Abstract
Introduction
: Ovotestis is a rare cause of sexual ambiguity characterized by the presence in a patient of both testicular and ovarian tissue, leading to the development of both male and female structures. We report a case of ovotestis diagnosed in an adolescent, with a review of the literature.
Case Report
A 15-year-old patient presented with a right scrotal swelling associated with gynecomastia. Histology showed a juxtaposition of ovarian stroma with ovarian follicle and seminiferous tubules. Karyotype revealed a male subject (XY). We have therefore retained the diagnosis of ovotesticular disorders of sex development.
Conclusion
Ovotestis is a rare finding, heterogeneous in its genetic etiology and clinical presentation. While many patients are diagnosed during infancy or childhood, we presented a case diagnosed in a 15-year-old adolescent.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12905-023-02698-1.
Keywords: Ovotestis, Adolescent, Histology, Karyotype, Disorders of Sex Development (DSD)
Introduction
The term ‘Disorders Of Sex Development’ (DSD) is now proposed to define congenital conditions in which a dysharmony between chromosomal, gonadal and anatomical sex exists [1]. Ovotestis is a rare cause of sexual ambiguity characterized by the presence in a patient of both testicular and ovarian tissue, leading to the development of male and female structures [1–3]. The incidence and constitutive karyotype of patients with ovotestis are reported to vary geographically [4, 5]. Ovotestis accounts for 3–10% of all sex ambiguities [2]. Its incidence in South Africa is estimated at 4% [6]. The prevalence of ovotestis is estimated to be less than 1:20,000, and approximately 500 individuals have been reported to date [7]. Sex ambiguity is often discovered at birth. Karyotypes vary; 46,XX, 46,XY and several mosaic and aneuploid forms [1].
We report a case of ovotestis diagnosed in a 15-year-old adolescent, describe the clinical presentation and diagnostic features.
Case report
A 15-year-old patient, with no previous pathological history, raised as a boy, consulted the urology department of the University Hospital of Treichville for a right scrotal swelling, evolving for more than 5 years. The patient began full and normal male puberty at the age of 13.
The clinical examination revealed a patient in good general condition, measuring 1.56 m and weighing 47 kg, corresponding to a body mass index of 19.31 kg/m². The patient had Tanner stage 2 pubic hair, with a penis measuring 4 cm at rest, without hypospadias or cryptorchidism.
A painless, mobile and firm right scrotal mass was palpated. The left testicle was present but atrophic. He had a female morphotype, with marked gynecomastia (Fig. 1). The lymph nodes were free.
Fig. 1.

Male subject with bilateral gynecomastia
On pelvic and scrotal ultrasound, a right testicular solid tumor with a long axis of 6 cm was found, with absence of female genitalia. No uterus or adnexa was seen. The contralateral testis was without abnormality.
The biological workup consisted of TESTOSTERONE (0.1 ng/ml), ESTRADIOL (20 ng/ml), ALPHA-FETO-PROTEIN (5 ng/ml) and β HCG (< 01ui /l); all of which came back normal.
A right orchiectomy was performed and the specimen sent to the pathology laboratory.
Macroscopically, it was a lumpy mass. On section, there were several whitish nodules surrounded by a yellowish border (Fig. 2).
Fig. 2.

Whitish multinodular areas and whitish territories surrounded by a yellowish border
The resected specimen was fixed with 10% formaldehyde, followed by conventional dehydration, kerosene embedding, sectioning and hematoxylin and eosin (HE) staining. On histology, there was a juxtaposition of ovarian stroma with ovarian follicle and seminiferous tubules (Figs. 3 and 4, and 5). In view of this aspect we retained the diagnosis of ovotestis. The karyotype was determined to be male (46, XY), confirming the diagnosis of ovotesticular disorders of sex development. An initial interview was held with the parents in the presence of a psychologist to explain their child’s pathology, before the child was informed during a second interview in the presence of the parents and the psychologist.
Fig. 3.
