Abstract
Objective: The current study aimed to compare the impact of acupressure and clonazepam tablets on the quality of sleep in hemodialysis patients in light of the rising prevalence of chronic kidney disease (CKD), the high prevalence of sleep disturbance in these patients, and the side effects of hypnotic drugs.
Method : A total of 60 patients were selected for this randomized, controlled clinical trial and randomly assigned to two groups. For two weeks during the researcher's evening shift, one group received acupressure (six spots bilaterally for three minutes each day). The opposing group was administered clonazepam tablets (0.5 mg) for two weeks. The Pittsburgh Sleep Quality Index (PSQI), which measures sleep quality, was used to compare sleep in the two groups before and after the intervention.
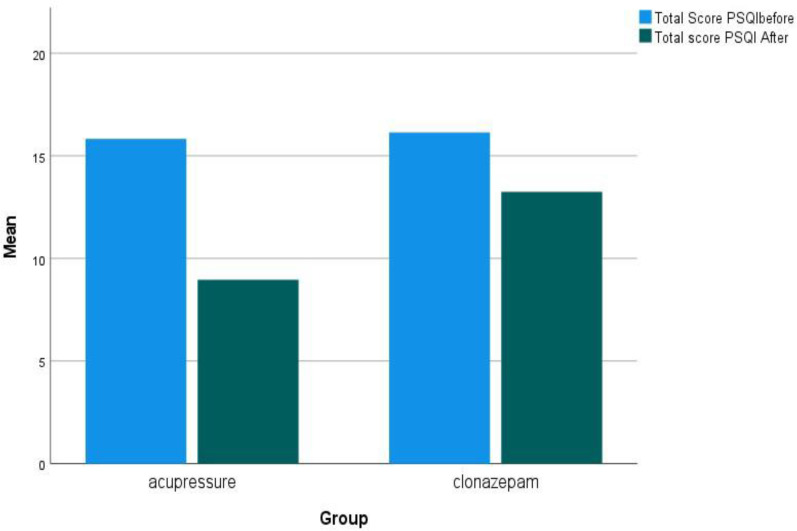
Results: There was no statistically significant difference between the two groups prior to the intervention (P = 0.75) in terms of the mean pre-intervention PSQI scores for the acupressure and clonazepam groups, which were 15.83 ± 1.51 and 16.17 ± 0.91, respectively. However, the average PSQI scores after the intervention in the clonazepam and acupressure groups were 13.25 ± 2.88 and 8.97 ± 4.29, respectively, indicating a statistically significant difference (P < 0.0001). Both the acupressure and the clonazepam groups showed improvements in their post-intervention sleep quality among the patients. However, when the percentage changed in the mean scores of the total score and all of the PSQI components were calculated for each group, it became clear that acupressure was more effective at enhancing sleep than clonazepam tablets.
Conclusion: The findings of the present investigation demonstrate that acupressure has a greater impact on patients’ sleep quality compared to clonazepam tablets. Depending on the circumstances, acupressure can be used as a simple, safe, and non-drug way to enhance hemodialysis patients' quality of sleep.
Key Words: Acupressure, Clonazepam, Hemodialysis, Renal Dialysis, Sleep Quality
Chronic kidney disease (CKD) is an irreversible kidney problem (1), that is becoming more common nowadays as a result of the rise in conditions including diabetes, hypertension, and cancer (2). Hemodialysis and, eventually, a kidney transplant are required for patients with end-stage chronic renal failure (ESRD) in order to prolong their lives (1, 3). In Iran, the frequency of CKD is rising (4) and the number of people receiving permanent hemodialysis rises by 15% per year (5). Furthermore, each year, 29,000 people in Iran are affected by this condition, 14,000 of whom receive hemodialysis (6). CKD patients encounter a variety of issues as a result of the disease process, including anxiety, despair, social isolation, disease denial, hallucinations, delirium, and poor sleep quality (7).
Hemodialysis patients frequently experience sleep abnormalities (8), and between 20 and 83% of patients experience various sleep-related disorders (9), with 60% of patients reporting disturbed sleep (10). Hemodialysis patients experience a variety of sleep abnormalities, such as restless legs syndrome and sleep apnea syndrome (11), as well as daytime drowsiness (12), and insomnia at night (13). The low sleep quality disrupts patients' feelings, thoughts, and motivations, fatigue, difficulty concentrating, loss of appetite, nervousness, depression, and anxiety (14). It also affects the social adaptation of these patients (15). Poor sleep is linked to an increased risk of hypertension, progressive CKD, impaired glucose tolerance, diabetes mellitus, depression, and greater use of medical services (16). If left untreated, these conditions are also more likely to result in heart disease and a higher mortality rate (17, 18). Sedative medicines are the first line of treatment for sleep disruption in these individuals (19). Benzodiazepines, especially clonazepam, are used to treat sleep disturbance in hemodialysis patients, which cause side effects such as physical dependence and sleep apnea (20). Other negative effects of these medications include drowsiness, instability, and lightheadedness, which raise the risk of falling (21). Non-pharmacological treatments are recommended for the management of sleep disturbance in hemodialysis patients due to the significant negative effects of medications (22). Among non-pharmacological therapies, acupressure has drawn attention due to its low risk and lack of invasiveness (23). Fingers are used in acupressure, a complementary therapy, to stimulate pressure points to maintain energy balance (24). It is cost-free and can be self-administered by patients themselves (25).
