Abstract
OBJECTIVES:
Unexpected lucidity is a phenomenon of scientific, clinical, and psychological relevance to health professionals, to those who experience it, and their relatives. This paper describes qualitative methods used to develop an informant-based measure of lucidity episodes.
METHODS:
The approach was: refinement of the operationalization of the construct; review of seminal items, modification, and purification; and confirmation of the feasibility of reporting methodology. Modified focus groups were conducted with 20 staff and 10 family members using a web-based survey. Themes included: reaction when hearing the term; words that come to mind; description of and first reaction to referenced or observed “lucidity” events. Semi-structured cognitive interviews were conducted with 10 health professionals working with older adults with cognitive impairment. Data were extracted from Qualtrics or Microsoft 365 Word for analysis using NVivo.
RESULTS:
Conceptual issues, as well as issues regarding comprehension, interpretation, clarity, semantics, and standardization of definitions derived from an external advisory board, focus groups and cognitive interviews informed items’ modification, and resulted in the final lucidity measure.
CONCLUSIONS:
An obstacle to understanding the mechanisms and estimating the prevalence of lucid events among individuals with dementia and other neurological conditions is the scarcity of reliable and valid measures. The substantive and varied data gathered from multiple methods including the collaborative work of an External Advisory Board, modified focus groups with staff and family caregivers, and structured cognitive interviews with health professionals were central in creating the revised version of the lucidity measure.
Keywords: Dementia, Cognitive impairment, Lucidity, Qualitative methods, Measurement
1. Introduction
Unexpected lucidity is a phenomenon of scientific, clinical, and psychological relevance to health professionals, to those who experience it, and their relatives. Literature reviews have documented its manifestation across individuals suffering varied health conditions (Morris & Bulman, 2021), many with underlying cognitive impairment.
Unexpected lucidity has been described as brief periods of increased mental clarity and alertness, demonstrating augmented awareness of self and surroundings, and enhanced expression and communication, like that extant prior to the onset of cognitive impairment (Nahm, 2009; Nahm & Greyson, 2009; Nahm et al., 2011). These episodes have been reported to sometimes occur close to the end of life (Chiriboga-Oleszczak, 2017). Accordingly, the literature reflects references to paradoxical (Mashour et al., 2019; Peterson et al., 2021) as well as to terminal lucidity (Nahm, 2009; Nahm & Greyson, 2009; Nahm et al., 2011); the actual distinction between the two however, is a current subject of dialogue, needing further examination, and standardized definition (see Nahm, 2021; Peterson et al., 2022).
Because the overall goal of the present project is to examine this phenomenon granularly for augmented precision in measurement, and to develop a definition understood by front-line informants, inclusive nomenclature of “unexpected” (instead of paradoxical, or terminal) lucidity was used. This approach is consistent with suggestions (Gilmore-Bykovskyi, Griffin, Mueller, Parnia, and Kolanowski, 2023) for an inclusive, broad definition when characterizing lucidity events, with the goal of achieving clarity in the operationalization of the associated features and attributes to facilitate comparability across studies.
Broadly, lucidity episodes have been documented through anecdotal evidence, clinical narratives, and case histories (Nahm & Greyson, 2009; Nahm et al., 2011; Mashour et al., 2019; Bostanciklioğlu, 2021). However, the overall phenomenological scope of unexpected lucidity, including operational definitions requires further refinement (Bostanciklioğlu, 2021; Gilmore-Bykovskyi et al., 2021; Morris & Bulman, 2021; Peterson et al., 2022; Nahm, 2022a, 2022b; Gilmore-Bykovskyi et al., 2023). For instance, Nahm (2022a) calls for a conceptual reconsideration of terminal- and paradoxical lucidity, advocating for interdisciplinary approaches that integrate advances on dementia and end-of-life research. Additional, rigorous scientific study has been solicited and is ongoing (See RFA-AG-20–017, Lucidity in Dementia).
Lucidity is a complex phenomenon, and it is challenging to measure. One of the main obstacles to understanding the mechanisms and estimating the prevalence of lucid events among individuals with dementia and other neurological conditions is the scarcity of reliable and valid measures. This paper documents and describes qualitative methods used to develop a measure of lucidity episodes to be implemented with informants, in this case professional caregivers.
The importance of qualitative methods for measure development has been emphasized (Gordon et al., 2016; Keeley et al., 2016) particularly in the context of cross-cultural research and of assessment of constructs needing further refinement (Krause, 2006; Robinson et al., 2020). Conceptual measurement equivalence is key to maximizing the quality of quantitative survey items by discerning item intent and relevance as well as consistency of item interpretation, which ultimately affects the psychometric properties of the measure (Brod et al., 2009; Ramírez, et al., 2005). This article addresses this gap, providing a detailed description of the qualitative methodology for the development of a measure to capture the complex phenomenon of lucidity.
The purpose of this article is to contribute to knowledge of lucidity in long-term services and supports settings (LTSS) by documenting the development strategy for a new informant-based measure to describe episodes of lucidity using qualitative methodology. Individuals with dementia, neurological and other illnesses were targeted, and individual and episodic characteristics associated with events, suitable for reports by staff and family informants were identified.
