Abstract
Objectives
To conduct a comprehensive scoping review focusing on published anesthesiology-specific training based on simulation to assess up-to-date uses of simulation-based education in anesthesiology training. Our goal was to establish a solid ground for building standardized and accredited curricula for simulation-based education in the specialty of anesthesia in the near future.
Methods
We searched the PubMed, CINAHL and EMBASE databases on May 10, 2021 for relevant articles. We followed the five-stage scoping review methodology: identifying a research question, identifying relevant studies, study selection, charting the data, and synthesis of results.
Results
Our initial electronic search identified 5609 potential articles. After abstract screening and removing duplicates, 636 articles were evaluated in full text for inclusion or exclusion. Based on this strategy, 283 articles were included in this review. We mapped the current practice of simulation in training and certification across different anesthesiology subspecialties.
Conclusions
Significant effort has been placed into the use of simulation for training, certification, and recertification in anesthesiology. Future effort to develop simulation-based training that can be generalized to trainees in this specialty, similar to other fields such as aviation and space sciences, will enhance the standardization of training and hence patient safety.
Keywords: Anesthesia, Certification, Education, Recertification, Residency, Simulation
الملخص
أهداف البحث
تم إجراء هذه الورقة لإجراء مراجعة نطاق شاملة تركز على التدريب المنشور الخاص بالتخدير بناءً على المحاكاة لتقييم الاستخدامات الحديثة للتعليم القائم على المحاكاة في التدريب على التخدير. هدفنا هو إنشاء موثوقية لبناء مناهج موحدة ومعتمدة للتعليم القائم على المحاكاة في تخصص التخدير في المستقبل القريب.
طريقة البحث
تم البحث في المقالات في ” ببميد “ و ”سيناهل“ و ”إمبيز“ في 10 مايو 2021م. لقد اتبعنا منهجية مراجعة النطاق المكونة من خمس مراحل: تحديد سؤال البحث، وتحديد الدراسات ذات الصلة، واختيار الدراسة، ورسم البيانات وتوليف النتائج.
النتائج
حدد بحثنا الإلكتروني الأولي 5609 مقالة محتملة. بعد فحص الملخصات وإزالة التكرارات، تم تقييم 636 مقالة في النص الكامل لإدراجها أو استبعادها. وبناء على ذلك، تم تضمين 283 مقالة في هذه المراجعة. قمنا برسم خريطة الممارسة الحالية للمحاكاة في التدريب ومنح الشهادات عبر تخصصات فرعية مختلفة من التخدير.
الاستنتاجات
لقد تم بذل جهد كبير في استخدام المحاكاة للتدريب ومنح الشهادات وإعادة التأهيل في مجال التخدير. الجهود المستقبلية لتطوير تدريب قائم على المحاكاة يمكن تعميمه على المتدربين في هذا التخصص، على غرار المجالات الأخرى مثل علوم الطيران والفضاء لتعزيز توحيد التدريب وبالتالي سلامة المرضى.
الكلمات المفتاحية: التخدير, الشهادة, التعليم, إعادة التأهيل, الإقامة, المحاكاة
Introduction
The development of mannequin simulators and simulation programs for education and training was greatly aided by anesthesiologists. It is already over half a century since the introduction of the first fully automated cardiac auscultation mannequin as a modern-day simulator (Singh et al., 2013). Many remarkable advances have been developed, implemented and flourished in practice to further augment the permanent place of simulation-based education (SBE) in anesthesiology and many other medical and health educational programs.
Since the 1990s, medical students and anesthesiology residents have received extensive training on high-fidelity simulators. With simulator training, anesthesia residents answered more quickly and performed better.1 The rapid and progressive increase in professional realization about the utility and usefulness of SBE in anesthesiology is evidenced by the growth of courses, centers, users, and publications. This fast growth is evident in many dimensions. In addition to larger user numbers, the utility of SBE in anesthesiology has been growing in terms of various forms, modalities, technologies and interfaces.1
We conducted a comprehensive scoping review to focus on published anesthesiology-specific training based on simulation to assess the current use of SBE in anesthesiology training. The purpose of our review was to investigate and define the body of literature and concepts of SBE modalities used in anesthesiology training, certification, and recertification to serve as a guide for implementation in different programs globally and to represent the basis for future research effort.
