Abstract
Background:
Nearly 1 million Americans are living with multiple sclerosis (MS) and 30–50% will experience memory dysfunction. It remains unclear whether this memory dysfunction is due to overall white matter lesion burden or damage to specific neuroanatomical structures. Here we test if MS memory dysfunction is associated with white matter lesions to a specific brain circuit.
Methods:
We performed a cross-sectional analysis of standard structural images and verbal memory scores as assessed by immediate recall trials from 431 patients with MS (mean age 49.2 years, 71.9% female) enrolled at a large, academic referral center. White matter lesion locations from each patient were mapped using a validated algorithm. First, we tested for associations between memory dysfunction and total MS lesion volume. Second, we tested for associations between memory dysfunction and lesion intersection with an a priori memory circuit derived from stroke lesions. Third, we performed mediation analyses to determine which variable was most associated with memory dysfunction. Finally, we performed a data-driven analysis to derive de-novo brain circuits for MS memory dysfunction using both functional (n=1000) and structural (n=178) connectomes.
Results:
Both total lesion volume (r=0.31, p<0.001) and lesion damage to our a priori memory circuit (r=0.34, p<0.001) were associated with memory dysfunction. However, lesion damage to the memory circuit fully mediated the association of lesion volume with memory performance. Our data-driven analysis identified multiple connections associated with memory dysfunction, including peaks in the hippocampus (T=6.05, family-wise error p=0.000008), parahippocampus, fornix and cingulate. Finally, the overall topography of our data-driven MS memory circuit matched our a priori stroke-derived memory circuit.
Conclusions:
Lesion locations associated with memory dysfunction in MS map onto a specific brain circuit centered on the hippocampus. Lesion damage to this circuit fully mediated associations between lesion volume and memory. A circuit-based approach to mapping MS symptoms based on lesions visible on standard structural imaging may prove useful for localization and prognosis of higher order deficits in MS.
Keywords: multiple sclerosis, memory, white matter lesion, lesion network mapping, fMRI
Introduction
Nearly 1 million Americans are living with multiple sclerosis (MS) and around 30–50% will experience memory dysfunction.[1–4] Focal central nervous system lesions, primarily in the white matter, are the hallmark diagnostic marker of MS[5] and the main imaging surrogate used to monitor disease progression and assess treatment responsiveness.[6] White matter lesions (WML) are easily visualized on standard brain MRI and correspond with areas of demyelination and axonal injury.[4] Accumulation of WMLs is associated with both worsening cognition in general and worsening memory;[7–15] however, this finding is not specific to memory as total lesion burden has also been associated with worsening fatigue,[16] depression[17] and gait dysfunction.[18, 19] Efforts to relate lesion locations visible on standard MRI to memory have produced conflicting results.[7–15, 20–26] Previous studies have associated memory dysfunction with lesions in the temporal lobe[25, 26], hippocampus[13], and at least 10 other brain regions not typically associated with memory[7, 10–12, 15, 20–24] leading to questions as to whether there is any neuroanatomical relationship between MS lesion location and memory dysfunction.[10, 27] This is in contrast to other brain diseases where symptoms associated with a lesion location often align with the known function of that region[28, 29] leaving a gap in understanding the relationship between MS lesion locations and memory dysfunction.
One advance that has helped with symptom localization in ischemic stroke is the ability to test whether different lesions causing a common symptom map to a connected brain circuit rather than a single brain region.[30] This technique, termed lesion network mapping (LNM), uses an atlas of normative brain connectivity to identify brain regions connected to each lesion location.[30–38] Connections associated with a specific symptom can then be identified. In a recent study[36], stroke lesions causing memory dysfunction occurred in many different brain locations, but they were all part of a functionally connected brain circuit centered on the hippocampus.[36] This lesion-based memory circuit aligned with neuroanatomical models of memory[39], including the classic circuit of Papez. Intersection of lesion locations with this memory circuit also correlated with memory dysfunction in independent lesion datasets.[36] As such, this stroke-based memory circuit provides an a priori template that may be useful for investigating MS memory dysfunction.
Despite the success of lesion network mapping to map the connectivity of stroke-associated lesions, there are many differences between stroke lesions and MS lesions, and the network mapping approach that has worked well for stroke may not work well in MS. Unlike stroke lesions, MS lesions are more distributed, multi-focal, progressive, and can be clinically silent.[40] Though MS is radiologically defined primarily by white matter lesions,[5] cognitive deficits may come from more subtle grey matter injury rather than the white matter lesions.[1, 41] Finally, it’s unclear whether fMRI signal fluctuations at white matter lesion locations have sufficient signal for network mapping [42]. However, there are also reasons to think that a network mapping approach could be successful in MS, as it has worked well in other conditions with progressive, multi-focal lesions such as tuberous sclerosis [35] and worked well in a recent lesion network mapping study of MS depression.[43]
Materials and Methods
Patient population and testing
Patient data for the current study is a retrospective, cross-sectional analysis of data from “Systems Biology Study of Clinical, Radiological, and Molecular Markers in Subjects with Multiple Sclerosis” (SysteMS). The SysteMS study is a broader, prospective, clinical, MRI and biomarker study of patients with MS designed to identify factors associated with MS disease severity and progression conducted at Brigham and Women’s Hospital from September 2015-December 2019.[44] All patients within SysteMS were included the present study who: 1) met McDonald criteria for MS or clinically isolated syndrome (CIS), 2) completed memory testing and 3) structural MRI brain suitable for lesion segmentation. We included the earliest imaging scan and verbal memory assessment. We also completed subgroup analyses limited to: 1) patients imaged on the same scanner type (Siemens Skyra) within 90 days of cognitive testing and 2) patients with relapsing-remitting MS (RRMS). We employed the California Verbal Learning Test-II (CVLT-II) total immediate recall trials 1–5 as a marker of verbal memory since immediate recall trials are recommended to detect verbal memory dysfunction in MS [45–47] and initial learning/acquisition seem most impacted.[48] Memory scores were inverted for the analysis so a higher score reflects worse performance.
Structural neuroimaging
Structural neuroimaging was performed primarily on Siemens Skyra 3T MRI scanner (98.8% of images); however, three images were on Siemens Verio and two on Siemens Avanto scanners. (See Supplementary Table 1 for further specifications.)
The automated segmentation pipeline has been described in detail previously[49] and, in brief, employs structural brain MRI to parcellate T2 hyperintense WMLs employing a dual-sensitivity approach for lesion segmentation to reduce false positives. (See Supplementary Table 1.) This lesion segmentation technique also incorporates a region growing approach sensitive to local contrasts. Brain lesion masks were then warped into normalized space using bspline registration to MNI152 2mm atlas[50] resulting in a binary mask of MS WML locations for each patient for subsequent analyses. (Figure 1A and Supplementary Figure 1.)
Figure 1: Methodology to test if MS memory dysfunction is associated with disruption of memory circuits.
