Abstract
Nodular fasciitis is a benign reactive soft tissue tumor arising from fibroblasts and myofibroblasts. Its incidence is low and misdiagnosis is frequent especially for malignant lesions. This can lead to inappropriate and unnecessary invasive treatment. Nodular fasciitis of the external auditory canal is extremely rare. So far, around fifteen cases have been reported. We present here the case of a 90-year-old patient with nodular fasciitis of the right external auditory canal. The lesion extends anteriorly for 6.5 cm and reaches the posterior wall of the maxillary sinus. To our knowledge, this is the first case in the literature of an external auditory canal nodular fasciitis presenting as an inflammatory ear polyp with such a wide extension.
Keywords: Nodular fasciitis, External ear canal, Polyp
1. Case
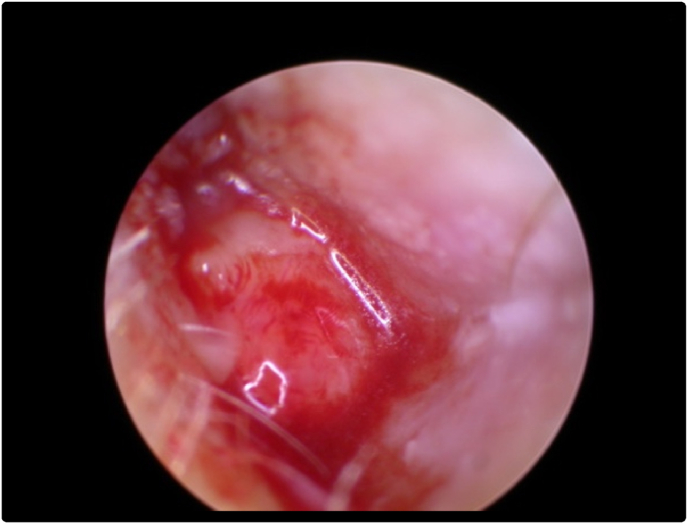
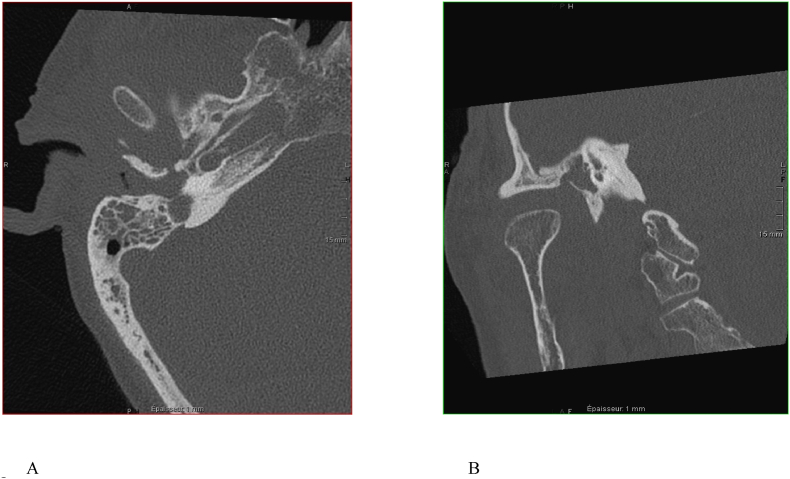
A 90-year-old man showed up to an ENT consultation for spontaneous right otalgia which was exacerbated while chewing. The patient had a history of renal aneurysm, colic adenocarcinoma treated 27 years ago by chemotherapy and surgery, currently in a cured state, and an active myelodysplastic syndrome. The ENT clinical examination showed an inflammatory and fleshy polyp in the right external auditory canal (EAC), the eardrum was not visible (Fig. 1). Biopsies were performed, bringing back inflammatory material including numerous polymorphonuclear neutrophils for which no conclusion could be made. The patient was seen again in order to perform new biopsies and to perform a Computed Tomography of the temporal bone. The latter showed a full middle ear, an irregular and micro-erosive aspect of the external auditory canal as well as a focal transfixion of the hypotympanum on its external side towards the temporomandibular joint. A significant tumefaction of the soft tissues of nodular aspect was also objectified. (Fig. 2).
Fig. 1.
Right ear microscope otoscopy.
Fig. 2.
CT-Scanner Siemens Somatom Definition AS. Ultra high-resolution spiral acquisition in 0.4 mm and MPR reconstruction 1 mm: axial (A) and sagittal (B) section of the right petrous bone.
