Abstract
Background
Toxocariasis has been listed among the most neglected parasitic diseases worldwide, with approximately one fifth of the global population exposed, particularly those living under poverty. In Brazil, communities of descendants of enslaved blacks (quilombola) have historically had some of the highest rates of vulnerability and poverty, characterized by lack of health assistance, poor quality of life, and nutritional insecurity.
Methods
A cross-sectional sampling of quilombola individuals living in four communities of southern Brazil, as well as their dogs and the soil, was carried out from December 2021 to March 2022. Sociodemographic and other information such as water source, alimentary habits, and dog and cat ownership were gathered using a semi-structured questionnaire for assessing toxocariasis risk factors. Human serum samples were tested by ELISA for anti-Toxocara spp. IgG antibody detection was carried out on dog feces and hair, and soil samples were surveyed for presence of Toxocara spp. eggs.
Results
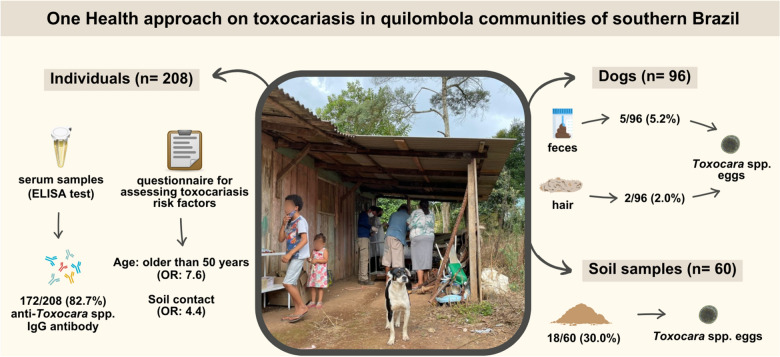
Overall, 172/208 individuals (82.7%, 95% CI = 77.0–87.2) were seropositive, the highest seroprevalence rate to date in Brazil. Male gender (P = 0.029), educational level (P = 0.026), and drinking water source (P = 0.043) were associated with seropositivity by univariate analysis. Final logistic regression revealed increased odds (P = 0.017, OR = 7.6, 95% CI = 1.5–42.7) to have seropositivity in individuals > 50 years old (< 10 years old). As expected, individuals with soil contact were more likely seropositive (P = 0.038, OR = 4.4, 95% CI = 1.1–18.8). Although retrieved in only 5/96 (5.2%) dog feces, Toxocara spp. eggs were found in 18/60 (30.0%) soil samples.
Conclusions
The high vulnerability and seroprevalence observed in quilombola communities clearly demand a One Health approach for detection, monitoring, and prevention of infection by Toxocara spp. in both human and dog populations.
Graphical Abstract
Supplementary Information
The online version contains supplementary material available at 10.1186/s13071-023-06010-w.
Keywords: Epidemiology, Poverty, Quilombo, Seroprevalence, Toxocara spp., Zoonosis
Background
Toxocariasis has been a prevalent zoonosis with a significant socioeconomic impact, particularly on impoverished communities worldwide [1], and has been included among the six most important neglected parasitic infections in the USA along with Chagas disease, cyclosporiasis, cysticercosis, toxoplasmosis, and trichomoniasis [2]. Characterized by significant seroprevalence and chronic disease and associated with poverty [3], this disease has also been considered the fourth and, perhaps equally important, a soil-transmitted helminth infection along with ascariasis, trichuriasis, and hookworm [4].
Accidental ingestion of soil containing Toxocara canis or Toxocara cati infective eggs has been considered the primary transmission route of human toxocariasis [5]. As natural definitive hosts, dogs and cats may shed roundworm eggs in feces, become infective following an embryonation period of 2 to 5 weeks, and persist in the environment for months [6]. Although some studies in Brazil have observed a higher recovery of eggs from soil in public parks in winter and summer [7], and throughout the year [8], to our knowledge no study assessing the persistence of Toxocara spp. eggs in tropical environments over time has been conducted to date.
Migration or larva-induced immune response may lead to several clinical manifestations in humans, with visceral toxocariasis mostly resulting in hepatic and pulmonary disorders [9]. The ocular form has reportedly caused visual impairment and blindness, while neurological presentation (neurotoxocariasis) may cause central nervous system impairment [10].
Approximately one fifth of the global human population has been exposed to toxocariasis agents according to a meta-analysis study, presenting the highest seroprevalence in Africa and Latin America [11]. Associated risk factors to Toxocara spp. seropositivity revealed higher risk of young people, males, those living in rural areas, those in close contact with dogs, cats, or soil, those consuming raw meat, and those drinking untreated water [11]. In Brazil, the highest seroprevalence to date (247/344; 71.8%) was observed in adult inhabitants of rural southern Brazil [12]. As social vulnerability has also been associated with toxocariasis, different vulnerable Brazilian populations have demanded a One Health approach and required simultaneous human-animal-soil samplings to address zoonotic issues in animal keepers and the homeless, incarcerated, indigenous, and traditional island populations [13].