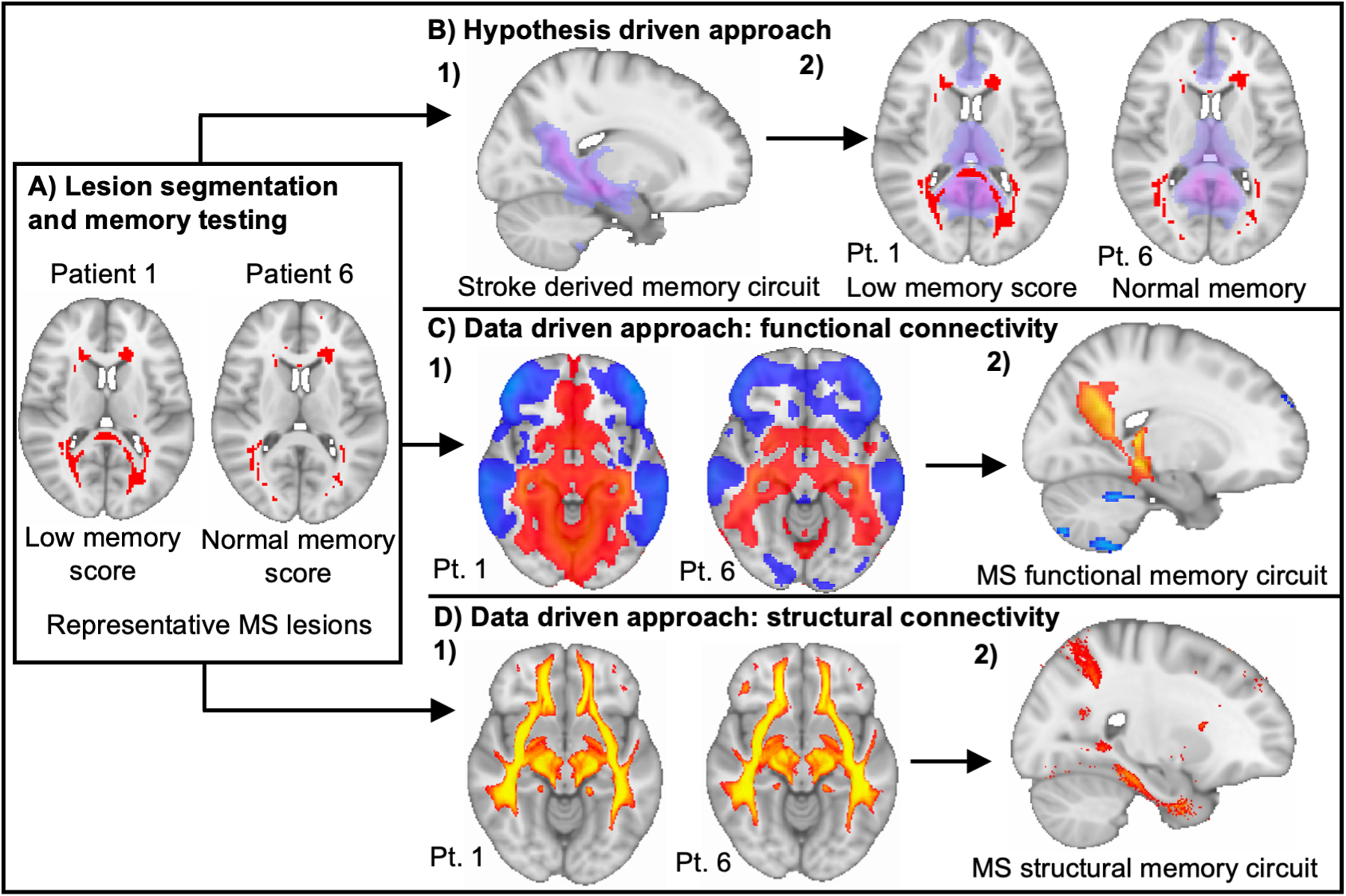
A) Structural imaging, lesion segmentation and memory assessment collected on patients with MS showing two representative lesion maps from a patient with normal and a patient with low memory score. Lesion maps and memory testing are used in subsequent analyses. B) Determine if MS lesion damage to the a priori stroke-derived memory circuit associates with memory dysfunction. B1. Assess lesion overlap with stroke derived memory circuit and then B2. analyze association of MS lesion overlap with stroke derived memory circuit to memory scores C) Derive a unique MS memory circuit based on lesion location employing a functional connectome. C1. Compute lesion connectivity using normative database of resting-state functional connectivity and then C2. perform voxelwise permutation testing to determine functional connections significantly associated with verbal memory scores. D) Derive a unique MS memory circuit based on lesion location employing a structural connectome. D1. Compute lesion connectivity using normative database of structural connectivity and then D2. perform voxelwise permutation testing to determine functional connections significantly associated with verbal memory scores.
Lesion volume & memory network damage score
First, we tested for a correlation between verbal memory score and total WML volume calculated as the number of voxels in each patient’s MS lesion mask. Then, we tested for correlation between verbal memory score and MS lesion damage to an a priori memory circuit derived from stroke lesions[36] taken from our recent paper on stroke-induced memory dysfunction;[36] the memory circuit consists of positive T values that reflect the strength of functional connectivity between each brain voxel to our circuit hub in the subiculum. For each MS patient, we computed a “network damage score” by summing all voxels in our memory circuit intersecting the patient’s MS lesion mask.[36, 51, 52] These values were then used in a Pearson correlation with the individual memory scores, controlling for lesion volume, controlling for Symbol Digit Modality Testing (SDMT), controlling for lesion volume and brain parenchymal fraction, and controlling for lesion volume, age, sex and disease duration. (Figure 1B.) Brain parenchymal fraction is a measure of normalized whole brain volume and a well-established estimate of brain atrophy in MS.[53] We control for brain parenchymal fraction to help validate the association of lesion connectivity with memory dysfunction rather than brain atrophy[54] and we control for SDMT to correct, to some degree, for the role of processing speed,[55] attention and working memory processes[56] in verbal immediate recall trials and strengthen the specificity to verbal memory. We use the term ‘network damage’ to refer to the voxelwise intersection between MS lesion locations and our a priori memory network. This is consistent with the use of this term in prior lesion network mapping studies by our group and others. [36, 51, 52] However, it is important to note that our MS lesion locations are predominantly based on T2 hyperintensities, which may miss other MS lesion types (e.g. T1 lesions) or damage to brain networks than might be seen with more advanced imaging modalities (e.g. DTI).
Because we found independent relationships between memory and both overall lesion volume and lesion network damage, we performed a mediation analysis to test whether one variable mediated the effect of another variable. First, we tested whether network damage mediated the relationship between lesion volume and memory dysfunction employing PROCESS[57] software. To ensure validity, the inverse analysis was also performed, assessing for mediation of the relationship between network damage and memory performance by lesion volume. A 95% confidence interval and 5000 bootstrap samples for confidence intervals not crossing zero were used to determine significance.
We also compared the memory network damage score in patients with memory scores 1 standard deviation above the mean to those with memory scores 1 standard deviation below the mean from our sample by two-sample t-test.[58] To ensure the validity of this analysis we also repeated the analysis and grouped by 1 standard deviation below T score norms (40 or less) versus 1 standard deviation above T score norms (60 or more).
To ensure lesion damage to the memory circuit was specific to memory we also tested for association between damage to the memory circuit and other symptoms associated with increasing lesion burden including depression and fatigue (Neuro-QoL, collected on 287/431 participants) and gait (timed 25-foot walk).
Data-driven functional LNM
LNM with each patient’s MS lesion mask was performed using the same methods previously described for stroke lesions.[30–33, 35, 36] In brief, resting state functional connectivity between each patient’s lesion mask and all other brain voxels was computed using a large functional connectome database from healthy young individuals (n=1000, mean age 21.3, 42.7% male, 2×2×2mm)[59]. The strategy of Fox et al.[60] was employed to process resting state fMRI data and the processed connectome data and code are publicly available.[59] Functional connectivity results were combined across the 1000 subjects using a random effects analysis, producing a single-subject functional connectivity map for each patient’s WML location. Unthresholded lesion network maps were then used for voxel-wise permutation testing in FSL PALM[61] to identify connections associated with verbal memory score. (Figure 1C.) A family-wise error (FWE) threshold p<0.05 was used for significance. Local maxima were identified by thresholding (FWE p<0.005), identifying peak clusters of >20 voxels, with 4 local maxima. We then used spatial correlation to assess the topographic similarity between the MS-derived memory circuit and our stroke-derived memory circuit. We tested the significance of the correlation between the two networks with a permutation testing approach.[37] The spatial correlation between the stroke-derived memory network and the MS-derived memory network was repeatedly computed after randomly re-assigning each patient’s memory score with a different patient’s neuroimaging. We performed 10,000 permutations and set our significance threshold so the true spatial correlation should be more similar to the stroke network than the randomly re-assigned score in more than 95% of permutations which would match p<0.05.
Data-driven structural LNM
We also performed LNM using a structural connectome. Structural connectivity maps were produced using BCBtoolkit “Disconnectome”[62] to calculate disconnection probability of lesions to white matter tracts from normalized diffusion tensor imaging (n=178, mean age 29.5, 38.8% male, 1×1×1mm resolution) from the Human Connectome Project.[63] We utilized diffusion-weighted imaging from controls, identified white matter fibers passing through each lesion location, then transformed these fiber maps into binarized visitation maps in MNI152 space and summed these maps across subjects.[62] This process results in single-subject structural connectivity maps for each patient’s WMLs and reflects the probability of structural disconnection between lesion locations and each brain voxel.[62] Unthresholded structural disconnection maps were then used for voxel-wise permutation based testing in FSL PALM[64] to identify connections associated with verbal memory score (FWE p<0.05 threshold for statistical significance). (Figure 1D.) Local maxima in the resulting map were identified by thresholding the map (FWE p<0.0005), identifying peak clusters of >160 voxels, allowing 4 local maxima. Different parameters were used for the different connectomes due to inherent differences in the data types, including spatial resolution and the method to derive individual maps.
Results
We included a total of 431 patients with MS (mean age 49.2 years, 71.9% female) from the SysteMS study. (See Table 1.)
Table 1.
