Abstract
Background:
Falls and their sequelae cost the healthcare system more than $50 billion every year. Older adults with hearing loss are at 2.4 times greater risk of falls than their normal hearing peers. Current research is inconclusive about whether hearing aids can offset this increased fall risk, and no previous studies considered if outcomes differed based on the consistency of hearing aid use.
Methods:
Individuals aged 60+ with bilateral hearing loss completed a survey consisting of the Fall Risk Questionnaire (FRQ) and questions about hearing loss history, hearing aid use, and other common fall risk factors. In this cross-sectional study, fall prevalence, as well as fall risk (based on FRQ score), was compared between hearing-aid users and non-users. A separate group of consistent hearing-aid users (at least 4 hours daily use for more than 1 year) were also compared to inconsistent/non-users.
Results:
Responses from 299 surveys were analyzed. Bivariate analysis found 50% reduced odds of experiencing a fall for any hearing aid users compared to non-users (OR=0.50 [95% CI: 0.29–0.85], p=0.01). After adjusting for age, sex, hearing loss severity, and medication usage, those who reported any hearing aid use still had lower odds of falls (OR=0.48 [95% CI: 0.26–0.90], p=0.02) and lower odds of being at risk for falls (OR=0.36 [95% CI: 0.19–0.66] p<0.001) than non-users. Results for consistent hearing-aid users demonstrate an even stronger association of lowered odds of falling (OR=0.35 [95% CI: 0.19–0.67], p<0.001) and lower odds of being at risk for falls (OR=0.32 [95% CI: 0.12–0.59], p<0.001), suggesting a potential dose-response relationship.
Conclusions:
These findings suggest that use of hearing aids—especially consistent hearing aid use—is associated with lower odds of experiencing a fall or being classified as at risk for falls in older individuals with hearing loss.
Keywords: hearing aids, falls, hearing loss, hearing impairment, older adults
1. Introduction
Approximately 1 in every 4 individuals older than 65 will experience a fall this year [1–3]. Injuries from falls cost $50 billion every year—a greater burden on the healthcare system than obesity or smoking [1]. As the average life expectancy increases, death rates due to falls are also increasing [4], up 30% from 2007 to 2016 [3]. If this trend continues, the CDC estimates approximately 50 million falls will occur annually in adults over 65 by the year 2030 [1]. Established risk factors for falling include: increasing age [1, 4, 5], female sex [1, 5], vision loss [5–7], greater severities of hearing loss [8, 9], previous falls [5, 10], vestibular dysfunction [11], Parkinson’s Disease [5, 12], cognitive impairment [5, 13], diabetes [14], and use of certain medications [15].
Like falls, hearing loss is also very common in individuals older than 60, with prevalence estimates between 33–40% in this population [16]. Data from the National Health and Nutritional Examination Survey (NHANES) demonstrated that adults aged 40–69 with hearing loss were at greater risk of falls than their normal-hearing counterparts [8]. Moreover, this study demonstrated a dose-response relationship: the risk of falling increased 1.4-fold for every 10 dB of hearing loss (pure tone average of 500, 1000, 2000, and 4000 Hz). Separately, meta-analysis has also shown that those with hearing loss are 2.4 times as likely to experience a fall than their normal-hearing peers [9].
These studies provide robust evidence that hearing loss is a risk factor for falls. However, the physiologic mechanism(s) that underlie this relationship are still not fully understood. Proposed hypotheses include: 1) concomitant factors that degrade the auditory system also degrade the vestibular system, 2) the increased communication load caused by hearing loss reduces the overall executive function capacity needed to maintain balance, and 3) hearing loss limits access to the auditory cues necessary for accurate spatial orientation, which can negatively affect postural stability, leading to falls [8, 9].
Since hearing aid use addresses reduction in communication cognitive load and increased access to auditory spatial cues, some researchers [9, 17] have posited that hearing aid use might reduce fall risk in individuals with hearing loss. However, studies of this relationship have provided heterogeneous results. Several have concluded that hearing aid users had higher odds of falling than non-users [17–20], three did not find the relationship significant [21–23], and two demonstrated statistically significant lower odds of falling for hearing aid users compared to non-users [24, 25].
A critical weakness of several of these studies is that they may have misclassified hearing aid use. Most of the previous studies used the question, “Have you ever worn hearing aids?” to dichotomize hearing aid users from non-users. This simple query did not provide recency or frequency information about the hearing aid use [20, 22, 23]. In an extreme case, a person who unsuccessfully trialed hearing aids many years ago might have been described as a hearing aid user. In some cases, the existing literature also failed to consider covariate data accounting for fall-risk factors between groups (e.g., severity of the hearing loss, medication usage, medical comorbidities) [20, 24]. Other limitations of previous studies include comparing their exposure group (hearing aid users) to those with normal hearing rather than those with untreated hearing loss [23] or being underpowered because their evaluation of the relationship between hearing aid use and falls was a subanalysis [21].
