Abstract
The bactericidal activities of vancomycin against two reference strains and two clinical isolates of Staphylococcus aureus and Staphylococcus epidermidis were studied with five different concentrations ranging from 2× to 64× the MIC. The decrease in the numbers of CFU at 24 h was at least 3 log10 CFU/ml for all strains. No concentration-dependent killing was observed. The postantibiotic effect (PAE) was determined by obtaining viable counts for two of the reference strains, and the viable counts varied markedly: 1.2 h for S. aureus and 6.0 h for S. epidermidis. The determinations of the PAE, the postantibiotic sub-MIC effect (PA SME), and the sub-MIC effect (SME) for all strains were done with BioScreen C, a computerized incubator for bacteria. The PA SMEs were longer than the SMEs for all strains tested. A newly developed in vitro kinetic model was used to expose the bacteria to continuously decreasing concentrations of vancomycin. A filter prevented the loss of bacteria during the experiments. One reference strain each of S. aureus and S. epidermidis and two clinical isolates of S. aureus were exposed to an initial concentration of 10× the MIC of vancomycin with two different half-lives (t1/2s): 1 or 5 h. The post-MIC effect (PME) was calculated as the difference in time for the bacteria to grow 1 log10 CFU/ml from the numbers of CFU obtained at the time when the MIC was reached and the corresponding time for an unexposed control culture. The difference in PME between the strains was not as pronounced as that for the PAE. Furthermore, the PME was shorter when a t1/2 of 5 h (approximate terminal t1/2 in humans) was used. The PMEs at t1/2s of 1 and 5 h were 6.5 and 3.6 h, respectively, for S. aureus. The corresponding figures for S. epidermidis were 10.3 and less than 6 h. The shorter PMEs achieved with a t1/2 of 5 h and the lack of concentration-dependent killing indicate that the time above the MIC is the parameter most important for the efficacy of vancomycin.
Vancomycin has been used for the treatment of severe infections caused by gram-positive bacteria since the 1950s. Its use has increased during the last decade due to the emergence of multiple antibiotic resistance in staphylococci, pneumococci, and enterococci. Even though vancomycin has been in clinical use for a long period of time, its pharmacodynamic properties are still incompletely known. The terminal half-life (t1/2) of vancomycin in serum is long, between 3 and 9 h, and the recommended dosing schedules are 1 g every 12 h or 500 mg every 6 h (14, 16–18). These recommended dosing regimens generally provide a trough concentration of approximately 5× the MIC for the infecting pathogen (7, 10, 20). The rate and extent of bacterial killing, the postantibiotic effect (PAE), and the postantibiotic sub-MIC effect (PA SME) (26, 27) provide a more accurate description of the antimicrobial activity than the MIC alone and thus offer a more rational basis for determining optimal dosing schedules. Another recently described pharmacodynamic parameter which may be important when determining dosing schedules for antibiotics is the post-MIC effect (PME) (22). This parameter is studied in an in vitro kinetic model, in which bacteria can be exposed to antibiotic concentrations with kinetics that mimic the kinetics of the drug in human serum. The PME represents the difference in time for the numbers of CFU to increase 1 log10/ml compared with the values obtained at the time when the antibiotic concentration has declined to the MIC and the corresponding time for a control culture grown in a test tube without antibiotic.
The aim of the present investigation was to study the rate and extent of bacterial killing, the PAE, PA SME, and PME of vancomycin against different strains of Staphylococcus aureus and Staphylococcus epidermidis.
MATERIALS AND METHODS
Bacterial cultures and media.
The following strains were investigated: S. aureus ATCC 29213 (methicillin susceptible), Colindale Col. 1841 (methicillin resistant), 352-3028 (methicillin susceptible), and 344-1011 (methicillin resistant) and S. epidermidis ATCC 29886 (methicillin susceptible), ATCC 29887 (methicillin resistant), 928-6002 (methicillin resistant), and 931-5028 (methicillin susceptible). The strains were grown in Todd-Hewitt broth at 37°C for 6 h before the experiments to obtain an exponential growth phase.
Determination of vancomycin concentrations.
Vancomycin was provided as a reference powder from Eli Lilly Sweden AB, Stockholm, Sweden. The drug concentrations were assayed by using a commercial fluorescence polarization immunoassay (TDXFLX; Abbott Laboratories, North Chicago, Ill.). The within-run coefficient of variation (CV) for vancomycin at a concentration of 7 μg/ml was 2.45%, and the within-run CV for vancomycin at a concentration of 75 mg/ml was 1.97%. The between-day CVs at these concentrations were 2.98 and 1.58%, respectively.
Determination of MICs.
The MICs for all strains were determined by the macrodilution technique in 2 ml of Todd-Hewitt broth by using twofold dilutions with an inoculum of approximately 105 CFU/ml. The MIC was defined as the lowest concentration of the antibiotic allowing no visible growth after 20 h of incubation (8). In addition, the MICs were also determined for all strains in the BioScreen C (Lab Systems, Helsinki, Finland) (21) and were defined as the lowest concentration of the antibiotic that prevented growth for 20 h, as measured by determining the optical density (OD). The lowest detectable OD for S. aureus and S. epidermidis corresponded to approximately 5 × 105 CFU/ml. Determinations of MICs were performed at least in duplicate on separate occasions.
