Abstract
Purpose/Objective:
To explore the impact of the COVID-19 pandemic as experienced and reported by individuals living with a spinal cord injury (SCI).
Research Method/Design:
Descriptive qualitative design using in-depth semistructured interviews with individuals with SCI (n = 33) followed by thematic analysis.
Results:
Three main themes described impacts of the COVID-19 pandemic, (a) Impact on health care use; subthemes elaborated that this was attributable to in-person health care facility restrictions or individual decisions to delay care. Individuals with SCI experienced lapses in primary and SCI-specialty care, rehabilitation/therapy services, and home care, but some made use of telehealth services. (b) Impact on weight and/or weight management lifestyle behaviors; subthemes discussed that engagement in physical activity declined because of fitness center closures, recreational activity cancellations, and safety precautions limiting community-based and outdoor activities. The pandemic disrupted participants’ independence in purchasing and making preferred food selections which impacted healthy eating. Participants ate due to boredom, at nonmealtimes, and consumed unhealthy foods during the pandemic, (c) Impact on psychosocial factors; included subthemes noting reduced social interactions, social participation, and ability to pursue pastimes with family, friends, and groups they belonged to. The pandemic also triggered emotional reactions such as worry, fear, doubt, demotivation, and feelings of social isolation.
Conclusions:
Our findings highlight the magnitude of consequences faced by individuals with SCI when restrictions to health care, healthy lifestyle endeavors, and social participation occurred during the COVID-19 pandemic. Findings may inform SCI health care providers on what is needed in response to future public health or natural disaster crises.
Keywords: COVID-19 pandemic, weight, healthcare use, psychosocial outcomes, qualitative research
Introduction
There is increasing evidence that public health crises, such as the SARS-CoV-2 (COVID-19) pandemic may have several negative impacts in individuals’ lives, including limited receipt of needed health care, reduced participation in healthy lifestyle behaviors, and poor psychosocial outcomes, all of which influence overall health and well-being (Matsuoka & Sumida, 2021). The COVID-19 pandemic has resulted in decreases in health care use, including preventive care and chronic disease management (Czeisler et al., 2020; Mehrotra et al., 2020), in populations at large. Four in 10 adults reported delays or nonreceipt of health care services (Mehrotra et al., 2020). Rehabilitation health care providers, internationally, have reported that the pandemic has limited access to health care and support services specifically For individuals with spinal cord injuries (SCI). In fact, 28% reported lack of availability for in-person visits, nearly half reported decreased availability of rehabilitation services, and 43% said their patients with SCI leared attending in-person visits to address their medical concerns because they were afraid of virus exposure (Gustafson et al., 2021). An online survey of individuals with SCI living in Italy indicated that the majority experienced deferred or cancelled non-COVID related health services (Right et al., 2022). Although rehabilitation health care providers reported a 25% increase in use of teteheallh, leading to 60% of individuals with SCI using it during the pandemic, most providers felt that telehealth technology did not completely meet the needs of their patients with SCI (Gustafson et al., 2021). Lack of or delays in health care services may lead to unmet care needs and potentially serious and/or irreversible health consequences.
The COVID-19 pandemic has also led to major changes in individuals’ lifestyle behaviors, often including a decrease in physical activity levels or leisure time physical activities and/or a deviation from healthy eating habits. During the pandemic, individuals with neurological conditions experienced a decreased level of physical activity participation, which was associated with worsening of disease symptoms and psychosocial concerns (Abasiyantk et al., 2022). Individuals with thoracic level SCI who used manual wheelchairs full-time engaged in lower levels of physical activity during the pandemic compared with the prepandennc period (Marco-Ahulló et al., 2021). In another study of individuals without SCI, more than half of survey participants reported increased snacking between meals and more sitting or screen time during the pandemic; in addition, higher body mass index was significantly associated with these variables (Hammouri et al., 2022). Prior to COVID-19, complex challenges around physical activity and healthy eating were present among persons with SCI (Bates et al., 2022; LaVela, Burkhart, et al., 2021; Pellegrini et al., 2021); hence, it is not surprising that the COVID-19 pandemic may have had even greater impacts on participation in healthy lifestyle behaviors in this population.
The chronic SCI population is vulnerable to negative health outcomes associated with excess weight including metabolic complications (Smith & Yarar-Fisher, 2016), and a high prevalence of cardiometabolic conditions (LaVela, Evans, et al., 2012) such as diabetes, dyslipidemia, cardiovascular disease, and hypertension (Farkas & Galer, 2018). Well over half of adults with chronic SCI meet criteria for overweight or obesity (Chen et al., 2011; Hatchett et al., 2016; Wen et al., 2021). Several barriers to weight management, at the individual, socioeconomic, and health care organization levels, among individuals with SCI have been documented (Pellegrini et al., 2021). In a pandemic environment, disruptions in health care use and healthy lifestyle behaviors, such as physical activity and healthy eating, may be especially impactful among individuals with SCI considering the many biological, individual, and social contextual factors at play (World Health Organization, 2013).
With regard to psychosocial outcomes, reports from a mailed survey of newly injured individuals with SCI in Japan showed that 40% of individuals experienced low health-related quality of life during the pandemic (Matsuoka & Sumida, 2021) and an online survey showed lower quality of life after the pandemic versus before (Elaraby et al., 2022). Other survey studies (mostly online, one by telephone) reported that individuals with SCI experienced anxiety (Gustafson et al., 2021: Hearn et al., 2021; Vives Alvarado et al., 2021) and depression (García-Rudolph et al., 2021; Gustafson et al., 2021; Vives Alvarado et al., 2021) during the pandemic. In addition, individuals with SCI were at risk of feeling socially isolated in response to the pandemic (Hearn et al., 2021; Mikolajczyk et al., 2021; Monden et al., 2021).
This handful of studies have used structured surveys with rehabilitation health care providers or individuals with neurological conditions, including SCI, to team about challenges during the COVID-19 pandemic; however, there are few studies that have used in-depth qualitative interviews to understand lived experiences and impacts of the pandemic from the perspectives of individuals with SCI. Hence, understanding patient lived experience through the patient’s voice, including their personal narratives and stories, is key knowledge that may enable health care providers to tailor care to meet patient’s needs and deliver patient-centered care. The objective of this study was to qualitatively explore the impact of The COVID-19 pandemic as experienced and reported by individuals wilh SCI.
Method
Transparency and Openness
We report how we determined our sample size, all data exclusions, all manipulations, and all measures in the study, and we Followed Journal Article Reporting Standards for qualitative reporting (American Psychological Association, 2000). Interview guide items as described in the Method section are provided as a figure. There were no relationships or interactions between the participants and the researchers prior to the research. NVivo software, designed to support layered qualitative analysis and concept building, was used to organize the data (QSR International. Version 12 NVivo, 2018; Doncaster, Victoria, Australia). Deidentified data will be made available on reasonable request to the senior author (study PI) pending approval of the organization’s institutional review board.
Design and Framework
A descriptive qualitative design using in-depth semistructured interviews and thematic analysis methodology (Braun & Clarke, 2006) was used to answer the research question: In what ways were individuals with SCI impacted by the COVID-19 pandemic? Thematic analysis was selected because there was limited research on the topic and the participants views on the topic were unknown (Braun & Clarke, 2006). The flexibility of this approach permitted us to understand how individuals make meaning of experiences and how biopsychosocial context (WHO, 2013) affects those meanings, while remaining focused on the data and recognizing practical and realistic limitations (Braun & Clarke, 2006).
The study was guided by the International Classification of Functioning, Disability, and Health (ICF) (WHO, 2013) which encourages individuals to be viewed in context. For example, an individual’s disability and level of functioning are factors of interactions between the person’s health condition (SCI) and their environment. The ICF provided an ideal framework to examine how the environment (COVID-19 pandemic) impacted the health, function, and disability of individuals with SCI in the context of biopsychosocial factors (biological, individual/personal, and social; WHO, 2013). Specifically, the ICF domains of body functions and structures, activities, participation, and environmental factors in the context of the pandemic, in part, drove our inquiry (detailed in the interview guide section below) and analysis of data. This study was approved by the Stanford University Institutional Review Board and the Research & Development committee of the VA Palo Alto Health Care System.
Setting
The Veterans Health Administration (VHA) SCI System of Care includes 25 regional SCI Centers across the United States, which provide comprehensive, coordinated, lifelong care delivered by interdisciplinary teams. The system also includes over 120 SCI sites at other VHA medical centers and outpatient clinics. VHA cares for over a quarter of individuals with SCI in the United States.
