Abstract
Background:
Observational data investigating the relationship between body habitus and outcomes in breast cancer have been variable and inconsistent, largely centered in the curative setting and focused on weight-based metrics. This study evaluated the impact of muscle measures on outcomes in patients with metastatic breast cancer receiving endocrine-based therapy.
Methods:
Baseline CT scans were collected from ECOG-ACRIN E2112, a randomized phase III placebo-controlled study of exemestane with or without entinostat. A CT cross-sectional image at the L3 level was extracted to obtain skeletal muscle mass and attenuation. Low muscle mass (LMM) was defined as skeletal muscle index <41 cm2/m2 and low muscle attenuation (LMA) as muscle density <25 HU or <33 HU if overweight/obese by body mass index (BMI). Multivariable Cox proportional hazard models determined the association between LMM or LMA and progression-free survival (PFS) and overall survival (OS). Correlations between LMM, LMA, and patient-reported outcomes were determined using 2-sample t tests.
Results:
Analyzable CT scans and follow-up data were available for 540 of 608 patients. LMM was present in 39% (n=212) of patients and LMA in 56% (n=301). Those with LMA were more likely to have obesity and worse performance status. LMM was not associated with survival (PFS hazard ratio [HR]: 1.13, P=.23; OS HR: 1.05, P=.68), nor was LMA (PFS HR: 1.01, P=.93; OS HR: 1.00, P=.99). BMI was not associated with survival. LMA, but not LMM, was associated with increased frequency of patient-reported muscle aches.
Conclusions:
Both low muscle mass and density are prevalent in patients with hormone receptor–positive metastatic breast cancer. Muscle measures correlated with obesity and performance status; however, neither muscle mass nor attenuation were associated with prognosis. Further work is needed to refine body composition measurements and select optimal cutoffs with meaningful endpoints in specific breast cancer populations, particularly those living with metastatic disease.
Background
Observational data investigating the relationship between body habitus and outcomes in breast cancer have been largely centered in the curative setting and focused on weight-based metrics, with variable and inconsistent results. Body weight, or weight-based metrics, such as body mass index (BMI), do not tell a complete story, because body composition is highly variable with respect to muscle and adipose tissue. Muscle is a large, active endocrine organ affecting physical function, quality of life, metabolism, and inflammation, and may impact outcome or toxicity in response to anticancer therapy.
Low muscle mass (LMM) has been associated with reduced survival and increased toxicity in advanced solid tumor malignancies.1,2 Low muscle attenuation (LMA), reflecting muscle “quality” and intramuscular fat infiltration, is also associated with poor survival outcomes and worse treatment tolerability.3,4 Compared with muscle mass, muscle attenuation appears to be a better predictor of muscle strength and physical function.5 In the setting of early-stage breast cancer specifically, LMM and LMA are both prognostic of significantly worse overall survival (OS), and both are more significant prognosticators than BMI.6 The few studies that have investigated muscle measures in patients with metastatic breast cancer (MBC) have been small and focused on patients receiving cytotoxic chemotherapy.7–9 Most patients with MBC, however, receive endocrine therapy as a treatment backbone at least in the first few years after diagnosis. In addition, patients with hormone receptor–positive breast cancer have potentially long survival that could be impacted positively by interventions focused on body composition and lifestyle modifications. Investigating the relationship between muscle characteristics and outcomes in hormone receptor–positive MBC may thus further refine our understanding of prognostic variables and mechanisms of therapeutic resistance, and identify opportunities for intervention.
To date, there has been limited evaluation of how muscle characteristics affect outcome or toxicity in patients receiving endocrine therapy for MBC. We hypothesized that LMM and LMA are prognostic of worse progression-free survival (PFS) and OS, as well as worse patient-reported quality of life, specifically in patients receiving endocrine-based therapy for MBC. We used clinical data and CT images from ECOG-ACRIN E2112, a randomized, placebo-controlled double-blind phase III study of exemestane with or without the histone deacetylase inhibitor entinostat in hormone receptor–positive MBC,10 to investigate the impact of muscle measures on outcomes.
Methods
Patient Population
ECOG-ACRIN E2112 was a phase III, randomized controlled trial of entinostat versus placebo in combination with exemestane in men or women with advanced hormone receptor–positive, HER2-negative breast cancer who had been previously treated with a nonsteroidal aromatase inhibitor. Trial eligibility and schema have been previously published.10 The study was open from March 2014 to October 2018 at 111 centers in the United States and South Africa. Participants eligible for this post hoc analysis included women with available CT scans of the abdomen collected for central review of sufficient quality for analysis of muscle measures and survival outcome data.
Measurement of Muscle Mass and Attenuation
Baseline imaging was performed within 4 weeks prior to randomization. Imaging included CT of the chest and CT or MRI of the abdomen and pelvis. CT scans of the abdomen received for central review were evaluated for muscle mass and attenuation. A single cross-sectional image at the level of the midthird lumbar vertebrae was extracted because muscle area at that level is linearly related to whole-body muscle mass.11 SliceOmatic 5.0 software (TomoVision) was used to process axial DICOM(Digital Imaging and Communications in Medicine) standard images, providing an accurate estimation of cross-sectional skeletal muscle area and muscle attenuation with high interobserver reliability.12 Two trained investigators (G. Xue, R. Hoffman) extracted the CT images and segmented muscle tissue using the semiautomated software. Muscle cross-sectional area was quantified in centimeters squared by tissue-specific Hounsfield unit (HU) ranges to discriminate muscle. A subset of images (10%) was read by both investigators, with a coefficient of variation of 0.14 for muscle area.