Determination of killing.
All strains, at an inoculum of approximately 5 × 105 CFU/ml, were incubated in tubes with vancomycin at concentrations of 2, 4, 8, 16, and 64× the MIC for 24 h. A growth control was also included. The tubes were incubated at 37°C. Samples were drawn at 0, 3, 6, 9, 12, and 24 h and, if necessary, were diluted in phosphate-buffered saline and spread onto agar plates, the plates were incubated at 37°C, and the colonies were counted after 24 h. Determinations of the numbers of CFU were based on plates with 10 to 500 colonies per plate. All experiments were performed in triplicate.
Induction of the PA phase.
The cultures in the exponential growth phase were diluted to obtain a bacterial density of approximately 5 × 107 CFU/ml. Four-milliliter aliquots were then exposed to 10× the MIC of vancomycin for 2 h in 10-ml, round-bottom glass tubes. Control cultures were left untreated. The exposed cultures and the controls were then washed twice by centrifugation at 1,500 × g for 10 min and were diluted in fresh broth to obtain a bacterial density of approximately 105 CFU/ml.
Determination and definition of the PAE with viable counts.
A PA phase was induced as described above with S. aureus ATCC 29213 and S. epidermidis ATCC 29886, and the cultures were then incubated at 37°C. Samples were drawn every 1 to 3 h for 11 h, and at 24 h samples were cultured as described above. The experiments were performed in triplicate for both strains.
The PAE was defined as described by Craig and Gudmundsson (5) as T − C, where T is the time required for the viable counts of the exposed bacteria to increase by 1 log10 above the counts observed immediately after washing and C is the corresponding time for the unexposed controls.
Determination and calculation of the PAE, PA SME, and SME in BioScreen C.
Experiments were performed in triplicate with S. aureus ATCC 29213 and S. epidermidis ATCC 29886 and once each with S. aureus Colindale Col. 1841, 352-3028, and 344-1011, and S. epidermidis ATCC 29887, 928-6002, and 931-5028. A PA phase was induced as described above. For measurement of PAE and PA SME, 360-μl volumes of broth with no antibiotic or with a concentration of 0.1 to 0.9× the MIC of vancomycin were placed in wells with a volume of 400 μl. Forty microliters of the cultures in the PA phase was then added, and the wells were incubated in the BioScreen C for 20 h at 37°C. To study the SME, previously untreated controls were similarly exposed to 0.0 to 0.9× the MIC of vancomycin. The absorbance (OD) was measured every 10 min during the experiment. The results were processed in the BioScreen C and were printed out as growth curves. At least three different dilutions of the control cultures were made in order to obtain a control with an inoculum as close as possible to that of the cultures exposed to the antibiotic. The PAE was defined as the difference in time for the exposed and the unexposed cultures to grow to a chosen point (A50) on the absorbance curve. A50 was defined as 50% of the maximum absorbance of the control cultures. PA SME and SME were likewise defined as the difference in time for the exposed culture and the control culture to reach an A50 (21).
In vitro kinetic model.
A recently described in vitro kinetic model was used (22). It consists of a spinner flask with a 0.45-μm-pore-size filter membrane and a prefilter fitted between the upper and the bottom parts. A magnetic stirrer ensures the homogeneity of the culture and prevents membrane pore blockage. The original model contains a stirrer with a magnet covered in Teflon. However, in preliminary experiments with this model, when the staphylococci were exposed to a constant concentration of vancomycin, regrowth occurred, even though the concentration was 10× the MIC. Staphylococci are known to adhere to Teflon (19, 28, 31), and we suspected that the bacteria were adhering to the surface of the stirrer. A new stirrer in which the magnet was encased in glass was therefore constructed (AB Wiklunds Glas Instrument, Stockholm, Sweden). Subsequent experiments with this stirrer and 10× the MIC of vancomycin showed no regrowth of bacteria during 24 h.
In one of the side arms of the culture vessel, a silicon membrane was inserted to enable repeated sampling. The other arm was connected with a thin plastic tube to a vessel containing fresh medium. The medium was removed from the culture flask, through the filter, at a constant rate with a pump. Fresh sterile medium was sucked into the flask at the same rate by the negative pressure that built up inside the culture vessel. The antibiotic was added to the vessel and was eliminated at a constant rate according to the first-order kinetics C = Co · e−kt, where Co is the initial antibiotic level, C is the antibiotic level at time t, k is the rate of elimination, and t is the time that has elapsed since the addition of antibiotic. The apparatus was placed in a thermostatic room at 37°C during the experiments. The culture vessel was sterilized by autoclaving between every experiment.
Definition and determination of PME.
