Abstract
Despite Hepatitis C Virus (HCV) cure availability, people experiencing homelessness (PEH) are challenged with initiating and completing HCV treatment. The design of culturally sensitive HCV treatment programs are lacking. The objective was to employ community-based participatory research methods to understand perceptions of HCV positive PEH, and providers, on the design and delivery of a culturally sensitive, nurse led community health worker (CHW) HCV initiation, and completion program.
Four focus group sessions were conducted with HCV positive PEH (n=30), as well as HSPs (n=7) in Skid Row, Los Angeles. An iterative, thematic approach provided the themes of Essentials of Successful Participant Engagement and Retention: Role of Nurse Led CHW in Promoting: 1) Tangible and Emotional Support; 2) Cognitive and Behavioral Support; and 3) Financial and Structural Resources. The goal of this study is to provide the groundwork for future research of HCV program design to support HCV cure among homeless populations.
Keywords: Hepatitis C Virus, Homeless Adults, Designing an HCV Treatment Program for Homeless Adults
Introduction
Hepatitis C virus (HCV), a blood-borne pathogen impacts millions globally and disproportionality impacts people experiencing homelessness (PEH). In the United States, between 2013 to 2016, an estimated 4.1 million persons were HCV antibody positive and 2.4 million were HCV RNA positive (Hofmeister et al., 2019). An estimated 47,000 people annually contract HCV; 75% of those currently infected may be unaware of their HCV status (CDC, 2020a; Tatar et al., 2020). PEH are at particularly high risk for HCV (Department of Health and Human Services, 2017) and experience challenges across the Hepatitis C Virus Cascade of Care, which is inclusive of diagnosis, treatment, and cure (Safreed-Harmon et al., 2019).
While the total number of PEH infected by HCV is challenging to ascertain, in the U.S., as of 2019, there are 567,715 persons reported to be experiencing homelessness (United States Department of Housing and Urban Development, 2019); further, HCV prevalence has varied (3.9% to 36.2%) across studies (Beijer, Wolf, Fazel, 2012). Across two major cities, between 46% (Page et al., 2017) to 86% (Fuster, Gelberg, 2019) of PEH were HCV infected (Masson et al., 2020). In one study among PEH (N=534), 26.7% were HCV positive and 46.1% were unaware of their infection (Gelberg et al., 2012). PEH are often designated as ‘hard to reach’ by the medical and scientific community; thus, there is a dearth of research into culturally sensitive interventions (Hanlon et al., 2018) to address the myriad of sociocultural factors that lead to both low participation and completion rates in HCV treatment interventions (Lambert et al., 2019).
Direct acting antivirals (DAA) HCV medications taken over six weeks have been found to be well tolerated, and highly effective in treating HCV, resulting in high levels of Sustained Viral Response at 12 weeks (SVR12; Kohli et al., 2015). The diagnosis of chronic HCV is often made decades after any initial infection, when chronic liver disease may develop (e.g., cirrhosis and liver cancer; CDC, 2020b). The American Association of The Study of Liver Diseases and Infectious Diseases Society of America have noted that injecting drug users (IDU) who are actively using and those who have previously injected drugs account for most HCV infections. The American Association of The Study of Liver Diseases and Infectious Diseases Society of America has recommended more frequent testing based on risk factors (American Association of the Study of Liver Diseases, 2019).
Given the inherent housing instability of PEH, the notable lack of access to healthcare, and associated risk behaviors, such as IDU, successful HCV treatment interventions are challenging for this population (Department of Health and Social Services, 2017). Increasingly, the intersectionality of the above conditions and other important factors (i.e., social, cognitive, structural, and financial, etc), describes the complex interplay of facilitators and barriers to treatment experienced in each sociodemographic (Dombrowski et al., 2016; Ho et al., 2015; Werb et al, 2016).
Culturally-Sensitive Methodology to Inform the Design of an HCV Intervention Trial
PEH and those unstably housed are often designated as ‘hard to reach’ by the medical and scientific community, and as such, little research exists into interventions that explore infectious disease treatment programs in this population (Hanlon et al., 2018). While recent research has explored therapeutic relationships between homeless individuals and healthcare providers (Moore-Nadler, Clanton, Roussel, 2020), the need for culturally sensitive treatment studies is important to understand, explain, and tailor to the complex sociocultural factors that create the conditions for both low participation and low HCV completion rates among PEH with curative HCV interventions (Hanlon et al., 2018; Lambert et al., 2019; Surey et al., 2019). Addressing the sociocultural factors from within a PEH community context is foundational to any HCV intervention among homeless adults (Dombrowski et al., 2016).
Prior to designing interventions, the importance of accessing and engaging with impacted communities cannot be underestimated (Gonzalez-Guarda et al., 2019). For example, community advisory boards (CAB) offer a critical introduction to any planned intervention, identifying the pertinent needs and observations of the population and establishing collaborative partnerships that create a tailored research strategy (Gonzalez- Guarda et al., 2019). Aggregating the insights and guidance of key stakeholders, particularly those formerly or currently unstably housed, or with a profound history and knowledge of PEH, and/or HCV treatment, can preemptively illuminate themes, barriers, and facilitators to the project, and enhancing potential for success (Avramovic et al., 2020; Grebely et al., 2017). Engaging the community can optimize efforts to ‘seek and treat’ or avoid loss to follow-up frequently experienced when working with underserved and transient PEH (Avramovic et al., 2020). Focus groups as a subsequent step, may provide further valuable feedback, highlighting the experience, the nuance, and the detail of other key players’ perspectives (Frey, 2018).
Social-Level Needs to Consider When Designing HCV Interventions
Without doubt, the societal burden of HCV far outweighs the challenges of designing a culturally sensitive, patient-centered treatment program for PEH with HCV infection (Betancourt et al., 2003). For PEH, culturally sensitive approaches to care will include the use of a culturally attuned team, encompassing researchers, peers, nurses, and counselors (MacLellan et al., 2017). Interestingly, in a grounded theory study, understanding the experiences of formerly homeless persons in terms of their views of the nature and quality of social ties, including those of peers and healthcare providers, sets the stage for the complexity of social ties, particularly as to how it relates to substance use and mental illness (Pahwa, Smith, Yuan, & Padgett, 2019). This is particularly significant when marginalized populations, such as PEH who suffer from mental illness and substance use disorder perceive healthcare providers as being biasing, lacking advocacy, and promoting feelings of being disrespected and dismissed (Moore-Nadler, Clanton & Roussel, 2020).
In the past, peer-led programs inclusive of community health workers (CHWs) who have lived experiences of homelessness, are role models, and have successfully transitioned out of homelessness have been implemented to improve vaccination uptake (Nyamathi et al., 2015), dialectical behavioral therapy (Nyamathi et al., 2017; Nyamathi et al., 2018), medication adherence (Salem et al., 2020), and to improve frailty and other health behaviors (Salem et al., 2017) among PEH and formerly incarcerated, PEH. In these various studies, peers were hired as CHWs and were able to build trust with the community and help participants meet health promotion goals, complete treatment regimens, and navigate systems.
Peer advocates, either in leadership or supportive roles, offer undeniable therapeutic benefits of rapport, built with personal self-disclosure (MacLellan et al., 2017; Surey et al., 2019). Given the vast social and emotional stigma, deprivation, and disparities that PEH manage daily, the core value of trust, in the treatment team and process is essential (Skeer et al., 2018; Treloar et al., 2013). Moreover, many PEH may be treatment-adverse due to mistrust, competing needs, fear, cultural beliefs around treatment protocols and misinformation (Treloar et al., 2013).