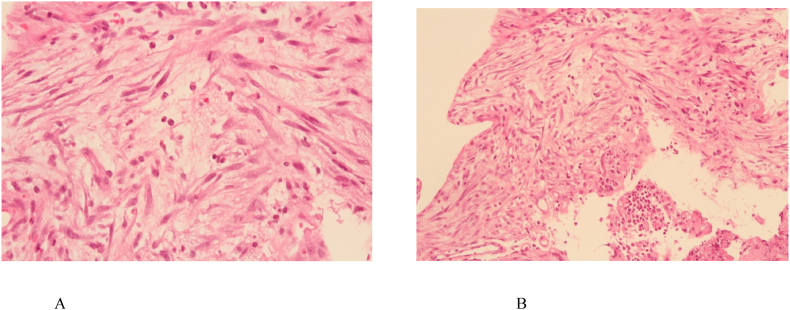
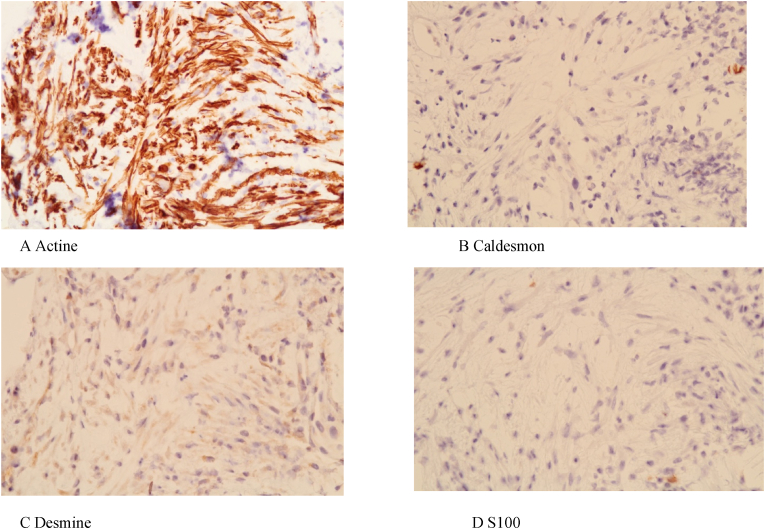
The anatomopathological result on a histological and immunohistochemical basis turned out to be positive for nodular fasciitis. (Fig. 3 and Fig. 4).
Fig. 3.
Histological images with hematoxylin and eosin magnification ×400 (Fig. 3A) and ×200 (Fig. 3B) demonstrating variable cellularity as well as a variable extracellular matrix, ranging from myxoid to fibrous. Note the presence of fusiform cells with a fascicular or storiform arrangement, ovoid nuclei with fine chromatin and low mitotic activity. No significant atypia. Presence of inflammatory elements, mainly scattered lymphocytes.
Fig. 4.
Immunohistochemistry. Myofibroblastic cells are Actin positive (4.A) and negative for Caldesmon (4.B), Desmin (4.C) and protein S100 (4.D).
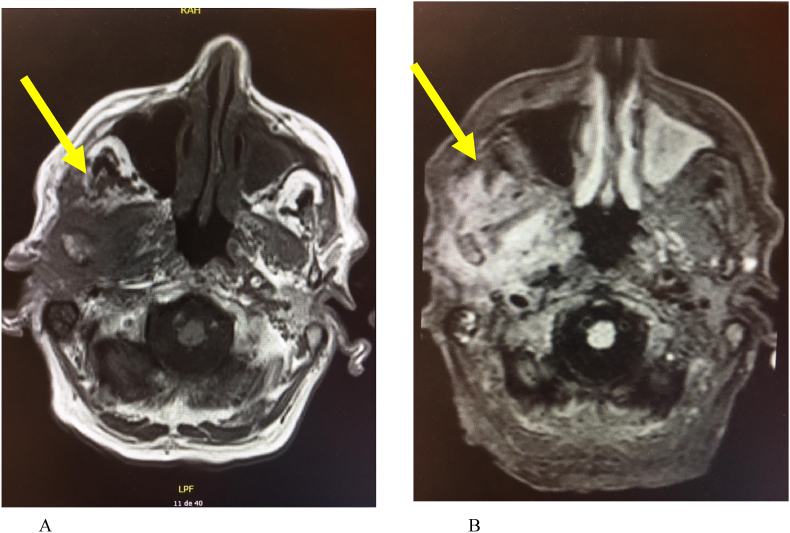
A Magnetic Resonance Imaging (MRI) was also performed, unfortunately of poor quality due to patient movements during the examination but it was still able to describe the size and the extension of the lesion (Fig. 5). The latter is 65 × 60 mm in size and extends from the external auditory canal to the posterior wall of the maxillary sinus in the axial plane.