Sample/Recruitment
VA medical record databases were used to identify veterans with at least two occurrences of ICD 9/10 codes for paraplegia or tetraplegia during FY2016–2019 separated by two years, in addition to at least one SCI health care encounter in FY2019. Our sample included adult veterans with chronic SCI. This included those with both traumatic and nontraumatic SCI, including nonmalignant neoplasms resulting in neurologic deficit; vascular insults of a thromboembolic, hemorrhagic, or ischemic nature; cauda equina syndrome producing neurologic deficit; inflammatory disease of the spine, spinal cord, or cauda equina resulting in nonprogressive neurologic deficit; and demyelinating disease of the spinal cord. Exclusions included SCI duration of less than two years and having acute or progressive central nervous system disease, for example, Multiple Sclerosis, amyotrophic lateral sclerosis. This yielded a sampling pool of 20,642 eligible veterans with SCI, from which we generated a random sample by sorting the sampling pool into a random sequence using an online randomizer and then used purposeful criterion sampling (Palinkas et al., 2015) as a secondary sampling approach to invite a diverse sample of individuals to participate in interviews. In January 2021, invitation letters were sent in small batches in the order of the random sequence. Veterans received $50.00 for participation in the one-time interview.
We followed the guidance of Adler & Adler (2012) and Warren (2002), who recommend 20–40 qualitative interviews, for our target sample size, which is deemed sufficient for the scale of the current study because it is ample to unfold a rich understanding, but small enough to facilitate in-depth analysis. Of 104 veterans with SCI to whom we mailed invitation letters and followed-up by telephone, 33 eligible veterans completed interviews for this study. Enrollment ended once the target sample was reached. Al initial contact, potential participants were screened for inclusion criteria to ensure they had a SCI and spoke fluent English.
Data Collection
Electronic Medical Record Database
We used VA electronic medical record databases to obtain basic demographic variables (sex, age, race, ethnicity, marital status) and injury characteristics (injury level and completeness).
Interviews
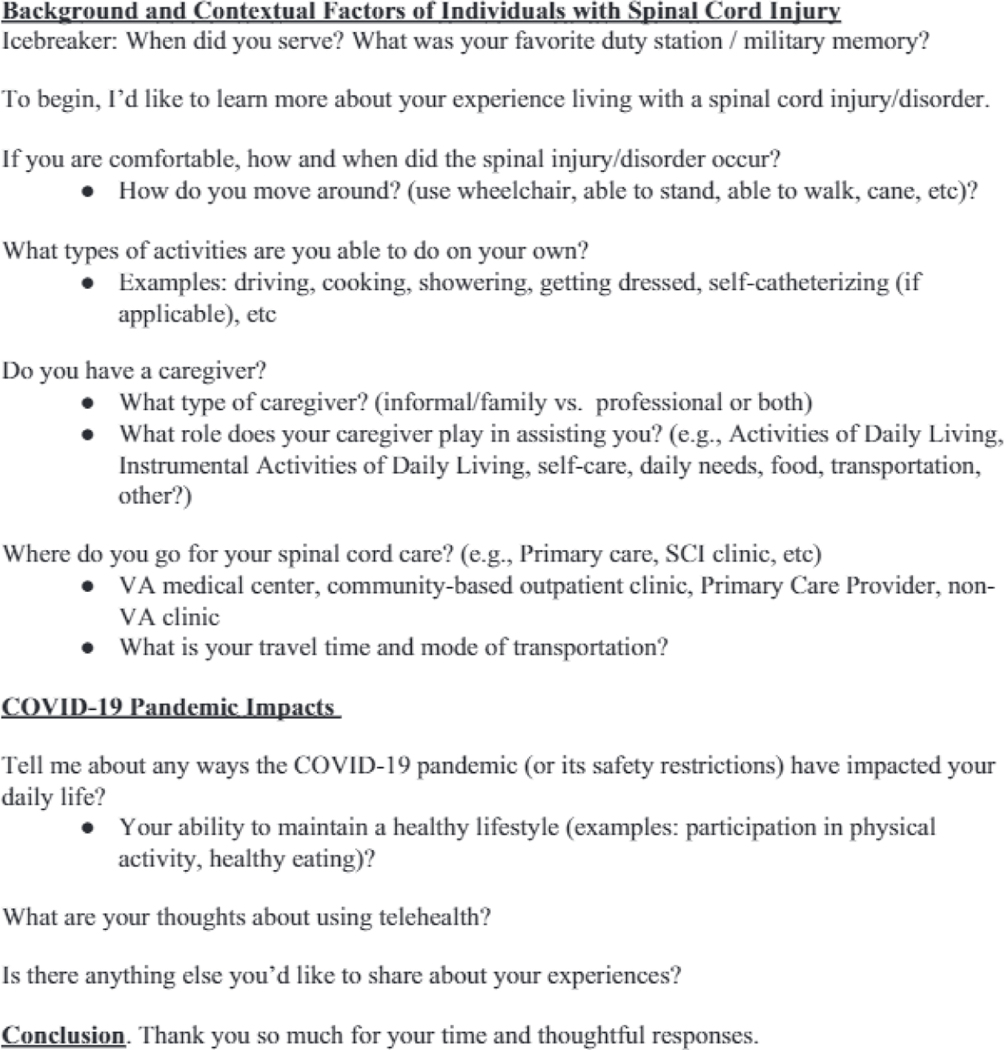
Interviews were conducted by two researchers experienced in qualitative methodology, interviewing techniques, health services research, public health, and anthropology (J.W.,. A.N.). The interviews were conducted by telephone in 2021. Each interview was one-on-one, look about 60 minutes, and followed a semistructured interview guide. The interview guide was developed based on the ICF-related literature and experience of the research team (Kallio et al., 2016), which included health professionals knowledgeable in SCI medicine, rehabilitation, psychology, health services research, and public health. The interview guide items asked individuals about their SCI level of impairment, what types of movement they were or were not able do on their own, and whether the pandemic impacted impairments owing to SCI (ICF domain: body functions and structures); what activity limitations, for example, general tasks, mobility were experienced during the pandemic (ICF domain: activities); whether and what participation restrictions were experienced during the pandemic, including interpersonal interactions and social participation (ICF domain: participation); and about how the individuals’ internal and external environment, for example, services, systems, built environment was influenced (ICF domain: environmental factors). We piloted the interview guide draft by conducting interviews with three individuals with SCI and asking their feedback about wording, order, and flow and incorporated feedback to ensure question applicability and clarity. An excerpt of relevant questions from the interview guide is shown in Figure 1.
Figure 1. Example Questions From Interviews With Individuals With SCI.
Note. There are no right or wrong answers, so please feel free to share honest responses. My goal is to understand your experiences and needs, so that we can improve care and resources for other individuals with SCI, This is meant to be a non-judgmental conversation, so please know that I will not judge you or what you say. Your responses will not be shared with your providers. Feel free to let me know if you need to take a break at any time or feel uncomfortable with any questions.
Interviews were audio-recorded and transcribed verbatim by a professional transcription service. A two-step quality control process was used that entailed initial transcription followed by audio-review verification to ensure accuracy of each transcript.
Analysis
Descriptive statistics were calculated for demographic and injury characteristics; this included frequencies for categorical variables and mean, range, and standard deviation for continuous variables. Transcripts were coded and analyzed using thematic analysis methodology (Braun & Clarke, 2006). The perspectives of the authors were ontological (reflecting realities from multiple participants and researchers and driven by quotes and themes from the data signifying individuals’ views and experiences) and methodological (shaped by the researchers experiences in collecting and analyzing the data; Creswell. 2018).
Two research scientists (S.L., J.W.) with experience in qualitative methodology and backgrounds in public health, physical medicine and rehabilitation, disability studies, and health services research, and a history of conducting SCI research conducted a thematic analysis driven by interview content. First, we became familiar with the data by listening to recorded interviews to get a sense of the breadth of the data content and reading textual data from the interview transcripts to begin to learn what the data meant. We used a mixed inductive-deductive approach to generate initial codes and create an initial codebook. This included applying the ICF domains to the data (deductive), such that the COVID-19 pandemic impacts were a factor of internal and external factors, including body functions/impairments, activities and activity limitations, participation in life and participation restrictions, and environmental factors that affect an individuals’ experiences (WHO, 2013), for example, closed facilities as barriers, lack of care in home environment, community posed as a threat. We also identified constructs driven directly by the data (inductive). We used in vivo and descriptive open coding, which allowed for identification of codes based on interpretation of the data and emphasized content meaning and quality rather than quantity (Frost et al, 2011; Miles et al., 2014). We then reviewed coded data to look for themes representing patterns of meaning and to explore relationships between themes. Next, we checked themes against groups of data excerpts and against all transcripts. In this phase, we assessed fit and modified codes by either relocating or discarding them and fine-tuned themes until saturation was reached (Bradley et al., 2007; Braun & Clarke, 2006; Miles et al, 2014). Saturation was defined as the point when no additional new information on higher level concepts or characterizations of concepts was found in the data (Ando et al., 2014). To reinforce dependability and confirmability, we maintained an audit trail of the themes and rationale for decisions using field notes, a codebook, coding rules, and analytic memos (Nowell et al., 2017). We constructed, named, and defined final themes, then met to compare and resolve discrepancies until agreement was reached (Kurasaki, 2000; Miles et al., 2014).
