Abstract
Background:
The burden of heart failure (HF) is unequally distributed among population groups. Few studies have described social determinants of health (SDoH) enabling/impeding self-care.
Aim:
Explore the relationship between SDoH and self-care in patients with HF.
Methods:
Using a convergent mixed-methods design, we assessed SDoH and self-care in 104 patients with HF using the Protocol for Responding to and Assessing Patients’ Assets, Risks, and Experiences (PRAPARE) and the Self-Care of HF Index v7.2 with self-care maintenance, symptom perception, and self-care management scales. Multiple regression was used to assess the relationship between SDoH and self-care. One-on-one in-depth interviews were conducted in patients with poor (standardized score ≤ 60, n=17) or excellent (standardized score ≥ 80, n=20) self-care maintenance. Quantitative and qualitative results were integrated.
Results:
Participants were predominantly male (57.7%), mean age 62.4±11.6 years, with health insurance (91.4%) and some college education (62%). Half were White (50%), many were married (43%), and most reported adequate income (53%). The money and resources core domain of PRAPARE significantly predicted self-care maintenance (p=0.019) and symptom perception (p=0.049) trended significant after adjusting for other PRAPARE core domains (personal characteristics, family and home, and social and emotional health) and Comorbidity. Participants discussed social connectedness, health insurance coverage, individual upbringing, and personal experiences as facilitators of self-care behavior.
Conclusion:
Several social determinants of health influence HF self-care. Patient specific interventions that address the broader effects of these factors may promote self-care in patients with HF.
Keywords: Social determinants of health, Heart failure, Self-care, Mixed Methods
Background and Objectives
Over 8 million Americans are projected to have heart failure (HF) by 2030, reflecting $69.8 billion in annual cost to society by 2030.1 The recent COVID-19 pandemic has highlighted long-standing disparities in HF burden across racial, ethnic, and socioeconomic groups.2 One theory is that social determinants of health (SDoH) influence the development of disease and the ability of individuals to care for themselves after illness develops.3
SDoH refers to the circumstances in which people are born, live, work and age, and the systems put in place to deal with illness.4 Two major domains (structural and intermediate) constitute the SDoH concept. The structural domain includes: (i) socioeconomic and political context determined by governance, macroeconomic, social, and public policies, culture, and societal values, and (ii) socioeconomic position determined by social class, gender, ethnicity/race, education, occupation, and income. The intermediary domain includes (i) material circumstances, reflecting one’s financial capability to obtain and maintain housing in safe neighborhoods, in addition to nutritious foods and warm clothing, (ii) behaviors and biological factors, (iii) psychosocial factors. and (iv) health systems. Differential exposure to structural and intermediate SDoH results in disparate health outcomes. That is, individuals with poor access to health-promoting social determinants have poor health outcomes.5 Self-care may be the mechanism by which social determinants influence health outcomes, but this is not well-studied. Thus, the purpose of this study was to describe the relationship between SDoH and self-care in community-dwelling adults with HF.
Self-care involves a decision-making process that influences actions that maintain physiologic stability and facilitate the perception and management of symptoms.6 Adequate self-care improves HF outcomes; patients with better self-care behaviors have fewer symptoms and improved overall well-being.7,8 Persons with HF who lack access to basic resources, education, employment, social and healthcare services may have competing needs that limit their choices and decisions about self-care.9 Therefore, finding ways to improve self-care in persons experiencing the negative effects of SDoH is anticipated to improve HF outcomes.
Few studies have assessed individual-level SDoH that enable or impede HF self-care. For instance, social support is known to contribute to better HF self-care.10–12 Racial differences exist in the clinical treatment and the self-care behavior of adults with HF,13 and income is known to be a risk factor for poor self-care.14 Others have also found an association between education, income, and diabetes self-care in the US population.15 Demographic variables such as education, age, and marital status have not only been found to be associated with HF self-care,16 but also self-care actions in end-of-life planning among older adults.17 To our knowledge, no study has comprehensively explored the relationship between SDoH broadly defined and HF self-care. Hence, we investigated the relationship between SDoH broadly defined and HF self-care in community dwelling adults with a recent HF exacerbation by addressing three specific aims. In aim 1, we described the relationship between SDoH and HF self-care behavior quantitatively. For aim 2, we explored participants’ perceptions, beliefs, and experiences surrounding SDoH and their self-care behavior using the Gibbs reflective cycle in qualitative interviews. We then integrated the quantitative and qualitative results to describe differences and similarities in the self-reported SDoH in relation to participants’ self-care behavior in aim 3. Our findings identify elements that can be addressed in targeted interventions.
Conceptual Model: The Social Determinants of Health Behavioral Model
The SDoH framework developed by the World Health Organization (WHO) Commission on SDoH posits that public policies and cultural norms shape one’s living and working conditions.4 The level of interaction with mainstream society defines the availability, accessibility, affordability, and equity within the community for the resources required for adequate self-care. This framework focuses on socioeconomic position as an essential component of SDoH and emphasizes the inequities that can exist at a particular socioeconomic position. These inequities shape experience and create disparate health outcomes. Socioeconomic position can be conceptualized as the prestige and resource-based status in society that determine access to health promoting resources.18 Hence, factors that shape socioeconomic position include but are not limited to gender, race, sexual orientation, occupation, education, and material circumstances. These factors produce differential exposure to health determining factors such as nutritional deficiency, hazardous working conditions, and residentially segregated neighborhoods that result in unhealthy self-care behaviors.19
Conversely, the revised Behavioral Model for Vulnerable Populations by Gelberg and colleagues9 theorizes that the use of healthcare services is a function of one’s predisposition to use services, factors that enable/impede that use, and the need for care. This model recognizes not only the dynamic nature of human behavior, but also the factors that predispose one to use resources and influence behavior (e.g., self-care). The model has two domains: traditional and vulnerable. Each domain is subcategorized into predisposing, enabling, and need characteristics that predict health behavior. While the vulnerable domain focuses on social structure and enabling resources, the traditional domain emphasizes demographic characteristics. Based on these categories, authors of the theory suggest that demographic characteristics (e.g., age, race, and gender) intersect with sociodemographic factors such as education, employment, and acculturation to differentially predispose an individual to use health care services.9
Integrating these two theories in the context of HF highlights the core domains of SDoH as predisposing and enabling/impeding factors that affect HF self-care (figure 1). Inequity in access creates differences in HF self-care choices between individuals of unequal socioeconomic position. We theorize that SDoH exert their influence on HF self-care through a lack of access to resources and the experiences associated with navigating the availability, accessibility, and affordability of resources. At a specific socioeconomic position, access to health promoting resources influences the choices available for adequate self-care.
