Abstract
Background.
Intensive care unit (ICU) clinicians struggle to routinely implement the ICU Liberation bundle (ABCDEF bundle). As a result, critically ill patients experience increased risk of morbidity and mortality. Despite extensive research related to the barriers and facilitators of bundle use, little is known regarding which implementation strategies are used to facilitate its adoption and sustainability.
Objectives.
To identify implementation strategies used to increase adoption of the ABCDEF bundle and how those strategies are perceived by end-users (i.e., ICU clinicians) related to their helpfulness, acceptability, feasibility, and cost.
Methods.
We conducted a national, cross-sectional survey of ICU clinicians from the 68 ICU sites that previously participated in the Society of Critical Care Medicine’s ICU Liberation Collaborative. The survey was structured using the 73 Expert Recommendations for Implementing Change (ERIC) implementation strategies. Surveys were delivered electronically to site contacts.
Results.
Nineteen ICUs (28%) returned completed surveys. Sites used 63 of the 73 ERIC implementation strategies, with frequent use of strategies that may be readily available to clinicians (e.g., providing educational meetings or ongoing training), but less use of strategies that require changes to well-established organizational systems (e.g., alter incentive allowance structure). Overall, sites described the ERIC strategies used in their implementation process to be moderately helpful (mean score >3<4 on a 5-point Likert scale), somewhat acceptable and feasible (mean score >2<3), and either not-at-all or somewhat costly (mean scores >1<3).
Conclusions.
Our results show a potential over-reliance on accessible strategies and the possible benefit of unused ERIC strategies related to changing infrastructure and utilizing financial strategies.
Keywords: Intensive Care Unit, ICU, ICU Clinicians, ICU Liberation Bundle, ABCDEF Bundle, implementation science, implementation strategies, implementation outcomes, ERIC, multidisciplinary, mechanical ventilation, Perceptions
INTRODUCTION
The ICU Liberation bundle (i.e., ABCDEF bundle) is a multidisciplinary care approach that incorporates many of the recommendations of the Society of Critical Care Medicine’s (SCCM’s) Clinical Practice Guidelines for the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult Patients in the ICU.1,2 Implementation of the ABCDEF bundle improves health outcomes of critically ill adults by decreasing both hospital- and ICU-associated morbidity and mortality, reducing total ventilator days, and preserving baseline functional mobility status.3,4 However, not all studies of the individual components of the ABCDEF bundle show equal effectiveness in obtaining these improved health outcomes. Of note is the early mobility intervention, the “E” component in ABCDEF bundle, which arguably shows the largest variation in improvement of health outcomes.5–11 Despite variations in results for the individual interventions of the bundle, a recent study by Pun et al. shows that improved health outcomes may be best achieved with a dose-response relationship: patients who received higher proportions of the overall bundle experienced improved health outcomes when compared to those who received lower proportions of the same treatment or those who received only partial bundle treatments.4 While the benefits of the bundle are well-established, so are the struggles of clinicians to effectively adopt the bundle into routine practice. Previous studies show patient-, provider-, and institutional-level barriers and facilitators to the delivery of this evidence-based bundle.12–16 These existing struggles with implementation appear to be intensified by the effects of the ongoing COVID-19 pandemic on clinical practice. For example, an international, 2-day point prevalence study by Liu and colleagues found low implementation of all six ABCDEF bundle components.17
Implementation strategies are fundamental to the field of implementation science because they provide specifications for how evidence-based recommendations derived from research are adopted into clinical practice.18 Implementation strategies can include a single or complex combination of strategies that address multiple barriers to implementation. In 2015, Powell et al. developed a taxonomy of implementation strategies to standardize the language used to describe implementation efforts and improve the generalizability of findings. This taxonomy, referred to as the Expert Recommendations for Implementing Change (ERIC) project, provided conceptual and operational definitions for 73 discrete implementation strategies combining expert opinion and a modified Delphi process.19 The 73 strategies from the ERIC taxonomy have been organized into nine thematic categories and ranked according to importance and feasibility.20
Understanding key stakeholders’ perceptions of the importance and feasibility of strategies are essential considerations when selecting implementation strategies for overcoming barriers to practice. To date, there is limited knowledge of the strategies used to implement the ABCDEF bundle into everyday clinical care. Balas et al. provided a guideline to facilitate implementation and quality improvement efforts of the PADIS guidelines using the ABCDEF bundle,1 and Stollings et al. reported best practices for facilitating the ABCDEF bundle using interprofessional team rounds.21 Others have reported clinical strategies for overcoming barriers to practice.13,22 However, these strategies are clinical practice strategies that describe actions for what to do to improve bundle implementation, such as “perform daily spontaneous breathing trials regardless of the perceived success”22 and “secure lines/tubes/drains” prior to early mobility.13 There is limited understanding of the process for how to best implement this best practice care bundle. By not understanding how to promote changes to clinical practice or the best strategies to overcome implementation barriers, we perpetuate the ongoing use of over-sedation, excessive use of analgesia, failure to recognize or treat delirium, prolonged immobility, and lack of family involvement among patients receiving care in the adult ICU.