Results
Sample Characteristics
Participants included 33 veterans with SCI, of whom 61% were male, 49% were non-Hispanic White, 24% were Hispanic or Latino, and 18% Black or African American. Slightly over half had tetraplegia (55%) and 42% sustained complete injuries, 55% incomplete, and for 3% this was unknown. Detailed participant characteristics are shown in Table 1.
Table 1.
Participant Characteristics (n = 33)
| Characteristic | (n) Frequency or M, Range, SD |
|---|---|
| Sex | |
| Male | (20) 60.6% |
| Female | (13) 39.4% |
| Race | |
| White (non-Hispanic) | (16) 48.5% |
| Black/African American | (6) 18.2% |
| American Indian or Alaska Native | (4) 12.1% |
| Asian, Native/Hawaiian/other Pacific Islander | (3) 9.1% |
| Unknown | (4) 12.1% |
| Ethnicity | |
| Not Hispanic or Latino | (24) 72.7% |
| Hispanic or Latino | (8) 24.2% |
| Unknown | (1) 3.1% |
| Age (years), M, range, SD | 59, 29–84, 12 |
| Marital status | |
| Separated/Divorced | (13) 39.4% |
| Married | (10) 30.3% |
| Never married | (6) 18.2% |
| Widowed | (4) 12.1% |
| Type/level of injury | |
| Tetraplegia | (18) 54.5% |
| Paraplegia | (13) 39.4% |
| Unknown | (2) 6.1% |
| Injury completeness | |
| Incomplete | (18) 54.5% |
| Complete | (14) 42.4% |
| Unknown | (1) 3.1% |
Themes
Three main themes were identified from the data that illustrate the impacts of the COVID-19 pandemic on individuals with SCI’s (1) health care use subthemes a) not receiving health care services due to delays or cancellations imposed by the facility or by personal choice, b) lack of in-home formal (paid) caregiver ability, c) experienced alternative health care delivery options; (2) weight and/or weight management lifestyle behaviors: physical activity subthemes a) fitness facilities closed, activity classes or activity events cancelled, b) personal choice to avoid PA/aclivily in the community to avoid virus exposure, c) community /recreational resources and activities unavailable; healthy eating subthemes a) interruptions in food choices (access), b) eating out of boredom, at nonmealtimes, and unhealthy foods); and (3) psychosocial factors: subthemes a) missing being around people and getting together with family and friends, b) unable to attend gatherings with organized groups, and emotional reactions or feelings triggered by the pandemic. Key themes and subthemes (underlined) are described below accompanied by representative quotations. A summary of themes and subthemes may be found in Table 2. Each quotation is identified by a unique participant ID and descriptions of each participant by ID are shown in Table 3.
Table 2.
Themes and Subthemes From Thematic Analysis
| Themes | Subthemes |
|---|---|
| Theme 1. COVID-19 pandemic impact on healthcare use | a. not receiving healthcare services due to delays and cancellations imposed by the healthcare facility or by choice b. lack of in-home formal (paid) caregiver availability c. experienced alternative healthcare delivery options |
| Theme 2. COVID-19 pandemic impact on weight and weight management lifestyle behaviors |
Physical activity a. fitness facilities closed/activity classes or events cancelled b. personal choice to avoid activity/PA in the community to avoid virus exposure c. community/recreational resources/activities unavailable Healthy eating a. interruptions in food choices b. eating out of boredom, at nonmealtimes, and eating unhealthy foods |
| Theme 3. COVID-19 pandemic impact on psychosocial factors | a. missing being around people and getting together with family and friends b. unable to attend gatherings with organized groups c. triggered emotional reactions or feelings |
Table 3.
Demographic and Injury Characteristics of Individuals With SCI by ID (n = 33)
| ID | Sex | Age (y) | Race/Ethnicity | Level and completeness of injury |
|---|---|---|---|---|
| V01 | F | 84 | White | Tetraplegia, incomplete |
| V02 | M | 65 | White | Paraplegia, incomplete |
| V03 | M | 67 | White | Paraplegia, incomplete |
| V04 | F | 61 | American Indian or Alaska Native | Paraplegia, incomplete |
| V05 | F | 59 | Black or African American | Tetraplegia, incomplete |
| V06 | F | 44 | American Indian or Alaska Native | Tetraplegia, incomplete |
| V07 | M | 56 | Black or African American | Paraplegia, complete |
| V08 | M | 64 | American Indian or Alaska Native | Tetraplegia, complete |
| V09 | M | 65 | White | Paraplegia, complete |
| V10 | M | 69 | Black or African American | Tetraplegia, incomplete |
| V11 | M | 61 | Unknown | Tetraplegia, complete |
| V12 | F | 66 | White | Unknown |
| VI3 | M | 34 | Asian, Native/Hawaiian/other Pacific Islander | Paraplegia, incomplete |
| V14 | M | 44 | White | Unknown |
| V15 | M | 54 | White | Tetraplegia, complete |
| V16 | F | 58 | Asian, Native/Hawaiian/other Pacific Islander | Paraplegia, incomplete |
| V17 | M | 70 | Black or African American | Tetraplegia, incomplete |
| V18 | F | 29 | Unknown | Paraplegia, complete |
| V19 | F | 59 | White | Paraplegia, incomplete |
| V20 | M | 50 | White | Paraplegia, complete |
| V21 | M | 50 | White | Paraplegia, complete |
| V22 | M | 66 | American Indian or Alaska Native | Tetraplegia, unspecified |
| V23 | M | 78 | Black or African American | Tetraplegia, incomplete |
| V24 | F | 63 | Unknown | Paraplegia, complete |
| V25 | F | 64 | White | Tetraplegia, incomplete |
| V26 | M | 74 | White | Tetraplegia, incomplete |
| V27 | M | 63 | White | Tetraplegia, complete |
| V28 | M | 55 | Asian, Native/Hawaiian/other Pacific Islander | Tetraplegia, incomplete |
| V29 | M | 60 | White | Tetraplegia, incomplete |
| V30 | F | 38 | Black or African American | Paraplegia, complete |
| V31 | F | 76 | White | Tetraplegia, incomplete |
| V32 | F | 52 | White | Tetraplegia, complete |
| V33 | M | 44 | Unknown | Tetraplegia, complete |
Theme 1: COVID-19 Pandemic Impact on Healthcare Use
Individuals with SCI described how the pandemic influenced their health care use experiences. Participants described not receiving health care services due to delays and cancellations imposed by the health care facility or by their own choice to avoid virus exposure. Individuals indicated that the pandemic resulted in them not receiving any preventive care or routine services, staling “I haven’t had any appointments or any medical things [visits] going on since COVID. Nothing at all. |V02].” Participants noted not being seen for primary care appointments, stating “before the actual coronavirus, I would go to the primary care appointments, but I haven’t been to an appointment well, for a while now. For about a year and a half [VI7]” or annual SCI evaluations indicating “I didn’t go last year [for an annual evaluation], of course, because of the pandemic [V08].” Others specified missing physical therapy and rehabilitation appointments, stating that “Once COVID hit, the scheduled appointments and therapies, rehab-type therapies, those all went away [V19]” and “We weren’t allowed to have physical therapy at all during that time [COVID pandemic] [V08]” Lack of hospital-provided transportation was cited as another reason individuals were unable to receive health care. “The last time I called for a [health care] appointment, that was last year ... I couldn’t go to the hospital because the travel office was closed because of COVID [V07].” As a result of in-person health care facility restrictions or individual decisions to delay care, individuals with SCI experienced lapses in health care receipt of various types, including primary care, SCI care, and rehabilitation therapy services, during the pandemic.
Additionally, individuals with SCI expressed concerns about lack of in-home formal (paid) caregiver availability during the pandemic. They were concerned not only about not getting needed help at home, but also about pushing the extra workload on their informal caregiver. Some “hoped to have help until this COVID thing was over and the VA could pick it [home attendant services] up again [V25].” Some had concerns about lack of formal caregiving help because their daily and medical needs became the responsibility of their informal caregiver. One participant described having to direct her informal caregiver on how to meet her care needs, but being concerned about the extra strain it had on the caregiver, stating “It was worse [during the pandemic], yeah, because he [informal caregiver] is kind of like out here, you know, floundering and I pretty much keep him appraised of what things to do and if I didn’t know it myself he would have really been lost [V12].” Individuals with SCI needed in-home formal caregiver help during the pandemic, but either did not receive it or their informal caregiver took on the extra care responsibilities.
