Abstract
Objective:
To assess urologists’ perceptions and practices related to smoking and smoking cessation.
Materials and Methods:
Six survey questions were designed to assess beliefs, practices, and determinants related to tobacco use assessment and treatment (TUAT) in outpatient urology clinics. These questions were included in an annual census survey (2021) offered to all practicing urologists. Responses were weighted to represent the practicing US population of nonpediatric urologists (N=12,852). The primary outcome was affirmative responses to the question, “Do you agree it is important for urologists to screen for and provide smoking cessation treatment to patients in the outpatient clinic?” Practice patterns, perceptions, and opinions of optimal care delivery were assessed.
Results:
In total, 98% of urologists agreed (27%) or strongly agreed (71%) that cigarette smoking is a significant contributor to urologic disease. However, only 58% agreed that TUAT is important in urology clinics. Most urologists (61%) advise patients who smoke to quit but do not provide additional cessation counseling or medications or arrange follow-up. The most frequently identified barriers to TUAT were lack of time (70%), perceptions that patients are unwilling to quit (44%), and lack of comfort prescribing cessation medications (42%). Additionally, 72% of respondents stated that urologists should provide a recommendation to quit and refer patients for cessation support.
Conclusions:
TUAT does not routinely occur in an evidence-based fashion in outpatient urology clinics. Addressing established barriers and facilitating these practices with multilevel implementation strategies can promote tobacco treatment and improve outcomes for patients with urologic disease.
Introduction
Cigarette smoking causes or adversely affects the severity of a number of benign and malignant urologic conditions. Smoking is causally linked to bladder and kidney cancer,1 can lead to erectile dysfunction and infertility,2 and can exacerbate urinary incontinence and lower urinary tract symptoms.3,4 Each year, in the outpatient setting, urologists see >300,000 patients who currently smoke for tobacco-related urologic conditions.5 The frequency of these encounters provides ample opportunity for urologists to screen for and intervene to help treat tobacco use, the underlying cause of their condition.
The benefits of smoking cessation, even after diagnosis, for patients with urologic cancers and benign conditions are well established.6–10 Furthermore, when urologists do provide smoking cessation treatment or advice to quit, such guidance is well received and effective.11–14 Advice to quit has been shown to improve quit attempts nearly 5-fold among patients with newly diagnosed bladder cancer.11
For tertiary prevention to be effective, tobacco use assessment and treatment (TUAT) is recommended to occur at each visit with a health professional, regardless of the reason for the visit or the specialty of the provider.15 These interventions are recommended by multiple professional societies and the Joint Commission on Accreditation of Healthcare Organizations and have been called the “fourth pillar of cancer care” in the oncology setting.16 However, previous work has demonstrated that evidence-based TUAT does not routinely occur in outpatient urology clinics.5,6,14 Addressing this gap in care quality can improve patients’ urologic conditions and their overall health.
Improving care delivery requires pragmatic strategies aligned with stakeholder resources, capabilities, and needs. Best practices for approaching strategy development and improvement require multilevel assessment of care delivery determinants to assure acceptance, fidelity to evidence-based practices, and sustainability. Therefore, as an initial step, we sought to assess urologists’ perceptions and practices related to smoking and cessation at the population level using a professional society census delivered annually to all practicing urologists in the US. We sought to elucidate current practice patterns and barriers to delivery of smoking cessation care to inform future efforts to implement TUAT.
Methods
Question development
Six survey questions were designed to assess beliefs, practices, and determinants related to TUAT in urology clinics (Supplemental Table 1). To maximize the generalizability of our findings and our ability to compare patterns across specialties, question content framework was sourced from previously published tobacco-related surveys in urology,17 thoracic oncology,18 and medical oncology.19 The language and content of the questions were then reviewed and modified through an iterative process with tobacco-treatment and psychometric experts before approval by the American Urological Association (AUA) Data Committee.