LMM was defined as skeletal muscle index (SMI; lean muscle area/height) <41 cm2/m2. LMA was defined as average muscle density on the L3 slice <41 HU, or <33 HU if the patient was overweight or obese by BMI. These cut points are based on previously determined thresholds associated with reduced survival in patients with metastatic solid tumors.1
Statistical Analysis
The primary objective of this study was to determine the prognostic value of LMM and LMA on PFS and OS. PFS was defined as duration of time from baseline CT imaging to a PFS event, including local invasive disease, regional recurrence, distant disease recurrence, contralateral breast cancer, or death from any cause. OS was assessed from the date of imaging until death or end of follow-up. Secondary endpoints included patient-reported outcomes.
Baseline patient characteristics and muscle measures were analyzed using descriptive statistics. Comparisons between those patient characteristics with binary LMM and LMA were performed using a t test for continuous variables and a chi-square test for categorical variables. Survival probability was estimated using the Kaplan-Meier method. Multivariable Cox proportional hazard models were used to model the association between LMM or LMA and PFS or OS while adjusting for age, race, prior chemotherapy, ECOG performance status (PS), and BMI. Additionally, as an exploratory analysis, we performed optimal stratification to determine whether alternative cut points than those in existing literature are prognostic of worse survival outcomes in this specific population.
The correlation between LMM and LMA and patient-reported quality of life and endocrine therapy symptoms of muscle ache and joint pain was assessed using the patient-reported outcome questionnaires FACT-G (Functional Assessment of Cancer Therapy—General), Patient-Reported Outcomes Measurement Information System (PROMIS)–Fatigue, and Patient-Reported Outcomes version of the CTCAE (PRO-CTCAE) muscle ache and joint pain obtained after three 28-day cycles of therapy. Two-sample t tests were used to compare mean scores in those who had LMM or LMA at baseline with those who did not.
Results
Patient Demographics and Muscle Characteristics
We previously reported results from the parent trial, showing no difference in the coprimary endpoints of PFS or OS by study arm.10 The final study set for this analysis included 540 participants with available and analyzable CT scan images and follow-up data available (supplemental eFigure 1, available with this article at JNCCN.org). Baseline characteristics of the participants are summarized in Table 1. A large portion of the participants were obese by BMI (n=242; 44.8%), and approximately one-third had prior chemotherapy in the metastatic setting (n=94; 29.8%). LMM was seen in 39.3% (n=212) and LMA in 55.8% (n=301) of participants. Total adipose tissue (subcutaneous plus visceral) was also measured but is not reported or analyzed here, because approximately 20% of participants had adipose tissue that was outside the edges of the CT scan images; therefore, any analysis would be biased to individuals with less subcutaneous adiposity.
Table 1.
Baseline Characteristics
| n (%) | |
|---|---|
| Total, n | 540 |
| Age, mean [SD], y | 63.2 [11.49] |
| Race | |
| White | 434 (80.4) |
| Black or African American | 82 (15.2) |
| Othera | 24 (4.4) |
| Ethnicity | |
| Hispanic or Latino | 34 (6.3) |
| Not Hispanic or Latino | 497 (92.0) |
| Unknown | 9 (1.7) |
| ECOG performance status | |
| 0 | 315 (58.3) |
| 1 | 225 (41.7) |
| BMI, mean [SD], kg/m2 | 29.9 [7.02] |
| BMI, groups | |
| Underweight: <18.5 kg/m2 | 6 (1.1) |
| Normal: 18.5 to <25 kg/m2 | 132 (24.4) |
| Overweight: 25 to <30 kg/m2 | 160 (29.6) |
| Obese: ≥30 kg/m2 | 242 (44.8) |
| BMI 30–34.9 kg/m2 | 126 (52.1) |
| BMI ≥35 kg/m2 | 116 (47.9) |
| Menopausal status | |
| Premenopausal | 21 (3.9) |
| Postmenopausal | 519 (96.1) |
| Study arm | |
| Entinostat | 270 (50.0) |
| Placebo | 270 (50.0) |
| Visceral disease | |
| No | 215 (39.8) |
| Yes | 325 (60.2) |
| Prior chemotherapy | |
| No | 226 (41.9) |
| Yes | 314 (58.1) |
| Prior chemotherapy setting | |
| Adjuvant | 173 (54.9) |
| Metastatic | 94 (29.8) |
| Both adjuvant/metastatic | 48 (15.2) |
| Muscle mass | |
| N | 540 |
| Mean skeletal muscle index [SD] | 43.6 [7.6] |
| LMM | 212 (39.3) |
| Muscle attenuation | |
| N | 539 |
| Mean HU [SD] | 32.5 [9.74] |
| LMA | 301 (55.8) |
Abbreviations: BMI, body mass index; HU, Hounsfield unit; LMA, low muscle attenuation; LMM, low muscle mass.
