Abstract
Introduction:
Interpersonal hopelessness (IH), as outlined in the Interpersonal Theory of Suicide, is theorized to include two correlated, distinct constructs: hopelessness about one’s thwarted belongingness (IH-TB) and about perceived burdensomeness on others (IH-PB). Few studies have explored IH, and none have explored its temporal stability or prospective prediction of suicidal desire.
Methods:
Undergraduates (N = 43) selectively recruited for past-2-week suicidal ideation completed five ecological momentary assessment surveys per day for 10-days. Intraclass correlations, root mean square of successive differences, and multilevel models were used to examine the data and test relationships among predictor variables.
Results:
IH-TB and IH-PB demonstrated greater temporal stability than general hopelessness. IH-TB, IH-PB, and their interaction were significant predictors of suicidal desire concurrently and prospectively. IH-PB was no longer significantly predictive of suicidal desire when adjusting for general hopelessness. Post-hoc models showed that suicidal desire was not predictive of IH-TB, IH-PB, or their interaction suggesting the relationship is not recursive.
Conclusion:
Results showed that interventions aimed at decreasing one’s hopelessness specific to TB and PB may be beneficial for decreasing suicidal desire. Future research should seek to replicate these results in larger and more diverse samples and consider the use of shorter ambulatory assessment intervals.
Keywords: ambulatory assessment, hopelessness, interpersonal theory of suicide, suicidal ideation
INTRODUCTION
In 2020, more than 12 million U.S. adults reported that they had thought “seriously” about trying to kill themselves during the previous 12 months (serious thoughts of suicide; SAMHSA, 2021). Among adults, the percentage of individuals with serious thoughts of suicide was highest among those aged 18–25 (SAMHSA, 2021), an age span that overlaps with most individuals enrolled in college (Hansen, 2021). In fact, about one in four college students report having experienced suicidal ideation (SI) in their life (Mortier et al., 2018). Of those with a history of SI, over 65% report having SI in the past year (Mortier et al., 2018). Scholars argue that understanding the nature of SI and how it can be reduced is essential for reducing risk for suicide (Jobes & Joiner, 2019).
The interpersonal theory of suicide (ITS) proposes that suicidal desire can be caused by the simultaneous presence of two interpersonal constructs: thwarted belongingness (TB) and perceived burdensomeness (PB; Van Orden et al., 2010). TB is conceptualized as feelings of social isolation and a lack of reciprocated social caring, while PB includes intense feelings of self-hate and a belief that one burdens the lives of others or communities (Van Orden et al., 2010). For suicidal desire to develop, there must be a simultaneous presence of both TB and PB, as well as hopelessness about future changes in these interpersonal constructs (Van Orden et al., 2010). This hopelessness about TB and PB changing has been termed interpersonal hopelessness (IH; Tucker et al., 2018).
Preliminary evidence supports the hypothesized role of IH within the ITS. A study of undergraduate students found that high general hopelessness (e.g., a general belief of negative future outcomes) intensified the relationship between SI/suicide planning/suicidal urges and the interaction between TB and PB (Hagan et al., 2015). Despite this finding, there is also evidence to suggest general hopelessness may in fact not moderate the relationship between the interaction of TB and PB, and SI. In a study of German psychiatric inpatients, general hopelessness did not moderate the relationships between either TB or PB, and SI (Forkmann et al., 2021). Similarly, Roeder and Cole (2019) found that general hopelessness, PB, and TB predict SI frequency when examined separately. However, none were uniquely predictive of SI frequency when examined simultaneously in the same model (Roeder & Cole, 2019).
One potential explanation for these conflicting findings could be the use of a general measure of hopelessness. In a review and meta-analysis of the ITS, Chu et al. (2017) outlined the need for a measure of hopelessness specific to the interpersonal constructs defined in the ITS. To fill this gap in the literature, Tucker et al. (2018) created a measure of IH, or hopelessness specific to perceptions of TB, and PB. To test the measure, college-student participants (n = 173) recruited for a history of SI were asked to complete an online questionnaire assessing IH and suicidal thoughts and behaviors. It was found that IH was positively correlated with TB (r = 0.56), PB (r = 0.75), SI severity (r = 0.46), and suicide risk (r = 0.44; e.g., a measure of recent suicidal thinking, historical suicidal behaviors, and belief in a future suicide attempt). Additionally, the three-way interaction between IH, TB, and PB predicted both SI severity and suicide risk, while general hopelessness did not interact with TB and PB to predict SI or suicide risk. Although the cross-sectional study design limits the ability to infer temporal or causal relationships between study variables, these findings align with the ITS hypothesis that IH is closely related to the experience of active suicidal desire (Van Orden et al., 2010).
The continued need for more research on IH was highlighted by Joiner et al.’s (2021) review of the state of the ITS literature. No research has tested the IHxTBxPB interaction proposed in the ITS (Joiner et al., 2021) other than that of Tucker et al. (2018). Additionally, the factor structure of the Interpersonal Hopelessness Scale (IHS; Tucker et al., 2018) has received further psychometric scrutiny. Recent research by Mitchell et al. (2023) suggests a superior two-factor solution for the IHS compared to the original one-factor solution found in Tucker et al. (2018). The two-factor solution appears to reflect that hopelessness regarding TB and PB are highly correlated yet separate constructs (Mitchell et al., 2023). These can be conceptualized as hopeless perceptions of burdensomeness (IH-PB) and hopeless beliefs that one lacks a sense of belonging (IH-TB). Further, Mitchell et al. (2023) explored the correlations of TB and PB as measured by the INQ-15 and IH-TB and IH-PB as measured by the IHS. It was found that TB and IH-TB were correlated at r = 0.54, while PB and IH-PB were correlated at r = 0.79. While the variables are highly correlated, they do not appear to be redundant. Therefore, it is important to explore both domains of IH, a line of research previously unexplored.
Ecological momentary assessment (EMA) is increasingly being used in suicide research to explore the dynamic versus static nature of factors, such as IH, that relate to vulnerability for suicide. EMA allows for frequent assessment and monitoring of suicidal thoughts and behaviors as they occur in real-time (Kleiman & Nock, 2018). Prior research has shown that common risk factors for SI, such as general hopelessness, perceived burdensomeness, and loneliness, vary considerably over the course of the day (Hallensleben et al., 2019; Kleiman et al., 2017). While general hopelessness can fluctuate in the span of hours (Kleiman et al., 2017), it is unclear whether the domains of IH follow a similar pattern or remain stable over time. Therefore, the temporal dynamics of IH require further exploration.
The current investigation studied the temporal dynamics of IH and its prospective relationship with suicidal desire. Given the dynamic nature of general hopelessness and SI severity (Kleiman et al., 2017) and the strong correlations between general hopelessness and IH (r = 0.72, Tucker et al., 2018; r = 0.47 and 0.52, Mitchell et al., 2023), we hypothesized that both IH-TB and IH-PB will vary considerably over the course of the day. We hypothesized that IH-TB and IH-PB would follow similar variability patterns to general hopelessness given few psychosocial predictors of SI severity demonstrate stable patterns (Kleiman et al., 2017). Additionally, based on findings that show correlations between active SI and both general hopelessness (Kleiman et al., 2017) and IH (Tucker et al., 2018), we hypothesized that higher IH-TB and IH-PB would be concurrently and prospectively related to increased suicidal desire. We also hypothesized that IH-TB and IH-PB would better predict suicidal desire both concurrently and prospectively than general hopelessness, given the results of Tucker et al. (2018) that demonstrated a stronger relationship between SI and IH compared to general hopelessness. Finally, although Mitchell et al. (2023) demonstrated IH-TB and IH-PB were correlated but separate constructs, they did not test the interaction between these constructs in its ability to predict active suicidal desire as hypothesized by the ITS (Van Orden et al., 2010). Therefore, it was hypothesized that the interaction of IH-TBxIH-PB would concurrently and prospectively predict suicidal desire above and beyond the main effects and general hopelessness.