Patient demographic, disease and cognitive performance data.
| MS patients (n=431) | |
|---|---|
| Age, y, mean (range, SD) | 49.2 (20–80, 10.7) |
| Female, n (%) | 310 (71.9) |
| Disease duration, y, mean (range, SD) | 17.6 (0.5–60, 10.2) |
| Multiple sclerosis type | |
| CIS, n (%) | 13 (3.0) |
| RRMS, n (%) | 349 (81.0) |
| SPMS, n (%) | 54 (12.5) |
| PPMS, n (%) | 15 (3.5) |
| EDSS, mean score (range, SD) | 2.4 (0–8.5, 1.8) |
| Memory performance | |
| CVLT immediate recall trials 1–5 total (range, SD) | 53.9 (18–78, 11.4) |
| CVLT immediate recall trials T score (range, SD) | 55.7 (12–87, 11.9) |
(CVLT = California Verbal Learning Test, EDSS = Expanded Disability Status Scale, CIS = clinically isolated syndrome, RRMS = relapsing-remitting MS, SPMS = secondary progressive MS, PPMS = primary progressive MS.)
MS lesion damage to memory circuit
Consistent with the existing literature, we found an association between total lesion volume and memory scores (r=0.31, p<0.001). Using an a priori memory circuit derived from focal strokes[36], we found that MS lesion damage to this circuit was correlated with memory scores (r=0.34, p<0.001, Figure 2). This relationship was still significant when controlling for lesion volume (r=0.153, p=0.001), controlling for lesion volume and brain parenchymal fraction (r=0.133, p=0.006), controlling for lesion volume and SDMT (r=0.113, p=0.019) and after controlling for lesion volume, age, sex and disease duration (r=0.128, p=0.008). The results were also similar when controlling for lesion volume and employing normalized CVLT T scores (r=0.127, p=0.008), limiting the analysis to subjects imaged on a Skyra scanner within 90 days of cognitive testing (n=419, r=0.158, p=0.001) or just those with RRMS (n=349, r=0.108, p=0.044).
Figure 2: MS lesion locations associated with memory dysfunction overlap an a priori memory circuit.
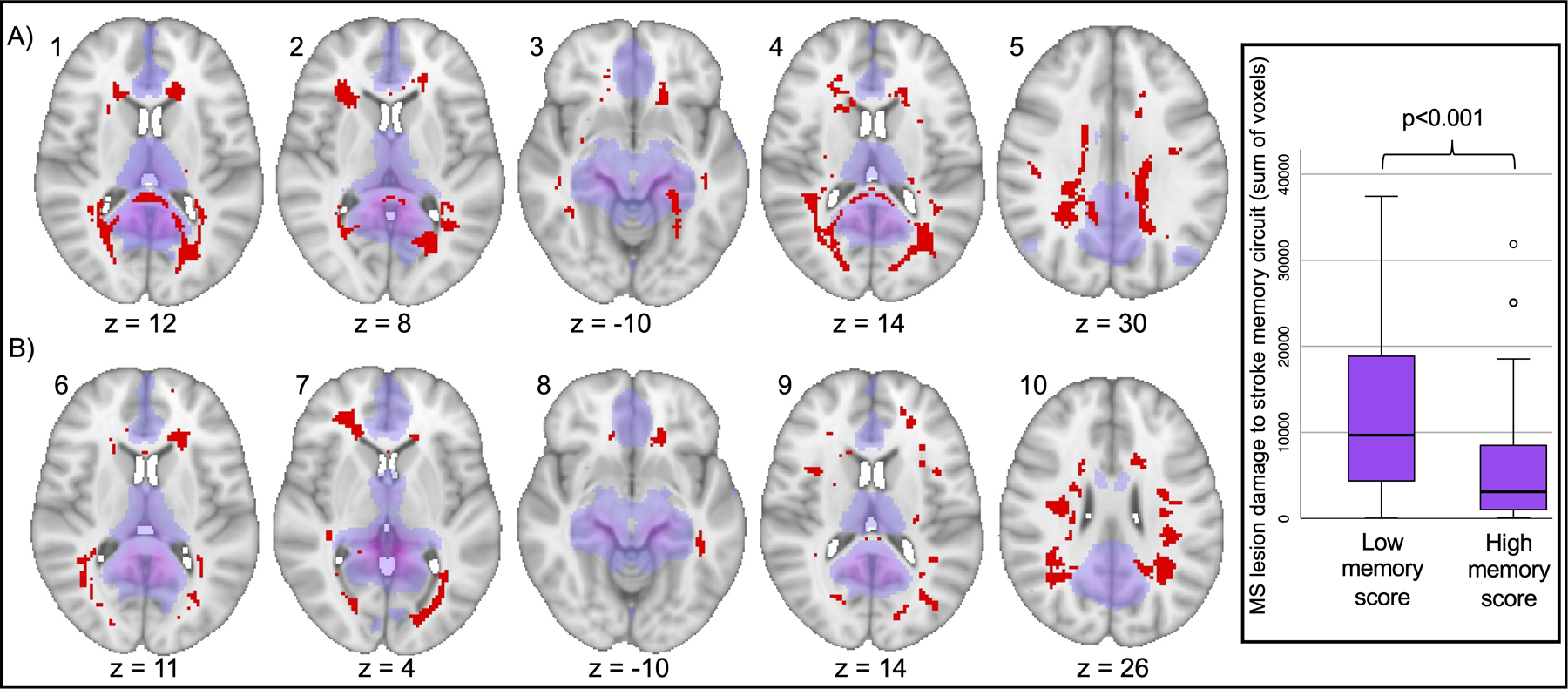
In purple is the a priori stroke derived memory circuit (Ferguson et. al. 2019) and in red are MS lesions grouped by A) lower memory performance and B) normal range memory performance. Intersection between MS lesion locations and our a priori memory circuit was correlated with memory performance (p<0.001). Inset) Box plot of MS lesion damage to the a priori stroke-derived memory circuit comparing patients with lower memory scores (1 standard deviation below mean of the group) versus patients with higher memory scores (1 standard deviation above mean of the group) (t=4.7, p<0.001).
Mediation analysis found that damage to our a priori memory circuit fully mediated (bootstrap CI 0.0011 to 0.0039), the relationship between lesion volume and memory scores (p=0.85, bootstrap CI −0.0018 to 0.0015). Conversely, when the mediation analysis was flipped, we found no mediation of the relationship between circuit damage and memory scores (p=0.0014, bootstrap CI 0.0002 to 0.0007) by lesion volume (bootstrap CI −0.0003 to 0.0002).
There was also a significant difference in MS lesion damage to the a priori stroke-derived memory circuit by comparing groups of patients with low (n=64) versus high (n=70) memory performance (t=4.7, p=0.000007) (Figure 2) based on standard deviation cutoffs from within our large MS cohort. Results were similar when grouped into low (n=46) versus high (n=173) memory performance (t=4.58, p=0.000028) using CVLT T score population based norms for memory dysfunction.
Lesion damage to the memory circuit was not associated with other symptoms that often worsen with increasing lesion burden such as worsening gait (r=0.06, p=0.26), depression (r=0.06, p=0.32) or fatigue (r=−0.01, p=0.93).
Data-driven functional LNM
In our data driven analysis, we found that functional connectivity between MS lesion locations and a distributed brain circuit was significantly associated with memory dysfunction (FWE p<0.05) (Figure 3A). This circuit included peaks in the bilateral hippocampi, fornix, precuneus, cingulate and retrosplenial cortex (Supplementary Table 2).
