Abstract
Internal medicine trainees learn a variety of clinical skills from resident clinical teachers in the inpatient setting. While diagnostic reasoning (DR) is increasingly emphasized as a core competency, trainees may not feel entirely comfortable teaching it. In this perspective article, we provide a framework for teaching DR during inpatient rounds, which includes focusing on the one-liner, structuring a reasoning-focused A&P, and performing a day of discharge reflection.
INTRODUCTION
Diagnostic reasoning (DR) is a fundamental clinical skill that involves a complex series of cognitive processes by which clinicians abstract the available data about a patient and use it to inform their differential diagnosis and testing algorithm.1–3 While DR is frequently demonstrated in grand rounds or educational conferences by peer-nominated expert clinicians, it is first honed and practiced under the guidance of resident clinical teachers during medical school and residency.4–6
Residents are integral to the clinical education of interns and medical students.6,7 Beyond their roles supervising and instructing near peers and more junior learners, residents often spend more time with students in the clinical learning environment than faculty do and become some of the most impactful and memorable educators for medical students. 6–8 Despite the fact that inpatient rotations rely on senior residents as clinical educators, the complexity of DR may leave residents underprepared to teach this crucial element of clinical practice. Furthermore, there are limited resources that support residents in learning to teach DR in the clinical learning environment.6–8
Inpatient rounds serve as a core educational activity on clinical services and offer a time when authentic DR decisions intersect with teaching opportunities.9–11 In this article, we review theoretical frameworks relevant to reasoning and apply them to a 3-step process for senior residents to teach DR on rounds using elements of daily patient presentations.
THEORETICAL FRAMEWORKS FOR DIAGNOSTIC REASONING
Information processing (IP) theory and situativity theory are two mutually supportive theoretical frameworks that can help inform strategies to teach DR in the inpatient setting (Table 1).2,12
Table 1.
Theoretical Frameworks for Diagnostic Reasoning14
| Information processing theory | Situativity theory | |
|---|---|---|
| Where is the center of the DR process? | Clinician’s mind | Clinical interactions |
| What facilitates accurate DR? | Well-organized and well-developed knowledge structures (e.g., diagnostic schemas) and mental models (e.g., illness scripts) | Well-developed knowledge structures and the ability to manage the dynamic, complex interactions in clinical environments |
| Examples in practice |
Organizing causes of chest pain into cardiac, pulmonary, gastrointestinal, and musculoskeletal causes Developing illness scripts that include differentiating features (e.g., findings that distinguish acute myocardial infarction from acute pericarditis) |
Considering how patient-physician communication influences the probability the physician assigns to different diagnoses (e.g., acute coronary syndrome and gastroesophageal reflux) Recognizing how the ability to access a patient’s prior cardiac stress test results in the electronic health record plays a role framing diagnostic probabilities |
Abbreviations: DR diagnostic reasoning
IP theory emphasizes the knowledge a clinician stores in their head and the internal mental processes they employ when solving a clinical problem.3,13–16 Principles related to IP theory include the development of knowledge structures for storage in long-term memory and retrieval in clinical settings (e.g., categorizing causes of chest pain into cardiac, pulmonary, gastrointestinal, and musculoskeletal etiologies) and the use of general reasoning strategies, such as hypothetico-deductive, inductive, and analogic reasoning, when retrieving, manipulating, and applying knowledge in practice (e.g., using negative serial troponins to contradict the hypothesis of an acute myocardial infarction as the cause of a patient’s chest pain).17–21 Situativity theory offers a theoretical framework that can help account for contextual influences on clinician’s reasoning processes. Situativity theories view cognition as a social process influenced by interactions between individuals and the clinical environment and thereby accommodate the role of situational factors in a clinician’s cognition (e.g., how a patient suggesting a specific diagnosis to a clinician influences the probability the clinician assigns to that diagnosis).15
