Abstract
Several technical variations of tympanoplasty have been reported, usually involving the type of graft and/or instruments used. Few studies have focused on the outcome of type-1 tympanoplasty specifically in teaching scenarios. We aimed to describe the results of type-1 tympanoplasty performed by residents, and to investigate potential predictive factors of surgical success. To do so, we did a retrospective analysis of medical records of patients who underwent type-1 tympanoplasty in a tertiary university hospital. We evaluated the tympanic membrane closure and audiometric outcomes during the first year of follow-up, and compared the results according to some clinical and surgical factors. 130 operated ears were included in the study. The closure rate reached 84.12% after one month and 72.72% after twelve months of surgery. The mean air-bone gap was 22.98 dB preoperatively, and reached 10.55 dB after surgery. Perforation closure rates were 85% and 57.14% for those operated by endoscopic and microscopic-assisted approaches, respectively (p = 0.004). The use of cartilage grafts and time without otorrhea of more than three months prior to surgery were also predictors of surgical success (p = 0.002 and 0.041, respectively). Gender, age, perforation size, contralateral disease, operated side, reoperation, and degree of hearing loss did not significantly interfere with outcomes. Tympanoplasty showed good overall results when performed by residents, although inferior to those reported by experienced surgeons. The use of the endoscope, cartilage grafting, and longer preoperative time without otorrhea were predictors of surgical success in this scenario.
Level of evidence
IIB.
Keywords: Tympanoplasty, Treatment outcome, Video-assisted surgery
Highlights
-
•
One-year closure rate after tympanoplasty performed by residents reached 72.72%.
-
•
An air-conduction pure-tone average improvement of around 10 dB was observed.
-
•
Closure rate was significantly higher in endoscopic-assisted technique.
-
•
Time without otorrhea prior to surgery was associated with better outcomes.
1. Introduction
Chronic otitis media (COM) is a frequent health problem, particularly in developing countries (Indorewala et al., 2015; Murari and Ajay, 2018). It could be broadly defined as the persistent inflammatory process within the middle ear cleft which leads to irreversible tissue changes such as perforations of the tympanic membrane (TM). Hearing loss, recurrent infections and chronic or relapsing otorrhea might also occur, with significant socio-economic burden (Indorewala et al., 2015; Murari and Ajay, 2018). Surgical repair of TM perforation through tympanoplasty is one of the most performed ear procedures, and it is employed for the treatment of stable, non-suppurative COM. The goals of tympanoplasty include prevention of recurrent otorrhea, reconstruction of the TM and hearing improvement (Indorewala et al., 2015; Murari and Ajay, 2018; Doh et al., 2019).
There are many technical variations of tympanoplasty, usually involving the type of graft and/or instruments used. In type-1 tympanoplasty, the TM repair is carried out after elevation of a tympanomeatal flap, but without manipulating the ossicular chain. As for the type of instruments used, microscopic-assisted (MAT) and endoscopic-assisted (EAT) techniques have shown satisfactory and comparable surgical results (Murari and Ajay, 2018; Doh et al., 2019; Choi et al., 2017; Bayraktar, 2017; Huang et al., 2016; Tseng et al., 2018a, 2018b). Although traditionally used during ear surgery training (Fukuchi et al., 2006), MAT has gradually being replaced by EAT in many services – as the use of endoscopes steadily grows across Otolaryngology (Gokgoz et al., 2019). However, few studies explored the results from type-1 tympanoplasty and compared the outcomes of MAT and EAT specifically when the procedure is performed by residents.
Furthermore, several investigations have already focused on the factors that could impact success rates of tympanoplasty (Dursun et al., 2020; Dhanapala et al., 2019; Lee et al., 2011; Pinar et al., 2008). However, most of them included only MAT in their analyses. Yet, they did not comprehend the results from performed by trainees.
This study aims to describe the results of type-1 tympanoplasty performed by residents in a tertiary university hospital, and to investigate potential predictive factors of surgical success.
2. Materials and methods
This is a retrospective study conducted at an Otology outpatient clinic of a university tertiary teaching hospital (Complexo Hospital de Clínicas, Universidade Federal do Paraná) in Curitiba, Brazil, between 2018 and 2021. The study was approved by the Institution Ethics and Research Committee (Certificate number: 31738620.7.0000.0096).