METHODS
Participants
Undergraduate participants (N = 52) were recruited from a large southeastern university in the United States. Students participating in research for credit in their psychology courses were recruited using an online research participation system. Participants endorsing past-2-week SI (as measured by the Depressive Symptom Index-Suicidality Subscale [DSI-SS; Joiner Jr et al., 2002]) were recruited through screening completed at the beginning of each semester. Enrollment occurred during three consecutive semesters. While the initial screening was completed at the beginning of each semester, participants could elect to enroll at any point throughout the semester. Therefore, self-reported SI scores could have changed between the initial screening and study participation. In the current analysis, six participants were omitted from the final analysis for not endorsing SI in the 2 weeks prior to study participation. An additional three participants were removed for only completing one EMA assessment. The final analyses included N = 43 participants. Most participants were White (N = 27, 62.79%) and identified as cisgender women (N = 30, 69.77%). See Table 1 for complete participant demographics information. Participants who completed the study were compensated up to $35 and awarded up to six course credits based on the percentage of survey prompts completed.
TABLE 1.
Descriptive and demographic data for college student sample (N=43).
| n (%) | ICC | ICC CI | RMSSD | RMSSD range | |
|---|---|---|---|---|---|
| Demographics | |||||
| Age | M = 19.12(SD = 1.29) | ||||
| Race/ethnicity | |||||
| % White | 27 (62.79) | ||||
| % Black/African American | 9 (20.93) | ||||
| % Asian/Asian-American | 3 (6.98) | ||||
| % Latino (a) (Latinx) | 2 (4.65) | ||||
| % Biracial | 2 (14.65) | ||||
| Gender | |||||
| % Woman | 30 (69.77) | ||||
| % Man | 6 (13.95) | ||||
| % Gender non-conforming | 5 (11.63) | ||||
| % Not listed | 2 (4.65) | ||||
| Sexual orientation | |||||
| % Straight | 18 (41.86) | ||||
| % Gay or lesbian | 3 (6.96) | ||||
| % Bisexual | 13 (30.23) | ||||
| % Not sure/not listed | 9 (20.93) | ||||
| DSI-SS past 2 weeks | |||||
| Total score | M = 3.98 (SD = 1.86) | ||||
| SBQR- How often have you thought of killing yourself in the past year? | M = 4 (SD = 0.98) | ||||
| Ambulatory assessment | |||||
| IH-TB | 0.36 (0.32) | 0.64 | 0.54, 0.74 | 0.20 | 0.01, 0.42 |
| IH-PB | 0.43 (0.31) | 0.53 | 0.43, 0.65 | 0.24 | 0.01, 0.41 |
| General hopelessness | 0.39 (0.31) | 0.37 | 0.28, 0.49 | 0.28 | 0.02, 0.44 |
| Suicidal desire | 0.18 (0.23) | 0.44 | 0.34, 0.56 | 0.19 | 0.01, 0.44 |
Note: Some percentages may not equate to 100% because participants could choose more than one option.
Abbreviations: CI, confidence interval; DSI-SS depressive symptom index-suicide subscale (range 0–12); ICC, intra-class correlation; IH-PB, interpersonal hopelessness-perceived burdensomeness; IH-TB, interpersonal hopelessness-thwarted belongingness; RMSSD, root mean square of successive differences.
Procedures
All procedures were approved by the University Institutional Review Board. Below, we describe the procedures for the various phases of the current study.
Baseline phase
Eligible participants were directed to a university research participation system where they could opt to sign up to participate in the study. Participants met with a research assistant via a video conferencing platform (Zoom) to provide informed consent, and they were informed of study procedures. After consenting, participants completed an online baseline survey through the online survey platform, Qualtrics. Immediately following the completion of the baseline survey, participants downloaded the PIEL EMA application (Jessup et al., 2012) on their smartphones. Participants were instructed to open a practice survey, and the research assistant guided the participant on how to use the application to answer daily survey prompts. Participants were informed that their responses would not be monitored throughout the duration of the study. All study participants were provided with local and national mental health resources (e.g., Suicide Prevention Lifeline) should the need for them arise. Participants were also guided through downloading and setting up the Virtual Hope Box mobile application as an additional resource if they experienced suicide-related distress (Moscardini et al., 2023).
EMA phase
Participants were prompted to respond to brief surveys (34 questions, 3–5 min per survey) five times per day for 10 days using the PIEL application. Participants received a notification on their smartphone to complete a survey at a random time during 3-h time blocks (e.g., 9 am–12 pm), five times per day between 9 am and 11:59 pm. Previous suicide-related EMA research has used a comparable number of pseudorandom surveys (e.g., four daily surveys in Kleiman et al., 2017) that varied from 2-h delays (Stenzel et al., 2020) to 4-to-8-h delays (Kleiman et al., 2017). After receiving a survey notification, participants had 60 min to begin a survey before it expired. Once a survey was started, participants had up to 30 min to complete it. The surveys included questions regarding suicidal desire, IH-TB, IH-PB, and general hopelessness. Emails were sent to study participants every other day during the EMA phase with reminders to complete the survey prompts, information on who to contact in the event of a problem, and a reminder of their study completion appointment.
Interpersonal hopelessness about thwarted belongingness and perceived burdensomeness
Self-reported IH-TB and IH-PB were measured using two questions from the Interpersonal Hopelessness Scale (IHS; Tucker et al., 2018), a questionnaire designed to assess hopelessness specific to the constructs of TB and PB outlined within the ITS. The subscales of the IHS have demonstrated excellent internal consistency (Mitchell et al., 2023), and item content was derived from the Interpersonal Needs Questionnaire (INQ; i.e., an assessment of TB and PB; Van Orden et al., 2012) and the Beck Hopelessness Scale (BHS: Beck et al., 1974), both of which have been previously validated. A question from the IH-TB subscale of the IHS, “I expect that people will never care about me,” was used to measure IH-TB in the current study, and a question from the IH-PB subscale of the IHS, “I believe I will always fail the people in my life,” was used to measure IH-PB (Tucker et al., 2018). The decision to use these items instead of others on the subscale was based on construct representativeness and factor loading strength from the finding demonstrated in Mitchell et al. (2023). Participants responded to statements using a continuous visual analogue slider scale that recorded responses up to two decimal places with anchors of zero (not at all) and one (completely) at each time point throughout the study.
General hopelessness
The question “How hopeless do you feel right now?” was asked at each time point, and participants responded to statements using a the previously described visual analogue slider scale.
Suicidal desire
At each of the daily prompts, participants were asked “How intense is your desire to kill yourself right now?” to assess active suicide desire (Kleiman et al., 2017). Participants responded to statements using the previously described visual analogue slider scale.
Debriefing
Following the 10-day EMA assessment period, all study participants met with a research assistant via Zoom to transfer their data from their cellphone to the researchers via email and arrange for compensation. Participants were encouraged to ask questions or raise concerns about study procedures.