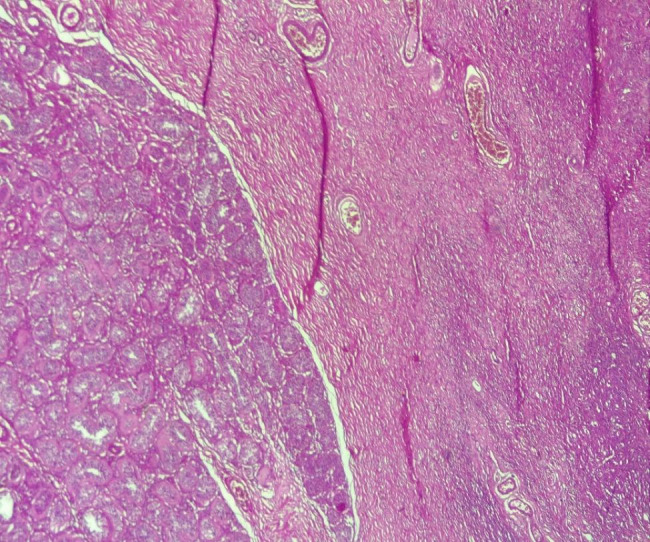
Juxtaposition of ovarian stroma and seminiferous tubules (HESx100)
Fig. 4.
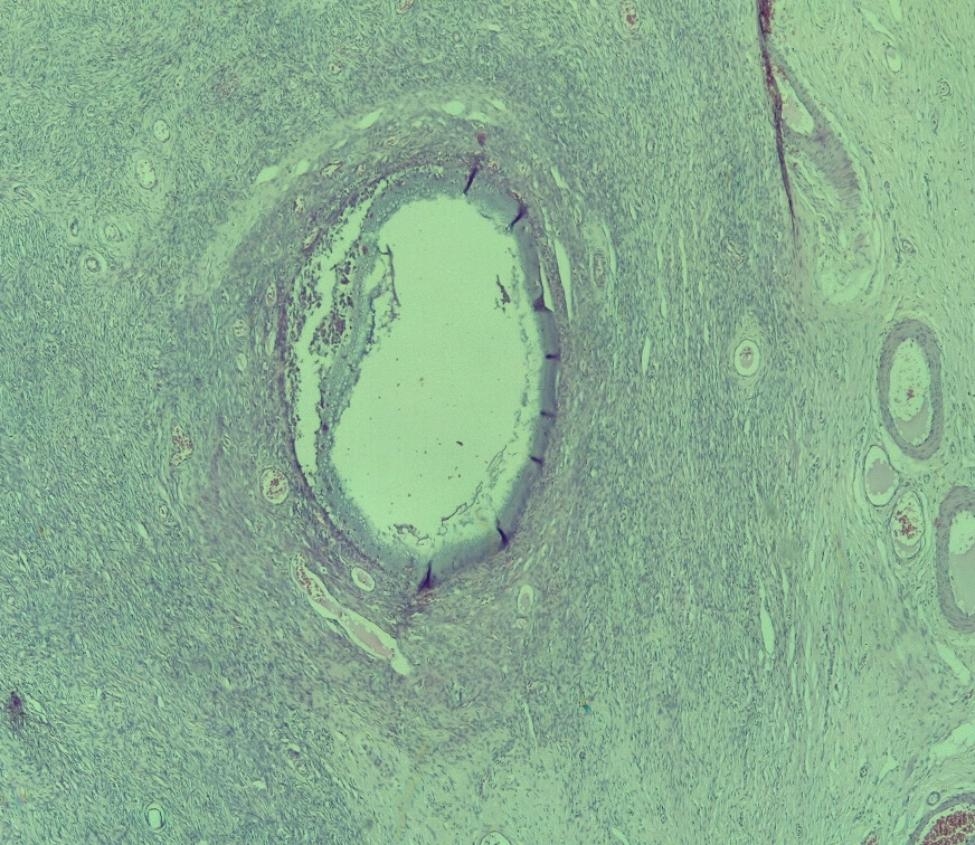
Ovarian tissue with a follicular cyst and an ovarian follicle (HESX100)
Fig. 5.