Figure 1:
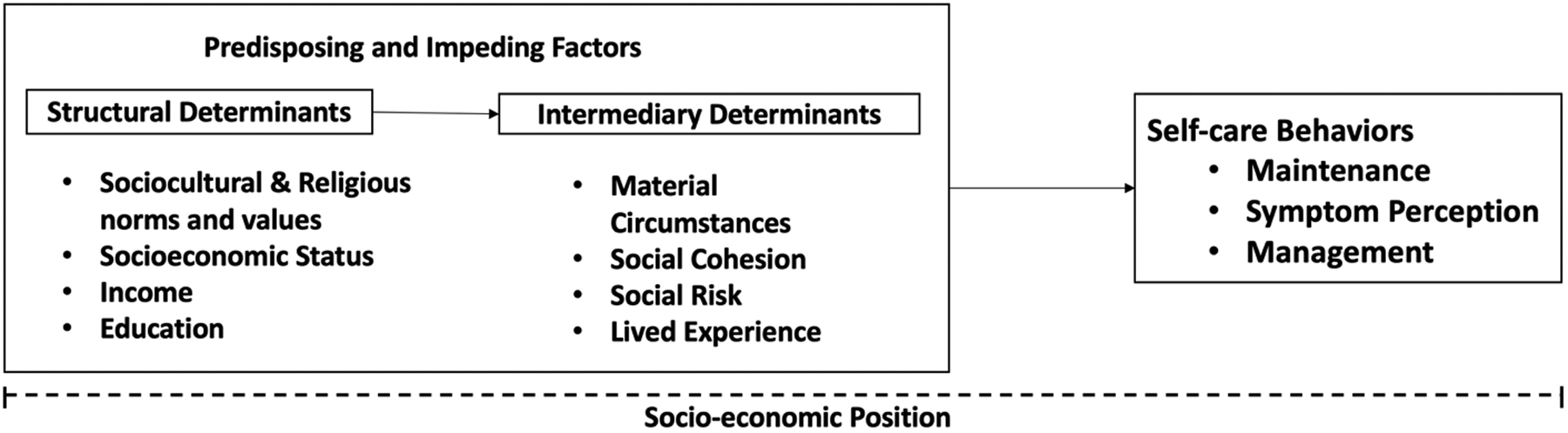
Social determinants of self-care behavior
Patients with HF perform their self-care behaviors within the context of their person specific SDoH. The Core domains of social determinants serve as predisposing or enabling factors affecting self-care behavior. Inequity and disparities in access creates differences in self- care choices between individuals of unequal socioeconomic position.
We conceptualize patient vulnerabilities in this manner to highlight the individual’s external health capability or the situational conditions that enable/impede optimal health.20 For instance, a patient with HF who has poor access to basic resources may have difficulty adhering to self-care behaviors such as exercising routinely, eating a low salt diet, and taking prescribed medications. Hence, we operationalize socioeconomic position as a relative position in society that determines an individual’s status, experiences, and access to both health promoting and basic resources that improve survivability.21
Research Design and Methods
We conducted a cross-sectional, convergent mixed-methods study22 with priority given to the quantitative study arm (QUAN + qual). Following Institutional Review Board approval, we enrolled a consecutive sample of community dwelling adults with HF from cardiac intermediate care settings in two university hospitals and one Program for All-inclusive Care for the Elderly (PACE) in the Northeastern US. These diverse sites serve as catchment centers for stable community dwelling patients with a recent HF exacerbation. Most exacerbations are due to lapses in self-care behaviors such as nonadherence to medications,23 so this approach allowed us to explore the circumstances surrounding the self-care behaviors leading to the exacerbation. We defined a recent HF exacerbation as a current admission or an admission within the past 30 days with HF as the admitting diagnosis. All participants provided written informed consent. We collected data on demographics, SDoH, and self-care behavior. A subset of participants was selected for interview based on their self-care maintenance scores as described below.
Sampling
We included English-speaking community dwelling adults (age ≥18 years) with any type of HF because self-care is required of all HF patients; it does not differ by HF type. We excluded patients who were clinically unstable, cognitively impaired (Montreal Cognitive Assessment [MoCA] ≤22)24 and anyone with an active, untreated psychiatric illness.
We anticipated recruiting 108 patients for the quantitative arm of the study. This sample size was adequate to test seven independent variables while controlling for nine other variables with a power of .80 and a medium effect size (R2 = .15) at an alpha of .05 (PASS V15.0.03, NCSS, Kaysville, UT). In March 2020, all nonessential research ceased due to COVID-19. At that point, 104 patients had completed the study, so we ended recruitment. For the qualitative arm, we anticipated interviewing two groups of 20 patients each based on their self-care maintenance scores. Prior to ending enrollment, 37 patients had been interviewed. Extreme case sampling was used to identify the two groups of participants for interview: 1) Poor Self-care Maintenance (maintenance score ≤ 60; n = 17) and 2) Excellent Self-care Maintenance (maintenance score ≥ 80; n = 20. Because we sought to explore the experiences of extreme cases, we did not seek saturation, but rather diversity in experiences of our identified cases. We also employed maximum variability based on age and gender. According to the 2010 census, the County where we recruited is racially diverse so we anticipated that about 40% of our study sample would be Blacks or African Americans and 6% would be of mixed race. We monitored enrollment biweekly to ensure adequate inclusion of women and minorities in the study.
Measurement
Self-care was measured with the Self-Care of Heart Failure Index (SCHFI v7.2), a disease-specific 29-item self-report instrument with three scales measuring Self-Care Maintenance, Symptom Perception, and Self-Care Management.25 Each scale uses a 5-point Likert scale and is scored separately, with scores standardized 0–100 (≥70 reflects adequate self-care).25 The SCHFI v7.2 also includes a 10-item measure of self-care self-efficacy or confidence, an important factor influencing HF self-care. The SCHFI v7.2 has demonstrated adequate factorial and predictive validity with internal consistency and reliability.25
SDoH were assessed using the Protocol for Responding to and Assessing Patients’ Risk and Experiences (PRAPARE), a tool kit developed to standardize the collection of patient-specific data on SDoH.26 The PRAPARE is a 21-item instrument with 17 items representing 4 core SDoH domains that align with Healthy People 2020 and the Center for Disease Control and Prevention’s agenda for prioritizing SDoH in health centers.27 The 4 core domains include: Personal Characteristics (5 items capturing ethnicity, race, history of seasonal or migrant farm work, veteran status, and English language proficiency), Family and Home (4 items capturing information on neighborhoods, housing status, and housing stability), Money and Resources (6 items capturing education, employment, insurance status, income, material circumstance and transportation needs), and Social and Emotional Health (2 items capturing social integration and stress). The four optional items capture incarceration history, refugee status, perceived physical and emotional safety, and domestic violence.
The PRAPARE is scored by assigning a maximum of 1 point (tally) for every SDoH risk present or 0 for the absence of risk with two exceptions.28 The first of the two exceptions is item 14, which captures material circumstance (minimum of 0 indicating the absence of risk and a maximum of 7 indicating the presence of 7 risks) reflecting unmet resources such as food, clothing, and medicine. The second exception is item 15, which captures transportation needs (minimum of 0 indicating the absence of risk and a maximum of 2 points indicating 2 risks relating to transportation needs). Hence, the possible range of scores for the 17 items representing the 4 core domains is 0–22, with higher points indicating a higher number of SDoH risks.29,30 Although PRAPARE was not developed as a research instrument, it is being used as such, as well as by clinicians as a screening tool.31 During development, Cronbach’s alpha coefficient was 0.86.29 The items have face validity.
Sociodemographic variables were collected by self-report. Comorbidity information was derived using the chart review version of the Charlson Comorbidity Index.32 All quantitative data were entered into REDCap, cross validated with survey forms, de-identified, and exported into the Statistical Analysis System (SAS v9) (SAS Institute, Cary, NC) for analysis.
Procedures
The lead author reviewed the charts of potential participants to identify eligible patients, introduced the study, and invited them to participate in the study. Those who agreed were consented and screened for cognitive impairment (Figure 2). Those who passed the cognitive screening were enrolled into the quantitative arm of the study and completed the survey using paper and pencil. Completion of the survey required 15 to 30 minutes.