Analytical strategy
All analyses were conducted in R (R Core Team, 2021) using the RStudio development environment (RStudio Team, 2022). All data analysis code and data that support the findings of this study are available at https://osf.io/pwamg/?view_only=a2e3c9529e734798baf08962a6eb96a5. The hypotheses and analytical strategy for the current study were not pre-registered. Descriptive statistics were conducted to determine means, standard deviations, range, and skew for variables of interest. Repeated measures correlation was conducted using the rmcorr package (Bakdash & Marusich, 2017) to determine the strength of relations among study variables. Repeated measures correlation accounts for the non-independence among observations without first averaging the data (Bakdash & Marusich, 2017). Consistent with previous EMA studies examining SI and risk factors for SI cross-sectionally and longitudinally (Kleiman et al., 2017; Stenzel et al., 2020), intraclass correlations (ICCs), root mean square of successive differences (RMSSD), and multilevel modeling (MLM) were used to analyze the data.
The first aim of the study was to investigate the temporal stability of IH-TB, IH-PB, and general hopelessness. To quantify the variability in the measure that can be attributed to between-person variability, ICCs were calculated from intercept only models (e.g., a MLM model with no predictor variables). As ICC is a measure of between-person variability, 1–ICC provides the proportion of variance that is attributed to within-person variability. An ICC value closer to one indicates higher similarity between persons. Using the ICC package (Wolak et al., 2012), ICCs of suicidal desire, general hopelessness, IH-TB, and IH-PB were calculated. Additionally, RMSSD was calculated using the psych package (Revelle, 2022) to show the average variability in the measure over time of suicidal desire, general hopelessness, IH-TB, and IH-PB. Larger RMSSD values indicate more variability from one time point to the next, on average. Lastly, to visually depict whether general hopelessness and the facets of IH follow similar patterns of change, the data were graphed using GGplot2.
The second aim of the study was to conduct the first prospective investigation of IH-TB, IH-PB, and suicidal desire using EMA. The relationships between predictor variables (e.g., general hopelessness, IH-TB, IH-PB) and suicidal desire were assessed using MLM. MLMs were conducted to account for the nested structure of the data, such that participants’ scores at each EMA assessment occasion (lower-level variables) were nested within person (upper-level variables). Models were analyzed using the nlme package in R and maximum log-likelihood estimation was used (Pinheiro et al., 2022). For all models, participants were set as a random factor. In line with previous works (Hallensleben et al., 2019; Kleiman et al., 2017), the predictor variables in our study were within-person mean centered,1 as we are interested in associations within person, considering their scores relative to their own mean score, rather than relative to all participants’ mean. Eight models were analyzed to examine the associations between the predictors (IH-TB, IH-PB, IH-TBxIH-PB, and general hopelessness) and suicidal desire. The first set of models examined concurrent suicidal desire. Model 1 examined IH-TB and IH-PB predicting concurrent suicidal desire. Model 2 added general hopelessness in as a predictor, with general hopelessness, IH-TB, and IH-PB predicting concurrent suicidal desire. Model 3 examined IH-TB, IH-PB, and IH-TBxIH-PB predicting concurrent suicidal desire. Model 4 examined IH-TB, IH-PB, IH-TBxIH-PB, and general hopelessness predicting concurrent suicidal desire. Deviance change tests using the difference in −2 Log Likelihood model fit statistics and differences in the number of model parameters were conducted to determine statistically significant change in model fit between models.
The second set of models included lagged analyses between predictor variables at T (e.g., general hopelessness, IH-TB, IH-PB, and IH-TBxIH-PB) predicting suicidal desire at time T + 1 using MLM. For time-lagged analyses, the last value of each day was not lagged. Suicidal desire at T was included in the models to control for autocorrelation with suicidal desire at T + 1. Model 5 examined IH-TB, IH-PB, and suicidal desire at T predicting suicidal desire at the next time point (T + 1). Model 6 added general hopelessness as a predictor, with general hopelessness, IH-TB, IH-PB, and suicidal desire at T predicting suicidal desire at T + 1. Model 7 examined IH-TB, IH-PB, IH-TBxIH-PB, and suicidal desire at T predicting suicidal desire at T + 1. Model 8 examined general hopelessness, IH-TB, IH-PB, IH-TBxIH-PB, and suicidal desire at T predicting suicidal desire at T + 1. Again, deviance change tests using the difference in −2 Log Likelihood were conducted to determined statistically significant change in model fit between models.
RESULTS
Participants completed an average of 42.88 surveys (range 20–50; out of 50 possible) during the 10-day ambulatory phase, resulting in k = 1844 completed surveys. Participants spent an average of 1 min and 46 s completing each survey (Range = 00:28–26:19, SD = 02:05). Temporal stability and reliability estimates were calculated using ICCs for predictor variables (see Table 1). Results of repeated measures correlations are shown in Table 2. All study variables exhibited moderate positive relationships (r values range = 0.31–0.44).
TABLE 2.
Repeated measures correlation matrix of study variables.
| General hopelessness | IH-PB | IH-TB | |
|---|---|---|---|
| General hopelessness | - | ||
| IH-PB | 0.42** | - | |
| IH-TB | 0.31** | 0.40** | - |
| Suicidal desire | 0.44** | 0.31** | 0.31** |
Abbreviations: IH-TB, interpersonal hopelessness-thwarted belongingness; IH-PB, interpersonal hopelessness-perceived burdensomeness.
p < 0.05
p < 0.01
p < 0.001.
ICCs indicated that 44.94% of the variance in suicidal desire, 36.15% of the variance in hopelessness, 53.04% in IH-PB, and 63.85% of the variance in IH-TB is between person, or explained by individual differences, as opposed to within person differences. RMSSD indicated some average variability between timepoints in all variables, with general hopelessness having the highest estimate (0.28). Higher RMSSD values indicate a stronger “saw-tooth” pattern when depicted graphically. Graphical depictions of the variables of interest can be seen in Figure 1 (see the Figure S1 for a color version).
FIGURE 1.
