ABSTRACT
Objective:
To identify the scientific evidence on the impacts caused by the use of screens during the COVID-19 pandemic in children and adolescents, raising reflections for future interventions with this public.
Data source:
This is an integrative literature review, conducted in the databases Medical Literature Analysis and Retrieval System Online (MEDLINE), Literatura Latino-Americana e do Caribe em Ciências da Saúde (LILACS), Cumulative Index to Nursing and Allied Health Literature (CINAHL), United States National Library of Medicine (PubMed), Scopus, Web of Science, and Embase, published from March 2020 to January 2022, in Portuguese, English and Spanish.
Data synthesis:
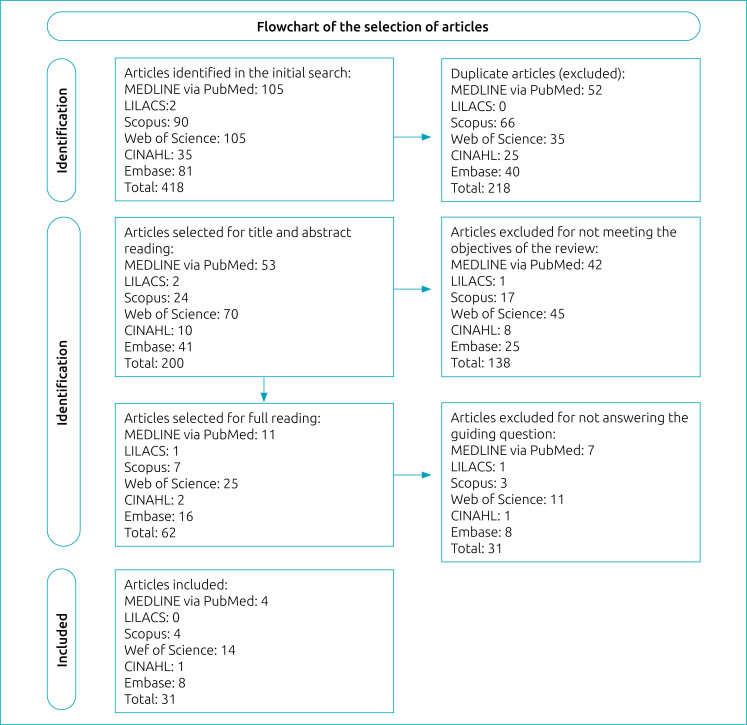
The search strategies allowed retrieving 418 articles, of which 218 were duplicates. The analysis of titles and abstracts resulted in the maintenance of 62 studies. Of these, 31 were excluded from the reading of the full text, since they did not clearly present the phenomenon investigated. Thirty-one were eligible, resulting in five categories: eye consequences; increased sedentary behavior and weight; change in eating habits; implications for sleep quality and impacts on mental health.
Conclusions:
The excessive use of screens during the pandemic led to numerous consequences for children and adolescents, with a higher incidence of visual damage, sedentary lifestyle, inadequate eating habit and increased weight gain, in addition to impaired sleep quality and mental health. This study provides subsidy for health professionals to carry out continuing education focused on this theme, and elaborate effective interventions for this public in this transition to the post-pandemic period.
Keywords: Child development, Mobile applications, Exposure time, Risk factors, Coronavirus infections
RESUMO
Objetivo:
Identificar as evidências científicas sobre os impactos causados pelo uso de telas durante a pandemia da COVID-19 em crianças e adolescentes, almejando reflexões para futuras intervenções com esse público.
Fontes de dados:
Trata-se de uma revisão integrativa da literatura, realizada nas bases de dados Medical Literature Analysis and Retrieval System Online (MEDLINE), Literatura Latino-Americana e do Caribe em Ciências da Saúde (LILACS), Cumulative Index to Nursing and Allied Health Literature (CINAHL), United States National Library of Medicine (PubMed), Scopus, Web of Science e Embase, publicados de março de 2020 a janeiro de 2022, em português, inglês e espanhol.
Síntese dos dados:
As estratégias de busca possibilitaram recuperar 418 artigos, sendo 218 duplicados. A análise de títulos e resumos resultou na manutenção de 62 estudos. Destes, após a leitura do texto integral foram excluídos 31, uma vez que não apresentavam com clareza o fenômeno investigado. Foram elegíveis 31 estudos, emergindo cinco categorias: consequências oculares; aumento do comportamento sedentário e do peso; alteração dos hábitos alimentares; implicações na qualidade do sono e impactos na saúde mental.
Conclusões:
Percebe-se que o uso telas em excesso durante a pandemia trouxe inúmeras consequências para o público infantojuvenil, com maior incidência de acometimentos visuais, sedentarismo, alimentação inadequada e, por consequência, maior ganho de peso, além de prejuízos à qualidade do sono e à saúde mental. Este estudo fornece subsídios para que os profissionais da saúde realizem educação continuada voltada para essa temática e elaborem intervenções efetivas para esse público nesta transição para o período pós-pandêmico.