Finally, some participants did receive health care during the pandemic, although typically not in-person, and they described their experiences with alternative health care delivery options, such as telehealth (i.e., telephone or video). Some simply described the shift in health care delivery methods, noting “With the virus, it’s gone to a lot of telephone appointments or video appointments [V03].” Others highlighted their use of telehealth with the exceptions of physically going to the facility for bloodwork or laboratory testing, “[During COVID] most of them [health care appointments] were over the phone, but I did go in for Woodwork and labs [V23]” and “Most of ‘em [health care appointments during COVID] were done virtual unless I had to do labs or something [V27].” Some participants described their attitude toward the changes, indicating, “I think given where society is and COVID is ... telehealth is just going to have to be the way life is for a while [V06].” Others highlighted their appreciation of the convenience of using telehealth for their health care. “Right now there’s a lot of telehealth that goes on which I didn’t think I would like, but I actually really love the convenience of it all [VI1].” Some individuals with SCI had not used telehealth services prior to the pandemic and were hesitant about using it yet found a new appreciation for the technology and the accessibility it offered, when needed. This was especially important to individuals with SCI who lived rurally or had long travel limes to get to their health care facility.
Theme 2: COVID-19 Pandemic Impact on Weight and Weight Management Lifestyle Behaviors
Individuals with SCI reported that the COVID-19 pandemic adversely impacted their engagement in physical activity and leisure time physical activity (and often weight maintenance) owing to facilities, such as fitness centers, gyms, and aquatics centers/ pools being closed, or classes, group exercise activities, and events being cancelled. Participants noted “Going to water aerobics ... I used to do that prior to all these things happening. But because of the pandemic, everything is shutdown [V05]” and “[The pandemicl restricted activity, you’re not able to go out like to bike, the bike riding group they slopped. Because of the lockdown, gyms were closed and things like that. So, if you had to go outside the home to get resources then you lost that ability [V22].” Others noted that before the pandemic, they experienced benefits from physical activity such as feeling good and comfortable about their weight, but the pandemic-related restrictions influenced their weight. One participant mentioned, “Before COVID hit, I was able to get down to the VA and do a workout three times a week, and I was feeling pretty good at that juncture. Yeah, the gym’s been closed. So, during that period, my weight went up [V09].” Another articulated, “COVID hit and they wouldn’t let me up there [VA gym] no more ... So, I really had no way of working out. So, that’s where the weight packed on. I just gained weight and got my gut back [V20].” Another said, “Before the pandemic, I was able to maintain my weight at the VA, as long as I was in their swim program. They had a swim exercise program for spinal cord and other hospital veterans who needed it, and I had a guaranteed spot in there until they shut it down with COVID [VI9].”
Others noted “COVID is interfering with me trying to do some type of just moving around so I haven’t really done anything and started gaining the weight back [V05]” and “I got involved in a workout program and started losing some weight again and got to where I was fairly comfortable. Then the pandemic hit, so ... [VI5].” Veterans noted lack of caregiver assistance during the pandemic with “stretching my legs every morning, and [doing] range of motion movements [V11].” Participants’ ability to engage in physical activity was impeded by exercise facility closures, the cancellation of classes and events, and lack of help at home to stretch and move, which hampered the benefits they were previously experiencing, for example, feeling good or comfortable and had negative consequences on their weight (slopped losing or gained).
In addition, the pandemic influenced individuals’ participation within the community which was a prepandemic source of physical activity. Some individuals with SCI made a personal choice to not go out into the community to avoid becoming exposed to the virus. “This pandemic thing [has had] a very significant negative impact on my weight. I’ve been restricting myself to the house to avoid contact with others ... and so, going out in my neighborhood or going out to a public park and doing some endurance [wheelchair] pushes is still [not occurring] and then not every place is opened up, [limiting] where I can push ... ‘cuz of places that are shut down [V11].” Other participants described not getting out because community activities were not available which led to their limited movement. “Well, certainly [COVID impacted] the amount of activities that are available in the community which might get me out and being more active in the community, so that, no question and then just once you’re out, you’re moving around more, I have become almost housebound [V03].” Likewise, engagement in physical activity through recreational and sports events was hindered during the pandemic, as one participant indicated “It [skiing with veteran’s group] was a really nice experience, yeah. We were supposed to go again in March, but they cancelled it because of COVID [V02].” Individuals with SCI experienced decreased movement and physical activity because of limited availability and access to recreational and public activities in the community.
Individuals with SCI described ways in which healthy eating behaviors were impacted by the pandemic. Participants described interruptions in food choices including having to let others do their grocery shopping, “because of the pandemic, somebody just goes grocery shopping for me [V105]” and not being able to select fresh produce “my food choices were [impacted] because like, when they had the Farmer’s Market, I was not able to go [V04].” Barriers to independence during the pandemic were described as having negative impacts on healthy eating behaviors.
Participants discussed eating out of boredom, at nonmealtimes, and eating unhealthy foods during the pandemic. One participant articulated “because of the stress of it [COVID], I probably snacked more than I needed to ... on unhealthy snacks [V33].” Others said “A lot of boring evenings, it’s just like sitting around and so, I go, and I find myself rooting through the pantry. It’s like, I shouldn’t be eating right now [VI5]” and “all I do is sit and eat sometimes, sit, and eat, sit, and eat [V17].” Participants expressed that during the pandemic “I just ate everything [V24]” and “I basically just stayed home and eat and sleep [V29]” and “Well, I’m at home. Nothing’s happening. I’m just going to eat a sleeve of Oreos, because why not? Like, I’m bored. So, it’s been harder to stay focused on doing the right things [VI8].” One participant indicated that he “skipped meals,” ate “microwaveable meals,” and had “a field day with sweets” [V09] because he did not have caregiver help to cook and prepare meals during the pandemic. The tedium and stress felt as a result of the pandemic environment and the implications on daily living without caregiver help led to eating for reasons other than hunger as well as unhealthy food choices.
Theme 3: COVID-19 Pandemic Impact on Psychosocial Factors
Individuals with SCI described the psychosocial implications the pandemic had on their lives. Many people felt that the pandemic limited their social interactions, social participation, and their ability to pursue their interests or pastimes. Participants described missing being around people and getting together with family and friends, expressing “with the virus, there’s no way to get together with folks the way there used to be [V03]” and “I miss the company. You know. I’m a social person, it’s almost like you’re in jail [V08].” Another said “COVID-19 has pretty much changed my life drastically because I’m unable to get about. Before, I could go here and go there. I was not alone all the time. Now I’m alone most of the time, and socializing is something that I miss since the COVID epidemic [V17].” Individuals commented not visiting with family during the pandemic, expressing “I haven’t seen my daughter in over a year, or my grandkids [VI9]” and “family wouldn’t come over [V27].” One individual indicated that the pandemic hindered his ability to spend time with his SCI peers, “COVID hit and they [VA] also didn’t allow you up there no more to hang out, so I couldn’t see any of my VA wheelchair buddies or nothing. Couldn’t do any of that [V20].” Individuals with SCI experienced negative emotional consequences due to lack of seeing and socially interacting with family and friends.
Participants indicated that they were not able to attend gatherings with organized groups they were part of, such as service organizations, advocacy groups, and church. One participant stated, “I regularly attended church, of course, that all changed with this COVID thing. It would have been nice if I could have—you know, gone to church, gone to the American Legion [V03].” Individuals with SCI also discussed the negative impact the pandemic had on their ability to pursue their interests and pastimes, especially recreation outside of the home selling such as shopping, dining, sporting events, and travel. Participants noted that “the pandemic just hampered a lol of things ... I do not go out or I mean you know you just do not travel [V20]” and “COVID has directly affected my lifestyle because there’s a lot of things I used to do that I cannot do anymore ... shopping, eat at Denny’s. All those things were gone, so I just had to learn to readjust [V08].” One participant stated, “If this COVID ever broke, you know, that would be nice to get out and go on a fishing trip and do different things. You know, go to a football game or a baseball game ... go play some dominoes again you know, that would be nice. Right now, that’s something I haven’t done [V104].” Individuals with SCI expressed undesirable impacts due to COVID-related absence of in-person connections through organized groups as well as discontinued engagement in their pastimes, hobbies, and interests.