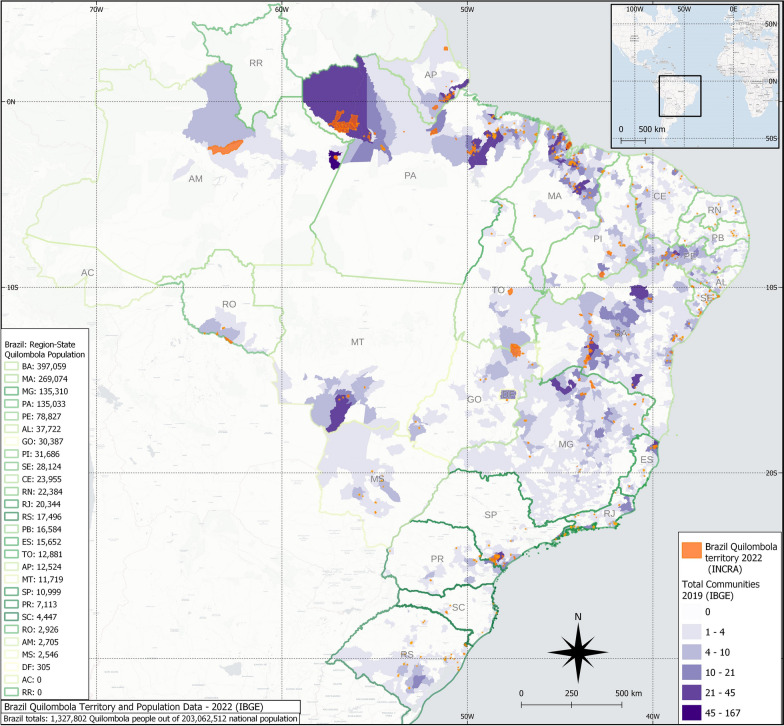
Another vulnerable and traditional Brazilian community (named quilombola) comprises former African slaves and their descendants, who have historically remained in rural and semi-isolated areas since the time of slavery [14], preserving their African culture and subsisting on agriculture and forest resources [15]. Despite historical government efforts, this population has lived under poverty, greater social and health needs, poor quality of life, and nutritional insecurity [16]. A total of 494 quilombola communities were registered in the recent 2022 census by the Brazilian Institute of Geography and Statistics (IBGE), with 167,202/1,327,802 (12.6%) individuals living within these territories out of the total of self-declared quilombola population in Brazil (Fig. 1) [17]. Quilombola communities have mostly dogs as companion animals, usually wandering but also including owned restricted and semi-restricted ones, which may carry zoonotic pathogens including Ehrlichia spp., Anaplasma spp., Leishmania spp., Borrelia burgdorferi s.l., and Dirofilaria immitis [18].
Fig. 1.
Quilombola communities, territories, and population in Brazil, according to the Brazilian Institute of Geography and Statistics (IBGE)
Besides social vulnerability, a favorable scenario for Toxocara spp. transmissionin quilombola communities may also include close and daily contact with agricultural labor and presence of untreated dogs, as dogs and cats in low-income and rural regions have played an important role in toxocariasis [5]. Nonetheless, to our knowledge no comprehensive study has been conducted in this susceptible population, particularly regarding a One Health approach. Accordingly, this study aimed to survey and analyze risk factors associated with human toxocariasis, including the presence of Toxocara spp. eggs in dog hair and feces and in soil samples in four rural quilombola communities of southern Brazil.
Methods
Study design
The present study was a cross-sectional survey conducted in four Brazilian quilombola (out of 34) communities located in Paraná State, southern Brazil, from December 2021 to March 2022 (Table 1). The study area herein included natural and degraded areas of two Brazilian biomes (Atlantic Forest and Cerrado), with humid temperate climate and averaging 17.5 °C in temperature and 1495 mm3 in annual precipitation. The land use and occupations in traditional quilombola communities have often been connected to a common use approach of territory. However, surrounding properties usually have not followed the same land use pattern, leading to conflicts and influencing the changes in perspective of what land means for members of traditional communities [19, 20]. Quilombola communities of Paraná State have lived mostly on subsistence agriculture and livestock, with continuous land struggle caused by surrounding commercial wood and cellulose production companies, mostly of Eucalyptus spp. trees.
Table 1.
Characteristics of four quilombola communities located in rural areas of Paraná State, southern Brazil, for assessing risk factors of toxocariasis
| Quilombola communities | Geographic coordinates | Estimated population* | n sampled (%) |
|---|---|---|---|
| Limitão | 24°40′37.04′′S 49°35′53.05′′O | 106 | 45 (42.5) |
| Mamans | 24°55′11.73′′S 49°41′4.78′′O | 48 | 42 (87.5) |
| Serra do Apon | 24°51′45.40′′S 50°2′42.97′′O | 145 | 70 (48.3) |
| Tronco | 24°51′21.0′′S 50°01′49.0′′O | 62 | 51 (82.3) |
*Priori et al. [21]
The human sample size was calculated considering a 27.6% toxocariasis seropositivity in the general Brazilian population, based in a recent worldwide meta-analysis study [11], and an estimated population of 3800 quilombola individuals in the Paraná State [21]. An assumption of 6% precision was considered in an expected range prevalence of 10–90%, based on preliminary studies with 95% confidence level [22, 23], resulting in a minimum of 203 individuals.
A structured epidemiological questionnaire was applied, after the subjects provided an individual signed consent form, which included information on sociodemographic aspects such as age, gender, educational level, and potential associated risk factors such as the drinking water source or type, contact with soil, raw meat intake, ingestion of game meat, onychophagy, and owning dogs, cats, or both. Parents and other relatives provided written consent for subjects < 18 years old and illiterate individuals prior to blood collection and epidemiological questionnaire. In addition, dog owners were interviewed on the epidemiological questionnaires about themselves and their dogs and provided a signed consent form for blood samplings from them and their dogs.
Blood samples were conveniently collected from quilombola individuals by peripheral venipuncture, performed by a certified physician, nurse, or pharmacist and using commercial vacuum tubes, after providing a signed consent form. Samples were centrifuged at 1295 × g for 5 min and the obtained serum stored at −20 °C until processing.
Detection of anti-Toxocara spp. IgG
Antigen preparation
In vitro production of T. canis excretory-secretory larval antigens (TES) was based on the method described by Savigny et al. [24], with some modifications [25].
Pre-adsorption of human serum
Serum samples were pre-adsorbed with Ascaris suum adult worm extract (AWE) following an established protocol [25] to remove antibodies elicited by exposure to Ascaris that could cross-react with Toxocara spp. antigens and, consequently, enhance the specificity of the ELISA test [26].
