STRUCTURED ABSTRACT
Background:
Older adults, particularly those with Alzheimer’s Disease and Alzheimer’s Disease Related Dementias (AD/ADRD), have high rates of emergency department (ED) visits and are at risk for poor outcomes. How best to measure quality of care for this population has been debated. Healthy Days at Home (HDAH) is a broad outcome measure reflecting mortality and time spent in facility-based healthcare settings vs. home. We examined trends in 30-day HDAH for Medicare beneficiaries after visiting the ED and compared trends by AD/ADRD status.
Methods:
We identified all ED visits among a national 20% sample of Medicare beneficiaries ages 68 and older from 2012–2018. For each visit, we calculated 30-day HDAH by subtracting mortality days and days spent in facility-based healthcare settings within 30 days of an ED visit. We calculated adjusted rates of HDAH using linear regression, accounting for hospital random effects, visit diagnosis, and patient characteristics. We compared rates of HDAH among beneficiaries with and without AD/ADRD, including accounting for nursing home residency status.
Results:
We found fewer adjusted 30-day HDAH after ED visits among patients with AD/ADRD compared to those without AD/ADRD (21.6 vs. 23.0). This difference was driven by a greater number of mortality days, SNF days, and, to a lesser degree, hospital observation days, ED visits, and long-term hospital days. From 2012–8, individuals living with AD/ADRD had fewer HDAH in each year but a greater mean annual increase over time (p<.001 for the interaction between year and AD/ADRD status). Being a nursing home resident was associated with fewer adjusted 30-day HDAH for beneficiaries with and without AD/ADRD.
Conclusions:
Beneficiaries with AD/ADRD had fewer HDAH following an ED visit but saw moderately greater increases in HDAH over time compared to those without AD/ADRD. This trend was visit driven by declining mortality and utilization of inpatient and post-acute care.
Keywords: Emergency medicine, Alzheimer’s disease, dementia, Medicare, geriatrics
INTRODUCTION
Older adults have particularly high rates of emergency department (ED) utilization, as they disproportionately use the ED for acute unscheduled care.1,2 ED visits are frequently a sentinel event in this population, signaling a serious medical condition and carrying an inherent risk of adverse outcomes, such as delirium and functional decline.3–5 Individuals living with Alzheimer’s Disease and Alzheimer’s Disease Related Dementias (AD/ADRD) are especially vulnerable to decline associated with an acute illness.6 Thus, high-quality emergency care for this population is of paramount importance and requires a timely and accurate diagnosis, appropriate treatment, risk-stratification and selection of the ideal site for ongoing care. The disposition decision, i.e. whether to admit or discharge a patient, is a particularly important one, with implications for patient outcomes7 and healthcare costs.8,9 For the older adult, both admission and discharge carry potential risks, and the margin of error is likely smaller for patients with chronic conditions and limited physiologic reserve, such as those with AD/ADRD. Given the aging of the population and the rising prevalence of dementia in the United States,10 a greater understanding of the broader quality of emergency care for older adults, particularly those with AD/ADRD, is needed.
How best to measure the quality of acute care, including emergency care, has been the subject of substantial debate. Mortality is an objective, important measure but captures only the most severe harm and may miss other aspects of quality. Utilization measures such as readmissions or days spent in acute care have raised concerns about incentivizing harmful rationing of care.11 Healthy Days at Home (HDAH) is a measure developed in conjunction with the Medicare Payment Advisory Commission that broadly captures quality by accounting for both mortality and time spent in facility-based healthcare settings.12 Yet, data on HDAH after an ED visit is lacking and evidence is needed on how performance has changed over time, particularly for the most vulnerable patients, including those with AD/ADRD. Additionally, individuals with AD/ADRD have higher rates of long-term care utilization13 and is it unknown the degree to which nursing home (NH) residency status is associated with emergency care outcomes.
We used comprehensive claims among a national sample of Medicare beneficiaries ages 68 and older from 2012–2018 to address the following key questions. First, how does HDAH and its components vary among older adults within 30 days of an ED visit, and has there been an increase in HDAH over time? Second, to what degree is having an AD/ADRD diagnosis associated with HDAH within 30 days of an ED visit, and have adults with AD/ADRD and those without seen similar trends over time? Finally, to what degree is the association between AD/ADRD status and 30-day HDAH consistent between NH residents versus community-dwelling individuals?
METHODS
Beneficiary Characteristics
We identified a 20% random sample of fee-for-service Medicare beneficiaries ages 68 and older continuously enrolled in Medicare Parts A and B for the year (Supplemental Methods S1). We chose age 68 for the minimum age (rather than 65) because the AD/ADRD variable uses a 3-year look-back period to identify an AD/ADRD diagnosis. We obtained the following characteristics from the Master Beneficiary Summary File: age, sex, race, and Medicaid eligibility (defined by at least one month of Medicaid eligibility) and death date (if applicable). We obtained beneficiary chronic conditions from the Chronic Conditions Warehouse File (including AD/ADRD diagnosis) in the calendar year preceding the ED visit. Finally, we determined beneficiary NH residency status using a previously validated approach using Medicare professional and skilled nursing facility (SNF) claims (Supplemental Methods S1).14,15
ED Visits
We identified all ED visits among eligible beneficiaries to EDs in the 50 United States and the District of Columbia. For each visit, we determined the principal diagnosis and categorized them into 284 Healthcare Utilization Project Clinical Classification Software (CCS) Categories. We assigned each visit a disposition according to the following categories: died in the ED, admitted, observation, transferred to another hospital, and discharged.9,16
Utilization of Other Services
We identified each hospitalization type in the Medicare inpatient claims file and calculated the total number of days spent in each setting: inpatient acute care (i.e., short-term), inpatient psychiatry, inpatient rehabilitation, and long-term acute care hospital stays. ED visits and observation stays were identified in the outpatient file. We assigned each outpatient ED visit a duration of one day unless the claim indicated a longer duration. We obtained number and duration of SNF stays from the SNF file.
Calculating HDAH
For each ED visit, we calculated the total number of HDAH at 30 days starting from the date of the ED visit according to the equation below. While other studies of HDAH and other days at home measures have considered longer time periods,12,17–19 we chose a 30-day time window because outcomes during this period can reasonably be attributed to the quality of emergency care7,16,20–22 and other quality measures for acute episodes have similarly used a 30-day window.11,23,24 For each visit, if the beneficiary did not die during the 30-day mortality period, mortality days equaled zero. If the beneficiary died on the day after the ED visit, mortality days amounted to 29. We did not subtract hospice days from HDAH.
HDAH = 30 days – (Index Visit Days + Mortality Days + Inpatient Days + Observation Days + SNF Days + Outpatient ED Visits + Inpatient Psychiatry Days + Inpatient Rehabilitation Days + Long-term Hospital Days)
We adapted the components of the original concept of HDAH12 to include “index visit days, ” in accordance with prior work.9 The duration of the index visit represents the total time the patient spent in the hospital from ED presentation. If the patient was discharged from the ED, that would typically be 1 day; if the patient remained under observation or was admitted, then the length of observation or inpatient stay would be attributed to the index visit. All time spent in inpatient, observation, SNF, inpatient psychiatry, inpatient rehabilitation and long-term hospital settings were defined as the total time spent in each of these respective settings after the index visit. Consistent with other studies using HDAH,12,17,25 we counted an ED visit as one day, in contrast to other measures that have counted ED visits as half of a day.26,27 We considered multiple ED visits per person within the same 30-day period as separate index visits and counted these visits toward deductions in HDAH from previous ED visits.
Analysis
HDAH Overall and by Beneficiary Characteristics
We first examined the cross-sectional association between beneficiary characteristics and 30-day HDAH after an ED visit, using the two most recent study years (2017–2018). We calculated unadjusted HDAH overall and for each component. We did this for all beneficiaries and stratified by the beneficiary characteristics noted above. We then calculated trends over time in 30-day HDAH and its components using a linear regression model with year as the linear predictor, adjusting for principal visit diagnosis, hospital random effects and beneficiary demographic characteristics (age, sex, race, Medicaid eligibility) and chronic conditions. To examine the key drivers of trends in HDAH, we repeated these models separately for each of the key components of HDAH. While our primary analysis considered all ED visits, as a sensitivity analysis, we repeated our models stratified by whether the patient was admitted (including observation visits) or discharged.