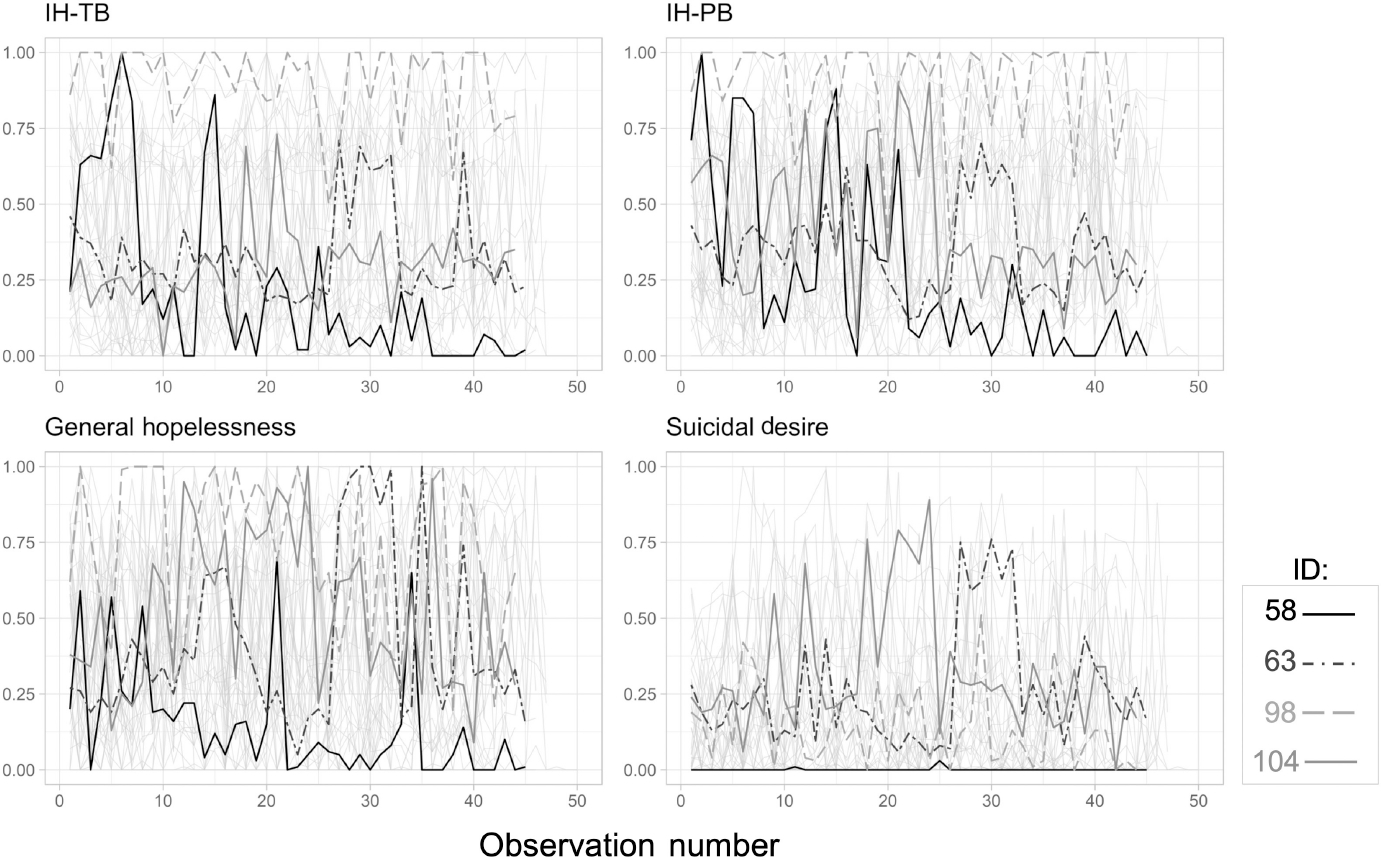
Time series plot of raw individual IH-PB, IH-TB, General hopelessness, and suicidal desire data. Highlighted subjects were randomly selected; IH-TB, interpersonal hopelessness-thwarted belongingness; IH-PB, interpersonal hopelessness-perceived burdensomeness; A color version of the figure can be found in the supplemental material (Figure S1).
Results from the four concurrent MLMs can be found in Table 3. In Model 1, both IH-TB and IH-PB were significant concurrent predictors of suicidal desire at baseline with small effect sizes (Marginal R2 = 0.08). The deviance −2 Log Likelihood test indicated that model fit was significantly improved with the inclusion of these predictors when compared to the intercept only model (χ2[Δdf = 2] = 264.60, p < 0.001). In Model 2, IH-TB, IH-PB, and general hopelessness remained significant concurrent predictors of suicidal desire with medium effect sizes (Marginal R2 = 0.13). The deviance −2 Log Likelihood test indicated that model fit was significantly improved with the inclusion of general hopelessness when compared to Model 1 (χ2[Δdf = 1] = 221.29, p < 0.001). In Model 3, IH-TB, IH-PB, and IH-TBxIH-PB were all significant concurrent predictors of suicidal desire at baseline with small effect sizes (Marginal R2 = 0.08). The deviance −2 Log Likelihood test indicated that model fit was significantly improved with the inclusion IH-TBxIH-PB when compared to model 1 (χ2[Δdf = 1] = 5.50, p = 0.019). In Model 4, IH-TB, IH-PB, IH-TBxIH-PB, and general hopelessness remained significant concurrent predictors of suicidal desire with medium effect sizes (Marginal R2 = 0.13). The deviance −2 Log Likelihood tests indicated that model fit was significantly improved with the inclusion of all predictors (IH-TB, IH-PB, IH-TBxIH-PB, and general hopelessness) when compared to model 2 (χ2[Δdf = 1] = 11.33, p < 0.001) and model 3 (χ2[Δdf = 1] = 227.12, p < 0.001).
TABLE 3.
Concurrent prediction models using multilevel regression analyses to test the relation between IH-TB, IH-PB, general hopelessness, and suicidal desire at T.
| Model 1 |
Model 2 |
Model 3 |
Model 4 |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fixed effects | β | SE | CI | t | β | SE | CI | t | β | SE | CI | t | β | SE | CI | t |
| Intercept | 0.19 | 0.02 | 0.14, 0.23 | 7.31*** | 0.19 | 0.02 | 0.14, 0.23 | 7 31*** | 0.18 | 0.02 | 0.14, 0.23 | 7.10*** | 0.18 | 0.02 | 0.14, 0.23 | 7.63*** |
| IH-TB | 0.20 | 0.02 | 0.16, 0.24 | 9.28*** | 0.15 | 0.02 | 0.11, 0.19 | 7.10*** | 0.18 | 0.02 | 0.13, 0.22 | 3 09*** | 0.12 | 0.02 | 0.08, 0.17 | 5.68*** |
| IH-PB | 0.18 | 0.02 | 0.14, 0.21 | 9.19*** | 0.08 | 0.02 | 0.04, 0.12 | 4.04*** | 0.17 | 0.02 | 0.13, 0.21 | 9.01*** | 0.07 | 0.02 | 0.03, 0.11 | 3.75*** |
| General | - | - | - | - | 0.25 | 0.02 | 0.22, 0.28 | 15 33*** | - | - | - | - | 0.25 | 0.02 | 0.22, 0.29 | 15.54*** |
| Hopelessness | ||||||||||||||||
| IH-TBxIH-PB | - | - | - | - | - | - | - | - | 0.17 | 0.07 | 0.03, 0.31 | 2.34* | 0.23 | 0.07 | 0.10, 0.36 | 3.37*** |
| Random effects | ||||||||||||||||
| σ2 | 0.03 | 0.02 | 0.03 | 0.02 | ||||||||||||
| Intercept (τ00) | 0.02 | 0.02 | 0.02 | 0.02 | ||||||||||||
| Marginal/conditional R2 | 0.08/0.52 | 0.13/0.58 | 0.08/0.52 | 0.13/0.58 | ||||||||||||
Abbreviations: CI, confidence interval; ICC, intraclass correlation: IH-PB, interpersonal hopelessness-perceived burdensomeness; IH-TB, interpersonal hopelessness-thwarted belongingness; IH-TBxIH-PB, interaction term of IH-TB and IH-PB; T, time.
Note: IH-TB and IH-PB were within-person centered with “IH-TBXIH-PB” representing the interaction of the within-person centered IH-TB and IH-PB variables.
p< 0.05
p<0.01
p< 0.001.