ELISA test
Serum samples were tested for IgG antibodies to TES by ELISA (enzyme-linked immunosorbent assay) at a dilution of 1:200 [25] at the Laboratory of Medical Investigation, Institute of Tropical Medicine of São Paulo, University of São Paulo, Brazil. The negative sera controls were stored in the serum bank and have been routinely used in ELISA for toxocariasis, with 78.3% sensitivity and 92.3% specificity, as previously reported in other studies [27, 28]. The sera were previously tested by an established protocol [25] and were negative for parasites in previous studies [29, 30].
Absorbance readings were made at 492 nm (Titertek Multiskan MCC/340, Lab-System, Finland), and a cut-off absorbance value was defined as the mean absorbance reading for 90 negative control sera plus three standard deviations. Standard positive and negative control serum and a threshold reactive serum were used in all tests. The antibody levels were expressed as reactivity indices (RIs) that were calculated as the ratio between the absorbance values of each test sample and the cutoff value, set at 0.350. A serum sample was considered positive when its RI was > 1.
Dog samples
Dog samples included feces and hair and were individually collected from 96 dogs living in the studied quilombola communities. Dogs were physically restrained; feces were collected from the rectum and transferred to 50-ml plastic tubes with 10% formalin solution to preserve parasite eggs [31]. Hair samples were collected at the dorsal and perineal areas from each dog using commercial blades and placed in 50-ml plastic tubes. Fecal and dog hair samples were kept under refrigeration at 4 °C until processing and analysis.
Dog feces samples were processed to assess the presence of Toxocara spp. eggs by using a flotation technique (hypersaturated sodium chloride solution d = 1.20 g/cm3). Results were considered positive or negative.
Hair samples were processed using a previous protocol described elsewhere [32], with some modification [33]. Briefly, hair samples were rinsed with anionic detergent (Tween 80®), sieved (300, 212 and 38 μm), and centrifugated (5 min, 1090 ×g). Then, pellets were analyzed under a microscope (magnifications: 10 × and 40×).
Toxocara spp. eggs recovered from dog hair were classified according to criteria, as previously established [32]: embryonated eggs (containing larva); embryonating eggs (cellular division); viable (intact eggs with content); non-viable eggs (wall disruption).
Soil sampling and testing
Around 50 g of soil samples was randomly collected from the commonly used areas at the four quilombola communities, including community centers and trails. The sampling sites were selected by convenience, and free-roaming dogs were present there. Grass areas and presence of feces were considered exclusion criteria for local soil collection. Samples were collected at a depth of 5 to 10 cm, transferred to a plastic bag, and stored under refrigeration (4 ºC) until processing. A total of 60 soil samples were collected, ranging from 10 to 20 samples per community.
Soil analysis followed the protocol described elsewhere [34, 35] with some modifications [13]. Briefly, 20 g of soil was submitted to a protocol of rinsing with anionic detergent (100 ml 5% Tween 80®), sieving procedure (300 μm, 212 μm, 90 μm, and 38 μm), and centrifugation (800 × g for 5 min). Following this, the sediment was subjected to a centrifuge-flotation technique (zinc sulfate solution d = 1.35 g/cm3). After a 5-min flotation period, 5 ml of the floating content was transferred to two other graduated tubes (2.5 ml each). Then, 10 ml distilled water was added, and another centrifugation (800 ×g for 5 min) performed. The washing process was repeated three times to remove the sulfate solution. Then, the entire sediment was analyzed under a microscope (magnifications: 10 × and 40 ×), and Toxocara spp. eggs recovered from soil were classified as described [32].
Statistical analysis
Categorical variables were subjected to univariate analysis to select possible factors associated with seropositivity for Toxocara spp. in quilombola populations, considering up to 15.0% missing data. The association was tested using the Chi-square test or Fisher test when expected values were < 5.0, with estimates of odds ratio and 95% confidence intervals. Variables with a significance level < 0.2 were used as potential predictors of seropositivity for a multivariate logistic model with variable selection by the backward stepwise algorithm. The model was evaluated for the presence of collinearity by estimating the variance inflation factor (VIF) and the accuracy in predicting seropositivity by ROC curve. The receiver-operating characteristic (ROC) is a graphical tool commonly used to assess the performance and accuracy of predictive models, particularly binary classification models like logistic regression for risk factors in epidemiological surveys [36]. The AUC was estimated by integral calculus of the ROC curve. The result provided a single value summarizing the model's discriminatory power, varying between 0.5 (indicating absence of discriminatory power between seropositive and seronegative cases) and 1.0 (representing perfect discrimination between seropositive and seronegative cases). All analyses were conducted using R software v. 4.2.2 and auxiliary packages, considering a significance level of 5% [37, 38].
Results
The studied population was composed by adults (77.4%; 161/208) ranging from 1 to 99 years old (median: 37), mostly females (126/208; 60.6%). Most participants declared having elementary school level education (128/208; 61.5%) and contact with soil (188/208; 90.4%). All the adult participants mentioned subsistence agriculture activities (Additional file 2).