The PME was defined as the difference between the time needed for the numbers of CFU in the culture vessel to increase 1 log10/ml from the numbers obtained at the time when the antibiotic concentration had declined to the MIC and the corresponding time for a control culture grown in a test tube without antibiotic (22).
S. aureus ATCC 29213, 344-1011, and 352-3038 and S. epidermidis ATCC 29886 were exposed in the kinetic model to an initial concentration of 10× the MIC of vancomycin with a t1/2 of 1 or 5 h. Samples for bacterial counts and antibiotic concentrations were drawn at appropriate intervals during the experiments. The samples were cultured as described above. Samples from the waste were also drawn at intervals during the experiments to ensure that there was no filter leakage. The experiments were performed in triplicate with the reference strains and once each with the clinical isolates.
RESULTS
MICs.
The MICs were 2 mg/liter for all strains except S. aureus Colindale Col. 1841 and S. epidermidis ATCC 29887, for which the MICs were 4 mg/liter. Identical results were obtained by the macrodilution method and with BioScreen C.
Antibiotic concentration.
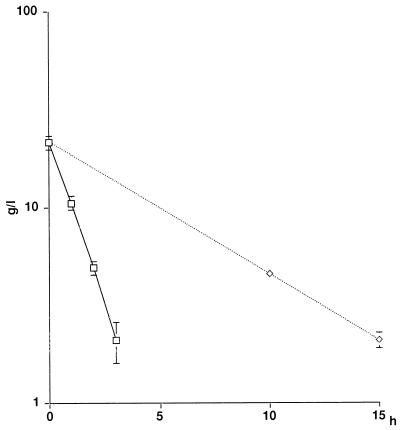
The concentrations of vancomycin obtained in the in vitro kinetic model showed little variation between experiments (Fig. 1).
FIG. 1.
Concentration-time curves from the experiments with an initial concentration of 10× the MIC of vancomycin and t1/2s of 1 h (□) and 5 h (◊). Values are the means of six experiments. Bars indicate standard deviations.
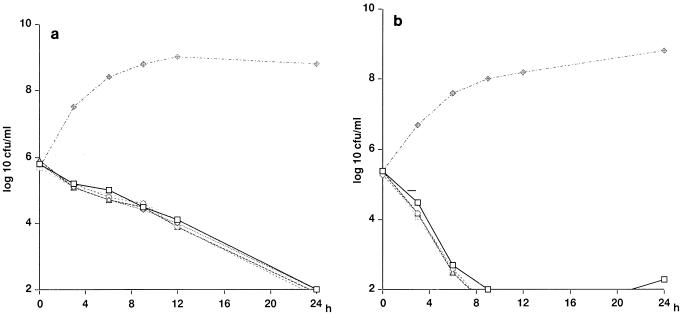
Killing curves.
No concentration-dependent killing of any of the strains tested was detected (Fig. 2a and b). The reductions in the numbers of log10 CFU per milliliter at 3 and 9 h with a concentration of 8× the MIC of vancomycin are listed in Table 1. The killing rate was low for all strains. However at 24 h, a reduction of >3 log CFU/ml was achieved for all strains with all concentrations. The only exception was S. epidermidis ATCC 29886 exposed to 2× the MIC, which showed a reduction of >3 log CFU/ml after 9 h, but regrowth occurred at between 12 and 24 h in two of three experiments (Fig. 2b).
FIG. 2.
(a) Killing curves for S. aureus ATCC 29213 exposed to 2, 4, 8, 16, and 64× the MIC of vancomycin. (b) Killing curves for S. epidermidis ATCC 29886 exposed to 2, 4, 8, 16, and 64× the MIC of vancomycin. Values are the means of three experiments. Standard deviations were less than 0.4 for all measurements.
TABLE 1.
Reduction in bacterial numbers at 3 and 9 h with a concentration of 8× the MIC of vancomycin
| Strain | Mean (range) reduction (log10 CFU/ml) at the following timesa:
|
|
|---|---|---|
| 3 h | 9 h | |
| S. aureus ATCC 29213 | 0.5 (0.4–0.6) | 1.2 (1.2) |
| S. aureus Colindale Col. 1841 | 1.2 (1.0–1.7) | 2.9 (2.5–3.1) |
| S. aureus 352-3028 | 0.4 (0.3–0.5) | 2.7 (2.3–3.1) |
| S. aureus 344-1011 | 0.5 (0.4–0.5) | 2.0 (1.8–2.3) |
| S. epidermidis ATCC 29886 | 1.1 (0.9–1.4) | 3.3 (2.8–3.6) |
| S. epidermidis ATCC 29887 | 0.9 (0.7–1.0) | 3.3 (3.1–3.4) |
| S. epidermidis 931-5028 | 0.2 (0.0–0.3) | 2.2 (2.0–2.4) |
| S. epidermidis 928-6002 | 0.7 (0.6–0.8) | 3.4 (3.1–3.9) |
Values are the means of three experiments. Results below the limit of detection were given a value of 2 log10 CFU/ml.
PAEs.