IP and situativity theories help teachers promote the development of knowledge structures as well as the ability to appreciate and manage the influence of context on reasoning. To effectively teach DR, resident clinical teachers need instructional strategies that allow them to apply these theoretical frameworks to education opportunities in the clinical learning environment, such as inpatient rounds.22–24
A CONCEPTUAL FRAMEWORK FOR TEACHING DIAGNOSTIC REASONING ON ROUNDS
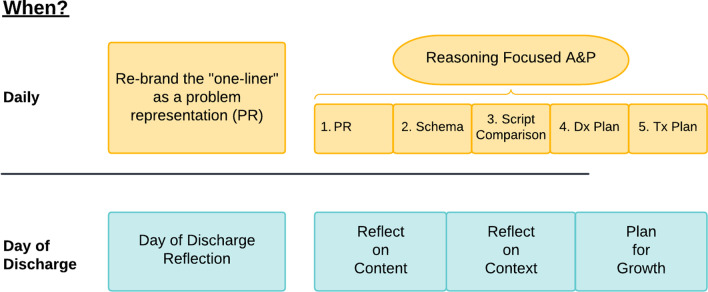
Here, we provide a framework that residents can use to teach DR during three discrete moments of inpatient oral presentations: the one-liner, the assessment and plan, and the day of discharge presentation. These strategies are easily adaptable to a variety of resident-led rounding formats (e.g., walk-rounds, bedside-rounds, and card-flip rounds) and scenarios.
Focus on the “One-Liner”
Practicing and rehearsing the oral presentation has long been a cornerstone in the development of trainees in the inpatient setting. Central to this practice is the recitation of the one-liner, a brief summary statement that traditionally includes the patient’s past medical history and presenting concerns. Yet, while the one-liner can serve to introduce the patient to the clinical team, it does little in the way of highlighting abstract thinking and DR. Many of us have recited or heard one-liners that become bloated with somewhat irrelevant information (e.g., the patient’s entire past medical history) or that change little from day to day despite the clear evolution in the team’s thinking about a clinical problem. We suggest intentionally rebranding the one-liner as a “problem representation” to provide an opportunity for learners to refine core DR principles.
IP theory highlights the creation of a problem representation as a key initial step in the reasoning process.22,23 The PR has variably been defined as a concise, abstracted summary of the most relevant clinical data aimed to guide one’s thinking (analogous to a phrase one may input into an online search engine).24 The structure of the PR includes key contextual information, a description of the time course, and labeling of the clinical syndrome.24 We encourage residents to highlight how the PR is principally distinct from the traditional one-liner with regard to the level of data abstraction and manipulation (e.g., translating an erythematous, swollen, and tender knee to “monoarticular arthritis”) (Table 2).
Table 2.
Examples of the Progression of the One-Liner to a Problem Representation
| One-liner | Problem representation |
|---|---|
| A 50-year-old woman with a new diagnosis of acute myeloid leukemia undergoing induction chemotherapy who presents with chills and malaise for 1 day. Her temperature was 101.8°F with labs showing a white blood cell count of 0.8 per mm3 and an absolute neutrophilic count of < 100 per mm3. Her urinalysis was normal and her chest x-ray was clear | A 50-year-old woman with AML undergoing induction chemotherapy presenting with acute, high-risk, non-localizing febrile neutropenia |
| A 35-year-old man with a history of diabetes, asthma and IV drug use presenting with 6 days of worsening right shoulder pain, tachycardia, fevers, leukocytosis, and thrombocytosis | A 35-year-old man with a history of injection drug use presenting with acute, progressive febrile monoarticular arthritis |
| An 85-year-old woman with a history of tobacco use, peripheral arterial disease, rheumatoid arthritis, hypertension, diabetes, chronic kidney disease presenting with 6 months of worsening shortness of breath and weight loss, 3 days of forgetfulness and decreased arousal, found to have a large, dense right lung opacity on CT chest, and elevated calcium | An 85-year-old woman with a 30-pack-year smoking history presenting with chronic, progressive dyspnea and acute altered mental status found to have hypercalcemia and a new right lung mass |
Context (who) in bold, timing (when) in italics, syndrome (what) underlined
Abbreviations: PR problem representation, IV intravenous
Concrete strategies that could be incorporated on rounds include editorialization, the use of semantic qualifiers, and iteratively updating the PR each day. By editorialization, we are referring to the critical appraisal of what clinical data is included. For example, in a patient presenting with an acute myocardial infarction, a prior traumatic wrist fracture may be less relevant than an 80-pack-year smoking history. Resident clinical teachers can probe the PR of their learners and ask them to critically appraise the relevance of the data they choose to include. Separately, the PR can be further strengthened through the incorporation of “semantic qualifiers,” or opposing descriptors that can be used to compare and contrast considerations in one’s differential diagnosis (e.g., unilateral vs bilateral, acute vs chronic) and add specificity to the