Figure 3:
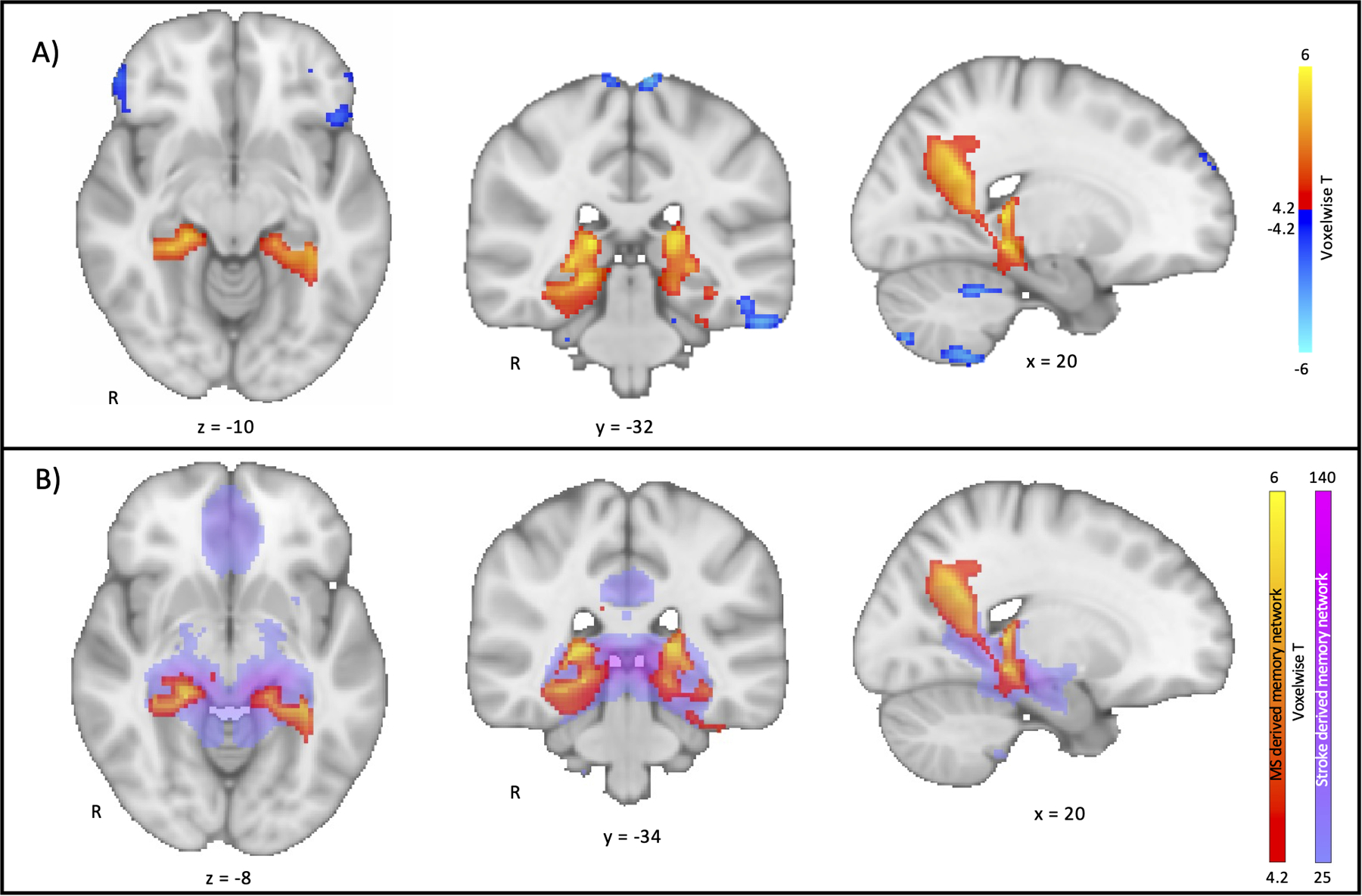
Lesion network mapping of memory dysfunction in multiple sclerosis using a functional connectome. A) Functional connections with MS lesion locations significantly associated with verbal memory. Voxels displayed are p<0.05 on voxelwise family-wise error correction. B) Comparison of the topography of the MS lesion derived functional memory circuit from 4A (warm colors) to the stroke derived memory circuit from Ferguson et. al. 2019 (purple). The high threshold for the stroke-based memory circuit in 4B was chosen to facilitate comparison to the MS-based circuit topography.
The topography of this data-driven MS memory circuit was similar after controlling for age, sex, disease duration and lesion volume (Supplementary Figure 2A). Results were also similar after controlling for lesion volume, brain parenchyma fraction, MS subtype, SDMT score and when the analysis was limited to patients with relapsing-remitting MS (n=349) or to patients imaged on a Skyra scanner within 90 days of cognitive testing (n=419) (Supplementary Figure 2B-G)
The topography of the data-driven MS memory circuit matched the topography of our previously published memory circuit derived from focal strokes (Figure 3B, spatial r=0.52, p<0.05 after permutation testing). The results were similar when including only subjects imaged on a Skyra scanner within 90 days of cognitive testing (n=419, spatial r=0.51, p=0.045) or limiting the analysis to patients with a diagnosis of RRMS (n=349, r=0.58, p=0.021).
Data-driven structural LNM
Intersection between MS lesion locations and a distributed set of white matter connections was also significantly associated with memory dysfunction, with peaks in the parahippocampus, hippocampus and cingulum. (Figure 4A and Supplementary Table 2.)
Figure 4:
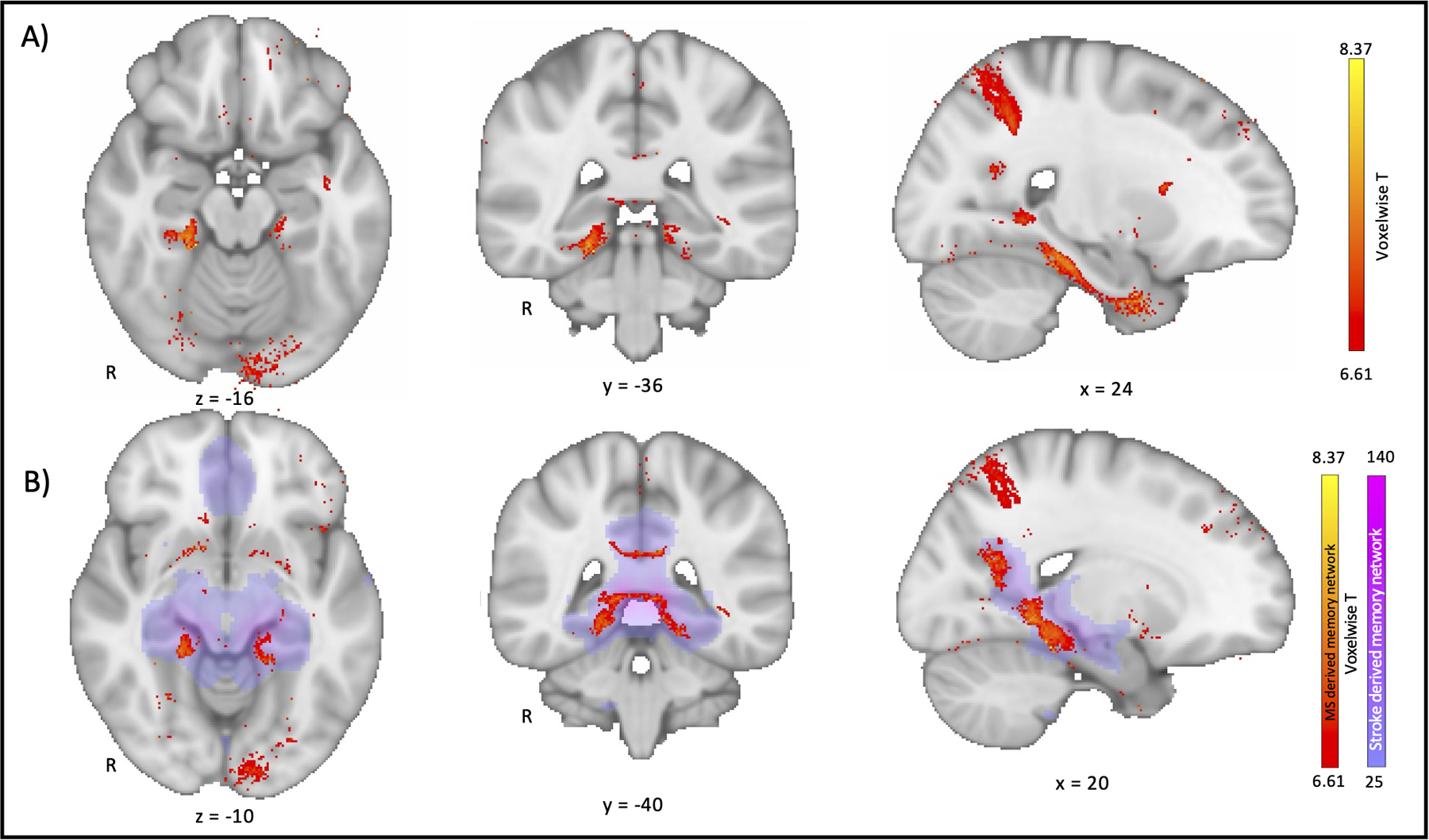
Lesion network mapping of memory dysfunction in multiple sclerosis using a structural connectome. A) Structural connections with MS lesion locations significantly associated with verbal memory. Voxels are displayed after voxelwise family-wise error p<0.0005 B) Comparison of the topography of the MS lesion derived structural memory circuit from 4A (warm colors) to the stroke derived memory circuit from Ferguson et. al. 2019 (purple).