2.1. Patients
Medical records of patients who underwent type-1 tympanoplasty performed by training residents between 2018 and 2020 were analyzed. Inclusion criteria were: patients older than 8 years who underwent type-1 tympanoplasty using the underlay grafting technique; patients who underwent surgery performed by residents; patients with available preoperative audiometry and; patients with at least 30 days of follow-up. Accordingly, surgeries with any intraoperative need for ossicular chain manipulation, expanded approaches (eg, atticotomy), or use of alternative surgical techniques (myringoplasty) (Eavey, 1998), were not included in the study.
2.2. Surgical procedure
All procedures were performed under general anesthesia by second- and third-year Otolaryngology residents, and with the supervision of experienced otologists. Those included in the study were submitted to type-1 tympanoplasty either with MAT and a retroauricular approach, or with EAT and a transcanal approach (Wullstein, 1956). The choice between MAT and EAT did not rely on any specific criteria, such as the physician's preference or a particular clinical feature. Instead, the surgeries were carried out following an institutional waiting list and the patients were submitted to EAT or MAT according to the day of the week their procedure was scheduled. Depending on the day, either the microscope or the endoscope apparatus were available in the operating room. A 14 cm long 0° 4 mm rigid endoscope or an operating microscope were used in EAT and MAT, respectively. In Brazil, particularly in university tertiary hospitals, computed tomography (CT) scans are not performed prior to every ear surgery. For example, typical cases of stable uncomplicated tympanic membrane perforations, otosclerosis, or otitis media with effusion are often treated without the need of radiological evaluation. Due to financial and logistic reasons, CT scans are usually reserved for more-advanced cases of chronic otitis media, or whenever there remains any clinical doubt in atypical presentations of ear diseases. Hence, only a few of the patients included in the study had CT scans, preventing us from using the radiological data in our study.
Both techniques used underlay placement of the graft after elevation of an anterior-based tympanomeatal flap. In MAT, temporal fascia was the most used material, whereas cartilage, with or without perichondrium, was the preferred one in EAT. For both techniques, the surgeon freshened the edges of the TM remnant before elevating the flap. Then, the graft was placed medial to the TM remnant, and the flap was re-positioned back down over the graft.
2.3. Follow-up
Postoperative visits were scheduled after 1, 3, 6 and 12 months of the surgery. Data regarding perforation closure, presence or absence of complications, and pre- and postoperative audiometric results were obtained for each patient during each attended visit.
Postoperative pure-tone audiometry was performed at least 3 months after the procedure. For both pre- and postoperative audiological investigations, air-conduction thresholds were obtained at 0.5, 1, 2, 3, 4 and 6 KHz. The average pure-tone air-conduction threshold (PTA) was recorded as the mean value obtained at 0.5, 1 and 2 KHz. In addition, the mean air-bone gap (ABG) was obtained by calculated by averaging the intervals between air- and bone-conduction thresholds at .5, 1, 2, 3 and 4 KHz.
2.4. Success rate and prognostic factors
Tympanic membrane closure was considered as the primary outcome of surgical success. The secondary outcomes were the quantitative improvements in PTA and ABG after 3 months or more of surgery.
The rate of tympanic membrane closure of the overall sample was determined at 1, 3, 6, and 12 months postoperatively. For each time point, data from patients who lost follow-up were not included. The success rate was defined as the ratio between patients with intact neotympanum and the number of individuals followed up until the reference period. In order to account for the possible effect of loss of follow-up on closure rates, the rate of surgical failure was also calculated, herein defined as the ratio between patients with confirmed residual perforations and the overall sample.
To study predictors of primary surgical outcomes without the deleterious effects of the mounting rates of loss of follow-up, data from patients at the 6-months visit were used. Information on the following possible prognostic factors were obtained: age, perforation size, time without otorrhea prior to surgery, involvement of the contralateral ear, reoperation, preoperative audiometric mean variables and type of graft used. Then, the comparison of the outcomes between patients grouped according to each of these parameters was made.
2.5. Data collection and analysis
The data were collected and tabulated in an Excel® spreadsheet and received the appropriate statistical treatments for analysis, using the R Software (version 4.1.2). The significance level was set at 0.05.
3. Results
Data from 117 patients, including 147 surgical procedures, were scrutinized. One hundred and thirty ears met the study criteria and had their data collected and analyzed. Among those excluded, five were submitted to myringoplasty, eight underwent ossicular chain reconstruction, seven had the intraoperative diagnosis of cholesteatoma, and three lost follow-up within the first month after surgery.