Includes Asian, American Indian, Alaskan Native, Native Hawaiian, and Pacific Islander.
Participants with LMA were more likely to have obesity (53.8%), whereas those with LMM were not (24.5%). Those with LMA were also more likely to have a worse PS compared with those with normal muscle attenuation (ECOG PS 1 in 49.2% with LMA vs 32.4% without), whereas there was no difference in PS based on muscle mass. Participants with LMA and those with LMM had similar populations by race (Table 2).
Table 2.
Associations of LMA and LMM With BMI, Performance Status, and Race
| LMA |
LMM |
|||||
|---|---|---|---|---|---|---|
| Non-LMA n (%) | LMA n (%) | Total n (%) | Non-LMM n (%) | LMM n (%) | Total n (%) | |
| Total, N | 238 | 301 | 539 | 328 | 212 | 540 |
|
| ||||||
| BMI | ||||||
|
| ||||||
| <30 kg/m2 | 158 (66.4) | 139 (46.2) | 297 (55.1) | 138 (42.1) | 160 (75.5) | 298 (55.2) |
|
| ||||||
| ≥30 kg/m2 | 80 (33.6) | 162 (53.8) | 242 (44.9) | 190 (57.9) | 52 (24.5) | 242 (44.8) |
|
| ||||||
| ECOG performance status | ||||||
|
| ||||||
| 0 | 161 (67.6) | 153 (50.8) | 314 (58.3) | 191 (58.2) | 124 (58.5) | 315 (58.3) |
|
| ||||||
| 1 | 77 (32.4) | 148 (49.2) | 225 (41.7) | 137 (41.8) | 88 (41.5) | 225 (41.7) |
|
| ||||||
| Race | ||||||
|
| ||||||
| White | 183 (76.9) | 250 (83.1) | 433 (80.3) | 256 (78.0) | 178 (84.0) | 434 (80.4) |
|
| ||||||
| Black | 41 (17.2) | 41 (13.6) | 82 (15.2) | 57 (17.4) | 25 (11.8) | 82 (15.2) |
|
| ||||||
| Other | 14 (5.9) | 10 (3.3) | 24 (4.5) | 15 (4.6) | 9 (4.2) | 24 (4.4) |
Abbreviations: BMI, body mass index; LMA, low muscle attenuation; LMM, low muscle mass.
Association of Muscle Mass and Attenuation With Survival Outcomes
As of May 5, 2020, there were 368 OS events and 507 PFS events. Median OS was 22.9 months (95% CI, 19.9–25.5 months) for LMA versus 25.5 months (95% CI, 21.2–28.0 months) for non-LMA. Median OS was 22.9 months (95% CI, 20.0–25.7 months) for LMM versus 23.8 months (95% CI, 21.9–27.5 months) for non-LMM participants. There was no significant difference in OS by LMA or LMM category. Similarly, PFS for LMA versus non-LMA was 3.7 months (95% CI, 3.5–3.8 months) and 3.6 months (95% CI, 3.5–3.7 months), respectively. Participants with LMM versus non-LMM had a median PFS time of 3.7 months (95% CI, 3.5–3.9 months) and 3.6 months (95% CI, 3.5–3.7 months), respectively. There was no significant difference in PFS for LMA or LMM.
Univariate and multivariate cox regression analyses are shown in Table 3. In univariate cox regression models, neither muscle mass nor muscle attenuation as continuous variables or as dichotomous variables were associated with PFS or OS. Multivariate models for LMA and LMM were adjusted for age, race, prior chemotherapy, ECOG PS, and dichotomized BMI. When adjusting for these confounders, neither LMA nor LMM was associated with PFS or OS. In the PFS multivariate models, older age and worse PS were associated with increased risk of PFS events. In the OS models, race and PS were significant. Importantly, Black race was associated with a 43% higher risk of death compared with white race when adjusting for all other confounders. LMA, LMM, and obesity by BMI were not prognostic of PFS or OS, as shown in the Kaplan-Meier curves in Figure 1.
Table 3.