2. Methods
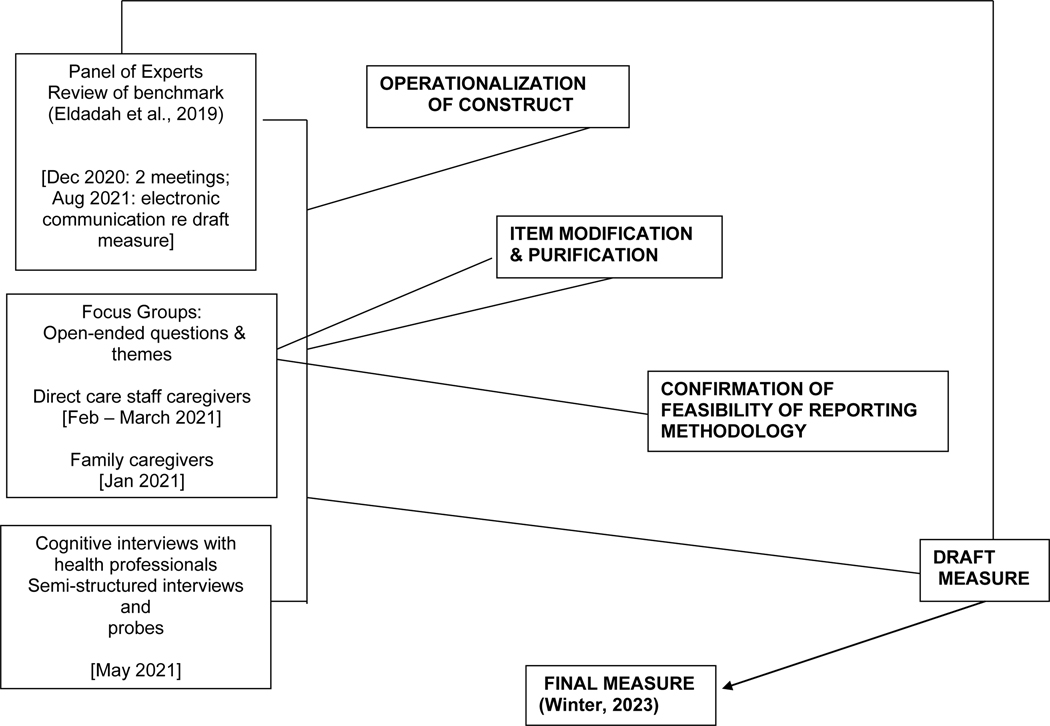
The sequential approach for the creation of lucidity items focused on three main tasks: 1) refinement of the operationalization of the construct; 2) review of seminal items used in prior pilot testing (see Teresi et al., 2023), item modification and purification; and 3) confirmation of the feasibility of the reporting methodology. These goals were achieved through formation of an interdisciplinary external advisory board; conduct of modified focus groups comprised of frontline health and direct providers in a long-term care institution, and family caregivers of cognitively impaired older adults; and cognitive interviews with health professionals. (See Figure 1 for depiction of the timeframe and the methods used in addressing the tasks.)
Figure 1:
Timeframe and methods used to address each task for lucidity measure development.
2.1. Participants
2.1.1. External Advisory Board (panel of experts (n=7))
Seven health professionals representing disciplines such as: clinical geriatrics, social gerontology, social work, geriatric nursing, and psychiatry were convened to review the items and provide general advice regarding the project. The external advisory board was comprised of three men and four women.
2.1.2. Modified Focus Groups
Staff caregivers: Twenty (90% female) frontline health and direct care providers currently employed in a long-term care facility participated in the web-based survey. The majority (11/20) of the staff caregivers were certified nurse assistants (CNA); four were licensed practical nurses (LPN), three registered nurses (RN), one social worker and one dietician. Flyers were posted and distributed throughout the participant institution to enhance recruitment. A $25.00 gift card was offered as a token of appreciation for the completion of the survey.
Family caregivers: Ten (90% female), self-identified family caregivers, seven of which were primary caregivers, completed the web-based survey questionnaire. Six (60%) were current caregivers for mothers, three (20%) were performing the caregiving role for their mothers until death. One was the caregiver for her father- and mother in-law, and one for her spouse. Six (60%) performed caregiving roles consistently from 2 to 5 years, 30% from 7 to 10 years, and one was a primary caregiver for 45 years. Word of mouth was used as the recruitment method. All individuals contacted agreed to participate in this project.
2.1.3. Cognitive Interviews with Health Professionals
Ten (90% female) health professionals with experience working with older adults with cognitive impairment: two MDs (internists), two LPNs, two clinical psychologists, two social workers and two CNAs completed cognitive interviews. The representation of the varied professions was purposely designed a priori. Word-of-mouth was used as the recruitment method.
2.2. Ethical Considerations
The study was approved by the primary institution’s IRB (PROTOCOL: 0120I/P142/01). Verbal informed consent was obtained from all participants. Participants were informed about the right to refuse to answer any question or stop the interview/web-based survey at any point. Interview data were not shared with other (staff or family) caregivers or any health professional.
2.3. Data Collection
2.3.1. Operationalization of the Lucidity Construct
The modified version of the NIA RFA-AG-20–016 derived definition of lucidity (see Eldadah et al., 2019), applied in the piloted questionnaire (see Teresi et al., 2023) was used as the benchmark for refined operationalization: “We define lucidity as unexpected episodes of spontaneous mental clarity such as the ability to communicate in persons who had seemingly lost such abilities. This could include return to a higher level of communication, even if for a brief period.”