Materials and Methods
Our approach was to conduct a scoping review rather than a systemic or narrative review due to the large body and vast variability in the existing research which preclude from properly assessing and conducting analysis. By identifying the body of literature through a scoping review, findings can be used in the future as a precursor to for a rigorous systemic or narrative review.2
For this review, we followed the four-stage scoping review methodology as described by Arksey and O'Malley's framework.3 The stages and their application in this study are described as follows.
Stage 1: Identifying the research question
To ensure a wide range of results, we asked a broad question: what are the simulation modalities that have been used in training anesthesia residents or in the primary certification or recertification of anesthesia physicians? Our population focused on anesthesia residents or anesthesia physicians sitting for primary or recertification.
Stage 2: Identifying relevant studies
With the aid of a librarian, we searched PubMed, CINAHL and EMBASE databases on May 10, 2021 for relevant articles (Appendix 1). We also searched gray literature via Google Scholar and simulation and anesthesia societies databases.
Stage 3: Study selection
After performing the search, we used the following criteria to include or exclude articles:
Inclusion criteria:
-
1.
Articles with simulation-based interventions where residency training, certification, or recertification was the main goal.
Exclusion criteria:
Simulation-based training not geared towards residency training, certification, or recertification of an anesthesiologist.
Initially, titles and abstracts were sequenced and reviewed by two independent authors for inclusion. Full articles of the included abstracts were screened again by two independent authors for final inclusion. In the case of different findings at any step, we used a third senior author to moderate and derive a final decision.
Stage 4: Charting the data
Final data extraction from the included articles was completed by two independent authors in a similar manner. We extracted the following data: author's name, title, publication date, subspeciality, and topic of training.
Stage 5: Synthesis of results
The included articles were categorized based on subspecialties of training. We further described the topic of training in each article in a quantitative manner (Appendix 2).
Results
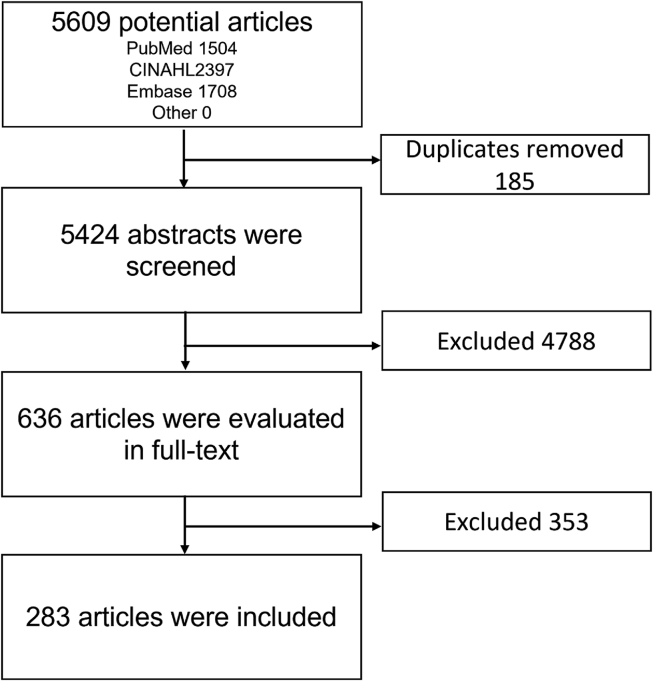
Our initial electronic search identified 5609 potential articles and no articles were added based on a manual search by hand. After abstract screening and removing duplicates, 636 articles were evaluated in full text for inclusion or exclusion. Based on this strategy, 306 articles were included in this review. The PRISMA flow diagram shown in Figure 1 provides a summary of the selection process and a detailed list of included articles is given in Appendix 2.