Dissemination of survey and weighting of responses
The AUA Annual Census was available for completion on the AUA website from May 1 to September 30, 2021. Invitations to take the survey were disseminated via biweekly email blasts, online advertisements, and promotions on AUA websites and publications. Weights were applied at the individual-physician level to generate a representative population of practicing US nonpediatric urologists. Pediatric urologists were excluded. Data from the census were collected and analyzed using the survey methodology developed by Groves et al.20 and according to standard practice by the AUA data team. Two data files were established: (1) a population file containing basic demographic, geographic, and certification information on all practicing urologists in the US in 2021 and (2) a sample data file containing a broad range of information collected from the census. The two files were linked through poststratification factors to adjust for nonresponses and the contribution of each respondent in a census survey by assigned sample weight. Poststratification factors include sex, geographic location, certification status, and years since initial certification. These factors were used to develop stratification cells for calculating sample weights.
The TUAT questions were randomly assigned to half of the census respondents. Matrix sampling was performed to identify a representative sample (n=771) of US nonpediatric urologists who received and answered the TUAT questions (all respondents who completed the census, N=1601). This represents a sampling weight of 2.076, with respect to the total population of US nonpediatric urologists (N=12,852). Characteristics of the final weighted population can be found in Supplemental Table 2.
Outcomes and measures
The primary outcome of interest was affirmative responses to the question, “Do you agree it is important for urologists to screen for and provide smoking cessation treatment to patients in the outpatient clinic?” Responses are reported disaggregated but were dichotomized as “agree” (“strongly agree” or “agree”) versus “disagree” (“neutral,” “disagree,” or “strongly disagree”) for multivariable modeling. The remainder of the question responses are reported disaggregated.
Additional measures included physician characteristics and practice characteristics, details of which are listed in the study tables. Responses were either self-reported at the time of the survey or sourced from official AUA data files.
Area deprivation index (ADI) was included as a measure to better understand the equity between urologists’ patient catchment area (and, by proxy, patient socioeconomic status) and delivery of care. ADI was generated according to the address of the primary practice location of the urologist.21 The multidimensional ADI is derived from 17 education, employment, housing-quality, and poverty measures and provides granularity of location-based socioeconomic disadvantage down to the “block” level, ranking groups from 1 to 100, with those ranked 1 the least disadvantaged and those ranked 100 the most disadvantaged.
Statistical analysis
Descriptive statistics are reported as proportions of responses; differences were assessed using χ2 testing. Continuous variables are reported as medians and interquartile ranges. To elucidate the association each variable had on our primary outcome, an a priori multivariable logistic regression model was developed and used to assess the odds of agreement or disagreement about the importance of urologist TUAT. Exemption for the AUA census was granted to the AUA by the Memorial Sloan Kettering institutional review board.
Results
Most respondents (98%) agreed (27%) or strongly agreed (71%) that cigarette smoking is a significant contributor to urologic disease. However, only 58% agreed that it is important for urologists to screen for and provide smoking cessation treatment to patients in outpatient clinics. Agreement that urologist TUAT is important varied by demographic, training, and practice characteristics (Table 1). Younger urologists and female urologists were more likely to agree that urologist TUAT is important compared, respectively, to older urologists and male urologists. Urologists who had completed a fellowship (66% vs. 54% who did not), attended medical school outside the US (67% vs. 57% who trained in the US), or were trained in oncology (72% vs. 55% general urology and 60% “other” specialties) were more likely to agree that urologist TUAT is important. Those who worked in metropolitan and institutional settings (academic vs. private vs. solo) and in settings with more advanced practice provider (APP) support were also more likely to agree that urologist TUAT is important (Table 1). After adjustment for multilevel factors (Table 2), similar relationships were seen for the odds of agreeing that urologist TUAT is important, with the strongest effects among female urologists (odds ratio [OR], 1.90 [95% CI, 1.63-2.22]), those who went to medical school outside the US (OR, 1.33 [95% CI, 1.15-1.53]), those with a higher number of patients per week (OR, 2.04 [95% CI, 1.77-2.35] for ≥96 visits per week vs. <50 visits per week), and those who practice in a metropolitan area (OR, 1.81 [95% CI, 1.55-2.11]). Higher ADI of primary practice location (consistent with a catchment area including more-disadvantaged patients) was independently associated with higher odds of agreeing that urologist TUAT is important.
Table 1.