HDAH Trends for Beneficiaries with AD/ADRD
While overall outcomes for ED visits have improved for Medicare beneficiaries in recent years,16 it is unclear whether beneficiaries with AD/ADRD have also seen improvements, particularly on broader measures of quality. Thus, to understand if any trends in HDAH have varied by beneficiary AD/ADRD status, we repeated our models with total HDAH as the outcome and year, AD/ADRD status, and an interaction between year and AD/ADRD diagnosis as the primary predictors, again adjusting for primary diagnosis and patient characteristics.
HDAH by NH Residency Status
NH residency status is a marker of overall beneficiary health28 and is associated with patterns of healthcare utilization.29,30 Individuals with AD/ADRD, in particular, have higher rates of long-term NH utilization as their disease progresses.31 We repeated our models with 30-day HDAH in 2017 and 2018 incorporating beneficiary AD/ADRD status, NH residency status and an interaction between the two to examine if the association between AD/ADRD status and 30-day HDAH varied by NH residency status. We then calculated adjusted mean 30-day HDAH following an ED visit for the four combinations of beneficiary AD/ADRD and NH status, again adjusting for the same set of beneficiary covariates.
90-Day HDAH
To examine if our results were sensitive to the observation period duration, we repeated our models examining overall trends and comparing trends by AD/ADRD status, using the outcome of HDAH within 90 days of the ED visit.
We analyzed data using SAS package 9.4. and considered results significant at a two-sided p-value of less than 0.05. The Office of Human Research Administration at the Harvard School of Public Health approved this study.
RESULTS
Study Sample Characteristics
In this study of traditional Medicare beneficiaries ages 68 and older, there were 19,626,287 ED visits from 2012–2018 among 4,754,041 beneficiaries who had 1 or more ED visits at 4,801 hospitals. The ED utilization rate in 2018 was 621 visits per 1000 eligible beneficiaries but varied by beneficiary characteristics (Supplemental Figure S2). Beneficiaries with and without AD/ADRD were generally seen in the ED and admitted for similar diagnoses (Supplemental Table S3). Key patient characteristics by year and AD/ADRD status are presented in Table 1. Compared to visits among those without AD/ADRD, visits among those with AD/ADRD more often involved NH residents (2.4% versus 22.1% in 2018). A greater proportion of ED visits among beneficiaries with AD/ADRD involved patients who were also Medicaid eligible compared to visits among those without AD/ADRD (35.9% vs. 18.2% in 2018), which may also be driven by NH residency status. A greater proportion of beneficiaries with ADRD (compared to those without ADRD) were Black (11.0% vs. 9.0% in 2018) and Hispanic (2.2% vs. 1.5%) and fewer were White (82.7% vs. 85.3%).
Table 1. Sample characteristics* of Emergency Department (ED) in 2012 and 2018 for Medicare beneficiaries* with and without Alzheimer’s Disease and Alzheimer’s Disease Related Dementias (AD/ADRD).
| 2012 | 2018 | ||||
|---|---|---|---|---|---|
| AD/ADRD | No AD/ADRD | AD/ADRD | No AD/ADRD | ||
| Number (%) of ED visits | 585,958 (21.7%) | 2,112,708 (78.3%) | 599,870 (22.2%) | 2,096,570 (77.8%) | |
| Age, mean (SD) in years | 83.6 | 79.0 | 83.2 | 78.4 | |
| Age range (years), % | 68–74 | 79,605 (13.6%) | 712,502 (33.7%) | 99,984 (16.7%) | 779,117 (37.2%) |
| 75–79 | 90,927 (15.5%) | 452,196 (21.4%) | 100,248 (16.7%) | 465,385 (22.2%) | |
| 80–84 | 131,349 (22.4%) | 413,770 (19.6%) | 126,148 (21.0%) | 374,056 (17.8%) | |
| 85 and older | 284,077 (48.5%) | 534,240 (25.3%) | 273,490 (45.6%) | 478,012 (22.8%) | |
| Female, % | 386,051 (65.9%) | 1,252,594 (59.3%) | 375,031 (62.5%) | 1,196,004 (57.0%) | |
| Race, % | White | 482,151 (82.3%) | 1,815,064 (85.9%) | 496,117 (82.7%) | 1,789,347 (85.3%) |
| Black | 73,650 (12.6%) | 202,922 (9.6%) | 69,112 (11.5%) | 188,274 (9.0%) | |
| Hispanic | 15,215 (2.6%) | 35,240 (1.7%) | 12,932 (2.2%) | 32,055 (1.5%) | |
| Asian | 7,382 (1.3%) | 25,556 (1.2%) | 9,185 (1.5%) | 28,704 (1.4%) | |
| Other | 4,458 (0.76%) | 21,076 (1.0%) | 6,793 (1.1%) | 26,127 (1.2%) | |
| Unknown | 776 (0.13%) | 2,527 (0.12%) | 2,551 (0.43%) | 19,862 (0.95%) | |
| North American Native | 2,326 (0.40%) | 10,323 (0.50%) | 3,180 (0.53%) | 12,201 (0.58%) | |
| Nursing Home Resident | Yes | 159,850 (27.3%) | 71,799 (3.4%) | 132,301 (22.1%) | 50,709 (2.4%) |
| No | 426,108 (72.7%) | 2,040,909 (96.6%) | 467,569 (77.9%) | 2,045,861 (97.6%) | |
| Medicaid Eligible, % | 238,058 (40.6%) | 453,394 (21.5%) | 215,277 (35.9%) | 381,362 (18.2%) | |
| Comorbidity, % | Congestive Heart Failure | 253,611 (43.3%) | 612,295 (29.0%) | 253,579 (42.3%) | 551,468 (26.3%) |
| Chronic Kidney Disease | 216,313 (36.9%) | 541,774 (25.6%) | 321,437 (53.6%) | 778,802 (37.1%) | |
| COPD | 158,828 (27.1%) | 455,820 (21.6%) | 175,035 (29.2%) | 452,196 (21.6%) | |
| Acute Myocardial Infarction | 13,574 (2.3%) | 37,700 (1.8%) | 17,029 (2.8%) | 38,194 (1.8%) | |
Random 20% sample of fee-for-service Medicare beneficiaries ages 68 and older in the 50 United States and the District of Columbia.
Unadjusted HDAH
Overall mean unadjusted 30-day HDAH in 2017–2018 was 22.4. Older age was associated with fewer HDAH; mean unadjusted HDAH was 24.0 for beneficiaries ages 68–74 compared to 20.4 for beneficiaries age 85+ (Table 2, Supplemental Table S4). These differences were primarily driven by greater number of index visit, mortality and SNF days for older adults. The number of outpatient ED days was highest among the 68–74 age group (0.20 days) and declined among successively older populations (0.15 among those 85 and older). This likely reflects the fact that ED visits among older age groups are more likely to result in admission from the ED (vs. discharge) as opposed to a lower rate of ED utilization (Supplemental Figure S2), and thus have fewer outpatient ED visits as a proportion of all ED encounters. Differences by race are shown in Table 2 and Supplemental Table S4. Black and Asian beneficiaries had the fewest HDAH (both 22.2), whereas beneficiaries with a race listed as Unknown had the highest HDAH (24.4) followed by Hispanic and North American Native beneficiaries (both 22.9). Medicaid-eligible beneficiaries had 2.6 fewer unadjusted 30-day HDAH (20.4 vs. 23.0), driven by a greater number of days spent in acute and post-acute care settings in addition to higher mortality (1.2 vs. 1.0 mortality days among beneficiaries who were not Medicaid eligible). Some of the observed changes in post-acute care utilization may represent changes in payer status for the same bed for NH residents.