The results of the four time-lagged models are shown in Table 4. In Model 5, IH-TB and IH-PB were significant predictors of suicidal desire at time T + 1, with small effect sizes (Marginal R2 = 0.03), while controlling for autocorrelation of suicidal desire at T. The deviance −2 Log Likelihood test indicated that model fit was significantly improved with the inclusion of these predictors when compared to the intercept only model (χ2[Δdf = 3] = 108.79, p < 0.001). In Model 6, IH-TB and general hopelessness, but not IH-PB, were significant predictors of suicidal desire at T + 1 with small effect sizes (Marginal R2 = 0.04). The deviance −2 Log Likelihood test indicated that model fit was significantly improved with the inclusion of these general hopelessness when compared to model 5 (χ2[Δdf = 1] = 11.09, p = 0.001). In Model 7, IH-TB and IH-PB, but not IH-TBxIH-PB, were significant predictors of suicidal desire at T + 1 with small effect sizes (Marginal R2 = 0.03). The deviance −2 Log Likelihood test indicated that model fit was not significantly improved with the inclusion of IH-TBxIH-PB when compared to Model 5 (χ2[Δdf = 1] = 3.05, p = 0.081). In Model 8, IH-TB and general hopelessness were significant predictors of suicidal desire at time T + 1 with small effect sizes (Marginal R2 = 0.04), while IH-PB and IH-TBxIH-PB were not significant predictors. The deviance −2 Log Likelihood tests indicated that model fit was not significantly improved with the inclusion of all predictors (IH-TB, IH-PB, IH-TBxIH-PB, and general hopelessness) when compared to Model 6 (χ2[Δdf = 1] = 2.23, p = 0.14). However, the inclusion of all predictors (IH-TB, IH-PB, IH-TBxIH-PB, and general hopelessness) significantly improved model fit compared to model 7 (χ2[Δdf = 1] = 10.27, p = 0.002). Given significant prospective relationships between predictor variables and suicidal desire, post-hoc analyses were conducted to further test the temporal associations between IH-TB, IH-PB, IH-TBxIH-PB, and suicidal desire. Three reverse-direction models exploring whether suicidal desire at T predicts IH-TB, IH-PB, or IH-TBxIH-PB at T + 1 were conducted. Results for the three models were not significant. Model results can be found in Table S1 of the supplemental materials.
TABLE 4.
Prospective prediction models using multilevel regression analyses to test the relation between IH-TB, IH-PB, general hopelessness, and suicidal desire at T +1.
| Model 5 |
Model 6 |
Model 7 |
Model 8 |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Fixed effects | β | SE | CI | t | β | SE | CI | t | β | SE | CI | t | β | SE | CI | t |
| Intercept | 0.18 | 0.02 | 0.14, 0.23 | 7.82*** | 0.18 | 0.02 | 0.14, 0.23 | 7.83*** | 0.19 | 0.02 | 0.14, 0.23 | 7.91*** | 0.19 | 0.02 | 0.14, 0.23 | 7.89*** |
| IH-TB | 0.07 | 0.02 | 0.03, 0.12 | 3.07** | 0.06 | 0.02 | 0.02, 0.11 | 2.71** | 0.08 | 0.02 | 0.04, 0.13 | 3 45*** | 0.07 | 0.02 | 0.03, 0.12 | 3.04** |
| IH-PB | 0.05 | 0.02 | 0.01, 0.09 | 2.33* | 0.03 | 0.02 | −0.01, 0.07 | 1.31 | 0.05 | 0.02 | 0.01, 0.09 | 2.43* | 0.03 | 0.02 | −0.01, 0.07 | 1.42 |
| Suicidal desire | 0.17 | 0.02 | 0.13, 0.22 | 7.04*** | 0.14 | 0.03 | 0.09, 0.20 | 5.50*** | 0.18 | 0.02 | 0.13, 0.23 | 7.34*** | 0.15 | 0.03 | 0.10, 0.20 | 5.60*** |
| General | - | - | - | - | 0.06 | 0.02 | 0.03, 0.10 | 3.33*** | - | - | - | - | 0.06 | 0.02 | 0.02, 0.10 | 3.20** |
| Hopelessness | ||||||||||||||||
| IH-TBxIH-PB | - | - | - | - | - | - | - | - | −0.14 | 0.08 | −0.28, 0.02 | −1.75 | −0.11 | 0.08 | −0.26, 0.04 | −1.49 |
| Random effects | ||||||||||||||||
| σ2 | 0.03 | 0.03 | 0.03 | 0.03 | ||||||||||||
| Intercept (τ00) | 0.01 | 0.02 | 0.01 | 0.02 | ||||||||||||
| MARGiNAL/conditional R2 | 0.03/0.48 | 0.04/0.48 | 0.03/0.48 | 0.04/0.48 | ||||||||||||
Abbreviations: CI, confidence interval; ICC, intraclass correlation; IH-PB, interpersonal hopelessness-perceived burdensomeness; IH-TB, interpersonal hopelessness-thwarted belongingness; IH-TBxIH-PB, interaction term of IH-TB and IH-PB.
Note: IH-TB, IH-PB, and suicidal desire were within-person centered with “IH-TBXIH-PB” representing the interaction of the within-person centered IH-TB and IH-PB variables.
p < 0.05
p < 0.01
p < 0.001.
DISCUSSION
The ITS theorizes that a simultaneous presence of TB and PB, as well as hopelessness about the tractability of these states is sufficient to lead to suicidal desire (Van Orden et al., 2010). The IHS measures hopelessness specific to the interpersonal constructs of TB and PB (Tucker et al., 2017), and recent findings support a two-f actor solution (IH-TB and IH-PB; Mitchell et al., 2023). The current study is the first to explore the daily experiences of these constructs among individuals prescreened for past-2-week SI using EMA.
Consistent with the first hypothesis, findings indicate that IH-TB, IH-PB, and general hopelessness all dynamically varied over the course of the day as evidenced by the RMSSD values (IH-TB = 0.20, IH-PB = 0.24, General Hopelessness = 0.28) and graphical depictions of the raw data. These findings are consistent with previous research that has found considerable short-term variability in SI and SI risk factors (Hallensleben et al., 2019; Kleiman et al., 2017). Regarding the second hypothesis, IH-TB and IH-PB exhibited visually higher between-person variation than general hopelessness when examining the ICCs (IH-TB = 0.64, IH-PB = 0.53, general hopelessness = 0.36). The RMSSD values suggest that general hopelessness was more variable between timepoints than IH-TB, IH-PB, and suicidal desire (IH-TB = 0.20, IH-PB = 0.24, suicidal desire = 0.19, Hopelessness = 0.28). Phenomenologically, this could point to the relative stability of interpersonal variants of hopelessness when compared to broad, general conceptions of hopelessness. These analyses suggest that general hopelessness may be more variable from one timepoint to the next than hopeless perceptions of burdensomeness or hopelessness regarding one’s belonging.
Connecting the temporal dynamics of these constructs to what is seen in the existing literature is obscured by differences in study design and sample characteristics. When compared to Kleiman et al.’s (2017) investigations of adults recently treated for suicidal thoughts and behaviors and Forkmann et al.’s (2018) investigation of psychiatric inpatients reporting current or lifetime SI, general hopelessness and suicidal desire in the current investigation exhibit more within person variance (suicidal desire = 0.45, general hopelessness ICC = 0.36). For reference, in the study by Kleiman et al. (2017), SI had ICCs ranging from 0.53 to 0.67, while general hopelessness had ICCs ranging from 0.57 to 0.66. In the study by Forkmann et al. (2018), SI had an ICC of 0.73 and hopelessness had an ICC of 0.74. These differences could be the result of the study of the more clinically severe samples represented by both Kleiman et al. (2017) and Forkmann et al. (2018). In both studies, samples of psychiatric inpatients were included (Forkmann et al., 2018; Kleiman et al., 2017) while the current study utilized college students prescreened for past-2-week SI.