Palavras-chave: Desenvolvimento infantil, Aplicativos móveis, Tempo de exposição, Fatores de risco, Infecções por Coronavírus
INTRODUCTION
Technologies evolve rapidly, and are inserted in the daily lives of children and adolescents through pocket, mobile and portable devices, having consequences for healthy development. 1 In childhood, heavy use of these devices may increase the risk of cardiovascular diseases and psychological disorders, in addition to favoring exposure to inadequate content. Some authors associate prolonged screen exposure to delays in linguistic domains and fine motor skills. 1 In adolescence, it significantly influences social and family interactions and mood, with a greater risk of developing depression, self-extermination attempts, low self-esteem, as well as other behavioral problems. 2
Children's early access to technologies and the inappropriate use of these tools can compromise their social, cognitive, and affective development. In these media, they are exposed to advertisements that rely on persuasive and appealing techniques to reach mainly children, exercising intense control over their behavior. 3 The trajectory of screen use was analyzed at 24, 36 and 60 months of age in Canadian children, and heavy use showed poorer child development and sub-optimal learning outcomes. 4 In addition, intense use of screens contributes to weight gain that can trigger obesity, sedentarism, and accelerate or accentuate possible physical and mental disorders. 4,5
Use of screens, including television sets, video games, and computers, is a practice that works as a source of leisure and entertainment for adolescents, replacing outdoor activities. The impact of this habit results in consumption of unhealthy foods and physical inactivity, increasing the prevalence of overweight and obesity in this age group. In addition, excessive use of these technologies can have negative consequences on vision development, as well as on sleep quality and psychological health. 6
Such a reality and its problems have been intensified with the advent of COVID-19. In March 2020, the World Health Organization declared the Coronavirus Disease 2019 (COVID-19) pandemic — an acute, potentially serious respiratory infection with high transmissibility 7 that required necessary global preventive measures, such as social distancing to break the disease's transmission chain. Currently, the impacts of these restrictions on the population's health, communication, interpersonal, family, social and economic relationships can be observed. 4
Initially, with the interruption of school activities, children and adolescents witnessed abrupt changes in their daily routines, were physically more distant from friends, remained in home confinement, and were more exposed to alarming information about the pandemic, increasing feelings of anxiety, stress and sadness. 4 There was an absence of school space and decreased outdoor leisure activities, increasing the use of screens and affecting quality of life. This new reality presents short, medium and long-term effects directly linked to the development of comorbidities, in addition to physical, psychological and behavioral complications that may arise. 8
In January 2021 the vaccination campaign against COVID-19 began in Brazil, in a gradual progress, and in 2022 the vaccine was made available to children. 9 With the advancement of vaccination and its benefits, there was a decrease in restrictive measures, including the return to school. However, studies show that even after going back to school children have low levels of physical activity and increased screen time and sedentary activities. 5
This study is justified by the need to investigate the impacts caused by screen use during the pandemic in children and adolescents, grouping information essential for the performance of health professionals given the repercussions of the COVID-19 pandemic. Thus, it aimed to identify scientific evidence of the impacts of screen use during the COVID-19 pandemic in children and adolescents, raising reflections for future interventions with this public.
METHOD
This is a study that used the integrative review, broad method, which combines experimental and non-experimental research to achieve a more didactic understanding of a phenomenon of interest, presenting the state of science and applicability in health practice. 10
For the elaboration of this integrative review, the following steps were performed: identification of the problem (clear definition of the review purpose), search of the literature (delimitation of keywords, databases, establishment of inclusion and exclusion criteria for the selection of articles), evaluation and data analysis.
To guide the integrative review, the following question was formulated: What are the impacts caused by the use of screens during the COVID-19 pandemic on children and adolescents?
The following electronic databases were used: Medical Literature Analysis and Retrieval System Online (MEDLINE), Latin American and Caribbean Literature in Health Sciences (LILACS), Cumulative Index to Nursing and Allied Health Literature (CINAHL), National Library of Medicine and National Institutes of Health (PubMed), Scopus, Web of Science, and Embase. The search was conducted by the authors independently in order to ensure the legitimacy of the study, recovering scientific articles published from March 2020, after the beginning of the pandemic and the consequent establishment of prevention measures.
The inclusion criteria of the articles were: original, complete studies, published in English, Portuguese and Spanish, with full texts, available online in the selected databases, addressing the impacts of the use of screens on children and adolescents during the COVID-19 pandemic in the period from March 2020 to January 2022. This is the period between the recognition by the World Health Organization of COVID-19 as a pandemic and the date of the search for articles in the databases. 11 Articles that did not include the guiding question, review, abstracts and conference proceedings, editorials, experience reports, theoretical essays, single case study and duplicate studies were excluded from the selection.
The search was conducted during the month of January 2022, using combinations between the keywords, which are descriptors in Descriptors in Health Sciences (DeCS), Medical Subject Headings (MeSH) and Embase subject headings (Emtree): Screen Time/Tempo de Tela/Tiempo de Pantalla and Child/Criança/Niño and Adolescent/Adolescente/Adolescente, combined with the term COVID-19 in all three languages.
The studies retrieved by searching the databases were exported to the Rayyan QCRI Program. Subsequently, duplicate studies were removed, and titles and abstracts were read by three reviewers (MAAR, MLF e JTF) using the double-blind method in order to identify potentially eligible studies. Those studies that presented doubts and/or divergences between the reviewers regarding the inclusion or exclusion were solved by a fourth author with expertise in child and adolescent health (ECRG).
For the compilation of results, a table was built with the main characteristics of the studies, such as: title, authors and year of publication, journal, language, country of origin, objective, methodological approach, population, main results, conclusions, and bibliographic references.
There was no need for approval by the Research Ethics Committee because this is a bibliographic study. Ethical aspects and copyright were respected, and the studies referenced.