There was a good correlation between the PAEs determined by obtaining viable counts and those obtained in BioScreen C. The PAE for S. aureus ATCC 29213 was 1.2 h (range, 0.6 to 1.9 h) by the viable counting method and 1.6 h (range, 1.3 to 2.0 h) in BioScreen C. For S. epidermidis ATCC 29886 the corresponding figures were 6.0 h (range, 5.7 to 6.5 h) and 4.8 h (range, 4.3 to 5.4 h). The PAEs for all strains in BioScreen C are presented in Table 2.
TABLE 2.
PAE and PA SME after exposure to 10× the MIC of vancomycin for 2 h for S. aureus and S. epidermidis strains studied in BioScreen C
| Strain | PAE (h) | PA SME (h) with the following multiples of the MIC:
|
|||||
|---|---|---|---|---|---|---|---|
| 0.1 | 0.2 | 0.3 | 0.4 | 0.5 | 0.6 | ||
| S. aureus ATCC 29213a | 1.6 (1.3–2.0) | 3.1 (2.4–3.6) | 5.3 (4.6–6.1) | 8.2 (7.3–9.6) | 10.0 (9.1–11.0) | 13.3 (12.4–14.7) | NCb (13.9–>20) |
| S. epidermidis ATCC 29886a | 4.8 (4.3–5.4) | 9.2 (7.4–10.1) | NC (11.3–>12) | ||||
| S. aureus | |||||||
| 1841 | 2.0 | 7.3 | 10.0 | 11.6 | >13.0 | ||
| 3028 | 0.7 | 2.3 | 4.6 | 10.7 | >14.6 | ||
| 1011 | 1.8 | 3.3 | 5.7 | 7.6 | 11.1 | >16 | |
| S. epidermidis | |||||||
| ATCC 29887 | 2.6 | 10.0 | >11 | ||||
| 6002 | 2.1 | 6.0 | 10.3 | >10.3 | |||
| 5028 | 1.4 | 10.0 | 13.8 | >14.0 | |||
For these strains, values are means (ranges).
NC, not calculated.
PA SMEs and SMEs.
The PA SMEs and SMEs in BioScreen C for the different strains are presented in Tables 2 and 3. The PA SMEs were very long for all strains tested, while the SMEs were shorter. Long SMEs were seen, however, when S. aureus Colindale Col. 1841 and S. epidermidis ATCC 29887, 928-6002, and 931-5028 were challenged with vancomycin at sub-MICs greater than 0.4 to 0.5× the MIC. No regrowth could then be demonstrated for 20 h in BioScreen C, indicating that the true MICs for these strains were lower than those determined with twofold serial dilutions.
TABLE 3.
SME of vancomycin for S. aureus and S. epidermidis strains studies in BioScreen C
| Strain | SME (h) at the following multiples of the MIC:
|
|||||
|---|---|---|---|---|---|---|
| 0.1 | 0.2 | 0.3 | 0.4 | 0.5 | 0.6 | |
| S. aureus ATCC 29213a | 0.1 (0.0–0.3) | 0.3 (0.1–0.4) | 0.6 (0.3–1.0) | 1.9 (1.1–2.9) | 5.9 (3.7–9.0) | NCb (7.0–15.8) |
| S. epidermidis ATCC 29886a | 0.1 (0.0–0.3) | 0.3 (0.0–0.6) | 0.8 (0.0–1.3) | 1.8 (1.0–2.3) | 3.4 (2.0–4.3) | 5.9 (3.3–7.7) |
| S. aureus | ||||||
| 1841 | 0.1 | 0.9 | 10.0 | >13.1 | >13 | >13 |
| 3028 | 0.1 | 1.0 | 1.7 | 2.7 | 5.6 | 8.1 |
| 1011 | 0.0 | 0.0 | 0.3 | 1.3 | 4.6 | 10.7 |
| S. epidermidis | ||||||
| ATCC 29887 | 4.3 | 5.6 | 6.7 | 10.7 | >10.9 | >10.9 |
| 6002 | 3.3 | 3.3 | 4.6 | 7.0 | >9.9 | >9.9 |
| 5028 | 0.1 | 0.9 | 2.9 | >14.1 | >14.1 | >14.1 |
For these strains, values are means (ranges).
NC, not calculated.
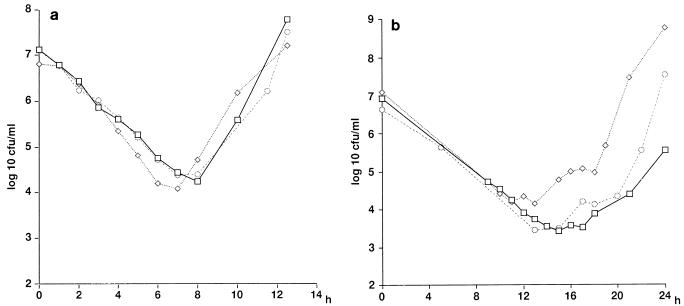
PMEs.