Table 2. Unadjusted Healthy Days at Home (2017–2018) and Key Components by Beneficiary Characteristics.
| Number of Visits |
Index Visit Days |
Mortality Days | SNF Days | Inpatient Days | Observation Days | Outpatient ED Days | Total HDAH | |
|---|---|---|---|---|---|---|---|---|
| All Visits | 5,655,717 | 2.8 | 1.0 | 2.4 | 1.0 | 0.08 | 0.17 | 22.4 |
| AD/ADRD diagnosis | ||||||||
| Yes | 1,241,146 | 3.2 | 1.5 | 4.2 | 1.1 | 0.10 | 0.21 | 19.5 |
| No | 4,415,121 | 2.7 | 0.9 | 1.9 | 0.9 | 0.08 | 0.16 | 23.3 |
| Age | ||||||||
| 68–74 | 1,842,134 | 2.6 | 0.7 | 1.3 | 1.0 | 0.08 | 0.20 | 24.0 |
| 75 – 79 | 1,177,302 | 2.8 | 0.8 | 1.9 | 1.0 | 0.08 | 0.18 | 23.0 |
| 80 – 85 | 1,046,034 | 2.9 | 1.1 | 2.6 | 1.0 | 0.09 | 0.17 | 22.1 |
| 85 + | 1,191,244 | 3.0 | 1.6 | 3.8 | 0.9 | 0.08 | 0.15 | 20.4 |
| Sex | ||||||||
| Male | 2,352,930 | 2.9 | 1.2 | 2.1 | 1.1 | 0.08 | 0.19 | 22.3 |
| Female | 3,303,787 | 2.7 | 0.9 | 2.6 | 0.9 | 0.08 | 0.17 | 22.5 |
| Race | ||||||||
| White | 4,798,740 | 1.0 | 1.0 | 2.4 | 1.0 | 0.08 | 0.17 | 22.4 |
| Black | 544,263 | 0.9 | 0.9 | 2.3 | 1.0 | 0.10 | 0.23 | 22.2 |
| Other | 67,285 | 1.0 | 1.0 | 1.9 | 0.9 | 0.07 | 0.15 | 22.9 |
| Asian | 78,287 | 1.2 | 1.2 | 2.2 | 0.9 | 0.06 | 0.13 | 22.2 |
| Hispanic | 94,545 | 0.9 | 0.9 | 1.8 | 0.9 | 0.08 | 0.20 | 22.9 |
| Native | 31,790 | 1.0 | 1.0 | 1.8 | 1.2 | 0.11 | 0.31 | 22.9 |
| Unknown | 41,807 | 0.6 | 0.6 | 1.2 | 0.8 | 0.07 | 0.16 | 24.4 |
| Nursing Home Resident | ||||||||
| Yes | 383,463 | 1.2 | 2.2 | 5.6 | 1.1 | 0.08 | 0.19 | 17.4 |
| No | 5,271,254 | 1.0 | 0.9 | 2.2 | 1.0 | 0.08 | 0.17 | 22.8 |
| Medicaid Eligible | ||||||||
| Yes | 1,262,743 | 2.2 | 1.2 | 3.7 | 1.2 | 0.11 | 0.25 | 20.4 |
| No | 4,393,974 | 0.9 | 1.0 | 2.0 | 0.9 | 0.08 | 0.15 | 23.0 |
Trends in HDAH
Similar to prior studies,9,16,32 we found that the proportion of ED visits ending in discharge increased over time (from 53.0% in 2012 to 54.8% in 2018), as the decline in admissions (from 37.0% to 33.5%) and death (0.49% to 0.39%) was greater than the observed increases in visits ending in observation (7.4% to 8.8%; Supplemental Figure S5). 30-day HDAH rose by 2.4% from 22.29 in 2012 to 22.83 in 2018 (0.095 days/year, 95% CI 0.093 to 0.097; p<.001; Supplemental Figures S6 and S7), after adjusting for visit diagnosis and patient characteristics. This trend was driven by reductions in mortality days (−0.024 days/year, 95% CI −0.025 to −0.023; p<.001) and index stay duration (−0.040 days/year, 95% CI −0.041 to –0.039; p<.001; Supplemental Figure S6), which was primarily due to a reduction in admission rate (Supplemental Figure S5). When we stratified by whether the initial visit led to an admission or discharge, we found an increase in HDAH in both groups (Supplemental Figure S7) and a decline in the proportion of total visits ending in admission, suggesting that both shifting of patients out of the inpatient setting and broad improvement in HDAH components across disposition categories drove the observed increases in HDAH.
HDAH by Beneficiary AD/ADRD Diagnosis
Beneficiaries with AD/ADRD had more than double the rate of ED utilization compared to beneficiaries without AD/ADRD (1,226 vs. 545 visits per 1,000 beneficiaries in 2018). Additionally, people with AD/ADRD had markedly fewer unadjusted HDAH (19.5 vs. 23.3 among those without AD/ADRD). After adjusting for demographics characteristics (especially important given that beneficiaries with AD/ADRD are disproportionately older than those without AD/ADRD), visit diagnosis and other chronic conditions, beneficiaries with AD/ADRD still had 1.4 fewer HDAH within 30 days (21.6 vs. 23.0 for beneficiaries without AD/ADRD in 2017–2018). This difference was driven primarily by a greater number of mortality days (1.33 vs. 0.96), SNF days (3.05 vs. 2.10), and index visit days (2.41 vs. 2.29; Figure 1).
Figure 1. Comparison of adjusted 30-day Healthy Days at Home (HDAH)* overall and its components, stratified by beneficiary diagnosis of Alzheimer’s Disease and Related Dementias (AD/ADRD) in 2017–2018.