Figure 1.
PRISMA flow diagram summarizing the selection process.
Using thematic coding, the 283 included articles were organized based on the main training subspeciality. We identified 112 articles about general anesthesia, 57 articles about non-technical skills (NTS) training, 40 about regional anesthesia, 23 about obstetrics anesthesia, 20 about cardiothoracic anesthesia, 10 about critical care, 9 about certification/recertification in anesthesia, 6 about pediatrics anesthesia, and 6 about chronic pain management.
A detailed topics list divided by specialty is given in Table 1. The number of articles varied greatly between different specialties. The number of topics per specialty also varied greatly. Numerically, the number of unique topics were as follows: general anesthesia (112 articles), followed by non-technical skills training (57 topics), regional anesthesia (40 topics), obstetrics anesthesia (23 topics), cardiothoracic anesthesia (20 topics), critical care (10 topics), certification/recertification (9 topics), pediatric anesthesia (6 topics), and pain (6 topics).
Table 1.
Training topics divided by specialty.
| Specialty | Number of articles | Topics |
|---|---|---|
| General Anesthesia | 112 | Advanced cardiac life support, cricoid pressure, basic airway management, advanced airway management (including videolaryngoscopy, fiberoptic and blind intubation), difficult airway, out of operating room airway management, bronchoscopy training, surgical airway, airway emergencies, anesthetics emergencies, intraoperative care, arterial access, central venous access, career re-entry, mass casualty, delayed emergence, electroencephalogram (EEG) monitoring, equipment failure, machine check, estimated blood loss, hemorrhage, volume management, hand hygiene, inhaled anesthetics, liver transplant, trauma, malignant hyperthermia, mechanical ventilation, medication error, novice anesthesiology programs, patient safety, perioperative care, rapid sequence intubation, sepsis in the operating room and World Health Organization (WHO) preoperative checklist. |
| NTS | 57 | Communication skills, breaking bad news, cognitive aid, conflict management, Crisis Resource Management (CRM), fatigue, opioid addiction, patient hand off, human factors, ANTS, OR environment safety, team training, wellness and stress and workload. |
| Regional Anesthesia | 40 | Anesthesia emergencies, axillary brachial plexus block, brachial plexus block, crisis resource management (CRM), Femoral nerve block, interscalene blocks, Local anesthetics toxicity, lower extremity block, Lumbar puncture, needle driving, paravertebral block, spinal sonoanatomy, supraclavicular block, ultrasound-guided regional anesthesia and transversus abdominis plane block. |
| Obstetrics Anesthesia | 23 | Airway emergencies, anesthesia obstetric crisis, aseptic techniques, cardiopulmonary resuscitation, crisis resource management (CRM), epidural anesthesia, failed intubation, general anesthesia for cesarean delivery, high neuraxial block, informed consent, interdisciplinary care, postpartum hemorrhage, rapid response team and team training. |
| Cardiothoracic Anesthesia | 20 | Cardiac ultrasound, cardiopulmonary bypass, chest drain, single lung isolation, tracheoesophageal echocardiogram and transthoracic echocardiogram. |
| Critical care | 10 | Bronchoscopy, hemorrhage, anticoagulation, septic shock, arrhythmia, Interhospital transfer, tracheostomy/laryngectomy care, point of care ultrasound, novice course, anaphylaxis and critical events. |
| Certification/recertification | 9 | Primary certification, regional anesthesia, primary certification, milestones and recertification. |
| Pediatric Anesthesia | 6 | Emergencies in pediatric anesthesia, induction of anesthesia in an infant, Infant's airway management, surgical airway, perioperative care, difficult airway, airway scope. |
| Pain | 6 | CRM, lumbar sympathetic block, transforaminal epidural injection, radiation exposure and cervical medial branch block. |
No quantitative statistical analysis was completed due to the high variability of topics, designs, and measurement tools in these articles.