The PMEs for S. aureus ATCC 29213 when t1/2s of vancomycin of 1 h and 5 h were simulated in the kinetic model were 6.5 h (range, 5.1 to 8.1 h) and 3.6 h (range, 2.6 to 4.6 h), respectively (Fig. 3a and b). The PMEs for S. aureus 344-1011 and 352-3038 were 5.6 and 6.3 h, respectively, with a t1/2 of 1 h and 3.6 and 3.8 h, respectively, with a t1/2 of 5 h.
FIG. 3.
(a) Killing and regrowth of S. aureus ATCC 2913 exposed to 10× the MIC of vancomycin with a t1/2 of 1 h. Three separate experiments were performed on different occasions. The concentration declined to the MIC at approximately 3.3 h, and the time for a control to grow 1 log10 CFU/ml was 1.4 h. The PME was 6.5 h (range, 5.8 to 8.1 h). (b) Killing and regrowth of S. aureus ATCC 2913 exposed to 10× the MIC of vancomycin with a t1/2 of 5 h. Three separate experiments were performed on different occasions. The concentration declined to the MIC at approximately 15.3 h, and the time for a control to grow 1 log10 CFU/ml was 1.4 h. The PME was 3.6 h (range, 2.6 to 4.6 h).
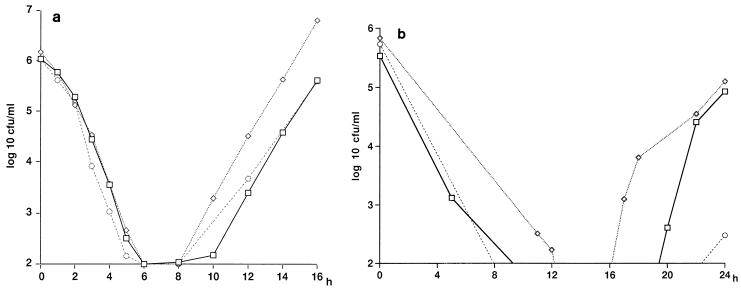
For S. epidermidis ATCC 29886 the PME with a t1/2 of 1 h was 10.3 h (range, 8.8 to 11.4 h). When a t1/2 of 5 h was used, the bacterial density declined to below the level of detection (102 CFU/ml) and was not measurable at the time when the concentration had declined to the MIC (Fig. 4a and b). The exact length of the PME therefore could not be calculated. However, in two of the three experiments the numbers of CFU per milliliter were above 103 before the MIC was reached, at approximately 15.5 h, or at 21 h; hence, the PME in these experiments was less than 6 h.
FIG. 4.
(a) Killing and regrowth of S. epidermidis ATCC 29886 exposed to 10× the MIC of vancomycin with a t1/2 of 1 h. Three separate experiments were performed on different occasions. Values below the detection limit were given a value of 2. The concentration declined to the MIC at approximately 3.3 h, and the time for a control to grow 1 log10 CFU/ml was 1.2 h. The PME was 10.3 h (range, 8.8 to 11.4 h). (b) Killing and regrowth of S. epidermidis ATCC 29886 to 10× the MIC of vancomycin with a t1/2 of 5 h. Three separate experiments were performed on different occasions. Values below the detection limit were given a value of 2. The concentration declined to the MIC at approximately 15.3 h, and the PME could not be calculated because the bacterial density declined to below the level of detection.
DISCUSSION
The MICs and the minimum bactericidal concentrations of antibiotics have been the major parameters used to quantify the in vitro antimicrobial activities of antibiotics against infecting pathogens, and together with the pharmacokinetic properties of the drug they are still the major factors determining antibiotic dosing regimens. Since the MICs are determined after 20 to 24 h of incubation with a constant antibiotic concentration, they represent the net result of a series of events that may have taken place during this time. Furthermore, the MIC does not provide any information about the activities of increased drug concentrations, the antibacterial effects that may persist after elimination of the drug, or the influence of sub-MICs. Pharmacodynamic parameters such as the rate of bacterial killing, the PAE, and the PA SME may therefore provide a more accurate description of the antimicrobial activity than the MIC alone (3, 5, 25–27, 34).
Small and Chambers (33) reported a slow rate of killing of S. aureus exposed to 4× the MIC of vancomycin for 24 h. At 4 h a reduction of 1.1 log10 CFU/ml was seen, and at 24 h no further significant change in the numbers of CFU was observed. Also, in our experiments the rate of killing was slow for all strains; however, killing continued beyond 4 h and there was a reduction of >3 log10 CFU/ml at 24 h for all strains of S. aureus. Our results showed no concentration-dependent killing against any of the strains of S. aureus and S. epidermidis that were studied, which is in agreement with the results of several previous studies (1, 6, 9, 15, 30). However, Greenberg and Benes (12) compared the efficacies of oxacillin, vancomycin, and teicoplanin against different strains of S. aureus incubated with 50% bovine serum and reported a significantly increased rate and amount of killing when the concentration of vancomycin was increased from 20 to 80 mg/liter, even though the free drug concentration still exceeded the MIC with the lower dose. Peetermans et al. (29) have shown concentration-dependent killing for concentrations below the MIC but not for higher concentrations.