The topography of this circuit was similar after controlling for age, sex, disease duration and lesion volume, brain parenchymal fraction, MS type, SDMT score or when limiting the analysis to patients with relapsing-remitting MS (n=349) or to patients imaged on a Skyra scanner within 90 days of cognitive testing (n=419) (Supplementary Figure 3.) We cannot directly compare circuit topography using spatial correlation, as the two results were derived from different connectomes and datatypes; however, the topography of our data-driven structural MS memory circuit was qualitatively similar to our a priori memory circuit derived from stroke lesions using the functional connectome with shared anatomical peaks. (Figure 4B and Supplementary Table 2.)
Discussion
In this study we show that memory dysfunction in multiple sclerosis is associated with lesions to a specific human brain circuit. Lesion damage to this brain circuit fully mediated the often-reported relationship between total lesion burden and memory dysfunction. Data-driven circuits for MS memory dysfunction could be derived using either functional or structural connectivity and align with the neuroanatomy of memory dysfunction due to stroke.
Increasing WML burden has been consistently associated with worsening memory dysfunction in MS[10–14] but lesion burden is also associated with other common MS symptoms including fatigue,[16] depression[17] and gait dysfunction.[18, 19] Attempts to understand MS memory dysfunction by lesion location have been heterogenous, with different studies implicating different brain regions.[11, 13, 20–22, 25, 27] By applying a circuit-based localization approach our results help reconcile these heterogenous findings by showing that MS memory dysfunction is associated with damage to a distributed memory circuit, not just individual brain regions.[65]
Our work also lends potential insight into why increasing MS lesion burden is associated with memory dysfunction, suggesting that this may occur because more lesions are more likely to hit the memory circuit. Once memory circuit damage was accounted for in the analysis, total lesion burden was no longer an independent determinant of memory dysfunction. This circuit-based localization approach could be employed to other MS symptoms commonly associated with lesion burden such as fatigue or depression to clarify symptom localization.
Connecting stroke and MS
An important finding is that MS and ischemic stroke lesions causing a common symptom (memory dysfunction) map to a common brain circuit. We showed this convergence in multiple ways, including MS lesion damage to our stroke-derived memory circuit and spatial correlation in the topography of the two circuits. Similarities between the MS and stroke-based memory circuits includes peaks in the bilateral hippocampi,[66] parahippocampi, fornix, posterior cingulate/retrosplenial cortices and precuneus.[67] These regions form the key nodes of Papez circuit and the posterior default mode network which have been repeatedly implicated in episodic memory.[67] This convergence between MS lesions and ischemic stroke lesions may seem surprising given the many differences in pathophysiology, lesion etiology, and lesion location. However, this result is consistent with a growing body of evidence suggesting that a specific brain circuit is associated with the same symptom across different pathologies.[30, 33]
It is worth noting that the MS and stroke-based memory circuits were not identical. The peak of the stroke-based memory circuit was in the gray matter of the subiculum while the peak of the MS-based memory circuit was at the junction of the fornix and the white matter of the hippocampus. MS memory dysfunction related to WMLs may show greater disruption of white matter connections at the fornix-hippocampal junction[68]. In addition, the MS derived memory network was more limited to the posterior hippocampus with relatively little involvement of the more anterior hippocampus. There are several possible reasons for this difference including our reliance on verbal immediate recall trials which may bias towards memory registration and retrieval of very recent memories,[69] the reliance on repeated lists[70] or may be due to the distinct memory dysfunction in MS where acquisition is more impacted.[48]
Functional and structural connectomes
A strength of the present study is the inclusion of both a functional and structural connectome to investigate MS memory dysfunction. To date, the majority of LNM studies have utilized either a functional or structural connectome, with few studies including both and ongoing debate as to which might be better and in which situations.[71] Our positive results using both functional and structural connectomes, is consistent with increasing evidence that white matter has BOLD signal fluctuations which can be used to map relevant neuroanatomy.[42, 72] Future work is needed to determine how best to combine the complementary information obtained from LNM using a functional versus structural connectome.
Limitations
A key limitation of our work is that the analysis was limited to analyzing the connectivity of T2-FLAIR hyperintense white matter lesions which was motivated by our interest in validating the technique in standard of care clinical scans. While our results add important new information regarding the role of the connectivity of white matter lesions in MS memory dysfunction, it is surely not the whole picture. We didn’t evaluate T1 hypointense lesions, which may be more destructive and have different relative contributions to memory dysfunction[24] or gray matter lesions which are challenging to define on standard MRI imaging. Recent work has also highlighted the association between cerebral gray matter atrophy, especially of the thalamus and hippocampus, and memory dysfunction[3], but we focused on WMLs to particularly address whether specific lesion locations disrupt a memory circuit. The exact relationship between white matter injury and gray matter atrophy in MS remains uncertain[20] with emerging evidence that in early disease stages, white matter damage is a contributor to gray matter atrophy [73] highlighting the need for better tools to predict symptom specific deficits based on WML location. Different types of white matter injury, gray matter lesions and atrophy, as well as inflammation in general, likely all contribute in some way to memory dysfunction in MS.[1] Future work is needed to assess the relative contribution of the connectivity of gray matter and white matter lesions and atrophy patterns.
Another limitation is our cognitive testing which was limited to verbal memory with reliance on the CVLT immediate recall trials. While initial learning/acquisition trials[48] are considered a valid metric for assessing memory in MS[45–47] this is by no means a complete method for assessing episodic memory. In MS, memory encoding is significantly impacted[48] and immediate recall trials have shown sensitivity for memory dysfunction.[47] For this reason we relied on immediate recall trials as a marker of memory. Brief MS batteries recommend employing the immediate recall trials of the CVLT as a marker of verbal memory[45] partly due to the prominence of these encoding difficulties. Word learning on immediate recall assesses verbal memory function as demonstrated by the fact that the first five immediate recall trials on CVLT has a high degree of interdependence with the other parts of the CVLT.[45, 46] Many clinical neuropsychologists and cognitive studies employ immediate recall/learning over successive trials as a marker of episodic memory[74, 75] while other studies have questioned this.[76] We have controlled for SDMT scores to help to increase the specificity of our findings for verbal memory (rather than other elements of learning such as processing speed, attention and working memory) but our reliance on immediate recall is indeed a limitation of our results. Future work is planned that will directly test both immediate and delayed verbal and visual memory paradigms applying lesion network mapping.
We also used of a normalized connectome from healthy controls rather than one constructed from people with MS. However, previous LNM studies have shown little benefit from using a disease specific versus normative control connectome[31, 35, 38] and prior work using resting-state fMRI in MS from the patients themselves to explore memory has led to conflicting results.[77, 78] Of note, most patients in our study did not have frank memory impairment by standardized scores which in some ways strengthens our results.[9] By demonstrating that memory function in MS associates with the connectivity of WMLs even in people with normal range functioning on cognitive tests, we add important information to the role of WMLs across the range of cognitive function.
In summary, our results demonstrate that memory dysfunction in multiple sclerosis associates with the functional and structural connectivity of WMLs and anatomically aligns with the well-defined neuroanatomy of episodic memory.
Ethical Approval of Studies and Informed Consent
The study was approved by Mass General Brigham/Partners Institutional Review Board Protocols 2015P001248, 2020P002987 and 2020P000737 and all participants provided written informed consent.
Supplementary Material
Acknowledgements
The authors thank the patients who participated in the SysteMS study and the research staff at the Brigham MS Center for assistance, especially Mark Anderson. The authors thank Dr. Margaret O’Connor and Dr. Rebecca Amariglio for their advice and guidance. The authors thank the members of the Center for Brain Circuit Therapeutics for assistance especially Christopher Lin. Data were provided, in part, by the Human Connectome Project, WU-Minn Consortium (Principal Investigators: David Van Essen and Kamil Ugurbil; 1U54MH091657) funded by the 16 NIH Institutes and Centers that support the NIH Blueprint for Neuroscience Research; and by the McDonnell Center for Systems Neuroscience at Washington University.
Funding
AC was funded by NIH/NIMH K23MH120510, the Child Neurology Foundation, and the Simons Foundation Autism Research Initiative. M.D.F. was supported by the Nancy Lurie Marks Foundation, the Mather’s Foundation, the Ellison / Baszucki Foundation, the Kaye Family Research Endowment and National Institutes of Health grants R21 MH126271, R56 AG069086, R01 MH113929, R01 MH115949, and R01 AG060987. The SysteMS cohort of the CLIMB study was supported in part by Verily Life Sciences. The CLIMB study is supported in part by the Watercove Foundation.