While no investigations to date have explored the temporal dynamics of IH-TB or IH-PB, the study by Kleiman et al. (2017) measured TB and PB using one word affect labels (“loneliness” and “burdensomeness”). If we compare these constructs to those measured in the current study, IH-TB (“loneliness”; ICC = 0.64) had similar within-person variation than “loneliness” (ICC’s range from 0.41 to 0.61), while IH-PB (“burdensomeness”; ICC = 0.53) had similar within person variability than “burdensomeness” (ICC = 0.58). While not directly comparable, there are similar patterns exhibited between the constructs across studies.
When examined concurrently and prospectively, the main effects of IH-TB and IH-PB were both predictive of suicidal desire at T and T + 1 (with suicidal desire at the previous time point considered) when not adjusting for general hopelessness. These findings are in line with the hypothesis outlined in the ITS, that the simultaneous presence of PB and TB is a potentially proximal cause of suicidal desire (Van Orden et al., 2010). Within the current study, the item assessing suicidal thoughts is specific to suicidal desire (“How intense is your desire to kill yourself right now?”), which further supports the theory outlined by Van Orden et al. (2010) that IH is related to suicidal desire, not simply passive thoughts of death. Additionally, whether adjusting for general hopelessness or not, the interaction of IH-TBxIH-PB was predictive of suicidal desire concurrently, but not prospectively while considering suicidal desire at the previous timepoint. This could be explained by the relatively short duration of suicidal crises (Deisenhammer et al., 2009) in addition to the dynamic fluctuation seen in risk factors for suicide (Kleiman et al., 2017). However, it may be that when considering suicidal desire at the next time point, the interaction of IH-TBxIH-PB is not prospectively related to suicidal desire above and beyond main effects. Additionally, as noted by Mitchell et al. (2019), the hypothesis outlined by Van Orden et al. (2010) may be more accurately tested by examining the additive effects of TB and PB, instead of the interactions. In the current study, it could be that IH-TB and IH-PB are not synergistically related, but instead additive when adjusting for suicidal desire at previous time points.
Inconsistent with our hypothesis that IH-TB and IH-PB would better predict suicidal desire both concurrently and prospectively than general hopelessness, IH-TB and IH-PB were not stronger unique predictors of suicidal desire than general hopelessness. In the concurrent model (Table 3, Model 2), general hopelessness (β = 0.25) has a higher estimate and non-overlapping confidence intervals with IH-TB (β = 0.15) and IH-PB (β = 0.08). Although IH-TB and IH-PB were both concurrently and prospectively related to suicidal desire when excluding general hopelessness from the model (Models 1 and 5), only IH-TB was prospectively related to suicidal desire at T + 1 when general hopelessness and suicidal desire at T were considered (Model 6). This finding is unexpected given the central role IH is hypothesized to have on suicidal desire. One possible explanation is the use of single-item constructs. It is possible that the use of a single item is sufficient for assessing general hopelessness but not for interpersonal variants of hopelessness. Further, as discussed in more detail in the limitations, the lack of a temporal descriptor (i.e., “right now”) for the IH-TB and IH-PB items may have limited our ability to draw in the moment conclusions.
Finally, our hypothesis that the interaction of IH-TBxIH-PB would concurrently and prospectively predict suicidal desire above and beyond the main effect of general hopelessness was also not supported. While the estimate of IH-TBxIH-PB (β = 0.23) is similar to that of general hopelessness (β = 0.25) in the concurrent models, general hopelessness has a narrower confidence interval (CI = 0.22, 0.28), suggesting more stability than the interaction of IH-TBxIH-PB (CI = 0.10, 0.36). Additionally, model fit improved in all models in which general hopelessness was added, whereas IH-TBxIH-PB was not significant in any of the prospective models and therefore model fit was not improved with the addition of IH-TBxIH-PB. As mentioned previously, it is possible that the interaction of IH-TBxIH-PB is not associated with suicidal desire above and beyond main effects. Additionally, as pointed out by Mitchell et al. (2019), the hypothesis outlined by Van Orden et al. (2010) indicates that these constructs may be additive in nature and therefore are not accurately tested through an interaction term. Overall, suicidal desire at T was the strongest predictor of SI at T + 1, consistent with past research (Kleiman et al., 2017).
The fact that the main effect of IH-PB was no longer significant in Model 6 appears related to the addition of general hopelessness. It is possible that IH-PB is no longer significant due to the stronger correlation between general hopelessness and IH-PB (r = 0.42) when compared to the correlation between general hopelessness and IH-TB (r = 0.31), reducing the unique association between IH-PB and suicidal desire when also adjusting the previous suicidal desire. The fact that IH-PB was no longer a significant predictor of prospective SI appears contrary to existing literature. In a systematic review of the literature on the ITS, Ma et al. (2016) found that the effect of PB on SI was the most tested and supported relationship in the literature when compared to TB and other variables of the ITS. Over three-quarters of the studies examined in the literature review yielded significant main effects of PB on SI across various settings, while TB was tested less frequently and yielded insignificant results in over half of the studies examined (Ma et al., 2016). One possible explanation for the findings in the current study could be that the studies included in the Ma et al. (2016) review did not focus on hopelessness or IH, thus providing only partial tests of the ITS hypotheses. Further, the studies included in the review by Ma et al. (2016) relied on the INQ to measure TB and PB. The INQ may be a more stable assessment of PB than the single-item assessment of IH-PB used in the current study. Hopeless perceptions of burdensomeness may be more fleeting in nature than TB, PB, or IH-TB, which would lessen the ability of IH-PB to predict suicidal desire at future timepoints.
An additional explanation for our findings is a possible effect of gender. Donker et al. (2014) found that while PB was associated with increased SI in both men and women, TB was associated with increases in SI in women only. The sample in the current study identified as mostly cisgender women (N = 30, 69.77%), which could explain why IH-TB remained significant in the model, while IH-PB did not. However, we would be under powered to test gender effects given our sample size, leaving this postulation to be tested future studies. Moreover, it is possible that hopelessness regarding PB may not be as strong of a predictor of suicidal desire as PB on its own.
Finally, post-hoc analyses were conducted to determine whether the findings exist in the opposite direction to further speculate on temporal relationships between study variables. None of the post-hoc models supported the opposite temporal relationships from what was hypothesized. This aligns with the hypothesis outlined in the ITS that states “thwarted belongingness and perceived burdensomeness … [are] a proximal and sufficient cause of active suicidal desire” (Van Orden et al., 2010, p. 589). Thus, the ITS does not posit that the experience of SI subsequently increases IH-TB and/or IH-PB, and current results appear to support not adapting the model to do so. These findings suggest that when IH-TB and IH-PB increase, risk for active suicidal desire increases at future timepoints.
Limitations & future directions
The results of the current study should be interpreted in light of methodological limitations. First, there were no measures of TB or PB (excluding hopelessness) included within the EMA portion of study, so we were unable to further determine any associations between IH-TB and TB and IH-PB and PB. Given strong correlations found between IH-PB and PB in particular (Mitchell et al., 2023), future EMA research should include both measures of TB/PB and their interpersonal variants to determine relative stability as well as their interactive relationship with suicidal desire. Additionally, while the study sample was rather diverse regarding race/ethnicity and sexual orientation, this was a relatively small undergraduate sample that primarily consisted of cisgender young adult women. Future studies should replicate these results in more diverse samples to determine the broader generalizability of these findings. Similarly, the current study did not collect information on participants’ cultures and geographic backgrounds or measures of socioeconomic status. The sample was comprised exclusively of undergraduate students. Therefore, results may not generalize to clinical populations (e.g., psychiatric inpatients, treatment seeking versus non-treatment seeking adults, etc.), despite prescreening our sample for past-2-week SI. Additionally, it is unclear how the constructs of general hopelessness, IH-TB, and IH-PB function in individuals without SI as all participants at baseline indicated past-2-week SI. Future research could benefit from measuring these constructs in individuals without a recent history of suicidal desire as many psychological theories of suicide, including the ITS, delineate how SI develops and how it intensifies (Klonsky & May, 2015; Van Orden et al., 2010).