Acupressure is based on meridian theory, which holds that there are meridians or energy channels throughout the body (26). A blockage in a meridian leads to diseases and disorders, while applying pressure on some points along these channels causes energy balance and cures diseases (27). By releasing nerve mediators like endorphins, enkephalin, dopamine, and serotonin in the central nervous system, acupressure also lessens discomfort and improves comfort (19). One of the neurotransmitters involved in sleep, mood, and muscular contractions is serotonin. In response to serotonin signals, melatonin is released from the pineal region of the brain, which shortens the time it takes to fall asleep and lengthens and improves the quality of sleep. Additionally, acupressure point stimulation controls the functioning of the parasympathetic nervous system (28).
The impact of acupressure on the quality of sleep in hemodialysis patients has been the subject of numerous studies. In a research study, hemodialysis patients who received acupressure felt improvement in their sleep quality (19). In another study, hemodialysis patients' sleep quality was enhanced using acupressure at wrist, foot, and ear locations. The findings of the mentioned study demonstrated that acupressure, as a non-invasive technique, enhances sleep quality among hemodialysis patients (29). Shenmen (HT7) is the most commonly used acupressure point to enhance hemodialysis patients' sleep quality, according to a review of research (22). Although the acupressure points and length employed in the aforementioned investigations varied, the Pittsburgh Sleep Quality Questionnaire (PSQI), a measure of sleep quality, was used in both. The spots specified in earlier research (16, 19, 29, 30) were employed in this study to examine the impact of acupressure on the amount and quality of sleep among hemodialysis patients in the acupressure group.
The research that is currently available does not include a study that contrasts acupressure with clonazepam tablets. The current study sought to examine the impact of acupressure and clonazepam tablets on the quality of sleep in hemodialysis patients in light of the rising incidence of CKD, the high prevalence of sleep disturbance in these patients, and the adverse effects of sedative drugs.
Materials and Methods
Study Design
The study was a randomized control trial (IRCT20110906007494N41) conducted on individuals undergoing hemodialysis at the Sari Comprehensive Dialysis Center (Shahrvand Renal Patients Center) who suffered from sleep disturbance as indicated by the PSQI (scores 5 and above). The sample size was estimated using the results of Nasiri et al.'s study (29). Considering this study, a 99% confidence interval, a test power of 95% for the two-tailed test, and using the formula for average difference and G POWER software, and also taking into account a 20% drop-out, the total number of samples was estimated to be 60 people (n = 30 per group).
A statistical consultant employed permuted block randomization to split the eligible participants into intervention and control groups (n = 30 per group). A total of 15 blocks were utilize, with each block comprised of four individuals (block size = 4) - two from the acupressure group and two from clonazepam group. As a result, 60 envelopes were created, which were labeled with letters A (for the acupressure group) and B (for the clonazepam group) using computer instructions. After obtaining written informed consent, the first qualified patient admitted to the hospital ward was included in the study, and the sampling process continued until 60 patients were chosen.
Inclusion and Exclusion Criteria
The following conditions had to be met: participants needed to be at least 18 years old, have the PSQI score of 5 or higher indicating their sleep disturbance, undergo hemodialysis twice or three times per week, be Iranian citizens, possess mental alertness and the ability to respond to questions, not be experiencing delirium or cognitive disorders, and not have undergone amputations of limbs or exhibited ulcers at pressure points. Additionally, patients who employed adjuvant therapies, including acupuncture, herbal remedies, hypnosis, or yoga, were not included in the study as well as those patients who required anti-anxiety or hypnotic medications due to psycho-neurocognitive illnesses.
Exclusion criteria included situations where patients requested cessation of the intervention, experienced a worsening of sleep disturbance, faced the death of a first-degree relative, were transferred to the acute care unit, needed to have transplant surgery, traveled during the study, experienced an allergic reaction, or passed away during the research.
Instruments for Data Collection
The Mini-Mental Status Examination (MMSE), Nursing Delirium Screening Scale (NDSS), and Pittsburgh Sleep Quality Index (PSQI) were among the equipment used to collect data. In this study, questions on age, sex, occupation, marital status, education level, length of hemodialysis, history of underlying diseases, and body mass index are part of the demographic and medical questionnaire. To investigate the mental perceptions and cognitive impairment of the participants before the intervention, the MMSE was employed.
The MMSE is completed in the form of an interview which investigates five dimensions: orientation, information recording, attention and calculation, recall, and language. Orientation consists of two five-part questions and each participant receives a score by answering each part. The information recording section consists of a three-part question, resulting in three marks. The attention and calculation section consists of five scores, assessing attention ability by practicing numbers. Recall and language sections have three and nine points, respectively. The total possible score ranges from 0 to 30. Scores 25 > , 21-24, 10-20, and > 9 indicate a normal condition, mild, moderate, and severe cognitive impairment, respectively (30-33). The cut-off point of 22 has a sensitivity of 90% and a specificity of 93.5% (34). This cut-off point was used in the present study. The interrater reliability was measured at 0.97 using Spearman's correlation coefficient after evaluating 10 patients by two evaluators.
Delirium was assessed using the Nurse Delirium Screening scale (Nu-DESC), which is another exclusion factor. A nurse can complete this scale, which has five variables for measuring delirium and is based on a three-point rating scale (0 = no symptom, 1 = moderate, and 2 = severe). It can be administered in less than two minutes. Using this scale, the patient can be checked for delirium symptoms twice a day. Lack of insight, inappropriate behavior, inappropriate communication, delirium or hallucinations, and motor delay is among the studied variables. It should be noted that this scale was measured every day before the intervention, and individuals scoring 2 or higher were excluded from the study due to having delirium symptoms. This scale examines the person in terms of confusion, inappropriate behavior, inappropriate communication, delirium, delusions, and mental retardation. A score of 2 or higher in the Nu-DESC indicates delirium symptoms and the person was excluded from the study. For this purpose, the Nu-DESC was completed every other day throughout the study period so that the study would be stopped in the case of delirium symptoms. The Nu-DESC has 85.7% sensitivity and 86.8% specificity (35, 36). Inter-rater reliability was calculated at 0.80 using the Kappa correlation coefficient after 10 patients were evaluated by two evaluators.