In addition, individuals wilh SCI voiced several emotional reactions or feelings that were triggered by the COVID-19 pandemic. Participants described feelings of isolation and loss of motivation, in general, stating “so you were pretty much isolated [V09]” and “then COVID hit, and I lost all kinds of motivation [V09].” For some, the pandemic caused worry, fear, and cautiousness. Notably, fear and caution were triggered by both the COVID-19 virus and by the alarming behaviors of other people about mask-wearing and supply rationing, ‘That new Delta strain has got me worried, and then, you know, I mean you cannot even go out with a mask on without people losing their damn minds, I’m still very cautious. I’m worried about the nuts out there that wanna rip everybody’s mask off ... or people rationing [supplies, protective wear] [V11].” Another stated “That’s something else we have to woriy about. I’m still a little leery about being out, putting myself in settings with people [V05].” One participant indicated that the pandemic triggered worries about his pain because he no longer had the distractions of getting out and doing activities as he did prepandemic noting, “COVID-19 has definitely had an impact in terms of worrying about the pain ... nobody’s around and you start thinking negative thoughts, you know? I think that being outside and just trying to put my mind on something else, that would prevent me from thinking about the pain [VI7].” One individual with SCI was concerned about her relationship with her spouse and felt culpable for the extra caregiving responsibilities imposed on him during the pandemic (because formal care was unavailable), “he’s stuck with me in the house now and I know a lot of times he gets tired [V12].” The COVID-19 pandemic triggered several emotions in individuals with SCI, such as worry, fear, doubt, lack of motivation, and feelings of social isolation which were attributed to both the exposure to the virus and to not going out to avoid the public’s reactions to restrictions.
Discussion
This study is among few in-deplh qualitative interview studies to explore the perspectives of individuals with SCI about the impacts of the COVID-19 pandemic. We identified three key themes to describe pandemic impacts on health care use, weight management lifestyle behaviors, and psychosocial factors as described by individuals with SCI in the context of their functioning, disability, and participation from a physical, individual, and social perspective (WHO, 2013).
Impact of Pandemic on Health Care
Individuals with SCI in the current study identified ways that the COVID-19 pandemic precluded them from receiving their typical level of health care. They specifically described not receiving primary care (including their annual examinations), rehabilitation and therapy, and home care during the pandemic. This is consistent with other research that reported 82% of individuals with SCI experienced deferred or cancelled non-COVID related health care services (Right et al., 2022). Similarly, another survey study found that community-dwelling individuals with SCI experienced access barriers to medical supplies and had concerns about not receiving needed health care due to rationing of medical services (Monden et al., 2021). In an international online survey, rehabilitation health care providers reported that their patients with SCI had limited access to clinical and health care support services, along with worsening medical problems during the COVID-19 pandemic (Gustafson et al., 2021). Rehabilitation and therapy services were described as especially important by persons with SCI, because this is needed for functioning and is often the only movement or physical activity they get. Nearly half of SCI providers reported decreased availability of rehabilitation/therapy due to the facilities’ rehabilitation resources being used by medical and surgical patients during the pandemic rather than by individuals with SCI requiring rehabilitation (Gustafson et al., 2021). It is essential to make rehabilitation accessible because it improves an individuals’ independence, encourages return to social roles and life participation, and has been reported to prevent complications, decrease hospital admissions, reduce hospital length of stay, and reduce costs of care and support (Krug & Cieza, 2017). Rehabilitation services are designed to optimize functioning and reduce disability and should be delivered seamlessly across the continuum of care and throughout the life span as part of comprehensive person-centered care.
Individuals with SCI experience access barriers to health care due to physical distance to facilities, transportation challenges, lack of availability of specialized care, and health care cost (Barrows & Goldstein, 2021; LaVela et al., 2004; Pacheco Barzallo et al., 2021). It is possible that the themes identified by veterans with SCI in this study, pointing to unmet care needs, may be even more challenging for nonveterans with SCI, given the access advantages that many veterans with SCI have, including health care cost benefits and VA-supplied health care transportation services. Barrows and Goldstein (2021) reported another potential advantage for veterans with SCI, including major efforts taken by the VA SCI System of Care before and during the COVID-19 pandemic to overcome access barriers through provision of telehealth services for veterans with SCI. Our study revealed that the pandemic prompted some initially hesitant veterans with SCI to try telehealth, and some reported liking the convenience of telehealth services. In a large U.S. integrated health system, patients’ positive telehealth experiences were attributed to appreciation of the ability to maintain access and to the visit being more focused (than in-person; Hays & Skoolsky, 2022). Future research is warranted to examine health care outcomes as a result of incorporating telehealth services into care compared with facility-based alone. In a scoping review of patients with neurological conditions, including spine injury, Fiani et al. (2020) concluded that use of telerehabilitation was beneficial for improvements in outcomes such as improved physical function and reduced pain. In the current study, disruptions in health care stemmed from lack of in-person visits, often leaving basic and preventive health care needs unmet. In future pandemics or health care threats, efforts are needed to overcome the challenges faced by people with SCI in accessing care. Telehealth may represent a successful health care delivery option to complement in-person care in this population.
Impact of Pandemic on Healthy Weight Management Lifestyle Behaviors (Physical Activity and Healthy Eating)
Individuals with SCI in this study highlighted the ways in which the pandemic complicated their physical activity engagement. Prepandemic common barriers to physical activity and leisure time physical activity experienced by individuals with SCI include lack of access to facilities and usable equipment, lack of support of others to aid with activity (e.g., stretching, set-up), and psychological challenges (Pellegrini et al., 2021; van den Akker et al., 2020; Williams et al., 2014). Often already faced with such barriers but having found workarounds, the pandemic added a layer of complexity for individuals with SCI to engage in physical activity. Participants with SCI in the current study indicated that the help they typically received from caregivers to aid with physical activity was not available during the pandemic which ceased their ability to be physically active. They also described that the accessible gyms they attended prepandemic were closed and that the leisure time physical activities that they had planned, for example, skiing with Veteran groups, were cancelled. Similar findings showed that individuals with SCI spent less time (in minutes) engaged in physical activity, including recreational and leisure time physical activity, during the pandemic than prior to (Marco-Ahulló et al., 2021), Likewise, Righi et al. (2022) found that more than half of individuals with SCI decreased their activities and recreations during the pandemic and that these decreases were significantly correlated with anxiety. The decrease in physical activity (Buoite Stella et al,, 2021; Ferrante et al., 2020) and the relationship between stress and anxiety with decreased physical activity during the pandemic was also seen in the general population (Duncan et al,, 2020).
As with the general population, the COVID-19 pandemic limited physical activity engagement among individuals with SCI for several reasons, such as closures of gyms and fitness centers and social distancing measures. However, this problem may be exacerbated in the SCI population who already face multiple barriers and often have low levels of physical activity Extra obstacles may include lack of caregiver support (needed to initiate and/or perform physical activity), cancellation of recreational events intended for wheelchair users, and the need to remain home and indoors to limit virus transmission, especially given the immunocompromised stale (Riegger et al., 2009) and susceptibility to respiratory infection among individuals with SCI (Sassoon & Baydur, 2003), especially during a pandemic (LaVela, Goldstein, et al., 2012). Hence, we agree with the recommendations of Bales et al. (2022) highlighting the need to establish COVID-19 safe recommendations to reduce sedentary behavior and promote activity in persons with SCI. In the face of such restrictions, additional efforts are needed to facilitate physical activity in persons with SCI.
Concerns around healthy eating and nutrition in persons with SCI have been previously reported. For example, Silveira et al. (2019) reported consumption of high calories from fat, and poor intake of fruits, vegetables, fiber, and protein in persons with SCI. Intake of fiber as well as multiple micronutrients (vitamins A, B5, B7, B9, D, E, potassium, and calcium) were found to be below U.S. Department of Agriculture recommendations among individuals with chronic SCI (Farkas et al., 2019). Individuals with SCI themselves have reported unhealthy eating, citing reasons such as lack of autonomy about food choices (LaVela, Ehrlich-Jones, et al., 2021; LaVela, Jones, et al., 2021).
During the pandemic, individuals with SCI described additional obstacles to healthy eating, such as loss of independence in obtaining groceries and lack of caregiver help with meal preparation, which can further exacerbate the aforementioned intake deficiencies. Individuals with SCI also described that due to being quarantined and feeling stress related to the pandemic, they tended to make unhealthy food choices and eat at nonmealtimes and/or out of boredom. This is consistent with research reporting increased general population consumption of unhealthy foods and snacking between meals (Ferrante et al., 2020; Hammouri et al., 2022; Werneck et al., 2021), and in persons with SCI limited access to food and groceries (Vives Alvarado et al., 2021) during the COVID-19 pandemic. Furthermore, Lamy et al. (2022) found that internationally during the pandemic, mood and emotional well-being influenced dietary habits and food choices. This association between poor nutritional choices and stress, depression, and anxiety has been previously established (Aoun et al., 2019; Devonport et al., 2019). As with physical activity, alternative options to facilitate healthy eating (such as virtual meal preparation classes) are needed for the SCI population during times when restrictions are in place.
During the pandemic and beyond, a lack of physical activity and healthy eating may exacerbate the impact of SCI by adding a higher risk of cardiometabolic disease and secondary chronic health complications (Gater et al., 2019). Efforts are needed to identify ways to mitigate barriers to weight management faced by individuals with SCI that are worsened by crises such as a pandemic because reversing the complications of obesity-related diseases is challenging, especially in the SCI population (Gater et al., 2019; Selassie et al., 2013). In addition, individuals may experience emotional consequences associated with lack of physical activity and nutritional deficits due to unhealthy eating. Collectively, this suggests that more flexible healthy behavior intervention ideas are needed to accommodate individuals in unanticipated situations.