Figure 2:
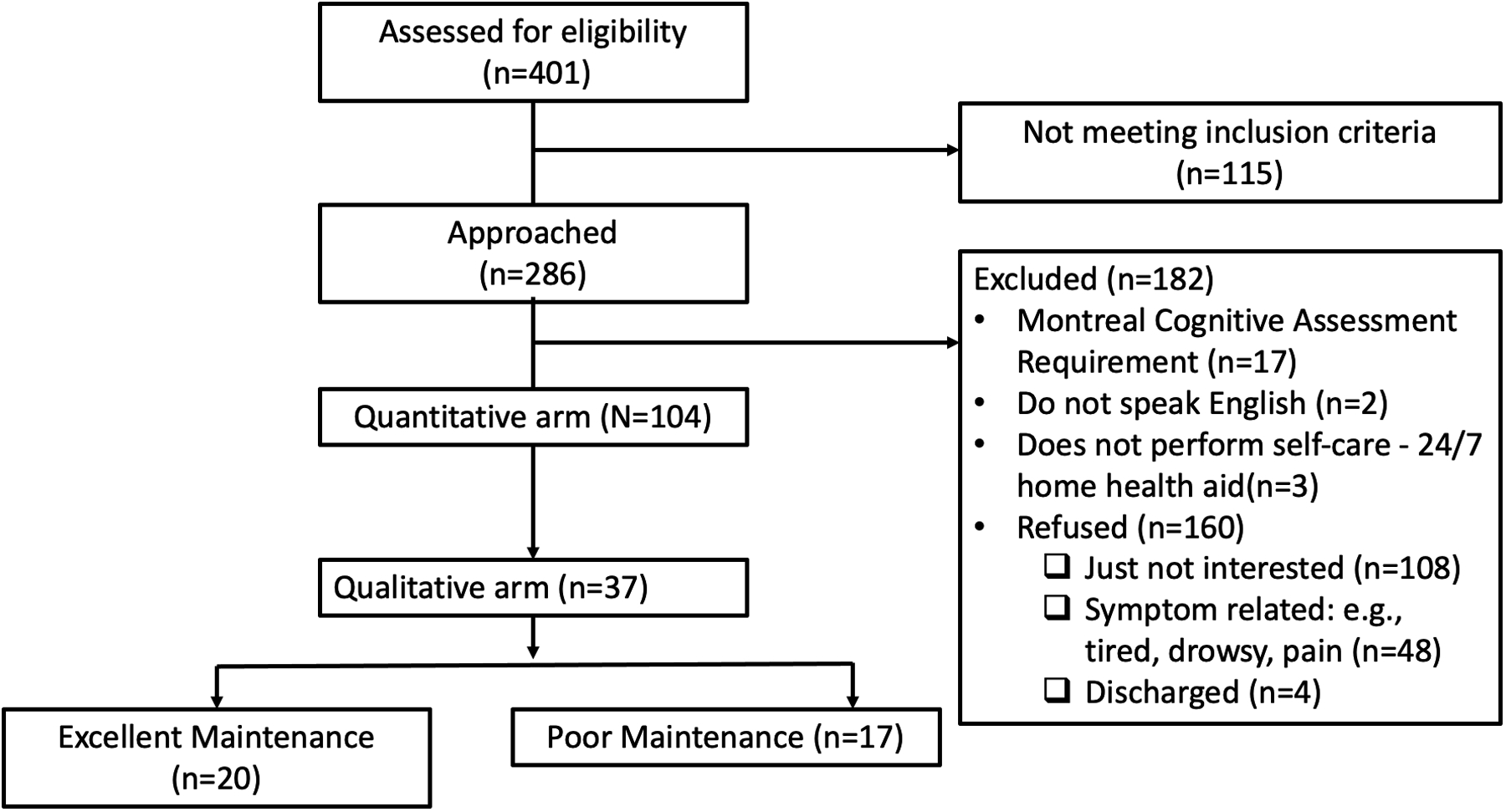
Consort flowchart of enrollment
Flow diagram of participant enrollment showing exclusion criteria
We selected participants for interview based on their Self-Care Maintenance scores because self-care maintenance includes behaviors that reflect HF treatment adherence. Once a participant completed the survey, the scale was scored before offering the opportunity to be interviewed. We also ensured that the poor and excellent self-care maintenance groups included an approximately equal distribution of participants by race and gender. Those who agreed to the interview consented to audiotaping of the interview.
Interviews
Interviews were guided by the Gibb’s Reflective Cycle, an approach used in experiential learning.33 The cycle has six phases: Description, Feelings, Evaluation, Analysis, Conclusion, and Action Plan. Structured questions (Supplemental table 1) were used as prompts to stimulate reflection on experiences. Participants were asked to retrospectively describe a specific experience, identify their reactions and feelings, evaluate the experience, and analyze the situation. During the two final phases of the cycle, participants were prompted to make both general and specific conclusions and suggest an action plan for future experiences. All interviews were conducted by the lead author immediately following survey administration in the patient’s hospital room or scheduled for a later date and time. Only one interview was conducted at the patient’s home after discharge. Interviews lasted an average of 40 minutes and were transcribed verbatim.
Analysis
Descriptive statistics were used to analyze the demographic, PRAPARE, and self-care data. Results were displayed using tables and graphs to illustrate means, standard deviations, medians, interquartile ranges, frequencies, and percentages. Total PRAPARE scores and PRAPARE core domains (e.g., personal characteristics, family and home, money and resources, and social and emotional health) were analyzed as continuous variables.
We conducted bivariate analyses between the total PRAPARE score and the PRAPARE core domains to assess their relationship with the self-care scores using Pearson correlations. All 4 PRAPARE core domains and the comorbidity index were considered as predictors of HF self-care in regression model building. We employed the multiple regression approach to identify which PRAPARE core domains were significant predictors of HF self-care instead of a variable selection approach.34 First, we built four separate unadjusted regression models using each of the self-care constructs as outcome variables and PRAPARE core domains as predictors. Statistically significant models were subsequently adjusted for comorbidity.
Qualitative data analysis
We employed directed content analysis35 to explore participants’ perceptions, beliefs and experiences surrounding SDoH and their self-care choices. Atlas.ti v8 (Berlin, Germany) was used for coding. Directed content analysis allowed us to use a combined inductive and deductive approach to develop codes. Guided by our conceptual framework, we began by developing a priori codes from the SDoH core measures (personal characteristics, family and home, money and resources, and social and emotional health) and HF self-care constructs (e.g., self-care maintenance).
During the initial coding process, we derived in-vivo codes from the line-by-line coding review of the data. The codebook was revised iteratively, and new codes were subsequently applied to previously coded transcripts. The codes were then sorted, and related codes grouped into clusters. We assessed the degree of recurrence and importance of codes during the process of sorting into clusters and themes. This technique allowed us to include unique, non-recurrent codes36 that were important and to develop themes from related code clusters.37 We extracted both latent and manifest content from the data38 to qualitatively explore participants’ perceptions, beliefs, and experiences beyond the SDoH and self-care constructs.
Trustworthiness and Reliability
The research team held bi-weekly peer debriefing sessions to discuss the data and resolve issues. At these meetings we discussed codes and themes with experts in SDoH, HF self-care, and health equity to maximize credibility and reliability.39 All codes and themes were reviewed by BMB, a mixed methods research expert. Before coding began, transcribed interviews were read thoroughly and repeatedly for in-depth understanding and familiarity with the data. A co-coder independently coded four transcripts (11% of the total sample). We discussed coding differences until a consensus was reached and a percent agreement of 90%40 was achieved. The interview guide was revised based on preliminary findings, which were confirmed in subsequent interviews in our sample.
Integration of Quantitative and Qualitative Data
In our final step, we integrated the quantitative and qualitative data using triangulation to identify patterns of convergence, differences, mutual corroboration, and validation of our quantitative and qualitative data.41 First, we used a joint display table (Supplemental table 2) to merge the data sets, anchoring the qualitative SDoH data on the self-care maintenance scores of the two interviewed groups. The created codes, themes, SDoH and self-care results were then added to the display table for analysis. We performed within case, across case, and within and between group comparisons on the jointly displayed data to identify patterns of differences or convergence in self-reported SDoH in relation to participants’ self-care maintenance scores.
