Abstract
Individuals with severe cartilage degeneration of the hip or knee or collapsed vertebrae that cause spine deformities can suffer from joint and neuropathic pain in the back, disuse of the affected limb, and restriction of movements. Surgical intervention is the most widespread and successful solution to date. There is a general belief that eating healthy and staying physically and mentally active might have a preventive role against musculoskeletal disease occurrence, while instead, we are more certain of the benefits deriving from a healthy diet and exercise therapy after major orthopaedic procedures. These aspects are in fact vital components in enhanced recovery after surgery programmes. However, they are applied in hospital settings, are often centre-dependent, and lack primary and tertiary preventive efficacy since end once the patient is discharged. There is the lack of initiatives at the territorial level that ensure a continuum in the patient’s journey towards orthopaedic surgery, home transition, and a healthy and long-lasting life. The expert panel advocates the integration of an intermediate lifestyle clinic that promotes healthy eating, physical activity, and sleep hygiene. In this facility directed by professionals in enhancing recovery after surgery, patients can be referred after the surgical indication and before home discharge. Surgery is in fact a moment when individuals are more curious to do their best to heal and stay healthy, representing a timepoint and opportunity for educating patients on how lifestyle changes may optimise not only their surgical recovery but also long-term future health state.
Keywords: access to health care, health care facilities, manpower, services, surgeries, orthopaedic rehabilitation, dietary habits, physical therapy modalities, good sleep habit
Background
We are an aging world. Within the next 40 years, there will probably be more grandparents than grandchildren, with the senior population exceeding 2 billions.1 The natural aging process affects the musculoskeletal health of older people, which can lead to joint pain, limitations to daily activities, and a decline in physical activity. Symptoms may include pain in the neck, back, or leg, stiffness in the upper or lower limbs, and eventually cause difficulty to walking, standing, lifting and carrying heavy objects, rising from the floor, dressing, eating, and sleeping. Individuals can often experience accompanying tiredness, worry, sadness, anxiety, or extreme fatigue. Globally, there are 0.77 billion people over the age of 65, and it is estimated that almost 0.5 billion suffer from a musculoskeletal condition that would benefit from rehabilitation.2 In two out of ten, symptoms are so disabling that there is the need for surgical treatment. These figures are expected to double in the coming decades, approaching the 0.3 billion older adults who will undergo a major orthopaedic surgery.3 Diseases of the joints, bones, and muscles are related to chronic inflammation, limit the ability to move, can contribute to weight gain, and pain can disturb sleep. Musculoskeletal illnesses were shown to independently increase of 17% the odds of developing other non-communicable diseases, such as cardiovascular diseases, cancer, diabetes, or mental health issues.4 The concomitant presence of malnutrition, myosteatosis, and sarcopenia in older patients is often found,5 meaning there is a potential to optimise the physical status of many patients undergoing major orthopaedic surgery. These ailments are known to complicate the clinical picture, with the patients themselves encountering serious difficulty in recovery, especially after major spinal procedures that require longer rehabilitation.