To assure that all components of “lucidity” were measured systematically, a critical action was the operationalization of the construct. Two Zoom meetings with the external advisory board and project staff were held in early December 2020 to discuss and review the operational definition. The benchmark definition was dissected to identify: 1) phrases that could potentially create confusion and needed clarification, substitution, or deletion, 2) central features of lucidity missing in the definition extant. Each point was examined individually, the proponent of amendment(s) presented the rationale or argument, followed by group discussion. All final decisions, after discussion led by one of the principal investigators of the study, were made by consensus. Zoom meetings were recorded from which verbatim notes were derived. The Advisory Board was sent updated versions of the measures in August 2021, after the revision was completed. All members provided additional feedback via email.
2.3.2. Survey as Alternative to Focus Groups with Staff and Family Caregivers
The originally proposed use of in-person focus groups comprised of frontline health and direct care providers in long-term geriatric care and of family caregivers was abandoned due to social distancing guidelines and contact restrictions amid the COVID-19 pandemic (see Eigege et al., 2022; Vindrola-Padros et al., 2020). Seeking to minimize in-person contact, and weighing the resources needed to transition from in-person to online focus groups, an asynchronous individualized, (rather than group) online distribution platform application was considered. Recommendations for capitalizing on online panels for research (Miller et al., 2020) and previous experience using the platform informed the decision to use Qualtrics for data collection over other available options, e.g., RedCAP.
A sequentially displayed, long-response form with 20 primary questions about lucidity, demographic questions about gender identity, sex and professional occupation was developed. Each non-demographic question had an option to refuse an answer; however, if this option was selected, survey logic displayed a secondary question asking to specify a reason for refusal. The rationale was to obtain further insight into item quality, e.g., the refusal was a result of an inability to understand the questions, or to articulate a response based on the complexity of or comfort with the question. This information was instructive for item adaptation.
Surveys were embedded with a unique tracking code for each respondent which allowed for anonymity of response, ensured completion of the survey, and prevented survey sharing. Respondents entered the unique code to access the survey, and each code was programmed to a unique URL that allowed multiple access to a personalized survey. Respondents were given unlimited privilege to close and reopen the survey from their last completed response within a two-week period to accommodate their work schedules and any unanticipated interruptions that may prevent completion within a single sitting. The tracking codes were used to validate participation when distributing the advertised compensation for participation (for staff caregivers). Completed responses triggered automatic emails to the research team staff with final data reports that were available immediately upon completion. Data were extracted from Qualtrics to Microsoft Excel for analysis using NVivo. Survey metadata, including start and end date and time, total time required for completion, and embedded tracking data were included in each final response.
A telephone interview was offered as an alternative data collection format to both staff and family caregivers. Two family members and eight staff caregivers chose this option, and one was conducted as an in-person interview. All data were entered into Qualtrics regardless of interview modality.
The content of the themes originally developed for application during the focus groups was adapted into open-ended questions. This format allowed participants to answer in their own words by typing into a text box. Of 23 total questions, 17 were open-ended, free text. Sample themes were: a) immediate reaction when hearing the term lucidity; b) three words that come to mind when hearing or thinking of lucidity; c) familiarity with lucidity; d) description of referenced or observed “lucidity” event; e) first reaction when “lucidity” event was observed; f) thoughts and/or feelings that come to mind when thinking about the event(s); g) similarities or common elements between observed events (if any).
2.3.3. Cognitive Interviews with Health Professionals
Semi-structured, in-depth cognitive interviews utilizing concurrent probes were conducted over the telephone. Sample questions were: “Please tell me, based on the definition (provided), the main elements of a lucid event. I will read the definition again”; “There are different circumstances that might occur together with an observed lucidity event, for instance, a medical event. What would you consider a medical event in this context?”; “I am going to read you another list of behaviors or form of expressions that a person with dementia may show during a lucid event, and I would like you to give me examples of how that would look, for instance “agitated”: How would you know that a person is agitated”. Following each structured question specific probes (e.g., Why is that?; Can you give me an example?; Can you explain your answer?) were implemented as needed to obtain clarity, specificity, and a deeper insight into the answers. Verbatim responses were entered into a Microsoft 365 Wor document by the interviewer. Material was transferred to NVivo for analysis.
3. Data Analysis
A thematic, summative approach (Roberts & Dowell, 2019) was applied for analysis of verbatim responses provided by participants in all group categories, i.e., staff caregivers, family caregivers, and health professionals. A sequential method for review was used with two main foci, i.e., solidification of the operational definition of the main construct (“lucidity”), and the purification of items. An initial examination of the data was conducted to identify any issues with respect to comprehension, clarity, and consistency in the operationalization of lucidity. Responses reflecting inconsistencies from the provided definition were flagged and coded. Similarly, any indication regarding difficulties with comprehension and/or clarity of the items impacting the interpretation of their original intent was flagged and coded. A subsequent more selective and comprehensive review was then conducted to explore remediation of the identified problems with the operational definition of lucidity, and with the items’ interpretation, respectively. The measurement development team identified and discussed patterns of underlying problems and by examining the putative sources of those problems, by consensus, decided on solutions and modifications for improvement. The information obtained from the implemented structured and spontaneous probes was instrumental in elucidating the putative cause of such underlying problems. Comments provided by the external advisory board regarding the operational definition of lucidity were taken into consideration and incorporated. Trustworthiness was built via triangulation across the multiple data sources, where two investigators consistently reviewed and discussed the codes throughout the data processing and analysis.