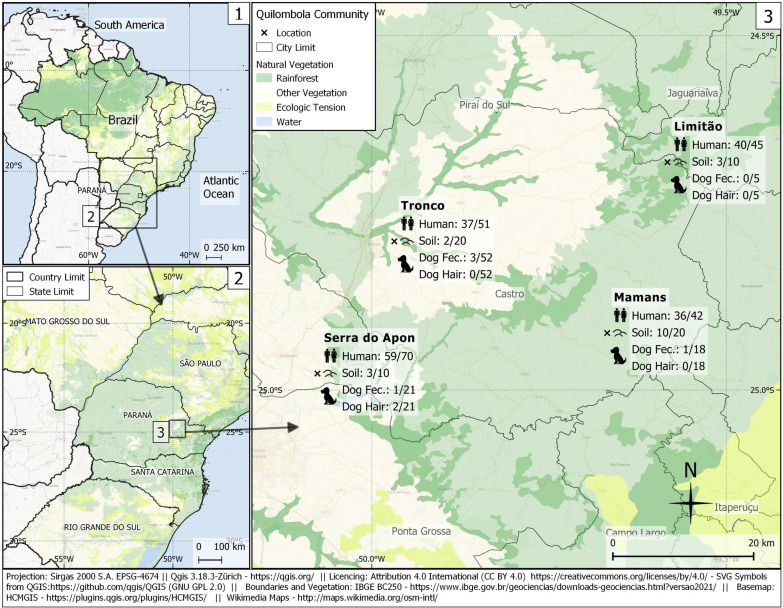
Overall, 172/208 (82.7%; 95% CI = 77.0–87.2) quilombola individuals were seropositive for circulating anti-Toxocara spp. antibodies (Fig. 2). Seroprevalence ranged from 72.6% to 88.9% in Tronco and Limitão communities, respectively (Table 2), with no statistical difference (P = 0.153) among frequencies. Associated Risk factors for the presence of anti-Toxocara spp. antibodies in participants by uni- and multivariate analysis were tested (Table 3), and five variables (gender, age, educational level, contact with soil, and drinking water source) were included in the multivariate logistic model. Logistic regression revealed only age and contact with soil as predictive variables for seropositivity. Increased odds (P = 0.017, OR = 7.6, 95% CI = 1.5–42.7) for seropositivity (Table 3) were observed in individuals aged > 50 years old compared to the reference group (< 10 years old) and in quilombola participants who had close contact with soil (P = 0.038, OR = 4.4, 95% CI = 1.1–18.8).
Fig. 2.
Sampling locations, frequency of occurrence of anti-Toxocara spp. antibodies in quilombola individuals, and the presence of feces, hair, and soil-positive samples in quilombola communities of southern Brazil
Table 2.
Seroprevalence of anti-Toxocara spp. antibodies (IgG) detected by ELISA test in quilombola persons (N = 208) living in five communities of Paraná State, southern Brazil
| Communities | Seropositivity/ subjects | Frequency (%) | 95% CI |
|---|---|---|---|
| Limitão | 40/45 | 88.9 | 76.5–95.2 |
| Mamans | 36/42 | 85.7 | 72.2–93.3 |
| Serra do apon | 59/70 | 84.3 | 74.0–91.0 |
| Tronco | 37/51 | 72.6 | 59.1–82.3 |
| Total | 172/208 | 82.7 | 77.0–87.2 |
Table 3.
Univariate and logistic multivariate regression association between characteristics of quilombola communities (N = 208) and presence of anti-Toxocara spp. antibodies IgG, in communities of Paraná State, southern Brazil
| Characteristics | Seropositive (%) | Seronegative (%) | Univariate analysis | Multivariate analysis | ||
|---|---|---|---|---|---|---|
| 172 (82.7) | 36 (17.3) | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Gender | 0.029* | |||||
| Female | 98 (56.5) | 28 (77.8) | 1.0 [Reference] | 1.0 [Reference] | ||
| Male | 74 (43.5) | 8 (22.2) | 2.7 (1.2–6.5) | 2.7 (0.9–9.7) | 0.099 | |
| Age (years old) | 0.001* | |||||
| < 10 | 13 (7.6) | 9 (25.0) | 1.0 [Reference] | 1.0 [Reference] | ||
| 10 to 17 | 16 (9.4) | 8 (22.2) | 1.4 (0.4–4.8) | 1.1 (0.2–6.5) | 0.944 | |
| 18 to 49 | 80 (46.7) | 14 (38.9) | 3.9 (1.4–11.0) | 3.5 (0.7–17.8) | 0.137 | |
| ≥ 50 | 62 (36.3) | 5 (13.9) | 8.2 (2.4–31.5) | 7.6 (1.5–42.7) | 0.017* | |
| Educational level | 0.026* | |||||
| High school | 31 (18.3) | 12 (34.3) | 1.0 [Reference] | 1.0 [Reference] | ||
| Elementary | 113 (66.9) | 15 (42.9) | 2.9 (1.2–6.9) | 2.7 (0.8–9.0) | 0.111 | |
| Illiterate | 25 (14.8) | 8 (22.9) | 1.2 (0.4–3.6) | 0.11 (0.1–3.5) | 0.576 | |
| Contact with soil | 0.003* | |||||
| No | 7 (4.17) | 7 (20.6) | 1.0 [Reference] | 1.0 [Reference] | ||
| Yes | 161 (95.8) | 27 (79.4) | 5.9 (1.8–18.9) | 4.4 (1.1–18.8) | 0.038* | |
| Drinking water source | 0.043* | |||||
| River | 22 (14.4) | 1 (3.2) | 1.0 [Reference] | 1.0 [Reference] | ||
| Artesian well | 42 (27.5) | 15 (48.4) | 0.2 (0.01–0.8) | 0.2 (0.01–1.0) | 0.104 | |
| Springer water | 89 (58.2) | 15 (48.4) | 0.3 (0.01–1.7) | 0.4 (0.02–2.7) | 0.455 | |
| Onicophagy | 0.912 | |||||
| No | 121 (73.8) | 26 (76.5) | 1.0 [Reference] | |||
| Yes | 43 (26.2) | 8 (23.5) | 1.1 (0.5–2.9) | |||
| Ingestion of raw meat | 0.743 | |||||
| No | 154 (91.7) | 34 (94.4) | 1.0 [Reference] | |||
| Yes | 14 (8.33) | 2 (5.56) | 1.5 (0.4–10.4) | |||
| Game meat consumption | 0.581 | |||||
| No | 145 (85.8) | 31 (91.2) | 1.0 [Reference] | |||
| Yes | 24 (14.2) | 3 (8.8) | 1.6 (0.5–7.5) | |||
| Owning a dog | 0.472 | |||||
| No | 13 (7.8) | 1 (2.9) | 1.0 [Reference] | |||
| Yes | 153 (92.2) | 33 (97.1) | 0.4 (0.02–2.2) | |||
| Owning a cat | 1.0 | |||||
| No | 79 (47.6) | 16 (47.1) | 1.0 [Reference] | |||
| Yes | 87 (52.4) | 18 (52.9) | 1.0 (0.5–2.1) | |||
| Owning a dog and a cat | 1.0 | |||||
| No | 81 (48.8) | 16 (47.1) | 1.0 [Reference] | |||
| Yes | 85 (51.2) | 18 (52.9) | 0.9 (0.4–2.00) | |||
*Statistically significant
Area under the ROC curve (AUC = 0.823, 95% CI = 0.739–0.907) suggested that the final logistic regression model showed a moderate to excellent performance [39] (Additional file 1: Figure S1). No collinearity among variables was observed in the logistic regression model. All variables, except gender, presented inconsistent or missing data in the questionnaires; however they were maintained in the analysis since they incurred losses < 15.0%.