The present study was designed to test the hypotheses that hearing aid use was associated with reduced rates and risk of falls while addressing some of the shortfalls of previous research. Our study collected information about frequency and duration of hearing aid use, degree of hearing loss, and potential medical and pharmaceutical covariates directly from the electronic health record (EHR), thus providing robust covariate data for analysis.
Methods
Individuals aged 60 and older who were seen at the outpatient University of Colorado Hospital Audiology Clinic between September 2020 and September 2021 with documented bilateral sensorineural hearing loss were surveyed about their hearing aid use and fall risk. Hearing loss was defined as air and bone conduction thresholds poorer than 30 dB at any 2 frequencies in the speech range (500–6000 Hz) for the better ear. This criterion was chosen to ensure participants had enough hearing loss to at least be marginal hearing aid candidates so that even non-hearing aid users were potential hearing aid candidates. Potential participants were excluded if they had a knee or hip replacement in the past 12 months, were non-ambulatory (could not walk 20 feet unassisted), were actively taking meclizine, had a diagnosis of vestibular dysfunction or Parkinson’s, or were legally blind. The research study was approved by the Colorado Multiple Institutional Review Board (COMIRB 20–0384).
Those identified as meeting inclusion criteria were invited to complete a study survey either on paper in the clinic or by email invitation (up to three email invitations sent if no response) following their appointment. The complete data collection tool was comprised of a standardized questionnaire along with an additional 12 demographic and health-comorbidity questions. The Fall Risk Questionnaire (FRQ) is a validated patient reported outcome measurement tool consisting of 12 “yes” or “no” questions [26]. The primary outcome measure of fall prevalence was determined by response to the first question of the FRQ, “I have fallen in the past 6 months” to categorize a participant as having “any fall” or “no falls.” The other questions on the FRQ ask about potential risk factors for falls, including lower extremity strength, peripheral neuropathy, urinary urgency, medication usage, and depression. Collectively, the composite score on the 12-item FRQ was used to classify an individual’s fall risk. Consistent with development of the tool, a participant with 4 or more affirmative answers on the FRQ was considered a “fall risk,” and a participant with 3 or fewer affirmative answers was considered “not a fall risk” [26]. The authors viewed fall prevalence and fall risk as different outcomes providing distinct perspectives to the research question because: an individual could be at risk for falls but never experience one; alternately, an individual could report a fall that occurred for environmental or circumstantial reasons yet was unrelated to their balance or risk of falls.
Additional questions on the survey asked participants to self-report how many years they have had hearing loss, if they wear hearing aids, and if they experience positional dizziness. Those who answered “yes” to “Do you wear a hearing aid?” were considered “any hearing aid users” and were asked to self-report how long (in years) and how often (hours/day) they have used their hearing aids. These responses were then used to dichotomize “consistent hearing aid users” and “inconsistent/non hearing aid users.” Because our survey asked about falls that occurred in the past 6 months, any new hearing-aid users (reporting less than one year of use) were not considered consistent users, given they could have experienced a fall event and then received their hearing aids after that occurrence. Further, studies have shown that acclimatization and full benefit from hearing aids does not occur unless an individual uses their aids for at least 4 hours/day [27]. Therefore, only those who self-reported at least 4 hours of hearing-aid use/day for at least 1 year were considered “consistent users.”
Once a participant completed the survey questionnaire, covariate data was collected from their EHR. Data included age, sex, race, hearing loss severity, and asymmetry (using pure tone averages of 500, 1000, and 2000 Hz from the audiogram). Their anticholinergic risk score (ARS) [28] was also calculated from their medication list. This tool stratifies medications on a 0-to-3-point scale based on their likelihood of having anticholinergic properties, the primary central effects being falls, dizziness, and confusion. Finally, it was also documented if the participant had a CPT code in their EHR indicating diabetes, cognitive decline, a previous fall (occurring greater than 6 months prior to survey collection), or stroke.
Data analysis
Logistic regression analysis was used to model the data for both the fall-prevalence and fall-risk outcome measures for both exposure groups–those with any hearing aid use and those with consistent hearing aid use. Both an unadjusted model (only the exposure and outcome entered) and a model adjusted for age, sex, hearing loss severity, and medication usage were completed. The covariates entered into the adjusted model were chosen a priori, as substantial evidence [5, 8, 9, 10, 13, 15] has established their propensity to affect the rate of falls in older adults.