The primary objective of this survey study was to identify the strategies used to increase adoption of the ABCDEF bundle in ICUs that participated in the SCCM ICU Liberation Collaborative.23 Our secondary objective was to assess clinicians’ perceptions of how helpful, acceptable, feasible, and costly they found each strategy when implementing the bundle. This manuscript was developed following the Checklist for Reporting of Survey Studies (CROSS) guidelines.24
METHODS
Study Design
This cross-sectional, national survey was developed to assess which strategies were used by ICUs to facilitate adoption of the ABCDEF bundle during their participation in the ICU Liberation Collaborative. Briefly, the ICU Liberation Collaborative was a nationwide quality improvement project that ran from August 2015 to April 2017. The Collaborative aimed to improve ICU teamwork and foster the implementation of the ABCDEF bundle in diverse ICUs across the United States.3,25 This study was approved by the Institutional Review Board at The Ohio State University, Columbus Ohio (2019H0092, Determinants of Implementation Success Coordinating Ventilator, Early Ambulation and Rehabilitation Efforts in the ICU, approved April 14, 2019). All participants provided informed consent.
Survey
The Consolidated Framework for Implementation Research (CFIR) and the ERIC strategies guided survey development [see Supplement A].27,28 The survey had ten categories. The first nine categories asked participants to identify their use of the 73 discrete ERIC implementation strategies during their ABCDEF bundle implementation by themes, and the final category contained free-text entry, allowing participants to share additional implementation strategies not addressed in the survey. Categories 1–9 used a skip logic method to ask participants yes/no questions for each implementation strategy (e.g., Strategy: conduct ongoing training; Q: Did your institution plan for and conduct ABCDEF bundle training in an ongoing way?). If answered ‘yes’, participants were then prompted to identify how helpful, acceptable, feasible, and costly they perceived each strategy using a 5-point Likert scale. If answered ‘no’, the survey skipped the Likert prompts and moved to the next question. Due to the skip logic format, the total items varied by site (minimum 73, maximum 365, excluding free-text answers). A participant profile for up to 4 participants per site requested information on a) responsibilities held during the course of ICU Liberation Collaborative; b) profession; and c) current years of experience.
Survey Administration and Data Collection
The survey was administered between November 2020 and February 2021 by email via REDCap (The Ohio State University), a secure, web-based data collection and management software platform.27,28 Each site was provided access to the survey using an electronic link provided in the invitational email.
Participants
Participants were recruited using convenience sampling from the 68 adult ICU sites that participated in the SCCM’s ICU Liberation Collaborative. Each site was required to have at least one participant who held responsibilities during the ICU Liberation Collaborative: acted as ICU Liberation team leader or team member; participated as a bundle champion; trained or educated other ICU clinicians on the ABCDEF bundle; completed data for the collaborative; revised bundle-related policies, communicated with hospital administration regarding bundle implementation efforts, needs, or results. Because each site was limited to one survey, we encouraged participation from colleagues across multiple disciplines to promote input from diverse perspectives. Each participant (up to four per site) was eligible to receive a $25 Amazon e-gift card after survey completion, with an additional $25 provided to the person who entered the responses.
Data Analysis
Frequencies were used to describe the characteristics of ICU sites and survey respondents, and frequencies and percentages were used to summarize the usage of each implementation strategy among the sites that completed the survey. Based on the 5-Likert scales, we visualized the mean and standard deviation of the average implementation outcomes (i.e., helpfulness, acceptability, feasibility, and costliness) of strategies within each category. All the analyses were conducted in R 4.1.1.
RESULTS
Sample
Of the 68 sites invited to participate, 29 completed the consent process; 19 completed the full survey and were included in the final analysis (response rate 27.9%). Most of the 19 sites were from large (n=11), mixed medical/surgical ICUs (n=10) located in urban settings (n=13) (Table 1). The 19 sites were in three distinct geographical regions in the United States: east coast (n=6), west coast (n=7), and Midwest (n=6). A total of 53 individuals participated in the survey across the 19 sites. The disciplines most frequently represented were nurse and physician leaders (n=22), ICU pharmacists (n=11), and respiratory or physical therapists (n=7). Forty-eight participants had responsibilities in their site’s ICU at the time of the SCCM’s ICU Liberation Collaborative, and each site had at least two members who held responsibilities in their ICU during the original ICU Liberation Collaborative. The mean years of professional experience among respondents was 18.75 years.
Table 1.
Characteristics of ICU Sites and Survey Respondents
| Characteristics of ICU sites | n = 19 |
|---|---|
| ICU Type | |
| Medical | 4 |
| Surgical | 3 |
| Cardiac | 0 |
| Neurological | 2 |
| Mixed Medical/Surgical | 10 |
| ICU Size | |
| Small (<10 beds) | 2 |
| Medium (11–30 beds) | 6 |
| Large (31+ beds) | 11 |
| Academic Status | |
| Teaching | 12 |
| Non-teaching | 7 |
| Region in the United States | |
| East | 6 |
| Midwest | 6 |
| West | 7 |
| Location | |
| Urban | 13 |
| Suburban | 5 |
| Rural | 1 |
| Characteristics of survey respondents | n = 53 |
| Profession | |
| Registered Nurse | 3 |
| Nurse Leadership | 16 |
| Physician | 3 |
| Physician Leadership | 6 |
| Pharmacist | 11 |
| Respiratory or Physical Therapist | 7 |
| Quality Improvement | 3 |
| Other | 4 |
Use of Implementation Strategies
Across the 19 sites, 63 of the 73 ERIC implementation strategies were used to increase adoption of the ABCDEF bundle (Table 2). Ten strategies were not used by any site (Table 3). Following the grouping and categorization of ERIC strategies by Waltz et al.,20 the unused strategies were primarily those in the Change Infrastructure and Utilize Financial Strategies categories.
Table 2.