Overall, 186/208 (89.4%) quilombola individuals owned at least one dog (range: 1 to 10; average: 2.8) and 105/208 (50.5%) at least one cat (range: 1 to 10; average: 2.0); a total of 103/208 (49.5%) declared raising both. Most of the dogs (90/96; 93.8) were > 1 year old, according to their owners. During the visits, low body condition score was mostly observed in dogs. Lack of vaccine and deworming scheme was reported by all dog owners. Toxocara spp. eggs were detected in 5/96 (5.2%) dog fecal samples from quilombola communities (Table 4). The community with the highest prevalence of Toxocara spp. in dogs was Tronco (3/52; 5.8%), followed by Mamans (1/18; 5.5%) and Serra do Apon (1/21; 4.8%). No positive sample was verified in the Limitão community. Regarding hair samples, 2/96 (2.0%) dogs, both from Serra do Apon community, had Toxocara spp. eggs adhered to fur. One of these dogs presented viable Toxocara spp. eggs in hair from the dorsal (1 egg) and perineal (30 eggs) regions, while the other presented just one viable Toxocara spp. egg in the dorsal region. The presence of Toxocara spp. eggs in both feces and hair samples was observed in a dog. No Toxocara spp. eggs were recovered in dog hair samples from the others visited quilombola communities (Table 4).
Table 4.
Frequency of Toxocara spp. eggs in fecal and hair samples of dogs living in quilombola communities of Paraná State, southern Brazil
| Communities | Samples: positive /total (%) | |
|---|---|---|
| Feces | Hair | |
| Limitão | 0/5 (0.0) | 0/5 (0.0) |
| Mamans | 1/18 (5.5) | 0/18 (0.0) |
| Serra do Apon | 1/21 (4.8) | 2/21 (9.5) |
| Tronco | 3/52 (5.8) | 0/52 (0.0) |
| Total | 5/96 (5.2) | 2/96 (2.0) |
A total of 18/60 (30.0%) soil samples were positive for Toxocara spp. eggs (Table 5). Herein, as the total number of recovered eggs was low (42 eggs), the average number of eggs per community was calculated considering 100 g of soil. The highest frequency of positive samples and number of recovered Toxocara spp. eggs were observed in quilombola community Mamans (7 eggs/100 g of soil), followed by Serra do Apon (4.5 eggs/100 g of soil), Limitão (1.5 egg/100 g of soil) and Tronco (1 egg/100 g of soil). Most of the Toxocara ssp. eggs recovered from soil were classified as non-viable (35/42; 83.3%) (Table 5).
Table 5.
Toxocara spp. eggs recovered from soil samples collected in quilombola communities of Paraná State (southern Brazil) according to its morphological characteristic
| Communities | Positive/total (%) | Morphological characteristics of Toxocara spp. eggs | |||
|---|---|---|---|---|---|
| V | NV | EM | E | ||
| Limitão | 3/10 (30.0) | 0 | 3 | 0 | 0 |
| Mamans | 10/20 (50.0) | 3 | 24 | 0 | 1 |
| Serra do Apon | 3/10 (30.0) | 2 | 7 | 0 | 0 |
| Tronco | 2/20 (10.0) | 1 | 1 | 0 | 0 |
| Total (%) | 18/60 (30.0) | 6/42 (14.3) | 35/42 (83.3) | 0 | 1/42 (2.4) |
V viable, NV non-viable, EM embryonated egg, E: embryonated (containing larvae)
Discussion
This is the first serosurvey to our knowledge based on a One Health approach that investigates the potential risk factors for toxocariasis in Brazilian quilombos along with environmental contamination and dog infection by Toxocara spp. Moreover, quilombola communities presented the highest seroprevalence (172/208; 82.7%) for toxocariasis in Brazil to date, surpassing a serosurvey in a rural adult population (247/344; 71.8%) of southern Brazil [12]. Living in rural areas itself is a major risk factor associated with seropositivity for Toxocara spp. (OR = 1.9) according to a global meta-analysis [11], corroborated by surveys in rural populations of Gabon, Africa (199/332; 53.6%) [40], and Thailand (101/132; 76.5%), Asia [41].
In addition to rural area exposure, higher toxocariasis seroprevalence is also more likely in those with lower educational and socioeconomic levels living under poor sanitary conditions as observed in our study [9]. Not surprisingly, a nationwide Brazilian survey has observed inadequate sanitation in 8291/8743 (94.8%) quilombola communities [16]. The main reported factors associated with quilombola vulnerability included low family income and education, difficulty in accessing drinking water, lack of health services [42–45], and food insecurity in the household [16, 46]. In this scenario, the lifestyle of quilombola populations favors high exposure to Toxocara spp. infection.
Aging remains controversial as an associated risk factor for toxocariasis. Logistic regression revealed age and contact with soil as predictive factors for toxocariasis, with a direct increase of seropositivity by age, corroborating a national USA serosurvey in which individuals > 50 years old were more likely seropositive than 6–11 year olds [47]. However, a study in a rural area in northern Brazil with 466 individuals from 5 to 90 years old showed higher seropositivity in 5 to 14 year old children (36.6%) than in older subjects (22.5%) [48]. In addition, higher toxocariasis seroprevalence was observed in younger subjects (10–19 years) followed by a decline in early adulthood and a second rise during older age in Jamaica [49]. This pattern in younger persons may be due to decreased exposure to infective Toxocara spp. stages with age and a subsequent decline in antibody levels over time, while an increase in prevalence at older age may be due to later exposure due to agricultural or other outdoor land activities [49].