Following the initial regression analysis, a sensitivity analysis was also completed. To examine if the adjusted-model covariate selection significantly impacted the data analysis or if a more robust model was available, forward stepwise logistic regression accounting for all potential covariates was run. Additionally, because Poisson regression with robust standard errors can provide more precise confidence intervals and/or more interpretable point estimates than logistic regression (for high-prevalence outcomes), the adjusted models were rerun under Poisson regression with robust standard errors and evaluated for any differences in the results compared to the primary adjusted logistic regression models. All analyses were run on JASP 0.16.4 (Amsterdam, Netherlands)
Results
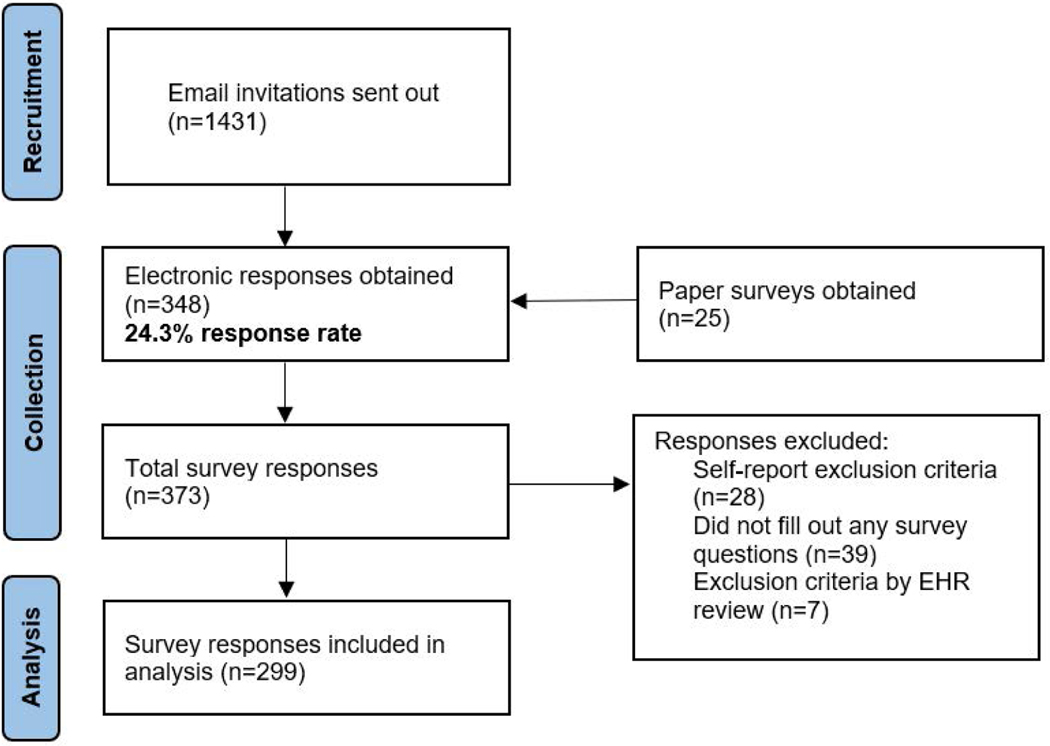
A total of 373 survey responses were collected—348 electronically and 25 paper. Of the total, 74 were excluded due to self-reported exclusion criteria, incompletion, or exclusion criteria met after EHR review (e.g., taking meclizine, Parkinson’s diagnosis), leaving 299 responses for statistical analysis (Figure 1). Overall participant characteristics are summarized in Table 1. Briefly, the mean age of respondents was 73.8 years (SD 6.7), 51.2% of respondents were female, 96.1% were white, and the average hearing loss severity (pure tone average of both ears) was 35.9 dB (SD 15.2). More than 26% of participants reported a fall in the past 6 months, and 31.3% were classified as being at risk for falls based on their FRQ responses. The percentage of respondents reporting any hearing-aid use was 68.8% with 60.5% of respondents being consistent hearing-aid users.
Figure 1.
Flow diagram showing recruitment, collection, and analysis of surveys.
TABLE 1.
Demographic characteristics for all participants and for consistent vs inconsistent users. Continuous variables are shown by their means (standard deviations) and categorical variables are shown by proportion.
| Characteristic | All participants | Consistent users | Inconsistent/non-users | P-value |
|---|---|---|---|---|
| (n=299) | (n=181) | (n=118) | ||
| Demographics | ||||
| Age | 73.8 (6.7) | 74.8 (6.6) | 72.5 (6.6) | 0.004 |
| Female sex | 51.2% | 52.8% | 50.9% | 0.74 |
| White race | 96.1% | 97.1% | 94.7% | 0.38 |
| Fall Characteristics | ||||
| *Any fall | 26.4% | 19.3% | 37.3% | <0.001 |
| *Fall-risk | 31.3% | 24.0% | 42.4% | <0.001 |
| Hearing Characteristics | ||||
| *Any HA use | 68.8% | – | – | – |
| *Consistent HA use | 60.5% | – | – | – |
| Hearing loss severity (dB) | 35.9 (15.3) | 40.7 (15.4) | 28.7 (11.7) | <0.001 |
| Hearing loss asymmetry (dB) | 6.6 (11.8) | 7.1 (11.6) | 5.8 (12.1) | 0.39 |
| *Hearing loss duration (years) | 12.2 (14.0) | 14.7 (15.0) | 8.0 (11.1) | <0.001 |
| Comorbidities | ||||
| ARS score | 1.1 (1.7) | 1.1 (1.7) | 1.2 (1.7) | 0.40 |
| Diabetes | 15.8% | 14.8% | 17.3% | 0.58 |
| Stroke | 4.7% | 7.1% | 0.9% | 0.02 |
| Cognitive decline | 2.1% | 1.8% | 2.8% | 0.58 |
| Previous falls | 3.2% | 3.0% | 3.7% | 0.74 |
| *Positional dizziness | 11.8 | 11.0% | 12.9% | 0.62 |
indicates any characteristic collected by participant self-report. P-values are for Welch’s t-tests (continuous variables) and chi-squared tests (categorical variables) between consistent and inconsistent/non users, significant p-values are in bold. ARS=Anticholinergic Risk Scale, dB=decibel, HA=hearing aid.
