The prevalence of cardiovascular disease (CVD) is rising due to an aging population1. Consequently, there will likely be an increased demand for cardiologists with a predicted shortage of physicians by the year 2034,2 including in cardiology3.
Yet little research has quantified “proximity” to cardiologists with a primary focus on analyzing hospitals, emergency departments, and procedural labs3,4. To fill this gap, we conducted this analysis to comprehensively quantify geographical distance to cardiologists by utilizing national level data.
In June 2022, we obtained data on national provider identification from the Centers for Medicare and Medicaid National Plan and Provider Enumeration System (NPI). We then filtered the dataset for cardiologists, defined according to taxonomy numbers for cardiovascular diseases, Interventional Cardiology (IC), Advanced Heart Failure & Transplant Cardiology (HF), and/or Clinical Cardiac Electrophysiology (EP).
Using their business addresses, we geocoded each cardiologist’s longitude and latitude. We then calculated the distance between the longitude/latitude of the centroid of each US census block to that of the nearest cardiologist (overall, interventional, EP, and HF). The national median distance to the nearest cardiologist was determined, weighted by census block population (based on 2020 Census), and stratified by Urban vs Rural areas (Census Bureau classification). Similarly, we quantified the distance to the nearest primary care provider with taxonomy codes for internal medicine or family medicine (IM/FM). Variations in distance based on race and ethnicity were calculated by weighting corresponding population count in each census block.
Analyses were conducted using QGIS version 3.22, Python version 3.9.12, and Geopandas version 0.11.0. Institutional review board approval was not required as no patient-level data was used. The data that support the findings of this study are available from the corresponding author upon reasonable request.
Of 8,132,968 census blocks in the US, 4,191,709 of the census blocks belong to urban areas with a population of ~265 million, while 3,941,259 of the census blocks belong to rural areas with a population of ~66 million.
Across the US, a total of 47,225 cardiologists were identified, including 9,594 interventional, 4,328 EP, and 973 HF physicians. The overall median distance to the closest cardiologist was 2.84km (25th percentile (Q1): 0.79km, 75th percentile (Q3): 11.13km), with 85.2% of individuals living within 20km of a cardiologist. Distance was lower in the eastern US (Figure 1A). Among specialties, interventional cardiologists had the shortest distance (5.06km, Q1: 1.46km,Q3: 18.76km), followed by EP (7.35 km, Q1: 2.12km, Q3: 27.16km) and HF (16.46km, Q1: 4.8km, Q3: 61.18km) cardiologists (Figure 1B). Notably, access to HF cardiologists often requires individuals to travel over 100km, except for those living in large cities. While we noticed a general trend of subspecialists practicing in hospitals, there are exceptions to this finding, as highlighted by the closer proximity to IC and EP.
Figure 1.
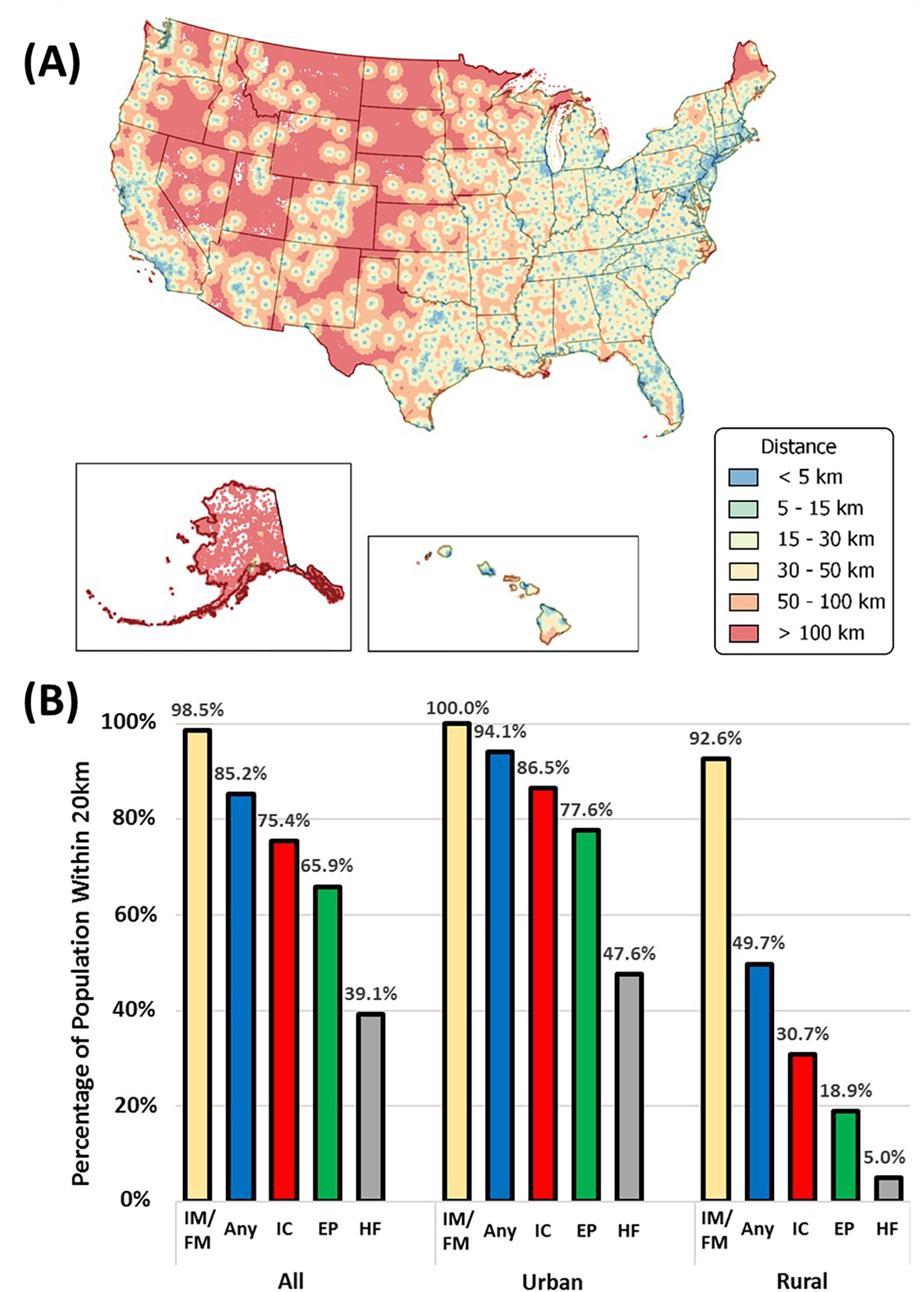
Mapping geographic proximity to cardiologists in the US (A) Map of mean distance from each census block to any cardiologist and (B) Percentage of residents within 20km of an internal medicine or family medicine (IM/FM) physician, cardiologist, and cardiologist subspecialties, including Interventional Cardiology (IC), Electrophysiology (EP), and Heart Failure (HF). Data also categorized by urban and rural areas.
In contrast, the median distance to the nearest primary care provider (IM/FM physician) was 0.81km (Q1: 0.22km, Q3: 3.11km). Notably, 98.5% reside within a 20km radius of a primary care provider, and there is minimal variation between urban and rural areas.