Cox Regression Models for Muscle Measures and Covariates on Survival Outcomes
| Univariate |
Multivariate With LMA |
Multivariate With LMM |
||||
|---|---|---|---|---|---|---|
| Hazard Ratio | P Value | Hazard Ratio | P Value | Hazard Ratio | P Value | |
| Progression-free survival | ||||||
|
| ||||||
| Muscle density, HU (per 1 SD) | 1.03 | .4967 | ||||
|
| ||||||
| Skeletal muscle index (per 1 SD) | 0.99 | .7482 | ||||
|
| ||||||
| Age, y (per 10 y) | 0.86 | .0003 | 0.87 | .0021 | 0.86 | .0007 |
|
| ||||||
| Race | ||||||
|
| ||||||
| White | Ref | Ref | Ref | |||
|
| ||||||
| Black | 1.32 | .0228 | 1.20 | .1477 | 1.21 | .1282 |
|
| ||||||
| Other | 0.81 | .3274 | 0.80 | .3077 | 0.80 | .2927 |
|
| ||||||
| Prior chemotherapy | ||||||
|
| ||||||
| No | Ref | Ref | Ref | |||
|
| ||||||
| Yes | 1.30 | .0041 | 1.26 | .0113 | 1.28 | .0081 |
|
| ||||||
| ECOG performance status | ||||||
|
| ||||||
| 0 | Ref | Ref | Ref | |||
|
| ||||||
| 1 | 1.08 | .3753 | 1.11 | .2529 | 1.10 | .2775 |
|
| ||||||
| BMI, dichotomized | ||||||
|
| ||||||
| <30 kg/m2 | Ref | Ref | Ref | |||
|
| ||||||
| ≥30 kg/m2 | 0.99 | .8814 | 0.93 | .4522 | 0.97 | .7722 |
|
| ||||||
| LMA | ||||||
|
| ||||||
| No | Ref | Ref | ||||
|
| ||||||
| Yes | 0.92 | .3417 | 1.01 | .9295 | ||
|
| ||||||
| LMM | ||||||
|
| ||||||
| No | Ref | Ref | ||||
|
| ||||||
| Yes | 1.02 | .8510 | 1.13 | .2327 | ||
|
| ||||||
| Overall survival | ||||||
|
| ||||||
| Muscle density, HU (per 1 SD) | 1.00 | .9379 | ||||
|
| ||||||
| Skeletal muscle index (per 1 SD) | 0.99 | .9176 | ||||
|
| ||||||
| Age, y (per 10 y) | 0.94 | .2040 | 0.95 | .3377 | 0.95 | .2923 |
|
| ||||||
| Race | ||||||
|
| ||||||
| White | Ref | Ref | Ref | |||
|
| ||||||
| Black | 1.48 | .0038 | 1.43 | .0101 | 1.43 | .0101 |
|
| ||||||
| Other | 1.04 | .8944 | 1.02 | .9378 | 1.02 | .9413 |
|
| ||||||
| Prior chemotherapy | ||||||
|
| ||||||
| No | Ref | Ref | Ref | |||
|
| ||||||
| Yes | 1.11 | .3093 | 1.08 | .4876 | 1.09 | .4420 |
|
| ||||||
| ECOG performance status | ||||||
|
| ||||||
| 0 | Ref | Ref | Ref | |||
|
| ||||||
| 1 | 1.33 | .0066 | 1.35 | .0052 | 1.35 | .0053 |
|
| ||||||
| BMI, dichotomized | ||||||
|
| ||||||
| <30 kg/m2 | Ref | Ref | Ref | |||
|
| ||||||
| ≥30 kg/m2 | 0.88 | .2185 | 0.84 | .1040 | 0.85 | .1310 |
|
| ||||||
| LMA | ||||||
|
| ||||||
| No | Ref | Ref | ||||
|
| ||||||
| Yes | 0.96 | .6979 | 1.00 | .9889 | ||
|
| ||||||
| LMM | ||||||
|
| ||||||
| No | Ref | Ref | ||||
|
| ||||||
| Yes | 1.05 | .6520 | 1.05 | .6796 | ||
Abbreviations: BMI, body mass index; HU, Hounsfield unit; LMA, low muscle attenuation; LMM, low muscle mass.
Figure 1.
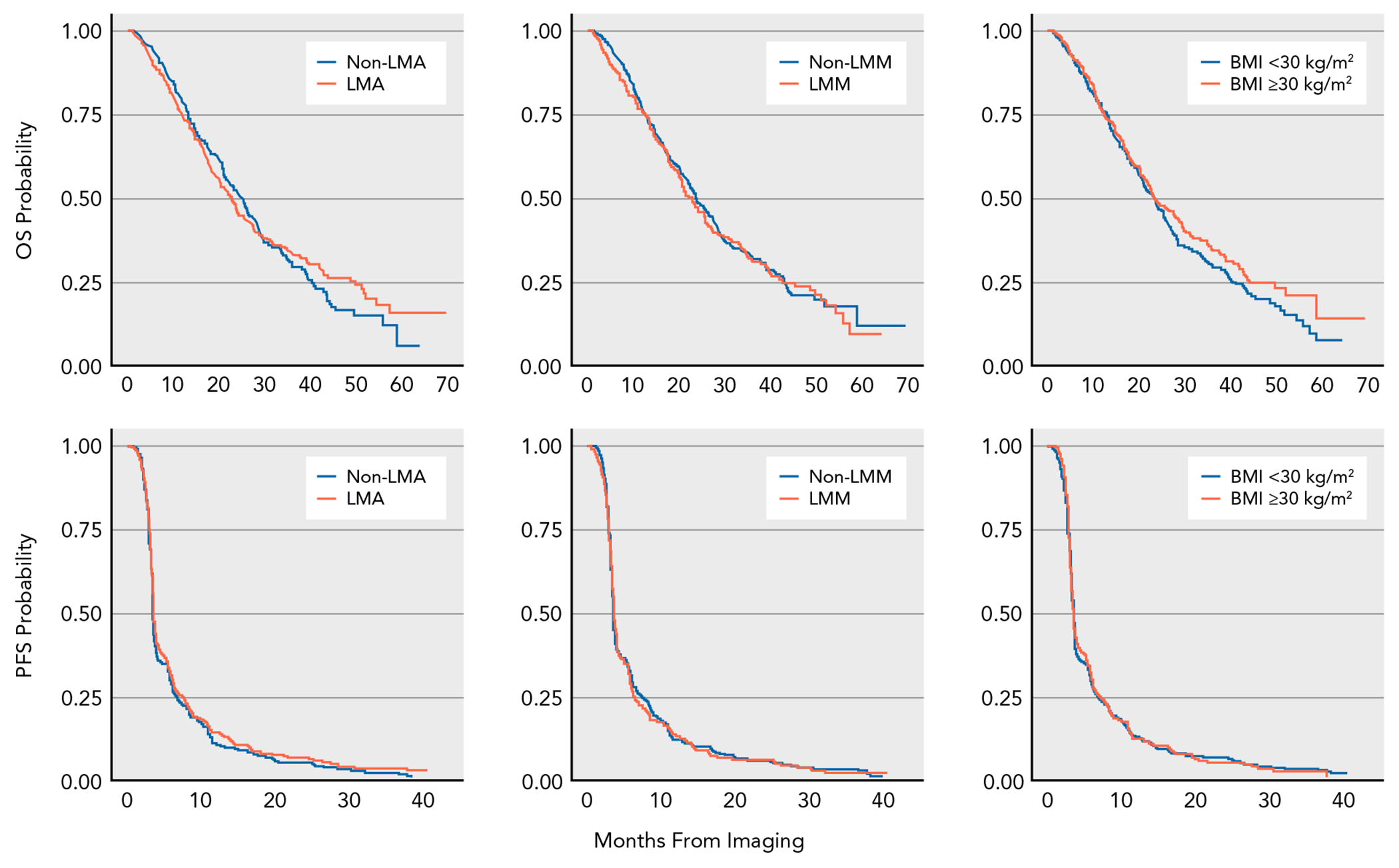
Kaplan-Meier curves for PFS and OS by muscle attenuation, muscle mass, and BMI.
Abbreviations: BMI, body mass index; LMA, low muscle attenuation; LMM, low muscle mass; OS, overall survival; PFS, progression-free survival.
Exploratory analysis to find an optimal cut point that is prognostic in this specific patient population found that a lower cut point for skeletal muscle (SMI, 36 vs 41 cm2/m2 used in the primary analysis) was prognostic of worse PFS and OS (HR: 1.33 [95% CI, 1.04–1.70]; P=.02, and 1.37 [95% CI, 1.03–1.82]; P=.03, respectively). This degree of LMM was seen in only 14.6% of the population (n=79). No alternative cut points were discovered to be prognostic of survival outcomes for muscle attenuation.