While EMA allows for the examination of temporal fluctuations in these constructs, it is possible that a more nuanced investigation is required to fully capture the fluctuations of these constructs. It could be that the time delay between surveys (about 3 h) missed important fluctuations in the constructs of interest. Further, the ITS does not explicitly define the timescale of “proximal” suicide risk and how soon before the onset of suicidal desire should IH occur. It is possible that interpersonal variants of hopelessness are a stronger predictor of suicidal desire at longer time intervals (e.g., next day). Coppersmith et al. (2023) found that current suicidal desire was predictive of future suicidal desire up to 20 h later, so it is possible that interpersonal variants of hopelessness could continue to predict suicidal desire at later timepoints. Future research would benefit by exploring the predictive ability of these constructs on longer timescales. Another limitation of the current study is the length of time participants had to begin the assessments. Participants were able to delay the start of the survey by up to 60 min, which could have severely limited the moment-r elatedness of the study. Additionally, one notable limitation of the current study is that the items used to assess IH-TB and IH-PB did not include moment-related wording (i.e., “right now”) compared to all other variables assessed. The IH items lacked a temporal descriptor (e.g., “I believe I will always fail the people in my life” and “I expect that people will never care about me”), while the general hopelessness and suicidal desire items included the descriptor “right now” (e.g., “How hopeless do you feel right now?”). It is possible that the lack of temporal description in the item itself dampened within person variability in IH-TB and IH-PB, relative to the other suicidal desire and general hopelessness, which is supported by the lower RMSSD values exhibited by IH-TB (0.20) and IH-PB (0.24) compared to general hopelessness (0.28). Further, the observed stronger temporal stability of the IH variables compared to general hopelessness could be the result of the item wording. Finally, a bi-polar visual-analogue slider scale was used in the current study, meaning that any responses provided between the two anchors is somewhat ill-defined and can only be interpreted in reference to their general relation to the poles. Future research could benefit from utilizing Likert-style responses.
Conclusions
The interpersonal constructs of IH-TB and IH-PB represent important risk factors within the ITS, as well as potential targets for intervention. It is important to understand individuals’ day-to-day experiences with suicidal desire and risk factors to better inform theory and improve interventions and treatments (Kleiman et al., 2017). Results were consistent with previous research showing the dynamic variability of IH-TB, IH-PB, general hopelessness, and suicidal desire over the course of the day. These results suggest that while the fluctuations in IH-TB and IH-PB are similar to general hopelessness, they may be slightly more stable over time. Additionally, results suggest that the main effects IH-TB and IH-PB, and the interaction of IH-TBxIH-PB are significant predictors of suicidal desire concurrently (regardless of whether adjusting for general hopelessness), although not as predictive as general hopelessness. When examined prospectively, the main effects IH-TB and IH-PB, though not the interaction of IH-TBxIH-PB, are predictive of suicidal desire. However, when including general hopelessness in the model the main effect of IH-PB is no longer significant. While general hopelessness is an important and beneficial target in many therapies for individuals experiencing suicidal desire (e.g., CAMS; Jobes, 2016, BCBT; Bryan & Rudd, 2018), these results show that interventions aimed at decreasing one’s hopelessness specific to TB and PB may be beneficial for decreasing suicidal desire. Future research should seek to replicate these results in larger and more diverse samples and consider the use of shorter ambulatory assessment intervals (Coppersmith et al., 2023).
Supplementary Material
FUNDING INFORMATION
Time for this research was supported, in part, by funding from the National Institute of Mental Health (L30MH120575) and the Military Suicide Research Consortium (MSRC), an effort supported by the Office of the Assistant Secretary of Defense for Health Affairs under Award No. (W81XWH-16–2–0004).
Footnotes
Although the current analyses focus on within-person effects, other work utilizing multilevel models have shown the importance of also modeling between-person effects (Rogers et al., 2022). As such, additional models that include between-person effects can be found in Tables S2 and S3.
CONFLICT OF INTEREST STATEMENT
The authors have no conflicts of interest to disclose.
SUPPORTING INFORMATION
Additional supporting information can be found online in the Supporting Information section at the end of this article.
REFERENCES
- Bakdash JZ, & Marusich LR (2017). Repeated measures correlation. Frontiers in Psychology, 8, 456. 10.3389/fpsyg.2017.00456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Weissman A, Lester D, & Trexler L (1974). The measurement of pessimism: The hopelessness scale. Journal of Consulting and Clinical Psychology, 42(6), 861–865. 10.1037/h0037562 [DOI] [PubMed] [Google Scholar]
- Bryan CJ, & Rudd MD (2018). Brief cognitive-behavioral therapy for suicide prevention. Guilford Publications. [Google Scholar]
- Chu C, Buchman-Schmitt JM, Stanley IH, Hom MA, Tucker RP, Hagan CR, Rogers ML, Podlogar MC, Chiurliza B, Ringer FB, Michaels MS, Patros CHG, & Joiner TE Jr. (2017). The interpersonal theory of suicide: A systematic review and meta-analysis of a decade of cross-national research. Psychological Bulletin, 143(12), 1313–1345. 10.1037/bul0000123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coppersmith DDL, Ryan O, Fortgang RG, Millner AJ, Kleiman EM, & Nock MK (2023). Mapping the timescale of suicidal thinking. Proceedings of the National Academy of Sciences of the United States of America, 120(17), e2215434120. 10.1073/pnas.2215434120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deisenhammer EA, Ing CM, Strauss R, Kemmler G, Hinterhuber H, & Weiss EM (2009). The duration of the suicidal process: How much time is left for intervention between consideration and accomplishment of a suicide attempt? Journal of Clinical Psychiatry, 70(1), 19–24. 10.4088/JCP.07m03904 [DOI] [PubMed] [Google Scholar]
- Donker T, Batterham PJ, Van Orden KA, & Christensen H (2014). Gender-differences in risk factors for suicidal behaviour identified by perceived burdensomeness, thwarted belongingness and acquired capability: Cross-sectional analysis from a longitudinal cohort study. BMC Psychology, 2(1), 1–10. 10.1186/2050-7283-2-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forkmann T, Glaesmer H, Paashaus L, Rath D, Schönfelder A, Juckel G, Gauggel S, Beginn-Göbel U, & Teismann T (2021). Testing the four main predictions of the interpersonal–psychological theory of suicidal behavior in an inpatient sample admitted due to severe suicidality. Behavior Therapy, 52(3), 626–638. 10.1016/j.beth.2020.08.002 [DOI] [PubMed] [Google Scholar]