clinical syndrome under consideration.25 The use of such semantic qualifiers can be emphasized on teaching rounds and has been associated with improved diagnostic performance.22,24 Lastly, we all recognize that our patients’ conditions evolve over time, and our PRs should reflect that progression rather than be copied forward from day to day. For example, a patient may present with a chief concern of nausea and diaphoresis but be ultimately found to have a non-ST-elevation myocardial infarction, rendering reference to the initial symptoms less diagnostically relevant in the student’s problem representation on the day after left-heart catheterization. Encouraging learners to meticulously update their problem representations in the electronic health record (EHR) can also serve as a similar educational activity, with the added benefit of communicating a concise and up-to-date framing of the patient to the larger interprofessional care team.26 Resident clinical teachers can challenge their learners to reframe their PR as their progressive understanding of their patient’s syndrome evolves.
A Reasoning-Focused Assessment and Plan
One of the primary challenges faced by early learners is coherently processing large amounts of clinical data. A structured approach to organizing and articulating DR may be of benefit to early trainees, especially as they construct their assessment and plans in oral presentations.27 A conceptual model of the reasoning process suggests that diagnosticians first represent a problem, evoke a specific schema (a structured approach to a common clinical scenario, such as chest pain) for that syndrome, and then compare and contrast amongst their library of illness scripts (pre-formed knowledge structures about a given disease entity, such as their knowledge about the presentation of ST-elevation myocardial infarctions) to select the best fit for that specific diagnosis (Fig. 1).28 Here, we suggest applying this model to create a reasoning-focused structure for the assessment and plan (A&P) that can promote knowledge organization and DR amongst trainees (Fig. 1). This structure is most useful when the team is still working towards a definitive diagnosis or the etiology of a new clinical problem (e.g., when presenting a new admission, when there is ongoing diagnostic uncertainty, or when a new problem develops during the patient’s hospitalization). In our experience, this framework for the assessment and plan is just as, if not more, efficient than traditional presentation formats because it provides an established and focused structure for oral presentations.
Fig. 1.
A conceptual framework for teaching DR on rounds. Figure legend: PR, problem representation; Dx, diagnostic; Tx, treatment
Applying this framework to the A&P involves 5 steps: (1) abstractly label each problem; (2) identify and discuss a relevant schema; (3) compare, contrast, and prioritize illness scripts within that schema (i.e., akin to constructing the differential diagnosis); and present both (4) diagnostic and (5) therapeutic plans. For example, one may encourage a learner who is presenting the A&P for a patient with chest pain to highlight relevant risk factors in their PR (e.g., 75-year-old man with significant vascular disease presenting with acute chest pain), evoke an approach to chest pain (cardiac, pulmonary, gastrointestinal, and musculoskeletal), and then compare and contrast illness scripts from their schema (acute coronary syndrome vs pulmonary embolism vs gastroesophageal reflux) to create a prioritized differential diagnosis. Based on this differential diagnosis, which is supported by a diagnostic schema and illness script comparison, the learner suggests initial diagnostic and therapeutic interventions. The illness script selection portion also offers a rich opportunity to articulate how situational factors promote or impede their diagnostic accuracy. For example, a learner may note that, while they did not notice a murmur on a patient with bacteremia, the noisy environment reduces their confidence in using the absence of a murmur to decrease their suspicion for infective endocarditis. These approaches can support the incorporation of structured knowledge organization and the influence of situational factors, which may promote improved retention and diagnostic performance.29
Lastly, we posit that the use of a formalized structure for the A&P can help teachers guide their feedback on specific reasoning elements (Table 3). For example, a trainee may create an appropriate PR, but struggle in evoking the correct schema, thereby allowing their resident to provide more directed and targeted feedback. With such an explicit template for the A&P, the barrier for residents to directly comment on the reasoning performance may be lessened.