Based on the self-reported average daily hours of usage and duration of hearing aid use in years, a total of 181 participants were considered consistent hearing aid users, 23 were inconsistent users, and the remaining 95 had no hearing aid use. Independent sample t-tests showed no significant difference between the inconsistent and non-hearing aid users–the groups did not significantly vary by age, sex, race, hearing-loss severity, diabetes, stroke, cognitive decline, or previous falls (see supplemental material). As a result, these groups were collapsed into one inconsistent/non-user group for our models of “consistent hearing aid use” as the exposure group. Table 1 reviews multiple respondent characteristics both for all participants and as separated by hearing aid use. Consistent users significantly varied from inconsistent/non-users by fall status, fall-risk classification, age, hearing loss severity, hearing loss duration, dizziness and proportion who had experienced a stroke.
Seventy-nine respondents reported a fall in the past 6 months, while 220 reported no falls in the same period (Table 2). Those with any fall significantly varied from those with no falls by any hearing aid use, consistent hearing-aid use, age, ARS score, and previous falls documented in their EHR. Those who reported a fall were significantly younger than those who had not. Ninety-two participants were classified as being “at risk for falls” based on their FRQ scores. The remaining 197 participants scored 3 or less on their FRQ, categorizing them as “not at risk for falls.” Those at risk for falls significantly varied from those not at risk by any hearing aid use, consistent hearing aid use, ARS score, and proportion who had diabetes or had experienced a previous fall.
TABLE 2.
Collected covariates by fall-status and by fall-risk classification
| Characteristic | No falls (n=220) | Any falls (n=79) | P-value | Not at fall-risk (n=197) | Fall-risk (n=92) | P-value |
|---|---|---|---|---|---|---|
| Demographics | ||||||
| Age | 74.3 (6.8) | 72.4 (6.4) | 0.03 | 74.0 (6.5) | 73.4 (7.0) | 0.46 |
| Female sex | 47% | 50.6% | 0.57 | 53.8% | 47.8% | 0.34 |
| White race | 97.0% | 94.9% | 0.4 | 96.4% | 95.6% | 0.96 |
| Hearing Characteristics | ||||||
| *Any HA use | 72.7% | 56.9% | 0.01 | 74.5% | 54.8% | <0.001 |
| *Consistent HA use | 66.4% | 44.3% | <0.00 | 66.6% | 46.2% | <0.001 |
| Hearing loss severity (dB) | 35.9 (15.3) | 35.9 (15.1) | 0.99 | 35.9 (15.9) | 35.9 (13.7) | 0.99 |
| Hearing loss asymmetry (dB) | 5.9 (9.2) | 8.4 (16.7) | 0.2 | 6.8 (12.7) | 6.0 (9.6) | 0.55 |
| *Hearing loss duration (years) | 12.3 (14.6) | 11.9 (12.3) | 0.8 | 12.2 (14.8) | 11.9 (12.2) | 0.85 |
| Comorbidities | ||||||
| ARS score | 1.0 (1.5) | 1.6 (2.0) | 0.03 | 0.9 (1.5) | 1.7 (2.0) | 0.001 |
| Diabetes | 14.8% | 18.4% | 0.46 | 12.8% | 22.2% | 0.04 |
| Stroke | 3.6% | 6.3% | 0.36 | 4.3% | 5.6% | 0.64 |
| Cognitive decline | 1.8% | 2.5% | 0.74 | 1.6% | 3.3% | 0.36 |
| Previous falls | 1.4% | 7.6% | 0.007 | 1.6% | 6.7% | 0.03 |
| *Positional dizziness | 15.2% | 10.8% | 0.27 | 5.0% | 26.9% | <0.001 |
| *Use glasses | 78.7% | 70.5% | 0.14 | 76.5% | 76.1% | 0.94 |
indicates any characteristic collected by participant self-report. Continuous variables are shown by their means (standard deviations) and categorical variables are shown by proportion. P-values are for Welch’s t-tests (continuous variables) and chi-squared tests (categorical variables), significant p-values are in bold. ARS=Anticholinergic Risk Scale, dB=decibel, HA=Hearing Aid.
The results of each of the logistic regression models (crude, adjusted, stepwise) for both fall outcomes, as separated by any hearing aid use, are shown in Table 3. After adjusting for age, ARS, sex, and hearing loss severity, results demonstrate significantly lower odds of falling for hearing aid users compared to non-users (OR 0.48 [0.26–0.90]) and an even greater reduction in odds of falling for consistent users (OR 0.35 [0.19–0.67]). This significance remains even after considering all covariates in the stepwise model adjusting for age, ARS, previous falls, and hearing asymmetry in those with any hearing aid use (OR 0.51 [0.28–0.93]) and, to a greater extent, in consistent hearing-aid users (OR 0.43 [0.24–0.77]).