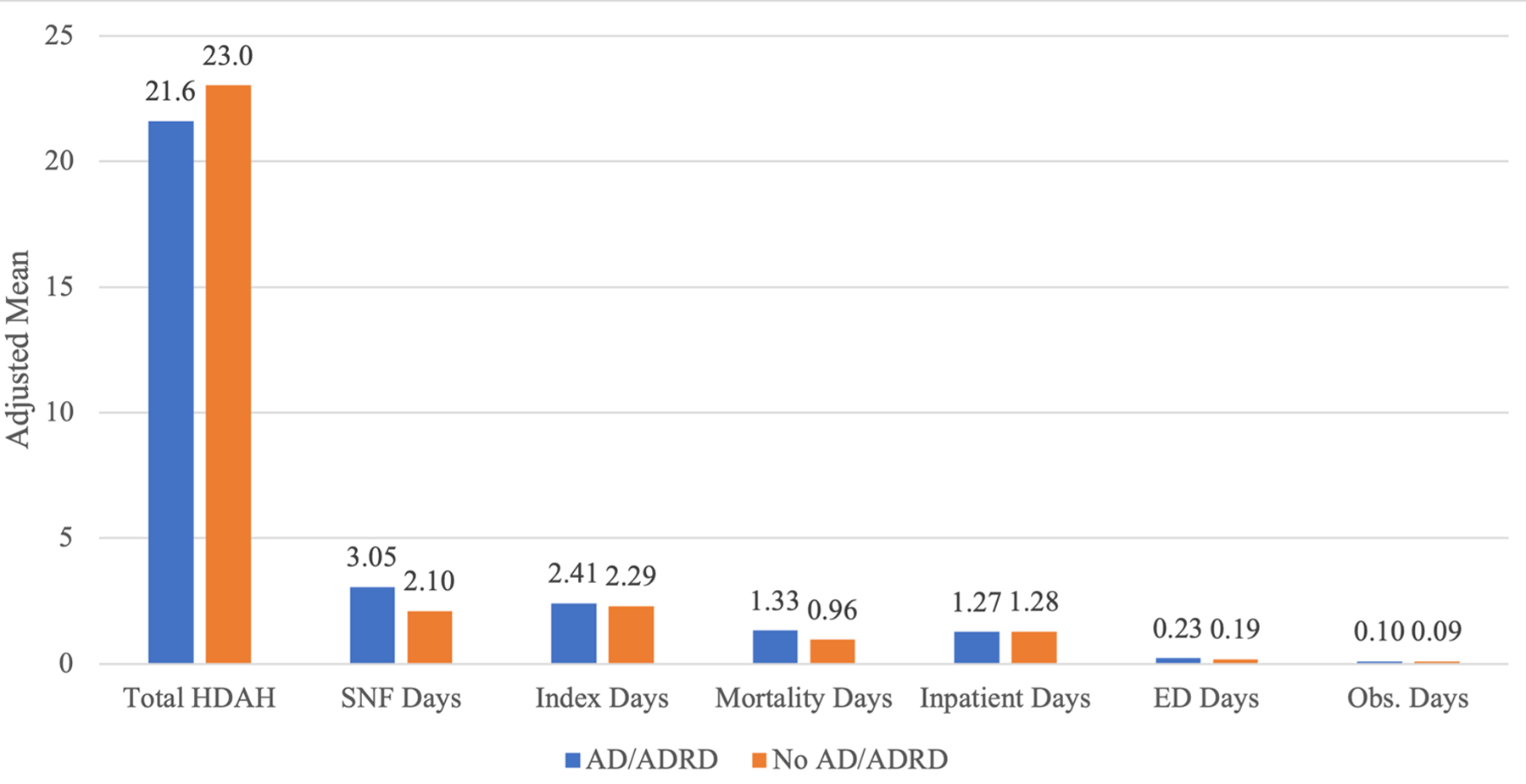
*Data years are 2016–2017 and adjusted means derived from linear regression model with 30-day HDAH and the respective component parts [skilled nursing facility (SNF) days, duration of the index visit, inpatient days after the index stay, mortality days, ED visit
Beneficiaries with AD/ADRD saw a 3.2% increase in adjusted 30-day HDAH from 21.1 in 2012 to 21.8 in 2018 (+0.114 days/year, 95% CI 0.110 to 0.119; p<.001; Supplemental Table S8 and Supplemental Figure S9). Beneficiaries without AD/ADRD saw a 2.2% increase in HDAH from 22.6 in 2012 to 23.1 in 2018 (+0.090 days/year, 95% CI 0.087 to 0.092; p<.001). The p-value for the interaction between year and AD/ADRD status was <.001, indicating that there was a differential time trend in 30-day HDAH for emergency care by AD/ADRD status. Thus, while beneficiaries with AD/ADRD had fewer HDAH in all study years compared to those without AD/ADRD, they saw a modest, but significantly faster increase in HDAH over time (Supplemental Figure S9).
Adjusted trends in the individual components of HDAH by AD/ADRD status are shown in Figure 2. Beneficiaries with AD/ADRD saw a larger decline in SNF days (−0.069 days/year, 95% CI −0.072 to −0.066; p<.001) compared to those without AD/ADRD (−0.025 days/year, 95% CI −0.027 to −0.024; p<.001). Additionally, beneficiaries with AD/ADRD saw a greater decline in mortality days (−0.031 days/year, 95% CI −0.033 to −0.029; p<.001) compared to those without AD/ADRD (−0.022 days/year, 95% CI −0.023 to −0.021; p<.001). However, those with AD/ADRD had a lesser decline in index visit days (−0.036 days/year, 95% CI −0.038 to −0.035; p<.001) compared to those without AD/ADRD (−0.041, 95% CI −0.042 to −0.040; p<.001). Additionally, those with AD/ADRD saw an increase in inpatient days after the index visit (0.002 days/year, 95% CI 0.001 to 0.004; p=0.002) compared to a decline for those without AD/ADRD (−0.006 days/year, 95% CI −0.007 to −0.006; p<.001). Both groups saw an increase in days spent in ED and observation settings, but these increases were greater for those with AD/ADRD (Figure 2, Supplemental Table S8).
Figure 2. Adjusted trends* over time (2012–2018) in 30-day Healthy Days at Home (HDAH) and its components, stratified by Alzheimer’s Disease and Alzheimer’s Disease Related Dementias (AD/ADRD) diagnosis.
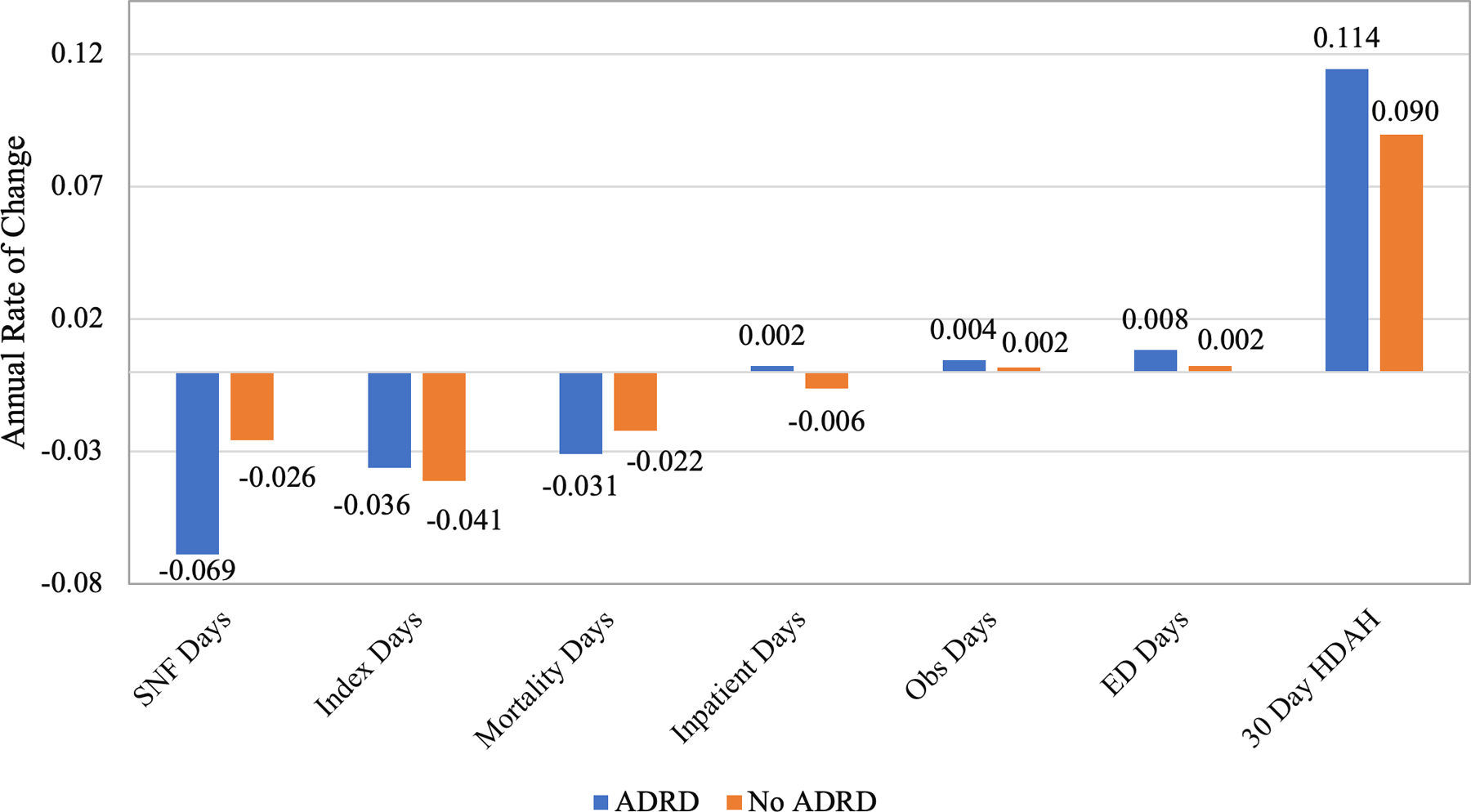
*Slope (days/year) from a linear regression model with 30-day HDAH and each respective component as the outcome and time (year) as the linear predictor, adjusting for hospital random effects as well as beneficiary age, sex, Medicaid eligibility, race and chronic conditions.
