ABSTRACT
Total anomalous pulmonary venous connection (TAPVC) is a critical congenital heart disease which is often missed on prenatal echocardiography because of the decreased pulmonary blood flow in fetal life. Improvement in technology has resulted in increasing prenatal diagnosis of this condition. We report a foetus with infra cardiac TAPVC in whom prenatal diagnosis was facilitated by the use of STIC technology.
Keywords: Fetal echocardiogram, Infracardiac TAPVC, prenatal diagnosis, STIC imaging
Total anomalous pulmonary venous connection (TAPVC) is a critical congenital heart disease (CHD), and failure to recognize the condition in the 1st few days of life can result in significant morbidity and mortality. However, the standard obstetric screening views of the heart are often normal in TAPVC, resulting in missed prenatal diagnosis.[1] With improvement in the resolution of ultrasound imaging and the advent of advanced imaging modalities, including spatiotemporal imaging correlation (STIC), the condition is increasingly recognized on prenatal ultrasound.[2] We report a fetus with infracardiac TAPVC, in whom STIC imaging permitted an excellent visualization of the infracardiac drainage as well as the potential site of obstruction.
A pregnant mother was referred to us at 26 weeks of gestational age. The imaging was performed on a Philips Epiq Elite ultrasound machine using a V9-2 volume transducer. There was usual arrangement of the abdominal organs. The cardiac mass was on the left side of the chest. There was a single right-sided superior caval vein that drained into the right atrium. The inferior caval vein was intact and drained into the right atrium. The pulmonary venous drainage to the left atrium (LA) could not be reliably imaged. The atrioventricular connections were concordant. There was ventricular asymmetry with a smaller left ventricle (LV) [Figure 1a]. The ventriculoarterial connections were concordant. The outflows were unobstructed. The pulmonary veins appeared to drain through a descending vertical vein [Figure 1b] into the portal venous system suggesting infracardiac TAPVC. Three-dimensional (3D) color Doppler imaging was obtained using spatiotemporal imaging correlation (STIC), and the obtained image was rendered to demonstrate pulmonary venous drainage. This showed flow acceleration at the site of drainage of the vertical vein to the left portal vein suggesting possible obstruction [Figure 2 and Video 1].
Figure 1.
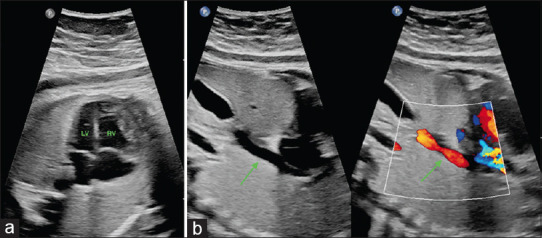
(a) Four-chamber view of the fetal heart demonstrating mild ventricular disproportion with the left ventricle smaller than the right ventricle. The left ventricle, however, still forms the apex of the heart (LV, RV). (b) Color-compare imaging of the fetal thorax and abdomen demonstrating the descending vertical vein (green arrow) draining into the abdomen. LV: Left ventricle, RV: Right ventricle
Figure 2.
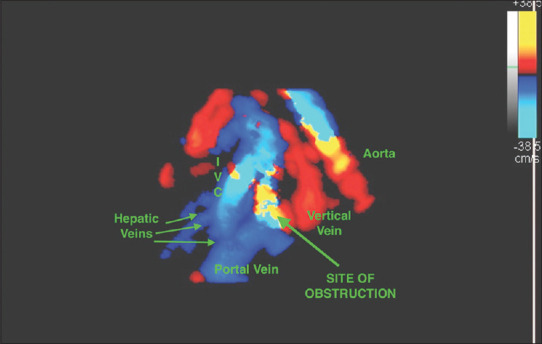
Still image of four-dimensional STIC imaging demonstrating the drainage of the vertical vein into the portal system as well as the site of obstruction of the vertical vein at its drainage into the portal system. IVC: Inferior caval vein, STIC: Spatio-temporal Imaging Correlation
TAPVC is a rare CHD with an incidence of approximately 8/100,000 live births.[3] Prenatal diagnosis probably has the highest impact on TAPVC among all critical CHDs. During prenatal life, only 10% of the combined cardiac output flows through the pulmonary veins. Hence, the pulmonary veins are small and often difficult to image. The diagnosis of TAPVC in prenatal ultrasound was traditionally established by a combination of “soft findings,” including mild ventricular disproportion with a smaller LV, increased retrocardiac space between the LA and the descending aorta, as well as the visualization of an additional vessel on the three-chamber view in cases of supracardiac TAPVC.[4-6] In a review of 424 children with TAPVC operated between 1998 and 2004 in all cardiac centers in the United Kingdom, only 1.9% were diagnosed prenatally.[7] Ganesan et al. reviewed their experience with prenatal diagnosis in 26 cases of TAPVC. However, there were only four cases of isolated TAPVC in their cohort, while the remaining fetuses had right isomerism with TAPVC in addition to complex CHD. They described the utility of pulse Doppler evaluation of the pulmonary veins in addition to two-dimensional (2D) imaging in establishing the diagnosis.[1]
3D fetal echocardiography using STIC has been shown to be superior to conventional 2D ultrasound in the diagnosis of anomalous pulmonary veins. Zhang et al. reported their experience with the prenatal diagnosis of TAPVC. Among 31 fetuses with adequate quality 2D and 3D imaging, in whom the prenatal suspicion of TAPVC was confirmed by postnatal ultrasound or fetal autopsy, the diagnosis was identified only on 3D echocardiogram in 5 (16%) cases establishing the additional utility of STIC imaging.[8] Although the diagnosis of TAPVC was established by 2D ultrasound in our case, STIC allowed us to delineate the course of the anomalous venous drainage and also identify the site of potential obstruction.