Cognitive-Level Needs to Consider When Designing HCV Interventions
Education that raises consciousness of the improved HCV treatment, its availability to PEH, the shorter treatment course duration and the limited negative treatment responses compared to prior protocols should be promoted within the entire community and may facilitate the uptake of the daily direct acting antiviral (DAA) medication (Skeer et al., 2018; Williams et al., 2019). Diligent care coordination, from screening to treatment to ongoing follow-up encourages retention and movement of homeless adults through an HCV intervention care continuum (Benitez et al., 2020; Ho et al., 2015; Surey et al., 2019). Substance use treatment linked to HCV services may likewise be critical for certain PEH participants (Lambdin et al., 2017), as well as on-site clinics, and financial incentivization (Brown et al., 2019; Ghose et al., 2019).
The perception that HCV is low risk, or that treatment is expensive and difficult, or that reinfection is inevitable, are plausible explanations for delaying treatment and prioritizing other needs in this population; particularly for those with ongoing substance use (Childs et al., 2019). Understanding the role that exclusion plays in lack of engagement in medical care is important (Skeer et al., 2018; Williams et al., 2019). For example, among young untreated HCV-infected participants who inject drugs, the stigma of being judged, poorly treated, and dismissed during interactions with health care providers (HCPs) has been verbalized (Skeer et al., 2018). When participants perceive HCPs as lacking cultural-competency, insensitive to addiction issues, and not respectful when giving results (Skeer et al., 2018), this often leads to fear, mistrust, and discrimination, and further dis-incentivizes any participation in treatment (Skeer et al., 2018; Williams et al., 2019). Reducing stigma from care providers, using patient-centric disclosure techniques, decreasing the perception of personal responsibility for HCV, and facilitating continuity of care may be fundamental for PEH inclusion (Skeer et al., 2018).
Similarly, mental health comorbidities such as depression and PTSD may have labelled patients as poor candidates for completing HCV treatment (Rifai et al., 2006). Increasingly, models of integrated care, using multidisciplinary approaches with mental health providers, case management and concurrent substance use treatment demonstrate success as HCV cure interventions (Ho et al, 2015). Findings reveal that substance users who participated in drug treatment services were 15% more likely to report screening for HCV versus those who never had drug treatment (Lambdin et al., 2017). Thus, the need for linkage of integrated simultaneous services to treat HCV, combined with rights to health services for drug users, are needed in programs of harm reduction (Alavi et al., 2019; Grebely et al., 2017; Lambdin, et al., 2017).
Structural-Level Needs to Consider When Designing HCV Interventions
Access to healthcare, linkage to treatment, and consistent engagement with services pose challenges in the design and execution of culturally sensitive interventions to cure infectious disease in marginalized groups, such as PEH (Surey et al., 2019). Prior qualitative research has identified challenges PEH experience navigating complex systems (Henwood, Lahey, Harris, Rhoades, Wenzel, 2018, Moore-Nadler, Clanton, Roussel, 2020). However, nurse-led programs have been shown to be successful in treating those unstably housed with HCV (Harney et al., 2019; O’Sullivan et al., 2020), as have patient-centered approaches involving extensive HCV education (Henry-Akintobi et al., 2016).
As homelessness increases the risk of contracting an infectious disease by as much as 50%, a focus on housing needs for PEH is important (Fokuo et al., 2020). For those with access to HCV treatment, challenges exist around HCV medication delivery, storage, and dispensing (Fokuo et al., 2020). This leads to the exploration of the nature of housing for the duration of HCV treatment for HCV positive PEH. Additionally, meagre healthcare infrastructure, and human resource issues may make HCV treatment strategies less effective (Fokuo et al., 2020).
Financial-Level Needs to Consider When Designing HCV Interventions
Over the past decade, HCV treatment costs have decreased from the prohibitive $84,000 price tag of Sovaldi, an early DAA, to the current regimen of Mavyret, currently priced at approximately $26,400 (Hepatitis C Online, 2021). HCV genotype 1, the most common in the U.S., has utilized all-oral therapy with a combination of DAAs; as of 2017, all-oral, safe, effective, and convenient regimens devoid of ribavirin have been available (Hepatitis C Online, 2021). Selection of the type of regimen depends on a confluence of factors (e.g., cost, insurance, provider preference, etc) (Hepatitis C Online, 2021). However, patient assistance programs (PAP) are likewise currently available for those unable to afford the medication regimen (AbbVie, 2020; Kardish, 2014; Mavyret, 2019).
Adapting to the lived realities of the PEH, studies have shown that incentivization can improve treatment completion rates (Fokuo et al., 2020). Well-funded, nationally supported, community-based intervention strategies, such as nurse-led programs with contingency management, or simpler standard care teams, may be cost-effective in the treatment of viral infectious disease in the community (Grebely et al., 2017; Zhang et al., 2018). As a result of the gaps in knowledge, the purpose of this study was to engage community-based stakeholders on best strategies in designing a culturally sensitive HCV treatment program for HCV positive homeless adults. Our goal was to ensure that our program was culturally sensitive, feasible, and acceptable to homeless adults who were HCV positive and in need of treatment.
Project Purpose and Aims
The purpose of this study was to employ community-based participatory research methods to understand the perceptions of HCV positive PEH, and homeless service providers (HSPs) on the design and delivery of a culturally sensitive HCV initiation and completion program.
Methods
Utilizing the Consolidated Criteria for Reporting Qualitative Research, the next section will present details of the following: 1) research team and reflexivity; 2) study design; and 3) analysis and findings (Tong, Sainsbury, Craig, 2007).
Study Overview and Design
Methodological Orientation and Theory.
To achieve the purpose of the study, community-based participatory methods were used to understand the perceptions of HCV positive homeless adults and treatment providers who cared for homeless adults. We selected community-based participatory method modality because of the intense collaboration between researchers and the community, and mutual sharing of information, with a focus on improving a planned intervention using a culturally sensitive approach (Buck et al., 2004). Furthermore, our focus of study was to understand the perspectives of both homeless adults and HSP in terms of barriers and facilitators to HCV engagement, retention, and treatment completion. This would promote the goal to design a program that is culturally sensitive as it is informed by both the community of residents as well as HSP.
Qualitative data were first collected from a community advisory board (CAB), and then focus groups were subsequently conducted by the research team. The University of California, Irvine Institutional Review Board Human Subjects Protection Committee approved the study). The data was collected between 2019 to 2020.
Preliminary Assessment: Engaging Stakeholders in a Community Advisory Board (CAB)
Formation of a CAB was one of the most critical steps the investigators sought to initiate early in the development of a culturally sensitive intervention. In total, two CAB sessions were held, with mixed groups ranging from 15 participants to 16 participants. We included 31 members of the CAB to help inform us about these issues and thus, advise us on ways to make our program culturally sensitive, acceptable, and feasible to our potential participants. The total sample included 24 PEH; most of them male and self-reported as homeless; several of them completing HCV treatment. The HSPs totaled 7 and were composed of Registered Nurses (n= 3) and Community Health Workers (n=4). The CAB membership was organized into groups that included both PEH who have been diagnosed and completed HCV treatment, as well as PEH, diagnosed with HCV but who did not complete treatment.
Based on our typical protocol for the CAB, depending on the issue at hand, perspectives were solicited from both groups to equally present facilitators and barriers to treatment completion; critical in understanding issues related to HCV engagement, retention, and treatment completion. We also were interested in hearing their thoughts about how we would deliver the intervention, as well as provide feedback on our draft semi-structured interview guide which would be utilized in our focus group sessions. Finally, the CAB members also advised on selection of members of the focus groups. All CAB participants joined one CAB session and were paid $15 at the end of the session.
In addition to homeless adults, we carefully sought to include HSPs from the community, who cared for homeless adults, such as community health workers (CHWs), physicians, nurses, or spiritual leaders. Having closely worked with homeless adults, their expertise and wisdom was critical, both at the professional level, and the experiential level by CHWs who have intimate knowledge of the experience of homelessness because of their own lived experience of homelessness.