Potential Conflicts of Interest
Rohit Bakshi has received consulting fees from Bristol-Myers Squibb and EMD Serono and research support from Bristol-Myers Squibb, EMD Serono, and Novartis. The other authors report no competing interests.
Data Sharing Statement
The functional connectivity data equivalent to that used in this study is available online through the Harvard Dataverse at: https://doi.org/10.7910/DVN/ILXIKS and the pipeline used to prepare the functional connectivity data is available at: https://github.com/bchcohenlab/BIDS_to_CBIG_fMRI_Preproc2016. The code to prepare structural connectivity maps is available at: https://storage.googleapis.com/bcblabweb/index.html and the structural connectivity data is available at: https://www.humanconnectome.org/study/hcp-young-adult/document/1200-subjects-data-release. Statistical analyses were performed in MatLab (version 2019b) or SPSS (version 27.0.1.0). MS lesion data is available for review upon reasonable request.
References
- 1.Benedict RHB, Amato MP, DeLuca J, Geurts JJG (2020) Cognitive impairment in multiple sclerosis: clinical management, MRI, and therapeutic avenues. Lancet Neurol 19:860–871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Benedict RH, Cookfair D, Gavett R, Gunther M, Munschauer F, Garg N, Weinstock-Guttman B (2006) Validity of the minimal assessment of cognitive function in multiple sclerosis (MACFIMS). J Int Neuropsychol Soc 12:549–558 [DOI] [PubMed] [Google Scholar]
- 3.De Meo E, Portaccio E, Giorgio A, Ruano L, Goretti B, Niccolai C, Patti F, Chisari CG, Gallo P, Grossi P, Ghezzi A, Roscio M, Mattioli F, Stampatori C, Simone M, Viterbo RG, Bonacchi R, Rocca MA, De Stefano N, Filippi M, Amato MP (2021) Identifying the Distinct Cognitive Phenotypes in Multiple Sclerosis. JAMA Neurol 78:414–425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McGinley MP, Goldschmidt CH, Rae-Grant AD (2021) Diagnosis and Treatment of Multiple Sclerosis: A Review. JAMA 325:765–779 [DOI] [PubMed] [Google Scholar]
- 5.Thompson AJ, Banwell BL, Barkhof F, Carroll WM, Coetzee T, Comi G, Correale J, Fazekas F, Filippi M, Freedman MS, Fujihara K, Galetta SL, Hartung HP, Kappos L, Lublin FD, Marrie RA, Miller AE, Miller DH, Montalban X, Mowry EM, Sorensen PS, Tintore M, Traboulsee AL, Trojano M, Uitdehaag BMJ, Vukusic S, Waubant E, Weinshenker BG, Reingold SC, Cohen JA (2018) Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol 17:162–173 [DOI] [PubMed] [Google Scholar]
- 6.Sormani MP, Bruzzi P (2013) MRI lesions as a surrogate for relapses in multiple sclerosis: a meta-analysis of randomised trials. Lancet Neurol 12:669–676 [DOI] [PubMed] [Google Scholar]
- 7.Swirsky-Sacchetti T, Mitchell DR, Seward J, Gonzales C, Lublin F, Knobler R, Field HL (1992) Neuropsychological and structural brain lesions in multiple sclerosis: a regional analysis. Neurology 42:1291–1295 [DOI] [PubMed] [Google Scholar]
- 8.Rao SM, Leo GJ, Haughton VM, St Aubin-Faubert P, Bernardin L (1989) Correlation of magnetic resonance imaging with neuropsychological testing in multiple sclerosis. Neurology 39:161–166 [DOI] [PubMed] [Google Scholar]
- 9.Uher T, Krasensky J, Sobisek L, Blahova Dusankova J, Seidl Z, Kubala Havrdova E, Sormani MP, Horakova D, Kalincik T, Vaneckova M (2018) Cognitive clinico-radiological paradox in early stages of multiple sclerosis. Ann Clin Transl Neurol 5:81–91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mollison D, Sellar R, Bastin M, Mollison D, Chandran S, Wardlaw J, Connick P (2017) The clinico-radiological paradox of cognitive function and MRI burden of white matter lesions in people with multiple sclerosis: A systematic review and meta-analysis. PLoS One 12:e0177727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rossi F, Giorgio A, Battaglini M, Stromillo ML, Portaccio E, Goretti B, Federico A, Hakiki B, Amato MP, De Stefano N (2012) Relevance of brain lesion location to cognition in relapsing multiple sclerosis. PLoS One 7:e44826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Izquierdo G, Campoy F Jr, Mir J, Gonzalez M, Martinez-Parra C (1991) Memory and learning disturbances in multiple sclerosis. MRI lesions and neuropsychological correlation. Eur J Radiol 13:220–224 [DOI] [PubMed] [Google Scholar]
- 13.Roosendaal SD, Moraal B, Pouwels PJ, Vrenken H, Castelijns JA, Barkhof F, Geurts JJ (2009) Accumulation of cortical lesions in MS: relation with cognitive impairment. Mult Scler 15:708–714 [DOI] [PubMed] [Google Scholar]
- 14.Sacco R, Bisecco A, Corbo D, Della Corte M, d’Ambrosio A, Docimo R, Gallo A, Esposito F, Esposito S, Cirillo M, Lavorgna L, Tedeschi G, Bonavita S (2015) Cognitive impairment and memory disorders in relapsing-remitting multiple sclerosis: the role of white matter, gray matter and hippocampus. J Neurol 262:1691–1697 [DOI] [PubMed] [Google Scholar]
- 15.Rocca MA, Amato MP, De Stefano N, Enzinger C, Geurts JJ, Penner IK, Rovira A, Sumowski JF, Valsasina P, Filippi M, Group MS (2015) Clinical and imaging assessment of cognitive dysfunction in multiple sclerosis. Lancet Neurol 14:302–317 [DOI] [PubMed] [Google Scholar]
- 16.Tedeschi G, Dinacci D, Lavorgna L, Prinster A, Savettieri G, Quattrone A, Livrea P, Messina C, Reggio A, Servillo G, Bresciamorra V, Orefice G, Paciello M, Brunetti A, Paolillo A, Coniglio G, Bonavita S, Di Costanzo A, Bellacosa A, Valentino P, Quarantelli M, Patti F, Salemi G, Cammarata E, Simone I, Salvatore M, Bonavita V, Alfano B (2007) Correlation between fatigue and brain atrophy and lesion load in multiple sclerosis patients independent of disability. J Neurol Sci 263:15–19 [DOI] [PubMed] [Google Scholar]
- 17.Feinstein A, Magalhaes S, Richard JF, Audet B, Moore C (2014) The link between multiple sclerosis and depression. Nat Rev Neurol 10:507–517 [DOI] [PubMed] [Google Scholar]
- 18.Brandstadter R, Ayeni O, Krieger SC, Harel NY, Escalon MX, Katz Sand I, Leavitt VM, Fabian MT, Buyukturkoglu K, Klineova S, Riley CS, Lublin FD, Miller AE, Sumowski JF (2020) Detection of subtle gait disturbance and future fall risk in early multiple sclerosis. Neurology 94:e1395–e1406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barkhof F (2002) The clinico-radiological paradox in multiple sclerosis revisited. Curr Opin Neurol 15:239–245 [DOI] [PubMed] [Google Scholar]
- 20.Engl C, Tiemann L, Grahl S, Bussas M, Schmidt P, Pongratz V, Berthele A, Beer A, Gaser C, Kirschke JS, Zimmer C, Hemmer B, Muhlau M (2020) Cognitive impairment in early MS: contribution of white matter lesions, deep grey matter atrophy, and cortical atrophy. J Neurol 267:2307–2318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rovaris M, Filippi M, Falautano M, Minicucci L, Rocca MA, Martinelli V, Comi G (1998) Relation between MR abnormalities and patterns of cognitive impairment in multiple sclerosis. Neurology 50:1601–1608 [DOI] [PubMed] [Google Scholar]
- 22.Deloire MS, Salort E, Bonnet M, Arimone Y, Boudineau M, Amieva H, Barroso B, Ouallet JC, Pachai C, Galliaud E, Petry KG, Dousset V, Fabrigoule C, Brochet B (2005) Cognitive impairment as marker of diffuse brain abnormalities in early relapsing remitting multiple sclerosis. J Neurol Neurosurg Psychiatry 76:519–526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mesaros S, Rocca MA, Riccitelli G, Pagani E, Rovaris M, Caputo D, Ghezzi A, Capra R, Bertolotto A, Comi G, Filippi M (2009) Corpus callosum damage and cognitive dysfunction in benign MS. Hum Brain Mapp 30:2656–2666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rocca MA, Amato MP, De Stefano N, Enzinger C, Geurts JJ, Penner I-K, Rovira A, Sumowski JF, Valsasina P, Filippi M (2015) Clinical and imaging assessment of cognitive dysfunction in multiple sclerosis. The Lancet Neurology 14:302–317 [DOI] [PubMed] [Google Scholar]