Following the completion of the necessary patient information, the patients' sleep quality was assessed using the PSQI. Consequently, only those patients with a PSQI score of 5 or higher were included in the study. Subjective sleep quality, sleep latency, sleep duration, sleep efficiency, sleep disturbance, usage of sleeping medications, and daytime dysfunction are the seven dimensions in this self-reported questionnaire that measure the quality of sleep. Open-ended, brief, single-answer questions can be used for questions 1 through 4, whereas multiple-choice questions can be utilized for questions 5 through 9 (37).
The first factor (question 9) is associated with subjective sleep quality. The mean score of question 2 and Part A of question 5 are utilized to calculate the score for the second component, which is connected to sleep latency. The final factor (question 4) has to do with sleep duration. The fourth factor, which is concerned with sleep efficiency, is calculated by multiplying a person's score by 100 and dividing their total number of hours of sleep by the total number of hours they spend in bed. The fifth component, associated with sleep disturbance, is determined by averaging the answers to question 5. The sixth element (question 6) addresses the usage of sedative drugs. By calculating the mean scores of questions 7 and 8, daytime dysfunction as the seventh component is identified (38). Each question can receive a score ranging from 0 and 3, correspondingly. The total score of the instrument, which varies from 0 to 21, is obtained by adding the mean scores of these seven components. Additionally, each dimension is given a number between 0 and 3, with lower values indicating higher sleep quality. (37). Farhadinasab & Azimi have verified the validity of the Persian translation of this questionnaire (39). Farahi et al. reported sensitivity, specificity, and Cronbach's alpha of 100%, 93%, and 0.89, respectively (37).
The research council and ethics committee for biomedical research at Mazandaran University of Medical Sciences gave their approval to the current work (IR.MAZUMS.REC.1400.245). The eligible patients were provided with appropriate explanations, and after gaining their informed consent, the researcher chose the samples. At baseline, both groups received necessary training about sleep hygiene. To determine the real points in acupressure in addition to training, the location of the desired points on the body was confirmed with 100% accuracy, and a certificate was received from a Chinese medicine specialist before the intervention.
Procedures
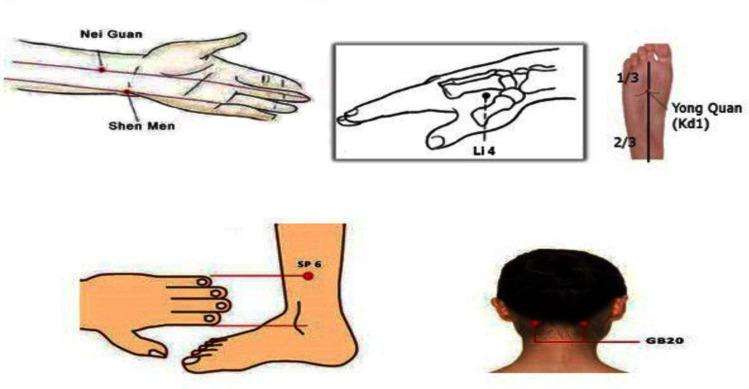
After reviewing the related literature and consulting with an acupuncture expert, a combined stimulation was applied to the following points: Shenmen (HT7) (19, 26), Neiguan (29) Hegu (Li4) (40), Sanyinjiao (sp6) (40), Yongquan (k11) (16, 29), and Fengchi (GB20) (41) (Figure 1). The Shenmen point is located in the little depression between the pisiform and ulna bones at the ulnar end of the transverse crease of the wrist (24, 42). Neiguan point (PC6) is situated between the flexor carpi radialis and palmaris longus on the anterior aspect of the forearm, two inches above the transverse crease of the wrist (43). Hegu can be found at the middle of the angle between the first and second bones of the palm on the back of the hand, between the thumb and the index finger (42). The fourth acupressure point is Sanyinjiao (SP-6), which is located on both feet at a point four fingers' width behind the tibia and above the ankle bone (44). Fengchi and Yongquan (KI-1) are the other two points. Yongquan is situated between the second and third toes at the intersection of the anterior third and the posterior two-thirds of the sole (42). A dip between the upper sternocleidomastoid muscle and the trapezius muscle, behind the head, is where Fengchi can also be found (45). The Shenmen point (HT7), which Hon. found to be the most often used acupressure point for treating insomnia, is situated on the wrist pisiform, between the pisiform and the ulna bone in the transverse crease of the wrists. According to the same review study, the Yongquan point (K11) of the foot sole has been utilized as a complementary point to the Shenmean point for the treatment of insomnia in dialysis patients (22). A sesamoid bone, the pisiform is the fourth wrist bone in the proximal row and is situated in the thickness of the flexor carpi ulnaris muscle (46).
Figure 1.
Acupoints Applied to Improve Sleep Quality
The points mentioned in the previous paragraph were pressed bilaterally and simultaneously using the finger for three minutes each (16, 19, 40), and the total intervention duration was 18 minutes. The pressure was exercised continuously and rotationally using the thumb at a speed of two rotations per second. The level of pressure was adjusted to the level of patients' tolerance. The intervention was performed one hour after the start of dialysis in the acupressure group (29, 40) as patients tend to be in a better emotional state at this time (40).