Focus Group Methodology:
Focus Group members were guided by the knowledge we received in the CAB sessions. The research team conducted the focus groups to fully understand the social, cognitive, structural, and financial issues related to designing a culturally sensitive HCV treatment program.
Sampling and Participant Selection: People Experiencing Homelessness (PEH) and Frontline Health and Social Service Providers (HSP)
Focus groups were composed of both PEH and HSPs and PEH were enrolled if they reported: 1) sleeping in the past night in a homeless living situation, 2) HCV-positive as documented by study sites, 3) history of substance use, 4) ≥ 18 years of age, and 5) able to speak English. Homeless service providers (HSPs) qualified for the study if they were: 1) clinicians (e.g., registered nurses, nurse practitioners, physicians, physician assistants, or service providers (e.g., CHWs or social workers, spiritual advisors), 2) provided educational and social services for homeless clients, and 3) worked in a homeless clinic for at least one year, including with PEH treated for HCV infection.
Setting
In Skid Row (Central City East, Los Angeles), three community-based sites (Union Rescue Mission, Downtown Women’s Center, and Illumination Foundation served as the agencies which facilitated recruitment of PEH and HCPs. The research staff worked closely with the leadership of these sites to assist in recruiting PEH, whom they were serving, or the HSPs in these sites were interested in participating.
For over a century, the URM has served homeless participants by providing temporary and long-term housing services (Union Rescue Mission, 2020). As a clinician-provider counterpart, Los Angeles County Health Centers operates clinics for homeless clients and outreach for varied services (Los Angeles Christian Health Centers, 2020). One of the few community-based organizations serving women experiencing homelessness, Downtown Women’s Center provides health care and employment services (Downtown Women’s Center, 2020). As a recuperative care setting, IF provides housing, healthcare, and services to homeless adults (Illumination Foundation, 2020).
Data Collection
Upon receipt of the institutional review board approval from the University of California Irvine and a SMART reliance agreement from University of California, Los Angeles, the research team posted flyers in our selected sites and utilized electronic means and word-of-mouth to share information with potential participants. As stated earlier, our goal was to hear the perspectives of both the PEH themselves who would be the recipients of the refined intervention program, as well as the HSPs who have had experience working with this population. In a private area of each research site, potential participants were provided more study information. Thereafter, verbal consent and a brief two-minute sociodemographic and HCV-related health history screener was administered to homeless participants. Date of birth and the first three letters of the mother’s first name were obtained to identify potential participants who were requesting screening a second time.
The investigators held four focus groups with PEH and HSP. At the beginning of FGS, participants were asked to select a pseudonym throughout the discussion to maintain confidentiality. During each FGS, the research team reviewed the key components of both programs, including the clinic-based standard of care versus the RN/CHW program. These components included the educational content provided in the HCV program, how HCV medication would be delivered by the nurse led CHW team; additional roles of the CHW in making referrals to medical and social services, and housing. Finally, we assessed acceptability and feasibility of the RN/CHW program by means of an acceptability and feasibility scale.
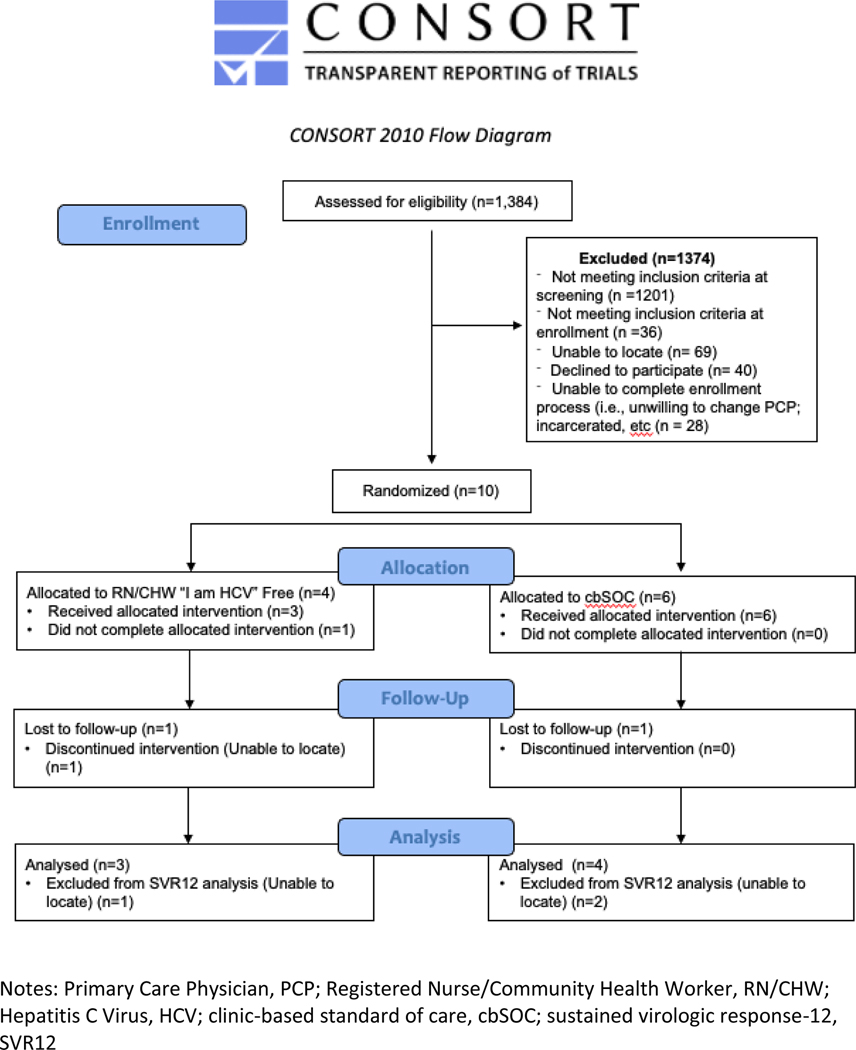
Observations and detailed field notes were recorded within 24 hours of each session. FGS lasted on average two hours, and participants received $3 for screening, and $20 for their participation in the focus groups. Findings of these FGS will inform the refinement of a culturally appropriate program. Figure 1 depicts the program description which was reviewed in FGS. Some questions posed in the FGS included. Please see the full set of FGS questions (see supplemental file 1):
Figure 1.
Please tell us what health services you have sought in the last few years?
For all adults who have been diagnosed with HCV and asked to complete a three-week treatment program (daily for seven days per week) regimen of a drug called Mavyret, we want to know what have been the facilitators for completion?
What would you say are the biggest barriers to completing the therapy?
We would like you to provide any final comments to help us design a program most helpful to you in enhancing completion of 3HP for homeless persons in this community?
Program Design Acceptability
The moderators of the FGS began the sessions with explaining the preliminary design of the program. They described there were two arms to the study; the first was the clinic-based Standard of Care, a clinic-based arm where participants completed the treatment by visiting the clinic and were provided a supply of medication; or a nurse-led CHW (RN/CHW) arm where the team would walk the streets and bring the medication to the enrolled participants. Rather than handing the participants a bottle of pills for a designated period, the CHW would meet with the client and provide one dose of the medication each day, along with education and referrals. However, critical components of the program were essential to promote recruitment and ensure retention.