Implementation Strategies Used by ICUs to Facilitate Adoption of the ABCDEF Bundle
| Implementation Strategy Categories | Implementation Strategy | N = 19 ICU n (%) |
|---|---|---|
| Category 1: Train and Educate Stakeholders | Conduct educational meetings | 18 (94.7%) |
| Develop educational materials | 17 (89.5%) | |
| Conduct ongoing training | 17 (89.5%) | |
| Distribute educational materials | 16 (84.2%) | |
| Use train-the-trainer strategies | 15 (78.9%) | |
| Make training dynamic | 14 (73.7%) | |
| Create a learning collaborative | 12 (63.2%) | |
| Conduct educational outreach visits | 10 (52.6%) | |
| Shadow other experts | 9 (47.4%) | |
| Provide ongoing consultation | 8 (42.1%) | |
| Work with educational institutions | 1 (5.3%) | |
| Category 2: Develop Stakeholder Interrelationships | Use an advisory board and/or workgroup | 18 (94.7%) |
| Identify and prepare champions | 15 (78.9%) | |
| Recruit, designate, and train for leadership | 13 (68.4%) | |
| Promote network weaving | 13 (68.4%) | |
| Involve executive boards | 13 (68.4%) | |
| Use an implementation advisor | 11 (57.9%) | |
| Inform local opinion leaders | 11 (57.9%) | |
| Organize clinician implementation team meetings | 11 (57.9%) | |
| Identify early adopters | 11 (57.9%) | |
| Develop an implementation glossary | 11 (57.9%) | |
| Capture and share local knowledge | 9 (47.4%) | |
| Conduct local consensus discussions | 9 (47.4%) | |
| Build a coalition | 8 (42.1%) | |
| Obtain formal commitments | 5 (26.3%) | |
| Visit other sites | 3 (15.8%) | |
| Develop academic partnerships | 2 (10.5%) | |
| Model and simulate change | 2 (10.5%) | |
| Category 3: Engage Consumers | Involve patients/consumers and family members | 14 (73.7%) |
| Prepare patients/consumers to be active participants | 13 (68.4%) | |
| Intervene with patients/consumers to enhance uptake and adherence | 5 (26.3%) | |
| Use mass media | 5 (26.3%) | |
| Increase demand | 1 (5.3%) | |
| Category 4: Use Evaluative and Iterative strategies | Purposely reexamine the implementation | 16 (84.2%) |
| Audit and provide feedback | 16 (84.2%) | |
| Conduct local needs assessment | 15 (78.9%) | |
| Assess for readiness and identify barriers and facilitators | 12 (63.2%) | |
| Develop and organize quality monitoring systems | 11 (57.9%) | |
| Develop and implement tools for quality monitoring | 9 (47.4%) | |
| Develop a formal implementation blueprint | 9 (47.4%) | |
| Stage implementation scale-up | 7 (36.8%) | |
| Conduct cyclical small tests of change | 6 (31.6%) | |
| Obtain and use patients/consumers and family feedback | 2 (10.5%) | |
| Category 5: Utilize Financial Strategies | Access new funding | 3 (15.8%) |
| Fund and contract for the clinical innovation | 3 (15.8%) | |
| Alter incentive/allowance structures | 1 (5.3%) | |
| Category 6: Provide Interactive Assistance | Provide clinical supervision | 10 (52.6%) |
| Facilitation | 9 (47.4%) | |
| Provide local technical assistance | 7 (36.8%) | |
| Centralize technical assistance | 3 (15.8%) | |
| Category 7: Adapt and Tailor Context | Promote adaptability | 12 (63.2%) |
| Tailor strategies | 8 (42.1%) | |
| Use data experts | 6 (31.6%) | |
| Use data warehousing techniques | 3 (15.8%) | |
| Category 8: Support Clinicians | Remind clinicians | 16 (84.2%) |
| Facilitate relay of clinical data to providers | 7 (36.8%) | |
| Create new clinical teams | 6 (31.6%) | |
| Develop resource sharing agreements | 2 (10.5%) | |
| Revise professional roles | 2 (10.5%) | |
| Category 9: Change Infrastructure | Mandate change | 13 (68.4%) |
| Change physical structure and equipment | 12 (63.2%) | |
| Change record systems | 10 (52.6%) | |
| Start a dissemination organization | 1 (5.3%) |
Table 3.
Implementation Strategies Not Used by any Site to Facilitate Adoption of the ABCDEF Bundle
| Implementation Strategy Categories | Implementation Strategy |
|---|---|
| Category 5: Utilize Financial Strategies | Alter patient/consumer fees |
| Make billing easier | |
| Use capitated payments | |
| Use other payment schemes methods | |
| Place the innovation on fee for service lists/formularies | |
| Develop disincentives | |
| Category 9: Change Infrastructure | Change liability Laws |
| Create or change credentialing and/or licensing standards | |
| Change accreditation or membership requirements | |
| Change service sites |
Category 1: Train and Educate Stakeholders (11 strategies)
Eight of the 11 strategies in the Train and Educate Stakeholders category were used by more than half the ICUs. The most frequently reported strategies were conducting educational meetings (94.7%, n=18), developing educational materials (89.5%, n=17), conducting ongoing training (89.5%, n=17), distributing educational materials (84.2%, n=16), and using train-the-trainer strategies (78.9%, n=15). More than half the sites also reported use of make training dynamic (73.3%, n= 14), create a learning collaborative (63.2%, n=12), and conduct educational outreach visits (52.6%, n=10).
Category 2: Develop Stakeholder Interrelationships (17 strategies)
Each strategy in the Develop Stakeholder Interrelationships category was used by at least one site. The most frequently reported strategies were use an advisory board and/or workgroup (94.7%, n=18), identify and prepare champions (78.9%, n=15). The strategies recruit, designate, and train for leadership; promote network weaving; and involve executive boards were used by 68.4% (n=13) sites. Eleven sites (57.9%) reported using an implementation advisor, informing local opinion leaders, organizing clinician implementation team meetings, identifying early adopters, and developing an implementation glossary.