The PAEs found in the present study were relatively short (0.7 to 2.6 h) for all strains except S. epidermidis ATCC 29886 (range, 4.3 to 6.5 h). Our results are in accordance with those reported previously (4, 15, 23). In contrast to the PAEs, the PA SMEs were very long for all strains tested. We have shown earlier (27) that vancomycin exhibits very long PA SMEs against strains of Streptococcus pyogenes and Streptococcus pneumoniae. Peetermans et al. (29) showed an initial killing when S. aureus was challenged with vancomycin concentrations just below the MIC; this may explain the long SMEs seen in the present study with concentrations close to the MIC.
In the in vivo situation, when intermittent antibiotic dosing is used, antibiotic levels in serum and tissues will gradually decrease and the microorganisms will often be exposed to both supra- and sub-MICs during the dosing interval. The killing of bacteria subjected to various drug concentrations may therefore provide more meaningful information about optimal dosing strategies than determinations obtained with static concentrations. To obtain conditions in vitro that stimulate the antibiotic pharmacokinetics in vivo, different kinetic models have been developed (2, 11, 12a, 24, 32).
In a recent study with an in vitro kinetic model in which bacteria are exposed to fluctuating antibiotic concentrations, a new parameter, the PME, was introduced (22). The PME was calculated as the difference in time for the bacteria to grow 1 log10 CFU/ml from the numbers obtained at the time when the drug concentration declined to the MIC and the corresponding time for a control culture not exposed to antibiotic. Beta-hemolytic streptococci were challenged with benzylpenicillin with different t1/2s, and the PMEs were calculated. The PME seemed to be dependent on the t1/2 of benzylpenicillin, and longer PMEs were obtained with a t1/2 of 1 h than with one of 3 h (22).
Vancomycin interferes with cell wall synthesis in susceptible bacteria by binding to the terminal aminoacyl d-alanyl–d-alanine sequence, which is different from the interference caused by benzylpenicillin, which binds to penicillin-binding proteins. It also has a longer terminal t1/2 in humans (approximately 3 to 9 h) whereas benzylpenicillin has a terminal t1/2 of approximately 1 h (14, 16–18). Since the PA SMEs were shown to be very long for vancomycin against staphylococci, we found it to be of interest to investigate the effects of different t1/2s of vancomycin on the length of the PME.
Vancomycin and teicoplanin both bind firmly to peptidoglycan. It has been suggested that the regrowth of staphylococci exposed to vancomycin and teicoplanin may occur if inadequately inhibited bacteria synthesize new peptidoglycan to override the antibacterial effect (13). The PAE, PA SME, and PME would then reflect the time that the amount of peptidoglycan is kept below a critical level needed for bacterial growth. The PMEs were shorter for both S. aureus and S. epidermidis with the longer t1/2 of 5 h, with which regrowth started when the drug concentration declined to the MIC (Fig. 3b and 4b). In these experiments the concentration declines slowly and remains close to the MIC for a longer period of time, during which synthesis of new peptidoglycan could be allowed. The level of peptidoglycan necessary for regrowth could therefore be reached when the drug concentration declined to the MIC and the following sub-MICs would not prevent cell division. In contrast, when a t1/2 of 1 h was used the MIC was already reached after 3.5 h and the killing continued even 3 to 4 h after this time point. One explanation for this could be that the amount of peptidoglycan at this time was not yet sufficient for the initiation of regrowth.
In conclusion, we found no concentration-dependent killing of vancomycin against the strains of S. aureus and S. epidermidis tested in this study, relatively short PAEs, but very long PA SMEs. The PA SMEs were calculated from the results of experiments performed with a very short exposure (2 h) to supra-MICs and seem to overestimate the effects of subinhibitory concentrations. When a short t1/2 was used, the PME exceeded the PAE probably due to the effects of subinhibitory concentrations. However, the PME was shorter when the t1/2 was extended to 5 h (simulating the terminal t1/2 in humans), and regrowth started when the drug concentration declined to the MIC. It is still unclear which serum concentration-time profile in relation to MIC leads to the optimal efficacy for glycopeptides. When Duffull et al. (6) used four different vancomycin dosing regimens against S. aureus in an in vitro kinetic model, they found that killing was not dependent on either the peak concentration or the area under the curve. Maintaining a constant concentration above the MIC was equally effective even with an area under the curve that was half of that obtained by the other three regimens. Our findings also indicate that the time that the concentration in serum exceeds the MIC is the parameter most important for the efficacy of this drug, hence suggesting that dosing schedules with vancomycin should maintain the concentration above the MIC for most of the dosing interval and that high peak concentrations are not needed. However, to further define the optimal dosing of vancomycin, studies with other species and multiple dosing regimens are needed.
ACKNOWLEDGMENTS
We thank Anita Perols and Ingegerd Gustafsson for excellent laboratory assistance.
This study was supported by a grant from Eli Lilly Sweden AB, Stockholm, Sweden.