Data Analysis
Credibility of the findings was ensured by an independent transcriptionist who logged verbatim the tapes. Thereafter, an experienced member of the research team (Salem et al., 2021; Salem et al., 2020) and a research assistant removed identifiable information, and uploaded audio files, and transcripts to Dedoose (Dedoose Version 8.3.35, 2020). Over the course of eight months, the select team members collaborated weekly on data analysis and writing. These members listened to the audio recordings, compared them against the verbatim transcript, and made red-lined modifications if the audio recording and transcript differed. All transcripts were subsequently moved to Microsoft Excel and reorganized (e.g., transcript number, pseudonym, raw data, date, and coding cycles).
In qualitative data analysis, trustworthiness of data is assured by credibility, dependability, confirmability, and transferability (Shenton, 2004). To ensure confirmability, an audit trail was established, at the beginning of the study, which documented all steps employed, utilizing evidence-informed research methods. Early familiarity with the culture of the participating organizations including understanding the culture, population, building trust ensured credibility (Shenton, 2004). During the data collection process, FGS were held in private areas of the community-based partner site to ensure honesty and openness of participants.
In particular, precoding, and subsequent independent line-by-line coding was conducted; thereafter, second cycle independent coding was conducted in which line-by-line coding was reassessed, and similarities and differences across the data was addressed (Saldaña, 2009). Credibility was further ensured by a debriefing with the team to discuss the themes and subtheme. To ensure dependability and confirmability, the methods have been described in detail, along with the limitations.
Results
Sociodemographic Characteristics
In total, 30 PEH participated in the focus group sessions. The mean age of PEH was 51.8 (SD 11.49; range 22–69); and the majority were male (63.3%). Half the sample were Black/African American, while about a quarter self-reported as being Hispanic/Latino. The rest were White (10%) or other race. In total, 41.6% of the sample completed less than 12th grade education, while 17.2% completed college or other post high school education. Most of the sample were unemployed (93.8%).
Characteristics of the ten (10) HCPs who participated revealed that the majority were predominantly CHW (70%) and fewer were Registered Nurses (30%). The majority were male (60%), and about half were white (50%); followed by Hispanic/Latino (30%) and Black/African American (10%).
Qualitative Findings
We found three overarching themes in the data and these included: 1) Essentials of Successful Program Design: Role of Nurse-Led CHW; 2) Essentials of Successful Participant Engagement and Retention: Promoting Social and Cognitive Resources; and 3) Essentials of Successful Participant Engagement and Retention: Promoting Financial and Structural Resources.
Theme 1: Essentials of Successful Engagement and Retention: Role of Nurse Led CHW in Promoting Tangible and Emotional Support
Subtheme 1: Appreciating Nurse Led, CHW Tangible Support
The PEH who participated in the FGS discussed the benefits of having nurse led CHW meet homeless persons and provide HCV medication daily, wherever they were living, versus receiving a supply of pills lasting one month. While one participant expressed that being given a week supply at one time would work well, other PEH disagreed and remarked that direct daily observation by the CHW of taking the medication was a good idea as it was noted that oftentimes, homeless persons would lose their medication, or it would be stolen at times as well. Three PEH also agreed that by delivering medication to PEH would ensure the medication was being taken and issues such as drugs or other distractions did not get in the way. As one PEH noted,
Because like I said…drugs get in our way. Lovers… or whatever, get in our way...and TV and radio; different things that distract you. But if they [CHW] be in a certain place, you … got to be right here…
Moreover, CHW provided tangible support which was valued by several PEH. It was exceptionally helpful to have the CHW walk participants to different services and advocate on their behalf. For example, two PEH particularly appreciated CHW assisting them to get their Social Security or taking people to the General Relief office was very helpful. One CHW mentioned she enjoyed advocating for her clients, ensuring that they had their ID, taking them to the doctor, or to get food if they were hungry, or beginning the housing application process. These tasks would often overwhelm homeless adults and as one CHW recalls, some health and social service providers can often be rude to homeless people. However, as one CHW articulated,
So, when you go in there with the badge and we use professional words, their whole perspective is different. And I always tell my clients, just have a seat and let me handle this. And that’s how I resolve and get things done for you guys…Let me help you do this…. That’s a lot of things that I do for my clients.
The CHW likewise offered support in assisting with paperwork as clients would often lose their paperwork and would be unable to navigate through the system to get replacement paperwork. One homeless healthcare provider, a Registered Nurse described the process of helping participants to follow up and schedule healthcare appointments, making sure they get where they need to be, and making sure they know what happened during the visit, so that the RN could follow-up thereafter to help the homeless adult “connecting all those dots. Sometimes they get really overwhelmed and they’d rather just not deal with it.”
Subtheme 2: Appreciating Nurse-Led, CHW Emotional Support
PEH also enjoyed the uplifting comments made by the CHW because as one homeless person stated, “you never know what type of frame of mind people are in.” HSPs also mentioned that motivation was perceived to be helpful by encouraging their homeless clients to overcome barriers to taking the prescribed medication and possible outcomes of not taking the medication as ordered. PEH agreed that the motivation indeed kept them strong and commented .... Yeah, you know what, if we don’t have self-motivation, that’s bad.
Several discussions also related to how the social skills of the nurse led CHW team would be critical to build trust in their relationship with PEH, so that they would be retained throughout the HCV program. One CHW described how they communicate with PEH to ensure confidentiality and trust. One participant said,
…The first thing I tell them is, we don’t report [you] to your PO [Parole Officer]. We don’t engage with the police. It’s confidential. Whatever, your drug use, whatever your preference is, we don’t judge you.
The CHW and other HSPs shared their own personal stories about how they connect with PEH. They freely discuss how they were similarly using drugs, “I was a dope fiend; I was a crackhead. But I’m two years clean now. … I want to give back to the community what was given to me.” The CHW gained the confidence of the PEH by sharing such stories.
A chaplain also noted the importance of helping PEH access care and was willing to help the researchers find housing for as many PEH who needed housing as possible. The synergy of the research team and the chaplain was reassuring as both groups wanted to improve the health and wellbeing of PEH.
Another participant shared the importance of joining support groups for those with HCV to ease their fear of being a part of the program. Such support meetings were designed to talk about the prospect of receiving HCV treatment with others, and to let go of shame of being diagnosed with HCV.
Theme 2: Essentials of Successful Participant Engagement and Retention: Role of Nurse-Led CHW in Promoting Cognitive and Behavioral Support
Subtheme 1: Enhancing Benefits of HCV Treatment
Participants mentioned the importance of informing PEH about HCV as a disease, its seriousness, and about the importance of completing the treatment as it can be a cure. Further, sharing their own treatment success stories was considered important for successful engagement.
“The more you talk to people about the seriousness of this illness… and what’s going to happen if they don’t get it treated within years to come, the more they’re going to be educated about it and they’re going to learn…what they have to do. Yes, because they’re going to have it around their kids or their family members …in case of contaminating the rest so, you know, everybody needs more information about this stuff.
Despite the stated benefits, several PEH raised concerns related to HCV medication and if the medication was being tested on them as if they were guiney pigs. One PEH questioned, “Are we first person’s that’s going to be taking this medicine?” Another formerly HCV positive PEH then expressed the need to share with the other members that this drug has been utilized for a long time and it was not experimental, and he was quick to tell others that it worked for him, “That’s the only thing I can say. Sharing my own, yeah, my own experience”.
Subtheme 2: Mitigating Barriers Related to Current Drug Use
When asked what type of drug or alcohol use prevented PEH from being offered HCV treatment, one PEH responded, “pretty much…everything.” The chaplain was forgiving in his eagerness to help by advising that a participant who was an active drug user was still allowed to reside in the shelter during treatment; however, no drug could be consumed in the shelter itself.
When asking a RN and CHW about how many people they know that are actively using and still adhering to the treatment for other conditions, the response was “a good 50%.” The HSP further clarified that alcohol was often more problematic than drugs. However, PEH were honest about their substance use because they make it clear to the PEH that they do not report to their parole officers, “This is all confidential, what you tell me”.