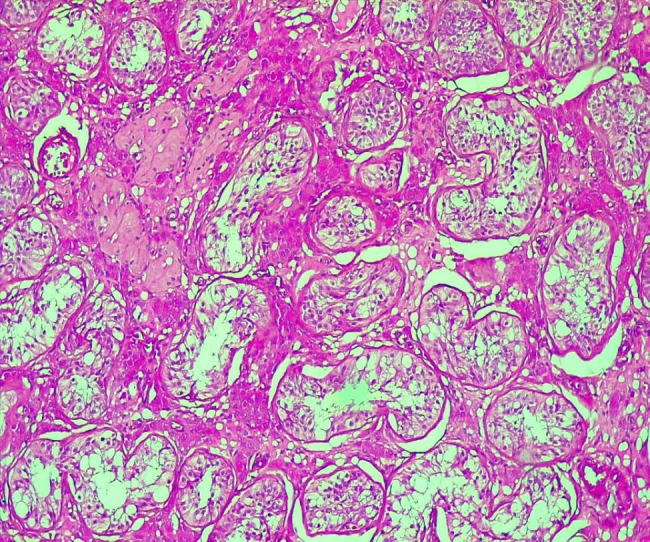
Testicular parenchyma seen at high magnification (HESX100)
Hormonal therapy based on 80 mg testosterone undecanoate capsules at a dose of once a day and mastectomy were proposed, but the patient was lost to follow-up.
Discussion
Sexual ambiguities are congenital conditions with atypical chromosomal, gonadal or anatomical sex development [8]. They occur in one in 4500 births and ovotestis accounts for 3–10% of all sex ambiguities [2]. Defined as congenital conditions in which development of chromosomal, gonadal, or anatomic sex is atypical, differences or disorders of sex development (DSDs) comprise many discrete diagnoses ranging from those associated with few phenotypic differences between affected and unaffected individuals to those where questions arise regarding gender of rearing, gonadal tumor risk, genital surgery, and fertility [9]. Controversies exist in numerous areas including how DSDs are conceptualized, how to refer to the set of conditions and those affected by them, and aspects of clinical management that extend from social media to legislative bodies, courts of law, medicine, clinical practice, and scholarly research in psychology and sociology [9, 10]. In addition to these aspects, this review covers biological and social influences on psychosocial development and adjustment, the psychosocial and psychosexual adaptation of people born with DSDs, and roles for clinical psychologists in the clinical management of DSDs [11].
Approximately 400 cases of ovotestis have been reported to date [8]. Although ovotestis is rare [12–14], it is thought to be more prevalent in black South Africans [8], particularly ovotesticular sex ambiguity 46,XX. Most cases are sporadic with few documented cases of familial recurrence [8]. It is often diagnosed at birth [1]. We report a case of ovotestis, diagnosed in a 15 year old adolescent of female morphotype with bilateral gynecomastia, who consulted for a right scrotal swelling. Clinical and ultrasound examinations revealed a right scrotal mass with an atrophic testicle, and a normal biological work-up. A large series of 20 Brazilian patients with ovotestis was diagnosed at a mean age of 11 years. Clinical features included bilateral gynecomastia and cyclic hematuria [15]. Clinical features often depend on the underlying karyotype. The most common karyotype in ovotestis is 46, XX [4, 15]. Our patient had a 46, XY karyotype. Amolo et al. found a predominance of 46, XY karyotype in 46.2% [8]. In the Indonesian series of Juniarto et al., 63.3% of the patients had 46, XY karyotype [16]. Individuals with 46, XY karyotype have the highest risk of developing a malignant gonadal tumor, due to the presence of a non-functional testicular component in the ovotestis, which requires removal of the non-functional gonads [17–20]. Emphasis is placed on a multidisciplinary approach in order to maximize the potential of these individuals to become normal socially functioning adults [20]. Hormone replacement therapy as well as mastectomy were proposed in our case, but the patient was lost to follow-up.