Association of Muscle Mass and Attenuation With Patient-Reported Outcomes
The association of LMM and LMA with patient-reported muscle aches or joint pain, health-related quality of life, and fatigue is shown in Table 4. Questionnaires were available only from a subset of participants (n=379 for PRO-CTCAE; n=363 for FACT-G; and n=373 for PROMIS-Fatigue). LMM had no association with patient-reported muscle aches or joint aches. Unlike muscle mass, LMA was significantly associated with increased muscle ache frequency, as well as severity and interference with daily activities. LMA had no association with joint pain frequency but did have a mild association with joint pain severity. Neither LMM nor LMA was significantly associated with quality of life or fatigue.
Table 4.
Association of Muscle Attenuation and Muscle Mass With Patient-Reported Outcomes
| LMA |
LMM |
|||||
|---|---|---|---|---|---|---|
| Non-LMA | LMA | Difference (95% CI) P Valuea | Non-LMM | LMM | Difference (95% CI) P Valuea | |
| PRO-CTCAE | ||||||
|
| ||||||
| Muscle ache | ||||||
|
| ||||||
| Frequency | ||||||
|
| ||||||
| N | 167 | 212 | −0.30 (−0.54 to −0.06) .0143 | 237 | 142 | 0.22 (−0.02 to 0.47) .0773 |
|
|
|
|||||
| Mean [SD] | 1.32 [1.15] | 1.62 [1.20] | 1.57 [1.15] | 1.35 [1.23] | ||
|
| ||||||
| Interference | ||||||
|
| ||||||
| N | 161 | 199 | −0.25 (−0.48 to −0.03) .0289 | 228 | 132 | 0.22 (−0.01 to 0.46) .0578 |
|
|
|
|||||
| Mean [SD] | 0.84 [1.02] | 1.10 [1.13] | 1.07 [1.10] | 0.84 [1.05] | ||
|
| ||||||
| Severity | ||||||
|
| ||||||
| N | 162 | 205 | −0.24 (−0.45 to −0.04) .0212 | 232 | 135 | 0.16 (−0.05 to 0.38) .1405 |
|
|
|
|||||
| Mean [SD] | 1.14 [0.96] | 1.38 [1.04] | 1.33 [1.00] | 1.17 [1.03] | ||
|
| ||||||
| Joint ache | ||||||
|
| ||||||
| Frequency | ||||||
|
| ||||||
| N | 168 | 211 | −0.21 (−0.47 to 0.05) .1177 | 237 | 142 | 0.16 (−0.11 to 0.43) .2391 |
|
|
|
|||||
| Mean [SD] | 1.74 [1.28] | 1.95 [1.31] | 1.92 [1.29] | 1.75 [1.31] | ||
|
| ||||||
| Interference | ||||||
|
| ||||||
| N | 164 | 205 | −0.19 (−0.42 to 0.04) .0973 | 232 | 137 | 0.17 (−0.06 to 0.40) .1492 |
|
|
|
|||||
| Mean [SD] | 1.07 [1.06] | 1.26 [1.13] | 1.24 [1.12] | 1.07 [1.07] | ||
|
| ||||||
| Severity | ||||||
|
| ||||||
| N | 165 | 204 | −0.22 (−0.44 to −0.01) .0388 | 232 | 137 | 0.09 (−0.13 to 0.31) .4107 |
|
|
|
|||||
| Mean [SD] | 1.39 [1.00] | 1.62 [1.06] | 1.55 [1.02] | 1.46 [1.06] | ||
|
| ||||||
| Health-Related Quality of Life (FACT-G TOI) | ||||||
|
| ||||||
| N | 161 | 202 | 0.46 (−1.42 to 2.34) .6325 | 225 | 138 | −0.86 (−2.78 to 1.06) .3801 |
|
|
|
|||||
| Mean [SD] | 31.57 [9.41] | 31.11 [8.74] | 30.99 [9.09] | 31.84 [8.96] | ||
|
| ||||||
| PROMIS-Fatigue T Score | ||||||
|
| ||||||
| N | 167 | 206 | 0.04 (−1.68 to 1.76) .9652 | 232 | 141 | 0.26 (−1.50 to 2.02) .7691 |
|
|
|
|||||
| Mean [SD] | 52.45 [8.48] | 52.41 [8.32] | 52.53 [8.16] | 52.26 [8.76] | ||
Abbreviations: FACT-G TOI, Functional Assessment of Cancer Therapy—General Trial Outcome Index; PRO-CTCAE, Patient Reported Outcomes–CTCAE; LMA, low muscle attenuation; LMM, low muscle mass; PROMIS, Patient-Reported Outcomes Measurement Information System.