2D ultrasound with color Doppler imaging remains the cornerstone of prenatal diagnosis of CHD. However, 2D ultrasound is an operator-dependent imaging modality, and only a highly skilled operator can diagnose TAPVC in prenatal life. 3D imaging by STIC permits review of the imaging in multiple planes to identify the vertical vein and can be performed offline. When a radiologist or fetal medicine specialist notices the above-mentioned “soft signs” of TAPVC, STIC imaging can be obtained to permit review by a specialist when referral to a specialist service is not available. It is important to remember that STIC imaging carries its own pitfalls, and the technology behind this acquisition continues to improve. Improvement in image acquisition speed and incorporation of algorithms to eliminate motion artifacts could pave the way for STIC imaging to become a mandatory part of fetal heart evaluation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Video available on: https://journals.lww.com/aopc
REFERENCES
- 1.Ganesan S, Brook MM, Silverman NH, Moon-Grady AJ. Prenatal findings in total anomalous pulmonary venous return: A diagnostic road map starts with obstetric screening views. J Ultrasound Med. 2014;33:1193–207. doi: 10.7863/ultra.33.7.1193. [DOI] [PubMed] [Google Scholar]
- 2.Li TG, Ma B, Gao YH, Zhang RH, Li PL, Da ZQ. Prenatal diagnosis of total anomalous pulmonary venous connection using 2D and HDlive flow combined with spatiotemporal image correlation. Echocardiography. 2022;39:1269–75. doi: 10.1111/echo.15429. [DOI] [PubMed] [Google Scholar]
- 3.Hoffman JI, Kaplan S, Liberthson RR. Prevalence of congenital heart disease. Am Heart J. 2004;147:425–39. doi: 10.1016/j.ahj.2003.05.003. [DOI] [PubMed] [Google Scholar]
- 4.Kao CC, Hsieh CC, Cheng PJ, Chiang CH, Huang SY. Total anomalous pulmonary venous connection: From embryology to a prenatal ultrasound diagnostic update. J Med Ultrasound. 2017;25:130–7. doi: 10.1016/j.jmu.2017.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bravo-Valenzuela NJ, Peixoto AB, Araujo Júnior E. Prenatal diagnosis of total anomalous pulmonary venous connection: 2D and 3D echocardiographic findings. J Clin Ultrasound. 2021;49:240–7. doi: 10.1002/jcu.22973. [DOI] [PubMed] [Google Scholar]
- 6.Nandhini U, Atkinson M, Krishna MR, Alahakoon TI. Antenatal diagnosis of isolated infracardiac infradiaphragmatic total anomalous venous connection –Pictorial essay and discussion. Australas J Ultrasound Med. 2019;22:61–5. doi: 10.1002/ajum.12119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Seale AN, Carvalho JS, Gardiner HM, Mellander M, Roughton M, Simpson J, et al. Total anomalous pulmonary venous connection: Impact of prenatal diagnosis. Ultrasound Obstet Gynecol. 2012;40:310–8. doi: 10.1002/uog.11093. [DOI] [PubMed] [Google Scholar]
- 8.Zhang Y, Shao Q, Sun L, Ge S, He Y. Prenatal diagnosis of total anomalous pulmonary venous connection by 2D and 3D fetal echocardiography. Echocardiography. 2017;34:1852–7. doi: 10.1111/echo.13698. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