Not Just Ailments
Other factors in addition to ailments can undermine the physical and mental recovery of patients treated surgically, making the body vulnerable and the mind exposed:6 pain, food insecurity, underdevelopment, illiteracy, civil disorders, absence of home care, medical malpractice, discontinuity of care, and lack of patient’s activation. These conditions rather aggravate the quality of life and affect resilience, regardless of the success of surgery. It is in fact not only the absence of disease that matters but the environment in which patients live. These determinants of social vulnerability are often overlooked as if the most decisive phase for the success of surgery was that in the hospital. This is not the case for orthopaedic surgery, where a broad range of socioeconomic factors influence recovery after surgery of patients, whether they live in developed areas or in low-/middle-income nations.7–9 Less than 5% of the world’s surgical procedures are performed in underdeveloped countries,10 reasonably assuming that there may exist a high number of older individuals living in vulnerable conditions with unoperated back pain or painful joints. Longevity is worthless if there is no enjoyment in life, and there is no joy in living with the burden of a disease. We need to develop a global territorial health system that takes care of the patient holistically and in the long term, regardless of their medical and social status. Such a system thinking has already been suggested to enable community participation, more coordinated responses to challenges, minimization of discrepancy between the optimal care and that basic assistance which patients are receiving, and maximization of patient safety.11–13
Conceptual Scenario
A large proportion of age-related illnesses could be potentially modifiable through the promotion of healthy eating, physical activity, and the preservation of mental health (HEPAS).14,15 With the adjunct of a self-management component to the HEPAS, we can outline the direction to take to empower orthopaedic patients and reduce the burden of musculoskeletal diseases before and after surgery.16,17 This is not a new discovery. Enhanced recovery after surgery (ERAS) programmes are a multidisciplinary approach designed to achieve early recovery after surgery, delivering advice about what to eat, drink, and what exercise to do before and after major orthopaedic surgery.6,18,19 This care pathway is part of perioperative medicine, being applied in the most advanced and virtuous centres. However, it lacks primary and tertiary preventive efficacy since it starts at the preoperative evaluation and ends once the patient is discharged. Few initiatives are designed at the territorial level caring for those most at risk. One example is the integrated care for older people (ICOPE) that aims at reorienting community service delivery models towards a continuum of care for older people.20 However, we must take advantage of the knowledge employed by ERAS professionals to ensure that educational efforts aimed at what is best for the orthopaedic patient are not in vain and maintained in the long term, because over time humans tend to return to old habits. There might be the need of a “facilitator” during the transition from a major orthopaedic surgery to home care for a healthy and long-lasting life. This intermediate care service shall be the HEPAS clinic. Enabling technologies are making their way to plan, navigate, monitor, and engage during surgical procedures. The HEPAS clinic would exploit the same technological advances to pave the way towards a service development facilitated by remote patient engagement and monitoring.
A multidisciplinary group of experts in prehabilitation, perioperative medicine, rehabilitation, and integrated home care applied to the orthopaedic field have gathered to define a conceptual, sustainable, and innovative scenario of healthcare organisation that integrates the hospital with the community. The group, made up of a health director, scientific director, anaesthetist, orthopaedic surgeon, physiotherapist, and dietitian, was asked to answer the following questions:
Is there a touch point when we should activate the patient?
What habits to promote for surgery?
Who should spend time, energy, and resources?
What means to overcome territorial barriers?
What are the indicators in this patient’s journey?
Is There a Touch Point When We Should Activate the Patient?
The general population has poor attitudes towards preventive recommendations for pathologies that could perhaps occur years later.21,22 Family responsibilities, demanding jobs, and forms of shift work are some of the reasons reported by individuals not to engage in healthy behaviours.23 Providing the most appropriate treatment at the right time is a necessary step in patient retention.24 It is not rare that patients with the indication of a major orthopaedic surgery ask what they can do to improve the odds of recovery during pre-admission visits. The ERAS team often tells the patient to quit smoking, eat better, not sit on the couch all the time, and try to follow a healthy sleep hygiene. This engagement is often too close to hospital admission, nevertheless. This is due to the limited temporal validity, dictated by biology and law, of preoperative testing. Changing lifestyle takes time,25 especially in patients who are old, have followed their routine for years, eat the same foodstuffs, and have their own beliefs about what is good for them. We argue that the moment when the surgical indication is given, which can happen even months before at the outpatient clinic, is the touch point. This anticipation might be beneficial to augment the access to an effective procedure for very frail individuals and reduce deferral for medical reasons, such as uncontrolled chronic disease or obesity.
What Habits to Promote for Surgery?
Poor lifestyle habits are pervasive among community-dwelling seniors and their caregivers.26,27 At preoperative visit, questionnaires aimed at stratifying older patients on the basis of their risk for perioperative complications contain questions on nutrition, physical function, and mental health,28,29 with the ERAS team comprising dietitians and physiotherapists to deliver evidence-based practice. The habits to promote are therefore those pertaining the HEPAS. If we know that unhealthy habits increase the perioperative risk and we would like patients to behave their best for surgery, why should not we educate them to eat well, move, sleep, and keep cognitively intact long before surgery and as much as possible after for a full recovery? The reasons why general practitioners do not discuss lifestyle behaviours rely on the belief that basic counselling efforts are futile and that time pressures prevent the adoption of an advanced motivational interviewing.25,30 However, it is vital to enable self-management in patients to prevent or manage ailments, requiring health professionals to move from a traditional model of care to a more collaborative care.31 Notably, any dietary or physical activity recommendations may vary based on the end user. For example, the exercises recommended for a patient undergoing heart surgery may not be the same as for a patient undergoing arthroplasty. We argue that the HEPAS multidisciplinarity, perfectly mirroring the ERAS team, will effectively manage specialized and personalized interventions, and this has to be organised in a dedicated facility (HEPAS clinic).