The articles included in this study were selected, evaluated, and classified hierarchically according to their level of evidence. This practice contributes to the decision-making of health professionals. In this study, the proposal of Melnyk and Fineout-Overholt was adopted, which is shown in Table 1.
Table 1. Level of evidence classification.
| I | Evidence from systematic review or meta-analysis of all relevant randomized controlled trials or from clinical guidelines based on systematic reviews of randomized controlled trials. |
| II | Evidence derived from at least one well-designed randomized controlled clinical trial. |
| III | Evidence obtained from well-designed clinical trials without randomization. |
| IV | Evidence from well-designed cohort and case-control studies. |
| V | Evidence from a systematic review of descriptive and qualitative studies. |
| VI | Evidence derived from a single descriptive or qualitative study. |
| VII | Evidence from opinion of authorities and/or report of expert committees. |
RESULTS
The search strategies allowed retrieving 418 articles, of which 218 were duplicates. The analysis of titles and abstracts resulted in 62 studies being included. Of these, 31 were excluded from reading of the full text, since they did not clearly present the phenomenon investigated, and 31 were included in the review, as shown in the flowchart (Figure 1).
Figure 1. Flowchart of article selection.
Of the 31 papers analyzed, all were quantitative articles, except one. As for year of publication, the highest incidence was 2021 (27 articles), 2020 (2 articles) and 2022 (2 articles). Seven were developed in China, four in Canada, two in Italy, India, France and Turkey, and one in the Netherlands, Spain, Japan, Brazil, Saudi Arabia, Iran, the United States of America (USA), Hungary, Jordan, Indonesia, Poland and Egypt. All studies were published in English. The table shows the studies’ main characteristics (Table 2). 2,5,6,12-39
Table 2. Characterization of articles according to author, year of publication, type of study, methodological approach, and level of evidence.
| Reference | Country | Type of study | Level of evidence |
|---|---|---|---|
| McArthur et al. 12 | Canada | Longitudinal cohort (n=846) | IV |
| Ten Velde et al. 5 | Netherlands | Exploratory cohort (n=233) | IV |
| Liu et al. 13 | China | Prospective cohort (n=3831) | IV |
| Choi et al. 14 | China | Exploratory cohort (n=171) | IV |
| Zhang et al. 15 | China | Prospective cohort (n=1793) | IV |
| Adachi et al. 16 | Japan | Prospective cohort (n=4875) | IV |
| Li et al. 17 | Canada | Longitudinal cohort (n=2026) | IV |
| Alghadir et al. 18 | Saudi Arabia | Prospective cohort (n=214) | IV |
| Saxena et al. 19 | India | Prospective cohort (n=1237) | IV |
| Cardy et al. 20 | Canada | Prospective cohort (n=414) | IV |
| Xiao et al. 2 | China | Prospective cross-sectional (n=1680) | IV |
| Pietrobelli et al. 21 | Italy | Observational longitudinal (n=32) | IV |
| Kołota and Głąbska 22 | Poland | Longitudinal (n=1334) | IV |
| Hartley et al. 23 | France | Longitudinal (n=1777) | IV |
| Alvarez-Peregrina et al. 24 | Spain | Cross-sectional (n=1600) | V |
| Helito et al. 25 | Brazil | Cross-sectional (n=387) | V |
| Shuai et al. 26 | China | Cross-sectional (n=192) | V |
| Oliva et al. 27 | Italy | Cross-sectional prospective (n=9974) | V |
| Surekha et al. 28 | India | Cross-sectional (n=2000) | V |
| Hadianfard et al. 6 | Islamic Republic of Iran | Cross-sectional (n=510) | V |
| Tandon et al. 29 | United States | Cross-sectional l (n=1000) | V |
| Peddie et al. 30 | Canada | Cross-sectional (n=146) | V |
| Guo et al. 31 | China | Descriptive cross-sectional (n=10,416) | V |
| Berki and Pikó 32 | Hungary | Cross-sectional (n=705) | V |
| Wang et al. 33 | China | Prospective cross-sectional (n=123,535) | V |
| Chambonniere et al. 34 | France | Cross-sectional (n=6491) | V |
| Hourani et al. 35 | Jordan | Cross-sectional (n=477) | V |
| Andriyani et al. 36 | Indonesia | Qualitative (n=20) | V |
| Ceylan et al. 37 | Türkiye | Descriptive cross-sectional (n=384) | V |
| Yakşi et al. 38 | Türkiye | Cross-sectional (n=506) | V |
| Hashem et al. 39 | Egypt | Cross-sectional (n=765) | V |
All the papers examined addressed the theme of the impacts of screen use during the COVID-19 pandemic on children and adolescents. Five categories emerged from these findings: eye consequences; increased sedentary behavior and weight; altered eating habits; implications for sleep quality and impacts on mental health.