TABLE 3.
Comparison of logistic regression models for each exposure group and for each outcome (fall prevalence and fall risk).
| Any HA use Odds ratio (95% CI) (Referenced to No HA Use) | Consistent HA use Odds ratio (95% CI) (Referenced to No/Inconsistent HA Use) | |
|---|---|---|
|
| ||
| Fall Prevalence | ||
| Unadjusted/crude model | 0.50 (0.29–0.85) p=0.01 |
0.40 (0.24–0.68) p<0.001 |
| * Adjusted model | 0.48 (0.26–0.90) p=0.02 |
0.35 (0.19–0.67) p<0.001 |
| † Stepwise model | 0.51 (0.28–0.93) p=0.03 |
0.43 (0.24–0.77) p=0.005 |
| Fall Risk | ||
| Unadjusted/crude model | 0.42 (0.25–0.70) p<0.001 |
0.43 (0.26–0.71) p<0.001 |
| * Adjusted model | 0.36 (0.19–0.66) p<0.001 |
0.32 (0.12–0.59) p<0.001 |
| ‡ Stepwise model | 0.41 (0.22–0.76) p<0.004 |
0.38 (0.21–0.69) p<0.001 |
Model adjusted for age, ARS, sex and hearing loss severity.
Model adjusted for age, ARS, previous falls and hearing loss asymmetry.
Model adjusted for age, ARS, previous falls, dizziness and diabetes.
HA=hearing aid; ARS=Anticholinergic Risk Scale.
Table 3 also shows the results of all models separated by hearing aid use for the “fall risk” outcome. Consistent with fall-prevalence models, all models find significantly lower odds of being classified as “at risk for falls” for both hearing aid status groups. The adjusted model shows that any hearing aid use is associated with 64% lower odds of being at risk for falls (OR 0.36 [0.19–0.66]), and consistent hearing-aid use is associated with 68% lower odds of being at risk for falls (OR 0.32 [0.12–0.59]). Similarly, adjusting for age, ARS, previous falls, dizziness, and diabetes, the stepwise model demonstrates that those with any hearing aid use have significantly lower odds of being at risk for falls (OR 0.41 [0.22–0.76]), as do consistent hearing-aid users (OR 0.38 [0.21–0.69]).
Comparison of logistic regression models for both fall outcomes as stratified by consistency of hearing aid use is shown in Table 4. Compared to no hearing aid use, inconsistent users show no significant difference in either fall prevalence or fall risk, whereas consistent hearing aid users do have significantly lower odds of experiencing a fall (OR 0.37 [0.19–0.73] or being at risk for a fall (OR 0.28 [0.14–0.54]), suggesting a potential dose-response relationship.
TABLE 4.
Comparison of adjusted logistic regression models stratified by consistency of hearing aid use for each outcome (fall prevalence and fall risk).
| No use (n=95) Odds ratio (95% CI) | Inconsistent use (n=23) Odds ratio (95% CI) | Consistent use (n=181) Odds ratio (95% CI) | |
|---|---|---|---|
| Fall Prevalence | |||
| Adjusted model | Reference | 1.44 (0.50–4.12) p=0.46 |
0.37 (0.19–0.73) p=0.004 |
| Fall Risk | |||
| Adjusted model | Reference | 0.94 (0.33–2.72) p=0.91 |
0.28 (0.14–0.54) p<0.001 |
Models are adjusted for age, ARS, sex and hearing loss severity
Sensitivity analysis
The regression modelling process was repeated by running the adjusted models using Poisson regression with robust standard errors; similar results (data not shown) were achieved. All p-values were identical for both logistic and Poisson regression models, but, as expected given our high outcome prevalence, our point estimates were closer to the null in Poisson models: fall-prevalence outcome for consistent hearing aid users found a prevalence ratio of 0.72 compared to 0.35 in logistic regression models, and fall-risk outcome for consistent hearing aid users found a prevalence ratio of 0.73 compared to 0.32 in logistic regression models.
Discussion
All models, regardless of analysis method (covariates selected a priori, stepwise process, Poisson regression), showed hearing aid users had significantly lower odds of experiencing either fall outcome. While any hearing aid use was significantly associated with lower fall outcomes, the association was stronger (lower point estimates and smaller p-values) for those who reported consistent hearing aid use, which may suggest a quasi-dose-response relationship. Of the three mechanisms proposed for the relationship between hearing loss and increased fall risk, two are addressed by hearing aid use. Our findings that hearing aid use is associated with significantly lower odds of falling and fall risk suggest that the reduction in communicative cognitive load and/or improved access to environmental spatial cues at least partially contribute to the underlying processes of this relationship.