Interaction between AD/ADRD Status and NH Residency
NH residents had lower unadjusted 30-day HDAH compared to community-dwelling individuals (17.4 vs. 22.8 days). AD/ADRD was associated with fewer adjusted 30-day HDAH for both community-dwelling beneficiaries (22.0 vs. 23.3 days; p<.001) and NH residents (17.7 vs. 17.9; p<.001). However, the difference in total HDAH between those with and without AD/ADRD was greater for community-dwelling beneficiaries compared to NH residents (1.3 vs. 0.2; p<.001 for the interaction between NH status and AD/ADRD; Figure 3).
Figure 3. Examining the association between AD/ADRD diagnosis, nursing home residency status and total adjusted 30-day Healthy Days at Home in 2017–2018.
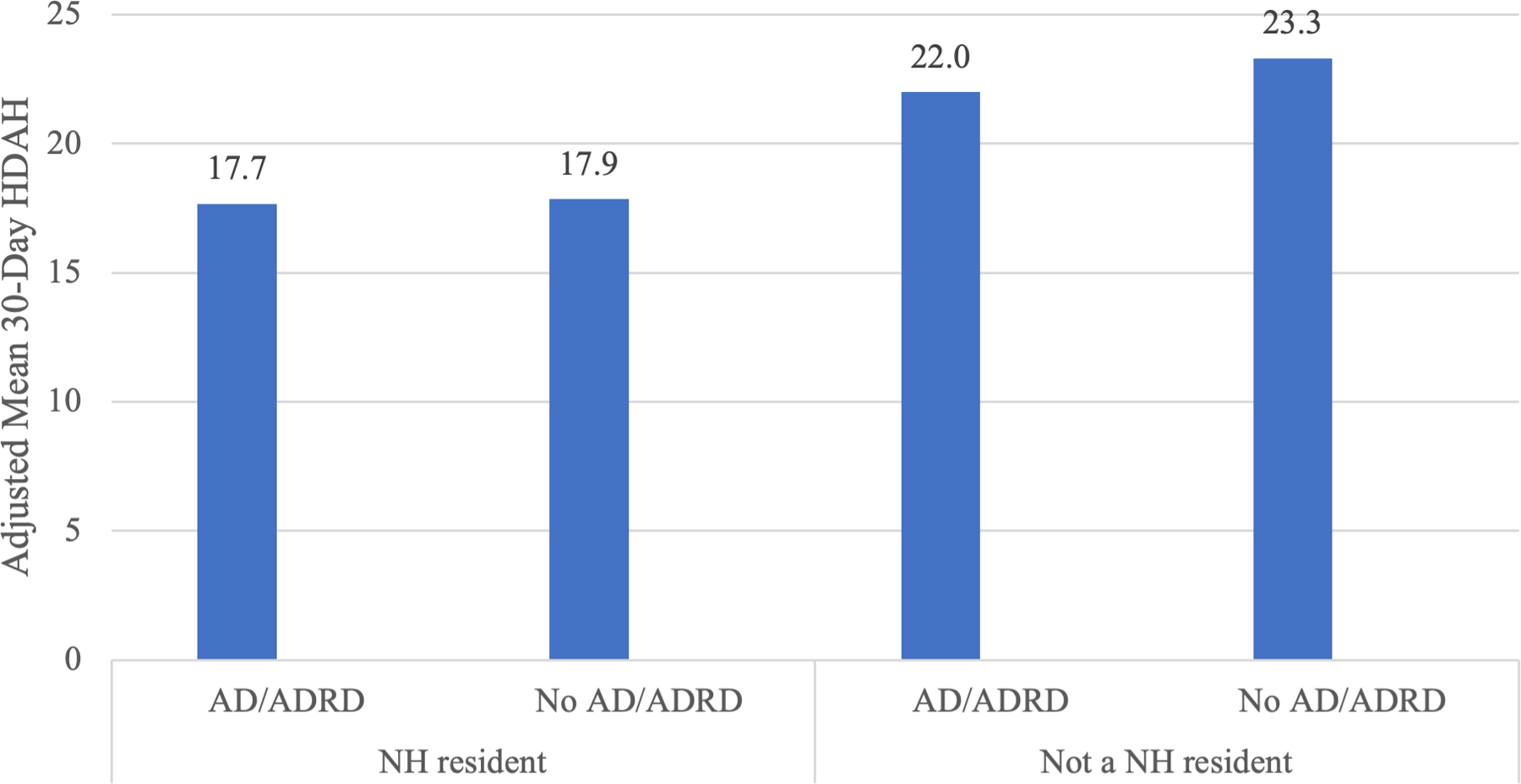
We specified a linear probability model, using 2017–2018 data for the outcome of 30-day HDAH. Our primary predictors were beneficiary AD/ADRD status, nursing home (NH) residency status and an interaction between AD/ADRD and NH status, adjusting for patient correlation at hospitals as well as beneficiary age, sex, Medicaid eligibility and chronic conditions.
Trends in 90-Day HDAH
Among all beneficiaries, there was an annual increase in 90-day HDAH of 0.32 days (95% CI 0.31 to 0.33; p<.001). Beneficiaries without AD/ADRD saw a mean annual increase in 90-day HDAH of 0.29 (95% CI 0.28 to 0.30) compared to 0.43 for beneficiaries with AD/ADRD (95% CI 0.41 to 0.45; p<.001 for the interaction of year and AD/ADRD).
DISCUSSION
In this study of over 19 million ED visits from 2012–2018, we found an increase over time in total 30-day HDAH associated with an ED visit, driven by declines in mortality and reductions in time spent in inpatient and post-acute care settings that offset the concomitant increase in observation and ED visit days. We found that beneficiaries with AD/ADRD, who were disproportionately Black or Hispanic, had substantially fewer HDAH compared to those without AD/ADRD, both due to higher mortality rates and greater utilization of inpatient, ED, observation and post-acute care. Yet, despite having fewer HDAH in all years, people with AD/ADRD saw modestly greater increases in HDAH over time and differential time trends in several measure components. Results were similar for 90-day HDAH. NH residency was associated with fewer HDAH, but differences by AD/ADRD status were more pronounced among community-dwelling beneficiaries. Taken together, these findings illustrate the degree to which HDAH can be used as an outcome measure for emergency care, taking into account the most severe outcome (mortality) as well as time spent in facility-based healthcare environments—an important outcome for many patients.33 Additionally, this measure can be used to identify unique patterns of care utilization and delivery that vary among populations of older adults using the ED.
The fact that older adults with AD/ADRD have fewer HDAH after an ED visit is consistent with the known significant morbidity and mortality associated with this disease. Delirium, falls, and deconditioning associated with acute care episodes in the AD/ADRD population are associated with poorer short and long-term outcomes.34 While the ED environment poses a number of challenges for the care of older adults,35 innovations (e.g., standardization of care via clinical pathways, accreditation for age-friendly emergency care)36,37 and services to support emergency physicians in finding alternatives to hospitalization for older adults (e.g., case management within the ED, observation units),38 when appropriate, have the potential to reduce the incidence of iatrogenic harms. While many of these interventions are aimed at reducing the use of inpatient care, our results suggest that post-acute care utilization, particularly SNF utilization, is another key driver of reduced total number of HDAH, particularly in the AD/ADRD population. Thus, interventions that keep older adults out of post-acute inpatient care settings39,40 may be particularly beneficial for the AD/ADRD population. Such interventions are likely to be broadly within the goals of care of many older adults and associated with lower total spending.41 Furthermore, given the differences in ED utilization by race among this population of older adults, attention to the drivers of HDAH may inform efforts to reduce disparities in emergency care quality and outcomes.