Impact of Pandemic on Psychosocial Factors
During the pandemic, veterans with SCI experienced various psychosocial challenges from pandemic-related disruptions in daily life, social interactions, participation in social and organization group activities, and pursuit of interests/pastimes. Our findings are similar to other research, including a study showing that individuals with SCI reported that the COVID-19 pandemic had a negative impact on their mental and social health, in particular that their feelings of social isolation increased (Monden et al., 2021). In another SCI cohort, feelings of social isolation were associated with a greater perceived impact of the COVID-19 pandemic on menial health and overall health (Mikolajczyk et al., 2021), Our study showed that the COVID-19 pandemic triggered several emotions in veterans with SCI, such as worry, fear, doubt, lack of motivation, and feelings of social isolation, veterans with SCI in the current study felt troubled by social isolation from their community, their family and loved ones, as well as their peers with SCI. Peer support plays a vital role in promoting participation, life satisfaction, and facilitating unmet SCI-relaled needs (Sweet et al., 2016). During public health crises, it may be prudent to capitalize on SCI peer support interactions or programs to combat negative emotions and social isolation.
Similarly, in response to an online survey, individuals with SCI in the United Kingdom reported feeling anxiety and social isolation as a result of the pandemic (Hearn et al., 2021). Other work found that individuals with SCI experienced decreased social integration and increased depression during the pandemic compared with their prepandemic self-reported scores on validated instruments (García-Rudolph et al., 2021). In another study, almost half of SCI health care providers (45%) reported depression or anxiety due to the pandemic in their patients with SCI (Gustafson et al.. 2021). In another study of persons with SCI, although depression and anxiety were relatively low (16% and 10%, respectively), statistically significant increases in depression were seen during the pandemic compared with 2 years prior (Vives Alvarado et al., 2021).
Mental health disorders are more prevalent in the SCI population, with rates three times that of the non-SCI population (Bombardier et al., 2021). Even though individuals with SCI typically have substantial contact with health care providers (prepandemic), mental and social health concerns are often not addressed (Bombardier et al., 2021). This is perhaps because mental and social health concerns are overshadowed by the pressing continuing care needs related to physical impairments (Murphy & Thomas, 2021). The social and menial effects of the pandemic have been far-reaching, yet we do not yet have a full understanding of the ramifications of direct and indirect influences of the pandemic and its long-term impacts (Holt-Lunslad & Perissinotto, 2022; Smith & Lim. 2020). Given the disparities in mental and social health in persons with SCI that existed before the pandemic, it is crucial to take actionable steps (e.g., resilience training, education on coping mechanisms and readjustment strategies) because the negative effects of the pandemic on the social and menial health of individuals with SCI may be harmful and long-lasting.
Limitations
The use of purposeful criterion sampling and the exclusion of non-English speaking participants may have introduced bias into the findings. Additionally, two thirds of the individuals contacted for participation in this study did not participate and the study participants represent only a small proportion of veterans with SCI, both of which may impact the transferability of findings. The study included only veterans with SCI receiving care at the VHA, so the findings may be different than what might be reported by veterans receiving care outside of the VHA or civilians with SCI, Finally, as with most qualitative research, we did not have a control group of persons without SCI with which to make direct comparisons of the findings.
Conclusions
Our findings highlight the magnitude of consequences faced by individuals with SCI when restrictions to health care, healthy lifestyle endeavors, and social interaction/participation are imposed. Disruptions in health care may have serious consequences for people with SCI who require routine care to manage a plethora of comorbid chronic conditions and SCI-related secondary conditions. Alternative options for care received in the home are needed, especially for physical tasks and health maintenance efforts. However, many individuals with SCI were able to use telehealth options during the pandemic and have reported having positive experiences and appreciating the convenience. Pandemic-related barriers to physical activity and healthy eating may put people with SCI at increased risk for complications from overweight and obesity and related cardiomelabolic diseases or nutritional deficiencies. Efforts are needed to mitigate barriers to weight management faced by individuals with SCI that become more challenging during crises such as a pandemic. Furthermore, psychosocial implications from crises such as this pandemic may be additive in persons with SCI, who already face harriers to social participation, and warrant further research.
Because barriers to health care and the practice of healthy behaviors were experienced for an extended period of lime during the pandemic, it will be prudent to understand how disease management and overall health may have been affected by reduced: (a) engagement in health care receipt. (b) physical activity, (c) healthy eating, and (d) social participation/interaction in the SCI population. Future research is warranted to understand the short and long-term postpandemic impacts on the prevalence and management of chronic disease in persons with SCI, with a special emphasis on cardiometabolic disease and whether there are any lasting mental/social health impacts. The study findings may inform and guide SCI health care providers on what is needed in response to similar and future public health or natural disaster crises. Actionable recommendations on ways to facilitate access to medical care and supportive services to meet rehabilitation, in-home care, physical activity, dietary, and mental and emotional health needs during public health crises are critically needed for the SCI population.
Impact and Implications.
As one of few studies to use qualitative interviews with in-depth thematic analysis, this article offers a novel method of examining the impact of the COVID-19 pandemic from the perspectives of individuals with SCI. Individuals with SCI offered insights on ways in which the pandemic disrupted their receipt of routine health care (including home care and rehabilitation/therapy), engagement in healthy eating and physical activity, and social participation. Other research indicates that the general population faced similar barriers: however, owing to several biopsychosocial realities related to function and disability, the obstacles appeared to be intensified for persons with SCI, for example reliance on home health caregivers for regular range of motion exercises, and perceptions of increased risk of virus exposure due to immunocompromised bodily systems in persons with SCI. Negative impacts from obstacles to receiving health care, engaging in healthy weight management lifestyle behaviors, and social participation may have both short- and long-term effects on increased risk for and management of chronic disease, particularly cardiometabolic conditions and SCI-related secondary conditions, as well as poor social health and emotional well-being.
Acknowledgments
This study was supported by Merit Review Award IIR 17-047 (Dan Eisenberg) and Research Career Scientist Award RCS14-232 (Alex H. S. Harris) from the U.S. Department of Veterans Affairs, Health Services Research and Development Service. We thank the Veterans who participated in this study. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs, Veterans Health Administration or the United Slates Government.
This study was not preregistered. On reasonable request and approval of the institution’s human subject and ethics committee, de-identified data may be available by contacting the PI.
Footnotes
All authors listed have contributed sufficiently to the project and manuscript to be included as authors, and all those who are qualified to be authors are listed in the agreed-on order in the author byline.
The authors do not have any conflicts of interest or commercial interests to disclose.