Our findings differ from several of the previous studies investigating this question. We limited our study sample to only those with hearing loss. In doing so, we were able to more effectively evaluate the association of hearing aid use and falls independent from the presence of hearing impairment. Several of the previous studies on the topic compared fall rates in hearing aid users to those with normal or self-perceived “good” hearing [19, 20, 23]. A non-significant finding using a “good hearing” comparison group would suggest similar conclusions to our findings—that hearing aid use modifies fall risk in those at increased risk due to hearing loss, bringing them to similar levels as normal hearing counterparts. Conversely, our comparison group all had hearing loss to a degree that made them hearing aid candidates (i.e., aidable hearing loss). This exclusion difference may offer an explanation as to why our results differ from those studies showing non-significance.
Table 4 demonstrates that inconsistent hearing aid users did not significantly differ from non-users. Since most of the other studies on this topic did not account for consistency of hearing aid use [18, 19, 21, 22], samples containing a higher number of inconsistent users could have contributed to the non-significant findings.
While every effort was made to collect and adjust for potential risk factors for falls, as with any non-randomized study, there is still the possibility that other variables not collected could account for at least some of the observed effects. Individuals who have the means to obtain hearing aids may also have greater access to other medical care [32]; consequently, they may have fewer comorbidities that would otherwise increase their risk of falling. However, for the health metrics collected, hearing-aid users do not appear to be “healthier” than non-users. When comparing hearing aid status groups, there were not significant differences in ARS scores or proportion with diabetes, cognitive decline, or previous falls. Conversely, the hearing aid users were significantly older than non-users, more had experienced a stroke, and more had significantly greater hearing loss and longer duration of hearing loss.
Study Limitations
Since our study design was cross-sectional, we are limited to evaluating for associations between hearing aid use and falls and cannot determine causality. The results did show that our participants reported higher hearing aid usage than the general population, which is likely due to the sampling of patients from an audiology/otolaryngology practice rather than the general population. Nevertheless, oversampling of hearing aid users likely would not result in differential misclassification assuming the overall proportion of hearing aid users that experience a fall is the same regardless of the total number of hearing aid users surveyed. This result does, however, suggest that our findings are only generalizable to the typical patient population of an audiology/otolaryngology practice, not community dwelling older adults as a whole.
Selection bias could also have been introduced from the electronic collection of most survey responses. There is evidence that age does not significantly differ in those that complete a paper survey compared to an electronic survey [33]; therefore, we do not suspect the age of our respondents was affected by collection mode. However, research has shown survey response varies by socioeconomic status and that more vulnerable populations are less likely to respond to research surveys [34]. Therefore, we cannot rule out the possibility that selection bias toward more affluent individuals exists in the current study given an email address was required to respond. This may mean only those with higher socioeconomic status participated and that these individuals may be “healthier” than the collective general population. Additionally, the survey took place during the height of the Covid epidemic which may have influenced response rates.
Self-reported outcomes are inherently subject to recall bias. More than 26% of survey respondents reported a fall in the past 6 months, which is similar to rates from other studies [1, 2], although those studies asked about falls occurring in the past 12 months. Given that the FRQ wording specifically asks about falls in the past 6 months, the cross-sectional nature of our study makes it difficult to compare fall prevalence to studies that ask about falls in the past year. However, recall bias related to recollection of a specific date when an event occurred is likely a contributing factor (i.e., respondents may be answering “yes” that they have had a fall even though it occurred more than 6 months ago).
Finally, hearing-aid-use data was also self-reported. Many hearing aids carry datalogging functions quantifying hours worn, but these data were generally not available for our patients for two reasons: 1) many respondents did not receive their hearing-aid services through University of Colorado Hospital, and 2) for those that did use UCH audiology, datalogging was not consistently documented in audiologic notes.
Conclusions
Our results indicate that hearing aid use is associated with lower odds of falling and reduction in fall risk in older adults with aidable sensorineural hearing loss, and that the association is stronger for those that use hearing aids for at least 4 hours/day on average. These findings provide cross-sectional evidence that is relevant to audiological clinical practice and in fall prevention programs. Audiologists can more confidently discuss with patients the association between hearing aid use and the probability of falling as well as encourage consistent hearing aid use of at least 4 hours each day. Finally, even though our results cannot determine causality, they do add to the evidence suggesting hearing loss may be a modifiable risk factor for falls [35]. Healthcare providers might consider adding a hearing screening to their assessments, referring those who do not pass to an audiologist and discussing the potential benefits of addressing hearing loss to reduce fall risk.
Supplementary Material
Key Points:
Use of hearing aids is associated with significantly reduced odds of both falling and risk for falls in older adults with hearing loss.
The association was strongest for consistent hearing aid users (at least 4 hours/day for 1 year).
Why does it matter?
Understanding the relationship between hearing aid use and falls helps clinicians counsel patients about potentially modifiable fall-risk factors.
Acknowledgements
This article has not been previously published and is not being considered for publication elsewhere, in whole or in part, in any language. The authors would like to thank Drew Bixby for his excellent editorial assistance.