Responses to the question, “Do you agree it is important for urologists to screen for and provide smoking cessation treatment to patients in the outpatient clinic?” by urologist and practice characteristics
| Characteristic | Agree or Strongly Agree | Neutral, Disagree, or Strongly Disagree |
|---|---|---|
| Age, years | ||
| ≤34 | 517 (71) | 209 (29) |
| 35-44 | 1975 (66) | 999 (34) |
| 45-54 | 1491 (55) | 1244 (46) |
| 55-64 | 1363 (56) | 1064 (44) |
| ≥65 | 1972 (54) | 1707 (46) |
| Years in practice | ||
| ≤8 | 2249 (67) | 1109 (33) |
| 9-20 | 1735 (56) | 1384 (44) |
| 21-34 | 1891 (58) | 1388 (42) |
| ≥35 | 1444 (52) | 1343 (48) |
| Sex | ||
| Male | 6467 (57) | 4817 (43) |
| Female | 852 (68) | 407 (32) |
| Fellowship training | ||
| No | 4416 (54) | 3700 (46) |
| Yes | 2903 (66) | 1525 (34) |
| Medical school location | ||
| International | 1044 (67) | 508 (33) |
| US | 6275 (57) | 4716 (43) |
| Primary subspecialty | ||
| General without subspecialty | 4290 (55) | 3583 (46) |
| Oncology | 1264 (72) | 483 (28) |
| Others | 1765 (60) | 1158 (40) |
| Work setting | ||
| Institutional | 3635 (60) | 2383 (40) |
| Private | 3194 (57) | 2453 (43) |
| Solo practice | 490 (56) | 389 (44) |
| AUA membership section | ||
| Mid-Atlantic | 713 (59) | 503 (41) |
| New England | 320 (48) | 354 (53) |
| New York | 586 (58) | 430 (42) |
| North Central | 1306 (58) | 944 (42) |
| Northeastern | 347 (73) | 129 (27) |
| South Central | 1091 (61) | 714 (40) |
| Southeastern | 1431 (54) | 1221 (46) |
| Western | 1525 (62) | 930 (38) |
| Metropolitan status | ||
| Metropolitan | 6824 (59) | 4692 (41) |
| Nonmetropolitan | 495 (48) | 532 (52) |
| ABU certified | ||
| No | 1730 (75) | 587 (25) |
| Yes | 5589 (55) | 4637 (45) |
| APPs in practice | ||
| ≤1 | 2681 (59) | 1902 (42) |
| 2 | 778 (48) | 847 (52) |
| 3-5 | 1735 (58) | 1283 (43) |
| ≥6 | 1907 (64) | 1079 (36) |
| RNs in practice | ||
| ≤1 | 2384 (59) | 1629 (41) |
| 2-3 | 1154 (48) | 1252 (52) |
| 4-6 | 1309 (60) | 868 (40) |
| ≥7 | 1556 (58) | 1109 (42) |
| Patient visits per week | ||
| ≤50 | 2196 (59) | 1547 (41) |
| 51-70 | 1549 (59) | 1078 (41) |
| 71-95 | 1607 (56) | 1252 (44) |
| ≥96 | 1967 (59) | 1347 (41) |
| Time spent in typical visit, min | ||
| ≤1 | 1886 (52) | 1715 (48) |
| 13-15 | 2583 (58) | 1894 (42) |
| 16-20 | 1790 (66) | 944 (35) |
| ≥21 | 1060 (61) | 671 (39) |
| Inpatient procedures per typical month | ||
| None | 1386 (54) | 1167 (46) |
| 1-4 | 2274 (58) | 1623 (42) |
| 5-9 | 1468 (54) | 1236 (46) |
| ≥10 | 2192 (65) | 1198 (35) |
| ADI of primary practice location | ||
| 1-25 | 2284 (59) | 1592 (41) |
| 26-50 | 1826 (54) | 1575 (46) |
| 51-75 | 1382 (58) | 1017 (42) |
| 76-100 | 935 (59) | 645 (41) |
Data are no. (%). All comparisons are statistically significant (p<0.001) except patient visits per week (p=0.062).