Category 3: Engage Consumers (5 strategies)
Each strategy in the Engage Consumer category was used by at least one site. The most frequently reported strategies were involve patients/consumers and family members (73.7%, n=14) and prepare patients/consumers to be active participants (68.4%, n=13). Only one site reported using increase demand (5.3%).
Category 4: Use Evaluative and Iterative Strategies (10 strategies)
Each strategy in the Use Evaluative and Iterative Strategies category was used by at least one site. The most frequently reported strategies were audit and provide feedback (84.2%, n=16), purposively reexamine the implementation (84.2%, n=16), and conduct local needs assessment (78.9%, n=15). Only two sites (10.5%) reported using obtain and use patients/consumers and family feedback to facilitate their implementation efforts.
Category 5: Utilize Financial Strategies (9 strategies)
Only three strategies were used, all infrequently. Three sites used access new funding and fund and contract for the clinical innovation (15.8%); one site used altering incentive/allowance structures (5.3%).
Category 6: Provide Interactive Assistance (4 strategies)
Each strategy was used by at least one site. Only one strategy, provide clinical supervision, was used by half the sites (52.6%, n=10).
Category 7: Adapt and Tailor Context (4 strategies)
Each strategy was used by at least one site. Only promote adaptability was used by more than half the sample (63.2%, n=12).
Category 8: Support Clinicians (5 strategies)
Each strategy was used by at least one site. Only remind clinicians was used by the majority of the sample (84.2%, n=16).
Category 9: Change Infrastructure (8 strategies)
Of the eight strategies in this category, only four were used by at least one site. These strategies include mandate change (68.4%, n=13), change physical structure and equipment (63.2%, n=12), change record systems (52.6%, n=10), and start a dissemination organization (5.3%, n=1).
Free-text Responses
After discussion and consensus among the research team, we found most free-text responses to be adequately described by the existing 73 ERIC strategies [Supplement B]. We identified one additional strategy from the free-text response section not described in the ERIC taxonomy: Engage the Naysayers. Participants described “We engaged the ‘naysayers’ at the beginning [of implementation efforts] to get them on board. They assisted with development of things like the Bundle Implementation Worksheet.”
Implementation Outcomes
Using a 5-point Likert scale (1=not at all, 2=somewhat, 3=moderately, 4=very, 5=extremely), we asked sites to describe their perceptions of the helpfulness, acceptability, feasibility, and costliness for the strategies used in their implementation efforts. A summary of these results, by category, are shown in Figure 1. Likert responses for the individual implementation strategies can be found in Supplement C.
Figure 1.
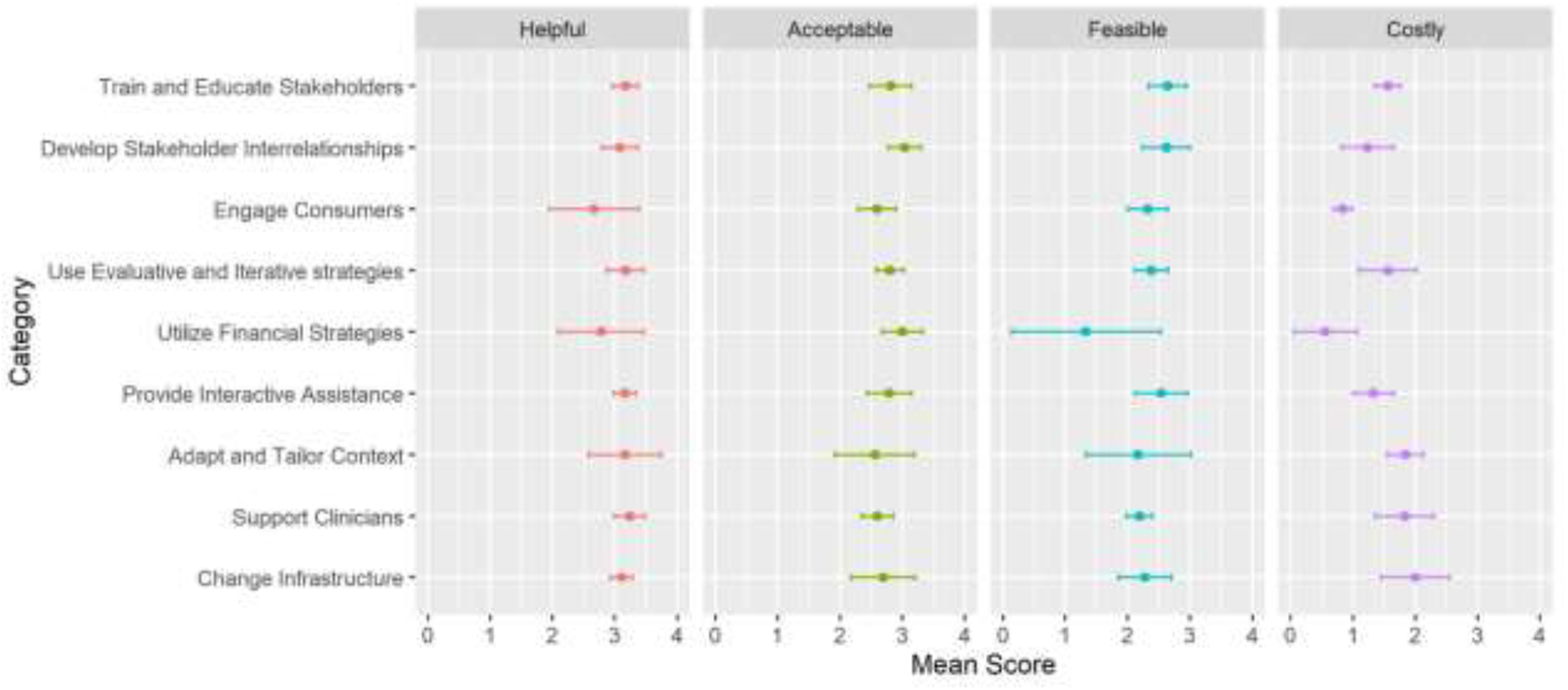
Implementation Outcomes: Perceptions of Helpfulness, Acceptability, Feasibility, & Costliness of the Nine Categories of Implementation Strategies
Helpfulness
Sites described the ERIC categories as moderately helpful (i.e., a mean score greater than 3 and less than 4), excluding those of Engaging Consumers and Utilizing Financial Strategies, which were described as only somewhat helpful (mean score 2.67 (SD 0.72) and 2.78 (SD 0.69), respectively).