This study builds upon a growing body of literature suggesting that emergency care has evolved in recent years in ways that deliver better patient outcomes16 and overall savings to the healthcare system by reducing expensive hospitalizations and total time spent in acute care settings.9,42 While much of the framing of emergency care has focused on high costs relative to other ambulatory settings,43 there has been less attention paid to the role of the ED in rapidly risk-stratifying older adults experiencing acute illness and finding the most appropriate site of ongoing care to maximize outcomes and improve value.8,44 This study builds on prior work by suggesting that the benefits of evolving emergency care patterns are associated with lower mortality and greater time at home for older Medicare beneficiaries and that these benefits have extended to the AD/ADRD population. While prior work has examined annual HDAH12 and HDAH at the end-of-life,17 this is the first study to use this outcome for emergency care. By including a broad set of components, this measure minimizes the risk that the consequences of emergency care patterns will go undetected.
This study has several limitations. First, just because a beneficiary is at home does not mean that health has been optimized.45 However, direct indicators of functional status and self-reported health are time-intensive to collect. HDAH has the advantage of being objective and easily identifiable across a large population and other work has suggested that similar measures do correlate with direct measures of functional status and symptom burden.27,46,47 Another limitation is that, for NH residents, the home setting as defined by this measure is actually a nursing home and it is possible that NH factors (e.g., staffing) may influence whether a patient is sent to the ED. Furthermore, HDAH does not measure the burden of informal care delivered by family members or others, which is associated with substantial caregiver stress.48–50 Any attempts to reduce time spent in acute or post-acute care environments must consider unintended consequences for caregivers and society.48–54 Furthermore, this study dataset precedes the COVID-19 pandemic, which has brought numerous disruptions to the healthcare delivery system. Yet, we believe that the scarcity of hospital and post-acute care resources during the pandemic further underscores the need to develop measures that encourage appropriate alternatives to facility-based healthcare settings for older adults. We also acknowledge that since visiting the ED is related to both ADRD and HDAH, our study design could suffer from collider bias, which can occur when an exposure and outcome each influence a common third variable that has been controlled for by design or in the statistical analysis.55 However, it would be impossible to measure HDAH as an ED outcome measure without limiting the analyses to those with ED visits. A similar concern exists for examining differences by NH status, so readers should be cautious about interpreting the results in Figure 3 as causal. Additionally, this is a study of fee-for-service Medicare beneficiaries and does not include the growing proportion of Medicare Advantage beneficiaries. However, given that studies suggest Medicare Advantage tends to enroll healthier individuals,56,57 this would suggest that our observed improvements in HDAH over time may be a conservative estimate. Finally, it is possible that we may miss events related to the quality of emergency care that occurred after the 30-day period, although our 90-day sensitivity analysis yielded similar results.
CONCLUSION
In conclusion, 30-day HDAH is a broad outcome measure that may be useful for evaluating outcomes for emergency care. In our study, both AD/ADRD and NH status were associated with fewer HDAH at 30 days after an ED visit for Medicare beneficiaries, and differences in HDAH by AD/ADRD status were more pronounced among community-dwelling beneficiaries compared to NH residents. Overall, there has been an increase in HDAH at 30 days after an ED visit in recent years for Medicare beneficiaries, driven both by reductions in mortality and time spent in acute and post-acute care settings, but beneficiaries with AD/ADRD have seen modestly greater improvements in HDAH over time compared to those without AD/ADRD. These findings suggest that evolving emergency care patterns are yielding improved outcomes for older patients, particularly for those with AD/ADRD, a trend which may also yield savings to the healthcare system by reducing time spent in facility-based healthcare settings.
Supplementary Material
Supplemental Methods S1.
Supplemental Figure S2. Rates of ED utilization per 1,000 eligible beneficiaries overall and stratified by beneficiary characteristics in 2018
Supplemental Table S3. Ten most frequent principal diagnosis categories among emergency department (ED) visits and admissions for beneficiaries with and without AD/ADRD in 2012 versus 2018
Supplemental Table S4. Unadjusted Healthy Days at Home (2017–2018) and components by beneficiary characteristics
Supplemental Figure S5. Trends in disposition among Medicare beneficiaries seen in the emergency department from 2011–2018
Supplemental Figure S6. Adjusted trends over time (2012–2018) in 30-day Healthy Days at Home (HDAH) and its components.
Supplemental Figure S7. Trends in adjusted 30-day HDAH overall and stratified by disposition of the index ED visit
Supplemental Table S8. Trends in 30-Day Healthy Days at Home (HDAH) and its components from 2012–2018 among Medicare beneficiaries ages 65 and older with an emergency department (ED) visit
Supplemental Figure S9. Adjusted trends over time (2012–2018) in 30-day Healthy Days at Home after an Emergency Department Visit for beneficiaries with and without Alzheimer’s Disease and Alzheimer’s Disease Related Dementias (AD/ADRD)
KEY POINTS
Healthy Days at Home (HDAH) is a broad quality measure that accounts for mortality as well as total time spent in facility-based healthcare settings.
This national study of fee-for-service Medicare beneficiaries found an increase over time in HDAH following an ED visit for Medicare beneficiaries ages 68 and older, due to reductions in mortality as well as time spent in inpatient and post-acute care settings.
Medicare beneficiaries with AD/ADRD had fewer HDAH compared to those without
AD/ADRD, but greater improvements over time in HDAH after an ED visit.
Why does this matter?
These findings suggest that emergency care patterns are evolving in ways that deliver better outcomes to older Medicare beneficiaries with and without AD/ADRD, including lower mortality and greater time at home. These trends may also be yielding overall savings to the healthcare system by reducing total time spent in acute and post-acute care settings.
ACKNOWLEDGEMENTS
Sponsor’s Role:
The sponsors had no role in the design, methods, subject recruitment, data collections, analysis, and preparation of the paper.
Funding Statement:
This work was funded by grants from the Emergency Medicine Foundation and the National Institutes of Health National Institute on Aging (grant R56AG075017).
Footnotes
Presentations: The work was presented at the 2022 AcademyHealth Annual Research Meeting.
Conflict of Interest: Laura G. Burke serves as a healthcare economics consultant to the Emergency Medicine Policy Institute. Jose F. Figueroa received grants from Commonwealth Fund, National Institute on Aging, Episcopal Health Foundation, and Arnold Ventures Foundation outside the submitted work.