Who Should Spend Time, Energy, and Resources?
The strength derived from the multidisciplinary of ERAS ought to be taken somewhat as a point of reference, giving its substantial prominence in the international recommendations for a successful clinical practice. In the HEPAS clinic, there should be specialism linked with primary care providers involved in the orthopaedic patient journey. For instance, dietitians, physiotherapists, nurses, and psychologists are needed to cover the three dimensions of food, movement, and sleep. The role of the coordinating specialist, similarly to the “ERAS nurse”, may be covered by allied health professionals based on the prevailing patient need (eg, “HEPAS dietitian” or “HEPAS physiotherapist”). The patient would be assisted to optimize the suitability for surgery, rehabilitate, and would be supported in the short term for healthy lifestyle choices. The level of intensity of care and modalities would be targeted on the patient and the goal. The HEPAS staff shall give the added benefit of managing the patient’s journey both horizontally (eg, continuity of care) and vertically (eg, from the community to the global level). The patient management shared between the HEPAS staff, ERAS team, and primary care providers will ensure a low-risk patient transition from postoperative diet, exercise therapy, and discharge therapy to short-term healthy eating, physical activity, and sleep hygiene. Furthermore, we argue that it may be useful to consider designing a new facility solely dedicated to the long-term promotion of healthy habits. Here, HEPAS and public health professionals, such as public health nurses and educators, dental hygienists, pharmacists, occupational therapists, and podiatrists would take care of maintaining adherence to the HEPAS principles and ensuring correct management of chronic home therapy of orthopaedic patients.
What Means to Overcome Territorial Barriers?
In a first phase of patient’s journey, the specialists of the HEPAS clinic could take charge of the patient awaiting surgery. After surgery, they would represent an intermediate stage of care for the patient transition to home. Telemedicine services should dominate to streamline the data flow of outpatient clinics, hospitals, and home care. Broadcasting educational videos, which is something already experimented with poor frameworks nevertheless,32 would certainly ensure early care delivery no matter how far the patient’s home will be. Remote patient management during preoperative waiting time and rehabilitation could generate significant opportunities and data from wearables or handheld digital devices (eg, smartwatches with activity trackers, smartphones for food recording or shopping tips) that have never been exploited before. Regardless of the health system integration, which arguably faces more hurdles in low- and middle-income countries,33,34 telehealth is a feasible solution as means for high-speed low-latency internet connection across the globe already exist even for the most remote and rural locations across the globe (eg, satellite internet). In the case of patients with lack of access to technology, the HEPAS clinic could provide for the necessary means in the short term, such as tablets and wrist-worn devices. The team will always have to evaluate the structural organisation of the community, from which flexible programs may arise considering for instance the proximity of supermarkets to patient’s home or the existence of local sports-related infrastructures and a city park for indoor or outdoor gymnastics, respectively.23
What are the Indicators in This Patient’s Journey?