Fig. 5.
MRI Siemens Magnetom Avento fit 1.5 T. Acquisition. Axial slices through the inferior turbinate in T1-weighted (Fig. 5A) and T2-weighted Flair Fat Sat (Fig5.B). The arrow pointing to the lesion: we note a filling of the right external ear and the middle ear extending by transfixion towards the temporomandibular joint with extensive infiltration of fatty and muscular tissues over 65 mm wide and of 60 mm on the anteroposterior axis around the ascending branch of the mandible. The lesion affects the deep plane of the tonsillar region and joins the posterior wall of the right maxillary sinus. It is contiguous with the right intrapetrous internal carotid and the right internal jugular gulf.
Given the extension of the lesion and the patient's age, empirical treatment was initiated with daily methylprednisolone 32 mg orally associated with topical treatment combining Dexamethasone and Chloramphenicol in the form of ear drops after a multidisciplinary consultation.
Even though the patient had severe hypoacusis and was wearing hearing aids, he reported an improvement of his hearing at the follow-up appointment after 18 days of treatment. However, the lesion had not changed significantly on the otoscopy. Another MRI had been scheduled but the patient died of a stroke unexpectedly before his appointment.
2. Discussion
Nodular fasciitis (NF) is a benign reactive proliferation of myofibroblasts, first described in 1955 by Konwaler as pseudosarcomatous fasciitis (Konwaller et al., 1955). NF has also been referred to as nodular fibrositis, subcutaneous fibromatosis or proliferative fasciitis. It develops intramuscularly, from subcutaneous tissue or fascia. The aetiology remains unknown to date, although there is a notion of trauma in 15% of the cases (Weinreb et al., 2009a).
Considered as reactive lesion for a long time, recent studies have shown a genetic fusion of the MYH9-USP6 genes in 83–92% of cases leading to the overexpression of the protein USP6 (Ubiquitin-specific peptidase 6), pro-oncogene, and which can help confirm the diagnosis (Erickson-Johnson et al., 2011; Chen et al., 2014).
Nodular fasciitis can occur throughout the human body but it is mainly located on the extremities of the upper limbs. The second most affected region is the head and neck region in the order of 3.1–24% (Konwaller et al., 1955; Meister et al., 1978; Lu et al., 2015; Dahl and karlstedt, 1980) which in this case preferentially reaches the cervical region (53%) (Lu et al., 2015). Head and neck involvement appears to be more common in children (Hseu et al., 2015; Bemrich-Stolz et al., 2010; DiNardo et al., 1991). The NF affects men more frequently (1.4 men/1 woman) with an average age of 36 years (Lu et al., 2015). It has the characteristics of a rapidly growing lesion that can reach 2–3 cm in a few weeks and can reach up to 8 cm in total (Nakagawa et al., 1994; Kumar et al., 1997). The lesions size is smaller in the head and neck region with an average of 1 cm (Weinreb et al., 2009b). It can cause mild pain or tenderness or cause symptoms through mass effect. The lesion is usually mobile and well-circumscribed.
Radiologically, NF generally appears as a well-defined hypo or isoechoic lesion on ultrasound (Lu et al., 2015). Fine needle punctures led in several cases to a wrong diagnosis of pleomorphic adenoma (Mardi et al.,2005; Al-Rahbi et al., 2015; Jain et al., 2008). Computed tomography (CT) can show a heterogeneous lesion in case of cystic or mucoid transformation with sometimes even peripheral enhancement. Usually, the FN is rather homogeneous and seems hypo-or even isodense compared to the surrounding muscles (Wang et al., 2002; Chin et al., 2003). On MRI, nodular fasciitis appears homogeneous hypointense or isointense on T1, heterogeneous and iso- or even hyperintense on T2, with enhancement after administration of gadolinium in 40% of cases (Chin et al., 2003; Dinauer et al., 2007). Specific MRI signs such as the “fascia tail sign” or the “cloud sign” can help to make the diagnosis of nodular fasciitis in soft tissue tumors (Wu et al., 2020).