Rigor in mixed method research is tied to the validity of the quantitative arm and the trustworthiness of the qualitative components.22 We ensured credibility, dependability, confirmability, and transferability by employing sound methods of study design and participant selection.39 We maintained an audit trail and employed prolonged engagement during data collection to establish credibility with detailed descriptive field notes and memos of observations during the interview. We documented in detail any changes in methodology, analytic strategy, issues that arose from team member debriefings, and how those issues were addressed.
Results
The sample (Table 1) was predominantly male (57.7%) with a mean age of 62.4±11.6 years. Half were White (50%), many were married (43%), and most reported an adequate income (53%). The majority had health insurance (91.4%) and some college education (62%). The range of PRAPARE risk tallies was 1–15 with a mean of 4.9±2.8, indicating a low number of risks for poor SDoH in our sample. Though self-care maintenance (71.7±17.9) and self-care self-efficacy (78.7±15.8) were adequate based on the mean scores, symptom perception (69.9±15.5) and self-care management (69.4±18.8) were marginally inadequate. There were no statistically significant differences in demographic characteristics between the two interview groups (Table 2).
Table 1:
Quantitative Sample Characteristics
| Participant Characteristics | Total Sample (Mean±SD or n [%]) |
|---|---|
| Age | 62.41±11.60 |
| • Age ≤ 64 | 58 (55.8) |
| • Age ≥ 65 | 46 (44.2) |
| Gender | |
| • Male | 60 (57.69) |
| • Female | 44 (42.31) |
| Race | |
| • White | 53(50.96) |
| • Black/African American | 41(39.42) |
| • Other (Mixed Race, Hispanic, Native American, Pacific Islander, American Indian/Alaskan Native) | 10 (9.62) |
| Education | |
| • More than High school | 63(60.58) |
| • High School or less | 41(39.42) |
| Public Assistance | |
| • Yes | 22(21.15) |
| • No | 82(78.85) |
| Incarceration History | |
| • Yes | 7 (6.73) |
| • No | 97(93.27) |
| Physical & Emotional safety | |
| • Yes | 100(96.15) |
| • No | 3(2.88) |
| • Do not know | 1(0.96) |
| Veteran | |
| • Yes | 15 (14.42) |
| • No | 89 (85.58) |
| Health Insurance Coverage | |
| • Health Insurance all the time | 95(91.35) |
| • Had time without insurance | 7(6.73) |
| • Do not know | 1(0.96) |
| Main Insurance | |
| • Private | 40 (38.46) |
| • Medicare/Medicaid | 54 (51.93) |
| • Other Public Insurance | 7 (6.73) |
| • Uninsured | 3 (2.88) |
| Social Integration | |
| • Less than once a week. | 7(6.73) |
| • 1 or 2 times a week. | 29(27.88) |
| • 3 to 5 times a week | 26(25.00) |
| • 5 or more times a week | 42(40.38) |
| Stress level | |
| • Not at all | 18(17.31) |
| • A little bit | 31(29.81) |
| • Some what | 28(26.92) |
| • Quite a bit | 12(11.54) |
| • Very Much | 15(14.42) |
| Housing Situation | |
| • I have housing | 100(96.15) |
| • I do not have housing | 4(3.85) |
| Income Adequacy | |
| • Comfortable | 53(50.96) |
| • Just Enough | 31(29.81) |
| • Not enough to make ends meet | 18(17.31) |
| • Refused | 2 (1.92) |
| Marital Status | |
| • Single | 36(34.62) |
| • Married | 43(41.35) |
| • Divorced/Widowed/Separated | 25(24.04) |
Table 2:
Qualitative Sample Characteristics
| Participants Characteristics | Excellent Self-care Maintenance (n=20 [%]) | Poor Self-care Maintenance (n=17[%]) | Chi square p value |
|---|---|---|---|
| Age (61.72 ± 10.25) | |||
| • Age ≤ 64 | 9 (45) | 12 (70.59) | 0.069 |
| • Age ≥ 65 | 11 (55) | 5 (29.41) | |
| Gender | |||
| • Male | 9 (45) | 12 (70.59) | 0.117 |
| • Female | 11 (55) | 5 (29.41) | |
| Race | |||
| • White | 12 (60) | 6 (35.29) | 0.324 |
| • Black/African American | 6 (30) | 8(47.06) | |
| • Other (Mixed Race, Hispanic, Native American, Pacific Islander, American Indian/Alaskan Native) | 2 (10) | 3 (17.65) | |
| Education | |||
| • More than High school | 5 (25) | 6(35.29) | 0.495 |
| • High School or less | 15 (75) | 11(64.71) | |
| Public Assistance | |||
| • Yes | 4 (20) | 3 (17.65) | 0.856 |
| • No | 16 (80) | 14 (82.35) | |
| Incarceration History | |||
| • Yes | 1 (5) | 1 (5.88) | 0.539 |
| • No | 19 (95) | 16 (94.12) | |
| Physical & Emotional Safety | |||
| • Yes | 19 (95) | 17 (100) | 0.350 |
| • No | 1 (5) | 0 | |
| Veteran | |||
| • Yes | 2 (10) | 1 (5.88) | 0.272 |
| • No | 18 (90) | 16 (94.12) | |
| Health Insurance Coverage | |||
| • Health Insurance all the time | 18 (90) | 15 (88.24) | 0.504 |
| • Had time without insurance | 1 (5) | 2 (11.76) | |
| • Do not know | 1 (5) | 0 | |
| Main Insurance | |||
| • Private | 13 (65) | 10 (58.82) | 0.287 |
| • Medicare/Medicaid/Public | 7 (35) | 5 (29.42) | |
| • Uninsured | 0 | 2 (11.76) | |
| Social Integration | |||
| • Less than once a week. | 1 (5) | 2 (11.76) | 0.691 |
| • 1 or 2 times a week. | 9 (45) | 5 (29.41) | |
| • 3 to 5 times a week | 3 (15) | 4 (23.53) | |
| • 5 or more times a week | 7 (35) | 6 (35.29) | |
| Stress level | |||
| • Not at all | 7 (35) | 3 (17.65) | 0.377 |
| • A little bit | 2 (10) | 6 (35.29) | |
| • Some what | 4 (20) | 4 (23.53) | |
| • Quite a bit | 2 (10) | 1 (5.88) | |
| • Very Much | 5 (25) | 3 (17.65) | |
| Housing Situation | |||
| • I have housing | 19 (95%) | 16 (94.12%) | 0.906 |
| • I do not have housing | 1 (5%) | 1 (5.88%) | |
| Income Adequacy | |||
| • Comfortable | 11 (55) | 9 (52.94) | 0.995 |
| • Just Enough | 5 (25) | 4 (23.53) | |
| • Not enough to make ends meet | 3 (15) | 3 (17.65) | |
| • Refused | 1 (5) | 1 (5.88) | |
| Marital Status | |||
| • Single | 4 (20) | 6 (35.29) | 0.0467 |
| • Married | 6 (30) | 9 (52.94) | |
| • Divorced/Widowed/Separated | 10 (50) | 2 (11.76) | |
Aim 1- Quantitative Aim: Relationship between SDoH and HF self-care
In bivariate analysis, the total PRAPARE tally revealed a significant positive correlation with symptom perception (r=0.25, p=0.01) but the correlation with self-care maintenance (r=0.18, p=0.07) trended significant. There was no significant correlation between the total PRAPARE score and self-care management or self-care self-efficacy or confidence scores.
When we assessed the bivariate relationship between the four PRAPARE core domains (personal characteristics, family and home, money and resources, and social and emotional health) and self-care, only the money and resources core domain (including education, employment, insurance type, transportation, and federal poverty level) was significantly and positively correlated with self-care: maintenance (r=0.30, p=0.002) and symptom perception (r=0.27, p=0.005). There was no statistically significant correlation between the remaining PRAPARE core domains and HF self-care.