ABU, American Board of Urology; ADI, area deprivation index; APP, advanced practice provider; AUA, American Urological Association; RN, registered nurse.
Table 2.
Adjusted odds of responding “Strongly Agree” or “Agree” to the question, “Do you agree it is important for urologists to screen for and provide smoking cessation treatment to patients in the outpatient clinic?”
| Variable | Odds Ratio (95% CI) | p |
|---|---|---|
| Years in practice | ||
| ≤8 | Reference | |
| 9-20 | 0.80 (0.70-0.91) | 0.001 |
| 21-34 | 1.26 (1.10-1.45) | <0.001 |
| ≥35 | 0.90 (0.77-1.05) | 0.197 |
| Sex | ||
| Male | Reference | |
| Female | 1.90 (1.63-2.22) | <0.001 |
| Fellowship Training | ||
| Yes | Reference | |
| No | 0.94 (0.84-1.07) | 0.359 |
| Medical school location | ||
| US | Reference | |
| International | 1.33 (1.15-1.53) | <0.001 |
| Primary subspecialty | ||
| Oncology | Reference | |
| General without subspecialty | 0.47 (0.40-0.56) | <0.001 |
| Other | 0.56 (0.47-0.66) | <0.001 |
| Work setting | ||
| Institutional | Reference | |
| Private group | 0.92 (0.83-1.01) | 0.083 |
| Solo practice | 0.83 (0.69-0.99) | 0.038 |
| AUA section | ||
| Mid-Atlantic | Reference | |
| New England | 0.35 (0.28-0.45) | <0.001 |
| New York | 0.66 (0.54-0.82) | <0.001 |
| North Central | 1.08 (0.90-1.28) | 0.423 |
| Northeastern | 1.63 (1.23-2.18) | 0.001 |
| South Central | 1.02 (0.85-1.22) | 0.837 |
| Southeastern | 0.73 (0.61-0.86) | <0.001 |
| Western | 0.95 (0.80-1.13) | 0.591 |
| Metropolitan status | ||
| Nonmetropolitan | Reference | |
| Metropolitan | 1.81 (1.55-2.11) | <0.001 |
| ABU certified | ||
| Yes | Reference | |
| No | 1.41 (1.23-1.62) | <0.001 |
| APPs in practice | ||
| ≤1 | Reference | |
| 2 | 0.50 (0.44-0.58) | <0.001 |
| 3-5 | 0.63 (0.56-0.71) | <0.001 |
| ≥6 | 0.79 (0.68-0.91) | 0.001 |
| RNs in practice | ||
| ≤1 | Reference | |
| 2-3 | 0.60 (0.54-0.68) | <0.001 |
| 4-6 | 0.99 (0.87-1.12) | 0.844 |
| ≥7 | 0.86 (0.76-0.98) | 0.026 |
| Patient visits per week | ||
| ≤50 | Reference | |
| 51-70 | 1.42 (1.25-1.61) | <0.001 |
| 71-95 | 1.31 (1.14-1.50) | <0.001 |
| ≥96 | 2.04 (1.77-2.35) | <0.001 |
| Time spent in typical visit, min | ||
| ≤12 | Reference | |
| 13-15 | 1.34 (1.20-1.49) | <0.001 |
| 16-20 | 2.22 (1.94-2.54) | <0.001 |
| ≥21 | 1.33 (1.13-1.56) | 0.001 |
| Inpatient procedures per typical month | ||
| None | Reference | |
| ≥10 | 1.19 (1.04-1.38) | 0.014 |
| 1-4 | 1.05 (0.92-1.19) | 0.498 |
| 5-9 | 0.97 (0.85-1.12) | 0.681 |
| ADI (continuous) of primary practice location | 1.00 (1.00-1.00) | 0.012 |
ABU, American Board of Urology; ADI, area deprivation index; APP, advanced practice provider; AUA, American Urological Association; RN, registered nurse.