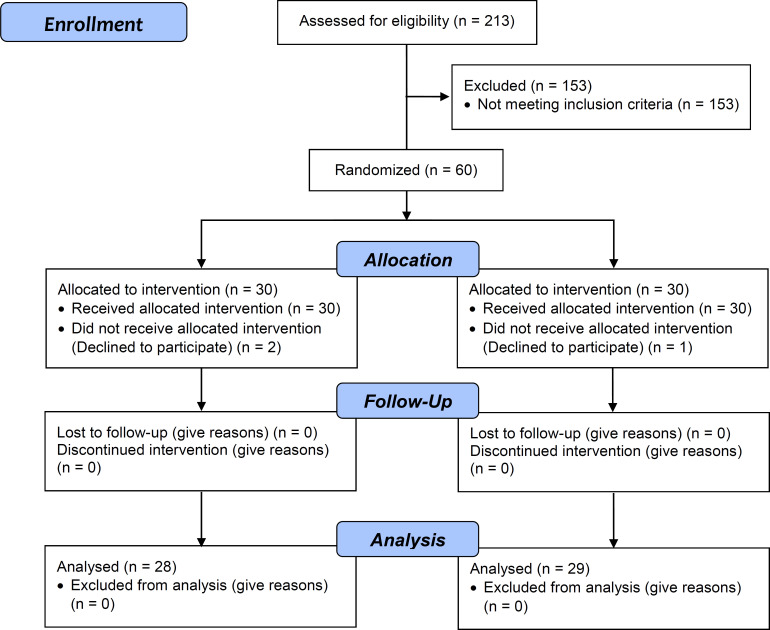
According to a similar study (26), the total duration of the intervention in the acupressure group was two weeks. The intervention sessions were carried out every other day in the evening on days 1, 3, 5, 7, 9, 11, and 13 of the study, resulting in seven eighteen-minute sessions. The second group used a clonazepam tablet (0.5 mg) (47) every night for two weeks. According to a similar study (20), the total duration of the intervention in the clonazepam group was two weeks. This tablet was provided by the Sobhan Daru Company. After the two-week intervention, the sleep quality of the patients in both groups was re-examined using the PSQI, which was completed by both groups on the evening of day 15. A total of 213 patients were assessed for eligibility criteria, of whom 60 were included in the study while the rest were excluded for various reasons (Consort flowchart in Figure 2). These reasons for exclusion included hearing and vision problems (n = two cases), delirium (n = 10 cases), drug addiction (n = 20 cases), use of anti-anxiety and sleeping pills (n = 98 cases), cognitive impairment (n = 12 cases), young age (17 years old) (n = one case), cancer (n = three cases), and unwillingness to participate in the study (n = seven cases).
Figure 2.
Consort Flowchart: Enrollment, Allocation, Follow-up, and Data Analysis Phases to Compare the Effects of Acupressure and Clonazepam Tablets on Sleep Quality of Hemodialysis Patients
Data Analysis
The SPSS software was used to analyze the data that was gathered. An independent t-test was used to compare the status of normal quantitative variables in the two groups. The Mann Whitney test was employed to compare the status of non-normal quantitative variables in the two groups, and the Wilcoxon test was used to compare sleep scores at baseline and end of the study in each group. The Chi-square test (in cases of encountering limitations), Fisher's exact test, an independent t-test, and the Mann-Whitney test were also applied to compare the status of demographic and background variables between the two groups. In all tests, a significance level of P-value < 0.05 was considered.
Results
According to the study's findings, there were no statistically significant differences between the acupressure and clonazepam groups in terms of age, sex, marriage, body mass index, history of dialysis, education level, employment position, or medical history (Table 1).
Table 1.
Comparison of Demographic and Medical Characteristics of Patients in Acupressure and Clonazepam Groups
| Characteristics |
Acupressure
Number (%) |
Clonazepam
Number (%) |
P-value | |
|---|---|---|---|---|
| Gender | Male | 12(40) | 18(60) | 0.121* |
| Female | 18(60) | 12(40) | ||
| Occupation | Unemployed | 19(66.33) | 15(50) | 0.456** |
| Manual worker | 8(26.66) | 9(30) | ||
| Retired | 3(10) | 6(20) | ||
| Educational level | Illiterate | 7(23.23) | 4(13.33) | 0.580 |
| Below diploma | 15(50) | 18(60) | ||
| Diploma and university degree | 8(26.66) | 8(26.66) | ||
| HTN disease | Yes | 22(73.33) | 20(66.66) | 0.573* |
| No | 8(26.66) | 10(33.33) | ||
| Diabetes disease | Yes | 17(56.66) | 16(55.33) | 0.795* |
| No | 13(43.33) | 14(46.66) | ||
| Marital status | Married | 24(80) | 27(90) | 0.470** |
| Spouseless (single and widowed) | 6(20) | 3(10) | ||
| Dialysis history (year) | Mean and standard deviation | 3.37 ± 2.35 | 3.90 ± = 3.20 | 0.775*** |
| BMI(body mass index) | Mean and standard deviation | 29.21 ± 4.60 | 28.16 ± 4.00 | 0.348**** |
| Age | Mean and standard deviation | 58.50 ± 10.32 | 60.07 ± 10.74 | 0.411*** |
: Chi-Square Test (chi-2),
: Fisher Test,
: Mann-Whitney Test,
: Independent T-Test
Before and after the intervention, the Mann-Whitney test was performed to determine whether all PSQI components were equal in the two groups. Prior to the intervention, the data did not reveal a statistically significant difference between the two groups (P = 0.75). Additionally, after the intervention, the data revealed a statistically significant association between the two groups for all PSQI components with the exception of the use of sleeping medications (non-use) and sleep disturbance. Following the intervention, the total sleep quality score declined in both groups, which was statistically significant (P ˂ 0.0001). However, the acupressure group experienced a greater decline (improvement) in the total sleep quality score. The outcomes demonstrated that acupressure is more effective in improving sleep quality than Clonazepam tablets (Figure 3).
Figure 3.