REFERENCES
- 1.Ackerman B H, Vanner A M, Eudy E B. Analysis of vancomycin time-kill studies with Staphylococcus species by using a curve stripping program to describe the relationship between concentration and pharmacodynamic response. Antimicrob Agents Chemother. 1992;36:1766–1769. doi: 10.1128/aac.36.8.1766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Blaser, J. 1985. Two compartment kinetic model with multiple artificial capillary units. J. Antimicrob. Chemother. 15(Suppl. A):131–137. [DOI] [PubMed]
- 3.Bundtzen R W, Gerber A U, Cohn D L, Craig W A. Postantibiotic suppression of bacterial growth. Rev Infect Dis. 1981;3:28–37. doi: 10.1093/clinids/3.1.28. [DOI] [PubMed] [Google Scholar]
- 4.Cooper M A, Jin Y F, Andrews J M, Wise R. In-vitro comparison of the postantibiotic effect of vancomycin and teicoplanin. J Antimicrob Chemother. 1990;26:203–207. doi: 10.1093/jac/26.2.203. [DOI] [PubMed] [Google Scholar]
- 5.Craig W A, Gudmundsson S. The postantibiotic effect. In: Lorian V, editor. Antibiotics in laboratory medicine. Baltimore, Md: The Williams & Wilkins Co.; 1986. pp. 515–536. [Google Scholar]
- 6.Duffull S B, Begg E J, Chambers T, Barclay M L. Efficacies of different vancomycin dosing regimens against Staphylococcus aureus determined with a dynamic in vitro model. Antimicrob Agents Chemother. 1994;38:2480–2482. doi: 10.1128/aac.38.10.2480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ehrenkranz N J. Antibiotics annual, 1958–1959. New York, N.Y: Medical Encyclopedia, Inc.; 1959. The clinical evaluation of vancomycin in treatment of multiantibiotic refractory staphylococcal infections; pp. 587–594. [PubMed] [Google Scholar]
- 8.Ericsson H M, Sherris J C. Antibiotic sensitivity testing-report of an international collaborative study. Acta Pathol Microbiol Scand Sect B Suppl. 1971;217:3–90. [PubMed] [Google Scholar]
- 9.Flandrois J P, Fardel G, Carret G. Early stages of in vitro killing curve of LY 146032 and vancomycin for Staphylococcus aureus. Antimicrob Agents Chemother. 1988;32:454–457. doi: 10.1128/aac.32.4.454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Geraci J E, Heilman F R, Nichols D R, Wellman W E, Rooss G T. Some laboratory and clinical experiences with a new antibiotic, vancomycin. Proc Mayo Clin. 1956;31:564–582. [PubMed] [Google Scholar]
- 11.Grasso S, Meinardi G, de Carneri I, Tamassia V. New in vitro model to study the effect of antibiotic concentration and rate of elimination on antibacterial activity. Antimicrob Agents Chemother. 1978;13:570–576. doi: 10.1128/aac.13.4.570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Greenberg R N, Benes C. Time-kill studies with oxacillin, vancomycin and teicoplanin versus Staphylococcus aureus. J Infect Dis. 1990;161:1036–1037. doi: 10.1093/infdis/161.5.1036. [DOI] [PubMed] [Google Scholar]
- 12a.Greenwood D, Tupper H. New in vitro device for examining the response of bacteria to changing drug concentrations. Curr Chemother Immunother. 1981;1981:100–102. [Google Scholar]
- 13.Greenwood D, Bidgood K, Turner M. A comparison of the responses of staphylococci and streptococci to teicoplanin and vancomycin. J Antimicrob Chemother. 1987;20:155–164. doi: 10.1093/jac/20.2.155. [DOI] [PubMed] [Google Scholar]
- 14.Griffith R S. Antibiotics annual, 1956–1957. New York, N.Y: Medical Encyclopedia, Inc.; 1957. Vancomycin: continued clinical studies; pp. 118–122. [PubMed] [Google Scholar]
- 15.Hahnberger H, Nilsson L E, Maller R, Isaksson B. Pharmacodynamics of daptomycin and vancomycin on Enterococcus faecalis and Staphylococcus aureus demonstrated by studies of initial killing and postantibiotic effect and influence of Ca2+ and albumin on these drugs. Antimicrob Agents Chemother. 1991;35:1710–1716. doi: 10.1128/aac.35.9.1710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Healy D P, Polk R E, Garson M L, Rock D T, Comstock T J. Comparison of steady-state pharmacokinetics of two dosage regimens of vancomycin in normal volunteers. Antimicrob Agents Chemother. 1987;31:393–397. doi: 10.1128/aac.31.3.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Krogstad D J, Moellering R C, Greenblatt D J. Single-dose kinetics of intravenous vancomycin. J Clin Pharm. 1980;20:197–201. doi: 10.1002/j.1552-4604.1980.tb01696.x. [DOI] [PubMed] [Google Scholar]