The statistical measures to help indicate the appropriateness of the new framework and track performance can include a wide range of possible health (eg, disability-adjusted life years, patient activation, experiences), structural/organisational (eg, adequacy of facilities), process/technological (eg, safety, the extent of the application of evidence-based care), and economic indicators (eg, cost-related), all in view of international comparisons.13,35–37 The evaluation of indicators from developmental data of an individual care plan could be attributed to case managers, epidemiologists, and health commissioners, whose expertise and global vision play a valuable role in the regular assessment of healthcare safety and quality. The ethics of the system draws on a mix of patient reported outcome and experience measures, which should therefore be included among the indicators that recalibrate the process. Constant clinical governance meetings and exploratory studies, in a process of continuous quality improvement, shall demonstrate clinical, patient-centred, and financial viability. It is therefore expected a close collaboration between primary care providers, the HEPAS and ERAS specialists, and public health professionals. Artificial intelligence algorithms would help identify the right treatment for the right patients, for instance, identifying the red flags for adverse outcome or low long-term adherence, thus creating a recovery-oriented journey towards health equity.38
Summary
Indication for arthroplasty or corrective anatomical alignment is given to patients suffering from painful musculoskeletal disorders of the hip, knee, or spine. These individuals are highly receptive after the surgical indication is given, and therefore this moment could reasonably be the touch point for patient’s activation, meaning to motivate and increase the individual’s abilities, self-confidence, awareness, and knowledge. The introduction of a HEPAS clinic that takes charge of the patient awaiting the operation would prove the necessary indications and medical devices for a holistic prehabilitation. The HEPAS specialists, encompassing dietitians, nurses, and physiotherapists, would stimulate the orthopaedic crowd to acquire a positive culture of healing in advance, cooperating with the ERAS team to educate towards the adoption of healthy habits in the view of the operation. Furthermore, it is broadly acknowledged that potential reoccurrence after surgery and the odds of developing non-communicable diseases can be countered by eating healthy, keeping active, and taking care of mental health regardless of age, gender, ethnicity, and environmental conditions. A team-based system navigation could be the ideal approach to enhance patient experiences with care.37 The HEPAS staff together with the professionals of the health promotion facility would be able to address the physiological and social determinants that push individuals into the cycle of disease, treatment, and relapse. We can list some limitations of this scenario. First, this conceptual framework is the genuine opinion of the panel experts, who are convinced of its value in relation to the global obligation of orthopaedics. However, it might not be applicable to other surgical specialties, patient populations, or healthcare pathways. Second, community care plans have been already tested39 and have highlighted that potential inequalities, such as the wider determinants of health like access to transport, still need to be resolved to assure patient-centred practices that are globally inclusive.40 Third, despite advancements in telemedicine services there are still-existing barriers like regulation and security. To date, one of the global epidemiological challenges is when to engage the population in health promotion programs and how to tailor the intervention according to individual needs. Future decision makers will need to be able to provide the best care for the right patient at the right time, bearing in mind three things: there is no one size that fits all realities, what worked today may not work tomorrow, and the success of a healthcare implementation depends on the readiness to change of the respective community.23 Feasibility and effectiveness of a system of people are dynamic, and ensuring the integrity and consistency of the path of care will require surveillance (eg, workflow analysis, feasibility analysis, health technology assessment, clinical trials, budgetary evaluation), especially for what concerns long-term economic sustainability.6,36 Nevertheless, improving communications between hospitals, intermediate care services, and primary care is the first necessary and decisive step to build a health system of excellence at sub-national, national, and global level.41
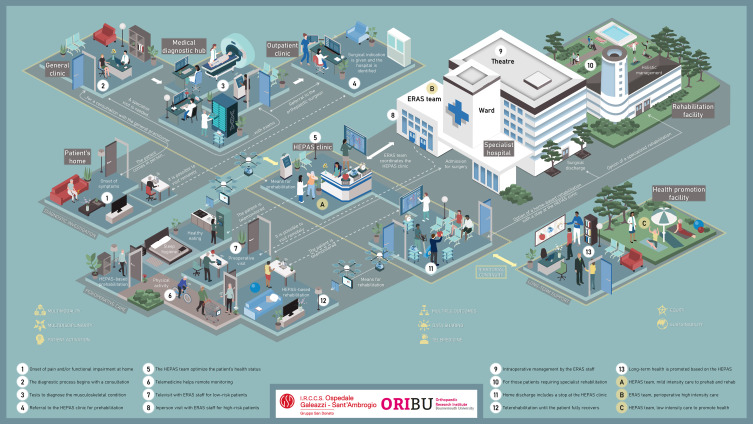
In conclusion, the proposed scenario could take care of the patient before and after the rehabilitation period to proactively give advice on healthy living42 to cope with the natural aging processes of the body and mind. This is what patients are looking for, meaning to have straightforward access to healthcare services, regain independence if treated surgically, overcome eventual mental strains of diseases, and enjoy life as soon as possible and in the long term. What is the point of spending healthcare resources to replace joints and correct spine deformities if we do not empower patients for a long-term lifestyle change? The HEPAS clinic could be a game changer to address the constraints that lead to premature aging of the musculoskeletal system, and we are certain that telehealth will be the means that will change the way orthopaedic care is designed, delivered, and experienced (Figure 1).