References
- Abasiyamk Z, Kurt M, & Kahraman T. (2022). COVID-19 and physical activity behaviour in people with neurological diseases: A systematic review. Journal of Developmental and Physical Disabilities. Advance online publication. 10.007/sl0882-022-09836-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adler P, & Adler P. (2012). Expert voices. In Baker SE & Edwards R. (Eds.), How many qualitative interviews is enough? National Centre fur Research Methods Review Discussion Paper; (pp. 8–11). http://eprints.ncrm.ac.uk/2273 [Google Scholar]
- American Psychological Association. (2000). Journal article reporting standards-Qual. https://apastyle.apa.org/jars/qualitative
- Ando H, Cousins C, & Young C. (2014). Achieving saturation in thematic analysis: Development and refinement of a codebook. Comprehensive Psychology, 3. Article 03.CP.3.4. 10.2466/03.CP.3.4 [DOI] [Google Scholar]
- Aoun C, Nassar L, Soumi S, El Osta N, Papazian T, & Rabbaa Khabbaz L. (2019). The cognitive, behavioral, and emotional aspects of eating habits and association with impulsivity, chronotype, anxiety, and depression: A cross-sectional study. Frontiers in Behavioral Neuroscience, 13, Article 204. 10.3389/fnbeh.20l900204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barrows D, & Goldstein B. (2021). Virtual care in the veterans affairs spinal cord injuries and disorders system of care during the COVID-19 national public health emergency. Physical Medicine and Rehabilitation Clinics of North America. 32(2), 207–221. 10.1016/j.pmr.2021.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bates LC, Conners R, Zieff G, Adams NT, Edgar KM, Stevens S, Faghy MA, Arena R, Vermeesch A, Joseph RP, Keith N, & Stoner L. (2022). Physical activity and sedentary behavior in people with spinal cord injury: Mitigation strategies during COVID-19 on behalf of ACSM-EIM and HL-PIVOT. Disability and Health Journal, 15( 1), Article 101177. 10.1016/j.dhjo.2021.101177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bombardier CH, Azuero CB, Fann JR, Kautz DD, Richards JS, & Sabharwal S. (2021). Management of mental health disorders, substance use disorders, and suicide in adults with spinal cord injury: Clinical practice guideline for healthcare providers. Topics in Spinal Cord Injury Rehabilitation, 27(2), 152–224. 10.46292/sci2702-152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley EH, Curry LA, & Dcvers KJ (2007). Qualitative data analysis for health services research: Developing taxonomy, themes, and theory. Health Services Research, 42(4), 1758–1772. 10.1111/j.1475-6773.2006.00684.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun V, & Clarke V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. 10.119l/1478088706qp063oa [DOI] [Google Scholar]
- Buoite Stella A, AjČeviČ M, Furlanis G, Cillotto T, Menichelli A, Accardo A, & Manganotti P. (2021). Smart technology for physical activity and health assessment during COVID-19 lockdown. The Journal of Sports Medicine and Physical Fitness, 6/(3), 452–160. 10.23736/S0022-4707.20.11373-2 [DOI] [PubMed] [Google Scholar]
- Chen Y, Cao Y, Allen V, & Richards JS (2011). Weight matters: Physical and psychosocial well being of persons with spinal cord injury in relation to body mass index. Archives of Physical Medicine and Rehabilitation, 92(3), 391–398. https://doi.org/IG.l0I6/j.apmr.2010.06.030 [DOI] [PubMed] [Google Scholar]
- Creswell JW (2018). Philosophical assumptions and interpretive frameworks. In Creswell JW & Poth CN (Eds.), Qualitative inquiry and research design: Choosing among five approaches (4th ed., pp. 15–34). SAGE Publications. [Google Scholar]
- Czeisler MÉ, Marynak K, Clarke KEN, Salah Z, Shakya I, Thierry JM, Ali N, McMillan H, Wiley JF, Weaver MD, Czeisler CA, Rajaratnam SMW, & Howard ME (2020). Delay or avoidance of medical care because of COVID-19-related concerns - United States, June 2020. MMWR. Morbidity and Mortality Weekly Report, 69(36), 1250–1257. 10.15585/mmwr.mm6936a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devonport TJ, Nicholls W, & Fullerton C. (2019). A systematic review of the association between emotions and eating behaviour in normal and overweight adult populations. Journal of Health Psychology, 24(1), 3–24. https://doi.org/Io1177/1359105317697813 [DOI] [PubMed] [Google Scholar]
- Duncan GE, Avery AR, Seto E, & Tsang S. (2020). Perceived change in physical activity levels and mental health during COVID-19: Findings among adult twin pairs. PLoS ONE, 15(8), Article e0237695. 10.1371/journal.pone.0237695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elaraby A, Shahein M, Bekhet AH, Perrin PB, & Gorgey AS (2022). The COVID-19 pandemic impacts all domains of quality of life in Egyptians with spinal cord injury: A retrospective longitudinal study. Spinal Cord, 60(8), 757–762. 10.1038/s4l393-022-00775-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farkas GJ, & Gater DR (2018). Neurogenic obesity and systemic inflammation following spinal cord injury: A review, /he Journal of Spinal Card Medicine, 41(4), 378–387. 10.1080/10790268.2017.1357104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farkas GJ, Pilot MA, Berg AS, & Gater DR (2019). Nutritional status in chronic spinal cord injury: A systematic review and meta-analysis. Spinal Cord, 57(1), 3–17. 10.1038/s41393-018-0218-4 [DOI] [PubMed] [Google Scholar]
- Ferranle G, Camussi E, Piccinelli C, Senore C, Armaroli P, Ortale A, Garena F, & Giordano L. (2020). Did social isolation during the SARS-CoV-2 epidemic have an impact on the lifestyles of citizens? Lpidemiologia e Prevenzione, 44(5–6 Suppl. 2), 353–362. 10.19191/EP20.5-6.S2.137 [DOI] [PubMed] [Google Scholar]
- Fiani B, Siddiqi I, Lee SC, & Dhillon L. (2020). Telerehabilitation: Development, application, and need for increased usage in the COVID-19 era for patients with spinal pathology. Cureus, 12(9), Article e10563. 10.7759/cureus.10563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frost N, Holt A, Shinebourne P, Esin C, Nolas SM, Mehdizadeh L, & Brooks-Gordon B. (2011). Collective findings, individual interpretations: An illustration of a pluralistic approach to qualitative data analysis. Qualitative Research in Psychology, 8(1). 93–113. 10.1080/14780887.2010.500351 [DOI] [Google Scholar]
- García-Rudolph A, Saurí J, López Carballo J, Cegarra B, Wright MA, Opisso E, & Tormos JM (2021). The impact of COVID-19 on community integration, quality of life, depression and anxiety in people with chronic spinal cord injury. The Journal of Spinal Cord Medicine. Advance online publication, 10.1080/l0790268.202l.l922230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gater DR Jr., Farkas GJ, Berg AS, & Castillo C. (2019). Prevalence of metabolic syndrome in veterans with spinal cord injury. The Journal of Spinal Cord Medicine. 42(1), 86–93. 10.1080/10790268.2017.1423266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafson K, Stillman M, Capron M, O’Connell C, Longoni Di Giusto M, Tyagi N, & Scivoletto G. (2021). COVID-19 and spinal cord injury and disease: Results of an international survey as the pandemic progresses. Spinal Cord Series and Cases, 7(1), Article 13. 10.1038/s41394-020-00356-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammouri H, Almomani F, Abdel Muhsen R, Abughazz A, Daghmash R, Abudayah A, Hasan I, & Alzein E. (2022). Lifestyle variations during and after the COVID-19 pandemic: A CrOSS-seclional study of diet, physical activities, and weight gain among the Jordanian adult population. International Journal of Environmental Research and Public Health, 19(3), Article 1346. https://doi.org/I0339G/ijerphl9031346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatchett PE, Mulroy SJ, Eberly VJ, Haubert LL, & Requejo PS (2016). Body mass index changes over 3 years and effect of obesity on community mobility for persons with chronic spinal cord injury. The Journal of Spinal Cord Medicine, 39(4), 421–432. 10.1080/10790268.2015.1133482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hays RD, & Skootsky SA (2022). Patient experience with in-person and telehealth visits before and during the COVID-19 pandemic at a large integrated health system in the United States. Journal of General Internal Medicine, 37(4), 847–852. 10.1007/s11606-021-07196-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hearn JH, Rohn EJ, & Monden KR (2021). Isolated and anxious: A qualitative exploration of the impact of the COVID-19 pandemic on individuals living with spinal cord injury in the U.K. The Journal of Spinal Cord Medicine. Advance online publication, 10.1080/10790268.2021.1949562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt-Lunstad J, & Perissinotto CM (2022). Isolation in the time of COVID: What is the true cost, and how will we know? American Journal of Health Promotion, 36(2), 380–382. 10.1177/08901171211064223 [DOI] [PubMed] [Google Scholar]
- Kallio H, Pietila AM, Johnson M, & Kangasniemi M. (2016). Systematic methodological review: Developing a framework for a qualitative semi-structured interview guide. Journal of Advanced Nursing, 72(12), 2954–2965. 10.1111/jan.1.3031 [DOI] [PubMed] [Google Scholar]
- Krug E, & Cieza A. (2017). Strengthening health systems to provide rehabilitation services. Bulletin of the World Health Organization, 95(3), Article 167. 10.2471/BLT.17.l9l809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurasaki KS (2000). Intercoder reliability for validating conclusions drawn from open-ended interview data. Field Methods, 12(3), 179–194. 10.1177/1525822X0001200301 [DOI] [Google Scholar]