Camparison of the Mean Total Score PSQI between Two Acupressure and Clonazepam Groups before and after the Intervention
The Wilcoxon test resulted in a statistically significant difference between the two groups' averages for all sleep quality dimensions after the intervention (P ˂ 0.05), and the findings demonstrated that the quality of sleep in both groups' patients improved as a result of the intervention. Additionally, the findings of comparing the Pittsburgh Questionnaire's dimensions and overall scores (PSQI) between the two groups (using the Mann-Whitney test) (Figure 3) revealed that, following the intervention, there was a statistically significant difference between the two groups in all dimensions except for sleep disturbances (P ˂ 0.05). The outcomes demonstrated that acupressure had a stronger impact on patients' sleep quality.
Both the acupressure and clonazepam interventions improved the overall sleep quality and all subcategories of sleep quality, according to calculations of percentage changes in the average overall sleep quality and subcategories of sleep quality in the two groups before and after the intervention (Table 2). However, the results clearly indicate that acupressure has a greater impact on the overall quality of sleep and all subclasses related to sleep quality.
Table 2.
Comparison of Dimensions and Total Sleep Quality Score between Two Acupressure and Clonazepam Groups before and after the Intervention
|
Components of the
Pittsburgh Sleep Quality Index |
Time |
Acupressure Group
(Mean ± SD) |
Clonazepam Group
(Mean ± SD) |
Mann-Whitney * |
|---|---|---|---|---|
| Subjective sleep quality | Before intervention | 2.79 ± 0.41 | 2.64 ± 0.48 | 0.240 |
| Two weeks after the intervention |
0.76 ± 0.95 | 1.61 ± 0.87 | 0.004 | |
| Wilcoxon** | ˂ 0.001 | ˂ 0.001 | ||
| Percentage of changes | -72.76 | -39.02 | ||
| Sleep latency | Before intervention | 2.72 ± 0.52 | 2.93 ± 0.26 | 0.070 |
| Two weeks after the intervention |
1.97 ± 0.77 | 2.54 ± 0.57 | 0.004 | |
| Wilcoxon | ˂ 0.001 | 0.002 | ||
| Percentage of changes | -27.57 | -13.31 | ||
| Sleep duration | Before intervention | 2.97 ± 0.18 | 3 ± 0.00 | 0.310 |
| Two weeks after the intervention |
1.97 ± 1.05 | 2.75 ± 0/51 | 0.002 | |
| Wilcoxon | ˂ 0.001 | 0.02 | ||
| Percentage of changes | -33.67 | -8.33 | ||
| Sleep efficiency | Before intervention | 2.41 ± 1.01 | 2.82 ± 0.47 | 0.220 |
| Two weeks after the intervention |
1.62 ± 1.26 | 2.50 ± 0.79 | 0.006 | |
| Wilcoxon | 0.003 | 0.014 | ||
| Percentage of changes | -32.78 | -11.35 | ||
| Sleep disturbance | Before intervention | 2.00 ± 0.37 | 1.93 ± 0.53 | 0.760 |
| Two weeks after the intervention |
1.38 ± 0.56 | 1.64 ± 0.48 | 0.070 | |
| Wilcoxon | ˂ 0.001 | 0.005 | ||
| Percentage of changes | -31 | -15.03 | ||
| Daytime sleepiness | Before intervention | 2.90 ± 0.31 | 2.86 ± 0.44 | 0.960 |
| Two weeks after the intervention |
1.34 ± 0.85 | 2.11 ± 0.87 | 0.002 | |
| Wilcoxon | ˂ 0.001 | ˂ 0.001 | ||
| Percentage of changes | -53.79 | -22.26 | ||
| Total sleep quality score | Before intervention | 15.83 ± 1.51 | 16.17 ± 0.91 | 0.750 |
| Two weeks after the intervention |
8.97 ± 4.29 | 13.25 ± 2.88 | ˂ 0.0001 | |
| Wilcoxon | ˂ 0.001 | ˂ 0.001 | ||
| Percentage of changes | -43.34 | -18.06 |
Test Result between Group
Intragroup Test Result
Discussion
The findings unambiguously demonstrate that acupressure has a stronger impact on the total PSQI score and its sub-components of subjective sleep quality, sleep latency, sleep duration, sleep efficacy, and daytime drowsiness, as well as disrupting and enhancing them compared to colonazpam. Similar studies (19, 20, 29, 40, 48) have highlighted the beneficial effects of acupressure on patients' sleep quality. As an illustration, the findings of the study by Arab and her coworkers revealed that the total PSQI score and all of its components, with the exception of sleep efficiency and the use of sedative medications, were statistically different in the acupressure group before and after the intervention, and even massage in the false points group improved the quality of sleep and some of its components (19). Furthermore, acupressure in both studies led to a significant improvement in the mean scores of subjective sleep quality, daytime sleepiness, sleep duration, sleep efficiency, sleep disturbance, and sleep latency. The above-mentioned study and the present one differ in several aspects. For example, there were three groups in the aforementioned study: acupressure, false points, and controls, while the present study had two groups of acupressure and clonazepam, so the superiority of one of them over the other could be determined. Moreover, six acupressure points were used in two weeks in the present study, but one point was used for four weeks in the aforementioned study. Another difference lies in the use of sedative medications before the intervention; patients who did not take sedative medications two weeks before the intervention were included in the present study. Both studies were similar in terms of using the same sleep quality instrument, i.e. the PSQI.