The sample had a mean age of 36.26 years, ranging from 10 to 78 years, and 73 (56.15%) ears were from women.
The overall rate of complications was 3.07%. One patient had a hematoma in the immediate postoperative period, requiring surgical drainage; two had incisional seroma, which disappeared with follow-up; one reported a transient metallic taste sensation and; two reported significant postoperative hearing loss, which was temporary according to follow-up visits.
3.1. Success rate
After the first month, a closure rate of 84.12% was obtained. This rate dropped in the third and sixth months to 74.54% and 69.66%, respectively. Meanwhile, surgical failure increased to 22.22% in the 3-month follow-up visit, remained stable in the 6-month visit, and finally dropped at the end of the 1-year follow-up to 14.28%. Twelve months after surgery, 72.72% of the surgeries were successful. The loss of follow-up increased considerably with time and, at our final study endpoint, 64 patients (49.23%) could not have their data retrieved. Data from primary outcomes and loss of follow-up are shown in Fig. 1.
Fig. 1.
Primary surgical outcomes and absolute number of dropouts, according to postoperative time point.
Source: the author
Sixty-one patients had their pre- and postoperative audiometric data available for evaluation. One patient was excluded for inconsistent responses during audiometry. The preoperative and postoperative mean PTA was 40 dB and 29.8 dB, respectively. Among those (n:44) with anatomical surgical success, the mean preoperative PTA was 39.8 dB. It decreased to 25.7 dB postoperatively (13.59 dB gain). For those with residual perforations (n:17), mean pre- and postoperative PTA were 40.39 and 38.9 dB, respectively (1.47 dB gain). The difference between the audiometric gain obtained for these groups was statistically significant (p = 0.00034, Mann-Whitney Test, Fig. 2).
Fig. 2.
PTA variation after surgery according to primary surgical outcome.
Legend: PTA: pure-tone average; TM: tympanic membrane; dB:decibels Source: the Author.
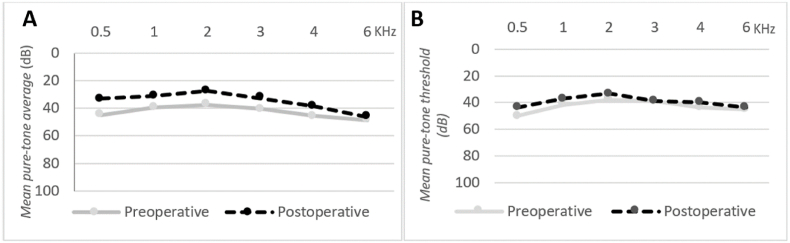
The mean ABG was 22.98 dB preoperatively, and reached 10.55 dB after surgery. Although the mean decrease in ABG was greater in the group of patients with complete perforation closure (13.32 dB versus 9.11 dB), it did not reach statistical significance (p = 0.099, Mann-Whitney Test). Fig. 3 depicts the frequency-specific air-conduction threshold means of the pre- and postoperative audiological evaluation of the patients according to their primary surgery outcome.
Fig. 3.
Frequency-specific air-conduction threshold means of the pre- and postoperative audiological evaluation of the patients according to their primary surgery outcome. A: Group with complete tympanic membrane closure. B: Group with residual perforations.
Legend: dB: decibels; KHz: Kilohertz. Source: the Author.
3.2. Prognostic factors
89 patients attended the 6-month appointment and had their data on possible predictors of tympanic closure collected (Table 1). Among the categorical variables, time without otorrhea prior to surgery longer than three months (p = 0.041), EAT (p = 0.004) and use of cartilage grafting (p = 0.002) were predictors of better primary surgical outcomes.
Table 1.
Effect of preoperative variables on the primary surgical outcome.