BRIEF DESCRIPTVE TITLE : Healthy Days at Home Trends
REFERENCES
- 1.Venkatesh AK, Mei H, Shuling L, et al. Cross-sectional Analysis of Emergency Department and Acute Care Utilization Among Medicare Beneficiaries. Acad Emerg Med Jul 2020;27(7):570–579. doi: 10.1111/acem.13971 [DOI] [PubMed] [Google Scholar]
- 2.Sun R KZ, Wong HS. Trends in Hospital Emergency Department Visits by Age and Payer, 2006–2015 2018. Accessed December 28, 2020. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb238-Emergency-Department-Age-Payer-2006-2015.jsp [PubMed]
- 3.Han JH, Vasilevskis EE, Chandrasekhar R, et al. Delirium in the Emergency Department and Its Extension into Hospitalization (DELINEATE) Study: Effect on 6-month Function and Cognition. J Am Geriatr Soc Jun 2017;65(6):1333–1338. doi: 10.1111/jgs.14824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Han JH, Shintani A, Eden S, et al. Delirium in the emergency department: an independent predictor of death within 6 months. Ann Emerg Med. Sep 2010;56(3):244–252 e1. doi: 10.1016/j.annemergmed.2010.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nagurney JM, Fleischman W, Han L, Leo-Summers L, Allore HG, Gill TM. Emergency Department Visits Without Hospitalization Are Associated With Functional Decline in Older Persons. Ann Emerg Med Apr 2017;69(4):426–433. doi: 10.1016/j.annemergmed.2016.09.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lamantia MA, Stump TE, Messina FC, Miller DK, Callahan CM. Emergency Department Use Among Older Adults With Dementia. Alzheimer Disease & Associated Disorders 2016–01-01 2016;30(1):35–40. doi: 10.1097/wad.0000000000000118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Obermeyer Z, Cohn B, Wilson M, Jena AB, Cutler DM. Early death after discharge from emergency departments: analysis of national US insurance claims data. BMJ Feb 1 2017;356:j239. doi: 10.1136/bmj.j239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smulowitz PB, Honigman L, Landon BE. A novel approach to identifying targets for cost reduction in the emergency department. Ann Emerg Med Mar 2013;61(3):293–300. doi: 10.1016/j.annemergmed.2012.05.042 [DOI] [PubMed] [Google Scholar]
- 9.Burke LG, Burke RC, Epstein SK, Orav EJ, Jha AK. Trends in Costs of Care for Medicare Beneficiaries Treated in the Emergency Department From 2011 to 2016. JAMA Netw Open Aug 3 2020;3(8):e208229. doi: 10.1001/jamanetworkopen.2020.8229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rajan KB, Weuve J, Barnes LL, Mcaninch EA, Wilson RS, Evans DA. Population estimate of people with clinical Alzheimer’s disease and mild cognitive impairment in the United States (2020–2060). Alzheimer’s & Dementia 2021–12-01 2021;17(12):1966–1975. doi: 10.1002/alz.12362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wadhera RK, Joynt Maddox KE, Wasfy JH, Haneuse S, Shen C, Yeh RW. Association of the Hospital Readmissions Reduction Program With Mortality Among Medicare Beneficiaries Hospitalized for Heart Failure, Acute Myocardial Infarction, and Pneumonia. JAMA Dec 25 2018;320(24):2542–2552. doi: 10.1001/jama.2018.19232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Burke LG, Orav EJ, Zheng J, Jha AK. Healthy Days at home: A novel population-based outcome measure. Healthc (Amst) Mar 2020;8(1):100378. doi: 10.1016/j.hjdsi.2019.100378 [DOI] [PubMed] [Google Scholar]
- 13.Long-term care providers and services users in the United States, 2015–2016 (2019). [PubMed]
- 14.Yun H KM, Curtis JR, Delzell E, Gary LC, Saag KG, Morrisey MA, Becker D, Matthews R, Smith W, Locher JL. Identifying types of nursing facility stays using Medicare claims data: an algorithm and validation. . Health Serv Outc Res Methodol 2010;10:100–10. 2010;10:100–110. doi:DOI 10.1007/s10742-010-0060-4 [DOI]
- 15.Goodwin JS, Li S, Zhou J, Graham JE, Karmarkar A, Ottenbacher K. Comparison of methods to identify long term care nursing home residence with administrative data. BMC Health Serv Res May 30 2017;17(1):376. doi: 10.1186/s12913-017-2318-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Burke LG, Epstein SK, Burke RC, Orav EJ, Jha AK. Trends in Mortality for Medicare Beneficiaries Treated in the Emergency Department From 2009 to 2016. JAMA Intern Med Nov 4 2019:1–9. doi: 10.1001/jamainternmed.2019.4866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lam MB, Riley KE, Zheng J, Orav EJ, Jha AK, Burke LG. Healthy days at home: A population-based quality measure for cancer patients at the end of life. Cancer Aug 10 2021;doi: 10.1002/cncr.33817 [DOI] [PubMed]
- 18.Freed SS, Kaufman BG, Van Houtven CH, Saunders R. Using a home time measure to differentiate ACO performance for seriously ill populations. J Am Geriatr Soc Sep 2022;70(9):2666–2676. doi: 10.1111/jgs.17882 [DOI] [PubMed] [Google Scholar]
- 19.Groff AC, Colla CH, Lee TH. Days Spent at Home - A Patient-Centered Goal and Outcome. N Engl J Med Oct 27 2016;375(17):1610–1612. doi: 10.1056/NEJMp1607206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schuur JD, Hsia RY, Burstin H, Schull MJ, Pines JM. Quality measurement in the emergency department: past and future. Health Aff (Millwood) Dec 2013;32(12):2129–38. doi: 10.1377/hlthaff.2013.0730 [DOI] [PubMed] [Google Scholar]
- 21.Galarraga JE, Pines JM. Costs of ED episodes of care in the United States. Am J Emerg Med Mar 2016;34(3):357–65. doi: 10.1016/j.ajem.2015.06.001 [DOI] [PubMed] [Google Scholar]
- 22.Miyawaki A, Jena AB, Burke LG, Figueroa JF, Tsugawa Y. Association Between Emergency Physician’s Age and Mortality of Medicare Patients Aged 65 to 89 Years After Emergency Department Visit. Ann Emerg Med Mar 22 2023;doi: 10.1016/j.annemergmed.2023.02.010 [DOI] [PubMed]
- 23.Joynt Maddox KE, Orav EJ, Zheng J, Epstein AM. Year 1 of the Bundled Payments for Care Improvement-Advanced Model. N Engl J Med Aug 12 2021;385(7):618–627. doi: 10.1056/NEJMsa2033678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Joynt KE, Orav EJ, Jha AK. Mortality rates for Medicare beneficiaries admitted to critical access and non-critical access hospitals, 2002–2010. JAMA Apr 3 2013;309(13):1379–87. doi: 10.1001/jama.2013.2366 [DOI] [PubMed] [Google Scholar]
- 25.Burke LG, Burke RC, Orav EJ, Duggan CE, Figueroa JF, Jha AK. Association of Academic Medical Center Presence With Clinical Outcomes at Neighboring Community Hospitals Among Medicare Beneficiaries. JAMA Netw Open Feb 1 2023;6(2):e2254559. doi: 10.1001/jamanetworkopen.2022.54559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wadhera RK, Joynt Maddox KE, Desai NR, et al. Evaluation of Hospital Performance Using the Excess Days in Acute Care Measure in the Hospital Readmissions Reduction Program. Ann Intern Med Jan 2021;174(1):86–92. doi: 10.7326/M20-3486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shen E, Rozema EJ, Haupt EC, et al. Assessing the concurrent validity of days alive and at home metric. J Am Geriatr Soc Sep 2022;70(9):2630–2637. doi: 10.1111/jgs.17506 [DOI] [PubMed] [Google Scholar]
- 28.Research Findings No. 5: Characteristics of Nursing Home Residents, 1996 (Agency for Healthcare Research and Quality.) (2011).