Acceptability
Sites described most ERIC categories as somewhat acceptable (i.e., mean scores greater than 2 and less than 3). The Utilize Financial Strategies and Develop Stakeholder Interrelationships categories were considered moderately acceptable (mean score 3.0 (SD 0.33) and 3.04 (SD 0.27), respectively).
Feasibility
Sites described most ERIC categories as somewhat feasible (i.e., mean scores greater than 2 and less than 3). An exception was the Utilize Financial Strategies category which was described as not-at-all feasible (mean score 1.33 (SD 1.2)).
Costliness
Sites described all ERIC categories as not-at-all or somewhat costly (i.e., mean scores greater than one and less than 3). The Utilize Financial Strategies category was described as not-at-all costly (mean score 0.56 (SD 0.51)).
DISCUSSION
This multicenter, national survey study identified the implementation strategies used by ICU sites to implement the ABCDEF bundle during their participation in the SCCM’s ICU Liberation Collaborative. We found broad use of strategies that may be readily available to clinicians or considered routine practice in the critical care setting, such as conducting educational meetings, conducting ongoing training, and providing educational materials. There was minimal use of strategies that require changes to well-established systems, such as those in the Change Infrastructure and Utilize Financial Strategies categories. There was a discrepancy in sites’ perceptions between the feasibility and helpfulness of highly used strategies, such as those in the Train and Educate Stakeholders category. This may indicate that educational strategies with high feasibility may not necessarily be perceived as the most helpful. There also exists a disconnect between the perceived helpfulness of strategies used to implement the ABCDEF bundle, and the observed bundle outcomes. Despite sites describing the ERIC strategies as helpful, overall bundle compliance remains low.17 Additionally, although only used by a few sites, financial strategies were perceived as low cost and had moderate acceptability.
Sites reported using 63 of the 73 strategies described in the ERIC taxonomy of implementation strategies; considerably more than other studies that measured the use of ERIC strategies in quality improvement implementation efforts.29,30 The higher number of reported strategies may be due to the bundle’s complexity. The ABCDEF bundle is a complicated intervention that requires coordination and collaboration across disciplines in a complex care environment. This may account for sites’ need to apply numerous strategies during implementation efforts.
The shear breadth of the strategies that were identified suggests a lack of precision and tailoring towards the needs of the specific facility. Indeed, less than half of our sample reported the use of tailored strategies. This finding has important implications for clinical practice because it shows that currently, there may exist a lack of consideration for the influence of ICU contextual variation on bundle adoption. It can be expected that each facility has unique structural, cultural, and clinical characteristics, each requiring equally unique implementation strategies to maximize ABCDEF adoption. End-users attempting to implement the ABCDEF bundle for the first time, or to increase ongoing adoption and sustainability, should consider an individualized approach to selecting implementation strategies. Individualization would be consistent with experts who recommend selecting strategies that target specific behaviors, rather than using an “it seemed like a good idea at the time” or non-individualized approach for strategy selection.31 One approach to identify organizational needs and achieve targeted implementation strategies would be to carry out institution-specific intervention mapping.32–34 Intervention mapping is a systematic process that is grounded in community-based participatory research methods and helps guide implementation teams with intervention development and implementation steps. Compared to non-targeted strategies, use of targeted implementation strategies shows early evidence of efficacy.35,36 The full benefits of a targeted approach, however, are still not fully defined, thus making them a priority area for future research.
Participants in this study had important insights regarding the perceived feasibility and perceived efficacy of the various implementation strategies. Importantly, at the individual sites, the relationship between feasibility and efficacy may not be aligned. These data were collected after the completion of the ABCDEF collaborative; ideally, facilities should gather this site-specific and intervention-specific data early after implementation. This knowledge could potentially avoid the waste of critical resources on ineffective and potentially costly strategies. Furthermore, implementation strategies without the support and feedback from frontline stakeholders are unlikely to achieve uptake and sustainability.37 Therefore, clinicians seeking to increase uptake and sustainability of the ABCDEF bundle should ensure that end-users of the intervention are active participants in the design, selection, and evaluation of implementation strategies. There remains a critical need to increase participatory approaches to ABCDEF bundle implementation research and evaluation to intentionally include the people and groups who are primarily responsible for everyday bundle delivery. This will help ensure that the methods and findings of such inquiry reflect the perspectives, cultures, priorities, or concerns of frontline clinicians and administrators.