| Variable | Number of ears with closed tympanic membrane (%) | Number of ears with residual perforation (%) | p-value |
|---|---|---|---|
| Age | |||
| ≤18 years | 14 (70%) | 6 (30%) | 0.970 (Chi-Square) |
| >18 years | 48 (69.56%) | 21 (30.44%) | |
| Gender | |||
| Female | 31 (62%) | 19 (38%) | 0.750 (Chi-Square) |
| Male | 31 (79.48%) | 8 (20.52%) | |
| Perforation size | |||
| Small (<25%) | 11 (84.61%) | 2 (15.38%) | |
| Moderate (25–75%) | 19 (76%) | 6 (24%) | 0.298 (Fisher's exact test) |
| Large (>75%) | 29 (64.4%) | 16 (35.6%) | |
| Time without otorrhea | |||
| ≤3 months | 8 (50%) | 8 (50%) | 0.041∗ (Chi-Square) |
| >3 months | 53 (75.71%) | 17 (24.28%) | |
| Contralateral ear disease | |||
| Yes | 32 (71.1%) | 13 (28.9%) | 0.764 (Chi-Square) |
| No | 30 (68.18%) | 14 (31.81%) | |
| Operated side | |||
| Right | 32 (65.3%) | 17 (34.7%) | 0.322 (Chi-Square) |
| Left | 30 (75%) | 10 (25%) | |
| Reoperation | |||
| Yes | 9 (75%) | 3 (25%) | 1 (Fisher's exact test) |
| No | 53 (68.8%) | 24 (31.2%) | |
| Technique | |||
| EAT | 34 (85%) | 6 (15%) | 0.004∗ (Chi-Square) |
| MAT | 28 (57.14%) | 21 (42.86%) | |
| Type of graft | |||
| Temporal fascia | 28 (57.14%) | 21 (42.86%) | 0.002∗ (Fisher's exact test) |
| Cartilage with or without perichondrium | 32 (88.88%) | 4 (11.12%) | |
Mean preoperative PTA and ABG were 40.6 and 23.06 dB, respectively, among individuals with tympanic membrane closure, and 39.69 and 25.81 dB, respectively, among those with residual perforation at the 6-month visit. Neither of these variables showed significant difference according to the surgical primary outcome (p > 0.05, Mann-Whitney Test).
4. Discussion
Success rates of type-1 tympanoplasty vary from 35 to as high as 95%. This wide range of results might be a consequence of a general lack of standardization in sample selection and success criteria, and a high heterogeneity in postoperative follow-up (Dangol and Shrivastav, 2017). Therefore, the results herein reported should be considered according to the scenario of the study. Studies carried out in university teaching hospitals tend to present poorer results (Fermi et al., 2021). In line with current evidence, the overall results in this study mirror the learning environment and complexity of a tertiary teaching hospital (Sirena et al., 2010; Salvador et al., 2021). In this perspective, the surgical outcomes described were satisfactory. However, it should be outlined that these results are clearly worse than those obtained and reported when the surgeries are performed by experienced surgeons and in private practice (Dangol and Shrivastav, 2017). Understanding the learning curve of ear surgery is crucial in otology. Nonetheless, robust evidence on the learning progress of tympanoplasty is still lacking, and this study might contribute to shed light into this important issue.
As it was noticed in this study, high dropout rates have been reported in similar investigations. After type-1 tympanoplasty, they might be explained at a large extent by subjective clinical improvement. Furthermore, the SARS-CoV-2 pandemic might have contributed at some level for loss of follow up. Finally, socioeconomic inequalities often hinder patients from public health systems in developing countries to attend medical appointments. Determining success rates only among those who completed the follow-up might overlook results from the individuals with the best postoperative performance, as these patients are more likely to feel well to drop out (Jalali et al., 2017). To avoid underestimate surgical outcomes, this study also calculated “failure rates”, which comprised the ratio between those with confirmed residual perforations during follow-up and the whole sample. With these complementary analyses, after one-year follow-up, 72.72% of the individuals had their TM perforations closed, whereas 14.28% presented definite surgical failure.
A large meta-analysis showed lower but non-significant decrease in the surgical success rate with time. At the 12-month visit, 85.61% of patients presented good outcomes (Tan et al., 2016). Another work has shown significant poorer graft take rate among patients whose procedures were performed by trainees, when compared to those operated by experienced surgeons. Yet, one year after surgery, 86.2% of patients submitted to type-1 tympanoplasty performed by in-training surgeons had their TM perforations closed (Emir et al., 2007).
As for the audiometric data, we observed a significant improvement in air-conduction mean thresholds among patients with good primary outcomes, as also reported previously in the literature (Sirena et al., 2010; Salvador et al., 2021). Even among those with residual perforation, postoperative investigation could show some audiological benefit. Importantly, in this study, there was no report of permanent hearing impairment following type-1 tympanoplasty.