In another similar study (26), the result of intervention in the sleep quality of patients showed that acupressure improved the total PSQI score and all its components except for sleep efficiency. However, this study and our study have different times of intervention. In the aforementioned study, the sleep quality was examined two and four weeks after the intervention, whereas in the present study, it was not possible to conduct the study for four weeks due to the use of clonazepam and its possible side effects. Additionally, a related study (16) conducted in Australia found that the mean PSQI scores decreased for the acupressure group from 8.1 (pre-intervention) to 7.62 (post-intervention), and for the sham group from 8.3 (pre-intervention) to 7.42 (post-intervention). Despite the fact that both groups' sleep quality scores dropped after the intervention, there was no discernible difference in the two groups' sleep scores, which is contradictory with the results of the current study. In line with the present study, the aforementioned research used the PSQI to evaluate sleep quality. Additionally, the patients were split into two groups: one received acupressure at the Shenmen and Yongquan points, while the other received sham acupressure. Contrary to earlier studies of a similar nature, both the intervention and control groups experienced improved sleep, as indicated by lower mean sleep quality scores. The proportion of males and females in the two groups is another distinction between the two studies.
Acupressure was applied to hemodialysis patients for four weeks every other day in a prior trial in India (48). Despite the fact that the majority of participants (73.3%) were men, this intervention considerably improved the patients' sleep quality. Similar to the present investigation, both studies found that acupressure significantly improved the mean scores of subjective sleep quality, daytime drowsiness, sleep length, sleep efficiency, and sleep disturbance. Consistent with the current study, acupressure led to a significant improvement in the mean scores of subjective sleep quality, daytime sleepiness, sleep duration, sleep efficiency, sleep disturbance, and sleep latency in the above-mentioned study. Moreover, the PSQI was utilized in both studies. Dashti et al. (20) compared clonazepam pills with zolpidem in order to determine how well hemodialysis patients slept when using clonazepam tablets. Their findings, which were consistent with the current study, indicated that the mean PSQI score diminished in the clonazepam group. Clonazepam reduced the overall mean PSQI score in both investigations, as well as its sub-scores for subjective sleep quality, daytime sleepiness, sleep duration, efficiency, disruption, and sleep latency. However, the dosage of clonazepam differed between the present study and the aforementioned study, with 0.5 mg of clonazepam being utilized in the current research. The findings of this study demonstrated that zolpidem was much better tolerated by hemodialysis patients than clonazepam, and that clonazepam had a higher effect on increasing the quality of their sleep.
Clonazepam appeared to have fewer side effects if administered at a dosage of 0.5mg in the aforementioned study, as it was in the current one, while having a bigger impact on sleep quality, according to the study described above. Patients in the clonazepam group in the current study reported symptoms such as dizziness and a decrease in the drug's effect in the second week (drug tolerance), while those in the acupressure group did not report any specific complications. Furthermore, in contrast to the clonazepam group, the intervention had a greater long-term impact on the patients' sleep quality.
Limitation
One of the weaknesses of the study was the participants' mental and emotional condition, which was beyond the researcher's control. Other restrictions on this study included the small sample size, lack of a control group, short follow-up duration, and low clonazepam dose. It is recommended that a higher dose of clonazepam be planned for a longer period of time to achieve its effectiveness in future research with a control group and a larger sample size. More research should be conducted on the effects of clonazepam and acupressure on these patients' sleep quality.
Conclusion
The findings of this study demonstrated that acupressure therapy and clonazepam tablets both improved the quality of hemodialysis patients' sleep. However, acupressure was more successful than clonazepam at enhancing patients' sleep quality. As a result, given the high prevalence of sleep disorders in these patients, this study recommends acupressure as a non-pharmacological method in the management of sleep disorders in these patients. Acupressure is advantageous as in addition to having no side effects, it is a practical and simple method that can be readily used by nurses and patients themselves.
Acknowledgment
The authors would like to express their thanks to the Vice-Chancellor of Technology and Research of Mazandaran University of Medical Sciences for receiving the grant (No: 9277). The authors also express their appreciation to officials, nurses and patients of the Shahrvand Renal Medical Center in Sari.
Conflict of Interest
None.
References
- 1.Tayebi A, Kasra Dehkordi A, Ebadi A, Sahraei H, Einollahi B. The effect of aromatherapy with lavender essential oil on depression, anxiety and stress in hemodialysis patients: A clinical trial. Evid Based Care J. 2015;5(2):65–74. [Google Scholar]