The low use of strategies in the Change Infrastructure and Utilize Financial Strategies categories is consistent with other research related to implementation strategies outside the ICU setting. In their concept mapping exercise using implementation and clinical experts, Waltz et al. showed that experts viewed the strategies contained in these two categories as among those with the least importance and lowest feasibility.20 Of the few sites in this study that reported using strategies from these two categories (i.e., mandate change, change physical structure and equipment, start a dissemination organization, access new funding, fund and contract for the clinical intervention, and alter incentives/allowance structures), most were perceived as feasible consistent with the perceptions described by Waltz et al. Surprisingly, however, sites also described these same strategies to be not-at-all costly, with mean response <1. Further research of implementation strategies in the adult ICU should measure cost of strategies, particularly those with low use, such as those in the Financial and Infrastructure categories. Data showing consistently acceptable cost levels associated with these strategies may increase perceptions of feasibility, thereby increasing the overall use of these potentially beneficial implementation strategies.
Strengths and Limitations
The main strength of this study was the purposeful inclusion of perspectives from interprofessional ICU team members, end-users, from a variety of ICUs across the United States. Because the online survey was able to be saved and accessed at a time most convenient to participants and was relatively inexpensive to conduct, we were able to reach practicing ICU clinicians during the ongoing and stressful COVID 19 pandemic. This study was strengthened by our use of the ERIC taxonomy for implementation strategies19 and use of the categorization described by Waltz et al.20 This allowed us to follow reporting guidelines for implementation research and provide consistent operationalization and conceptualization of implementation strategies, preventing possible homonymy and synonymy of strategies found in research not using existing taxonomies.18
The survey was designed by implementation experts familiar with implementation strategies but completed by clinical expert end-users. These clinical expert end-users may be unfamiliar with identifying and/or selecting implementation strategies, resulting in their use of numerous that may have not been tailored to their site. This discrepancy may have contributed to greater subjectivity that accounts for the higher number of reported strategies used by our sample, when compared to similar studies using the ERIC taxonomy. Finally, we measured end-user perceptions of which implementation strategies were used during implementation efforts but did not directly measure those used during the process of implementation and practice change. This may account for the inflated number of reported strategies compared to other studies.
A major limitation of this study was low response rate, which may limit the generalizability of which strategies were used by ICU sites and the perceptions related to the implementation outcomes of helpfulness, acceptability, feasibility, and costliness. While electronic surveys in health research typically have response rates consistent with those seen in this study,38 our response rate may have been influenced because of the timing of delivery of this survey, which coincided with high ICU hospitalization rates due to the COVID-19 pandemic and associate rising clinician burnout or competing demands.39 To minimize this limitation, we extended the survey window, provided ongoing communication, and sent targeted emails to incomplete survey responses. Nevertheless, our survey collected diverse feedback from 19 ICUs across the United States and provides insight into the implementation efforts related to the ABCDEF bundle. Additionally, our decision to sample clinicians exclusively from sites with previous participation in the SCCM’s ICU Liberation Collaborative may limit the generalizability of findings. ICU clinicians who are unfamiliar with or lack experience in implementing the ABCDEF bundle may report using additional or differing implementation strategies. They may also describe diverging perceptions of the helpfulness, acceptability, feasibility, and costliness of strategies when compared to those described by this sample. A further limitation of this study is the length of the survey. Depending on use, participants were asked to respond to at least 73 questions, with a maximum of 365 questions, excluding demographics information and free-text responses. While pilot testing of the survey among members of the research team showed the maximum questions could be answered in 40–50 minutes, the length of the survey may have lowered site response rate.
Conclusion
This survey study of implementation strategies used by ICU clinicians in their delivery of the ABCDEF bundle provides valuable insight into the implementation process of this best practice, but underused, liberation pathway. Considering the positive dose-response relationship between bundle performance and patient health outcomes,4 low implementation may result in widespread loss of bundle-related health benefits. Our findings point to a possible over-reliance on accessible educational strategies that may not be the most effective at promoting behavior change towards adoption of this complex clinical intervention.40 Our findings also point to potentially beneficial and unused strategies, (i.e., strategies in the Change Infrastructure and Utilize Financial Strategies categories). We recommend that future research is done to examine the role of ICU context in ABCDEF bundle adoption; specifically, how adoption is influenced by the individual and collective values, beliefs, and perceptions of ICU clinicians. Also, further exploration is necessary to understand the acceptability, helpfulness, feasibility, and cost of implementation strategies used to increase adoption and sustainability of the ABCDEF bundle. The results of this study can be used in further implementation research to overcome the multi-level barriers that impede routine delivery of the ABCDEF bundle and help close this research-practice gap.
Supplementary Material
Highlights.
Intensive care units use a breadth of strategies when implementing the ABCDEF Bundle.
There may be an overreliance on readily available educational strategies.
End-users provide insight to bundle implementation needs, challenges, and success.
Acknowledgments:
We would like to acknowledge the invaluable contributions of the ICU Liberation Collaborative participants, faculty, and Society of Critical Care Medicine staff partners.
Funding:
Research reported in this publication was supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health [Grant R01HL14678-01]. Funding for the Society of Critical Care Medicine’s ICU Liberation Collaborative was provided by the Gordon and Betty Moore Foundation and the Society of Critical Care Medicine. Funding for REDCap was provided by The Ohio State University Center for Clinical and Translational Science grant support (National Center for Advancing Translational Sciences, Grant UL1TR002733).