Since the 1950s, MAT has been the standard type of procedure for TM repair, with reported success rates as high as 93–100% (Doh et al., 2019; Tseng et al., 2017, 2018b). EAT emerged in the late 90s, and it has shown to be a safe and effective alternative to the use of microscopes (Murari and Ajay, 2018; Tseng et al., 2018b; Pinar et al., 2008). Indeed, recent meta-analysis and systematic reviews have demonstrated comparable satisfactory outcomes for both techniques (Murari and Ajay, 2018; Doh et al., 2019; Choi et al., 2017; Bayraktar, 2017; Huang et al., 2016; Tseng et al., 2018b; Santos et al., 2016). In this work, significantly better primary surgical outcomes were observed for EAT compared to MAT. One could postulate that there might have been an uncontrolled selection bias that could have gone unnoticed during data collection and analysis. However, we highlight that the patients were allocated to EAT or MAT in a near-random fashion, following an institutional waiting list. Hence, one could also claim that better outcomes could effectively result from a faster learning curve with EAT, as endoscopes have been increasingly used during Otolaryngology residency training. Also, some theoretical advantages of EAT might bring some positive impact on surgical results particularly in training scenarios. These include the quality of the images provided by the devices, which improves orientation and anatomical teaching in otology (Bazilio and Neto, 2021). Finally, the difference in the type of graft most commonly used in transcanal EAT and retroauricular MAT should be considered, as it acts as a confounding factor.
Cartilage grafts, used in this study preferably in EAT, could show better take rates than fascia grafts. It might occur for example due to the greater stability of cartilage when facing negative pressure changes within the tympanic cleft. A systematic review performed by Jalali et al. demonstrated a cartilage graft take rate significantly superior of that of fascia grafts (Jalali et al., 2017). Following this reasoning, some authors argue in favor of the use of cartilage in cases of high-risk TM perforations (Tan et al., 2016; Salviz et al., 2015; Tympanoplasty and Prognóstico, 2021).
A prospective study described smoking, tympanosclerosis and larger membrane perforation as independent prognostic factors for failure in tympanoplasty (Salvador et al., 2021). Here, the size of the perforation was not significantly determinant for TM closure, as replicated by another study (Tan et al., 2016). The involvement of the contralateral ear is frequently reported as a factor related to unfavorable prognosis in tympanoplasty (Salvador et al., 2021; Salviz et al., 2015; Hardman et al., 2015). This study could not demonstrate similar findings, which was also the case in recent studies carried out in a teaching hospital (Tan et al., 2016) and using EAT (Fukuchi et al., 2006).
Fifty percent of patients who had otorrhea three months or less before surgery experienced surgical failure in this series. Hence, it emerged here as a critical factor for surgical prognosis. Indeed, several authors advise awaiting a minimum interval of three months without otorrhea to perform tympanoplasty (Lee et al., 2011; Emir et al., 2007). The literature does not report significant difference between primary and revision type-1 tympanoplasty in terms of TM closure, as it was also noticed in our study (Salvador et al., 2021).
Young age has been traditionally associated with poorer outcomes in tympanoplasty (Tan et al., 2016; Salviz et al., 2015). However, most recent data have suggested that age should not be considered a significant independent factor for closure rate, as we have also observed (Salvador et al., 2021; Jalali et al., 2017; Hardman et al., 2015).
This work has some limitations, mostly due to its retrospective nature. First, it is clearly vulnerable to missing data and biased evaluation and follow-up. In addition, one should bear in mind the effect of the loss of follow-up while examining the results. Furthermore, postoperative audiological tests were performed at different time points across the sample population, partially limiting their comparability. As a large share of the overall sample did not attend the one-year follow-up, the authors chose to use audiological information collected after three months of surgery, at any time until one-year after the procedure or until dropout. Thus, in this study, the absence of a prospective design had a particular impact on the comparability of audiometric information, as there was a broad time window in which the test could have been performed. To investigate the prognostic factors for tympanic closure, the authors also had to choose the 6-month time point to avoid the impact of the steep rise on the loss of available data seen at the one-year evaluation. Finally, the lack of routine radiological evaluation should be mentioned, as the use of CT scan information might have provided useful complementary data on the grade of each patient's disease. Besides, CT scans yield objective parameters, such as mastoid pneumatization, which could play significant roles in the prognosis of ear surgeries. Hence, future prospective studies with larger samples and broader preoperative assessments are highly recommended to confirm and further elaborate the results herein presented.