Category one — eye consequences
The studies analyzed revealed the association between high use of screens and higher risks of myopia, as well as other eye problems in children and adolescents during the COVID-19 pandemic. 13-15,19,24,30,33
Chinese researchers carried out a large-scale survey, finding that the use of screens in this period increased due to school closures, as well as myopia was more prevalent among respondents who were in high school and fundamentally, screen time was associated with greater risks of symptomatic myopia progression and the study population used more computers and smartphones. 13 The researchers also claim, that the use of computers and smartphones has a higher probability of facilitating the progression of myopia compared to the use of television for remote education. 13
Similar results were found in other studies regarding the progression and incidence of myopia associated with restrictive measures to contain the spread of Covid-19, in addition to axial stretching. 14,15 An association was also found between excessive exposure to electronics eyestrain, blurred vision or dry eyes. 31
Category two — increased sedentary behavior and weight
The studies revealed greater use of screens during the period of restrictive measures to control COVID-19, providing increased sedentary activities, decreased physical exercise and less time outdoors, compared to the year before the pandemic. 5,6,15,18,19,21,24,28,34,37 Furthermore, there was an increase in children's weight and body mass index (BMI) due to longer time watching television and using computers. 18,21,28,37
With the restrictions imposed, the increased use of screens was inevitable, since they became educational tools and a form of leisure, especially for those with restricted access to external areas. 31,34,36 Electronic devices, whether televisions, computers, laptops or tablets, when located in bedrooms, present a greater risk of being used for long periods. 18
The alarming fact is that, even after relaxation of the restriction measures, children still reported performing fewer physical activities than in the previous year, showing that the reopening of schools did not fully restore these activities. This indicates that there may be a lasting impact related to screen use time in that such behavior has been normalized. 5 Therefore, ending the COVID-19 restriction measures alone will not by itself promote new habits in children and adolescents. 5
Category three — altered eating habits
Another issue analyzed in the studies was the diet associated with the use of electronics, where a common habit of eating while watching TV was found. 35 This is related to higher fat intake and consumption of advertised products, such as sugary cereals, sweets, drinks and snacks. 28 Such behavior was more observed as of the start of distance education during the pandemic, compared to the previous year. 22 The use of screens can indirectly increase food consumption and the intake of unhealthy foods, reduce physical activity and energy expenditure, increasing the risk of obesity. 6
Investigating the relationship between screen time and changes in the diet of children and adolescents showed that increased use of mobile phones, television, laptop and video games was associated with increased appetite, increased consumption of sweets and unhealthy foods, snacks and frequent snacks between meals, as well as with children who were indifferent to eating fruits and vegetables. 39 Scientific evidence suggests that the change in diet and lifestyle caused by the pandemic has led to excessive body weight gain in children and adolescents, and this can have serious health consequences. 21
Category four — implications for sleep quality
The excessive use of electronics, according to the studies analyzed, has consequences on hygiene and sleep quality, especially when these devices are used at night. 23,25 This can be explained due to changes in the biological clock, which plays an important role in the good performance of restorative sleep. 23 Night exposure to intense light can stimulate the wakefulness system, making individuals more alert and causing them to sleep later. 23
Poor sleep quality may be related to the exacerbated use of screens, changes in routines and schedules, little exposure to light during the day and a lot of exposure to light at night, changes that may be related to the restriction measures imposed during the pandemic, 23 bringing physical and psychological consequences to children and adolescentes. 12
Category five — impacts on mental health
The changes caused by social isolation had a great impact on the mental health of the pediatric and adolescent population. 12,20,27,29,38 This new reality implies less time for performing outdoor activities and lack of socialization with peers, consequently fostering the use of electronic devices both for education and as a form of leisure. 17,27
Children who use screens for long periods have higher levels of depressive and anxiety symptoms. 12,17,26-28,32,38 In contrast, although education implies spending several hours in front of a screen, learning can act as a form of protection, since it allows the reduction of stressors caused by confinement. 27
The use of smartphones at younger ages may be a risk factor for mental health in the context of the COVID-19 pandemic. 16 Therefore, it is necessary to adopt measures aimed at minimizing damage, using other devices in a moderate way and with limited time.
Studies show that more time on TV or digital media causes high levels of inattention and hyperactivity, and the excessive use of video games provoke irritability, inattention and hyperactivity. 26,27 In addition, longer screen time is associated with more conflicts with parents, since this habit can lead to a negative mood in adolescents. 2
DISCUSSION
With globalization, the use of technologies has become commonplace, and this reality has both positive and negative aspects; in the pandemic period experienced in recent years, this scenario has become more evident. 6 Although in developed countries access to electronic devices is easier compared to developing countries, among the studies analyzed, the largest amount of research was conducted in emerging countries (n=17), showing that the impacts of screen use have been a global concern, also confirmed by the diversity of countries developing research on the subject.
The more frequent access of children and adolescents to the web is not a recent concern, but has intensified in several countries including Brazil, since the problematic use of these devices can cause mental, visual and auditory disorders. 13,16,25 In 2019, Brazilians were ranked third in relation to daily hours online, 40 Brazilian teenagers in particular ranked second in internet connection time outside of school hours. 41 However, only one of the studies analyzed here was developed in Brazil, showing the need to develop more research on the subject, especially after the pandemic.