- 18.Lagast H, Didion P, Klastersky J. Comparison of pharmacokinetics and bactericidal activity of tecoplanin and vancomycin. J Antimicrob Chemother. 1986;18:513–520. doi: 10.1093/jac/18.4.513. [DOI] [PubMed] [Google Scholar]
- 19.Lopez-Lopez G, Pauscal A, Perea E J. Effect of plastic catheter material on bacterial adherence and viability. J Med Microbiol. 1991;34:349–353. doi: 10.1099/00222615-34-6-349. [DOI] [PubMed] [Google Scholar]
- 20.Louria D B, Kaminski T, Buchman J. Vancomycin in severe staphylococcal infections. Arch Intern Med. 1961;107:225–240. doi: 10.1001/archinte.1961.03620020075007. [DOI] [PubMed] [Google Scholar]
- 21.Löwdin E, Odenholt-Tornqvist I, Bengtsson S, Cars O. A new method to determine postantibiotic effect and effects of subinhibitory antibiotic concentrations. Antimicrob Agents Chemother. 1993;37:2200–2205. doi: 10.1128/aac.37.10.2200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Löwdin E, Odenholt I, Cars O. Pharmacodynamic effects of sub-MICs of benzylpenicillin against Streptococcus pyogenes in a newly developed in vitro kinetic model. Antimicrob Agents Chemother. 1996;40:2478–2482. doi: 10.1128/aac.40.11.2478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McDonald P J, Craig W A, Kunin C M. Persistent effect of antibiotics on Staphylococcus aureus after exposure for limited periods of time. J Infect Dis. 1977;135:217–223. doi: 10.1093/infdis/135.2.217. [DOI] [PubMed] [Google Scholar]
- 24.Navashin S M, Fomina I P, Firsov A A, Chernykh C M, Kuznetsova S M. A dynamic model for in-vitro evaluation of antimicrobial action by simulation of the pharmacokinetic profiles of antibiotics. J Antimicrob Chemother. 1989;23:389–399. doi: 10.1093/jac/23.3.389. [DOI] [PubMed] [Google Scholar]
- 25.Odenholt I, Holm S E, Cars O. Effects of benzylpenicillin on group A β-hemolytic streptococci during the postantibiotic phase in vitro. J Antimicrob Chemother. 1989;24:147–156. doi: 10.1093/jac/24.2.147. [DOI] [PubMed] [Google Scholar]
- 26.Odenholt-Tornqvist I, Löwdin E, Cars O. Pharmacodynamic effects of subinhibitory concentrations of β-lactam antibiotics in vitro. Antimicrob Agents Chemother. 1991;35:1834–1839. doi: 10.1128/aac.35.9.1834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Odenholt-Tornqvist I, Löwdin E, Cars O. The postantibiotic sub-MIC effect of vancomycin, roxitromycin, sparfloxacin, and amikacin. Antimicrob Agents Chemother. 1992;36:1852–1858. doi: 10.1128/aac.36.9.1852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pascual A, Fleer A, Westerdaal N A, Verhof J. Modulation of adherence of coagulase-negative staphylococci to Teflon catheters in vitro. Eur J Clin Microbiol. 1986;5:518–522. doi: 10.1007/BF02017694. [DOI] [PubMed] [Google Scholar]
- 29.Peetermans W E, Hoogeterp J J, Hazekamp von Dokkum A-M, van den Broek P, Mattie H. Antistaphylococcal activities of teicoplanin and vancomycin in vitro and in an experimental infection. Antimicrob Agents Chemother. 1990;34:1869–1874. doi: 10.1128/aac.34.10.1869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Raddatz J K, Larsson A J, Walker K J, Rotschafer J C. Program and abstracts of the 35th Interscience Conference on Antimicrobial Agents and Chemotherapy. Washington, D.C: American Society for Microbiology; 1995. Concentration-independent effect of monoexponential and biexponential decay of vancomycin (VM) in the killing of S. aureus (SA) under aerobic and anaerobic conditions, abstr. A101; p. 19. [Google Scholar]
- 31.Ramirez de Arellano E, Pauscal A, Martinez-Martinez L, Perea E J. Activity of eight antibacterial agents on Staphylococcus epidermidis attached to Teflon catheters. J Med Microbiol. 1994;40:43–47. doi: 10.1099/00222615-40-1-43. [DOI] [PubMed] [Google Scholar]
- 32.Reeves, D. S. 1985. Advantages and disadvantages of an in-vitro model with two compartments connected by a dialyser: results of experiments with ciprofloxacin. J. Antimicrob. Chemother. 15(Suppl. A):159–167. [DOI] [PubMed]
- 33.Small P M, Chambers H F. Vancomycin for Staphylococcus aureus endocarditis in intravenous drug users. Antimicrob Agents Chemother. 1990;34:1227–1231. doi: 10.1128/aac.34.6.1227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wilson D A, Rolinson G A. The recovery period following exposure of bacteria to penicillins. Chemotherapy (Basel) 1979;25:14–22. doi: 10.1159/000237817. [DOI] [PubMed] [Google Scholar]