Discussion
In this scoping review, we accumulated and organized literature published on SBE modalities to serve as a guide of choice for educators around the globe. Adopting this guide to develop global standardization will significantly enhance education, assessment and certification in anesthesiology and address the global worldwide anesthesia workforce deficiency and competency assessment crisis.4, 5, 6
Multiple publications relating to SBE in anesthesiology have shown promising results with regards to its application in anesthesia training, certification, and recertification. However, due to the high variability in study design and application of these publications, there is no strong evidence to support its universal application as a mandatory step. Furthermore, these variabilities preclude its application globally to unify the efforts in addressing shortages in the anesthesiologist workforce.
Traditionally, anesthesiologists gain experience in managing routine and critical events as they are exposed to patients. By the nature of their chosen field of specialization, they are dealing with dangerous and life-threatening situations with a narrow margin of error. These events are uncommon and many cases are rare and totally inconsistent in occurrence. To improve the education of future generations of anesthesia practitioners and provide consistent training outcomes, anesthesiologists have been very early adopters of simulation-based education (SBE) in training. Over the past decades,anesthesiology as a specialty, together with many critical care and emergency medicine specialties, have grown as major leading champions in medical fields in terms of using SBE for training, assessment, evaluation, certification, and recertification purposes.7,8
Although our review highlights the vast number and variety of anesthesiology simulation-based education (ASBE), this comes with high variability in design and delivery, resulting in the inability to synthesize strong evidence to support its validity and efficacy. Additionally, our results show that certain topics and subspecialties have adopted the use of ASBE for general anesthesia, regional anesthesia, and NTS on a much broader basis than critical care and pain medicine. This could be explained by the fact that new and emerging specialties such as NTS and regional anesthesia have adopted simulation during their infancy while older specialties are still heavily dependent on the classical education curriculum. Nonetheless, in the absence of compelling evidence to support ASBE, justifying the higher cost, resources, and efforts to support this strategy might be difficult.9 Moving forward, it is critical to address this issue by incorporating simulation-based education in all subspecialties and most importantly synthesizing credible research-based evidence to support this modality.
As for anesthesiology simulation-based certification and recertification (ASBCR), our review identified a major lack of publications relating to modalities or evidence. Only a few institutes, such as the Accreditation Council for Graduate Medical Education American Board of Anesthesiology and the Israeli National Board Examination in Anesthesiology have published their data; this is due to both the lack of use of ASBCR globally and the lack of scholarly work to support ASBCR. As with ASBE, ASBCR requires more evidence to be integrated more widely on a global basis.10, 11, 12
The main limitation of this review that we did not assess the quality of each article or the overall quality of evidence since many of the included articles were missing data about their design, thus preventing us from properly assessing their quality. Furthermore, assessing quality was beyond the scope of our review. Instead, we intended to use this review as a basic guide for educators to adopt existing literature for ASBE, ASBCR, and research purposes.
A unified effort based on our guide will contribute greatly to the future expansion of evidence based ASBEs and ASBCRs, and may help to address the global anesthesia workforce crisis.6
In summary, we collected research articles published on the use of SBE in anesthesiology training certification and recertification in all subspecialties so that this information could be used to unify efforts and modalities for future application in our field. The guide will also help to advance scholarly activities to build better evidence-based applications to support SBE in anesthesiology. We make the case to develop minimum level standard training requirements for all anesthesiologists as a first step in the standardization process. Finally, unifying the effort based on our findings will potentially reduce the variability and increase the validity of the potential benefit to address the global shortage of anesthesia workforce.
Source of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest
The authors have no conflict of interest to declare.
Ethical approval
Ethics approval was obtained from King Abdulaziz University Hospital Research Ethical Committee on 4 May 2020 (reference number 20-267).