As addressed in category one, although myopia is considered a benign alteration, its prevalence has become increasingly common. This pathology can lead to severe visual complications, including macular degeneration, posterior staphyloma, cataract, glaucoma, and retinal detachment, becoming a public health concern. 13,42
Myopia is related to individual characteristics, but it is also caused by environmental factors and lifestyle, thus prolonged screen use is an important factor in its development. 43 This should be taken into account and given due importance, since school activities through virtual tools during the pandemic significantly increased screen time, which contributed to symptomatic myopia incidence. 13
The size of the screen, as pointed out by the studies, can also influence the progression of myopia, devices that have larger screens provide viewing at a more acceptable distance, minimizing the use of close vision, which reduces stimulation of hypermetropic blur, while with smaller screens the distance is shorter, which can lead to increased eye impairment. 44 These effects are more frequently observed in children and adolescents, since optical development is not fully completed. 13,33
Based on these findings, it is necessary to disseminate information, especially to parents and guardians, to warn them of the recommendations regarding the necessary distance when looking at a screen, so they can prioritize those that appear to be less harmful and limit use time, since the risks of developing myopia increase every hour that a child is exposed to a digital device. 13
The change in the lifestyle of the investigated population during the pandemic, with the consequent exacerbated use and the consequent sedentary lifestyle are associated with several health risks, including hypertension, metabolic syndrome and obesity, which presented worrying indicators even before the pandemic. 45
According to data from the Brazilian Society of Bariatric and Metabolic Surgery, the COVID-19 pandemic has had a major impact on the childhood obesity picture in several countries, including Brazil, due to changing lifestyle habits and increased screen time. The Brazilian Institute of Geography and Statistics (IBGE) points out that, in a group of three children from five to nine years old, one is overweight in the country. The context of obesity in Brazil was already worrisome and worsened during the pandemic. Such reality implies morbidities that can cause various damage to health. 46
This corroborates the Brazilian study developed in 2022, which sought to investigate the consequences of social isolation in relation to weight gain in children, analyzing the nutritional diagnosis of children in the five Brazilian regions, between the years 2019 and 2021, through reports of the Food and Nutrition Surveillance System (SISVAN) of the Ministry of Health, which observed an increase in weight in children during the pandemic in all Brazilian regions, reflecting changes in lifestyle during this period. 47 On the other hand, the pandemic showed regional disparities in Brazil, as there were groups of children and adolescents with malnutrition caused by the worsening of the economic crisis, compromising the growth and development of children and youth. 48
Understanding that these long-term habits can have numerous consequences for this population, it is necessary to develop strategies to reduce screen time and stimulate physical activity by retrieving games that stimulate physical abilities and encouraging sports.
In addition to the increase in sedentary lifestyle, another concern related to the use of screens is poor diet. As well as the implications found in studies for the consumption of foods with low nutritional content and excess calories associated with technologies, other complications arise, which can be justified by the economic crisis faced during this period, the worsening in family income, the increase in food prices, providing food insecurity and malnutrition. Such reality is faced by Brazilian children and adolescents who suffer from neuropsychomotor impairments, that have a greater likelihood of developing chronic diseases such as diabetes, hypertension, and overweight. 49
The Brazilian Society of Pediatrics points out that during the pandemic families started to overeat foods with high sugar content that provide a sense of pleasure. Despite this, family meals can be a nutritional protection mechanism, by favoring the consumption of complete meals, with appropriate intervals, which can ensure an adequate intake of macronutrients, minerals, antioxidants, and vitamins, thus ensuring adequate nutrition. 50
Guidelines on food in the school environment or offered by the family members are necessary so that this public is encouraged to create healthier habits in the current transition to the post-pandemic period, an important factor for a good nutritional status, favoring the adequate development of children and adolescents.
Sleep is essential for the proper functioning of the human body, since it contributes to physical and mental homeostasis. 51 During childhood and adolescence, it gains even more importance by acting in the physiological processes of growth, maturation and health, 52 in addition to having an important role in strengthening the immune system. 42
As shown by the investigated studies, the exposure to light-emitting diodes (LED) with a short wavelength (blue range) at night also blocks the secretion of hormones that are important for sleep regulation, such as melatonin, thus morning awakening is later. 53 In addition, short sleep and early awakening can lead to depressive or stress symptoms. 54 Thus, it is essential to guide this public about creating routines, having regular and appropriate schedules for sleep, adapting exposure to light, and limiting the use of screens at night.
Thus the importance of stimulating outdoor activities to reduce risks to mental health. Although the quality of mental health is related to numerous factors, controlling exposure to screens is essential. 27 There is a need to identify the threats to the mental health of this population and to carry out prevention and intervention strategies to minimize the damage caused by confinement as a result of the COVID-19 pandemic.
Among the study's limitations is the fact that analysis of the impacts of screen use during the COVID-19 pandemic was restricted to the month of January 2022, not allowing these impacts to be evaluated up to the present moment. Another limiting factor is the publication of studies in different countries, with only one Brazilian study being retrieved, which shows regional disparities in publications on the subject and makes it impossible to generalize the data. Regarding the levels of evidence, a prevalence of cohort studies, case-control and systematic reviews of qualitative studies was noted. It is believed that the randomized clinical studies not found could clarify the most severe consequences of the use of screens in children and adolescents.
The findings reveal that excessive use of screens during the pandemic has led to numerous consequences for children and adolescents, with a higher incidence of visual impairments, sedentary lifestyle, inadequate eating habits, in addition to weight gain, impaired sleep quality and losses in mental health. The changes in habits due to the restrictive measures presented a contrast between the increase in the consumption of foods with low nutritional content and the excess of calories associated with technology, which points to the problem of overweight and malnutrition that compromises the development of children and adolescents, something that is no longer restricted to developed countries. Thus, this study provides subsidy for health professionals to carry out continuing education focused on this theme, warning parents and guardians of the implications of the use of screens, as well as developing interventions that are effective for children in the prevention and promotion of health in the transition to the post-pandemic period.
Footnotes
Funding
The study did not receive any funding.