As land subsistence practices and agricultural activities have been reportedly inherited in quilombola culture [16, 50], human infection risk may be related to close contact with soil contaminated by Toxocara spp. eggs in rural areas [11, 40], with all adult participants referring to agricultural practices in our study. Thus, labor activities of quilombola individuals may have favored a continuous exposure to infection via soil and, consequently, the maintenance of anti-Toxocara spp. antibodies levels over time. As expected in the present study, and reinforcing this statement, Toxocara spp. eggs were retrieved in soil samples of all four quilombola communities.
Male gender has been demonstrated as an associated risk factor for toxocariasis [47, 51, 52], with 1.3 increased odds of seropositivity in a meta-analysis study [11]. According to our results, both women and men were at risk of infection from ingestion of Toxocara spp. eggs via soil, probably from working in outdoor land activities and/or following poor hygienic habits.
Low educational level has been historically associated to toxocariasis [9], even in developed countries such as the USA [47, 51]. In Brazil, higher education was a protective factor against Toxocara spp. exposure (OR = 0.2) in persons experiencing homelessness [53]. Despite being considered a predictive factor for toxocariasis in univariate analysis but not in logistic regression, low educational level and socioeconomic status factors may concomitantly increase the risk of Toxocara spp. infection [9]. Likewise, univariate analysis here revealed an association with seropositivity and untreated water consumption (OR = 2.0), as source of drinking water has been considered a risk factor for Toxocara seropositivity [11]. As previously reported, untreated wastewater for irrigation was considered a contamination source of agricultural products with Toxocara spp. eggs in North Africa [54]. In addition, a systematic review included toxocariasis in the top list of water-borne transmitted parasitic diseases in the Middle East and North Africa, highlighting the importance of drinking water sources and sanitation facilities to reduce disease transmission [55]. No study on the persistence of Toxocara eggs in water has been found in Brazil or other Latin American countries.
Fecal and hair samples from the quilombola community dogs confirmed the presence of Toxocara spp. eggs. Although having dogs, cats, or both was not associated with human seropositivity, approximately 90% and 50% of quilombola individuals declared having at least one dog or one cat. Additionally, dogs and cats were mostly unleashed, free-roaming, and not dewormed in the studied quilombola communities. As contact with dogs and cats has already been considered another associated risk factor for toxocariasis, mainly in younger people [11, 56], companion animal deworming should be always recommended to reduce Toxocara spp. egg shedding into the environment and posterior transmission via soil ingestion to the exposed population [57].
In this study, no association was observed between seropositivity and ingestion of raw, undercooked, or game meat. The quilombola population in this study mostly (> 90.0%) reported no habits of consuming raw meat of either domestic or game animals, reducing the likelihood of toxocariasis via animal consumption. The ingestion of undercooked or raw meat from paratenic hosts, mainly cattle and chickens, has been associated with toxocariasis [58–60], mostly in Asian countries because of local habits of eating raw meat [61]. In Brazil, serosurveys and a review study [62] have indicated no association between consumption of raw meat and toxocariasis [13, 53, 63]. As previously shown for quilombola communities, although having low consumption of raw and undercooked meat, the logistic regression showed that those individuals who said they consumed raw or undercooked game meat were 2.4-fold more likely (P = 0.042, 95% CI = 1.1–5.9) to be seropositive for Toxoplasma gondii [64].
As limitations of our study, remote locations are difficult to access, restricting visits to quilombola communities. Thus, assessment of stool of quilombola individuals for potential infection by Ascaris lumbricoides was not possible. However, the protocol used herein for detecting anti-Toxocara spp. antibodies has been employed in other serosurveys evaluating people in vulnerabile conditions [13, 53], using pre-adsorption of sera with A. suum adult worm extract to mitigate cross-reactivity with other Ascaridia, including A. lumbricoides [26]. Additionally, the presence of Toxocara spp. in cat biological samples (hair and feces) was not analyzed because of refusal of quilombola communities due to health and cruelty risks when catching and restraining the animals. Furthermore, soil samples were collected from common areas used by the community, which may not fully reflect the individual exposure to contaminated soil with Toxocara spp. eggs. Finally, future studies should analyze soil samples from areas of land labor and include elderly subjects to fully establish Toxocara spp. in such quilombola communities.
Conclusions
The high seroprevalence observed in quilombola communities of southern Brazil suggested high exposure to toxocariasis. The high vulnerability and close human-soil contact observed here as risk factors demand a One Health approach for detection, monitoring, and prevention of Toxocara spp. infection in both human and dog populations. Furthermore, educational improvement is necessary to prevent toxocariasis and other zoonotic infections.
Supplementary Information
Additional file 1: Figure S1. Receiver-operating characteristic (ROC) curve [evaluating the accuracy of the multivariate logistic regression model (AUC = 0.823, 95% CI = 0.739–0.907)] to predict seropositivity for anti-Toxocara spp. antibodies in individuals of quilombola communities of Paraná State, southern Brazil
Additional file 2: Raw data of associated risk factors of toxocariasis in quilombola communities of southern Brazil..
Acknowledgements
The authors thank the Association of Rural Black Communities, City of Castro, Paraná State, for the support in advertising the visits, data collection, guidance, infrastructure, samplings, and follow-up information. The authors also thank the State University of Ponta Grossa and the Federal University of Paraná for providing professional and technical support.
Author contributions
LBK, AWB, and GMF have contributed to the design of the work; OJD, JHF, FRD, IBF, RTSF, LMB, SAZL, and RG to the analysis, VAS, LBK, AWB, RG, and GMF to the interpretation of data; VAS, LBK, AWB drafted the work and substantively revised the manuscript. All authors have approved the submitted version (and any substantially modified version that involves the author's contribution to the study). All authors have agreed both to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated and resolved and the resolution documented in the literature.