In the regression analyses (Table 3), when we used self-care maintenance as an outcome variable, the unadjusted model explained 10.95% of the variance and only the money and resources PRAPARE core domain (p=0.003) was statistically significant. When we adjusted for comorbidity, the model explained 17.4% of the variance in self-care maintenance and only the money and resources PRAPARE core domain (P=0.019) remained statistically significant.
Table 3:
Regression models for self-care maintenance and symptom perception
| Adjusted and Unadjusted Regression models (*significance at p<0.05, **significance at p<0.01) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Self-care Maintenance | ||||||||
| Predictors | Unadjusted - Model 1 | Adjusted (Age and Comorbidity) - Model 2 | ||||||
| Estimate | Standard Error | t value | p value | Estimate | Standard Error | t value | p value | |
| PRAPARE Personal Characteristics | − 2.758 | 2.847 | − 0.969 | 0.336 | −3.245 | 2.790 | −1.163 | 0.248 |
| PRAPARE Family & Home | − 1.866 | 5.490 | − 0.340 | 0.735 | −0.109 | 5.490 | −0.020 | 0.984 |
| PRAPARE Money & Resources | 3.214 | 1.058 | 3.038 | 0.003** | 2.599 | 1.082 | 2.403 | 0.019* |
| Social & Emotional Health | −1.283 | 2.649 | −0.485 | 0.629 | −2.402 | 2.634 | −0.912 | 0.365 |
| Comorbidity (ref. Severe) | ||||||||
| Mild | - | - | - | - | −5.220 | 5.369 | −0.972 | 0.334 |
| Moderate | - | - | - | - | 4.926 | 5.052 | 0.975 | 0.332 |
| R Squared = 0.1095: F=2.552, P=0.0449* | R Squared = 0.1737: F=2.839, P=0.0147* | |||||||
| Self-care Symptom Perception | ||||||||
| PRAPARE Personal Characteristics | 3.685 | 3.066 | 1.202 | 0.233 | 3.942 | 3.051 | 1.292 | 0.200 |
| PRAPARE Family & Home | − 0.599 | 5.911 | − 0.101 | 0.920 | 1.859 | 6.003 | 0.310 | 0.758 |
| PRAPARE Money & Resources | 2.961 | 1.139 | 2.600 | 0.011* | 2.367 | 1.183 | 2.002 | 0.0487* |
| Social & Emotional Health | −1.568 | 2.852 | −0.550 | 0.584 | −2.394 | 2.880 | −0.831 | 0.4082 |
| Comorbidity (ref. Severe) | ||||||||
| Mild | - | - | - | - | −11.189 | 5.871 | −1.906 | 0.0602 |
| Moderate | - | - | - | - | −7.700 | 5.524 | −1.394 | 0.1671 |
| R Squared = 0.1207: F=2.848, P=0.0289* | R Squared = 0.1585: F=2.542, P=0.0263** | |||||||
Using symptom perception as the outcome variable, the unadjusted model explained 12.1% of the variance and only the money and resources PRAPARE domain (p=0.011) was statistically significant. After adjusting for comorbidity, the model explained 15.9% of the variance in symptom perception and only the money and resources PRAPARE domain (p=0.049) was statistically significant.
The unadjusted models for self-care management (p=0.23) and self-care confidence (p=0.63) were not statistically significant (table 4). Hence, none of the PRAPARE core domains were significant predictors of self-care management or confidence.
Table 4:
Regression models for self-care management and confidence
| Regression Models of PRAPARE Core Domains & Self-care Maintenance and Confidence (*significance at p<0.05, **significance at p<0.01) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Self-care Management | Self-care Confidence | ||||||||
| Predictors | Estimate | Standard Error | t value | p value | Estimate | Standard Error | t value | p value | Estimate |
| PRAPARE Personal Characteristics | − 0.745 | 2.627 | − 0.284 | 0.777 | − 2.605 | 2.503 | − 1.041 | 0.301 | − 2.605 |
| PRAPARE Family & Home | − 7.159 | 5.064 | − 1.414 | 0.161 | 2.929 | 4.827 | 0.607 | 0.546 | 2.929 |
| PRAPARE Money & Resources | 1.631 | 0.976 | 1.671 | 0.099 | −0.971 | 0.930 | −1.044 | 0.300 | −0.971 |
| Social & Emotional Health | −3.466 | 2.444 | −1.419 | 0.160 | 0.473 | 2.329 | 0.203 | 0.840 | 0.473 |
| R Squared = 0.065: F=1.438, P=0.229 | R Squared = 0.030: F=0.652, P=0.627 | ||||||||
Aim 2 – Qualitative Aim: Beliefs, perceptions and experiences surrounding SDoH domains and HF self-care
We identified three major themes or factors influencing self-care choices in this community dwelling sample: 1) Social connectedness influences self-care behavior, 2) Individual upbringing and personal experiences influence self-care choices, and 3) Health insurance coverage enhances access to care. These three themes are discussed below.
Social connectedness influences self-care behavior:
Many participants reported that connectedness to their family, community, and health professionals had a major influence on their self-care behavior. The nature of the support they received through these connections helped them in two important ways: 1) to navigate both healthcare and social services, and 2) by facilitating adherence to their HF discharge plans. A 59-year-old Puerto Rican man explained, “I am lucky… I got the network of other people that, if it weren’t for them, I don’t know where I would be…” (poor self-care maintenance [SCM]). He further explained “my family lives in the area, so, we are pretty close… We all live with each other, so no matter what, we all take care of each other”. A 77-year-old White woman also explained, “If I needed anything, I don’t have to go, I can get somebody else to get it for me… I have a good friend that will take me wherever I have to” (excellent SCM). Regarding adherence to discharge plans, a 60-year-old White man shared that, although he sometimes perceives his wife’s constant reminders of what not to eat as “nagging”, he appreciates her for it, stating:
“my wife can be the biggest nag in the world and she only means well… “you can’t have that, or that much salt in it,” … “you sure you want to eat that, that sounds awfully salty.” Yeah it does, alright I will put it down… “did you take your pills? Did you do your nebulization treatment, did you do this? Have you done this today?” stuff like that constantly and I appreciate her for it”.
(excellent SCM)
Several participants expressed that support from healthcare professionals was important in facilitating access to healthcare and adherence to the plan of care. A 50-year-old mixed-race man shared his experience of navigating the healthcare system and social services by stating that he gains access to resources through his caseworker: “…they provide me with information and if I can’t get there, if I don’t have transportation, they will provide me with transportation” (excellent SCM).
Others expressed that support from nurses and reminders from staff through phone calls, in addition to consistent check-ins, made them become like family. For instance, a 67-year-old Black man recounted:
“I had no doctor. No primary … I have a primary care doctor now, and I got a support system, medical support system… they going to check on me. They going to call me at home, send me a case worker… and they going to make me part of their family.”
(poor SCM)
A 72-year-old Black woman also explained her relationship to her nurse by stating that “she helped me a lot when I was here the first time… I adopted the nurse, my nurse because she is always so nice to me… I call her my blue-eyed daughter…” (excellent SCM).
These social connections provided a safe space to decrease stress, develop a sense of belonging, and share information about health and social resources. For instance, a 69-year-old Black participant shared that, shipments of fresh fruits and vegetables are often provided to her church members for free. She explained that those acts of kindness by the church “helps a lot” (excellent SCM, female). When asked specifically about how beliefs and perceptions surrounding living/personal conditions influence HF self-care, a 42-year-old White woman explained,
“I mean spiritually, I believe in Christ, and we go to church, and I pray every day…, I think maybe that’s helped a little bit with my mindset and not being so scared…, I think that helps me calm down at times… the different people at our church, … the pastor, and just my family and everybody else around”.