REFERENCES
- 1.Nobre JN, Santos JN, Santos LR, Guedes SC, Pereira L, Costa JM, et al. Determining factors in children's screen time in early childhood. Ciênc Saúde Colet. 2021;26:1127–1136. doi: 10.1590/1413-81232021263.00602019. [DOI] [PubMed] [Google Scholar]
- 2.Xiao S, Yan Z, Zhao L. Physical activity, screen time, and mood disturbance among chinese adolescents during COVID-19. J Psychosoc Nurs Ment Health Serv. 2021;59:14–20. doi: 10.3928/02793695-20201104-04. [DOI] [PubMed] [Google Scholar]
- 3.Lima MG, Sousa FN. O uso excessive de telas por crianças e adolescents: uma análise do context da COVID-19. Revista Livre de Sustentabilidade e Empreendedorismo. 2023;8:90–108. doi: 10.5281/zenodo.7705271. [DOI] [Google Scholar]
- 4.McArthur BA, Browne D, Tough S, Madigan S. Trajectories of screen use during early childhood: predictors and associate behavior and learning outcomes. Comput Human Behav. 2020;113:106501–106501. doi: 10.1016/j.chb.2020.106501. [DOI] [Google Scholar]
- 5.Ten Velde G, Lubrecht J, Arayess L, van Loo C, Hesselink M, Reijnders D, et al. Physical activity behaviour and screen time in Dutch children during the COVID-19 pandemic: pre-, during-and post-school closures. Pediatr Obes. 2021;16:e12779. doi: 10.1111/ijpo.12779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hadianfard AM, Mozaffari-Khosravi H, Karandish M, Azhdari M. Physical activity and sedentary behaviors (screen time and homework) among overweight or obese adolescents: a cross-sectional observational study in Yazd, Iran. BMC Pediatr. 2021;21:421–421. doi: 10.1186/s12887-021-02892-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brazil Ministerio da Saúde [homepage on the Internet]. O que é a COVID-19? [[cited 2023 Apr 27]]. Available from: https://www.gov.br/saude/pt-br/coronavirus/o-que-e-o-coronavirus .
- 8.Hall G, Laddu DR, Phillips SA, Lavie CJ, Ross AA. A tale of two pandemics: how will COVID-19 and global trends in physical inactivity and sedentary behavior affect one another? Prog Cardiovasc Dis. 2021;64:108–110. doi: 10.1016/j.pcad.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fundação Oswaldo Cruz [homepage on the Internet] COVID-19: balanço de dois anos da pandemia aponta vacinação como prioridade. [[cited 2023 Apr 24]]. Available from: https://portal.fiocruz.br/noticia/covid-19-balanco-de-dois-anos-da-pandemia-aponta-vacinacao-como-prioridade .
- 10.Melnyk BM, Fineout-Overholt E. Evidence-based practice in nursing & healthcare. A guide to best practice. 5th ed. Philadelphia: Lippincot Williams & Wilkins; 2005. [Google Scholar]
- 11.Organização Mundial da Saúde [homepage on the Internet] OMS afirma qie COVID-19 é agora caracterizada como pandemia. [[cited 2023 Apr 24]]. Available from: https://www.paho.org/pt/news/11-3-2020-who-characterizes-covid-19-pandemic .
- 12.McArthur BA, Racine N, McDonald S, Tough S, Madigan S. Child and family factors associated with child mental health and well-being during COVID-19. Eur Child Adolesc Psychiatry. 2023;32:223–233. doi: 10.1007/s00787-021-01849-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu J, Li B, Sun Y, Chen Q, Dang J. Adolescent vision health during the outbreak of COVID-19: association between digital screen use and myopia progression. Front Pediatr. 2021;9:662984–662984. doi: 10.3389/fped.2021.662984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Choi KY, Chun RK, Tang WC, To CH, Lam CS, Chan HH. Evaluation of an optical defocus treatment for myopia progression among schoolchildren during the COVID-19 pandemic. JAMA Netw Open. 2022;5:e2143781. doi: 10.1001/jamanetworkopen.2021.43781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang X, Cheung SS, Chan HN, Zhang Y, Wang YM, Yip BH, et al. Myopia incidence and lifestyle changes among school children during the COVID-19 pandemic: a population-based prospective study. Br J Ophthalmol. 2022;106:1772–1778. doi: 10.1136/bjophthalmol-2021-319307. [DOI] [PubMed] [Google Scholar]
- 16.Adachi M, Takahashi M, Shinkawa H, Mori H, Nishimura T, Nakamura K. Longitudinal association between smartphone ownership and depression among schoolchildren under COVID-19 pandemic. Soc Psychiatry Psychiatr Epidemiol. 2022;57:239–243. doi: 10.1007/s00127-021-02196-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li X, Vanderloo LM, Keown-Stoneman CD, Cost KT, Charach A, Maguire JL, et al. Screen use and mental health symptoms in Canadian children and youth during the COVID-19 pandemic. JAMA Netw Open. 2021;4:e2140875. doi: 10.1001/jamanetworkopen.2021.40875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Alghadir AH, Iqbal ZA, Gabr AS. The relationships of watching television, computer use, physical activity, and food preferences to body mass index: gender and nativity differences among adolescents in Saudi Arabia. Int J Environ Res Pub Health. 2021;18:9915–9915. doi: 10.3390/ijerph18189915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Saxena R, Gupta V, Rakheja V, Dhiman R, Bhardawaj A, Vashist P. Lifestyle modification in school-going children before and after COVID-19 lockdown. Indian J Ophthalmol. 2021;69:3623–3629. doi: 10.4103/ijo.IJO_2096_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cardy RE, Dupuis A, Anagnostou E, Ziolkowski J, Biddiss EA, Monga S, et al. Characterizing changes in screen time during the COVID-19 pandemic school closures in Canada and its perceived impact on children with autism spectrum disorder. Front Psychiatry. 2021;12:702774–702774. doi: 10.3389/fpsyt.2021.702774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pietrobelli A, Fearnbach N, Ferruzzi A, Vrech M, Heo M, Faith M, et al. Effects of COVID-19 lockdown on lifestyle behaviors in children with obesity: longitudinal study update. Obes Sci Pract. 