Conclusion
Ovotestis is a rare finding, heterogeneous in its genetic etiology and clinical presentation, its diagnosis is based on comprehensive clinical information, coupled with pelvic ultrasound and histopathology results, confirmed by karyotype. While many patients are diagnosed in infancy or childhood, we reported a case diagnosed in a 15-year-old adolescent with a 46, XY karyotype. This was diagnosed late due to normal male phenotypic development over time, with the need for long-term follow-up to assess hormonal status and sexual function. Because of the high risk of developing gonadal cancer in these patients, emphasis is placed on long-term multidisciplinary management, including psychologists, endocrinologists, gynaecologists, paediatricians and even plastic surgeons.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
Not applicable.
Abbreviations
- DSD
Disorders/ Differences of Sex Development
Authors’ contributions
KBBS, AAD and DJT performed the laboratory analyses and their interpretation and drafted the manuscript. TB, KM, KKE, and ANA participated in the management of the specimens; reviewed the manuscript. All authors have read and approved the final version of the manuscript to be submitted for publication.
Funding
The authors did not receive funding from any source to conduct this study.
Data availability
All data supporting the conclusions of this article are included in the manuscript.
Declarations
Ethical approval and consent to participate
The study received approval from the head of the laboratory to be conducted. We have obtained written informed consent from patient’s parents. The manuscript was not submitted to more than one journal for simultaneous review and has not been previously published. Single study, not divided into multiple parts and no data were generated.
Consent for publication
The patient’s parents have given written informed consent for the publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Conflict of interest
The authors declare that they have no conflict of interest.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Chouhan JD, Chu DI, Birs A, Pyle LC, Van Batavia JP, Linn RL, et al. Ovotestis in Adolescence: Two Case Reports Urology. 2017;105:171–4. doi: 10.1016/j.urology.2017.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Talreja SM, Banerjee I, Yadav SS, Tomar V. A rare case of lateral ovotesticular disorder with Klinefelter syndrome mosaicism 46, XX/47, XXY: an unusual presentation. Urol Ann. 2015;7:520–3. doi: 10.4103/0974-7796.164855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ozsu E, Mutlu GY, Cizmecioglu FM, Ekingen G, Muezzinoglu B, Hatun S. Ovotesticular disorder of sexual development and a rare 46,XX/47,XXY karyotype. J Pediatr Endocrinol Metab JPEM. 2013;26:789–91. doi: 10.1515/jpem-2012-0386. [DOI] [PubMed] [Google Scholar]
- 4.Matsui F, Shimada K, Matsumoto F, Itesako T, Nara K, Ida S, et al. Long-term outcome of ovotesticular disorder of sex development: a single center experience. Int J Urol off J Jpn Urol Assoc. 2011;18:231–6. doi: 10.1111/j.1442-2042.2010.02700.x. [DOI] [PubMed] [Google Scholar]
- 5.Meftah A, Moumen A, Eljadi H, Gaouzi A. Ovotestis 46 xy: a propos d’un cas. Ann Endocrinol. 2016;77(4):481. doi: 10.1016/j.ando.2016.07.688. [DOI] [Google Scholar]
- 6.Wiersma R, Ramdial PK. The gonads of 111 South African patients with ovotesticular disorder of sex differentiation. J Pediatr Surg. 2009;44:556–60. doi: 10.1016/j.jpedsurg.2008.08.013. [DOI] [PubMed] [Google Scholar]