Figure 1.
A framework for integrating a health promotion clinic based on the HEPAS principles to develop a health system that takes care for the orthopaedic patient before and after surgery, ensuring that individuals are willing to maintain in the long term the behaviours learned during the perioperative path of care.
Abbreviation: HEPAS, healthy eating, physical activity, sleep hygiene.
Funding Statement
This research was part of the project “Ricerca Corrente” of the Italian Ministry of Health, which funded the APC.
Abbreviations
HEPAS, Healthy Eating, Physical Activity, and Sleep hygiene; ERAS, Enhanced Recovery After Surgery.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.United Nations, Department of Economic and Social Affairs, Population Division. World Population Prospects 2022: Graphs and Profiles; 2022. Available from: https://population.un.org/wpp/. Accessed October 18, 2023.
- 2.Cieza A, Causey K, Kamenov K, Hanson SW, Chatterji S, Vos T. Global estimates of the need for rehabilitation based on the Global Burden of Disease study 2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2021;396(10267):2006–2017. doi: 10.1016/S0140-6736(20)32340-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rullán PJ, Deren ME, Zhou G, et al. The Arthroplasty Surgeon Growth Indicator: a Tool for Monitoring Supply and Demand Trends in the Orthopaedic Surgeon Workforce from 2020 to 2050. J Bone Joint Surg Am. 2023;105(13):1038–1045. doi: 10.2106/JBJS.22.00874 [DOI] [PubMed] [Google Scholar]
- 4.Williams A, Kamper SJ, Wiggers JH, et al. Musculoskeletal conditions may increase the risk of chronic disease: a systematic review and meta-analysis of cohort studies. BMC Med. 2018;16(1):167. doi: 10.1186/s12916-018-1151-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Briguglio M. Nutritional Orthopedics and Space Nutrition as Two Sides of the Same Coin: a Scoping Review. Nutrients. 2021;13(2). doi: 10.3390/nu13020483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Briguglio M, Wainwright TW. Nutritional and Physical Prehabilitation in Elective Orthopedic Surgery: rationale and Proposal for Implementation. Ther Clin Risk Manag. 2022;18:21–30. doi: 10.2147/TCRM.S341953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yap ZL, Summers SJ, Grant AR, Moseley GL, Karran EL. The role of the social determinants of health in outcomes of surgery for low back pain: a systematic review and narrative synthesis. Spine J. 2022;22(5):793–809. doi: 10.1016/j.spinee.2021.11.013 [DOI] [PubMed] [Google Scholar]
- 8.Kamalapathy PN, Dunne PJ, Yarboro S. National Evaluation of Social Determinants of Health in Orthopedic Fracture Care: decreased Social Determinants of Health Is Associated With Increased Adverse Complications After Surgery. J Orthop Trauma. 2022;36(7):e278–e282. doi: 10.1097/BOT.0000000000002331 [DOI] [PubMed] [Google Scholar]
- 9.Mohanty S, Lad MK, Casper D, Sheth NP, Saifi C. The Impact of Social Determinants of Health on 30 and 90-Day Readmission Rates After Spine Surgery. J Bone Joint Surg Am. 2022;104(5):412–420. doi: 10.2106/JBJS.21.00496 [DOI] [PubMed] [Google Scholar]
- 10.Weiser TG, Regenbogen SE, Thompson KD, et al. An estimation of the global volume of surgery: a modelling strategy based on available data. Lancet. 2008;372(9633):139–144. doi: 10.1016/S0140-6736(08)60878-8 [DOI] [PubMed] [Google Scholar]
- 11.Clarkson J, Dean J, Ward J, Komashie A, Bashford T. A systems approach to healthcare: from thinking to -practice. Future Healthc J. 2018;5(3):151–155. doi: 10.7861/futurehosp.5-3-151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Morgan MJ, Stratford E, Harpur S, Rowbotham S. A Systems Thinking Approach for Community Health and Wellbeing. Systemic Practice Action Res. 2023. doi: 10.1007/s11213-023-09644-0 [DOI] [Google Scholar]