- 25.Sperling RA, Guttmann CR, Hohol MJ, Warfield SK, Jakab M, Parente M, Diamond EL, Daffner KR, Olek MJ, Orav EJ, Kikinis R, Jolesz FA, Weiner HL (2001) Regional magnetic resonance imaging lesion burden and cognitive function in multiple sclerosis: a longitudinal study. Arch Neurol 58:115–121 [DOI] [PubMed] [Google Scholar]
- 26.Brainin M, Goldenberg G, Ahlers C, Reisner T, Neuhold A, Deecke L (1988) Structural brain correlates of anterograde memory deficits in multiple sclerosis. J Neurol 235:362–365 [DOI] [PubMed] [Google Scholar]
- 27.Altermatt A, Gaetano L, Magon S, Haring DA, Tomic D, Wuerfel J, Radue EW, Kappos L, Sprenger T (2018) Clinical Correlations of Brain Lesion Location in Multiple Sclerosis: Voxel-Based Analysis of a Large Clinical Trial Dataset. Brain Topogr 31:886–894 [DOI] [PubMed] [Google Scholar]
- 28.Weaver NA, Kuijf HJ, Aben HP, Abrigo J, Bae HJ, Barbay M, Best JG, Bordet R, Chappell FM, Chen C, Dondaine T, van der Giessen RS, Godefroy O, Gyanwali B, Hamilton OKL, Hilal S, Huenges Wajer IMC, Kang Y, Kappelle LJ, Kim BJ, Kohler S, de Kort PLM, Koudstaal PJ, Kuchcinski G, Lam BYK, Lee BC, Lee KJ, Lim JS, Lopes R, Makin SDJ, Mendyk AM, Mok VCT, Oh MS, van Oostenbrugge RJ, Roussel M, Shi L, Staals J, Del CV-HM, Venketasubramanian N, Verhey FRJ, Wardlaw JM, Werring DJ, Xin X, Yu KH, van Zandvoort MJE, Zhao L, Biesbroek JM, Biessels GJ (2021) Strategic infarct locations for post-stroke cognitive impairment: a pooled analysis of individual patient data from 12 acute ischaemic stroke cohorts. Lancet Neurol 20:448–459 [DOI] [PubMed] [Google Scholar]
- 29.Biesbroek JM, van Zandvoort MJ, Kappelle LJ, Schoo L, Kuijf HJ, Velthuis BK, Biessels GJ, Postma A, Utrecht VCIsg (2015) Distinct anatomical correlates of discriminability and criterion setting in verbal recognition memory revealed by lesion-symptom mapping. Hum Brain Mapp 36:1292–1303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fox MD (2018) Mapping Symptoms to Brain Networks with the Human Connectome. N Engl J Med 379:2237–2245 [DOI] [PubMed] [Google Scholar]
- 31.Boes AD, Prasad S, Liu H, Liu Q, Pascual-Leone A, Caviness VS Jr, Fox MD (2015) Network localization of neurological symptoms from focal brain lesions. Brain 138:3061–3075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Joutsa J, Corp DT, Fox MD (2022) Lesion network mapping for symptom localization: recent developments and future directions. Curr Opin Neurol [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kletenik I, Ferguson MA, Bateman JR, Cohen AL, Lin C, Tetreault A, Pelak VS, Anderson CA, Prasad S, Darby RR, Fox MD (2022) Network Localization of Unconscious Visual Perception in Blindsight. Ann Neurol 91:217–224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kletenik I, Gaudet K, Prasad S, Cohen AL, Fox MD (2023) Network Localization of Awareness in Visual and Motor Anosognosia. Ann Neurol [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cohen AL, Mulder BPF, Prohl AK, Soussand L, Davis P, Kroeck MR, McManus P, Gholipour A, Scherrer B, Bebin EM, Wu JY, Northrup H, Krueger DA, Sahin M, Warfield SK, Fox MD, Peters JM, Tuberous Sclerosis Complex Autism Center of Excellence Network Study G (2021) Tuber Locations Associated with Infantile Spasms Map to a Common Brain Network. Ann Neurol 89:726–739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ferguson MA, Lim C, Cooke D, Darby RR, Wu O, Rost NS, Corbetta M, Grafman J, Fox MD (2019) A human memory circuit derived from brain lesions causing amnesia. Nat Commun 10:3497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Siddiqi SH, Schaper F, Horn A, Hsu J, Padmanabhan JL, Brodtmann A, Cash RFH, Corbetta M, Choi KS, Dougherty DD, Egorova N, Fitzgerald PB, George MS, Gozzi SA, Irmen F, Kuhn AA, Johnson KA, Naidech AM, Pascual-Leone A, Phan TG, Rouhl RPW, Taylor SF, Voss JL, Zalesky A, Grafman JH, Mayberg HS, Fox MD (2021) Brain stimulation and brain lesions converge on common causal circuits in neuropsychiatric disease. Nat Hum Behav 5:1707–1716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Joutsa J, Moussawi K, Siddiqi SH, Abdolahi A, Drew W, Cohen AL, Ross TJ, Deshpande HU, Wang HZ, Bruss J, Stein EA, Volkow ND, Grafman JH, van Wijngaarden E, Boes AD, Fox MD (2022) Brain lesions disrupting addiction map to a common human brain circuit. Nat Med 28:1249–1255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Eichenbaum H (2000) A cortical-hippocampal system for declarative memory. Nat Rev Neurosci 1:41–50 [DOI] [PubMed] [Google Scholar]
- 40.Wattjes MP, Rovira A, Miller D, Yousry TA, Sormani MP, de Stefano MP, Tintore M, Auger C, Tur C, Filippi M, Rocca MA, Fazekas F, Kappos L, Polman C, Frederik B, Xavier M, group Ms (2015) Evidence-based guidelines: MAGNIMS consensus guidelines on the use of MRI in multiple sclerosis--establishing disease prognosis and monitoring patients. Nat Rev Neurol 11:597–606 [DOI] [PubMed] [Google Scholar]
- 41.Tedone N, Preziosa P, Meani A, Pagani E, Vizzino C, Filippi M, Rocca MA (2023) Regional white matter and gray matter damage and cognitive performances in multiple sclerosis according to sex. Mol Psychiatry [DOI] [PubMed] [Google Scholar]
- 42.Grajauskas LA, Frizzell T, Song X, D’Arcy RCN (2019) White Matter fMRI Activation Cannot Be Treated as a Nuisance Regressor: Overcoming a Historical Blind Spot. Front Neurosci 13:1024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Siddiqi SH, Kletenik I, Anderson MC, Cavallari M, Chitnis T, Glanz BI, Khalil S, Palotai M, Bakshi R, Guttmann CRG, Fox MD (2023) Lesion network localization of depression in multiple sclerosis. Nature Mental Health 1:36–44 [Google Scholar]
- 44.Healy BC, Zurawski J, Gonzalez CT, Chitnis T, Weiner HL, Glanz BI (2019) Assessment of computer adaptive testing version of the Neuro-QOL for people with multiple sclerosis. Mult Scler 25:1791–1799 [DOI] [PubMed] [Google Scholar]
- 45.Langdon DW, Amato MP, Boringa J, Brochet B, Foley F, Fredrikson S, Hämäläinen P, Hartung HP, Krupp L, Penner IK, Reder AT, Benedict RH (2012) Recommendations for a Brief International Cognitive Assessment for Multiple Sclerosis (BICAMS). Mult Scler 18:891–898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Stegen S, Stepanov I, Cookfair D, Schwartz E, Hojnacki D, Weinstock-Guttman B, Benedict RH (2010) Validity of the California Verbal Learning Test-II in multiple sclerosis. Clin Neuropsychol 24:189–202 [DOI] [PubMed] [Google Scholar]
- 47.Fink F, Eling P, Rischkau E, Beyer N, Tomandl B, Klein J, Hildebrandt H (2010) The association between California Verbal Learning Test performance and fibre impairment in multiple sclerosis: evidence from diffusion tensor imaging. Mult Scler 16:332–341 [DOI] [PubMed] [Google Scholar]
- 48.Lafosse JM, Mitchell SM, Corboy JR, Filley CM (2013) The nature of verbal memory impairment in multiple sclerosis: a list-learning and meta-analytic study. J Int Neuropsychol Soc 19:995–1008 [DOI] [PubMed] [Google Scholar]
- 49.Meier DS, Guttmann CRG, Tummala S, Moscufo N, Cavallari M, Tauhid S, Bakshi R, Weiner HL (2018) Dual-Sensitivity Multiple Sclerosis Lesion and CSF Segmentation for Multichannel 3T Brain MRI. J Neuroimaging 28:36–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Klein S, Staring M, Murphy K, Viergever MA, Pluim JP (2010) elastix: a toolbox for intensity-based medical image registration. IEEE Trans Med Imaging 29:196–205 [DOI] [PubMed] [Google Scholar]