(poor SCM)
Conversely, participants who were unable to integrate into society lacked this social connectedness and expressed loneliness, isolation, and difficulty accessing social resources and healthcare services. For instance, a 63-year-old White man who was previously incarcerated was repeatedly denied work from multiple places despite not seeking compensation. This participant described his unique experience of trying to reintegrate into society after release from prison.
“…there was a church across my street … told them I was in prison for armed robbery as a kid …, I could come wash your toilets every Sunday a couple of hours, do whatever for nothing, just something to give back and they said …,“we don’t think so”. There is another church down the way…, they said “nah, I am sorry we can’t”… Then I went to Habitat for humanity, said I wanted to help do something, I don’t want no money, just to help, I couldn’t because there are 3 people they don’t take there, child molesters, cats that sell drugs in front of a school and violent criminals. I was a violent criminal with armed robbers, so I couldn’t help there either. So, at that point I was like well, f**k them, f**k them all, I was angry (starts sobbing)… I tried though … I got off parole and I felt getting edged out”.
(poor SCM)
Individual upbringing and personal experiences influence self-care choices:
Several participants discussed the effect of their upbringing and personal experiences on their self-care behavior. They explained that their upbringing had influenced their taste preferences and current food choices, which influenced the ability to adhere to the prescribed diet. A 78-year old White participant recounted, “I guess it’s culture. It’s what you’re used to and it’s very hard to change” (excellent SCM). A 56-year-old Black woman explained, when asked about religious or cultural preferences for specific types of food, “… religiously, I don’t have special foods… Just go by what we have been eating from the time we were little” (poor SCM). A 42-year-old White woman stated, “…other than like country cooking and growing up…, making sure there is potatoes and vegetables at dinner, I don’t really have anything culturally” (poor SCM). This participant further explained that country cooking is “like comfort food. Like the chicken pot pie and mashed potatoes, meatloaf and stuff like that.”
Participants expressed that their food preferences are comfort measures that provide an escape from stress. A 67-year old Black woman stated, “…sometimes I’m so stressed out. It’s like food could be a comfort”(excellent SCM). A 43-year-old White man explained, “I yearn for that taste that takes me back to childhood where I didn’t have the stress and stuff that I have now” (excellent SCM). The cost of food, in addition to life circumstances, shaped perceptions surrounding these comfort foods. When asked specifically about why those foods were eaten while growing up, a 43-year-old White man explained,
“…that’s not what they (parents) asked us to eat, that’s what they will make for us to eat, because it was cheap for them to make…we had five kids in our family and our parent weren’t the richest. So, they need cheap meals…frozen hamburgers…McDonald’s food…it was a lot cheaper for them to do it that way than to actually go out and make a healthy meal for us”.
(excellent SCM)
Other participants explained that they ate comfort foods as a matter of convenience. A 60-year-old Black man shared his everyday experience of making decisions regarding food choices while running a shoe store.
“I was eating fast food across the street every day because it was convenient… shoe store here, pizza shop is across the street, Chinese store…up there…soul food down the street…you are even rushing to hurry up and get back to work. So, you are not really conscious of the best thing for you…”.
(poor SCM)
Health insurance coverage enhances access to care:
Health insurance coverage was another major determinant of HF self-care behavior. A 71-year-old White woman explained,
“…the only thing that ever limited my access to healthcare was the insurance company…, my cardiologist wanted me to have an echocardiogram and the insurance company would not allow it because it was still within a 12-month time. Also, my cardiologist wanted me to go into a study…and the insurance company would not allow it because it is an investigational program and not authorized…”.
(excellent SCM)
When asked how balancing other expenses with the co-payments influenced her self-care decisions, this participant further explained “I got to pay it if I want to live”. Insurance co-payment requirements were a major concern that influenced access to care. A 46-year-old Black woman who identified as previously homeless and currently living on a very tight budget stated, “I don’t think we should have co-payments” (excellent SCM), explaining: “…it might be petty, it is like $3.20…, and then you got to pay a dollar something else and two dollars here. … that just adds up and takes money out of my pocket”. Employment facilitated access to healthcare coverage and the lack of insurance raised major concerns about the affordability of care, medications, and the type of care received. A 57-year-old White man stated:
“… it’s not financial, it’s not how much you make. It is the benefit you are given as part of a job. … I have medical insurance because of my job that in no way limits me”.
(excellent SCM)
Aim 3 – Integrative Aim: Integrating qualitative and quantitative findings on SDoH and self-care
Both quantitative and qualitative results provided evidence that the PRAPARE core domain of money and resources (including education, employment status, health insurance, federal poverty level, material circumstance and transportation) was a major determinant of self-care behavior in this population. For instance, only the money and resources core domain significantly predicted self-care maintenance and symptom perception. Qualitatively, we found that health insurance coverage facilitated access to care. The lack of health insurance or limitations in coverage raised major concerns about affordability of care, medications, and the type of care received, thus influencing their self-care decisions and choices.
Quantitative and qualitative results regarding money and resources and self-care maintenance were consistent across data sources. However, the quantitative findings regarding self-care symptom perception and PRAPARE core domains were discordant. That is, the money and resources core domain significantly predicted symptom perception, but participants did not describe any element of this PRAPARE construct as influencing symptom perception. Our findings regarding the PRAPARE core domains and HF self-care management and confidence were confirmed by both the quantitative and qualitative results. Quantitatively, none of the PRAPARE core domains predicted either self-care management or confidence. Similarly, participants did not discuss PRAPARE core domains as determinants of self-care management or confidence behaviors.
Further discordance was seen in relation to social connectedness. Quantitatively, the social and emotional health PRAPARE core domain was not a significant predictor of self-care behavior. However, in the interviews, social connectedness was described as a major determinant of HF self-care. Social connections enhanced the navigation of both healthcare and social services and facilitated adherence to HF discharge plans. Participants described how their social connections influenced their ability to access and afford healthcare and social services. Additionally, social connections facilitated their ability to adhere to the HF discharge plan through sharing of health information and experiences surrounding HF management. Participants who were unable to integrate into society had trouble navigating and accessing health and social services that enhance self-care behavior.
Discussion and Implications
The purpose of this study was to describe the relationship between SDoH and HF self-care in community dwelling adults with a recent exacerbation of HF symptoms and explore perceptions, beliefs and experiences surrounding SDoH and HF self-care. We expected participants reporting high SDoH risk to have low self-care, however, low monetary and other resources (i.e., education, employment, insurance, income, material security, and transportation) were associated with better self-care maintenance and symptom perception. Qualitatively, we found that social connections, individual upbringing, and personal experiences, in addition to health insurance coverage were the main determinants of self-care behavior in our sample. Regardless of the direction of the association between money and resources and HF self-care, both our qualitative and quantitative findings indicate that money and resources shape the perception, beliefs and experiences surrounding HF self-care behavior. Specifically, experiences with health insurance and material resources such as food, utilities, childcare, and other unmet needs either enable or impede adequate self-care behavior.
Our finding that participants with low monetary and other resources having better self-care maintenance and symptom perception behaviors differs from that of other studies. For example, financial stress, a factor in health insurance access and material circumstances (including access to food, medicine, and childcare) is known to negatively affect HF self-care.42,43 Others have also found that being married and having college education are associated with better self-care behavior.16 Yet, high risk for low monetary and other resources (including being unemployed, lacking health insurance, living below the federal poverty level, lack of material resources and transportation) was associated with better self-care behavior in our sample. Perhaps, this sample was compensating through one of the constructs included in the money and resources core domain. For instance, we also found that health insurance enhanced access to care and a lack of insurance raised concerns about the affordability of care, medications, and the type of care received.