- 29.Marincowitz C, Preston L, Cantrell A, Tonkins M, Sabir L, Mason S. Factors associated with increased Emergency Department transfer in older long-term care residents: a systematic review. Lancet Healthy Longev Jun 2022;3(6):e437–e447. doi: 10.1016/S2666-7568(22)00113-1 [DOI] [PubMed] [Google Scholar]
- 30.Gruneir A, Bell CM, Bronskill SE, Schull M, Anderson GM, Rochon PA. Frequency and pattern of emergency department visits by long-term care residents--a population-based study. J Am Geriatr Soc Mar 2010;58(3):510–7. doi: 10.1111/j.1532-5415.2010.02736.x [DOI] [PubMed] [Google Scholar]
- 31.Arrighi HM, Neumann PJ, Lieberburg IM, Townsend RJ. Lethality of Alzheimer disease and its impact on nursing home placement. Alzheimer Dis Assoc Disord Jan-Mar 2010;24(1):90–5. doi: 10.1097/WAD.0b013e31819fe7d1 [DOI] [PubMed] [Google Scholar]
- 32.Burke LG, Wild RC, Orav EJ, Hsia RY. Are trends in billing for high-intensity emergency care explained by changes in services provided in the emergency department? An observational study among US Medicare beneficiaries. BMJ Open Jan 30 2018;8(1):e019357. doi: 10.1136/bmjopen-2017-019357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Xian Y, O’Brien EC, Fonarow GC, et al. Patient-Centered Research into Outcomes Stroke Patients Prefer and Effectiveness Research: Implementing the patient-driven research paradigm to aid decision making in stroke care. Am Heart J Jul 2015;170(1):36–45, 45 e1–11. doi: 10.1016/j.ahj.2015.04.008 [DOI] [PubMed] [Google Scholar]
- 34.Fox A, Macandrew M, Ramis MA. Health outcomes of patients with dementia in acute care settings—A systematic review. International Journal of Older People Nursing 2020–09-01 2020;15(3):e12315. doi: 10.1111/opn.12315 [DOI] [PubMed] [Google Scholar]
- 35.Hwang U, Morrison RS. The Geriatric Emergency Department. Journal of the American Geriatrics Society 2007–11-01 2007;55(11):1873–1876. doi: 10.1111/j.1532-5415.2007.01400.x [DOI] [PubMed] [Google Scholar]
- 36.Mechanic OJ, Pascheles CY, Lopez GJ, et al. Using the Boston Syncope Observation Management Pathway to Reduce Hospital Admission and Adverse Outcomes. West J Emerg Med Mar 2019;20(2):250–255. doi: 10.5811/westjem.2018.11.39657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Marill MC. Age-Friendly Care At The Emergency Department. Health Aff (Millwood) Nov 2019;38(11):1780–1785. doi: 10.1377/hlthaff.2019.01202 [DOI] [PubMed] [Google Scholar]
- 38.Venkatesh AK, Geisler BP, Gibson Chambers JJ, Baugh CW, Bohan JS, Schuur JD. Use of observation care in US emergency departments, 2001 to 2008. PLoS One 2011;6(9):e24326. doi: 10.1371/journal.pone.0024326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Regenbogen SE, Cain-Nielsen AH, Syrjamaki JD, Chen LM, Norton EC. Spending On Postacute Care After Hospitalization In Commercial Insurance And Medicare Around Age Sixty-Five. Health Aff (Millwood) Sep 2019;38(9):1505–1513. doi: 10.1377/hlthaff.2018.05445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhu JM, Patel V, Shea JA, Neuman MD, Werner RM. Hospitals Using Bundled Payment Report Reducing Skilled Nursing Facility Use And Improving Care Integration. Health Aff (Millwood) Aug 2018;37(8):1282–1289. doi: 10.1377/hlthaff.2018.0257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mechanic R Post-acute care--the next frontier for controlling Medicare spending. N Engl J Med Feb 20 2014;370(8):692–4. doi: 10.1056/NEJMp1315607 [DOI] [PubMed] [Google Scholar]
- 42.Lin MP, Baker O, Richardson LD, Schuur JD. Trends in Emergency Department Visits and Admission Rates Among US Acute Care Hospitals. JAMA Intern Med Dec 1 2018;178(12):1708–1710. doi: 10.1001/jamainternmed.2018.4725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Weinick RM, Burns RM, Mehrotra A. Many emergency department visits could be managed at urgent care centers and retail clinics. Health Aff (Millwood) Sep 2010;29(9):1630–6. doi: 10.1377/hlthaff.2009.0748 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schuur JD, Venkatesh AK. The growing role of emergency departments in hospital admissions. N Engl J Med Aug 2 2012;367(5):391–3. doi: 10.1056/NEJMp1204431 [DOI] [PubMed] [Google Scholar]
- 45.Ankuda CK, Grabowski DC. Is every day at home a good day? J Am Geriatr Soc Sep 2022;70(9):2481–2483. doi: 10.1111/jgs.17973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fonarow GC, Liang L, Thomas L, et al. Assessment of Home-Time After Acute Ischemic Stroke in Medicare Beneficiaries. Stroke Mar 2016;47(3):836–42. doi: 10.1161/STROKEAHA.115.011599 [DOI] [PubMed] [Google Scholar]
- 47.Taran S, Coiffard B, Huszti E, et al. Association of Days Alive and at Home at Day 90 After Intensive Care Unit Admission With Long-term Survival and Functional Status Among Mechanically Ventilated Patients. JAMA Netw Open Mar 1 2023;6(3):e233265. doi: 10.1001/jamanetworkopen.2023.3265 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Gilhooly KJ, Gilhooly MLM, Sullivan MP, et al. A meta-review of stress, coping and interventions in dementia and dementia caregiving. BMC Geriatrics 2016–12-01 2016;16(1)doi: 10.1186/s12877-016-0280-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Musich S, Wang SS, Kraemer S, Hawkins K, Wicker E. Caregivers for older adults: Prevalence, characteristics, and health care utilization and expenditures. Geriatric Nursing 2017;38(1) [DOI] [PubMed] [Google Scholar]
- 50.Pinquart M, Sörensen S. Differences between caregivers and noncaregivers in psychological health and physical health: a meta-analysis. Psychol Aging Jun 2003;18(2):250–67. doi: 10.1037/0882-7974.18.2.250 [DOI] [PubMed] [Google Scholar]
- 51.Mausbach BT, Chattillion EA, Roepke SK, Patterson TL, Grant I. A Comparison of Psychosocial Outcomes in Elderly Alzheimer Caregivers and Noncaregivers. The American Journal of Geriatric Psychiatry 2013–01-01 2013;21(1):5–13. doi: 10.1016/j.jagp.2012.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Garlo K, O’Leary JR, Van Ness PH, Fried TR. Burden in Caregivers of Older Adults with Advanced Illness. Journal of the American Geriatrics Society 2010–12-01 2010;58(12):2315–2322. doi: 10.1111/j.1532-5415.2010.03177.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Spillman BC, Long SK. Does High Caregiver Stress Predict Nursing Home Entry? INQUIRY: The Journal of Health Care Organization, Provision, and Financing 2009–05-01 2009;46(2):140–161. doi: 10.5034/inquiryjrnl_46.02.140 [DOI] [PubMed] [Google Scholar]
- 54.Langa KM, Chernew ME, Kabeto MU, et al. National estimates of the quantity and cost of informal caregiving for the elderly with dementia. Journal of General Internal Medicine 2001–11-01 2001;16(11):770–778. doi: 10.1111/j.1525-1497.2001.10123.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Holmberg MJ, Andersen LW. Collider Bias. JAMA Apr 05 2022;327(13):1282–1283. doi: 10.1001/jama.2022.1820 [DOI] [PubMed] [Google Scholar]
- 56.Meyers DJ, Belanger E, Joyce N, McHugh J, Rahman M, Mor V. Analysis of Drivers of Disenrollment and Plan Switching Among Medicare Advantage Beneficiaries. JAMA Intern Med Feb 25 2019;doi: 10.1001/jamainternmed.2018.7639 [DOI] [PMC free article] [PubMed]
- 57.Ndumele CD, Elliott MN, Haviland AM, et al. Differences in Hospitalizations Between Fee-for-Service and Medicare Advantage Beneficiaries. Med Care Jan 2019;57(1):8–12. doi: 10.1097/MLR.0000000000001000 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Methods S1.
Supplemental Figure S2. Rates of ED utilization per 1,000 eligible beneficiaries overall and stratified by beneficiary characteristics in 2018
Supplemental Table S3. Ten most frequent principal diagnosis categories among emergency department (ED) visits and admissions for beneficiaries with and without AD/ADRD in 2012 versus 2018
Supplemental Table S4. Unadjusted Healthy Days at Home (2017–2018) and components by beneficiary characteristics
Supplemental Figure S5. Trends in disposition among Medicare beneficiaries seen in the emergency department from 2011–2018
Supplemental Figure S6. Adjusted trends over time (2012–2018) in 30-day Healthy Days at Home (HDAH) and its components.
Supplemental Figure S7. Trends in adjusted 30-day HDAH overall and stratified by disposition of the index ED visit
Supplemental Table S8. Trends in 30-Day Healthy Days at Home (HDAH) and its components from 2012–2018 among Medicare beneficiaries ages 65 and older with an emergency department (ED) visit
Supplemental Figure S9. Adjusted trends over time (2012–2018) in 30-day Healthy Days at Home after an Emergency Department Visit for beneficiaries with and without Alzheimer’s Disease and Alzheimer’s Disease Related Dementias (AD/ADRD)