Comparison of means.
Discussion
This analysis of 540 patients with hormone receptor–positive MBC from ECOG-ACRIN E2112 demonstrated no association between muscle measures (LMM or LMA) as determined by CT and survival outcomes using established prognostic cutoffs for muscle mass and muscle attenuation. Both LMM and, particularly, LMA, defined by cut points from prior literature in advanced cancers predicting worse survival outcomes,1 were highly prevalent in this patient population with metastatic hormone receptor–positive breast cancer. On exploratory analysis, we did find that the 15% of patients with the lowest muscle mass (SMI<36 cm2/m2) had worse OS and PFS. LMA was significantly associated with worse PS, whereas LMM had no association with PS, consistent with geriatric literature indicating that muscle attenuation correlates with function, whereas mass does not.5 Further supporting this relationship, patient-reported muscle aches were significantly higher in frequency and severity in patients with LMA, whereas LMM had no association with pain. Muscle aches are an underrecognized toxicity secondary to endocrine therapy in MBC. Recognizing LMA on routinely obtained CT scans in patients with MBC may identify those with worse PS and increased muscle aches who may benefit from additional supportive care, including physical therapy, acupuncture, or massage therapy, among others.13,14
The lack of association of LMM and LMA with survival outcomes is contrary to our hypothesis. Although these measures are associated with survival in early-stage breast cancer,6 it is possible that once diagnosed with MBC, there is no correlation given shorter OS times. Prior studies of muscle mass or attenuation with survival and toxicity outcomes in MBC have shown lower muscle mass and/or attenuation to be associated with increased toxicity and shorter time to progression.7–9 However, these studies have been in smaller sample sizes and in patients receiving chemotherapy. Three small studies in patients receiving chemotherapy for MBC found sarcopenia (defined as LMM) was associated with increased therapy-related toxicity, but had an inconsistent impact on progression and survival outcomes (Lee et al,15 N=53; Shachar et al,8 N=40; and Prado et al,7 N=55). In an analysis by Rier et al9 of 166 patients with MBC receiving frontline taxane chemotherapy, baseline muscle mass had no association with survival, whereas LMA was associated with worse survival only as a categorical, and not a continuous, variable. Similarly, an analysis by Sheean et al4 of 152 patients with hormone receptor–negative MBC found no association between muscle mass and survival but a significant relationship between LMA and worse 2-year survival. It is likely that all of these prior analyses represented patient populations with more biologically aggressive disease, given that they were being treated with chemotherapy and had a median survival <24 months across frontline studies. In our analysis, only one-fourth had required cytotoxic chemotherapy in the metastatic setting, and the population had a median OS of 23.5 months from randomization, despite most being pretreated for MBC.