- 7.Özdemir M, Kavak RP, Yalcinkaya I, Guresci K. Ovotesticular disorder of Sex Development: an unusual presentation. J Clin Imaging Sci. 2019;9:34. doi: 10.25259/JCIS_45_2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Amolo P, Laigong P, Omar A, Drop S. Etiology and clinical presentation of disorders of Sex Development in Kenyan children and adolescents. Int J Endocrinol. 2019;2019:2985347. doi: 10.1155/2019/2985347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sandberg DE, Gardner M. Differences/Disorders of Sex Development: medical conditions at the intersection of sex and gender. Annu Rev Clin Psychol. 2022;18:201–31. doi: 10.1146/annurev-clinpsy-081219-101412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Diaz A, Lipman Diaz EG. Disorders of Sex Development. Pediatr Rev. 2021;42(8):414–26. doi: 10.1542/pir.2018-0183. [DOI] [PubMed] [Google Scholar]
- 11.Subspecialty Group of Endocrinologic, Hereditary and Metabolic Diseases, the Society of Pediatrics, Chinese Medical Association [Consensus statement on the diagnosis and endocrine treatment of children with disorder of sex development] Zhonghua Er Ke Za Zhi Chin J Pediatr. 2019;57(6):410–8. doi: 10.3760/cma.j.issn.0578-1310.2019.06.003. [DOI] [PubMed] [Google Scholar]
- 12.Khadilkar KS, Budyal SR, Kasaliwal R, Sathe PA, Kandalkar B, Sanghvi BV, et al. Ovotesticular disorder of sex development: a single-center experience. Endocr Pract off J Am Coll Endocrinol Am Assoc Clin Endocrinol. 2015;21:770–6. doi: 10.4158/EP15606.OR. [DOI] [PubMed] [Google Scholar]
- 13.Jaruratanasirikul S, Engchaun V. Management of children with disorders of sex development: 20-year experience in southern Thailand. World J Pediatr WJP. 2014;10:168–74. doi: 10.1007/s12519-013-0418-0. [DOI] [PubMed] [Google Scholar]
- 14.Heeley JM, Hollander AS, Austin PF, Merritt DF, Wesevich VG et al. Washington University School of Medicine in St Louis DSD Team,. Risk association of congenital anomalies in patients with ambiguous genitalia: A 22-year single-center experience. J. Pediatr. Urol. 2018;14:153.e1-153.e7. [DOI] [PubMed]
- 15.Sircili MHP, Denes FT, Costa EMF, Machado MG, Inacio M, Silva RB, et al. Long-term followup of a large cohort of patients with ovotesticular disorder of sex development. J Urol. 2014;191:1532–6. doi: 10.1016/j.juro.2013.10.037. [DOI] [PubMed] [Google Scholar]
- 16.Juniarto AZ, van der Zwan YG, Santosa A, Ariani MD, Eggers S, Hersmus R, et al. Hormonal evaluation in relation to phenotype and genotype in 286 patients with a disorder of sex development from Indonesia. Clin Endocrinol (Oxf) 2016;85:247–57. doi: 10.1111/cen.13051. [DOI] [PubMed] [Google Scholar]
- 17.Kim HI, Lee I, Kim SH, Lee YS, Han SW, Yun BH. Ovotesticular disorder of Sex Development in Korean Children: a single-center analysis over a 30-Year period. J Pediatr Adolesc Gynecol. 2021;34:626–30. doi: 10.1016/j.jpag.2021.02.105. [DOI] [PubMed] [Google Scholar]
- 18.Kojima Y, Mizuno K, Nakane A, Kato T, Kohri K, Hayashi Y. Long-term physical, hormonal, and sexual outcome of males with disorders of sex development. J Pediatr Surg. 2009;44:1491–6. doi: 10.1016/j.jpedsurg.2008.10.111. [DOI] [PubMed] [Google Scholar]
- 19.Man E, Mushtaq I, Barnicoat A, Carmichael P, Hughes CR, Davies K, et al. A Single-Center, Observational Study of 607 children and Young people presenting with differences of Sex Development (DSD) J Endocr Soc. 2022;7:bvac165. doi: 10.1210/jendso/bvac165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Meenal B, Meenakshi G, Pratibha S, Garima Y, Priyanka K, Poonam E. 46 XY ovotesticular disorder: a rare case report with review of literature. Gynecol Minim Invasive Ther. 2021;10:171–3. doi: 10.4103/GMIT.GMIT_107_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data supporting the conclusions of this article are included in the manuscript.