Table 3.
Sample Strategies for Resident Clinical Teachers to Promote DR Teaching During Conversations on Inpatient Rounds
| Component | Learner | Resident’s response |
|---|---|---|
| Problem representation | “This is a 45-year-old man living with HIV/AIDS (CD4 = 20) who presents with 4 weeks of escalating headaches and neck stiffness, found to have a lymphocytic pleocytosis, increased CSF protein, and low glucose on his LP.” |
“Awesome summary! To push you a bit, how could you synthesize his symptoms and CSF parameters more concisely?” Instructional aim: Prompt learner to distill the patient’s symptoms to “chronic meningitis.” |
| Reasoning-focused assessment and plan | “I think the most likely causes of his headache is tuberculous meningitis. Another possible cause is S. pneumoniae, though this is less likely. I want to follow up the cultures and start rifampin, isoniazid, pyrazinamide, and ethambutol.” |
“You’re absolutely right that TB can cause a chronic meningitis. My illness script for S. pneumoniae meningitis is an acute, rather than chronic, meningitis. I would suggest replacing pneumococcus with fungal pathogens, like Cryptococcus, on your chronic meningitis schema; Let’s add to his CSF a cryptococcal antigen, to test for Cryptococcus, and a Mycobacterium tuberculosis (TB) polymerase chain reaction, to test for TB. We can decide on treatment once these tests return.” Instructional aim: Refine illness scripts, expand diagnostic schemas, and anchor testing decisions to both |
| Day of discharge reflection | “Ok, for Mr. Smith, our patient with HIV-associated cryptococcal meningitis, is ready to discharge today. He’s going to SNF on fluconazole and will be leaving at 2 pm.” |
Great! Let’s reflect on the diagnostic journey we experienced with Mr. Smith. What’s one thing you’ve learned that you’ll bring to the next time you see a patient with HIV and headaches? We can also think about how our conversations with his outpatient care team supported our clinical decisions Instructional aim: Prompt reflection on both content and context |
Day of Discharge Reflection
Deliberate reflection is an important element of clinical skill building, particularly the skill of DR. This could be best incorporated through institutionalization of systematic reflection, which involves a retrospective examination of the team’s diagnostic journey through a patient’s diagnostic journey.30 The day of discharge serves as a particularly useful time for this reflection, as this transition offers a natural opportunity to consider one’s own reasoning through the patient encounter and develop insights that will support learning and improve future performance.30
In guiding this reflection, residents can explore the evolution in the team’s collective thinking about a case, including the various factors that served to inform or distract from reaching the ultimate diagnosis. For example, a team may reflect on the diagnostic journey of a patient with end-stage renal disease admitted for fever who is ultimately found to have Staphylococcus aureus bacteremia from their tunneled dialysis catheter. Whereas the source of fever may have initially been unclear, a retrospective analysis of case details (e.g., newly placed catheter, negative chest x-ray, and urinalysis) can help the team identify clues that will serve as prospective reasoning tools in the future.
We encourage residents to draw on concepts from both IP and situativity theories during the day of discharge reflection. Through the lens of IP theory, a resident can prompt learners to reflect on the accuracy and comprehensiveness of their own diagnostic schemas and illness scripts (i.e., “content,” see Fig. 1). Additionally, situativity theory can help learners reflect on situational elements that supported or impeded their reasoning (i.e., “context,” see Fig. 1). These might include their overall workload, the quality of communication with the patient and other health professionals, the acuity or complexity of the case, or other elements of the clinical environment.