4. Results
4.1. Operationalization of the Lucidity Construct
The External Advisory Board raised issues regarding the descriptive clarity, breadth, and scope in conceptualizing lucidity reflected in the definition. The inclusion of “spontaneous” was questioned because it may suggest that the patient initiates communication; it was thought that “spontaneity” was not a core element or requirement in the definition. The final decision made was to remove it. The same consideration was given regarding the inclusion of verbal communication (talking ability was not present before the event). Because of the limited empirical evidence in this early-stage research it was recommended to take a broad, more inclusive approach, incorporating nonverbal (behavior) communication as well, e.g., facial expression, gestures, smiles, behaviors that show recognition, when there was none before. Similarly, after deciding to keep “unexpected” as part of the definition, the importance of capturing the context, and antecedents of the event, and whether there were stimuli, was stressed. The potential subjective interpretation of what might constitute “relevant communication” and “coherent speech” from caregivers was also highlighted. Thus, the inclusion of definitions and examples of terms was suggested.
The terms included in the definition such as “unexpected episodes of mental clarity”; “meaningful communication”; and “coherent speech” were examined further through focus groups and cognitive interviews. Responses reflected the need for clarification, especially by simplifying wording and providing examples. After considering the applicability of all suggestions, the measurement development team and external advisory board developed a consensus definition:
“We define lucidity events as unexpected episodes of mental clarity in persons who had apparently lost such abilities, for example ability to communicate verbally or non-verbally or do things. This could include return to a higher level of communication or functioning (behavior), even if for a brief period. In other words, individuals who have lost abilities to communicate (verbally or non-verbally) or to do certain things, can return to having brief periods of mental clarity in which they are able to communicate and do movements or activities previously lost. These incidents are called lucid events.”
Additionally, a video-clip showing brief examples of lucidity events in individuals with traumatic brain disorder and Alzheimer’s disease was integrated as a visual aid to the written (verbal) operational definition, to augment conceptual comprehension.
4.2. Review of Seminal Items (see Teresi et al., 2023), Item Modification, and Item Purification
4.2.1. Recommendations from the External Advisory Board