Future Research
Since the results of this study are only able to show an association between hearing aid use and reduced odds of falling/fall risk, determination of causality is still needed. A randomized controlled trial (RCT) would be useful to better elucidate if hearing aid use causes the reduced fall prevalence and fall risk observed in our study. In addition, other cross-sectional studies on the topic may want to survey individuals from the broader community of older adults to improve external validity and should aim to capture information related to SES.
Sponsor’s Role
No funding was obtained for this study. LLC’s graduate program was supported by in part by NIH/NCATS Colorado CTSA Grant (UL1 TR002535) during her graduate study. Contents are the author’s sole responsibility and do not necessarily represent official NIH views.
Footnotes
Supplemental Material
Further comparison of inconsistent and consistent hearing aid users. Results of Welch’s t-tests for each of the collected covariates and results from the same logistic regression modeling presented in the manuscript comparing inconsistent users to consistent users (reference).
Conflict of interest
All authors report no relevant disclosures.
References
- [1].Bergen G, Stevens MR, and Burns ER (2014) Falls and Fall Injuries Among Adults Aged >/=65 Years - United States. MMWR: Morbidity and Mortality Weekly Report, 65 (37), 993–998. [DOI] [PubMed] [Google Scholar]
- [2].Florence CS, Bergen G, Atherly A, Burns E, Stevens J, and Drake C. (2018) Medical Costs of Fatal and Nonfatal Falls in Older Adults. Journal of the American Geriatrics Society, 66 (4), 693–698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Burns E. and Kakara R. (2018). Deaths from Falls Among Persons Aged ≥65 Years — United States, 2007–2016. MMRW: Morbidly and Mortality Weekly Report, 67, 509–514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Galet C, Zhou Y, Eyck PT, and Romanowski KS (2010) Fall injuries, associated deaths, and 30-day readmission for subsequent falls are increasing in the elderly US population: a query of the WHO mortality database and National Readmission Database from. Clinical Epidemiology, 10, 1627–1637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Deandrea S, Lucenteforte E, Bravi F, Foschi R, Vecchia CL, and Negri E. (2010) Risk factors for falls in community-dwelling older people: a systematic review and meta-analysis. Epidemiology, 21 (5), 658–668. [DOI] [PubMed] [Google Scholar]
- [6].Lord S. and Dayhew J. (2001) Visual Risk Factors for Falls in Older People. Journal of the American Geriatrics Society (JAGS), 49 (5), 508–515. [DOI] [PubMed] [Google Scholar]
- [7].Klein BEK, Klein R, Lee KE, and Cruickshanks KJ (1998) Performance-based and self-assessed measures of visual function as related to history of falls, hip fractures, and measured gait time: The Beaver Dam Eye Study. Ophthalmology, (1), 160–164. [DOI] [PubMed] [Google Scholar]
- [8].Lin FR and Ferrucci L. (1960) Hearing Loss and Falls Among Older Adults in the United States. Archives of internal medicine, 172 (4), 369–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Jiam NT, Li C, and Agrawal Y. (2016) Hearing loss and falls: A systematic review and meta-analysis. Laryngoscope, 126 (11), 2587–2596. [DOI] [PubMed] [Google Scholar]
- [10].Whitney SL, Marchetti GF, and Schade AI (2006) The relationship between falls history and computerized dynamic posturography in persons with balance and vestibular disorders. Archives of Physical Medicine and Rehabilitation, 87 (3), 402–407. [DOI] [PubMed] [Google Scholar]
- [11].Agrawal Y, Carey JP, Santina CCD, Schubert MC, and Minor LB (1960) Disorders of Balance and Vestibular Function in US Adults: Data From the National Health and Nutrition Examination Survey. Archives of internal medicine, (10), 938–944. [DOI] [PubMed] [Google Scholar]
- [12].Creaby MW and Cole MH (2018) Gait characteristics and falls in Parkinson’s disease: A systematic review and meta-analysis. Parkinsonism & Related Disorders, 57, 1–8. [DOI] [PubMed] [Google Scholar]
- [13].Tinetti ME, Speechley M, and Ginter SF (1988) Risk factors for falls among elderly persons living in the community. New England Journal of Medicine, 319 (26), 1701–1707. [DOI] [PubMed] [Google Scholar]
- [14].Yang Y, Hu X, Zhang Q, and Zou R. (2016) Diabetes mellitus and risk of falls in older adults: a systematic review and meta-analysis. Age and Ageing, 45 (6), 761–767. [DOI] [PubMed] [Google Scholar]
- [15].Updated AGS Beers Criteria® for Potentially Inappropriate Medication Use in Older Adults. (2019) Journal of the American Geriatrics Society, 67 (4), 674–694. [DOI] [PubMed] [Google Scholar]