Few urologists reported that they provide their own smoking cessation counseling and/or prescribe medications themselves (7%), and even fewer reported that someone on their team, such as an APP, provides such support (3%) (Figure 1). Most urologists (61%) reported that they advise patients who smoke to quit but do not provide additional cessation counseling or medications or arrange follow-up. However, more than one-third (37%) refer patients to programs outside of their clinic, and some (9%) use public health resources, such as 1-800-QUITNOW. In total, 11% reported that they deliver no smoking cessation advice, counseling, or treatment.
Figure 1.
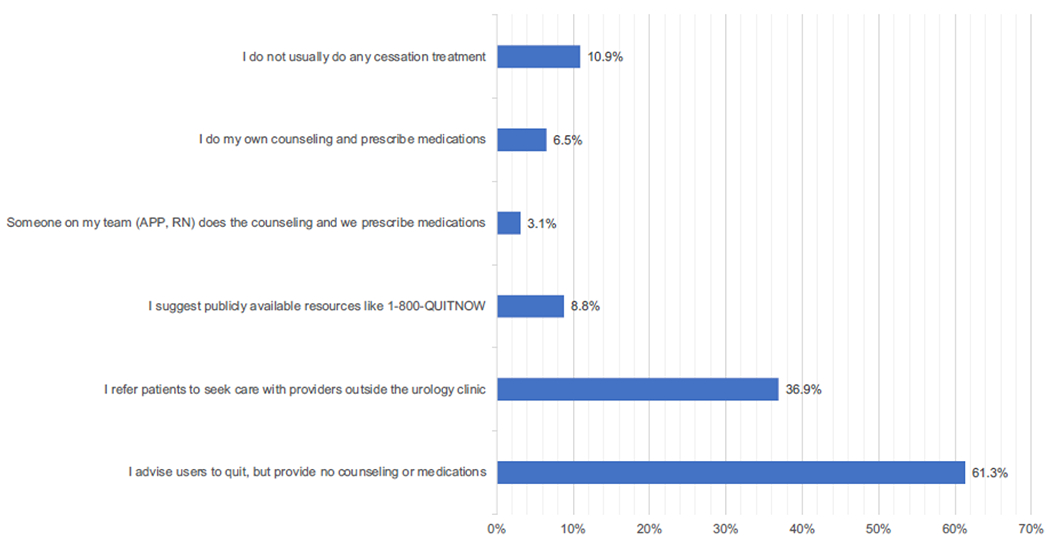
Responses to the question, “How do you typically approach smoking cessation treatment in your clinic?”
The most frequently identified barriers to TUAT in urology clinics were lack of time (70%), perceptions that patients were unwilling to quit (44%), and lack of comfort with prescribing cessation medications (42%) (Supplemental Table 3). Many urologists (28%) stated that providing smoking cessation is poorly compensated. Few urologists stated that a lack of clinical benefit (4%) or effective treatments (4%) is a barrier to TUAT.
When asked to select the ideal way to help patients quit smoking, 72% of respondents stated that urologists should provide a recommendation to quit and then refer patients for follow-up cessation support (Supplemental Table 4). Only 5% stated that urologists should have full responsibility for the provision of such treatment (counselling and prescription of medications). The remainder stated that urologists should provide or assist with medications but should refer patients for counseling with either APPs or other appropriately trained clinicians with expertise in tobacco treatment outside of the urology clinic. Very few respondents (3%) stated that urologists should play no role in smoking cessation treatment.
Discussion
Our study revealed four important findings: First, despite almost universal agreement among urologists that smoking contributes to urologic disease, many do not screen for tobacco use, and a higher percentage do not actively assist or facilitate smoking cessation in the outpatient setting. This is in stark contrast to recommendations that TUAT should occur at all medical encounters. Second, several physician and practice factors were associated with variation in agreement that urologist TUAT is important. These findings can be used to develop and target interventions to promote delivery of evidence-based care. Third, barriers to TUAT, such as lack of adequate reimbursement and more time spent with patients, are clear and should be addressed. Last, and perhaps most important, urologists overwhelmingly prefer to “outsource” TUAT to tobacco treatment specialists, a widely accepted clinical practice with evidence of effectiveness.22 These findings provide a foundation for designing workflows and other implementation strategies to improve access and use of TUAT services for patients receiving urologic care and potentially across other surgical subspecialties that see tobacco-related diagnoses.