- 2.Kanani M, Mazloum S, Emami A, Mokhber N. The effect of aromatherapy with orange essential oils on anxiety in patients undergoing hemodialysis. JSUMS. 2012;19(13):249–257. [Google Scholar]
- 3.Hydarinia Naieni Z, Nobahar M, Ghorbani R. The relationship between sleep quality in patients' undergoing hemodialysis at different therapeutic'shifts. Koomesh. 2016;18(1):42–50. [Google Scholar]
- 4.Einollahi B, Motalebi M, Rostami Z, Nemati E, Salesi M. Sleep quality among Iranian hemodialysis patients: a multicenter study. Nephrourol Mon. 2015;7(1):e23849. doi: 10.5812/numonthly.23849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zarurati M, Pishgooie SAH. The effect of music therapy on comfort level and some vital signs of patients undergoing hemodialysismodialysis. Mil Caring Sci. 2017;3(4):221–32. [Google Scholar]
- 6.Arzhangi R, Ghasemi S, Mohammadi S, Norouzi M, Norouzi K. Investigating the relationship between health literacy and quality of life on hemodialysis patients in selected medical centers under the auspices of Ardabil University of Medical Sciences. IJRN. 2022;8(2):21–31. [Google Scholar]
- 7.Molaie E, Royani Z, Moujerloo M, Behnampour N, Golage J, Khari M. Anxiety, depression and quality of sleep related to fatigue in patients undergoing hemodialysis. J Res Dev Nurs Midw. 2014;11(1):99–107. [Google Scholar]
- 8.Zheng C, Xu J, Chen C, Lin F, Shao R, Lin Z, et al. Effects of sleep disorders and sedative-hypnotic medications on health-related quality of life in dialysis patients. Int Urol Nephrol. 2019;51(1):163–74. doi: 10.1007/s11255-018-2018-3. [DOI] [PubMed] [Google Scholar]
- 9.Najafi Z, Tagharrobi Z, Shahriyari-Kale-Masihi M. Effect of aromatherapy with Lavender on sleep quality among patients undergoing hemodialysis. KAUMS Journal (FEYZ) 2014;18(2):145–50. [Google Scholar]
- 10.Shibata S, Tsutou A, Shiotani H. Relation between sleep quality and daily physical activity in hemodialysis outpatients. Kobe J Med Sci. 2014;59(5):E161–6. [PubMed] [Google Scholar]
- 11.Mirghaed MT, Sepehrian R, Rakhshan A, Gorji H. Sleep Quality in Iranian Hemodialysis Patients: A Systematic Review and Meta-analysis. Iran J Nurs Midwifery Res. 2019;24(6):403–9. doi: 10.4103/ijnmr.IJNMR_184_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.vatandoost s, Mohammadi H, nouri b, mohammadi bolbanabad a, zamani p. Relation between dialysis adequacy and sleep quality in hemodialysis patients. The J Urmia Nurs Midwifery Fac. 2018;16(1):30–7. [Google Scholar]
- 13.Soleimani M, Asgari M, Imani A, Tammadon M. The effect of cool temperature dialysate on sleep quality in hemodialysis patients. J Adv Med Biomed Res. 2017;25(111):128–38. [Google Scholar]
- 14.Mahmoud MM, AboZead SE, Mohammad WH, El-all A, Abd ElRazik H. Assessment Quality of Sleep in Patients undergoing Hemodialysis. Assiut sci nurs j. 2019;7(17):74–80. [Google Scholar]
- 15.Wu Y, Yang L, Li L, Wu X, Zhong Z, He Z, et al. Auricular acupressure for insomnia in hemodialysis patients: study protocol for a randomized controlled trial. Trials. 2018;19(1):171. doi: 10.1186/s13063-018-2546-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shen K, Cho Y, Pascoe EM, Hawley CM, Oliver V, Hughes KM, et al. The SIESTA Trial: A Randomized Study Investigating the Efficacy, Safety, and Tolerability of Acupressure versus Sham Therapy for Improving Sleep Quality in Patients with End-Stage Kidney Disease on Hemodialysis. Evid Based Complement Alternat Med. 2017;2017:7570352. doi: 10.1155/2017/7570352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Arache W, Laboudi F, Ouanass A, el kabbaj D. Poor quality of sleep in patients on chronic hemodialysis. Ibnosina J Med Biomed Sci. 2019;11(1):20–4. [Google Scholar]
- 18.Kasra Dehkordi A, Ebadi A, Sahraei H, Einollahi B. Effects of aromatherapy with lavender on sleep quality of hemodialysis patients (A Clinical Trial) Nurs midwifery res j. 2016;13(11):995–1003. [Google Scholar]
- 19.Arab Z, Shariati A, Bahrami H, Asayesh H, Vakili M. The effect of acupressure on quality of sleep in hemodialysis patients. The J Urmia Nurs Midwifery Fac. 2012;10(2):237–45. [Google Scholar]
- 20.Dashti-Khavidaki S, Chamani N, Khalili H, Hajhossein Talasaz A, Ahmadi F, Lessan-Pezeshki M, et al. Comparing effects of clonazepam and zolpidem on sleep quality of patients on maintenance hemodialysis. Iran J Kidney Dis. 2011;5(6):404–9. [PubMed] [Google Scholar]
- 21.Kamrani F, Nazari M, Sahebalzamani M, Amin G, Farajzadeh M. Effect of aromatherapy with lemon essential oil on anxiety after orthopedic surgery. Iran Rehabil J. 2016;2(4):26–31. [Google Scholar]
- 22.Wang X, Gu J, Liu J, Hong H. Clinical evidence for acupressure with the improvement of sleep disorders in hemodialysis patients: A systematic review and meta-analysis. Complement Ther Clin Pract. 2020;39:101151. doi: 10.1016/j.ctcp.2020.101151. [DOI] [PubMed] [Google Scholar]
- 23.Rehman IU, Wu DB, Ahmed R, Khan NA, Rahman AU, Munib S, et al. A randomized controlled trial for effectiveness of zolpidem versus acupressure on sleep in hemodialysis patients having chronic kidney disease-associated pruritus. Medicine (Baltimore) 2018;97(31):e10764. doi: 10.1097/MD.0000000000010764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shahdadi H, Allah-yari J, Mansouri A. Effect of acupressure on sleep quality in patients with diabetes mellitus. J Diabetes Nurs. 2017;5(2):78–85. [Google Scholar]