Theme 3: Essentials of Successful Participant Engagement and Retention: Role of Nurse-Led CHW in Promoting Financial and Structural Resources
Subtheme 1: Expertise in Promoting Continued Engagement
In a discussion about ways the study staff can successfully track and retain participants throughout the study, PEH agreed receiving minimal incentives (e.g., money) would help start each day to stay in touch for receiving medication. In addition, clothing items like scarves, beanies, socks, and underwear would also be very helpful. Other PEH described the importance of providing “something that you cannot get” such as chocolate and soda. Other PEH described it would be helpful to be able to take showers as well. Such incentives could be as minimal as $1 per day or $10 per week. However, regular incentives were emphasized.
It would be like …a dollar, something that you can work with, you know… And it’ll give you something to work with to start the day out with.
In terms of how to track participants, one PEH reported that homeless participants can often be found in detox places and at hospitals. Another PEH noted that they can be found in the tents. One HSP oftentimes would find PEH in a local store and how helpful it was to just walk around the community and run into them.
Subtheme 2: Promoting Financial and Structural Support
Once PEH and HSP focus group participants heard more details about the design of the program; they sought to clarify more about the structural nature of incentives to be provided. Structural support included incentives linked to housing, and job training. PEH also questioned about transportation (e.g., bus tokens), refreshments, and when they would be incentivized. However, housing predominated the conversation. One PEH reiterated about the importance of housing to “lead them in some directions that they can start working; …so they can get off the street and step up a little bit more”. Further, the Chaplain emphasized the combination of housing and available drug addiction programs for which 226 beds were available.
PEH advised that the focus on who should get housing would be those who were HCV and that the length of time should be equivalent to the length of the program.
… Something like 90-day housing … because it’s eight weeks [length of treatment]… After all that’s done, then you give them the money. But …make sure that they’re taking it [the HCV medication]…like 90-day detox …
Discussion
The goal of this qualitative study was to assess the perceptions of PEH who have been diagnosed with HCV, and treatment providers, on the development of culturally sensitive designs to support HCV initiation and completion. Awareness of socio-cultural differences is crucial in the design of any successful intervention to achieve HCV sustained virologic response (Phillips et al., 2020). We discovered three major themes which included: 1) Essentials of Successful Participant Engagement and Retention: Role of Nurse-Led CHW in Promoting Tangible and Emotional Support; 2) Essentials of Successful Participant Engagement and Retention: Role of Nurse-Led CHW in Promoting Cognitive and Behavioral Support; and 3) Essentials of Successful Participant Engagement and Retention: Promoting Financial and Structural Resources.
Our findings revealed that essentials of successful participant engagement and retention included an appreciation of the support role of the nurse led, CHW, as well as the advocacy that they provided. CHW advocacy may include being a spokesperson, translator, or accompanying PEH to where they need to go. By having a support system which advocates for PEH in the community, PEH may be more likely to adhere to HCV treatment, with further understanding of how to maneuver and function within their community (Surey et al., 2019). Previous research has found that injection drugs or substance use was not necessarily associated with completion and cure of HCV (Avramovic, et al., 2020). However, competing needs often do jeopardize the use of services, such as screening, and cripple the ability to plan or follow up with PEH (Kerman & Sylvestre, 2020).
One barrier PEH experienced included HCV stigma which can be mitigated through building trust (Treloar et al., 2013). Engaging existing health and social service providers, including community outreach workers and peer counsellors who have expertise in PEH concerns is important (Fukuo et al., 2020). This prioritizes the role of trust in building and maintaining effective relationships between the HCV positive participant, their provider, and the healthcare infrastructure (Treloar et al., 2013). Further, by assisting PEH to access insurance, providing linkage to harm-reduction programs, and offering direct referrals, CHW and HSP build rapport and create the bonds of trust (Fukuo et al., 2020). Collaboration between local social services agencies that facilitate screening for shelter placement in the community is commendable (Fukuo et al., 2020).
One way in which CHW have built trust and rapport is through storytelling of their own lived experiences. Among PEH, this is an acceptable communication strategy and demonstrates that CHW are role models who have similar life course experiences and understand strengths and challenges. CHW also reiterate the importance of confidentiality and how PEH learn that sensitive information (e.g., drug and alcohol use) is kept confidential.
In our second theme, the promotion of resources in the form of cognitive and behavioral support emerged as part of a successful intervention design to support successful engagement and retention. PEH and HSP articulated the importance of cognitive support provided. Fear was another barrier to engagement of PEH in HCV treatment. A contributor to fearing treatment is a lack of education about the seriousness of HCV and the importance of a cure (Swan et al., 2010). The more HCV is discussed from a realistic standpoint of how one contracts the disease, what HCV is, and how the cure works, PEH are at a better position to make sound decisions towards corrective behaviors for their health.
Moreover, informing participants experiencing homelessness that current treatments use a proven drug, and that the drug is not experimental, goes a long way in overcoming the stereotypical fears of the Tuskegee era and other atrocities experienced (Gamble, 1997). Furthermore, sharing stories of completion success by CHW promote critical cognitive resources throughout the program. Education is critical to dispel historic concerns that persist regarding deleterious side effects as a reason for HCV treatment avoidance (Bass et al., 2018).
A third theme for successful design was the need for financial and structural resources. Previous research has found that lack of stability serves as a major hurdle to treatment consideration (Phillips et al., 2020). Among PEH with HCV, unstable housing, competing priorities that make keeping appointments challenging, and erroneous perceptions about HCV infection and treatment are indeed barriers to treatment (Daw et al., 2012; Malespin et al., 2019; Fukuo et al., 2020).
Our findings revealed that housing was a resource that can ensure completion of treatment for PEH. If housing were offered with simultaneous detox, addiction counseling, meetings, and other support mechanisms, PEH would have a clearer trajectory to recovery and treatment that can serve as a greater transition into society. We also found that providing essential clothing (e.g., undergarments, socks, etc) and other items not easily accessible will serve as motivator to keep a line of communication, access, and adherence among PEH. Providing these essential resources consistently will allow for continued access and trust with PEH.
Furthermore, food insecurity and lack of transportation jeopardize treatment initiation and completion and result in loss to follow up (Fukuo et al., 2020; Greer, 2019; Nguyen et al., 2020; Wohl et al., 2017). Thus, financial incentives can be a useful motivator to complete testing or taking medication (Masson et al., 2020). In a previous study conducted among injection drug users, small incremental incentives seemed justified given the high cost of DAA therapy (Gane, 2020). Innovations such as incentivizing treatment with nutrition and money, offering case-management services during therapy, facilitating access to mental and behavioral health, scheduling alternative clinic hours, and using community peer supports to maintain contact with, and encourage patients to follow through with the commitment to be treated, can lead to successful outcomes (Fokuo et al., 2020).
Limitations
Despite a multitude of strengths in this study, the generalizability of these results is subject to three main limitations. For instance, a disproportionate number of men versus women were able to take part in the FGS sessions. Second, these findings are limited to the recruitment within four main research sites within the Skid Row vicinity. Third, we were only able to learn the perspectives of some HSPs including CHWs, RNs, and Chaplains. Thus, future research needs to consider the perspectives of other mid-level providers (e.g., nurse practitioners, physician assistants, physicians) and social workers.
Summary and Future Research Implications
Notwithstanding these limitations and taken together, these findings contribute in three main ways to the extant literature and our understanding of HCV interventions among PEH and provide a basis for integrating these findings in future intervention trials. First, future interventions need to consider the utilization of the expanded role of a nurse-led CHW team as an extension of primary care providers who provide advocacy and support to meet clients, wherever they are, and may include both sheltered or unsheltered PEH. Second, keeping clients in an HCV treatment trial necessitates building trust with participants and dispelling concerns related to HCV treatment availability by providing education, information, and access to HCV treatment. Consideration of alcohol and drug use while on HCV treatment is critical as PEH may need wraparound services (e.g., drug treatment, housing, etc.) while participating in HCV treatment. Third, providing financial and structural resources throughout the program will likely aid in HCV treatment retention and medication adherence.