- Forkmann T, Spangenberg L, Rath D, Hallensleben N, Hegerl U, Kersting A, & Glaesmer H (2018). Assessing suicidality in real time: A psychometric evaluation of self-report items for the assessment of suicidal ideation and its proximal risk factors using ecological momentary assessments. Journal of Abnormal Psychology, 127(8), 758. 10.1037/abn0000381 [DOI] [PubMed] [Google Scholar]
- Hagan CR, Podlogar MC, Chu C, & Joiner TE (2015). Testing the interpersonal theory of suicide: The moderating role of hopelessness. International Journal of Cognitive Therapy, 8(2), 99–113. 10.1521/ijct.2015.8.2.99 [DOI] [Google Scholar]
- Hallensleben N, Glaesmer H, Forkmann T, Rath D, Strauss M, Kersting A, & Spangenberg L (2019). Predicting suicidal ideation by interpersonal variables, hopelessness and depression in real-time. An ecological momentary assessment study in psychiatric inpatients with depression. European Psychiatry, 56(1), 43–50. 10.1016/j.eurpsy.2018.11.003 [DOI] [PubMed] [Google Scholar]
- Hansen M (2021). College enrollment & student demographic statistics. Education Data Initiative https://educationdata.org/college-enrollment-statistics [Google Scholar]
- Jessup GM, Bian S, Chen YW, & Bundy A (2012). PIEL survey application manual. https://core.ac.uk/download/pdf/41237186.pdf [Google Scholar]
- Jobes DA (2016). Managing suicidal risk: A collaborative approach. Guilford Publications. [Google Scholar]
- Jobes DA, & Joiner TE (2019). Reflections on suicidal ideation [editorial]. Crisis: The Journal of Crisis Intervention and Suicide Prevention, 40(4), 227–230. 10.1027/0227-5910/a000615 [DOI] [PubMed] [Google Scholar]
- Joiner TE Jr., Pfaff JJ, & Acres JG (2002). A brief screening tool for suicidal symptoms in adolescents and young adults in general health settings: Reliability and validity data from the Australian national general practice youth suicide prevention project. Behaviour Research and Therapy, 40(4), 471–481. 10.1016/S0005-7967(01)00017-1 [DOI] [PubMed] [Google Scholar]
- Joiner TE, Jeon ME, Lieberman A, Janakiraman R, Duffy ME, Gai AR, & Dougherty SP (2021). On prediction, refutation, and explanatory reach: A consideration of the interpersonal theory of suicidal behavior. Preventive Medicine, 152, 106453. 10.1016/j.ypmed.2021.106453 [DOI] [PubMed] [Google Scholar]
- Kleiman EM, & Nock MK (2018). Real-time assessment of suicidal thoughts and behaviors. Current Opinion in Psychology, 22, 33–37. 10.1016/j.copsyc.2017.07.026 [DOI] [PubMed] [Google Scholar]
- Kleiman EM, Turner BJ, Fedor S, Beale EE, Huffman JC, & Nock MK (2017). Examination of real-time fluctuations in suicidal ideation and its risk factors: Results from two ecological momentary assessment studies. Journal of Abnormal Psychology, 126(6), 726–738. 10.1037/abn000027 [DOI] [PubMed] [Google Scholar]
- Klonsky ED, & May AM (2015). The three-step theory (3ST): A new theory of suicide rooted in the “ideation-to-action” frame-work. International Journal of Cognitive Therapy, 8(2), 114–129. 10.1521/Ijct.2015.8.2.114 [DOI] [Google Scholar]
- Ma J, Batterham PJ, Calear AL, & Han J (2016). A systematic review of the predictions of the interpersonal–psychological theory of suicidal behavior. Clinical Psychology Review, 46, 34–45. 10.1016/j.cpr.2016.04.008 [DOI] [PubMed] [Google Scholar]
- Mitchell SM, Brown SL, Moscardini EH, LeDuc M, & Tucker R (2023). A psychometric evaluation of the interpersonal hopelessness scale among individuals with elevated suicide risk. Assessment. 10.1177/10731911231161766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitchell SM, Brown SL, Roush JF, Tucker RP, Cukrowicz KC, & Joiner TE (2019). The interpersonal needs questionnaire: statistical considerations for improved clinical application. Assessment, 27(3), 621–637. 10.1177/1073191118824660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mortier P, Cuijpers P, Kiekens G, Auerbach RP, Demyttenaere K, Green JG, Kessler RC, Nock MK, & Bruffaerts R (2018). The prevalence of suicidal thoughts and behaviours among college students: A meta-analysis. Psychological Medicine, 48(4), 554–565. 10.1017/S0033291717002215 [DOI] [PubMed] [Google Scholar]
- Moscardini EH, Le TP, Cowan T, Gerner JL, Robinson A, Cohen AS, & Tucker RP (2023). Frequency and predictors of virtual hope box use in individuals experiencing suicidal ideation: An ecological momentary assessment investigation. Manuscript submitted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinheiro J, Bates D, & R Core Team. (2022). Nlme: Linear and nonlinear mixed effects models. R Package Version, 3, 1–157. https://CRAN.R-project.org/package=nlme [Google Scholar]
- R Core Team. (2021). R: A language and environment for statistical computing. R Foundation for Statistical Computing; https://www.R-project.org/ [Google Scholar]
- Revelle W (2022). Psych: Procedures for personality and psychological research. Northwestern University, Evanston, Illinois: https://CRAN.R-project.org/package=psych Version = 2.2.5 [Google Scholar]
- Roeder KM, & Cole DA (2019). Simultaneous longitudinal examination of hopelessness, thwarted belongingness, and perceived burdensomeness as predictors of suicide ideation. Suicide and Life-Threatening Behavior, 49(4), 1058–1071. 10.1111/sltb.12508 [DOI] [PubMed] [Google Scholar]
- Rogers ML, Jeon ME, Duffy ME, & Joiner TE (2022). Thinking too much: Rumination as a catalyst of the real-time associations between affective states and suicidal ideation. Journal of Consulting and Clinical Psychology, 90(9), 670–681. 10.1037/ccp0000753 [DOI] [PubMed] [Google Scholar]
- Team RStudio. (2022). RStudio: Integrated development environment for R. RStudio; http://www.rstudio.com/ [Google Scholar]
- Stenzel JS, Höller I, Rath D, Hallensleben N, Spangenberg L, Glaesmer H, & Forkmann T (2020). Do feelings of defeat and entrapment change over time? An investigation of the integrated motivational—Volitional model of suicidal behaviour using ecological momentary assessments. International Journal of Environmental Research and Public Health, 17(13), 4685. 10.3390/ijerph17134685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2021). Key substance use and mental health indicators in the United States: Results from the 2020 National Survey on drug use and health (HHS publication No. PEP21–07-01 003, NSDUH series H-56). Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; https://www.samhsa.gov/data/ [Google Scholar]
- Tucker RP, Hagan CR, Hill RM, Slish ML, Bagge CL, Joiner TE, & Wingate LRR (2018). Empirical extension of the interpersonal theory of suicide: Investigating the role of interpersonal hopelessness. Psychiatry Research, 259, 427–432. 10.1016/j.psychres.2017.11.005 [DOI] [PubMed] [Google Scholar]
- Van Orden KA, Cukrowicz KC, Witte TK, & Joiner TE Jr. (2012). Thwarted belongingness and perceived burdensomeness: Construct validity and psychometric properties of the interpersonal needs questionnaire. Psychological Assessment, 24(1), 197–215. 10.1037/a0025358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, & Joiner TE (2010). The interpersonal theory of suicide. Psychological Review, 117(2), 575–600. 10.1037/a001869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolak ME, Fairbairn DJ, & Paulsen YR (2012). Guidelines for estimating repeatability. Methods in Ecology and Evolution, 3(1), 129–137. 10.1111/j.2041-210X.2011.00125.x [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