Some authors suggest that nodular fasciitis should be part of the differential diagnosis of head and neck masses found superficially and showing iconographic enhancement after injection, both on MRI and CT. This might be even more relevant if there exists a history of trauma and the lesion grows rapidly (Kim et al., 2005). In addition to rapid growth, bone erosion or destruction can be observed on imaging (which can make iconographic differential diagnosis complicated) (Chin et al., 2003). Some case reports also report hyper-metabolic activity of nodular fasciitis at Fluorodeoxyglucose Positron Emission Tomography (FDG-PET) (Kessels et al., 2004; Gotthardt et al., 2010; Seo et al., 2017).
The treatment of choice is surgical excision (Bernstein and Lattes, 1982). Recurrence is often linked to incomplete excision and is low, around 1–2%. It must also suggest another diagnosis. Some case reports report a good response to the injection of intralesional corticosteroids (Hseu et al., 2015; Graham, 1999; Nishi et al., 2006). Spontaneous regressions after biopsy or incomplete excision have also been described (Nishi et al., 2006; Dahl and. Nodularfasciitis, 1981). Lesions of the face for which the excision can leave unsightly scars can therefore possibly be treated non-surgically thanks to intralesional injections of corticosteroids, provided that there is histopathological certainty of the lesion (Oh et al., 2015).
Nodular fasciitis seems to be expressed in the external ear in approximately 1.5% of cases and is the culprit for 1.9% of external ear lesions (including malignant, benign or inflammatory lesions) according to a case series of 50 cases of external ear nodular fasciitis (50 out of 2930 auricular lesions) (Lu et al., 2015; Lester et al., 2001). At this location, they are usually smaller (average 1.9 cm) and recurrences are more frequent (9.3%) (Agarwal et al., 2013). Among nodular fasciitis of the outer ear, 12% are located in the external auditory canal (6 out of 50), making it a fairly rare region of presentation. In this case series of 50 cases of external ear nodular fasciitis, a wrong diagnosis was made in ¾ of the cases. It should be noted that 30% (9 cases out of 30) were wrongly considered as sarcomas after pathological analysis. This is why NF is also called “pseudosarcomatous fasciitis” because it has often been confused with a sarcomatous lesion due to its similar pathological characteristics (mitotic activity, cellularity and infiltration) associated with its clinical rapid growth. In these cases, a wrong diagnosis is likely to lead to more aggressive treatment with significant side effects. Therefore, it is imperative for physicians (clinicians and pathologists) to recognize nodular fasciitis presentation and characteristics.
To our knowledge, this case is the first presentation of nodular fasciitis as an inflammatory ear polyp with such extension (Table 1). Ear polyps can be due to inflammatory pathologies (infectious, cholesteatomatous, granulomatous) or neoplasms (benign or malignant) (Tay and Hussain, 1997). The infectious origin could be eliminated from negative bacteriological samples, a normal blood test (except a slight increase of the C-reactive protein) and the absence of purulent secretions. Moreover, the patient did not have predisposing conditions to malignant otitis externa such as diabetes or chronic renal failure. Polyps are associated with cholesteatomas in 25–45% of cases but these polyps usually arise from the attic or from posterosuperior marginal tympanic membrane defects. The absence of squamous epithelium with a granular cell layer or keratine on biopsies and the iconographic extension were not in favor of this type of pathologies. Benign tumors may also present with an ear polyp such as a jugular glomus tumor, middle ear adenoma, or facial nerve neuroma (Tay and Hussain, 1997). However, the data from the imaging performed on our patient did not point in this direction. The large size of the lesion and the associated osteolysis raised suspicion of an invasive and malignant lesion. Langheransian histiocytosis is an extensive osteolytic pathology that can cause an ear polyp. However, it usually occurs in young people and nearly half of the cases present bilateral involvement as well as pathological sites other than the temporal bone (Modest et al., 2016). The typical histological appearance showing multinucleated Langerhans cells, eosinophils and histiocytes was also not found on biopsies.
Table 1.