5. Conclusion
In this study, surgery for TM repair performed by residents in a university teaching scenario showed complete closure of the tympanic perforation in 72.72% of cases after one year, also with significant improvement in audiometric parameters. An increasing dropout rate was observed during follow-up. Of those operated, 14.28% showed definite surgical failure at the study endpoint. Endoscopic-assisted technique, the use of cartilage graft, and time without otorrhea of more than three months prior to surgery were predictors of better outcomes.
Footnotes
Peer review under responsibility of PLA General Hospital Department of Otolaryngology Head and Neck Surgery.
References
- Bayraktar C. Endoscopic tympanoplasty : learning curve for a surgeon already trained in microscopic tympanoplasty. Published online. 2017:1853–1858. doi: 10.1007/s00405-016-4428-0. [DOI] [PubMed] [Google Scholar]
- Bazilio F., Neto N. em hospital universitário ଝ. 2021;87(4):434–439. [Google Scholar]
- Choi N., Noh Y., Park W., et al. vol. 10. 2017. pp. 44–49. (Comparison of Endoscopic Tympanoplasty to Microscopic Tympanoplasty). 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dangol K., Shrivastav R.P. Study of various prognostic factors affecting successful myringoplasty in a tertiary care centre. Int. Arch. Otorhinolaryngol. 2017;21(3):250–254. doi: 10.1055/s-0036-1593818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhanapala N., Hussain S.M., Reddy L.S., Bandadka R. 2019. Comparative Study of Clinical and Audiological Outcome between Anterior Tucking and Circumferential Flap Methods of Type I Tympanoplasty in Large Central Perforation; pp. 190–193. Published online. [DOI] [Google Scholar]
- Doh S.L., Lee Y., Seo Y., Ho Y. Can endoscopic tympanoplasty Be a good alternative to microscopic tympanoplasty. A Syst. Rev.Meta-Anal. 2019;12(2):145–155. doi: 10.21053/ceo.2018.01277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dursun E., Terzi S., Demir E., et al. The evaluation of prognostic factors in endoscopic cartilage tympanoplasty. Eur. Arch. Oto-Rhino-Laryngol. 2020;277(10):2687–2691. doi: 10.1007/s00405-020-05992-y. [DOI] [PubMed] [Google Scholar]
- Eavey R.D. Inlay tympanoplasty: cartilage butterfly technique. Laryngoscope. 1998;108(5):657–661. doi: 10.1097/00005537-199805000-00006. [DOI] [PubMed] [Google Scholar]
- Emir H., Ceylan K., Kizilkaya Z., Gocmen H., Uzunkulaoglu H., Samim E. Success is a matter of experience: type 1 tympanoplasty : influencing factors on type 1 tympanoplasty. Eur Arch oto-rhino-laryngology Off J Eur Fed Oto-Rhino-Laryngological Soc Affil with Ger Soc Oto-Rhino-Laryngology - Head Neck Surg. 2007;264(6):595–599. doi: 10.1007/s00405-006-0240-6. [DOI] [PubMed] [Google Scholar]
- Fermi M., Maccarrone F., Villari D., et al. Endoscopic tympanoplasty type I for tympanic perforations: analysis of prognostic factors. Eur. Arch. Oto-Rhino-Laryngol. 2021 doi: 10.1007/s00405-020-06588-2. [DOI] [PubMed] [Google Scholar]
- Fukuchi I., Cerchiari D.P., Garcia E., Borges C.E. vol. 72. 2006. pp. 267–271. (Timpanoplastias: resultados cirúrgicos e análise dos fatores que podem interferir no seu sucesso). 2. [Google Scholar]
- Gokgoz M.C., Tasli H., Helvacioglu B. 2019. Results of Endoscopic Transcanal Tympanoplasty Performed by a Young Surgeon in a Secondary Hospital ଝ. xx. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardman J., Muzaffar J., Nankivell P., Coulson C. Tympanoplasty for chronic tympanic membrane perforation in children. Otol. Neurotol. 2015;36(5):796–804. doi: 10.1097/mao.0000000000000767. [DOI] [PubMed] [Google Scholar]