Abbreviations List:
- ABCDEF bundle (ICU Liberation Bundle)
Assess, Prevent, and Manage Pain, Both Spontaneous Awakening Trials (SAT) and Spontaneous Breathing Trials (SBT), Choice of analgesia and sedation, Delirium: Assess, Prevent, and Manage, Early mobility and Exercise, and Family engagement and empowerment
- CFIR
The Consolidated Framework for Implementation Research
- COVID-19
coronavirus disease 2019
- CROSS
Checklist for Reporting of Survey Studies Guidelines
- ERIC
Expert Recommendations for Implementing Change
- ICU
Intensive Care Unit
- SCCM
Society of Critical Care Medicine
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of Interest: Dr. Balas is current Co-Chair of the Society of Critical Care Medicine’s PADIS guideline update and a member of the American Psychiatric Association Delirium Guideline Writing Group. She has also served as a consultant for Ceribell.
REFERENCES
- 1.Balas MC, Weinhouse GL, Denehy L, et al. Interpreting and Implementing the 2018 Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption Clinical Practice Guideline. Crit Care Med. 2018;46(9):1464–1470. doi: 10.1097/CCM.0000000000003307 [DOI] [PubMed] [Google Scholar]
- 2.Devlin JW, Skrobik Y, Gélinas C, et al. Clinical Practice Guidelines for the Prevention and Management of Pain, Agitation/Sedation, Delirium, Immobility, and Sleep Disruption in Adult Patients in the ICU. Crit Care Med. 2018;46(9):e825–e873. doi: 10.1097/CCM.0000000000003299 [DOI] [PubMed] [Google Scholar]
- 3.Barnes-Daly MA, Phillips G, Ely EW. Improving Hospital Survival and Reducing Brain Dysfunction at Seven California Community Hospitals: Implementing PAD Guidelines Via the ABCDEF Bundle in 6,064 Patients. Crit Care Med. 2017;45(2):171–178. doi: 10.1097/CCM.0000000000002149 [DOI] [PubMed] [Google Scholar]
- 4.Pun BT, Balas MC, Barnes-Daly MA, et al. Caring for Critically Ill Patients with the ABCDEF Bundle: Results of the ICU Liberation Collaborative in Over 15,000 Adults. Crit Care Med. 2019;47(1):3–14. doi: 10.1097/CCM.0000000000003482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morris PE, Goad A, Thompson C, et al. Early intensive care unit mobility therapy in the treatment of acute respiratory failure. Crit Care Med. 2008;36(8):2238–2243. doi: 10.1097/CCM.0b013e318180b90e [DOI] [PubMed] [Google Scholar]
- 6.Alaparthi GK, Gatty A, Samuel SR, Amaravadi SK. Effectiveness, Safety, and Barriers to Early Mobilization in the Intensive Care Unit. Crit Care Res Pract. 2020;2020:7840743. doi: 10.1155/2020/7840743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Castro-Avila AC, Serón P, Fan E, Gaete M, Mickan S. Effect of Early Rehabilitation during Intensive Care Unit Stay on Functional Status: Systematic Review and Meta-Analysis. PLoS One. 2015;10(7):e0130722. doi: 10.1371/journal.pone.0130722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tipping CJ, Harrold M, Holland A, Romero L, Nisbet T, Hodgson CL. The effects of active mobilisation and rehabilitation in ICU on mortality and function: a systematic review. Intensive Care Med. 2017;43(2):171–183. doi: 10.1007/s00134-016-4612-0 [DOI] [PubMed] [Google Scholar]
- 9.Schweickert WD, Pohlman MC, Pohlman AS, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet. 2009;373(9678):1874–1882. doi: 10.1016/S0140-6736(09)60658-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schaller SJ, Anstey M, Blobner M, et al. Early, goal-directed mobilisation in the surgical intensive care unit: a randomised controlled trial. Lancet. 2016;388(10052):1377–1388. doi: 10.1016/S0140-6736(16)31637-3 [DOI] [PubMed] [Google Scholar]
- 11.TEAM Study Investigators and the ANZICS Clinical Trials Group, Hodgson CL, Bailey M, et al. Early Active Mobilization during Mechanical Ventilation in the ICU. N Engl J Med. 2022;387(19):1747–1758. doi: 10.1056/NEJMoa2209083 [DOI] [PubMed] [Google Scholar]
- 12.Costa DK, White MR, Ginier E, et al. Identifying Barriers to Delivering the Awakening and Breathing Coordination, Delirium, and Early Exercise/Mobility Bundle to Minimize Adverse Outcomes for Mechanically Ventilated Patients: A Systematic Review. Chest. 2017;152(2):304–311. doi: 10.1016/j.chest.2017.03.054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dubb R, Nydahl P, Hermes C, et al. Barriers and Strategies for Early Mobilization of Patients in Intensive Care Units. Annals of the American Thoracic Society. 2016;13(5):724–730. doi: 10.1513/annalsats.201509-586cme [DOI] [PubMed] [Google Scholar]
- 14.Parry SM, Knight LD, Connolly B, et al. Factors influencing physical activity and rehabilitation in survivors of critical illness: a systematic review of quantitative and qualitative studies. Intensive Care Med. 2017;43(4):531–542. doi: 10.1007/s00134-017-4685-4 [DOI] [PubMed] [Google Scholar]
- 15.Balas MC, Tan A, Mion LC, et al. Factors Associated With Spontaneous Awakening Trial and Spontaneous Breathing Trial Performance in Critically Ill Adults: Analysis of a Multicenter, Nationwide, Cohort Study. Chest. January 2022. doi: 10.1016/j.chest.2022.01.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barr J, Ghaferi AA, Costa DK, et al. Organizational Characteristics Associated With ICU Liberation (ABCDEF) Bundle Implementation by Adult ICUs in Michigan. Crit Care Explor. 2020;2(8):e0169. doi: 10.1097/CCE.0000000000000169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liu K, Nakamura K, Katsukawa H, et al. ABCDEF Bundle and Supportive ICU Practices for Patients With Coronavirus Disease 2019 Infection: An International Point Prevalence Study. Crit Care Explor. 