- 13.Haldane V, Chuah FLH, Srivastava A, et al. Community participation in health services development, implementation, and evaluation: a systematic review of empowerment, health, community, and process outcomes. PLoS One. 2019;14(5):e0216112. doi: 10.1371/journal.pone.0216112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Briguglio M, Vitale JA, Galentino R, et al. Healthy Eating, Physical Activity, and Sleep Hygiene (HEPAS) as the Winning Triad for Sustaining Physical and Mental Health in Patients at Risk for or with Neuropsychiatric Disorders: considerations for Clinical Practice. Neuropsychiatr Dis Treat. 2020;16:55–70. doi: 10.2147/NDT.S229206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Briguglio M. The Burdens of Orthopedic Patients and the Value of the HEPAS Approach (Healthy Eating, Physical Activity, and Sleep Hygiene). Front Med. 2021;8:650947. doi: 10.3389/fmed.2021.650947 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jönsson T, Eek F, Hansson EE, Dahlberg LE, Dell’Isola A. Factors associated with clinically relevant pain reduction after a self-management program including education and exercise for people with knee and/or Hip osteoarthritis: data from the BOA register. PLoS One. 2023;18(2):e0282169. doi: 10.1371/journal.pone.0282169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zheng F, Zheng Y, Liu S, et al. The Effect of M-Health-Based Core Stability Exercise Combined with Self-Compassion Training for Patients with Nonspecific Chronic Low Back Pain: a Randomized Controlled Pilot Study. Pain Ther. 2022;11(2):511–528. doi: 10.1007/s40122-022-00358-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Briguglio M, Wainwright TW, Crespi T, et al. Oral Hydration Before and After Hip Replacement: the Notion Behind Every Action. Geriatr Orthop Surg Rehabil. 2022;13:21514593221138665. doi: 10.1177/21514593221138665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Briguglio M, Wainwright T, Southern K, Riso P, Porrini M, Middleton R. Healthy eating for elective major orthopedic surgery: quality, quantity, and timing. J Multidiscip Healthc. 2023;Volume 16:2081–2090. doi: 10.2147/JMDH.S415116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tavassoli N, de Souto Barreto P, Berbon C, et al. Implementation of the WHO integrated care for older people (ICOPE) programme in clinical practice: a prospective study. Lancet Healthy Longev. 2022;3(6):e394–e404. doi: 10.1016/S2666-7568(22)00097-6 [DOI] [PubMed] [Google Scholar]
- 21.Godycki-Cwirko M, Panasiuk L, Brotons C, Bulc M, Zakowska I. Perception of preventive care and readiness for lifestyle change in rural and urban patients in Poland: a questionnaire study. Ann Agric Environ Med. 2017;24(4):732–738. doi: 10.26444/aaem/81393 [DOI] [PubMed] [Google Scholar]
- 22.Brotons C, Bulc M, Sammut MR, et al. Attitudes toward preventive services and lifestyle: the views of primary care patients in Europe. the EUROPREVIEW patient study. Fam Pract. 2012;29(Suppl 1):i168–i176. doi: 10.1093/fampra/cmr102 [DOI] [PubMed] [Google Scholar]
- 23.Kehl M, Brew-Sam N, Strobl H, Tittlbach S, Loss J. Evaluation of community readiness for change prior to a participatory physical activity intervention in Germany. Health Promot Int. 2021;36(Supplement_2):ii40–ii52. doi: 10.1093/heapro/daab161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Beutler LE, Someah K, Kimpara S, Miller K. Selecting the most appropriate treatment for each patient. Int J Clin Health Psychol. 2016;16(1):99–108. doi: 10.1016/j.ijchp.2015.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bardach SH, Schoenberg NE. The Role of Primary Care Providers in Encouraging Older Patients to Change Their Lifestyle Behaviors. Clin Gerontol. 2018;41(4):326–334. doi: 10.1080/07317115.2017.1376029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ni W, Yuan X, Zhang Y, Zhang H, Zheng Y, Xu J. Sociodemographic and lifestyle determinants of multimorbidity among community-dwelling older adults: findings from 346,760 SHARE participants. BMC Geriatr. 