Conceptual issues with implications for item content and protocol development were raised by the External Advisory Board, for example, how to capture the “not reversable” feature of lucidity. The solution suggested was to collect more granular information about the lucid event by including a list of specific behaviors that may have occurred during the event, similar to the Cohen Mansfield Agitation Index (Cohen-Mansfield, 1986; Cohen-Mansfield & Billig, 1986; Finkel et al., 1992; Kupeli et al., 2018). An additional recommendation was to ask the interviewee to qualify and describe the change in the resident (patient) during their lucid event regarding memory, ability to speak with others, ability to communicate non-verbally, and ability to do things like help with their care. Similarly, it was suggested that the length of baseline (non-lucid) state be considered and to add items related to function before and after the lucid event, e.g., ADL, behaviors (data from the Minimum Data Set) (Centers for Medicare & Medicaid Services, 2019). Noteworthy were suggestions about including exclusion criteria to the protocol, i.e., what is not lucidity, for example, resolution of delirium. It was suggested that the Confusion Assessment Method (CAM; Inouye, 2003; Inouye et al., 2014) be included. Additionally, it was suggested that changes due to adjustments in medications, i.e., additions/reductions, resolution of infections and medical events be measured by obtaining lists of medications, infection history, and events from medical records and/or the Minimum Data Set (Centers for Medicare & Medicaid Services, 2019), pre, during, and post event. Although sleep deprivation was also suggested as a potential exclusion criterion, collection of such data would not be feasible. Additionally, obtaining the caregiver perspective and emotional response to the lucid event was strongly recommended, given that these events tend to have an impact on caregivers.
4.2.2. Recommendations from the Results of Focus Groups and Cognitive Interviews
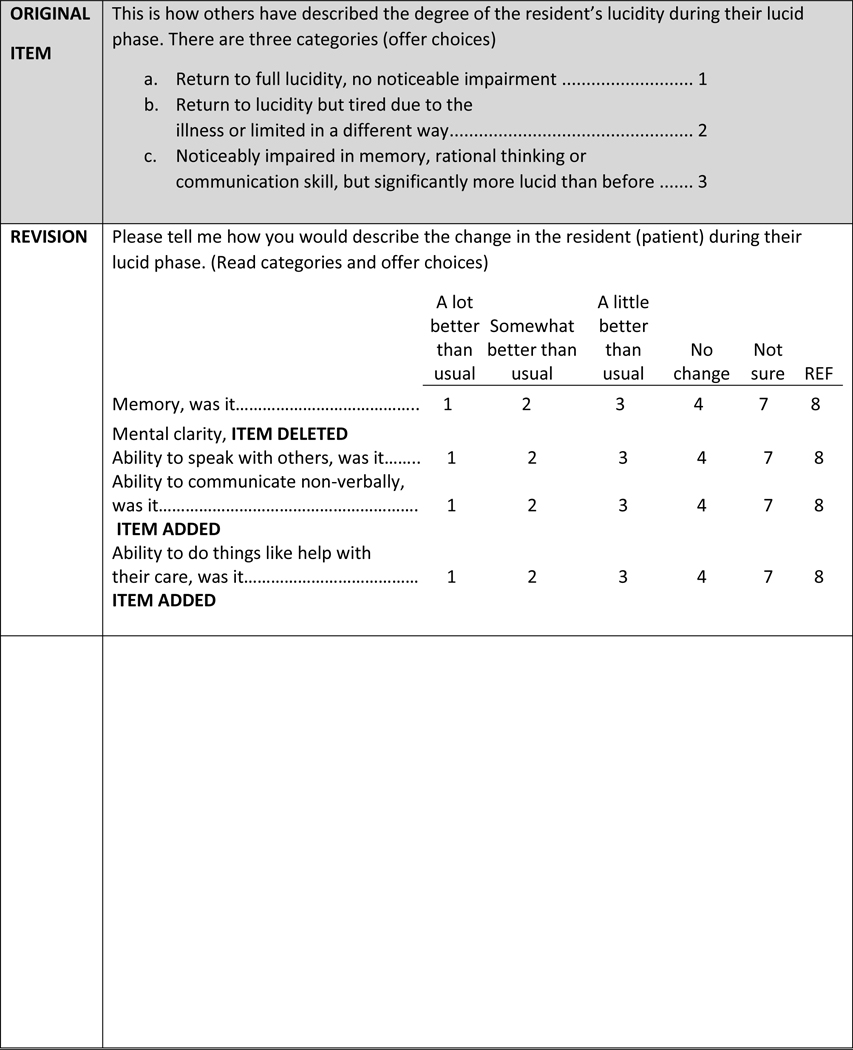
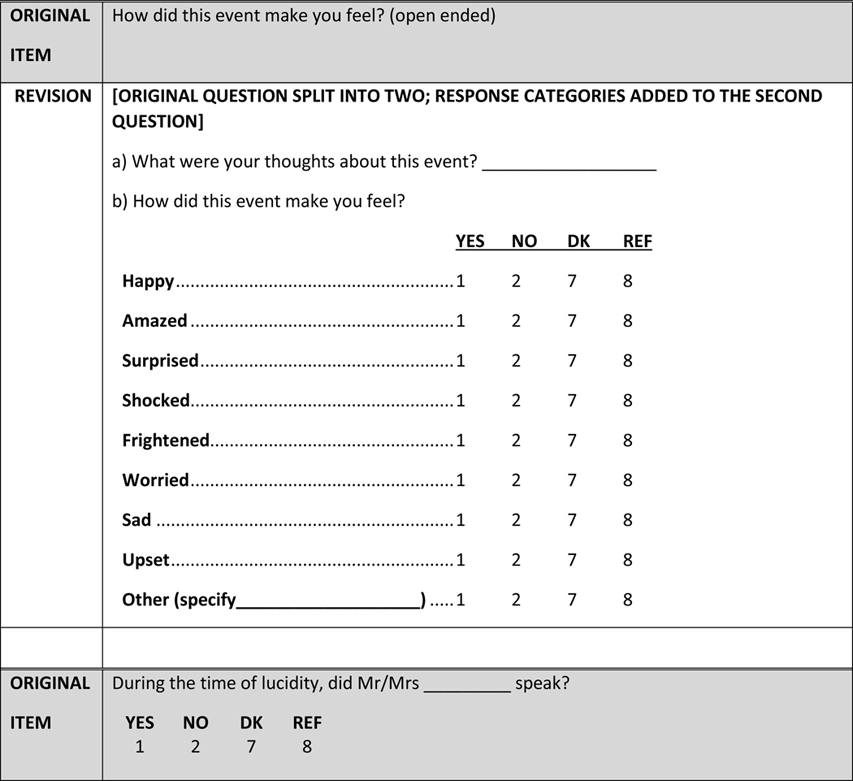
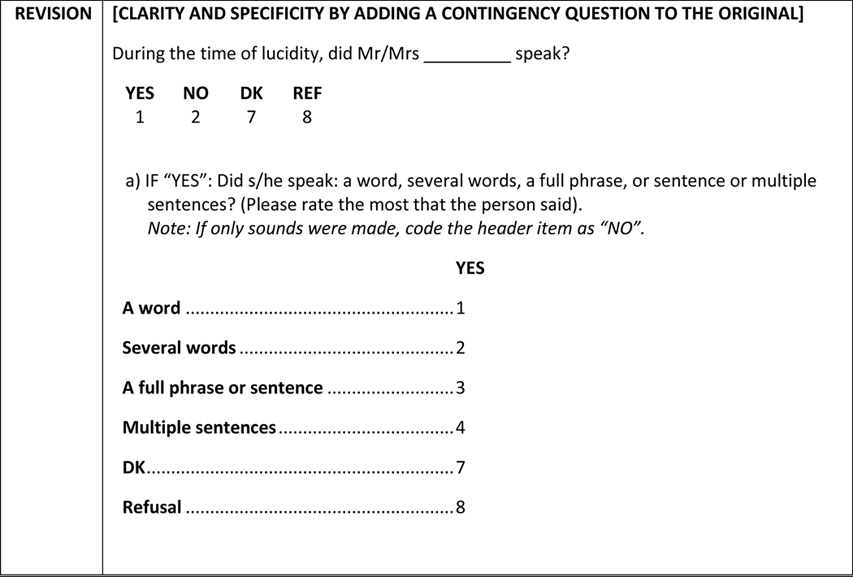
Complementary and supplemental suggestions for item modification were derived from the focus groups with staff and family caregivers, and from the cognitive interviews with health professionals. The application of a summative approach resulted in the following revisions to the measure: a) addition of items (contingent; segregating/splitting items into several) to augment comprehension, and to capture more granular aspects of the lucid event; b) revision of wording, expansion/abridgment and/or substitution of response categories/scales (e.g., from dichotomous (Yes/No) to nominal or ordinal scale); c) semantic modifications of items, i.e., rewording, use of simplified language to account for different levels of literacy, use of synonyms reflecting colloquial terms (e.g., “visit from a religious leader” instead of “clergy visit”); d) insertion of examples to clarify terms (e.g., “medical event (e.g., stroke, high blood pressure)”; (“medical treatment, e.g., procedure/ surgery”)); e) operationalization or definition of terms or concepts (e.g., providing a range of hours for each part of the day such as 6–11AM for “morning” and 11AM-2PM for “midday”); defining “repetitive questioning” “(asking the same thing over and over)”; f) substitution of open-ended questions with close ended questions with response categories. (See Table 1).