On a national level, Asians had the shortest distance to cardiologists, followed by non-Hispanic Black, Hispanic, non-Hispanic White, and Hawaiian individuals. Native Americans had the longest distance.
In this study, individuals in the eastern US have shorter distances to cardiologists of all subspecialties, with interventional cardiologists being the most accessible, followed by EP cardiologists. Significant distances were noted for HF cardiologists, especially in rural areas. Proximity to all cardiologist types was better in urban areas.
Few studies have delved into the topic of distance to cardiologists. Aneja et al demonstrated the geographical misdistribution of cardiologists5. Longer distances to cardiologists can reduce the likelihood of seeking a medical consultation at symptom onset, lead to less adherence to follow-up visits, and result in therapeutic inertia in serious conditions. Geographic proximity does not necessarily imply access. While proximity can improve access, social and financial barriers may hinder it.
Our study investigated regional variations in distance to cardiologists, including subspecialists. Identifying areas with greater distances, combined with patient density for cardiovascular disease (CVD), can aid in more effective resource allocation. This involves planning cardiology fellowships and offering incentives like loan repayment plans and visa waivers to encourage working in underserved areas. Additionally, our study supports exploring telehealth interventions in rural regions, although the challenge of providing high-speed internet access in these areas should not be overlooked.
Additionally, we found that subspecialists typically practice in hospitals, but this trend varies among subspecialties. Future research should explore these dynamics and their potential role in addressing healthcare disparities.
Our study carries limitations including not considering the prevalence of CVD and inaccuracies in NPI specialties and in Census data, as well as not accounting for the actual driving distances. Moreover, the published practice address may not capture rotating practices at other locations, such as locums. Nonetheless, the national scope of our data provides valuable insights into resource allocation and potential solutions.
Funding:
This work was partly funded by the National Institute on Minority Health and Health Disparities Award # P50MD017351
Footnotes
Disclosures: None of the authors have conflicts of interest relevant to the contents of this manuscript.
References
- 1.Mohebi R, Chen C, Ibrahim NE, et al. Cardiovascular Disease Projections in the United States Based on the 2020 Census Estimates. J Am Coll Cardiol. 2022;80(6):565–578. doi: 10.1016/j.jacc.2022.05.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.AAMC Report Reinforces Mounting Physician Shortage. AAMC. Accessed February 27, 2023. https://www.aamc.org/news-insights/press-releases/aamc-report-reinforces-mounting-physician-shortage
- 3.Rodgers GP, Conti JB, Feinstein JA, et al. ACC 2009 survey results and recommendations: Addressing the cardiology workforce crisis A report of the ACC board of trustees workforce task force. J Am Coll Cardiol. 2009;54(13):1195–1208. doi: 10.1016/j.jacc.2009.08.001 [DOI] [PubMed] [Google Scholar]
- 4.Balamurugan A, Delongchamp R, Im L, Bates J, Mehta JL. Neighborhood and Acute Myocardial Infarction Mortality as Related to the Driving Time to Percutaneous Coronary Intervention–Capable Hospital. Journal of the American Heart Association. 5(2):e002378. doi: 10.1161/JAHA.115.002378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aneja S, Ross JS, Wang Y, et al. US Cardiologist Workforce From 1995 To 2007: Modest Growth, Lasting Geographic Maldistribution Especially In Rural Areas. Health Affairs. 2011;30(12):2301–2309. doi: 10.1377/hlthaff.2011.0255 [DOI] [PMC free article] [PubMed] [Google Scholar]