Several questions remain to be answered. At the individual and systems level, what are ways to overcome challenges of providing HCV treatment during the COVID-19 pandemic? Further, what HCV treatment considerations need to be made for COVID-19 positive participants? The goal of this study was to lay the groundwork for future research integrating the essentials of successful HCV program design including recruitment, engagement, design, delivery, and retention to support HCV cure among homeless populations.
Supplementary Material
Acknowledgements:
We are grateful to people experiencing homelessness (PEH) and homeless service providers (HSP) who have participated in this research study and helped us design a program which is acceptable, feasible, and culturally sensitive to lead to HCV cure among this underserved population.
Funding:
This work was supported by the National Institute on Minority Health and Health Disparities (NIMHD) grant number, R21MD013580
Contributor Information
Adeline M. Nyamathi, University of California, Irvine.
Sarah Akure Wall, University of California, Los Angeles.
Kartik Yadav, University of California, Irvine.
Sanghyuk S. Shin, University of California, Irvine.
Alicia Chang, Los Angeles County Department of Public Health Tuberculosis, Control Program.
Nicholas Arce, University of California, Irvine.
Helena Cuellar, University of California, Irvine.
Shannon Fernando, Los Angeles Christian Health Centers.
Kathryn White, Los Angeles Christian Health Centers.
Lillian Gelberg, David Geffen School of Medicine at UCLA and VA Greater Los Angeles Healthcare System.
Benissa E. Salem, University of California, Los Angeles.
References
- AbbVie (2020). Patient assistance program. https://www.abbvie.com/patients/patient-assistance.html?utm_source=myAbbVie-Assist-URL
- Alavi M, Poustchi H, Merat S, Kaveh-ei S, Rahimi-Movaghar A, Shadloo B, Hajarizadeh B, Grebely J, Dore GJ, Malekzadeh R (2019). An intervention to improve HCV testing, linkage to care, and treatment among people who use drugs in Tehran, Iran: The ENHANCE study. International Journal of Drug Policy. 1(72), 99–105. 10.1016/j.drugpo.2019.07.002 [DOI] [PubMed] [Google Scholar]
- American Association of The Study of Liver Diseases (AASLD) and Infectious Diseases Society of American (ASLD-IDSA). (2019). Key Populations: Identification and Management of HCV in People Who Inject Drugs. https://www.hcvguidelines.org/unique-populations/pwid
- Avramovic G, Oprea C, Surey J, Story A, Macías J, Cullen W, Iglesias M, Mc Hugh T, Crowley D, Naughton AM and Horan A, (2020). HepCare Europe: A service innovation project. HepCheck: Characteristics of the patient population with active infection as defined by HCV RNA. International Journal of Infectious Diseases, 91, pp.246–251. 10.1016/j.ijid.2019.11.027 [DOI] [PubMed] [Google Scholar]
- Bass SB, Jessop A, Maurer L, Gashat M, Al Hajji M, & Gutierrez M (2018). Mapping the barriers and facilitators of HCV treatment initiation in methadone maintenance therapy patients: Implications for intervention development. Journal of Health Communication, 23(1), 117–127. [DOI] [PubMed] [Google Scholar]
- Beijer U, Wolf A,Fazel S. Prevalence of tuberculosis, hepatitis C virus, and HIV in homeless people: a systematic review and meta-analysis. Lancet Infect Dis. 2012;12(11):859–870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benitez TM, Fernando SM, Amini C, & Saab S (2020). Geographically focused collocated hepatitis c screening and treatment in Los Angeles’s Skid Row. Digestive Diseases and Sciences, 1–9. [DOI] [PubMed] [Google Scholar]
- Betancourt JR, Green AR, Carrillo JE, & Ananeh-Firempong O, (2003). Defining cultural competence: A practical framework for addressing racial/ethnic disparities in health and health care. Public Health Reports (Washington, D.C. : 1974), 118(4), 293–302. 10.1093/phr/118.4.293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown MA, Gellatley W, Hoffman A, Dowdell L, Camac A, Francois R, Boston B, & Zekry A (2019). Medical complications of homelessness: A neglected side of men’s health. Internal Medicine Journal, 49(4), 455–460. 10.1111/imj.14139 [DOI] [PubMed] [Google Scholar]
- Buck DS, Rochon D, Davidson H, & McCurdy S (2004). Involving homeless persons in the leadership of a health care organization. Qualitative Health Research, 14(4), 513–525. https://journals.sagepub.com/doi/10.1177/1049732303262642?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed [DOI] [PubMed] [Google Scholar]
- Centers For Disease Control and Prevention (CDC) (2020a). Viral Hepatitis Surveillance – United States 2018. Published 2020. https://www.cdc.gov/hepatitis/statistics/2018surveillance/pdfs/2018HepSurveillanceRpt.pdf
- Centers For Disease Control and Prevention. (2020b). Chronic kidney disease initiative: Prevention and risk management. https://www.cdc.gov/kidneydisease/prevention-risk.html
- Childs E, Assoumou SA, Biello KB, Biancarelli DL, Drainoni ML, Edeza A, Salhaney P, Mimiaga MJ, & Bazzi AR (2019). Evidence-based and guideline-concurrent responses to narratives deferring HCV treatment among people who inject drugs. Harm Reduction Journal, 16(1), 14. 10.1186/s12954-019-0286-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daw MA, Dau AA, & Agnan MM (2012). Influence of healthcare-associated factors on the efficacy of hepatitis C therapy. The Scientific World Journal, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dedoose Version 8.3.35. (2020). Web Application for Managing, Analyzing, and Presenting Qualitative and Mixed Method Research Data. SocioCultural Research Consultants, LLC. https://urldefense.com/v3/__http://www.dedoose.com__;!!OLgoXmg!D2_fXSPv4p9bSYN2UtWG0pwrioNj6sM_J57bjH7bVdZYmzUMnjpZDsQTYK69MH7Kzw$ [Google Scholar]
- Department of Health & Human Services (DHSS) (2017). National Viral Hepatitis Action Plan 20172020. https://www.hhs.gov/sites/default/files/National%20Viral%20Hepatitis%20Action%20Plan%202017-2020.pdf.
