AR. Changes in firearm mortality following the implementation of state laws regulating firearm access and use. Proc Natl Acad Sci USA. 2020;117(26):14906–14910. doi: 10.1073/pnas.1921965117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rosengart M. An evaluation of state firearm regulations and homicide and suicide death rates. Injury Prevention. 2005;11(2):77–83. doi: 10.1136/ip.2004.007062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hennekens CH. Statistical Association and Causation: Contributions of Different Types of Evidence. JAMA. 2011;305(11):1134. doi: 10.1001/jama.2011.322 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.