Many of our participants used some form of public insurance, which suggests that access to such programs is important in influencing HF self-care. That is, it may be that individuals lacking money and resources compensate by using public health programs that enhance their access to health promoting resources that facilitate self-care. For example, the Medicaid expansion under the Patient Protection and Affordable Care Act (Public Law 111–148) decreased cost-related barriers to care by enhancing health promoting behaviors such as reduced missed medication doses (medication adherence), increased office visits and checkups among minorities.44 This evidence suggests that the issue surrounding health insurance is probably not whether the insurance is from a private or public source. Rather, the quality of insurance coverage (e.g., low out-of-pocket co-payments for service and medications, easy access to providers) is more important because it eliminates cost-related barriers to facilitate adherence to HF discharge plans by increasing visits to healthcare providers and reducing out-of-pocket cost for medications. Therefore, public health policies that enhance access to care (e.g., quality public insurance) may be key to improving self-care and clinical outcomes such as rehospitalization rates.
We also found that individual upbringing and personal experiences shaped taste preferences, thus influencing the ability to adhere to prescribed dietary discharge advice. Participants also explained that the cost of food shaped their perceptions of comfort food. These findings support evidence from sensory nutritional science, which suggest that emotions, expectations, and memory shape the human taste experience.45 Participants of a recent qualitative study also identified that physical factors (e.g., food availability, accessibility, and prices), socioeconomic and cultural factors (e.g., culture, ethnicity, and parental upbringing), and psychological factors (e.g., mood, self-control, and addiction) influenced their food choices.46 Although some participants in our study were unsure whether their eating habits and food choices were influenced by culture, the majority were certain that their upbringing and past experiences influenced their regular dietary choices. Together, this evidence suggests that an individual’s ability to adhere to a prescribed diet is multifaceted. Thus, understanding the lived experiences of patients, the sociocultural influences on diet preferences, and the physical barriers to nutritious foods may suggest avenues for future intervention.
Finally, social connectedness influenced the ability to navigate both social and healthcare services and facilitated adherence to HF discharge plans. However, these findings were discordant in the quantitative and qualitative results. Specifically, while interviewees identified their social connectedness as an important determinant of their HF self-care behavior, the social and emotional health core domain measured with PRAPARE was not a significant predictor of self-care. A prior review found that complex measures of social and emotional health such as marital status and network size predicted health outcomes.47 Others also found that relationship type and quality, and social support were associated with HF self-care.48 Perhaps, social connectedness and/or support may be another pathway through which this population compensates for their low risk for money and resources. Together, these findings suggest that individuals with poor social and emotional health may be at risk for inadequate self-care behaviors. Further research is needed to understand the pathways through which SDoH influence self-care behavior to inform the design of interventions that reduce disparities and inequity in HF outcomes among vulnerable patient groups.
Limitations
We recognize several limitations of this study. First, the cross-sectional nature presents an inherent limitation regarding the temporal relationships between SDoH and self-care. Second, we limited enrollment to urban dwelling individuals living in the northeastern US; our results may not represent populations living in rural areas and other parts of the country. Third, a few of the PRAPARE items had low representation in our sample (e.g., ethnicity and English proficiency), suggesting that future studies using the PRAPARE will need a larger and more diverse sample. The internal consistency of the PRAPARE was poor in this study (Cronbach’s alpha of 0.58). Given that the core domains of the PRAPARE address four separate constructs, perhaps PRAPARE is a multidimensional scale requiring use of a technique other than the alpha coefficient to assess reliability.49 Finally, although the PRAPARE is a good step in advancing the science surrounding the collection of SDoH, it does not capture nuanced patient-specific social factors that may influence self-care behavior. For instance, although we were able to collect data on race and insurance type using the PRAPARE, it did not capture racism or insurance quality. While the PRAPARE asks about incarceration within the past year, it does not capture overall incarceration history. These are major limitations of the PRAPARE, given that a history of incarceration and the everyday experience of racism push individuals to a position in society that limits survivability due to a lack of access to health promoting social services. Clearly, more research is needed to develop and test scales that measure the nuanced complexity of SDoH.
Conclusion
In summary, we identified several SDoH that influence self-care in community dwelling adults with HF. These SDoH include money and resources (education, employment status, health insurance, federal poverty level, material circumstances and transportation) as measured by PRAPARE. The lack of health insurance coverage raises major concerns surrounding the affordability of healthcare, medications, food choices and the type of care received. These findings indicate that the relationship between self-care outcomes and SDoH may hinge on the actualization of positive social determinants such as access to quality health insurance coverage and strong social connections that facilitate access to social services and resources by enhancing the ability to navigate health and social services to improve adherence to HF discharge plans. Additionally, individual upbringing and lived personal experiences also influence self-care choices of community dwelling adults with HF. Hence, addressing the social determinants that influence the everyday self-care choices, behaviors, and experiences of community dwelling individuals with HF is imperative in identifying pathways for targeted intervention.
Supplementary Material
Funding
This work was supported by the National Institute of Nursing Research [F31NR018374], and University of Pennsylvania School of Nursing Office of Nursing Research.
Footnotes
Conflict of interest: None Declared
Contributor Information
Foster Osei Baah, Social Determinants of Obesity and Cardiovascular Risk Lab, National Heart, Lung, and Blood Institute, National Institute of Health, Bethesda, MD.
Bridgette M. Brawner, Villanova University, Philadelphia, PA.
Anne M. Teitelman, University of Pennsylvania, Philadelphia, PA.
Jennifer Prah Ruger, School of Social Policy & Practice, University of Pennsylvania.
Barbara Riegel, University of Pennsylvania, Philadelphia, PA.
References:
- 1.Tsao CW, Aday AW, Almarzooq ZI, et al. Heart disease and stroke statistics—2022 update: A report from the american heart association. Circulation. 2022;145(8):e153–e639. [DOI] [PubMed] [Google Scholar]
- 2.Alcendor DJ. Racial disparities-associated COVID-19 mortality among minority populations in the US. Journal of clinical medicine. 2020;9(8):2442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Havranek EP, Mujahid MS, Barr DA, et al. Social determinants of risk and outcomes for cardiovascular disease: A scientific statement from the american heart association. Circulation. 2015;132(9):873–898. doi: 10.1161/CIR.0000000000000228. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization. A conceptual framework for action on the social determinants of health. . 2010.