Lastly, the day of discharge reflection allows all team members to openly and dispassionately explore the sources of diagnostic error and embody diagnostic humility. Senior team members can remind learners that diagnostic missteps are unavoidable elements of patient care by openly discussing their own areas for diagnostic improvement, thereby modeling a growth mindset.31 Ultimately, the day of discharge reflection creates opportunities for DR skill development, fosters a culture of reflective practice, and allows team members to identify concrete ways they may approach similar situations in the future (i.e., “Plan for Growth,” see Fig. 1.) Those interested in applying these reflective principles prior to discharge may wish to explore the concept of a “diagnostic time out.” While this is beyond the scope of our proposed framework, we encourage those interested to explore the cited literature on this topic.32,33
Adapting These Strategies to Real-Life Rounds
Residents can use these flexible, learner-focused strategies in a variety of rounding formats (e.g., card-flipping, walk rounding, or bedside rounding). The primary area of consideration relates to the presence or absence of the patient, particularly when discussing whether a cognitive or medical error has occurred.34–36 In such scenarios, we suggest the team engage in a reflective conversation with one another and without the patient before facilitating a formal conversation during which any errors are disclosed; this can provide space for team members to more freely contemplate areas for diagnostic growth and improvement. We encourage clinical teams to consult further resources within their health system regarding the processing and disclosure of errors.
Additionally, teams may face time constraints (i.e., needing to prioritize medication review or discharge instructions with a patient at bedside) or other unanticipated events (i.e., unforeseen patient-directed discharges) that may limit the ability to complete one or more components of this framework on a given day. In such scenarios, we feel that the reflective practices described in this paper should not take away from important, time-sensitive conversations with the patient around their discharge and could be done with close temporal relation to the patient encounter (i.e., the day after discharge) with much the same anticipated benefit.
CONCLUSION
Although much of our growth as diagnostic reasoners occurs during our formative years of medical school and residency, teaching DR during busy inpatient rotations can be challenging. Here, we review two theories relevant to DR (IP and situativity theories) and provide a 3-step process (focusing on the one-liner, structuring a reasoning-focused A&P, and performing a day of discharge reflection) for resident clinical teachers to teach DR on their daily rounds.
DR, however, is a complicated topic comprised of various theoretical models. Our approach, while aimed at practical interventions to teach reasoning skills, is limited and does not comprehensively cover the various nuances of this concept. Nevertheless, we see it as an introduction to this field, and one that can easily be incorporated into the fast-paced mechanics of inpatient rounds.
The cognitive apprenticeship of clinical training relies on close iterative feedback from resident clinical teachers, who themselves often lack significant expertise in the content they are conveying. While instructing learners in DR may be an intimidating prospect for residents, it is crucial that residents are able to teach this critically important clinical skill. We hope that the theoretical background and practical framework provided in this perspective article will equip resident teachers with the tools to move from “seeing and doing” to “teaching” the fundamentals of reasoning.
Declarations
Conflict of Interest
John C. Penner has no conflicts of interest; Lindsey C. Shipley has no conflicts of interest; Daniel J. Minter has no conflicts of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Connor DM, Durning SJ, Rencic JJ. Clinical Reasoning as a Core Competency. Acad Med. 2020;95(8):1166–1171. doi: 10.1097/ACM.0000000000003027. [DOI] [PubMed] [Google Scholar]