- 51.Padmanabhan JL, Cooke D, Joutsa J, Siddiqi SH, Ferguson M, Darby RR, Soussand L, Horn A, Kim NY, Voss JL, Naidech AM, Brodtmann A, Egorova N, Gozzi S, Phan TG, Corbetta M, Grafman J, Fox MD (2019) A Human Depression Circuit Derived From Focal Brain Lesions. Biol Psychiatry 86:749–758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhao SZ, Zhao YX, Liao XH, Huo R, Li H, Jiao YM, Weng JC, Wang J, Liu B, Cao Y (2023) Unruptured brain arteriovenous malformations causing seizures localize to one common brain network. J Neurosci Res 101:245–255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sharma J, Sanfilipo MP, Benedict RH, Weinstock-Guttman B, Munschauer FE 3rd, Bakshi R (2004) Whole-brain atrophy in multiple sclerosis measured by automated versus semiautomated MR imaging segmentation. AJNR Am J Neuroradiol 25:985–996 [PMC free article] [PubMed] [Google Scholar]
- 54.Sotiropoulos MG, Lokhande H, Healy BC, Polgar-Turcsanyi M, Glanz BI, Bakshi R, Weiner HL, Chitnis T (2021) Relapse recovery in multiple sclerosis: Effect of treatment and contribution to long-term disability. Mult Scler J Exp Transl Clin 7:20552173211015503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Benedict RH, DeLuca J, Phillips G, LaRocca N, Hudson LD, Rudick R, Multiple Sclerosis Outcome Assessments C (2017) Validity of the Symbol Digit Modalities Test as a cognition performance outcome measure for multiple sclerosis. Mult Scler 23:721–733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lopez-Gongora M, Querol L, Escartin A (2015) A one-year follow-up study of the Symbol Digit Modalities Test (SDMT) and the Paced Auditory Serial Addition Test (PASAT) in relapsing-remitting multiple sclerosis: an appraisal of comparative longitudinal sensitivity. BMC Neurol 15:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hayes AF (2022) Introduction to Mediation, Moderation, and Conditional Process Analysis, Third Edition: A Regression-Based Approach. Guilford Publications, New York [Google Scholar]
- 58.Busse A, Hensel A, Guhne U, Angermeyer MC, Riedel-Heller SG (2006) Mild cognitive impairment: long-term course of four clinical subtypes. Neurology 67:2176–2185 [DOI] [PubMed] [Google Scholar]
- 59.Yeo BT, Krienen FM, Sepulcre J, Sabuncu MR, Lashkari D, Hollinshead M, Roffman JL, Smoller JW, Zollei L, Polimeni JR, Fischl B, Liu H, Buckner RL (2011) The organization of the human cerebral cortex estimated by intrinsic functional connectivity. J Neurophysiol 106:1125–1165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Fox MD, Snyder AZ, Vincent JL, Corbetta M, Van Essen DC, Raichle ME (2005) The human brain is intrinsically organized into dynamic, anticorrelated functional networks. Proc Natl Acad Sci U S A 102:9673–9678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Winkler AM, Ridgway GR, Webster MA, Smith SM, Nichols TE (2014) Permutation inference for the general linear model. Neuroimage 92:381–397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Foulon C, Cerliani L, Kinkingnehun S, Levy R, Rosso C, Urbanski M, Volle E, Thiebaut de Schotten M (2018) Advanced lesion symptom mapping analyses and implementation as BCBtoolkit. Gigascience 7:1–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Vu AT, Auerbach E, Lenglet C, Moeller S, Sotiropoulos SN, Jbabdi S, Andersson J, Yacoub E, Ugurbil K (2015) High resolution whole brain diffusion imaging at 7T for the Human Connectome Project. Neuroimage 122:318–331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Jenkinson M, Beckmann CF, Behrens TE, Woolrich MW, Smith SM (2012) Fsl. Neuroimage 62:782–790 [DOI] [PubMed] [Google Scholar]
- 65.Chard D, Trip SA (2017) Resolving the clinico-radiological paradox in multiple sclerosis. F1000Res 6:1828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Scoville WB, Milner B (1957) Loss of recent memory after bilateral hippocampal lesions. J Neurol Neurosurg Psychiatry 20:11–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sestieri C, Corbetta M, Romani GL, Shulman GL (2011) Episodic memory retrieval, parietal cortex, and the default mode network: functional and topographic analyses. J Neurosci 31:4407–4420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Valdes Cabrera D, Smyth P, Blevins G, Emery D, Beaulieu C (2022) Diffusion imaging of fornix and interconnected limbic deep grey matter is linked to cognitive impairment in multiple sclerosis. Eur J Neurosci 55:277–294 [DOI] [PubMed] [Google Scholar]
- 69.Poppenk J, McIntosh AR, Craik FI, Moscovitch M (2010) Past experience modulates the neural mechanisms of episodic memory formation. J Neurosci 30:4707–4716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Poppenk J, Kohler S, Moscovitch M (2010) Revisiting the novelty effect: when familiarity, not novelty, enhances memory. J Exp Psychol Learn Mem Cogn 36:1321–1330 [DOI] [PubMed] [Google Scholar]
- 71.Bowren M, Bruss J, Manzel K, Edwards D, Liu C, Corbetta M, Tranel D, Boes AD (2022) Post-stroke outcomes predicted from multivariate lesion-behaviour and lesion network mapping. Brain 145:1338–1353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Crockett RA, Hsu CL, Dao E, Tam R, Eng JJ, Handy TC, Liu-Ambrose T (2021) Painting by lesions: White matter hyperintensities disrupt functional networks and global cognition. Neuroimage 236:118089. [DOI] [PubMed] [Google Scholar]
- 73.Lie IA, Weeda MM, Mattiesing RM, Mol MAE, Pouwels PJW, Barkhof F, Torkildsen O, Bo L, Myhr KM, Vrenken H (2022) Relationship Between White Matter Lesions and Gray Matter Atrophy in Multiple Sclerosis: A Systematic Review. Neurology 98:e1562–e1573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Albert MS, Moss MB, Tanzi R, Jones K (2001) Preclinical prediction of AD using neuropsychological tests. J Int Neuropsychol Soc 7:631–639 [DOI] [PubMed] [Google Scholar]
- 75.Gavett BE, Horwitz JE (2012) Immediate list recall as a measure of short-term episodic memory: insights from the serial position effect and item response theory. Arch Clin Neuropsychol 27:125–135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Casaletto KB, Marx G, Dutt S, Neuhaus J, Saloner R, Kritikos L, Miller B, Kramer JH (2017) Is “Learning” episodic memory? Distinct cognitive and neuroanatomic correlates of immediate recall during learning trials in neurologically normal aging and neurodegenerative cohorts. Neuropsychologia 102:19–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Rocca MA, Valsasina P, Absinta M, Riccitelli G, Rodegher ME, Misci P, Rossi P, Falini A, Comi G, Filippi M (2010) Default-mode network dysfunction and cognitive impairment in progressive MS. Neurology 74:1252–1259 [DOI] [PubMed] [Google Scholar]
- 78.Tona F, Petsas N, Sbardella E, Prosperini L, Carmellini M, Pozzilli C, Pantano P (2014) Multiple sclerosis: altered thalamic resting-state functional connectivity and its effect on cognitive function. Radiology 271:814–821 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The functional connectivity data equivalent to that used in this study is available online through the Harvard Dataverse at: https://doi.org/10.7910/DVN/ILXIKS and the pipeline used to prepare the functional connectivity data is available at: https://github.com/bchcohenlab/BIDS_to_CBIG_fMRI_Preproc2016. The code to prepare structural connectivity maps is available at: https://storage.googleapis.com/bcblabweb/index.html and the structural connectivity data is available at: https://www.humanconnectome.org/study/hcp-young-adult/document/1200-subjects-data-release. Statistical analyses were performed in MatLab (version 2019b) or SPSS (version 27.0.1.0). MS lesion data is available for review upon reasonable request.