Funding
Not applicable.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its Additional file information.
Declarations
Ethics approval and consent to participate
This study was approved by Ethics Committee in Human Health of the Brazilian Ministry of Health (protocol 53828121.1.0000.0105) and by the Ethics Committee of Animal Use (protocol 22.000075139-9) of the State University of Ponta Grossa, Paraná, Brazil.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Vamilton Alvares Santarém and Giovanni Kalempa Panazzolo have equally contributed to this work and share first authorship.
References
- 1.Rostami A, Ma G, Wang T, Koehler AV, Hofmann A, Chang BCH, et al. Human toxocariasis—a look at a neglected disease through an epidemiological ‘prism’. Infect Genet Evol. 2019;74:104002. doi: 10.1016/j.meegid.2019.104002. [DOI] [PubMed] [Google Scholar]
- 2.CDC—Centers for Disease Control and Prevention. Parasites—Parasitic infections in the United States. 2020. https://www.cdc.gov/parasites/npi/index.html. Accessed 15 Aug 2023.
- 3.CDC—Centers for Disease Control and Prevention. Parasites—Soil-transmitted helminths. 2022. https://www.cdc.gov/parasites/sth/. Accessed 11 May 2023.
- 4.Hotez PJ. Toxocariasis: a neglected infection for the anthropocene epoch. Adv Parasitol. 2020;109:879–883. doi: 10.1016/bs.apar.2020.03.004. [DOI] [PubMed] [Google Scholar]
- 5.Holland CV. Knowledge gaps in the epidemiology of Toxocara: the enigma remains. Parasitology. 2017;144:81–94. doi: 10.1017/S0031182015001407. [DOI] [PubMed] [Google Scholar]
- 6.Despommier D. Toxocariasis: clinical aspects, epidemiology, medical ecology, and molecular aspects. Clin Microbiol Rev. 2003;16:265–272. doi: 10.1128/CMR.16.2.265-272.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tiyo R, Guedes TA, Falavigna DLM, Falavigna-Guilherme AL. Seasonal contamination of public squares and lawns by parasites with zoonotic potential in southern Brazil. J Helminthol. 2008;82:1–6. doi: 10.1017/S0022149X07870829. [DOI] [PubMed] [Google Scholar]
- 8.Santarém VA, Pereira VC, Alegre BCP. Contamination of public parks in Presidente Prudente (São Paulo, Brazil) by Toxocara spp eggs. Rev Bras Parasitol Vet. 2012;21:323–5. doi: 10.1590/s1984-29612012000300029. [DOI] [PubMed] [Google Scholar]
- 9.Ma G, Holland CV, Wang T, Hofmann A, Fan C-K, Maizels RM, et al. Human toxocariasis. Lancet Infect Dis. 2018;18:e14–24. doi: 10.1016/S1473-3099(17)30331-6. [DOI] [PubMed] [Google Scholar]
- 10.Mazur-Melewska K, Mania A, Sluzewski W, Figlerowicz M. Clinical pathology of larval toxocariasis. Adv Parasitol. 2020;109:153–163. doi: 10.1016/bs.apar.2020.01.004. [DOI] [PubMed] [Google Scholar]
- 11.Rostami A, Riahi SM, Holland CV, Taghipour A, Khalili-Fomeshi M, Fakhri Y, et al. Seroprevalence estimates for toxocariasis in people worldwide: a systematic review and meta-analysis. PLoS Negl Trop Dis. 2019;13:e0007809. doi: 10.1371/journal.pntd.0007809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Araújo AC, Villela MM, Sena-Lopes Â, da Farias NA, et al. Seroprevalence of Toxoplasma gondii and Toxocara canis in a human rural population of Southern Rio Grande do Sul. Rev Inst Med Trop Sao Paulo. 2018;60:e28. doi: 10.1590/S1678-9946201860028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Delai RR, Freitas AR, Kmetiuk LB, Merigueti YFFB, Ferreira IB, Lescano SAZ, et al. One Health approach on human seroprevalence of anti-Toxocara antibodies, Toxocara spp eggs in dogs and sand samples between seashore mainland and island areas of southern Brazil. One Heal. 2021;13:100353. doi: 10.1016/j.onehlt.2021.100353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Constantino DB, Xavier NB, Levandovski R, Roenneberg T, Hidalgo MP, Pilz LK. Relationship between circadian strain, light exposure, and body mass index in rural and urban quilombola communities. Front Physiol. 2021;12:773969. doi: 10.3389/fphys.2021.773969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Conde BE, Aragaki S, Ticktin T, Surerus Fonseca A, Yazbek PB, Sauini T, et al. Evaluation of conservation status of plants in Brazil’s Atlantic forest: an ethnoecological approach with Quilombola communities in Serra do Mar State Park. PLoS ONE. 2020;15:e0238914. doi: 10.1371/journal.pone.0238914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.de Cherol CC, Ferreira SAA, Salles-Costa R. Governmental programmes associated with food insecurity among communities of descendants of enslaved blacks in Brazil. Public Health Nutr. 2021;24:3136–46. doi: 10.1017/S1368980020004164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.IBGE. Indígenas. https://indigenas.ibge.gov.br/. Accessed 20 Jan 2023.
- 18.de Macedo LO, Bezerra-Santos MA, Filho CRCU, da Silva Sales KG, de Sousa-Paula LC, da Silva LG, et al. Vector-borne pathogens of zoonotic concern in dogs from a Quilombola community in northeastern Brazil. Parasitol Res. 2022;121:3305–3311. doi: 10.1007/s00436-022-07661-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Alves IR. Resiliência espacial em comunidades quilombolas: desafios relacionados ao uso e ocupação do solo em terras uso comum. 2020. https://locus.ufv.br//handle/123456789/28661. Accessed 4 May 2023.