- 5.Maness SB, Buhi ER. Associations between social determinants of health and pregnancy among young people: A systematic review of research published during the past 25 years. Public Health Rep. 2016;131(1):86–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Riegel B, Dickson VV. A situation-specific theory of heart failure self-care. In: Situation specific theories: Development, utilization, and evaluation in nursing. Springer; 2021:149–160. [Google Scholar]
- 7.Zou H, Chen Y, Fang W, Zhang Y, Fan X. Identification of factors associated with self-care behaviors using the COM-B model in patients with chronic heart failure. Eur J Cardiovasc Nurs. 2017;16(6):530–538. [DOI] [PubMed] [Google Scholar]
- 8.Jaarsma T, Cameron J, Riegel B, Stromberg A. Factors related to self-care in heart failure patients according to the middle-range theory of self-care of chronic illness: A literature update. Curr Heart Fail Rep. 2017;14(2):71–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gelberg L, Andersen RM, Leake BD. The behavioral model for vulnerable populations: Application to medical care use and outcomes for homeless people. Health Serv Res. 2000;34(6):1273–1302. [PMC free article] [PubMed] [Google Scholar]
- 10.Lee KS, Choi J, Jeon E, et al. Distinct factors associated with better self-care in heart failure patients with and without mild cognitive impairment. J Cardiovasc Nurs. 2019;34(6):440–447. [DOI] [PubMed] [Google Scholar]
- 11.Hu X, Hu X, Su Y, Qu M, Dolansky MA. The changes and factors associated with post-discharge self-care behaviors among chinese patients with heart failure. Patient Preference Adherence. 2015;9:1593–1601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heo S, Moser DK, Lennie TA, et al. Varied factors were associated with different types of self-care in heart failure. West J Nurs Res. 2020:0193945920950334. [DOI] [PubMed] [Google Scholar]
- 13.Dickson VV, Knafl GJ, Wald J, Riegel B. Racial differences in clinical treatment and self-care behaviors of adults with chronic heart failure. J Am Heart Assoc. 2015;4(4): 10.1161/JAHA.114.001561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ausili D, Rebora P, Di Mauro S, et al. Clinical and socio-demographic determinants of self-care behaviours in patients with heart failure and diabetes mellitus: A multicentre cross-sectional study. Int J Nurs Stud. 2016;63:18–27. [DOI] [PubMed] [Google Scholar]
- 15.Walker RJ, Gebregziabher M, Martin-Harris B, Egede LE. Independent effects of socioeconomic and psychological social determinants of health on self-care and outcomes in type 2 diabetes. Gen Hosp Psychiatry. 2014;36(6):662–668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Baah FO, Chittams J, Carlson B, et al. Sociodemographic indicators of social position and self-care maintenance in adults with heart failure. Clin Nurs Res. 2021;30(6):847–854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tzeng H, Barker A, Kang Y, Okpalauwaekwe U, Yin C. Are older adults’ demographic characteristics social determinants of their perceived importance, desire, and ability to perform end-of-life self-care actions?. 2019;54(4):565–574. [DOI] [PubMed] [Google Scholar]
- 18.Krieger N, Williams DR, Moss NE. Measuring social class in US public health research: Concepts, methodologies, and guidelines. Annu Rev Public Health. 1997;18(1):341–378. [DOI] [PubMed] [Google Scholar]
- 19.Whitehead M, Burström B, Diderichsen F. Social policies and the pathways to inequalities in health: A comparative analysis of lone mothers in britain and sweden. Soc Sci Med. 2000;50(2):255–270. [DOI] [PubMed] [Google Scholar]
- 20.Prah Ruger J. Health capability: Conceptualization and operationalization. Am J Public Health. 2010;100(1):41–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Baah FO, Teitelman AM, Riegel B. Marginalization: Conceptualizing patient vulnerabilities in the framework of social determinants of health—An integrative review. Nurs Inq. 2019;26(1):e12268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Creswell J, Plano Clark V. Designing and conducting mixed methods research. Vol 3rd Edition. 3rd ed. Thousand Oaks. California: Sage Publications; 2017. [Google Scholar]
- 23.Rabelo-Silva ER, Saffi MAL, Aliti GB, et al. Precipitating factors of decompensation of heart failure related to treatment adherence: Multicenter study-EMBRACE. Rev Gaucha Enferm. 2018;39:e20170292–1447.2018.20170292. [DOI] [PubMed] [Google Scholar]
- 24.Swartz RH, Cayley ML, Lanctot KL, et al. Validating a pragmatic approach to cognitive screening in stroke prevention clinics using the montreal cognitive assessment. Stroke. 2016;47(3):807–813. [DOI] [PubMed] [Google Scholar]
- 25.Riegel B, Barbaranelli C, Carlson B, et al. Psychometric testing of the revised self-care of heart failure index. J Cardiovasc Nurs. 2019;34(2):183–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gold R, Cottrell E, Bunce A, et al. Developing electronic health record (EHR) strategies related to health center patients’ social determinants of health. J Am Board Fam Med. 2017;30(4):428–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.National Association of Community Health Centers. PRAPARE implementation and action toolkit. National Association of Community Health Centers website. Web site. http://www.nachc.org/research-and-data/prapare/toolkit/. Updated 2019. Accessed May, 2020. [Google Scholar]
- 28.Wetta RE, Severin RD, Gruhler H. An evidence-based strategy to achieve equivalency and interoperability for social-behavioral determinants of health assessment, storage, exchange, and use. Health informatics journal. 2020;26(2):1477–1488. [DOI] [PubMed] [Google Scholar]
- 29. http://www.nachc.org/research-and-data/prapare/.
- 30.Weir RC, Proser M, Jester M, Li V, Hood-Ronick CM, Gurewich D. Collecting social determinants of health data in the clinical setting: Findings from national PRAPARE implementation. J Health Care Poor Underserved. 2020;31(2):1018–1035. [DOI] [PubMed] [Google Scholar]
- 31.Gottlieb L, Cottrell EK, Park B, Clark KD, Gold R, Fichtenberg C. Advancing social prescribing with implementation science. J Am Board Fam Med. 2018;31(3):315–321. [DOI] [PubMed] [Google Scholar]
- 32.Stavem K, Hoel H, Skjaker SA, Haagensen R. Charlson comorbidity index derived from chart review or administrative data: Agreement and prediction of mortality in intensive care patients. Clin Epidemiol. 2017;9:311–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gibbs G. Learning by doing: A guide to teaching and learning methods. Oxford Centre for Staff and Learning Development, Oxford Brookes University; 1988. [Google Scholar]
- 34.Chowdhury MZI, Turin TC. Variable selection strategies and its importance in clinical prediction modelling. Family Medicine and Community Health. 2020;8(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hsieh H, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 36.Lindgren B, Lundman B, Graneheim UH. Abstraction and interpretation during the qualitative content analysis process. Int J Nurs Stud. 2020:103632. [DOI] [PubMed] [Google Scholar]
- 37.Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs. 2008;62(1):107–115. [DOI] [PubMed] [Google Scholar]
- 38.Graneheim UH, Lundman B. Qualitative content analysis in nursing research: Concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2):105–112. [DOI] [PubMed] [Google Scholar]
- 39.Hanson CS, Ju A, Tong A. Appraisal of qualitative studies. Handbook of Research Methods in Health Social Sciences. 2018:1–15. [Google Scholar]
- 40.McHugh ML. Interrater reliability: The kappa statistic. Biochemia medica: Biochemia medica. 2012;22(3):276–282. [PMC free article] [PubMed] [Google Scholar]
- 41.Creswell JW. CUSTOM: CEC edition qualitative inquiry and research design 3e. SAGE Publications; 2017. [Google Scholar]
- 42.Dickens C, Dickson VV, Piano MR. Perceived stress among patients with heart failure who have low socioeconomic status: A mixed-methods study. J Cardiovasc Nurs. 2019;34(3):E1–E8. [DOI] [PubMed] [Google Scholar]
- 43.Negarandeh R, Aghajanloo A, Seylani K. Barriers to self-care among patients with heart failure: A qualitative study. J Caring Sci. 2020;10(4):196–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sommers BD, Blendon RJ, Orav EJ, Epstein AM. Changes in utilization and health among low-income adults after medicaid expansion or expanded private insurance. JAMA internal medicine. 2016;176(10):1501–1509. [DOI] [PubMed] [Google Scholar]
- 45.Vincis R, Fontanini A. Central taste anatomy and physiology. In: Handbook of clinical neurology. Vol 164. Elsevier; 2019:187–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nwaugochi I, Kennedy L. Qualitative study of the determinants of food choice of international students and its associated health risk (P10-080-19). Current developments in nutrition. 2019;3(Supplement_1):nzz034. P10-080-19. [Google Scholar]
- 47.Tay L, Tan K, Diener E, Gonzalez E. Social relations, health behaviors, and health outcomes: A survey and synthesis. Applied Psychology: Health and Well-Being. 2013;5(1):28–78. [DOI] [PubMed] [Google Scholar]
- 48.Bidwell JT, Vellone E, Lyons KS, et al. Determinants of heart failure self-care maintenance and management in patients and caregivers: A dyadic analysis. Res Nurs Health. 2015;38(5):392–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Barbaranelli C, Lee CS, Vellone E, Riegel B. Dimensionality and reliability of the self-care of heart failure index scales: Further evidence from confirmatory factor analysis. Res Nurs Health. 2014;37(6):524–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