- Dombrowski K, Sittner K, Crawford D, Welch-Lazoritz M, Habecker P, & Khan B (2016). Network approaches to substance use and HIV/Hepatitis C risk among homeless youth and adult women in the United States: A review. Health, 8(12), 1143. 10.4236/health.2016.812119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Downtown Women’s Center (DWC). (2020). About. Downtown Women’s Center. Retrieved July 16, 2020 from https://downtownwomenscenter.org/about/ [Google Scholar]
- Fokuo J. Konadu, Carmen L. Masson, August Anderson, Jesse Powell, Dylan Bush, Margaret Ricco, Barry Zevin, Claudia Ayala, & Khalili M. (2020). Recommendations for implementing hepatitis C virus care in homeless shelters: The stakeholder perspective. Hepatology communications, 4(5), 646–656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frey BB (Ed.). (2018). The SAGE encyclopedia of educational research, measurement, and evaluation. Sage Publications. [Google Scholar]
- Fuster D, & Gelberg L (2019). Community screening, identification, and referral to primary care, for hepatitis C, B, and HIV among homeless persons in Los Angeles. Journal of community health, 44(6), 1044–1054. https://link.springer.com/content/pdf/10.1007/s10900-019-00679-w.pdf [DOI] [PubMed] [Google Scholar]
- Gane E (2020). Should we incentivize patients to take hepatitis C virus therapy? Clinical Dilemmas in Viral Liver Disease, 122–124. [Google Scholar]
- Gelberg L, Robertson MJ, Arangua L, Leake BD, Sumner G, Moe A, … & Nyamathi A. (2012). Prevalence, distribution, and correlates of hepatitis C virus infection among homeless adults in Los Angeles. Public Health Reports, 127(4), 407–421. 10.1177/003335491212700409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghose T, Shubert V, Poitevien V, Choudhuri S, Gross R (2019). Effectiveness of a viral load suppression intervention for highly vulnerable people living with HIV. AIDS Behav 23, 2443–2452. 10.1007/s10461-019-02509-5 [DOI] [PubMed] [Google Scholar]
- Gonzalez-Guarda RM, Jones EJ, Cohn E, Gillespie GL and Bowen F (2017). Advancing nursing science through community advisory boards: Working effectively across diverse communities. ANS. Advances in Nursing Science, 40(3), p.278. 10.1097/ANS.0000000000000167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grebely J, Dore GJ, Morin S, Rockstroh JK, & Klein MB (2017). Elimination of HCV as a public health concern among people who inject drugs by 2030 - What will it take to get there? Journal of the International AIDS Society, 20(1), 22146. 10.7448/IAS.20.1.22146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greer PJ (2019). The health care of homeless persons - Part I - hepatitis C 41. National healthcare for the homeless council. p41–46 https://nhchc.org/wp-content/uploads/2019/08/HepatitisC.pdf [Google Scholar]
- Hanlon P, Yeoman L, Gibson L, Esiovwa R, Williamson AE, Mair FS, & Lowrie R (2018). A systematic review of interventions by healthcare professionals to improve management of non-communicable diseases and communicable diseases requiring long-term care in adults who are homeless. British Medical Journal Open, 8(4), e020161. 10.1136/bmjopen-2017-020161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harney BL, Whitton B, Lim C, Paige E, McDonald B, Nolan S, Pemberton D, Hellard ME and Doyle JS (2019). Quantitative evaluation of an integrated nurse model of care providing hepatitis C treatment to people attending homeless services in Melbourne, Australia. International Journal of Drug Policy, 72, 195–198. 10.1016/j.drugpo.2019.02.012 [DOI] [PubMed] [Google Scholar]
- Henry-Akintobi T, Laster N, Trotter J, Jacobs D, Johnson T, King Gordon T, & Miller A (2016). The health, enlightenment, awareness, and living (HEAL) intervention: Outcome of an HIV and hepatitis B and C risk reduction intervention. International Journal of Environmental Research and Public Health, 13(10), 948. 10.3390/ijerph13100948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henwood BF, Lahey J, Harris T, Rhoades H, & Wenzel SL (2018). Understanding Risk Environments in Permanent Supportive Housing for Formerly Homeless Adults. Qual Health Res, 28(13), 2011–2019. 10.1177/1049732318785355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hepatitis C Online (2021). Lesson 1. Treatment of HCV Genotype 1 - Topic 1. Introduction. https://www.hepatitisc.uw.edu/custom/treatment/treatment-genotype-1/1
- Ho SB, Bräu N, Cheung R, Liu L, Sanchez C, Sklar M, Phelps TE, Marcus SG, Wasil MM, Tisi A, Huynh L, Robinson SK, Gifford AL, Asch SM, & Groessl EJ (2015). Integrated care increases treatment and improves outcomes of patients with chronic hepatitis C virus infection and psychiatric illness or substance abuse. Clinical Gastroenterology and Hepatology 13(11), 2005–14.e143. 10.1016/j.cgh.2015.02.022 [DOI] [PubMed] [Google Scholar]
- Hofmeister MG, Rosenthal EM, Barker LK, Rosenberg ES, Barranco MA, Hall EW, Edlin BR, Mermin J, Ward JW, & Ryerson AB. (2019). Estimating prevalence of hepatitis C virus infection in the United States, 2013–2016. Hepatology (Baltimore, Md.), 69(3), 1020–1031. 10.1002/hep.30297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Illumination Foundation (IF). (2020). Our Impact. Illumination Foundation. Retrieved July 16, 2020 from https://urldefense.com/v3/__https://www.ifhomeless.org/about-illumination-foundation/impact/__;!!OLgoXmg!D2_fXSPv4p9bSYN2UtWG0pwrioNj6sM_J57bjH7bVdZYmzUMnjpZDsQTYK6o-zho9Q$ [Google Scholar]
- Kardish C. 2014. The risky business of limiting Medicaid access to Sovaldi. https://www.governing.com/topics/health-human-services/gov-hepatitis-coverage-solvaldi-lawsuits.html
- Kardish C 2014. The risky business of limiting Medicaid access to Sovaldi. https://www.governing.com/topics/health-human-services/gov-hepatitis-coverage-solvaldi-lawsuits.html
- Kerman N, & Sylvestre J (2020). Surviving versus living life: Capabilities and service use among adults with mental health problems and histories of homelessness. Health & Social Care in the Community, 28(2), 414–422. 10.1111/hsc.12873 [DOI] [PubMed] [Google Scholar]
- Kohli A, Osinusi A, Sims Z, Nelson A, Meissner EG, Barrett LL, Bon D, Marti MM, Silk R, Kotb C, Gross C, Jolley TA, Sidharthan S, Petersen T, Townsend K, Egerson D, Kapoor R, Spurlin E, Sneller M, Proschan M, … Kottilil S (2015). Virological response after 6 week triple-drug regimens for hepatitis C: a proof-of-concept phase 2A cohort study. Lancet (London, England), 385(9973), 1107–1113. 10.1016/S0140-6736(14)61228-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambert JS, Murtaugh R, Menezes D, O’Carroll A, Murphy C, Cullen W, McHugh T, Avramovic G, Tinago W, & Van Hout MC (2019). HepCheck Dublin: An intensified hepatitis C screening programme in a homeless population demonstrates the need for alternative models of care. BMC Infectious Diseases, 19(1), 1–9. 10.1186/s12879-019-3748-2J [DOI] [PMC free article] [PubMed] [Google Scholar]
- Los Angeles Christian Health Centers (LACHC). (2020). Los Angeles Christian Health Centers. Los Angeles Christian Health Centers. Retrieved July 16, 2020 from https://www.lachc.com/ [Google Scholar]
- MacLellan J, Surey J, Abubakar I, Stagg HR, & Mannell J (2017). Using peer advocates to improve access to services among hard-to-reach populations with hepatitis C: A qualitative study of client and provider relationships. Harm Reduction Journal, 14(1), 1–9. 10.1186/s12954-017-0202-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malespin M, Harris C, Kanar O, Jackman K, Smotherman C, Johnston A, Ferm J, de Melo SW Jr, Scolapio JS, Nelson DR, & Cotler SJ (2019). Barriers to treatment of chronic hepatitis C with direct acting antivirals in an urban clinic. Annals of Hepatology, 18(2), pp.304–309. [DOI] [PubMed] [Google Scholar]
- Masson CL, Fokuo JK, Anderson A, Powell J, Zevin B, Bush D, & Khalili M (2020). Clients’ perceptions of barriers and facilitators to implementing hepatitis C virus care in homeless shelters. BMC Infectious Diseases, 20, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mavyret, (2019). Cost https://www.mavyret.com/cost