- 2.Young M, Thomas A, Lubarsky S, et al. Drawing Boundaries: The Difficulty in Defining Clinical Reasoning. Acad Med. 2018;93(7):990–995. doi: 10.1097/ACM.0000000000002142. [DOI] [PubMed] [Google Scholar]
- 3.Durning SJ, Artino AR, Schuwirth L, van der Vleuten C. Clarifying assumptions to enhance our understanding and assessment of clinical reasoning. Acad Med. 2013;88(4):442–448. doi: 10.1097/ACM.0b013e3182851b5b. [DOI] [PubMed] [Google Scholar]
- 4.Rencic J, Trowbridge RL, Fagan M, Szauter K, Durning S. Clinical Reasoning Education at US Medical Schools: Results from a National Survey of Internal Medicine Clerkship Directors. J Gen Intern Med. 2017;32(11):1242–1246. doi: 10.1007/s11606-017-4159-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Aba Alkhail B. Near-peer-assisted learning (NPAL) in undergraduate medical students and their perception of having medical interns as their near peer teacher. Med Teach. 2015;37(Suppl 1):S33–39. doi: 10.3109/0142159X.2015.1006602. [DOI] [PubMed] [Google Scholar]
- 6.Remmen R, Denekens J, Scherpbier A, et al. An evaluation study of the didactic quality of clerkships. Med Educ. 2000;34(6):460–464. doi: 10.1046/j.1365-2923.2000.00570.x. [DOI] [PubMed] [Google Scholar]
- 7.Ramani S, Mann K, Taylor D, Thampy H. Residents as teachers: Near peer learning in clinical work settings: AMEE Guide No. 106. Med Teach. 2016;38(7):642–655. doi: 10.3109/0142159X.2016.1147540. [DOI] [PubMed] [Google Scholar]
- 8.Morrison EH, Friedland JA, Boker J, Rucker L, Hollingshead J, Murata P. Residents-as-teachers training in U.S. residency programs and offices of graduate medical education. Acad Med. 2001;76(10 Suppl):S1–4. doi: 10.1097/00001888-200110001-00002. [DOI] [PubMed] [Google Scholar]
- 9.Houchens N, Harrod M, Fowler KE, Moody S, Saint S. How Exemplary Inpatient Teaching Physicians Foster Clinical Reasoning. Am J Med. 2017;130(9):1113.e1–1113.e8. doi: 10.1016/j.amjmed.2017.03.050. [DOI] [PubMed] [Google Scholar]
- 10.Walton JM, Steinert Y. Patterns of interaction during rounds: implications for work-based learning. Med Educ. 2010;44(6):550–558. doi: 10.1111/j.1365-2923.2010.03626.x. [DOI] [PubMed] [Google Scholar]
- 11.Kulkarni VT, Salgado SM, Pelletier SR, Shields HM. Teaching methods used by internal medicine residents on rounds: what works? Adv Med Educ Pract. 2019;10:15–21. doi: 10.2147/AMEP.S181153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schuwirth L. Is assessment of clinical reasoning still the Holy Grail? Med Educ. 2009;43(4):298–300. doi: 10.1111/j.1365-2923.2009.03290.x. [DOI] [PubMed] [Google Scholar]
- 13.Croskerry P. Clinical cognition and diagnostic error: applications of a dual process model of reasoning. Adv Health Sci Educ Theory Pract. 2009;14(Suppl 1):27–35. doi: 10.1007/s10459-009-9182-2. [DOI] [PubMed] [Google Scholar]
- 14.Charlin B, Boshuizen HPA, Custers EJ, Feltovich PJ. Scripts and clinical reasoning. Med Educ. 2007;41(12):1178–1184. doi: 10.1111/j.1365-2923.2007.02924.x. [DOI] [PubMed] [Google Scholar]
- 15.Durning SJ, Artino AR. Situativity theory: a perspective on how participants and the environment can interact: AMEE Guide no. 52. Med Teach. 2011;33(3):188–199. doi: 10.3109/0142159X.2011.550965. [DOI] [PubMed] [Google Scholar]
- 16.Custers EJ, Regehr G, Norman GR. Mental representations of medical diagnostic knowledge: a review. Acad Med. 1996;71(10 Suppl):S55–61. doi: 10.1097/00001888-199610000-00044. [DOI] [PubMed] [Google Scholar]
- 17.Feltovich PJ, Barrows HS. Issues of generality in medical problem solving. Tutorials in problem-based learning. Published online 1984:128–142.
- 18.Norman G. Research in clinical reasoning: past history and current trends. Med Educ. 2005;39(4):418–427. doi: 10.1111/j.1365-2929.2005.02127.x. [DOI] [PubMed] [Google Scholar]
- 19.Schank RC, Abelson RP. Scripts, Plans, Goals and Understanding: An Inquiry into Human Knowledge Structures. Repr. Psychology Press; 2008
- 20.Patel VL, Arocha JF, Zhang J. Thinking and Reasoning in Medicine. In: The Cambridge Handbook of Thinking and Reasoning. Cambridge University Press; 2005:727–750.