- Huang T., Ho K., Wang L., Chien C., Wang H. A comparative study of endoscopic and microscopic approach type 1 tympanoplasty for simple chronic otitis media. J Int Adv Otol. 2016;vol. 12:28–31. doi: 10.5152/iao.2015.1011. 1. [DOI] [PubMed] [Google Scholar]
- Indorewala S., Adedeji T.O., Indorewala A., Nemade G. vol. 27. 2015. pp. 101–108. (Tympanoplasty Outcomes : A Review of 789 Cases). 79. [PMC free article] [PubMed] [Google Scholar]
- Jalali M.M., Motasaddi M., Kouhi A., Dabiri S., Soleimani R. Comparison of cartilage with temporalis fascia tympanoplasty: a meta-analysis of comparative studies. Laryngoscope. 2017;127(9):2139–2148. doi: 10.1002/lary.26451. [DOI] [PubMed] [Google Scholar]
- Lee J., Nadol J.B.J., Eddington D.K. Factors associated with incomplete insertion of electrodes in cochlear implant surgery: a histopathologic study. Audiol. Neurootol. 2011;16(2):69–81. doi: 10.1159/000316445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murari M., Ajay M. Original Research article comparison between microscopic and endoscopic assisted tympanoplasty- A BEGINNER-OTOLOGIST ’ S perspective. Original Res. Article. 2018;7(43):2016–2019. doi: 10.14260/jemds/2018/1032. [DOI] [Google Scholar]
- Pinar E., Sadullahoglu K., Calli C., Oncel S. Evaluation of prognostic factors and middle ear risk index in tympanoplasty. Otolaryngol. Head Neck Surg. 2008;139(3):386–390. doi: 10.1016/j.otohns.2008.05.623. [DOI] [PubMed] [Google Scholar]
- Salvador P., Gomes P., Silva F., Fonseca R. Type I Tympanoplasty: surgical success and prognostic factors. Acta Otorrinolaringol (English Ed. 2021;72(3):182–189. doi: 10.1016/j.otoeng.2020.04.006. [DOI] [PubMed] [Google Scholar]
- Salviz M., Bayram O., Bayram A.A., et al. Prognostic factors in type i tympanoplasty. Auris Nasus Larynx. 2015;42(1):20–23. doi: 10.1016/j.anl.2014.08.010. [DOI] [PubMed] [Google Scholar]
- Santos J., Andrade C De, Mangussi-gomes J., et al. Transcanal endoscopic myringoplasty : a case series. 2016;82(3):321–325. doi: 10.1016/j.bjorl.2015.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sirena E., Carvalho B., Buschle M., Mocellin M. Timanoplastia tipo 1 e miringoplastia na residência: resultados cirúrgicos e audiométricos. Arq. Int. Otorrinolaringol. 2010;14(4):417–421. doi: 10.1590/s1809-48722010000400006. [DOI] [Google Scholar]
- Tan H.E., Santa Maria P.L., Eikelboom R.H., Anandacoomaraswamy K.S., Atlas M.D. Type i tympanoplasty meta-analysis: a single variable analysis. Otol. Neurotol. 2016;37(7):838–846. doi: 10.1097/MAO.0000000000001099. [DOI] [PubMed] [Google Scholar]
- Tseng C., Lai M., Wu C., Yuan S., Ding Y. ScienceDirect Learning curve for endoscopic tympanoplasty : initial experience of 221 procedures. J. Chin. Med. Assoc. 2017;80(8):508–514. doi: 10.1016/j.jcma.2017.01.005. [DOI] [PubMed] [Google Scholar]
- Tseng C., Lai M., Wu C., Yuan S., Ding Y. ScienceDirect Cost-effectiveness analysis of endoscopic tympanoplasty versus microscopic tympanoplasty for chronic otitis media in Taiwan. J. Chin. Med. Assoc. 2018;81(3):284–290. doi: 10.1016/j.jcma.2017.06.024. [DOI] [PubMed] [Google Scholar]
- Tseng C., Lai M., Wu C., Yuan S., Ding Y. Short-term subjective and objective outcomes of patients receiving endoscopic transcanal myringoplasty for repairing tympanic perforations. Otolaryngol. Head Neck Surg. 2018;111 doi: 10.1177/0194599817735501. [DOI] [PubMed] [Google Scholar]
- Tympanoplasty P.T.I., Prognóstico F De. 2021. Acta Otorrinolaringológica Gallega , Núm . 13 Artículo Original Prognostic Factors Timpanoplastia Tipo I Pediátrica; pp. 1–11. Published online. [Google Scholar]
- Wullstein H. Theory and practice of tympanoplasty. Laryngoscope. 1956;66(8):1076–1093. doi: 10.1288/00005537-195608000-00008. [DOI] [PubMed] [Google Scholar]