MEDLINE/Pubmed literature review of external ear canal nodular fasciitis.
| Age | Ear trauma | Exact localisation | size | symptoms | treatment | Time of follow-up | recurrence | |
|---|---|---|---|---|---|---|---|---|
| Abdel-Aziz et al. (2008): 6 cases | mean age of 7 years and 3 months | none | No information | 0.5–1.5 cm | - All cases: unilateral earache - 3 cases: bleeding associated with offensive discharge in two of them |
Complete surgical removal | One year | 2 cases: - In one case after two months - In one case after 4 months. No recurrence after second chirugical removal |
| Halsey et al. (2020): case report | 19 months | Increase of an ear lesion after trauma | Concho bowl with obstruction of the external auditory canal | 2.1 × 2.1 × 0.8 cm | Ulceration and bleeding | Complete surgical removal | No information | No recurrence |
| Ahn et al. (2016): case report | 19 years old | none | Posterior wall of the cartilaginous portion of the right external auditory canal | 1.7 cm | itching | Complete surgical removal | One year | No recurrence |
| Liu et al. (2021): case report | 17 months | No information | Cavity of the auricular concha | 1 cm | none | Complete surgical removal | One year | No recurrence |
| Milo et al. (1999): case report | 39 years old | No information | Lesion involving the left external auditory canal and middle ear cavity with extension inferiorly to the parotid gland, temporomandibular joint, masseter, and pterygoid muscles | No information | minimal pain and drainage | Complete surgical removal | 13 months | No recurrence |
| Lester et al. (2001): 6 cases of EAC nodular fasciitis among 50 cases of auricular nodular fasciitis | no detailed subgroup information | 3 out of 6 | no detailed subgroup information | 1.3 cm (mean size) | no detailed subgroup information | surgical removal (no detailed subgroup information) | From 0.4 to 29.0 years (median, 11.4 years) with no detailed subgroup information | Yes (1 out of 6) |
| Della Volpe et al. (2022): case report | 4 years old | none | Lesion involving the left tragus and the lateral portion of the external auditory canal | 1.7 × 2.1 × 2.4 cm | No symptoms at the first meeting | Complete surgical removal | One year | No recurrence |
| Wang et al. (2022): 1 case of EAC nodular fasciitis among 3 cases of auricular nodular fasciitis | 1year and 9 months | none | Left ear with no other information | 1.7 × 1.6 × 0.9 cm | Painless lesion with bleeding | Complete surgical removal | 8 months | No recurrence |
| Yver (2021): case report | 49 years old | No information | Left concha bowl | 2 × 1.5 cm | No information | Complete surgical removal | No information | No recurrence |
| Cobanoglu et al. (2010) : case report | 8 years old | Yes, 3 weeks earlier | Cartilaginous part of the inferior canal wall of the left external auditory canal | 1.7 × 1.0 × 1 cm | No information | Excisional biopsy with positive surgical margins | 7 months | The lesion recurred within a month, no recurrence 7 months after a total excision. |
Malignant tumors of the external auditory canal or middle ear are rare. Squamous cell carcinomas are the most common followed by adenoid cystic carcinomas and basal cell carcinomas. A malignant ear polyp might be either a primary lesion or the result of the extension of adjacent tumor sites like the parotide, the temporomandibular joint, the infratemporal fossa, nasopharyngeal, the pre ou retroauricular region. Malignant melanoma, squamous cell carcinoma, adenocarcinoma, cystic adenoid carcinoma and soft tissue sarcomas of the ear and temporal bone might present with ear polpys. Anatomopathology analysis-clarification was needed and as previously mentioned, differentiating NF from sarcomas might be a difficult task for the contributing pathologist. Soft tissue sarcomas of the ear are more common in children and approximately 50% of these patients have neurological signs at the time of diagnosis (Kuhel et al., 1996). Despite the significant iconographic extension our patient showed no cranial nerve impairment.
In the majority of cases, ear polyps are simple benign inflammatory polyps (Agarwal et al., 2013). External auditory canal lesions are usually small and localized, so diagnosis is often delayed. An effective biopsy is also a challenge, leading in many cases to inadequate biopsies which are too superficial or scattered. Therefore, it is recommended to proceed to a biopsy and/or wide local excision with a rim of healthy tissue. Repetition of the procedure is suggested in the case of unfavourable evolution or doubtful and/or non-contributory histopathological results.
Declaration of competing interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Footnotes
Peer review under responsibility of PLA General Hospital Department of Otolaryngology Head and Neck Surgery.
Contributor Information
Adrien Philippart, Email: adrien.philippart@student.uclouvain.be.
Jean-Christophe Degols, Email: jean-christophe.degols@cspo.be.
Jacques Vilain, Email: jacques.vilain@cspo.be.