2021;8:525–528. doi: 10.1002/osp4.581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kołota A, Głąbska D. COVID-19 pandemic and remote education contributes to improved nutritional behaviors and increased screen time in a Polish population-based sample of primary school adolescents: diet and activity of youth during COVID-19 (DAY-19) study. Nutrients. 2021;13:1596–1596. doi: 10.3390/nu13051596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hartley S, Francs CC, Aussert F, Martinot C, Dagneaux S, Londe V, et al. The effects of quarantine for SARS-CoV-2 on sleep: an online survey. Encephale. 2020;46:S53–S59. doi: 10.1016/j.encep.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alvarez-Peregrina C, Martinez-Perez C, Villa-Collar C, Andreu-Vázquez C, ruiz-Pomeda A, Sánchez-Tena MA. Impact of COVID-19 home confinement in children's refractive errors. Int J Environ Res Public Health. 2021;18:5347–5347. doi: 10.3390/ijerph18105347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Helito AC, Lindoso L, Sieczkowska SM, Astley C, Queiroz LB, Rose N, et al. Poor sleep quality and health-related quality of life impact in adolescents with and without chronic immunosuppressive conditions during COVID-19 quarantine. Clinics (Sao Paulo) 2021;76:e3501. doi: 10.6061/clinics/2021/e3501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shuai L, He S, Zheng H, Wang Z, Qiu M, Xia W, et al. Influences of digital media use on children and adolescents with ADHD during COVID-19 pandemic. Global Health. 2021;17:48–48. doi: 10.1186/s12992-021-00699-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Oliva S, Russo G, Gili R, Russo L, Di Mauro AD, Spagnoli A, et al. Risks and protective factors associated with mental health symptoms during COVID-19 home confinement in Italian children and adolescents: the understandingkids study. Front Pediatr. 2021;9:664702–664702. doi: 10.3389/fped.2021.664702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Surekha BC, Karanati K, Venkatesan K, Sreelekha BC, Kumar VD. E-learning during COVID-19 pandemic: a surge in childhood obesity. Indian J Otolaryngol Head Neck Surg. 2021;74:3058–3064. doi: 10.1007/s12070-021-02750-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tandon PS, Zhou C, Johnson AM, Gonzalez ES, Kroshus E. Association of children's physical activity and screen time with mental health during the COVID-19 pandemic. JAMA Netw Open. 2021;4:e2127892. doi: 10.1001/jamanetworkopen.2021.27892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Peddie MC, Scott T, Haszard JJ. Using a 24 h activity recall (STAR-24) to describe activity in adolescent boys in New Zealand: comparisons between a sample collected before, and a sample collected during the COVID-19 lockdown. Int J Environ Res Public Health. 2021;18:8035–8035. doi: 10.3390/ijerph18158035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Guo YF, Liao MQ, Cai WL, Yu XX, Li SN, Ke XY, et al. Physical activity, screen exposure and sleep among students during the pandemic of COVID-19. Sci Rep. 2021;11:8529–8529. doi: 10.1038/s41598-021-88071-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Berki T, Pikó B. Sedentary lifestyle may contribute to the risk of depression during the COVID-19 pandemic: a snapshot of Hungarian adolescents. Eur J Mental Health. 2021;16:99–119. doi: 10.5708/EJMH.16.2021. [DOI] [Google Scholar]
- 33.Wang J, Li Y, Musch DC, Wei N, Qi X, Ding G, et al. Progression of myopia in school-aged children after COVID-19 home confinement. JAMA Ophthalmol. 2021;139:293–300. doi: 10.1001/jamaophthalmol.2020.6239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chambonniere C, Lambert C, Fearnbach N, Tardieu M, Fillon A, Genin P, et al. Effect of the COVID-19 lockdown on physical activity and sedentary behaviors in French children and adolescents: new results from the ONAPS national survey. Eur J Integr Med. 2021;43:101308–101308. doi: 10.1016/j.eujim.2021.101308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hourani HA, Alkhatib B, Abdullah M. Impact of COVID-19 lockdown on body weight, eating habits, and physical activity of Jordanian children and adolescents. Disaster Med Public Health Prep. 2022;16:1855–1863. doi: 10.1017/dmp.2021.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Andriyani FD, Biddle SJ, Cocker K. Adolescents’ physical activity and sedentary behaviour in Indonesia during the COVID-19 pandemic: a qualitative study of mothers’ perspectives. BMC Public Health. 2021;21:1864–1864. doi: 10.1186/s12889-021-11931-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ceylan SS, Erdoğan Ç, Turan T. Investigation of the effects of restrictions applied on children during COVID-19 pandemic. J Pediatr Nurs. 2021;61:340–345. doi: 10.1016/j.pedn.2021.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yakşi N, Eroğlu M, Özdemir M. COVID-19: predictors of depression and anxiety among high school students. Kıbrıs Türk Psikiyatri ve Psikoloji Dergisi. 2021;3:192–202. doi: 10.35365/ctjpp.21.3.20. [DOI] [Google Scholar]
- 39.Hashem SA, El Refay AS, Mostafa HH, Kamel IH, Sherif LS. Impact of coronavirus disease-19 lockdown on Egyptian children and adolescents: dietary pattern changes health risk. Open Access Maced J Med Sci. 2020;8:561–569. doi: 10.3889/oamjms.2020.5249. [DOI] [Google Scholar]
- 40.World Wide Web Foundation [homepage on the Internet] 2018 Accessibility Report. [[cited 2023 Apr 24]]. Available from: http://a4ai.org/wp-content/uploads/2018/10/A4AI-2018-Affordability-Report.pdf .