Table 1.
Examples of item modification after focus groups (survey) and cognitive interviews
|
|
|
The final modified version is a staff informant interview which includes questions related to resident characteristics, and to the lucidity event. The resident characteristics set of questions are focused on the specific resident and include staff reports of cognitive function, activities of daily living and mobility, behaviors, affect, communication, and medical conditions. Items related to delirium were added as were items related to the lucidity event including duration, location, occasion, presence of others, and triggering coincident situations. Additionally, a set of questions related to the staff informant include demographics, work-related experience, and reaction to and impact of the event (e.g., surprised, sad, worried).
The measure was formatted to be administered as a computer-assisted personal interview. One version of the developed questionnaire relates to persons who are still living and under the care of the informant (279 items including 202 close-ended items); a second version is used to describe persons who are no longer living or are no longer under the care of the respondent as well as information about the respondent and the LTSS facility (233 items including 202 close-ended items).
4.3. Confirmation of the Feasibility of Reporting Methodology
Although staff informant interviews are an established method to gather resident-related data in LTSS settings (see Lim et al., 2020; McCusker et al., 2011), a goal of the study was to assess whether it was feasible to obtain reports about lucid events, with a detailed, granular focus. The modified focus groups were instrumental in assessing the face validity of the measure. Nursing staff showed some degree of familiarity and experience with the concept of lucidity and were able to relate and provide witnessed examples of events.
5. Discussion
The present study extends existing work in the examination of lucid events in LTSS by providing a rich source of primary qualitative data with detailed information for measure development from different sources. To our knowledge, this is the first comprehensive qualitative measurement study of lucidity. The substantive and varied data gathered from the multiple methods and participants, including the collaborative work of an External Advisory Board, modified focus groups with staff and family caregivers, and structured cognitive interviews with health professionals were central in creating the revised version of the lucidity measure. These methodological approaches provided insight and feedback, key for item modification, enhancement, and addition. Besides being instrumental in highlighting problematic items, the combined methodology facilitated informed decisions for item enhancement after the nature of problem(s) were revealed. An additional benefit of the combined qualitative methodology for item development is the opportunity for an increased validation of the results via triangulation, and the examination of the fidelity with respect to the interpretation of key constructs and terminologies.
The range of adjustments from basic (e.g., response format) to more substantive (e.g., item wording and phraseology to characterize language agreeable to participants) are reflected in the finalized version of the measure. Examples of better-quality items (from original to modified) were presented to illustrate the way in which the applied methods enabled item improvement. Of particular interest was the divergent interpretation of terms that might be considered customary or familiar. For example, the reported range of hours that constituted the different times of the day: morning, afternoon, evening, and night showed negligeable concordance. This finding, although potentially considered trivial, in the context of ascertaining commonality in the time of occurrence of lucid events, such items, void of standardization will introduce error in the assessment, with detrimental implications for an enhanced understanding of the lucidity phenomenon. A similar example was what was considered “speaking” during an episode of lucidity. Responses varied widely from emission of just a sound (e.g., moaning) or even gestures, to using incoherent words, or a full sentence with or without contextual relevance to real time or stimuli. Lucidity pertains to the temporary recovery of the capacity for contextual interactions with individuals and/or the real environment. Thus, the standardization of what would be considered “speaking” during a lucidity episode was deemed necessary.
Like any other measure development (or adaptation) effort, the exercise presented in this manuscript does not suffice. Additional steps using quantitative methodologies (in which classical and modern psychometric analyses, including exploratory and confirmatory factor analyses and item response theory methods) are warranted to complement and supplement the end-product of qualitative methods, and to provide an adequate examination of measure performance (see Teresi, 2006). One of the major obstacles to understanding the features and attributes of lucidity and estimating the prevalence of lucid events in dementia is the scarcity of reliable and valid measures. Thus, this paper represents a step forward in this field.
5.1. Limitations
Arguably, findings drawn by the exclusive use of qualitative methods do not provide the opportunity for probabilistic generalizability. The main objective of this effort, however, was to provide in-depth explanations and meanings to terms and domains for item modification and development. Because participants were recruited via word of mouth, the sample may not be representative of the pool of potential respondents. Although a sample of convenience, the inclusion of varied health professionals for cognitive interviews was intentional to expand and optimize a broader perspective. The modification (due to COVID-19 related social interactions guidelines) of the originally proposed focus groups with caregivers to individual on-line surveys also presents a potential limitation. The structure of a focus group provides the opportunity for interactive discussion and immediate feedback which as a result, might have produced a more enriched and comprehensive set of answers. Despite these limitations, the application of the different types of qualitative methods with a cross-section of caregivers (staff and family) and of health professionals afforded triangulation of answers for item adjustments. Noteworthy is that these groups of participants are potential front-line observers with the highest likelihood of providing informed insights into the details and characteristics of the lucidity phenomenon.