2023;23(1):419. doi: 10.1186/s12877-023-04128-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liu X, King J, Boak B, et al. Effectiveness of a behavioral lifestyle intervention on weight management and mobility improvement in older informal caregivers: a secondary data analysis. BMC Geriatr. 2022;22(1):626. doi: 10.1186/s12877-022-03315-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cooper Z, Rogers SO, Ngo L, et al. Comparison of Frailty Measures as Predictors of Outcomes After Orthopedic Surgery. J Am Geriatr Soc. 2016;64(12):2464–2471. doi: 10.1111/jgs.14387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ozkalkanli MY, Ozkalkanli DT, Katircioglu K, Savaci S. Comparison of tools for nutrition assessment and screening for predicting the development of complications in orthopedic surgery. Nutr Clin Pract. 2009;24(2):274–280. doi: 10.1177/0884533609332087 [DOI] [PubMed] [Google Scholar]
- 30.Hall K, Gibbie T, Lubman DI. Motivational interviewing techniques - facilitating behaviour change in the general practice setting. Aust Fam Physician. 2012;41(9):660–667. [PubMed] [Google Scholar]
- 31.Boxer H, Snyder S. Five communication strategies to promote self-management of chronic illness. Fam Pract Manag. 2009;16(5):12–16. [PubMed] [Google Scholar]
- 32.Furtado R, MacDermid JC, Ziebart C, Bryant D, Faber KJ. Preoperative Patient Education Programs for Orthopaedic Surgery: what Do the Programs Include? How Are They Delivered? What Are the Knowledge Gaps? A Scoping Review of 46 Studies. J Orthop Sports Phys Ther. 2022;52(9):572–585. doi: 10.2519/jospt.2022.10614 [DOI] [PubMed] [Google Scholar]
- 33.Mills A. Health care systems in low- and middle-income countries. N Engl J Med. 2014;370(6):552–557. doi: 10.1056/NEJMra1110897 [DOI] [PubMed] [Google Scholar]
- 34.Aguirre-Sosa J, Vargas-Merino JA. Telemedicine Management: approaches and Perspectives-A Review of the Scientific Literature of the Last 10 Years. Behav Sci (Basel). 2023;13(3). doi: 10.3390/bs13030255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kristensen FB, Lampe K, Wild C, Cerbo M, Goettsch W, Becla L. The HTA Core Model. Value Health. 2017;20(2):244–250. doi: 10.1016/j.jval.2016.12.010 [DOI] [PubMed] [Google Scholar]
- 36.Briguglio M, Wainwright T. The potential link between dietary factors and patient recovery in orthopedic surgery research. Frontiers in Nutrition. 2023;10. doi: 10.3389/fnut.2023.1195399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Teggart K, Neil-Sztramko SE, Nadarajah A, et al. Effectiveness of system navigation programs linking primary care with community-based health and social services: a systematic review. BMC Health Serv Res. 2023;23(1):450. doi: 10.1186/s12913-023-09424-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Forrester N. From process to outcome: working toward health equity. Nature. 2023. doi: 10.1038/d41586-023-01911-3 [DOI] [PubMed] [Google Scholar]
- 39.Harari D, Hopper A, Dhesi J, Babic-Illman G, Lockwood L, Martin F. Proactive care of older people undergoing surgery (‘POPS’): designing, embedding, evaluating and funding a comprehensive geriatric assessment service for older elective surgical patients. Age Ageing. 2007;36(2):190–196. doi: 10.1093/ageing/afl163 [DOI] [PubMed] [Google Scholar]
- 40.Liu S, Wang B, Fan S, Wang Y, Zhan Y, Ye D. Global burden of musculoskeletal disorders and attributable factors in 204 countries and territories: a secondary analysis of the Global Burden of Disease 2019 study. BMJ Open. 2022;12(6):e062183. doi: 10.1136/bmjopen-2022-062183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chen N, Fong DYT, Wong JYH. Health and Economic Outcomes Associated With Musculoskeletal Disorders Attributable to High Body Mass Index in 192 Countries and Territories in 2019. JAMA Netw Open. 2023;6(1):e2250674. doi: 10.1001/jamanetworkopen.2022.50674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fadnes LT, Økland JM, Haaland Ø, Johansson KA. Estimating impact of food choices on life expectancy: a modeling study. PLoS Med. 2022;19(2):e1003889. doi: 10.1371/journal.pmed.1003889 [DOI] [PMC free article] [PubMed] [Google Scholar]