- Moore-Nadler M, Clanton C, & Roussel L (2020). Storytelling to Capture the Health Care Perspective of People Who Are Homeless. Qual Health Res, 30(2), 182–195. 10.1177/1049732319857058 [DOI] [PubMed] [Google Scholar]
- Nguyen P, Vutien P, Hoang J, Trinh S, Le A, Yasukawa LA, Weber S, Henry L & Nguyen MH (2017). Barriers to care for chronic hepatitis C in the direct-acting antiviral era: Asingle-centre experience. BMJ Open Gastroenterology, 4(1). e000181. 10.1136/bmjgast-2017-000181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyamathi A, Salem BE, Zhang S, Farabee D, Hall B, Khalilifard F, & Leake B (2015). Nursing case management, peer coaching, and hepatitis a and B vaccine completion among homeless men recently released on parole: Randomized clinical trial. Nurs Res, 64(3), 177–189. 10.1097/NNR.0000000000000083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyamathi AM, Shin SS, Smeltzer J, Salem BE, Yadav K, Ekstrand ML, Turner SF, & Faucette M (2017). Achieving drug and alcohol abstinence among recently incarcerated homeless women: A randomized controlled trial comparing dialectical behavioral therapy-case management with a health promotion program. Nurs Res, 66(6), 432–441. 10.1097/NNR.0000000000000249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyamathi A, Shin SS, Smeltzer J, Salem B, Yadav K, Krogh D, & Ekstrand M (2018). Effectiveness of dialectical behavioral therapy on reduction of recidivism among recently incarcerated homeless women: A pilot study. Int J Offender Ther Comp Criminol, 62(15), 4796–4813. 10.1177/0306624X18785516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Sullivan M, Jones AM, Gage H, Jordan J, MacPepple E, Williams H and Verma S, 2020. ITTREAT (Integrated Community Test-Stage-TREAT) Hepatitis C service for people who use drugs: Real-world outcomes. Liver International, 40(5), pp.1021–1031. 10.1111/liv.14403 [DOI] [PubMed] [Google Scholar]
- Page K, Yu M, Cohen J, Evans J, Shumway M, & Riley ED (2017). HCV screening in a cohort of HIV infected and uninfected homeless and marginally housed women in San Francisco, California. BMC Public Health, 17(1), 171. 10.1186/s12889-017-4102-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips C, Schulkind J, O’Sullivan M, Edelman N, Smith HE, Verma S, & Jones CJ (2020). Improving access to care for people who inject drugs: Qualitative evaluation of project ITTREAT—An integrated community hepatitis C service. Journal of Viral Hepatitis, 27(2), 176–187. 10.1111/jvh.13214 [DOI] [PubMed] [Google Scholar]
- Ramsay N, Hossain R, Moore M, Milo M, & Brown A (2019). Health care while homeless: barriers, facilitators, and the lived experiences of homeless individuals accessing health care in a Canadian regional municipality. Qualitative Health Research, 29(13), 1839–1849. https://journals.sagepub.com/doi/10.1177/1049732319829434?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed [DOI] [PubMed] [Google Scholar]
- Rifai MA, Moles JK, Short DD (2006). Hepatitis C treatment eligibility and outcomes among patients with psychiatric illness. Psychiat Serv, 57(4). 10.1176/ps.2006.57.4.570 [DOI] [PubMed] [Google Scholar]
- Safreed-Harmon K, Blach S, Aleman S, Bollerup S, Cooke G, Dalgard O, Dillon JF, Dore GJ, Duberg AS, Grebely J, Boe Kielland K, Midgard H, Porter K, Razavi H, Tyndall M, Weis N, & Lazarus JV (2019). The consensus hepatitis C cascade of care: Standardized reporting to monitor progress toward elimination. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America, 69(12), 2218–2227. 10.1093/cid/ciz714 [DOI] [PubMed] [Google Scholar]
- Saldaña J (2009). The coding manual for qualitative researchers. Sage Publications Ltd. [Google Scholar]
- Salem BE, Kwon J, Ekstrand ML, Hall E, Turner SF, Faucette M, & Slaughter R (2021). Transitioning into the community: Perceptions of barriers and facilitators experienced by formerly incarcerated, homeless women during reentry-a qualitative study. Community Ment Health J. 10.1007/s10597-020-00748-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salem BE, Ma-Pham J, Chen S, Brecht ML, Antonio AL, & Ames M (2017). Impact of a community-based frailty intervention among middle-aged and older prefrail and frail homeless women: A pilot randomized controlled trial. Community Ment Health J, 53(6), 688–694. 10.1007/s10597-017-0147-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salem BE, Klansek E, Morisky DE, Shin SS, Yadav K, Chang AH, & Nyamathi AM (2020). Acceptability and feasibility of a nurse-led, community health worker partnered latent tuberculosis medication adherence model for homeless adults. Int J Environ Res Public Health, 17(22). 10.3390/ijerph17228342 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skeer MR, Ladin K, Wilkins LE, Landy DM, & Stopka TJ (2018). ‘Hep C’s like the common cold’: Understanding barriers along the HCV care continuum among young people who inject drugs. Drug and Alcohol Dependence, 190, 246–254. 10.1016/j.drugalcdep.2018.06.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shenton AK (2004). Strategies for ensuring trustworthiness in qualitative research projects. Education for Information, 22(2), 63–75. 10.3233/EFI-2004-22201 [DOI] [Google Scholar]
- Surey J, Menezes D, Francis M, Gibbons J, Sultan B, Miah A, Abubakar I, & Story A (2019). From peer-based to peer-led: Redefining the role of peers across the hepatitis C care pathway: HepCare Europe. The Journal of Antimicrobial Chemotherapy, 74(5), 17–23. 10.1093/jac/dkz452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swan D, Long J, Carr O, Flanagan J, Irish H, Keating S, . . . Cullen W. (2010). Barriers to and facilitators of hepatitis C testing, management, and treatment among current and former injecting drug users: A qualitative exploration. AIDS Patient Care and STDs, 24(12), 753–762. doi: 10.1089/apc.2010.0142 [DOI] [PubMed] [Google Scholar]
- Tatar M, Keeshin SW, Mailliard M, & Wilson FA (2020). Cost-effectiveness of universal and targeted hepatitis C virus screening in the United States. JAMA network open, 3(9), e2015756. 10.1001/jamanetworkopen.2020.15756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong A, Sainsbury P, & Craig J (2007). Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. International Journal for Quality in Health Care, 19(6), 349–357. 10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- Treloar C, Rance J, & Backmund M (2013). Understanding barriers to hepatitis C virus care and stigmatization from a social perspective. Clinical Infectious Diseases, 57(suppl_2), [DOI] [PubMed] [Google Scholar]
- United States Department of Housing and Urban Development (USDHUD). (2019). HUD 2019 Continuum of Care Homeless Assistance Programs Homeless Populations and Subpopulations in https://files.hudexchange.info/reports/published/CoC_PopSub_NatlTerrDC_2019.pdf
- Werb D, Garfein R, Kerr T, Davidson P, Roux P, Jauffret-Roustide M, Auriacombe M, Small W and Strathdee SA (2016). A socio-structural approach to preventing injection drug use initiation: Rationale for the PRIMER study. Harm Reduction Journal, 13(1), pp.1–10. 10.1186/s12954-016-0114-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams BE, Nelons D, Seaman A, Witkowska M, Ronan W, Wheelock H, Zaman A and Garcia J (2019). Life projects: The transformative potential of direct-acting antiviral treatment for hepatitis C among people who inject drugs. International Journal of Drug Policy, 72,138–145. 10.1016/j.drugpo.2019.03.015 [DOI] [PubMed] [Google Scholar]
- Zhang SX, Shoptaw S, Reback CJ, Yadav K, & Nyamathi AM (2018). Cost-effective way to reduce stimulant-abuse among gay/bisexual men and transgender women: A randomized clinical trial with a cost comparison. Public Health, 154, 151–160. 10.1016/j.puhe.2017.10.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.