- 41.Education GPS the World of Education at your Fingertips [homepage on the Internet] Brazl. Student performance (PISA 2018) [[cited 2023 Apr 24]]. Available from: http://gpseducation.oecd.org/CountryProfile?primaryCountry=BRA&treshold=10&topic=PI .
- 42.Saw SM, Gazzard G, Shih-Yen EC, Chua WH. Myopia and associated pathological complications. Ophthalmic Physiol Opt. 2005;25:381–391. doi: 10.1111/j.1475-1313.2005.00298.x. [DOI] [PubMed] [Google Scholar]
- 43.Ting DS, Carin L, Dzau V, Wong TY. Digital technology and COVID-19. Nat Med. 2020;26:459–461. doi: 10.1038/s41591-020-0824-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Long J, Cheung R, Duong S, Paynter R, Asper L. Viewing distance and eyestrain symptoms with prolonged viewing of smartphones. Clin Exp Optom. 2017;100:133–137. doi: 10.1111/cxo.12453. [DOI] [PubMed] [Google Scholar]
- 45.Friedrich RR, Polet JP, Schuch I, Wagner MB. Effect of intervention programs in schools to reduce screen time: a meta-analysis. J Pediatr (Rio J) 2014;90:232–241. doi: 10.1016/j.jped.2014.01.003. [DOI] [PubMed] [Google Scholar]
- 46.Sociedade Brasileira de Cirurgia Bariátricia e Metabólica [homepage on the Internet] Estudos revelam que pandemia acelerou aumento de crianças com obedidade. [[cited 2023 Apr 24]]. Available from: https://www.sbcbm.org.br/estudos-revelam-que-pandemia-acelerou-aumento-de-criancas-com-obesidade/
- 47.Zani G, Cunha DC. Impact of social isolation caused by the COVID-19 pandemic on weight gain in school-age Brazilian children. Res Soc Dev. 2022;11:e162111436085. doi: 10.33448/rsd-v11i14.36085. [DOI] [Google Scholar]
- 48.Fundação Oswaldo Cruz. Instituto Nacional de Saúde da Mulher, da Criança e Adolescente Fernandes Figueira [homepage on the Internet] Atenção integral à criança na APS em tempo de pandemia. [[cited 2023 Apr 24]]. Available from: https://portaldeboaspraticas.iff.fiocruz.br/atencao-crianca/atencao-integral-a-crianca-na-aps-em-tempos-de-pandemia/
- 49.Sociedade Brasileira de Pediatria [homepage on the Internet] Mas de 40 mil menores de cinco anos foram internadas no SUS por desnutrição nos últimos dez anos, alerta SBP. [[cited 2023 Apr 24]]. Available from: https://www.sbp.com.br/imprensa/detalhe/nid/mais-de-40-mil-menores-de-cinco-anos-foram-internadas-no-sus-por-desnutricao-nos-ultimos-dez-anos-alerta-sbp/
- 50.Sociedade Brasileira de Pediatria [homepage on the Internet] Atenção aos aspectos nutrológicos da criança com COVID-19 em acompanhemando ambulatorial/domiciliar. [[cited 2023 Apr 24]]. Available from: https://www.sbp.com.br/fileadmin/user_upload/22604b-NA_-_Atencao_aspec_nutrol_crc_com_COVID19.pdf .
- 51.Gajardo YZ, Ramos JN, Muraro AP, Moreira NF, Ferreira MG, Rodrigues PR. Sleep-related problems and associated factors among the Brazilian population: National Health Survey, 2013. Cien Saude Colet. 2021;26:601–610. doi: 10.1590/1413-81232021262.08412020. [DOI] [PubMed] [Google Scholar]
- 52.Santos ES, Souza OF. Evidence of the association between sleep duration and blood pressure in adolescents: a systematic review. Rev Paul Pediatr. 2021;39:e2019225. doi: 10.1590/1984-0462/2021/39/2019225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cajochen C, Frey S, Anders D, Späti J, Bues M, Pross A, et al. Evening exposure to a light-emitting diodes (LED)-backlit computer screen affects circadian physiology and cognitive performance. J Appl Physiol (1985) 2011;110:1432–1438. doi: 10.1152/japplphysiol.00165.2011. [DOI] [PubMed] [Google Scholar]
- 54.Baglioni C, Battagliese G, Feige B, Spiegelhalder K, Nissen C, Voderholzer U, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. 2011;135:10–19. doi: 10.1016/j.jad.2011.01.011. [DOI] [PubMed] [Google Scholar]