Acknowledgments
Parts of this manuscript were presented at the Gerontological Society of America Annual Scientific Meeting, November 10, 2021, online.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Institute on Aging [grant number 1R21AG069748–01]; this work was also supported in part by the National Institute on Aging [grant numbers 1P30AG059303, 1P30AG028741].
Footnotes
Declaration of Conflicting Interest
The Authors declare that there is no conflict of interest.
Data Availability Statement
The node analyses used for the development of the manuscript are available from the corresponding author upon request.
References
- Bostanciklioğlu M (2021). Unexpected awakenings in severe dementia from case reports to laboratory. Alzheimers & Dementia, 17(1), 125–136. 10.1002/alz.12162 [DOI] [PubMed] [Google Scholar]
- Brod M, Tesler LE, & Christensen TL (2009). Qualitative research and content validity: developing best practices based on science and experience. Quality of Life Research, 18, 1263–1278. 10.1007/s11136-009-9540-9 [DOI] [PubMed] [Google Scholar]
- Centers for Medicare & Medicaid Services. MDS 3.0 RAI Manual. (2019). Minimum Data Set (MDS) 3.0 Resident Assessment Instrument (RAI) Manual | CMS [Google Scholar]
- Chiriboga-Oleszczak BA (2017). Terminal lucidity. Current Problems in Psychiatry, 18(1), 34–46. 10.1515/cpp-2017-0003 [DOI] [Google Scholar]
- Cohen-Mansfield J. (1986). Agitated behaviors in the elderly II. Preliminary results in the cognitively deteriorated. Journal of American Geriatric Society, 34, 722–727. 10.1111/j.1532-5415.1986.tb04303.x [DOI] [PubMed] [Google Scholar]
- Cohen-Mansfield J, & Billig N. (1986). Agitated behaviors in the elderly I. A conceptual review. Journal of American Geriatric Society, 34, 711–721. 10.1111/j.1532-5415.1986.tb04302.x [DOI] [PubMed] [Google Scholar]
- Eigege CY, Daundasekara SS, Gomez ML, Walton QL, & Hernandez DC (2022). Conducting research six feet apart: The feasibility of transitioning qualitative research to meet the emerging research needs during a pandemic. International Journal of Qualitative Methods, 21, 1–12. 10.1177/16094069211069442 [DOI] [Google Scholar]
- Eldadah BA, Fazio EM, & McLinden KA (2019). Lucidity in dementia: A perspective from the NIA. Alzheimers & Dementia, 15(8), 1104–1106. 10.1016/j.jalz.2019.06.3915 [DOI] [PubMed] [Google Scholar]
- Finkel SI, Lyons JS, & Anderson RL (1992). Reliability and validity of the Cohen-Mansfield Agitation Inventory in institutionalized elderly. International Journal of Geriatric Psychiatry, 7, 487–490. 10.1002/gps.930070706 [DOI] [Google Scholar]
- Gilmore-Bykovskyi A, Block L, Benson C, & Griffin JM (2021). The importance of conceptualizing and defining episodes of lucidity. Journal of Gerontological Nursing, 47(4), 5. 10.3928/00989134-20210326-01 [DOI] [PubMed] [Google Scholar]
- Gilmore-Bykovskyi A, Griffin JM, Mueller KD, Parnia S, & Kolanowski A. (2023). Toward harmonization of strategies for investigating lucidity in AD/ADRD: A preliminary research framework. Alzheimer’s and Dementia, 19(1), 343–352. 10.1002/alz.12709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon MF, Lenderking WR, Duhig A, Chandler J, Lundy JJ, Miller DS, Piault-Louis E, Doody RS, Galasko D, Gauthier S, & Frank L. (2016). Development of a patient-reported outcome instrument to assess complex activities of daily living and interpersonal functioning in persons with mild cognitive impairment: The qualitative research phase. Alzheimers & Dementia, 12(1), 75–84. 10.1016/j.jalz.2015.04.008 [DOI] [PubMed] [Google Scholar]
- Inouye SK (2003). The Confusion Assessment Method (CAM): Training Manual and Coding Guide. New Haven: Yale University School of Medicine. [Google Scholar]
- Inouye SK, Kosar CM, Tommet D, Schmitt EM, Puelle MR, Saczynski JS, Marcantonio ER, & Jones RN (2014). The CAM-S: Development and validation of a new scoring system for delirium severity in 2 cohorts. Annals of Internal Medicine, 160, 526–533. 10.7326/M13-1927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keeley T, Williamson P, Callery P, Jones LL, Mathers J, Jones J, Young B, & Calver M. (2016). The use of qualitative methods to inform Delphi surveys in core outcome set development. Trials, 17, 230. 10.1186/s13063-016-1356-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krause N. (2006). The use of qualitative methods to improve quantitative measures of health-related constructs. Medical Care, 44(11), S34–S38. 10.1097/01.mlr.0000245429.98384.23. [DOI] [PubMed] [Google Scholar]
- Kupeli N, Vickerstaff V, White N, Lord K, Scott S, Jones L, & Sampson EL (2018). Psychometric evaluation of the Cohen-Mansfield Agitation Inventory in an acute general hospital setting. International Journal of Geriatric Psychiatry, 33(1), e158–e165. 10.1002/gps.4741 [DOI] [PubMed] [Google Scholar]