Authors’ contribution
BT and AB conceived and designed the study, collected data, analyzed data, wrote and reviewed the manuscript, and supervised the project. KD, FS, AY, DD, EA and MA collected, analyzed and interpreted data and participated in writing the manuscript. All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
Acknowledgments
The authors would like to thank Dr. Daniel Carr and Amy Lapidow from Tufts Medical School for their assistance with conducting the literature search and their guidance at the start of this project.
Footnotes
Peer review under responsibility of Taibah University.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jtumed.2023.03.015.
Appendix A. Supplementary data
The following is/are the supplementary data to this article:
References
- 1.Lorello G.R., Cook D.A., Johnson R.L., Brydges R. Simulation-based training in anaesthesiology: a systematic review and meta-analysis. Br J Anaesth. 2014;112(2):231–245. doi: 10.1093/bja/aet414. [DOI] [PubMed] [Google Scholar]
- 2.Munn Z., Peters M.D.J., Tufanaru C., Stern C., McArthur A., Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18:143. doi: 10.1186/s12874-018-0611-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bosco L., Lorello G.R., Flexman A.M., Hastie M.J. Women in anaesthesia: a scoping review. Br J Anaesth. 2020;124(3):e134–e147. doi: 10.1016/j.bja.2019.12.021. [DOI] [PubMed] [Google Scholar]
- 4.Dubowitz G., Detlefs S., McQueen K.A.K. Global anesthesia workforce crisis: a preliminary survey revealing shortages contributing to undesirable outcomes and unsafe practices. World J Surg. 2010;34(3):438–444. doi: 10.1007/s00268-009-0229-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Epiu I., Tindimwebwa J.V.B., Mijumbi C., Chokwe T.M., Lugazia E., Ndarugirire F., et al. Challenges of anesthesia in low- and middle-income countries: a cross-sectional survey of access to safe obstetric anesthesia in East Africa. Anesth Analg. 2017;124(1):290–299. doi: 10.1213/ANE.0000000000001690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kempthorne P., Morriss W.W., Mellin-Olsen J., Gore-Booth J. The WFSA global anesthesia workforce survey. Anesth Analg. 2017;125(3):981–990. doi: 10.1213/ANE.0000000000002258. [DOI] [PubMed] [Google Scholar]
- 7.Riem N., Boet S., Chandra D. Setting standards for simulation in anesthesia: the role of safety criteria in accreditation standards. Can J Anaesth. 2011;58(9):846–852. doi: 10.1007/s12630-011-9541-3. [DOI] [PubMed] [Google Scholar]
- 8.Henson L.C., Lee A.C. Springer US; 2013. Simulators in anesthesiology education; pp. 115–118. [Google Scholar]
- 9.Maloney S., Haines T. Issues of cost-benefit and cost-effectiveness for simulation in health professions education. Adv Simulat. 2016;1:13. doi: 10.1186/s41077-016-0020-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Isaak R.S., Chen F., Martinelli S.M., Arora H., Zvara D.A., Hobbs G., et al. Validity of simulation-based assessment for accreditation Council for graduate medical education milestone achievement. Simulat Healthc J Soc Med Simulat J Soc Simulat Healthcare. 2018;13(3):201–210. doi: 10.1097/SIH.0000000000000285. [DOI] [PubMed] [Google Scholar]
- 11.Rochlen L.R., Tarnal V., Vance J.L., Alderink E., Bernstein W.K. Modules for the technical skills section of the OSCE component of the American board of anesthesiology APPLIED examination. J Teach Learn Resources. 2019;15 doi: 10.15766/mep_2374-8265.10820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Berkenstadt H., Ziv A., Gafni N., Sidi A. The validation process of incorporating simulation-based accreditation into the anesthesiology Israeli national board exams. Isr Med Assoc J: IMAJ. 2006;8(10):728–733. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.