- [16].Dillon CF, Gu Q, Hoffman HJ, and Ko CW (1999) Vision, hearing, balance, and sensory impairment in Americans aged 70 years and over: United States. NCHS Data Brief, (31), 1–8. [PubMed] [Google Scholar]
- [17].Chu SP, Kelsey JL, Keegan TH, Sternfeld B, Prill M, Quesenberry CP, and Sidney S. (2004) Risk factors for proximal humerus fracture. American Journal of Epidemiology, 160 (4), 360–367. [DOI] [PubMed] [Google Scholar]
- [18].Criter RE and Gustavson M. (2020) Subjective Hearing Difficulty and Fall Risk. Am J Audiol, 29 (3), 384–390. [DOI] [PubMed] [Google Scholar]
- [19].Gopinath B, Mcmahon CM, Burlutsky G, and Mitchell P. (2016) Hearing and vision impairment and the 5-Year incidence of falls in older adults. Age and Ageing, 45 (3), 353–358. [DOI] [PubMed] [Google Scholar]
- [20].Sprince NL, Zwerling C, Lynch CF, Whitten PS, Thu K, Gillette PP, Alavanja C, M. (2003) Risk factors for falls among Iowa farmers: a case-control study nested in the Agricultural Health Study. American Journal of Indus-trial Medicine, 44 (3), 265–272. [DOI] [PubMed] [Google Scholar]
- [21].Kamil RJ, Betz J, Powers BB, Pratt S, Kritchevsky S, Ayonayon HN, Lin,.., and R F. (2016) Association of Hearing Impairment With Incident Frailty and Falls in Older Adults. Journal of Aging and Health, 28 (4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Powell DS, Morales EEG, Pletnikova S, Deal JA, and Reed NS (2021) Self-Report Hearing and Injury or Falls in Older Adults from the National Health and Information Survey. Seminars in Hearing, 42 (1), 66–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Riska KM, Peskoe SB, Kuchibhatla M, Gordee A, Pavon JM, Kim SE, Smith, .., and L S. (2021) Impact of Hearing Aid Use on Falls and Falls-Related Injury: Results From the Health and Retirement Study. Ear and Hearing. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Mahmoudi E, Basu T, Langa K, Mckee MM, Zazove P, Alexander N, and Kamdar N. (2019) Can Hearing Aids Delay Time to Diagnosis of Dementia, Depression, or Falls in Older Adults. Journal of the American Geriatrics Society, 67 (11), 2362–2369. [DOI] [PubMed] [Google Scholar]
- [25].Tiase VL, Tang K, Vawdrey DK, Raso R, Adelman JS, Yu SP, Lalwani, .., and K A. (2020) Impact of Hearing Loss on Patient Falls in the Inpatient Setting. American Journal of Preventive Medicine, 58 (6), 839–844. [DOI] [PubMed] [Google Scholar]
- [26].Rubenstein LZ, Vivrette R, Harker JO, Stevens JA, and Kramer BJ (2011) Validating an evidence-based, self-rated fall risk questionnaire (FRQ) for older adults. J Safety Res, 42 (6), 493–499. [DOI] [PubMed] [Google Scholar]
- [27].Vestergaard M D. (2006). Self-report outcome in new hearing aid users: longitudinal trends and relationships between subjective measures of benefit and satisfaction. International Journal of Audiology, 45(7), 382–392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Rudolph JL, Salow MJ, Angelini MC, and Mcglinchey RE (2008) The anti- cholinergic risk scale and anticholinergic adverse effects in older persons. Archives of Internal Medicine, 168 (5), 508–513. [DOI] [PubMed] [Google Scholar]
- [29].Assi L, Reed N, Nieman C, and Willink A. (2021) Factors Associated with Hearing Aid Use Among Medicare Beneficiaries. Innovation in Aging, 5(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Butler AA, Lord SR, Taylor JL, and Fitzpatrick RC (2015) Ability Versus Hazard: Risk-Taking and Falls in Older People. The Journals of Gerontology: Series A, 70(5), 628–634. [DOI] [PubMed] [Google Scholar]
- [31].Gispen FE, Chen DS, Genther DJ, and Lin FR (2014) Association between hearing impairment and lower levels of physical activity in older adults. Journal of the American Geriatrics Society, 62 (8), 1427–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].McMaughan DJ, Oloruntoba O, Smith ML Socioeconomic Status and Access to Healthcare: Interrelated Drivers for Healthy Aging. Front Public Health. 2020. Jun 18;8:231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Muehlhausen W, Doll H, Quadri N, Fordham B, O’Donohoe P, Dogar N, & Wild DJ (2015). Equivalence of electronic and paper administration of patient-reported outcome measures: a systematic review and meta-analysis of studies conducted between 2007 and 2013. Health Qual Life Outcomes, 13, 167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Booker QS, Austin JD, & Balasubramanian BA (2021). Survey strategies to increase participant response rates in primary care research studies. Family Practice, 38(5), 699–702 [DOI] [PubMed] [Google Scholar]
- [35].Ekstrom E, Parker EM, Skakya I, and Lee R. (2021) Coordinated Care Plan to Prevent Older Adult Falls. Edition 1.1. Atlanta, GA. National Center for Injury Prevention and Control, Center for Disease Control and Prevention, 46–48. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.