This study represents the most comprehensive assessment to date of urologists’ beliefs and practices related to smoking and smoking cessation. Previous work by Bjurlin and colleagues focused on practices related only to patients with bladder cancer.17 That study was not conducted at the population level, across subspecialists and general urologists; instead, it focused on urologists who actively cared for patients with bladder cancer. Although the current study considered the treatment of all patients with urologic disease, comparisons can be made. In the Bjurlin study, 55.6% of urologists never discussed any component of smoking cessation with patients with bladder cancer. In our population, only 11% of urologists completely eschewed any discussion of smoking or cessation. These differences may be attributable to an evolving understanding of how smoking affects urologic disease. Supporting this point, in the Bjurlin study, 40.7% of urologists stated that smoking cessation would not alter the course or outcome of the disease. In contrast, in the present study, 98% stated that smoking is a significant contributor to urologic disease. However, it is also possible that differences in sampling allowed for a less biased estimation of true beliefs.
Changes in training over time may explain some of the differences in responses. In the Bjurlin study, urologists with formal smoking cessation training were significantly more likely to deliver smoking cessation treatment. In our study, practice differed by training experience and demographic characteristics, which suggests that details of medical school, residency, or fellowship training may influence practice. Younger urologists were more likely to agree that urologist TUAT is important—this could stem from a greater emphasis on the value of tobacco treatment in medical school or residency, and it could also reflect the lower rates of cigarette use among the younger generation. Additionally, female urologists were more likely to agree that urologist TUAT is important. Previous studies have shown that women spend more time with patients, and this may lead to better or more intensive counseling and, therefore, better outcomes; this is an area worth exploring in future studies.
System-level culture may also influence practice. Our responses differed in terms of practice setting, availability of resources, and time spent during visits, which likely reflect the “busyness” of a practice or physician. Interestingly, physicians with a primary practice location with a higher ADI (which is consistent with a local catchment area that includes more-disadvantaged patients) had a higher likelihood of agreeing that urologist TUAT is important. One promising system-level strategy for reducing variation by provider in smoking cessation practices would be for all health care clinicians and settings to adopt universal quality-of-care metrics that are inclusive of smoking cessation advice and support a practice consistent with the standards of the Centers for Disease Control, Joint Commission, National Committee for Quality Assurance, and Healthcare Effectiveness Data and Information Set.
Few urologists stated that a lack of benefit (4%) or effective treatments (4%) was a barrier to delivery of care. This prompts the question, if treatments are available and effective, what is preventing their delivery? Our results suggest that practical issues, such as lack of time, lack of familiarity with the medications, poor compensation, and competing clinical priorities, remain a hindrance to effective delivery. Clinician training and establishment of efficient workflows for screening and referral can help address these barriers. Our findings suggest a brief model of cessation support that consists of “ask, advise, and refer” (a well-accepted and evidence-based practice for tobacco treatment23) would be most effective, as most respondents (72%) stated that urologists should provide a recommendation to quit smoking and then refer patients to a formal tobacco treatment program.
To promote the health of urologic patients, the AUA should consider developing and disseminating best practices related to TUAT through either a white paper or the development of formal guidelines. The Urology Care Foundation should also consider developing additional patient-facing literature to promote tobacco use cessation and awareness as it relates to urologic disease. This should be followed by dissemination and education campaigns for both urologists and patients, to maximize the reach of these efforts.24,25 We have previously shown that guideline recommendations for TUAT for urologic conditions lag behind those for other tobacco-related diseases26; updating these guidelines would be an additional means of promoting tobacco awareness and encouraging urologists to perform TUAT. Advancing the perceived importance of TUAT through aligned incentives will also help address barriers such as lack of time, which practically can mean a lower perceived importance. Additionally, the AUA should immediately begin to advocate for policy change at the payor level to adequately compensate physicians for health-promotion counseling, particularly tobacco treatment.