References
- Abdel-Aziz Mosaad, Khattab Hany, El-bosraty Hussam, et al. Nodular fasciitis of the external auditory canal in six Egyptian children. Int. J. Pediatr. Otorhinolaryngol. 2008;72 doi: 10.1016/j.ijporl.2008.01.023. 643—646. [DOI] [PubMed] [Google Scholar]
- Agarwal N.M., Popat V.C., Traviad C., Srivastava A. Clinical and histopathological study of mass in ear: a study of fifty cases. Indian J. Otolaryngol. Head Neck Surg. 2013;65(Suppl. 3):520–525. doi: 10.1007/s12070-011-0434-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahn Jihyun, Kim Sunyoung, Park Youngsil. Nodular fasciitis of external auditory canal. J. Pathol. Translat. Med. 2016;50:394–396. doi: 10.4132/jptm.2016.03.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Rahbi Mohammed, Al-Kindi Hunaina, Al-Sheiban Salma. Post-aural Nodular Fasciitis Oman Med. J. 2015;30(No. 1):63–65. doi: 10.5001/omj.2015.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bemrich-Stolz C.J., Kelly D.R., Muensterer O.J., Pressey J.G. Single institution series of nodular fasciitis in children. J. Pediatr. Hematol. Oncol. 2010;32(5):354–357. doi: 10.1097/MPH.0b013e3181df6305. [DOI] [PubMed] [Google Scholar]
- Bernstein K.E., Lattes R. Nodular (pseudosarcomatous) fasciitis, a non recurrent lesion: clinicopathologic study of 134 cases. Cancer. 1982;49 doi: 10.1002/1097-0142(19820415)49:8<1668:aid-cncr2820490823>3.0.co;2-9. 1668—1678. [DOI] [PubMed] [Google Scholar]
- Chen J., Ye X., Li Y., Wei C., Zhang Q., Zhong P., et al. Chromosomal translocation involving USP6 gene in nodular fasciitis. Zhonghua Bing Li Xue Za Zhi. 2014;43:533–536. [PubMed] [Google Scholar]
- Chin J.H., Lee H.K., Cho K.-J., Han M.H., Na D.G., Choi C.G., et al. Nodular fasciitis of the head and neck: radiographic findings. Clin. Imag. 2003;27(1):31–37. doi: 10.1016/s0899-7071(02)00506-5. [DOI] [PubMed] [Google Scholar]
- Cobanoglu U., Caylan R., Ersoz S. Nodular fasciitis of the external auditory canal. B-ENT. 2010;6(2):131–133. PMID: 20681367. [PubMed] [Google Scholar]
- Dahl I., karlstedt J. Nodular fasciitis in the head and neck. A clinico-pathological study of 18 cases. Acta Otolaryngol. 1980;90:152–159. doi: 10.3109/00016488009131711. [DOI] [PubMed] [Google Scholar]
- Dahl I., Nodularfasciitis M.Akerman. A correlative cytologic and histologic study of 13 cases. Acta Cytol. 1981;25:215–223. [PubMed] [Google Scholar]
- Della Volpe A., Festa P., Varricchio A.M., Russo C., Covelli E.M., Bifano D., Piroli P., De Lucia A., Di Stadio A., Ionna F. Diagnosis and treatment of nodular fasciitis of ear region in children: a case report and review of literature. Healthcare (Basel) 2022;10(10):1962. doi: 10.3390/healthcare10101962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiNardo L.J., Wetmore R.F., Potsic W.P. Nodular fasciitis of the head and neck in children: a deceptive lesion. Arch. Otolaryngol. Head Neck Surg. 1991;117(9):1001–1002. doi: 10.1001/archotol.1991.01870210073013. [DOI] [PubMed] [Google Scholar]
- Dinauer P.A., Brixey C.J., Moncur J.T., Fanburg-Smith J.C., Murphey M.D. Pathologic and MR imaging features of benign fibrous soft-tissue tumors in adults. Radiographics. 2007;27:173–187. doi: 10.1148/rg.271065065. [DOI] [PubMed] [Google Scholar]
- Erickson-Johnson M.R., Chou M.M., Evers B.R., et al. Nodular fasciitis: a novel model of transient neoplasia induced by MYH9-USP6 gene fusion. Lab. Invest. 2011;91(10):1427–1433. doi: 10.1038/labinvest.2011.118. [DOI] [PubMed] [Google Scholar]