Our study specifically analyzed body composition and outcomes in patients receiving endocrine-based therapy for MBC. However, the ECOG-ACRIN E2112 trial was completed several years ago, with only one-third of patients receiving cyclin-dependent kinase (CDK4/6) inhibitor therapy, compared with nearly all patients in the current treatment paradigm. Two small, single-institution studies retrospectively analyzing body composition and outcomes in patients receiving CDK4/6 inhibitor therapy have found an association between LMM and worse survival outcomes.16,17 CDKs play essential roles in the regulation of muscle progenitor cells during muscle regeneration, aging, and response to exercise; thus, it is possible that CDK4/6 inhibitor therapy, particularly over long periods of time, may have an impact on muscle measures and function. Future work should analyze body composition within larger CDK4/6 inhibitor trials; the use of centrally collected CT scans as part of multicenter cooperative group trials, as done here, can be leveraged to investigate this question.
A major reason for inconsistencies regarding the role of obesity or muscle measures in breast cancer outcomes may be the lack of consensus on how to define muscle mass and density cutoffs and how to measure them. Many investigations use the term “sarcopenia” to describe LMM, although many societies define sarcopenia as the combination of LMM along with an objective measure of muscle frailty indicating functional deficits.5 The cut points for defining “low” muscle mass or attenuation has been defined differently across populations, and there is no consensus.18 In our analysis of patients receiving endocrine therapy for MBC, cutoffs used in prior literature (41 or 38.5 cm2/m2 for SMI) were not prognostic of survival. However, we did perform an exploratory analysis using optimal stratification and found that skeletal muscle relative to height (SMI) <36 cm2/m2 was associated with worse OS and PFS. It may be that in this population of patients with a high incidence of obesity and severe obesity, who are not receiving chemotherapy, survival is impacted only at the extreme of low skeletal muscle mass. This degree of loss of muscle can be noted clearly on routine CT scans and may be important to clinically recognize in order to offer supportive care interventions that could impact survival.
Beyond definitions and cutoff variability, methodologic issues exist. Muscle is not completely independent of body weight or body adiposity, and the way to best account for these variables is not consistent or well understood. The original work relating a CT slice of the L3 level to total body muscle mass was published in 2008 and found muscle area to scale to height by a power of 2.11 This is an important principle of body composition work to establish the independence from height; however, more recent work suggests that it is possible that scaling to height by a power of 2, particularly in female patients with cancer, may not actually achieve statistical independence from height.19 This would have significant consequences on the conclusions in this analysis and others. Beyond this, it is recognized that nearly all analyses of muscle mass and attenuation in patients with cancer have been performed in a predominately white, non-Hispanic population, and racial and ethnic differences in body composition in this setting are likely to exist, but the impact of these differences on outcomes is unknown. Notably, although not the purpose of this analysis, Black patients in this study had significantly worse survival outcomes compared with white patients. Although racial disparities are well described in early-stage breast cancer, additional work is needed to investigate etiologies of disparate outcomes in the metastatic setting.
Our study is the largest analysis of muscle measures in the most common subtype of MBC and has strengths in the prospectively followed, largely homogeneous population participating in a cooperative group clinical trial. Although this analysis was predefined and based on existing literature available in this space, the exploratory post hoc nature of the analysis is a limitation. As noted earlier, the cut point used in our analysis is based on metastatic populations without breast cancer. However, it is not expected that an alternate cut point would matter given that we saw no association with muscle mass or attenuation as a continuous variable and survival outcomes, and the P values were approaching 1. Additionally, in this population, participants with obesity had lower muscle attenuation but higher muscle mass. We were unable to reliably analyze total adipose tissue as a possible contributor or covariate given that many of the participants were obese and a significant portion of adipose tissue was outside the view of the CT scan image.
Conclusions
In this cohort of patients with hormone receptor–positive MBC, muscle measures correlated with PS and subjective muscle ache but were not prognostic of survival outcomes using established cutoffs. On exploratory analysis, we did find that very low muscle mass in approximately 15% of patients predicted worse survival outcomes; this population could be identified and provided early supportive care interventions that may improve outcomes. Further work is needed to refine body composition measures, including optimal cutoffs for specific populations and investigating trends in muscle and adipose tissue over time. In addition, future work will analyze the impact of specific compartments, including intramuscular adipose tissue, visceral adipose tissue, and adipose tissue density, on outcomes. Lower adipose tissue density is associated with larger adipocytes and worse metabolic profile, whereas higher adipose density is associated with inflammation and worse prognosis in several cancer populations, including those with early-stage breast cancer, and thus may be an impactful variable.20 This type of detailed body composition analysis may be particularly important in MBC, because many of these patients are obese and muscle wasting may go unrecognized at the bedside. Muscle mass and adipose infiltration are modifiable, and thus, further investigation of endpoints other than survival, such as physical function and toxicity, may identify populations in need of supportive care interventions.
Supplementary Material
Funding:
This study was coordinated by the ECOG-ACRIN Cancer Research Group (P.J. O’Dwyer, and M.D. Schnall, Group Co-Chairs). Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health under award numbers U10CA180820 and U10CA180794, as well as 100 Voices of Hope (T. Ballinger).