Locally, urologists should work to develop system- and practice-level tools to assist with identification and referral of patients to tobacco treatment programs. We have shown that this is acceptable to both urologists and patients, and these types of electronic medical record implementation strategies have been shown to help promote care delivery at National Cancer Institute Cancer Centers.27
While this census represents the first population-level assessment of urologists’ beliefs and practices related to TUAT, several limitations to our study must be noted. First, these reported practices are likely influenced by social desirability bias, despite individual and electronic delivery of the survey, with analyses conducted in a deidentified manner. Our results potentially represent a best-case scenario for real-world practice and may overreport delivery of evidence-based care. Second, we were unable to ask about awareness of existing National Comprehensive Cancer Network guidelines, resources that are available from the Centers for Disease Control and Prevention, or knowledge of recommendations from accrediting bodies or professional societies; insight into this may help explain some of the suspected knowledge gaps. This is an area of need for future investigations and the dissemination of professional education and training. Last, as the implementation of TUAT is complex, involving multilevel factors, individual physician and practice characteristics that were not accounted for by our measures may influence urologists’ beliefs and practices. Additional qualitative exploration may provide more granularity about these determinants.
Conclusions
Although most urologists agree that smoking and tobacco use have a negative effect on urologic health, TUAT does not routinely occur in an evidence-based fashion in outpatient clinics. Addressing established barriers and facilitating these practices by the use of multilevel implementation strategies can promote tobacco treatment and improve outcomes for patients with urologic disease.
Supplementary Material
Funding:
RSM is supported by the National Cancer Institute (K08 CA259452). MSK is supported by the National Cancer Institute (P30 CA008748).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
- Richard S. Matulewicz no conflict
- William Meeks no conflict
- Rachel Mbassa no conflict
- Raymond Fang no conflict
- Ashley Pittman no conflict
- Matthew Mossanen no conflict
- Helena Furberg no conflict
- Lou-Anne Chichester no conflict
- Michelle Lui no conflict
- Scott E. Sherman no conflict
- Danil V. Makarov no conflict
- Marc A. Bjurlin no conflict
-
Jamie S. Ostroff no conflictI accept the responsibility for the completion of this document and attest to its validity on behalf of the co-authors.
Data Availability Statement:
The data sets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- 1.US Dept of Health and Human Services. Smoking Cessation: A Report of the Surgeon General.; 2020. [Google Scholar]
- 2.Harlev A, Agarwal A, Gunes SO, Shetty A, du Plessis SS. Smoking and male infertility: an evidence-based review. World J Mens Health. 2015;33(3): 143–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Koskimäki J, Hakama M, Huhtala H, Tammela TL. Association of smoking with lower urinary tract symptoms. J Urol. 1998;159(5):1580–1582. [DOI] [PubMed] [Google Scholar]
- 4.Kawahara T, Ito H, Uemura H. The impact of smoking on male lower urinary tract symptoms (LUTS). Sci Rep. 2020;10(1):20212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bernstein AP, Bjurlin MA, Sherman SE, Makarov DV, Rogers E, Matulewicz RS. Tobacco screening and treatment during outpatient urology office visits in the United States. J Urol. 2021;205(6):1755–1761. [DOI] [PubMed] [Google Scholar]
- 6.Zhao C, Bjurlin MA, Roberts T, Rink M, Shariat SF, Matulewicz RS. A systematic review and scoping analysis of smoking cessation after a urological cancer diagnosis. J Urol. 2021;205(5):1275–1285. [DOI] [PubMed] [Google Scholar]
- 7.Mima M, Huang JB, Andriole GL, Freedland SJ, Ohlander SJ, Moreira DM. The impact of smoking on sexual function. BJU Int. 2022;130(2):186–192. [DOI] [PubMed] [Google Scholar]