- 21.Elstein AS, Shulman LS, Sprafka SA. Medical Problem Solving: An Analysis of Clinical Reasoning. Harvard University Press; 1978.
- 22.Bordage G. Prototypes and semantic qualifiers: from past to present. Med Educ. 2007;41(12):1117–1121. doi: 10.1111/j.1365-2923.2007.02919.x. [DOI] [PubMed] [Google Scholar]
- 23.Chang RW, Bordage G, Connell KJ. The importance of early problem representation during case presentations. Acad Med. 1998;73(10 Suppl):S109–111. doi: 10.1097/00001888-199810000-00062. [DOI] [PubMed] [Google Scholar]
- 24.Trowbridge RL. American College of Physicians. Teaching Clinical Reasoning.; 2015.
- 25.Bowen JL. Educational strategies to promote clinical diagnostic reasoning. N Engl J Med. 2006;355(21):2217–2225. doi: 10.1056/NEJMra054782. [DOI] [PubMed] [Google Scholar]
- 26.Bowker D, Torti J, Goldszmidt M. Documentation as composing: how medical students and residents use writing to think and learn. Adv Health Sci Educ. 2022;28:453–475. doi: 10.1007/s10459-022-10167-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Feldman W, Dhaliwal G. When Professors Don’t Return Essays. Teach Learn Med. 2015;27(4):431–434. doi: 10.1080/10401334.2015.1077129. [DOI] [PubMed] [Google Scholar]
- 28.Dhaliwal G. Developing teachers of clinical reasoning. Clin Teach. 2013;10(5):313–317. doi: 10.1111/tct.12082. [DOI] [PubMed] [Google Scholar]
- 29.Torre D, Durning SJ, Rencic J, Lang V, Holmboe E, Daniel M. Widening the lens on teaching and assessing clinical reasoning: from “in the head” to “out in the world”. Diagnosis (Berl). 2020;7(3):181–190. doi: 10.1515/dx-2019-0098. [DOI] [PubMed] [Google Scholar]
- 30.Croskerry P. Diagnostic Failure: A Cognitive and Affective Approach. In: Henriksen K, Battles JB, Marks ES, Lewin DI, eds. Advances in Patient Safety: From Research to Implementation (Volume 2: Concepts and Methodology). Advances in Patient Safety. Agency for Healthcare Research and Quality (US); 2005. Accessed November 20, 2020. http://www.ncbi.nlm.nih.gov/books/NBK20487/ [PubMed]
- 31.Klein J, Delany C, Fischer MD, Smallwood D, Trumble S. A growth mindset approach to preparing trainees for medical error. BMJ Qual Saf. 2017;26(9):771–774. doi: 10.1136/bmjqs-2016-006416. [DOI] [PubMed] [Google Scholar]
- 32.Ely JW, Graber ML, Croskerry P. Checklists to reduce diagnostic errors. Acad Med. 2011;86(3):307–313. doi: 10.1097/ACM.0b013e31820824cd. [DOI] [PubMed] [Google Scholar]
- 33.Trowbridge RL. Twelve tips for teaching avoidance of diagnostic errors. Med Teach. 2008;30(5):496–500. doi: 10.1080/01421590801965137. [DOI] [PubMed] [Google Scholar]
- 34.Mazor KM, Simon SR, Gurwitz JH. Communicating With Patients About Medical Errors: A Review of the Literature. Arch Intern Med. 2004;164(15):1690. doi: 10.1001/archinte.164.15.1690. [DOI] [PubMed] [Google Scholar]
- 35.Simpkin AL, Armstrong KA. Communicating Uncertainty: a Narrative Review and Framework for Future Research. J GEN INTERN MED. 2019;34(11):2586–2591. doi: 10.1007/s11606-019-04860-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dahm MR, Crock C. Understanding and Communicating Uncertainty in Achieving Diagnostic Excellence. JAMA. 2022;327(12):1127. doi: 10.1001/jama.2022.2141. [DOI] [PubMed] [Google Scholar]