- Lim C-Y, Park JY, Kim DY, Yoo KD, Kim HJ, Kim Y, & Shin S,J (2020). Terminal lucidity in the teaching hospital setting. Death Studies, 44, 285–291. 10.1080/07481187.2018.1541943 [DOI] [PubMed] [Google Scholar]
- Macleod AS (2009). Lightening up before death. Palliative & Supportive Care, 7(4), 513–516. 10.1017/S1478951509990526 [DOI] [PubMed] [Google Scholar]
- Mashour GA, Frank L, Batthyany A, Kolanowski AM, Nahm M, Schulman-Green D, Greysin B, Pakhomov S, Kalawish J, & Shah RC (2019). Paradoxical lucidity: A potential paradigm shift for the neurobiology and treatment of severe dementias. Alzheimer’s & Dementia, 15(8), 1107–1114. 10.1016/j.jalz.2019.04.002 [DOI] [PubMed] [Google Scholar]
- McCusker J, Cole MG, Voyer P, Monette J, Champoux N, Ciampi A, Vu M, & Belzile E. (2011). Prevalence and incidence of delirium in long-term care. International Journal of Geriatric Psychiatry, 26, 1152–1161. 10.1002/gps.2654 [DOI] [PubMed] [Google Scholar]
- Miller CA, Guidry JPD, Dahman B, & Thomson MD (2020). A tale of two diverse qualtrics samples: Information for online survey researchers. Cancer Epidemiology, Biomarkers & Prevention, 29(4), 731–735. 10.1158/1055-9965.EPI-19-0846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris P, & Bulman D. (2021). Reply: Importance of conceptualizing and defining episodes of lucidity. Journal of Gerontological Nursing, 47(4). 10.3928/00989134-20210309-01. Published Online: April 01, 2021. [DOI] [PubMed] [Google Scholar]
- Nahm M. (2022a). The Importance of the Exceptional in Tackling Riddles of Consciousness and Unusual Episodes of Lucidity. Journal of Anomalous Experience and Cognition, 2(2), 264–296. 10.31156/jaex.24028 [DOI] [Google Scholar]
- Nahm M. (2022b). Terminal lucidity vs. paradoxical lucidity: a terminological clarification. Alzheimer’s & Dementia, 1–2. 10.1002/alz.12574 Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- Nahm M. (2009). Terminal lucidity in people with mental illness and other mental disability: An overview and implications for possible explanatory models. Journal of Near-Death Studies, 28(2):87–106. [Google Scholar]
- Nahm M, & Greyson B. (2009). Terminal lucidity in patients with chronic schizophrenia and dementia: A survey of the literature. Journal of Nervous and Mental Disease, 197(12), 942–944. 10.1097/NMD.0b013e3181c22583 [DOI] [PubMed] [Google Scholar]
- Nahm M, Greyson B, Kelly E, & Harroldsson E. (2012). Terminal lucidity: A review and a case collection. Archives of Gerontology and Geriatrics, 55, 138–142. 10.1016/j.archger.2011.06.031 [DOI] [PubMed] [Google Scholar]
- Peterson A, Clapp J, Harkins K, Kleid M, Largent EA, Stites SD, & Karlawish J. (2022). Is there a difference between terminal lucidity and paradoxical lucidity? Alzheimer’s & Dementia, 1–2. 10.1002/alz.12579 Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson A, Clapp J, Largent EA, Harkins K, Stites SD, & Karlawish J. (2021). What is paradoxical lucidity? The answer begins with its definition. Alzheimer’s & Dementia, 1–9. 10.1002/alz.12424. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramírez M, Ford ME, Stewart AL, & Teresi J,A (2005). Measurement issues in health disparities research. Health Services Research, 40(5 Pt 2), 1640–1657. 10.1111/j.1475-6773.2005.00450.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- RFA-AG-20–017, Lucidity in Dementia (R21/R33 Clinical Trial Optional)
- Roberts K, Dowell A, & Nie JB (2019). Attempting rigour and replicability in thematic analysis of qualitative research data; a case study of codebook development. BMC Medical Research Methodology, 19(1), 66. 10.1186/s12874-019-0707-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson C,A, Bottorff JL, Pesut B, & Zerr J. (2020). Development and implementation of the Family Caregiver Decision Guide. Qualitative Health Research, 30(2), 303–313. 10.1177/1049732319887166. Epub 2019 Nov 19. PMID: 31744378. [DOI] [PubMed] [Google Scholar]
- Teresi JA (2006). Different approaches to differential item functioning in health applications. Medical Care, 44(11), S152–S170. 10.1097/01.mlr.0000245142.74628.ab [DOI] [PubMed] [Google Scholar]
- Teresi J,A, Ramirez M, Ellis J, Tan A, Capezuti E, Silver S, Boratgis G, Gonzalez-Lopez P, Devanand DP, & Luchsinger JA (2023). Reports about paradoxical lucidity from health care professionals: A pilot study. Journal of Gerontological Nursing, 49(1),18–26. doi: 10.3928/00989134-20221206-03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vindrola-Padros C, Chisnall G, Cooper S, Dowrick A, Djellouli1 N, Symmons SM, Singleton G, Vanderslott S, Vera N, & Johnson GA (2020). Carrying out rapid qualitative research during a pandemic: emerging lessons from COVID-19. Qualitative Health Research, 30(14):2192–2204. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The node analyses used for the development of the manuscript are available from the corresponding author upon request.