- 8.Kulaksiz D, Toprak T, Tokat E, et al. Sperm concentration and semen volume increase after smoking cessation in infertile men. Int J Impot Res. 2022;34(6):614–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cacciamani GE, Ghodoussipour S, Mari A, et al. Association between smoking exposure, neoadjuvant chemotherapy response and survival outcomes following radical cystectomy: systematic review and meta-analysis. J Urol. 2020;204(4):649–660. [DOI] [PubMed] [Google Scholar]
- 10.Rink M, Crivelli JJ, Shariat SF, Chun FK, Messing EM, Soloway MS. Smoking and bladder cancer: a systematic review of risk and outcomes. Eur Urol Focus. 2015;1(1): 17–27. [DOI] [PubMed] [Google Scholar]
- 11.Bassett JC, Gore JL, Chi AC, et al. Impact of a bladder cancer diagnosis on smoking behavior. J Clin Oncol. 2012;30(15):1871–1878. [DOI] [PubMed] [Google Scholar]
- 12.Bassett JC, Gore JL, Kwan L, et al. Knowledge of the harms of tobacco use among patients with bladder cancer. Cancer. 2014;120(24):3914–3922. [DOI] [PubMed] [Google Scholar]
- 13.Bassett JC, Matulewicz RS, Kwan L, McCarthy WJ, Gore JL, Saigal CS. Prevalence and correlates of successful smoking cessation in bladder cancer survivors. Urology. 2021;153:236–243. [DOI] [PubMed] [Google Scholar]
- 14.Matulewicz RS, Bassett JC, Kwan L, et al. Using a multilevel implementation strategy to facilitate the screening and treatment of tobacco use in the outpatient urology clinic: A prospective hybrid type I study. Cancer. 2022;128(6):1184–1193. [DOI] [PubMed] [Google Scholar]
- 15.Lowy DR, Fiore MC, Willis G, Mangold KN, Bloch MH, Baker TB. Treating smoking in cancer patients: an essential component of cancer care-The New National Cancer Institute Tobacco Control Monograph. JCO Oncol Pract. 2022;18(12):e1971–e1976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fiore MC, D’Angelo H, Baker T. Effective cessation treatment for patients with cancer who smoke-the fourth pillar of cancer care. JAMA Netw Open. 2019;2(9):e1912264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bjurlin MA, Goble SM, Hollowell CMP. Smoking cessation assistance for patients with bladder cancer: a national survey of American urologists. J Urol. 2010;184(5):1901–1906. [DOI] [PubMed] [Google Scholar]
- 18.Warren GW, Marshall JR, Cummings KM, et al. Practice patterns and perceptions of thoracic oncology providers on tobacco use and cessation in cancer patients. J Thorac Oncol. 2013;8(5):543–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Warren GW, Marshall JR, Cummings KM, et al. Addressing tobacco use in patients with cancer: a survey of American Society of Clinical Oncology members. J Oncol Pract. 2013;9(5):258–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Groves RM, Fowler FJ, Couper MP, Lepkowski JM, Singer E, Tourangeau R. Survey Methodology. 2nd ed. Wiley-Blackwell; 2013. [Google Scholar]
- 21.Kind AJH, Buckingham WR. Making neighborhood-disadvantage metrics accessible - the neighborhood atlas. N Engl J Med. 2018;378(26):2456–2458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sheffer CE, Payne T, Ostroff JS, et al. Increasing the quality and availability of evidence-based treatment for tobacco dependence through unified certification of tobacco treatment specialists. J Smok Cessat. 2016;11(4):229–235. [Google Scholar]
- 23.Vidrine JI, Shete S, Cao Y, et al. Ask-Advise-Connect: a new approach to smoking treatment delivery in health care settings. JAMA Intern Med. 2013;173(6):458–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Baumann AA, Hooley C, Kryzer E, et al. A scoping review of frameworks in empirical studies and a review of dissemination frameworks. Implement Sci. 2022;17(1):53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schipper K, Bakker M, De Wit M, Ket JCF, Abma TA. Strategies for disseminating recommendations or guidelines to patients: a systematic review. Implement Sci. 2016;11(1):82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Michael J, Matulewicz RS, Bjurlin MA. Assessment of tobacco screening and smoking cessation recommendations among bladder cancer guidelines: a call to action. J Urol. 2022;207(3):490–492. [DOI] [PubMed] [Google Scholar]
- 27.Hohl SD, Matulewicz RS, Salloum RG, et al. Integrating tobacco treatment into oncology care: reach and effectiveness of evidence-based tobacco treatment across National Cancer Institute-Designated Cancer Centers. J Clin Oncol. 2022. [Online ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data sets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.