- Gotthardt M., Arens A., van der Heijden E., de Geus-Oei L.F., Oyen W.J. Nodular fasciitis on F-18 FDG PET. Clin. Nucl. Med. 2010;35(10):830–831. doi: 10.1097/RLU.0b013e3181ef0b6c. [DOI] [PubMed] [Google Scholar]
- Graham Brad S. Nodular fasciitis: response to intralesional corticosteroids. J. Am. Acad. Dermatol. 1999;40:490–492. doi: 10.1016/s0190-9622(99)70506-2. [DOI] [PubMed] [Google Scholar]
- Halsey J.N., Hohenleitner J., Ciminello F.S. Nodular fasciitis—a rare cause of a rapidly growing ear lesion in a 19-month-old child. Eplasty. 2020;20:ic13. Oct 19. [PMC free article] [PubMed] [Google Scholar]
- Hseu Anne, Watters Karen, Perez-Atayde Antonio, et al. Pediatric nodular fasciitis in the head and neck evaluation and management. JAMA Otolaryngol.–Head & Neck Surg. 2015;141(1):54–59. doi: 10.1001/jamaoto.2014.2797. [DOI] [PubMed] [Google Scholar]
- Jain D., Khurana N., Jain S. Nodular fasciitis of the external ear masquerading as pleomorphic adenoma: a potential diagnostic pitfall in fine needle aspiration cytology. CytoJournal. 2008;5:14. doi: 10.4103/1742-6413.44242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessels L.W., Simsek S., Van Hattum A.H., Stam F., Comans E.F. Nodular fasciitis: an unexpected finding on computed tomography and positron emission tomography. Eur. J. Intern. Med. 2004;15(3):183–185. doi: 10.1016/j.ejim.2004.03.001. https://doi:10.1016/j.ejim.2004.03.001 Jun. [DOI] [PubMed] [Google Scholar]
- Kim S.T., Kim H.J., Park S.W., Baek C.H., Byun H.S., Kim Y.M. Nodular fasciitis in the head and neck: CT and MR imaging findings. AJNR Am. J. Neuroradiol. 2005;26(10):2617–2623. Nov- Dec. [PMC free article] [PubMed] [Google Scholar]
- Konwaller B.E., Keasbey L.E., Kaplan L. Subcutaneous pseudosarcomatous fibromatosis (fasciitis): report of 8 cases. Am. J. Clin. Pathol. 1955;25:241–252. doi: 10.1093/ajcp/25.3.241. [DOI] [PubMed] [Google Scholar]
- Kuhel W.I., Hume C.R., Selesnick S.H. Cancer of the external auditory canal and temporal bone. Otolaryngol. Clin. 1996;29(5):827–852. [PubMed] [Google Scholar]
- Kumar V., Corton R., Robbins S.L. sixth ed. Saunders; Philadelphia, Pennsylvania: 1997. Basic Pathology. [Google Scholar]
- Lester D.R., Thompson Julie, Fanburg-Smith C., Wenig Bruce M. Nodular fasciitis of the external ear region: a clinicopathologic study of 50 cases. Ann. Diagn. Pathol. 2001;5(No 4):191–198 191. doi: 10.1053/adpa.2001.26969. August. [DOI] [PubMed] [Google Scholar]
- Liu X., Li X. Nodular fasciitis in the cavity of auricular concha: a case report. Ear. Nose & Throat J. 2021 doi: 10.1177/01455613211006006. 0(0) [DOI] [PubMed] [Google Scholar]
- Lu Linhui, Lao Weng I., Liu Xiaohang, et al. Nodular fasciitis: a retrospective study of 272 cases from China with clinicopathologic and radiologic correlation. Ann. Diagn. Pathol. 2015;19:180–185. doi: 10.1016/j.anndiagpath.2015.03.013. [DOI] [PubMed] [Google Scholar]
- Mardi K., Sharma J., Kaur H. Nodular fasciitis of the hand - a potential diagnostic pitfall in fine needle aspiration cytology. J. Cytol. 2005 doi: 10.1309/PWD0-HB51-1L3V-R56W. https://www.jcytol.org/text.asp?2007/24/4/197/41895 [serial online] 2007 [cited 2023 Jan 5]; 24:197-8. Available from: [DOI] [PubMed] [Google Scholar]
- Meister P., Bückmann F.W., Konrad E. Nodular fasciitis (analysis of 100 cases and review of the literature) Pathol. Res. Pract. 1978;162:133–165. doi: 10.1016/S0344-0338(78)80001-6. [DOI] [PubMed] [Google Scholar]