2021;3(3):e0353. doi: 10.1097/CCE.0000000000000353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Proctor EK, Powell BJ, McMillen JC. Implementation strategies: recommendations for specifying and reporting. Implement Sci. 2013;8:139. doi: 10.1186/1748-5908-8-139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Powell BJ, Waltz TJ, Chinman MJ, et al. A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implement Sci. 2015;10:21. doi: 10.1186/s13012-015-0209-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Waltz TJ, Powell BJ, Matthieu MM, et al. Use of concept mapping to characterize relationships among implementation strategies and assess their feasibility and importance: results from the Expert Recommendations for Implementing Change (ERIC) study. Implement Sci. 2015;10:109. doi: 10.1186/s13012-015-0295-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Stollings JL, Devlin JW, Lin JC, Pun BT, Byrum D, Barr J. Best Practices for Conducting Interprofessional Team Rounds to Facilitate Performance of the ICU Liberation (ABCDEF) Bundle. Crit Care Med. 2020;48(4):562–570. doi: 10.1097/CCM.0000000000004197 [DOI] [PubMed] [Google Scholar]
- 22.Devlin JW, O’Neal HR, Thomas C, et al. Strategies to Optimize ICU Liberation (A to F) Bundle Performance in Critically Ill Adults With Coronavirus Disease 2019. Critical Care Explorations. 2020;2(6):e0139. doi: 10.1097/cce.0000000000000139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barnes-Daly MA, Pun BT, Harmon LA, et al. Improving Health Care for Critically Ill Patients Using an Evidence-Based Collaborative Approach to ABCDEF Bundle Dissemination and Implementation. Worldviews Evid Based Nurs. 2018;15(3):206–216. doi: 10.1111/wvn.12290 [DOI] [PubMed] [Google Scholar]
- 24.Sharma A, Minh Duc NT, Luu Lam Thang T, et al. A Consensus-Based Checklist for Reporting of Survey Studies (CROSS). J Gen Intern Med. 2021;36(10):3179–3187. doi: 10.1007/s11606-021-06737-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ely EW. The ABCDEF Bundle: Science and Philosophy of How ICU Liberation Serves Patients and Families. Crit Care Med. 2017;45(2):321–330. doi: 10.1097/CCM.0000000000002175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50. doi: 10.1186/1748-5908-4-50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: Building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Perry CK, Damschroder LJ, Hemler JR, Woodson TT, Ono SS, Cohen DJ. Specifying and comparing implementation strategies across seven large implementation interventions: a practical application of theory. Implement Sci. 2019;14(1):32. doi: 10.1186/s13012-019-0876-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bunger AC, Powell BJ, Robertson HA, MacDowell H, Birken SA, Shea C. Tracking implementation strategies: a description of a practical approach and early findings. Health Res Policy Syst. 2017;15(1):15. doi: 10.1186/s12961-017-0175-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Powell BJ, Fernandez ME, Williams NJ, et al. Enhancing the Impact of Implementation Strategies in Healthcare: A Research Agenda. Front Public Health. 2019;7:3. doi: 10.3389/fpubh.2019.00003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fernandez ME, Ruiter RAC, Markham CM, Kok G. Intervention Mapping: Theory- and Evidence-Based Health Promotion Program Planning: Perspective and Examples. Front Public Health. 2019;7:209. doi: 10.3389/fpubh.2019.00209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fernandez ME, Ten Hoor GA, van Lieshout S, et al. Implementation Mapping: Using Intervention Mapping to Develop Implementation Strategies. Front Public Health. 2019;7:158. doi: 10.3389/fpubh.2019.00158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bartholomew LK, Parcel GS, Kok G. Intervention mapping: a process for developing theory- and evidence-based health education programs. Health Educ Behav. 1998;25(5):545–563. doi: 10.1177/109019819802500502 [DOI] [PubMed] [Google Scholar]
- 35.Handley MA, Gorukanti A, Cattamanchi A. Strategies for implementing implementation science: a methodological overview. Emerg Med J. 2016;33(9):660–664. doi: 10.1136/emermed-2015-205461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Goorts K, Dizon J, Milanese S. The effectiveness of implementation strategies for promoting evidence informed interventions in allied healthcare: a systematic review. BMC Health Serv Res. 2021;21(1):241. doi: 10.1186/s12913-021-06190-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Goodrich DE, Miake-Lye I, Braganza MZ, Wawrin N, Am K. Quality Enhancement Research Initiative. QUERI Roadmap for Implementation and Quality Improvement. United States Department of Veterans Affairs Veterans Health Administration Office of Research and Development Health Services Research and Development; 2020. https://www.queri.research.va.gov/tools/QUERI-Implementation-Roadmap-Guide.pdf. [Google Scholar]
- 38.Fincham JE. Response rates and responsiveness for surveys, standards, and the Journal. Am J Pharm Educ. 2008;72(2):43. doi: 10.5688/aj720243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gualano MR, Sinigaglia T, Lo Moro G, et al. The Burden of Burnout among Healthcare Professionals of Intensive Care Units and Emergency Departments during the COVID-19 Pandemic: A Systematic Review. Int J Environ Res Public Health. 2021;18(15). doi: 10.3390/ijerph18158172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bero LA, Grilli R, Grimshaw JM, Harvey E, Oxman AD, Thomson MA. Closing the gap between research and practice: an overview of systematic reviews of interventions to promote the implementation of research findings. The Cochrane Effective Practice and Organization of Care Review Group. BMJ. 1998;317(7156):465–468. doi: 10.1136/bmj.317.7156.465 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