- 25.Shafiee-Darabi S-M, Khankeh H, Fallahi-Khoshknab M, Soltani P-R. Effect of acupressure on pain and fatigue in people with chronic heart failure. J Cardiovasc Nurs. 2015;3(4):14–22. [Google Scholar]
- 26.Emamverdi M, Mohammadpour A, Badiee Aval S, Sajjadi M. Comparing the effects of reflexology massage and acupressure on the quality of sleep in hemodialysis patients: A randomized clinical trial. J Maz Univ Med. 2019;29(176):34–46. [Google Scholar]
- 27.Aslani MA, Hanifi N, Ahmadi F, Fallah R. Effect of Acupressure on Amount of Gastric Emptying in Mechanically Ventilated Patients Hospitalized in Intensive Care Units. Hayat. 2014;20(2):69–81. [Google Scholar]
- 28.Dincer B, İnangil D, İnangil G, Bahçecik N, Ayaz EY, Arslanoğlu A, et al. The effect of acupressure on sleep quality of older people: A systematic review and meta-analysis of randomized controlled trials. Explore (NY) 2022;18(6):635–45. doi: 10.1016/j.explore.2021.11.010. [DOI] [PubMed] [Google Scholar]
- 29.Nasiri E, Raei M, Vatani J, Khajeh-Kazemi R. The effect of acupressure on sleep quality in hemodialysis patients. Shahroud University of Medical Sciences,Iran. 2011;11(5):236–40. [Google Scholar]
- 30.Folstein M. A practical method for grading the cognitive state of patients for the children. J Psychiatr Res. 1975;12:189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 31.Mitchell AJ. A meta-analysis of the accuracy of the mini-mental state examination in the detection of dementia and mild cognitive impairment. J Psychiatr Res. 2009;43(4):411–31. doi: 10.1016/j.jpsychires.2008.04.014. [DOI] [PubMed] [Google Scholar]
- 32.Mitchell AJ, Malladi S. Screening and case finding tools for the detection of dementia. Part I: evidence-based meta-analysis of multidomain tests. Am J Geriatr Psychiatry. 2010;18(9):759–82. doi: 10.1097/JGP.0b013e3181cdecb8. [DOI] [PubMed] [Google Scholar]
- 33.Stephan BC, Matthews FE, McKeith IG, Bond J, Brayne C. Early cognitive change in the general population: how do different definitions work? J Am Geriatr Soc. 2007;55(10):1534–40. doi: 10.1111/j.1532-5415.2007.01386.x. [DOI] [PubMed] [Google Scholar]
- 34.Seyedian M, Falah M, Nourouzian M, Nejat S, Delavar A, Ghasemzadeh H. Validity of the Farsi version of mini-mental state examination. J Med Counc Iran. 2008;25(4):408–14. [Google Scholar]
- 35.Gaudreau JD, Gagnon P, Harel F, Tremblay A, Roy MA. Fast, systematic, and continuous delirium assessment in hospitalized patients: the nursing delirium screening scale. J Pain Symptom Manage. 2005;29(4):368–75. doi: 10.1016/j.jpainsymman.2004.07.009. [DOI] [PubMed] [Google Scholar]
- 36.Ghana S, Saeedi S, Sanagoo A. The incidence of delirium in patients after surgery in recovery room. Jorjani Biomed J. 2012;1(1):23–9. [Google Scholar]
- 37.Farrahi J, Nakhaee N, Sheibani V, Garrusi B, Amirkafi A. Psychometric properties of the Persian version of the Pittsburgh Sleep Quality Index addendum for PTSD (PSQI-A) Sleep Breath. 2009;13(3):259–62. doi: 10.1007/s11325-008-0233-3. [DOI] [PubMed] [Google Scholar]
- 38.Safa A, Adib-Hajbaghery M, Fazel-Darbandi A. The relationship between sleep quality and quality of life in older adults. IJPN. 2015;3(3):53–62. [Google Scholar]
- 39.Farhadi Nasab A, Azimi H. Study of patterns and subjective quality of sleep and their correlation with personality traits among medical students of hamadan university of medical sciences. Avicenna J Clin Med. 2008;15(1):11–5. [Google Scholar]
- 40.Shariati A, Jahani S, Hooshmand M, Khalili N. The effect of acupressure on sleep quality in hemodialysis patients. Complement Ther Med. 2012;20(6):417–23. doi: 10.1016/j.ctim.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 41.Aygin D, Şen S. Acupressure on Anxiety and Sleep Quality After Cardiac Surgery: A Randomized Controlled Trial. J Perianesth Nurs. 2019;34(6):1222–31. doi: 10.1016/j.jopan.2019.03.014. [DOI] [PubMed] [Google Scholar]
- 42.Jokar A, Zynali F, Akbarzade M, Zare N. Comparison of the effects of acupressure at Yong Quan (KI-1) and Hegu (LI-4) acupoints on hot flashes in menopaus: clinical trial. J Adv Med Biomed Res. 2017;25(108):1–10. [Google Scholar]
- 43.Adib-Hajbaghery M, Etri M, Hosseinian M. The effect of acupressure on the Pericardium 6 point on pain, nausea and vomiting after appendectomy. J Complement Med. 2012;2(2):171–82. [Google Scholar]
- 44.Akbarzadeh R, koushan M, Rakhshani M, Hashemi NS. Effect of the benson relaxation technique on quality of sleep in patients with chronic heart disease. Quarterly Journal of Sabzevar University of Medical Sciences. 2014;21(3):492–500. [Google Scholar]
- 45.Yeung WF, Ho FYY, Chung KF, Zhang ZJ, Yu BYM, Suen LKP, et al. Self‐administered acupressure for insomnia disorder: a pilot randomized controlled trial. J Sleep Res. 2018;27(2):220–31. doi: 10.1111/jsr.12597. [DOI] [PubMed] [Google Scholar]
- 46.Rueff-Barroso CR, Delpupo FVB, Fazan VPS, Nascimento SRR, Nunes LF, Montenegro RN, et al. Clinical and anatomical aspects of anterior dislocation of the pisiform bone. J Morphol Sci. 2019;36(2):134–7. [Google Scholar]
- 47.Kilduff TS, Mendelson WB, editors. Chapter 41 – Hypnotic Medications: Mechanisms of Action and Pharmacologic Effects2017. [Google Scholar]
- 48.Arun R, Venkateshan M. Effectiveness of Acupressure on Quality of Sleep of Hemodialysis Patients. Int J Nurs Educ. 2019;11(1) [Google Scholar]