- Milo A.G.C., Vito K.J., Kinney S.E., Bauer T.W. Nodular fasciitis arising in the external auditory canal. Otolaryngology-Head Neck Surg. (Tokyo) 1999;120(4):591–592. doi: 10.1053/hn.1999.v120.a85073. [DOI] [PubMed] [Google Scholar]
- Modest M.C., Garcia J.J., Arndt C.S., Carlson M.L. Langerhans cell histiocytosis of the temporal bone: a review of 29 cases at a single center. Laryngoscope. 2016;126(8):1899–1904. doi: 10.1002/lary.25773. https://doi:10.1002/lary.25773 [DOI] [PubMed] [Google Scholar]
- Nakagawa T., Sugimoto T., Komiyama S., Yamamoto T., Uemura T. Giant tumor formed by nodular fasciitis of the pharynx: a case report. Auris Nasus Larynx. 1994;21:196–199. doi: 10.1016/s0385-8146(12)80145-3. [DOI] [PubMed] [Google Scholar]
- Nishi S.P., Brey N.V., Sanchez R.L. Dermal nodular fasciitis: three case reports of the head and neck and literature review. J. Cutan. Pathol. 2006;33(5):378–382. doi: 10.1111/j.0303-6987.2006.00437.x. https://doi:10.1111/j.0303-6987.2006.00437.x May. [DOI] [PubMed] [Google Scholar]
- Oh B.H., Kim J., Zheng Z., Roh M.R., Chung K.Y. Treatment of nodular fasciitis occurring on the face. Ann. Dermatol. 2015;27(6):694–701. doi: 10.5021/ad.2015.27.6.694. https://doi:10.5021/ad.2015.27.6.694 Dec. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seo M., Kim M., Kim E.S., Sim H., Jun S., Park S.H. Diagnostic clue of nodular fasciitis mimicking metastasis in papillary thyroid cancer, mismatching findings on 18F-FDG PET/CT and 123I whole body scan: a case report. Oncol. Lett. 2017;14(1):1167–1171. doi: 10.3892/ol.2017.6181. Jul. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tay H.L., Hussain S.S.M. Review Article the management of aural polyps. J. Laryngol. Otol.March. 1997;111(3):212–214. doi: 10.1017/s002221510013693x. Mar. [DOI] [PubMed] [Google Scholar]
- Wang X.L., De Schepper A.M., Vanhoenacker F., De Raeve H., Gielen J., Aparisi F., et al. Nodular fasciitis: correlation of MRI findings and histopathology. Skeletal Radiol. 2002;31:155–161. doi: 10.1007/s00256-001-0462-z. [DOI] [PubMed] [Google Scholar]
- Wang X., Liu W., He L., Chen M., Shao J., Zhang X., Ma N., Li Y., Zhang J. Clinical characteristics of nodular fasciitis of the ear in children. Eur. J. Pediatr. 2022;181:833–840. doi: 10.1007/s00431-021-04274-x. [DOI] [PubMed] [Google Scholar]
- Weinreb I., Shaw A.J., Perez-Ordoñez B., Goldblum J.R., Rubin B.P. Nodular fasciitis of the head and neck region: a clinicopathologic description in a series of 30 cases. J. Cutan. Pathol. 2009;36(11):1168–1173. doi: 10.1111/j.1600-0560.2009.01252.x. Nov. [DOI] [PubMed] [Google Scholar]
- Weinreb I., Shaw A.J., Perez-Ordoñez B., Goldblum J.R., Rubin B.P. Nodular fasciitis of the head and neck region: a clinicopathologic description in a series of 30 cases. J. Cutan. Pathol. 2009;36(11):1168–1173. doi: 10.1111/j.1600-0560.2009.01252.x. Nov. [DOI] [PubMed] [Google Scholar]
- Wu S.Y., Zhao J., Chen H.Y., Hu M.M., Zheng Y.Y., Min J.K., Yu R.S. MR imaging features and a redefinition of the classification system for nodular fasciitis. Medicine. 2020;99(45) doi: 10.1097/MD.0000000000022906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yver Christina M., Husson A.M., Friedman O. Pathology Clinic: Nodular Fasciitis Involving the External Ear. Nose & Throat J. 2021:1–3. doi: 10.1177/01455613211001958. [DOI] [PubMed] [Google Scholar]