- Lamy E, Viegas C, Rocha A, Raquel Lucas M, Tavares S, Capela E Silva F, Guedes D, Laureati M, Zian Z, Salles Machado A, Ellssel P, Freyer B, González-Rodrigo E, Calzadiila J, Majewski E, Prazeres I, Silva V, Juračak J, Platikivá Vorlíčkova L, & Consortium for Changes in Food Behavior - COVID-19. (2022). Changes in food behavior during the first lockdown of COVID-19 pandemic: A multi-country study about changes in eating habits, motivations, and food-related behaviors. Food Quality and Preference, 99, Article 104559. 10.1016/j.foodqual.2022.104559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaVela SL, Burkhart E, Jones K, & Pellegrini C. (2021). Health care provider views on the magnitude of overweight/obesity in spinal cord injury and awareness of evidence-based guidance for weight management. PM & R; Advance online publication, 10.1002/pmrj.12709 [DOI] [PubMed] [Google Scholar]
- LaVela SL, Ehrlich-Jones LS, Jones, Bartle, & Heinemann AW (2021). What are personal meanings of healthy eating and physical activity in individuals living with spinal cord injury? a qualitative exploration. Topics in Spinal Cord Injury Rehabilitation, 27(4), 68–78. 10.46292/sci21-00001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaVela SL, Evans CT, Prohaska TR, Miskevics S, Ganesh SP, & Weaver FM (2012). Males aging with a spinal cord injury: Prevalence of cardiovascular and metabolic conditions. Archives of Physical Medicine and Rehabilitation, 93(1), 90–95. 10.1016/j.apmr.2011.07.201 [DOI] [PubMed] [Google Scholar]
- Lavela SL, Goldstein B, Etingen B, Miskevics S, & Weaver FM (2012). Factors associated with H1N1 influenza vaccine receipt in a high-risk population during the 2009–2010 H1N1 influenza pandemic. Topics in Spinal Cord Injury Rehabilitation, 18(4), 306–314. 10.1310/scil804-306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaVela SL, Jones K, Heinemann AW, Bartle B, & Ehrlich-Jones LS (2021). Motivators, goal setting, and helpful feedback for weight management among individuals with spinal cord injury. Rehabilitation Psychology. 66(3), 257–264. 10.l037/rep0000385 [DOI] [PubMed] [Google Scholar]
- LaVela SL, Smith B, Weaver FM, & Miskevics SA (2004). Geographical proximity and health care utilization in veterans with SCI & D in the USA. Social Science the Medicine, 59(11), 2387–2399. 10.1016/j.socscimed.2004.06.033 [DOI] [PubMed] [Google Scholar]
- Marco-Ahulló A, Montesinos-Magraner L, González LM, Morales J, Bernabéu-García JA, & García-Massó X. (2021). Impact of COVID-19 on the self-reported physical activity of people with complete thoracic spinal cord injury full-time manual wheelchair users. The Journal of Spinal Cord Medicine. Advance online publication, 10.1080/10790268.2020.1857490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matsuoka M, & Sumida M. (2021). The effect of the COVID-19 pandemic on the health-related quality of life in home-based patients with spinal cord injuries in Japan. The Journal of Spinal Cord Medicine. Advance online publication. 10.l080/10790268.202l.1953313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehrotra A, Chemew M, Linetsky D, Hatch H, Cutler D, Schneider EC (2020). The impact of the COVID-19 pandemic on outpatient care: visits return to prepandemic levels, but not for all providers and patients. Accessed March 1, 2022, from https://www.commonwealthfund.org/publications/2020/oct/impact-covid-19-pandemic-outpatient-care-visits-return-prepandemic-levels [Google Scholar]
- Mikolajcxyk B, Draganich C, Philippus A, Goldstein RE, Andrews Pilarski C, Wudlick R, Morse LR, & Monden KR (2021). Resilience and mental health in individuals with spinal cord injury during the COVID 19 pandemic. Spinal Cord, 59(12). 1261–1267. 10.1038/s41393-021-00708-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miles M, Huberman M, & Saldana J. (2014). Qualitative data analysis: A methods sourcebook (3rd ed.). SAGE Publications, Inc. [Google Scholar]
- Monden KR, Andrews E, Pilarski C, Hearn J, Wudlick R, & Morse LR (2021). COVID-19 and the spinal cord injury community: Concerns about medical rationing and social isolation. Rehabilitation Psychology, 66(4), 373–379. 10.l037/rep0000407 [DOI] [PubMed] [Google Scholar]
- Murphy C, & Thomas FP (2021). Improving care for mental health disorders: The urgent needs of the population with spinal cord injury. The Journal of Spinal Cord Medicine, 44(1), Article 1. 10.1080/10790268.2021.1880229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nowell LS, Norris JM, White DE, & Moules NJ (2017). Thematic analysis: Striving to meet the trustworthiness criteria. International Journal of Qualitative Methods, 16( 1), 1–13. 10.1177/1609406917733847 [DOI] [Google Scholar]
- Pacheco Barzallo D, Oña A, & Gemperli A. (2021). Unmet health care needs and inequality: A cross-country comparison of the situation of people with spinal cord injury. Health Services Research, 56 (Suppl. 3), 1429–1440. 10.1111/1475-6773.13738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palinkas LA. Horwitz SM, Green CA, Wisdom JP, Duan N, & Hoagwood K. (2015). Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Administration and Policy in Mental Health, 42(5), 533–544. 10.1007/sl0488-013-0528-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pellegrini CA, Burkhart L, Jones K, & LaVela SL (2021). Health provider identified barriers and facilitators to weight management for individuals with spinal cord injury. Spinal Cord, 59(10), 1061–1071. 10.1038/s41393-021-00614-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riegger T, Conrad S, Schluesener HJ, Kaps HP, Badke A, Baron C, Gerstein J, Dietz K. Abdizahdeh M, & Schwab JM (2009). Immune depression syndrome following human spinal cord injury (SCI): A pilot study. Neuroscience, 158(5), 1194–1199. 10.1016/j.neuroscienee.2008.08.021 [DOI] [PubMed] [Google Scholar]
- Righi G, Baroni E, Righi L, Belloni L, & Del Popolo G. (2022). Perception of the COVID-19 pandemic among people with spinal cord injury: An Italian survey. Spinal Cord Series and Cases, 8(1), Article 2. 10.1038/s41394-021-00470-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sassoon CSH, & Baydur A. (2003). Respiratory dysfunction in spinal cord disorders. In Lin V. Cardenas DD, Cutter NC, Frost FS, Hammond MC, Lindblom LB, & Waters R. (Eds.), Spinal cord medicine: Principles and practice (pp. 155–168). Demos Medical Publishing, Inc. [Google Scholar]
- Selassie A, Snipe L, Focht KL, & Welldaregay W. (2013). Baseline prevalence of heart diseases, hypertension, diabetes, and obesity in persons with acute traumatic spinal cord injury: Potential threats in the recovery trajectory. Topics in Spinal Cord Injury Rehabilitation, 19(3), 172–182. 10.1310/sci1903-172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silveira SL, Winter LL, Clark R, Ledoux T, & Robinson-Whelen S. (2019). Baseline dietary’ intake of individuals with spinal cord injury who are overweight or obese. Journal of the Academy of Nutrition and Dietetics, 119(2), 301–309. 10.10l6/j.jand.20l8.08.l53 [DOI] [PubMed] [Google Scholar]
- Smith BJ, & Lim MH (2020). How the COVID-19 pandemic is focusing attention on loneliness and social isolation. Public Health Research & Practice, 30(2), Article 3022008. 10.17061/phrp3022008 [DOI] [PubMed] [Google Scholar]
- Smith DL Jr., & Yarar-Fisher C. (2016). Contributors to metabolic disease risk following spinal cord injury. Current Physical Medicine and Rehabilitation Reports, 4(3), 190–199. 10.1007/s40141-016-0124-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sweet SN, Noreau L, Leblond J, & Martin Ginis KA (2016). Peer support need fulfillment among adults with spinal cord injury: Relationships with participation, life satisfaction and individual characteristics. Disability and Rehabilitation, 38(6), 558–565. 10.3109/09638288.2015.1049376 [DOI] [PubMed] [Google Scholar]
- van den Akker LE, Holla JFM, Dadema T, Visser B, Valent LJ, de Groot S, Dallinga JM, Deutekom M, & The WHEELS-Study Group. (2020). Determinants of physical activity in wheelchair users with spinal cord injury’ or lower limb amputation: Perspectives of rehabilitation professionals and wheelchair users. Disability and Rehabilitation, 42(14), 1934–1941. 10.1080/09638288.2019.1577503 [DOI] [PubMed] [Google Scholar]
- Vives Alvarado JR, Miranda-Cantellops N, Jackson SN, & Felix ER (2021). Access limitations and level of psychological distress during the COVID-19 pandemic in a geographically-limited sample of individuals with spinal cord injury. The Journal of Spinal Cord Medicine. Advance online publication, 10.1080/10790268.2021.2013592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warren CAB (2002). Qualitative Interviewing. In Gubrium JF & Holstein JA (Eds.), Handbook of interview research: Context and method (pp. 83–103), Sage. [Google Scholar]
- Wen H, DeVivo MJ, Mehta T, Kaur Baidwan N, & Chen Y. (2021). The impact of body mass index on one-year mortality after spinal cord injury. The Journal of Spinal Cord Medicine, 44(4), 563–571. 10.1080/10790268.2019.1688021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werneck AO, Silva DR, Malta DC, Gomes CS, Souza-Júnior PR, Azevedo LO, Barros MB, & Szwarcwald CL (2021), Associations of sedentary behaviours and incidence of unhealthy diet during the COVID-19 quarantine in Brazil. Public Health Nutrition, 24(3), 422–126. 10.1017/S1368980020004188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams TL, Smith B, & Papathomas A. (2014). The barriers, benefits and facilitators of leisure lime physical activity among people with spinal cord injury: A meta-synthesis of qualitative findings. Health Psychology Review. 8(4), 404–425. 10.1080/17437199.2014.898406 [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2013). How to use the ICF: A practical manual for using the International Classification of functioning, Disability and Health (ICF). [Google Scholar]