Footnotes
Disclosures: Dr. Ballinger has disclosed serving as a consultant for Medscape and MedEdge. The remaining authors have disclosed that they have not received any financial consideration from any person or organization to support the preparation, analysis, results, or discussion of this article.
Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1.Martin L, Birdsell L, Macdonald N, et al. Cancer cachexia in the age of obesity: skeletal muscle depletion is a powerful prognostic factor, independent of body mass index. J Clin Oncol 2013;31:1539–1547. [DOI] [PubMed] [Google Scholar]
- 2.Shachar SS, Williams GR, Muss HB, et al. Prognostic value of sarcopenia in adults with solid tumours: a meta-analysis and systematic review. Eur J Cancer 2016;57:58–67. [DOI] [PubMed] [Google Scholar]
- 3.Kroenke CH, Prado CM, Meyerhardt JA, et al. Muscle radiodensity and mortality in patients with colorectal cancer. Cancer 2018;124:3008–3015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sheean P, Gomez-Perez S, Joyce C, et al. Myosteatosis at diagnosis is adversely associated with 2-year survival in women with estrogen receptor-negative metastatic breast cancer. Breast Cancer Res Treat 2021;190:121–132. [DOI] [PubMed] [Google Scholar]
- 5.Williams GR, Deal AM, Muss HB, et al. Skeletal muscle measures and physical function in older adults with cancer: sarcopenia or myopenia? Oncotarget 2017;8:33658–33665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Caan BJ, Cespedes Feliciano EM, Prado CM, et al. Association of muscle and adiposity measured by computed tomography with survival in patients with nonmetastatic breast cancer. JAMA Oncol 2018;4:798–804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Prado CM, Baracos VE, McCargar LJ, et al. Sarcopenia as a determinant of chemotherapy toxicity and time to tumor progression in metastatic breast cancer patients receiving capecitabine treatment. Clin Cancer Res 2009;15:2920–2926. [DOI] [PubMed] [Google Scholar]
- 8.Shachar SS, Deal AM, Weinberg M, et al. Skeletal muscle measures as predictors of toxicity, hospitalization, and survival in patients with metastatic breast cancer receiving taxane-based chemotherapy. Clin Cancer Res 2017;23:658–665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rier HN, Jager A, Sleijfer S, et al. Low muscle attenuation is a prognostic factor for survival in metastatic breast cancer patients treated with first line palliative chemotherapy. Breast 2017;31:9–15. [DOI] [PubMed] [Google Scholar]
- 10.Connolly RM, Zhao F, Miller KD, et al. E2112: randomized phase III trial of endocrine therapy plus entinostat or placebo in hormone receptor-positive advanced breast cancer. A trial of the ECOG-ACRIN Cancer Research Group. J Clin Oncol 2021;39:3171–3181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mourtzakis M, Prado CM, Lieffers JR, et al. A practical and precise approach to quantification of body composition in cancer patients using computed tomography images acquired during routine care. Appl Physiol Nutr Metab 2008;33:997–1006. [DOI] [PubMed] [Google Scholar]
- 12.van Vugt JL, Levolger S, Gharbharan A, et al. A comparative study of software programmes for cross-sectional skeletal muscle and adipose tissue measurements on abdominal computed tomography scans of rectal cancer patients. J Cachexia Sarcopenia Muscle 2017;8:285–297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dieli-Conwright CM, Courneya KS, Demark-Wahnefried W, et al. Effects of aerobic and resistance exercise on metabolic syndrome, sarcopenic obesity, and circulating biomarkers in overweight or obese survivors of breast cancer: a randomized controlled trial. J Clin Oncol 2018;36:875–883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hershman DL, Unger JM, Greenlee H, et al. Comparison of acupuncture vs sham acupuncture or waiting list control in the treatment of aromatase inhibitor-related joint pain: a randomized clinical trial. JAMA Netw Open 2022;5:e2241720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee HJ, Kim HS, Kim WY, et al. Sarcopenia as a predicting factor for chemotherapy in advanced breast cancer patients. Eur J Surg Oncol 2019;45:e31. [Google Scholar]
- 16.Franzoi MA, Vandeputte C, Eiger D, et al. Computed tomography-based analyses of baseline body composition parameters and changes in breast cancer patients under treatment with CDK 4/6 inhibitors. Breast Cancer Res Treat 2020;181:199–209. [DOI] [PubMed] [Google Scholar]
- 17.Kripa E, Rizzo V, Galati F, et al. Do body composition parameters correlate with response to targeted therapy in ER+/HER2- metastatic breast cancer patients? Role of sarcopenia and obesity. Front Oncol 2022;12:987012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rier HN, Jager A, Sleijfer S, et al. The prevalence and prognostic value of low muscle mass in cancer patients: a review of the literature. Oncologist 2016;21:1396–1409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brown JC, Heymsfield SB, Caan BJ. Scaling of computed tomography body composition to height: relevance of height-normalized indices in patients with colorectal cancer. J Cachexia Sarcopenia Muscle 2022;13:203–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cheng E, Caan BJ, Chen WY, et al. Adipose tissue radiodensity and mortality among patients with nonmetastatic breast cancer. Clin Nutr 2022;41:2607–2613. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