- 20.Campos MDC, Gallinari TS. Permanência e resistência das comunidades remanescentes de quilombos no Paraná. Geosaberes. 2017;8:131. [Google Scholar]
- 21.Priori A, Pomari LR, Amâncio SM, Ipólito VK. História do Paraná: séculos XIX e XX. EDUEM; 2012. http://books.scielo.org/id/k4vrh. Accessed 4 May 2023.
- 22.Naing L, Bin NR, Abdul Rahman H, Naing YT. Sample size calculation for prevalence studies using Scalex and ScalaR calculators. BMC Med Res Methodol. 2022;22:209. doi: 10.1186/s12874-022-01694-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Manitz J, Hempelmann M, Kauermann G, Kuechenhoff H, Shao S, Oberhauser C, et al. samplingbook: Survey Sampling Procedures. 2021. https://cran.r-project.org/web/packages/samplingbook/index.html. Accessed 4 May 2023.
- 24.de Savigny DH, Voller A, Woodruff AW. Toxocariasis: serological diagnosis by enzyme immunoassay. J Clin Pathol. 1979;32:284–288. doi: 10.1136/jcp.32.3.284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Elefant GR, Shimizu SH, Sanchez MCA, Jacob CMA, Ferreira AW. A serological follow-up of toxocariasis patients after chemotherapy based on the detection of IgG, IgA, and IgE antibodies by enzyme-linked immunosorbent assay. J Clin Lab Anal. 2006;20:164–172. doi: 10.1002/jcla.20126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Romasanta A, Romero JL, Arias M, Sánchez-Andrade R, López C, Suárez JL, et al. Diagnosis of parasitic zoonoses by immunoenzymatic assays—analysis of cross-reactivity among the excretory/secretory antigens of Fasciola hepatica, Toxocara canis, and Ascaris suum. Immunol Invest. 2003;32:131–142. doi: 10.1081/imm-120022974. [DOI] [PubMed] [Google Scholar]
- 27.Glickman L, Schantz P, Dombroske R, Cypess R. Evaluation of serodiagnostic tests for visceral larva migrans. Am J Trop Med Hyg. 1978;27:492–498. doi: 10.4269/ajtmh.1978.27.492. [DOI] [PubMed] [Google Scholar]
- 28.Fillaux J, Magnaval JF. Laboratory diagnosis of human toxocariasis. Vet Parasitol. 2013;193:327–336. doi: 10.1016/j.vetpar.2012.12.028. [DOI] [PubMed] [Google Scholar]
- 29.Matos Fialho PM, Correa CRS, Lescano SZ. Seroprevalence of toxocariasis in children with urticaria: a population-based study. J Trop Pediatr. 2017;63:352–357. doi: 10.1093/tropej/fmw094. [DOI] [PubMed] [Google Scholar]
- 30.Fialho PMM, Correa CRS, Lescano SZ. Asthma and seroconversion from Toxocara spp infection: which comes first? Biomed Res Int. 2018;2018:1–6. doi: 10.1155/2018/4280792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schwartz R, Bidaisee S, Fields PJ, Macpherson MLA, Macpherson CNL. The epidemiology and control of Toxocara canis in puppies. Parasite Epidemiol Control. 2022;16:e00232. doi: 10.1016/j.parepi.2021.e00232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Roddie G, Holland C, Stafford P, Wolfe A. Contamination of fox hair with eggs of Toxocara canis. J Helminthol. 2008;82:293–296. doi: 10.1017/S0022149X08996954. [DOI] [PubMed] [Google Scholar]
- 33.Merigueti YFFB, Santarém VA, Ramires LM, da Silveira BA, da Costa Beserra LV, Nuci AL, et al. Protective and risk factors associated with the presence of Toxocara spp. eggs in dog hair. Vet Parasitol. 2017;244:39–43. doi: 10.1016/j.vetpar.2017.07.020. [DOI] [PubMed] [Google Scholar]
- 34.Otero D, Alho AM, Nijsse R, Roelfsema J, Overgaauw P, de Carvalho M. Environmental contamination with Toxocara spp. eggs in public parks and playground sandpits of Greater Lisbon Portugal. J Infect Public Health. 2018;11:94–98. doi: 10.1016/j.jiph.2017.05.002. [DOI] [PubMed] [Google Scholar]
- 35.Rosa Xavier IG, Ramos BC, Santarém VA. Recovery threshold of Toxocara canis eggs from soil. Vet Parasitol. 2010;167:77–80. doi: 10.1016/j.vetpar.2009.09.052. [DOI] [PubMed] [Google Scholar]
- 36.Janssens ACJW, Martens FK. Reflection on modern methods: revisiting the area under the ROC Curve. Int J Epidemiol. 2020;49:1397–1403. doi: 10.1093/ije/dyz274. [DOI] [PubMed] [Google Scholar]
- 37.The R Project for Statistical Computing. https://www.r-project.org/. Accessed 10 Feb 2023.
- 38.Robin X, Turck N, Hainard A, Tiberti N, Lisacek F, Sanchez J-C, et al. pROC: an open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinformatics. 2011;12:77. doi: 10.1186/1471-2105-12-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nahm FS. Receiver operating characteristic curve: overview and practical use for clinicians. Korean J Anesthesiol. 2022;75:25–36. doi: 10.4097/kja.21209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lötsch F, Obermüller M, Mischlinger J, Mombo-Ngoma G, Groger M, Adegnika AA, et al. Seroprevalence of Toxocara spp. in a rural population in Central African Gabon. Parasitol Int. 2016;65:632–634. doi: 10.1016/j.parint.2016.09.001. [DOI] [PubMed] [Google Scholar]
- 41.Na-Ek P, Narkkul U, Phasuk N, Punsawad C. Seroprevalence of anti-Toxocara canis antibodies and associated risk factors among dog owners in the rural community of Nakhon Si Thammarat province, southern Thailand. Trop Med Health. 2022;50:32. doi: 10.1186/s41182-022-00425-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fernandes J, Coelho TA, de Oliveira RC, Guedes LSAL, Teixeira BR, Guterres A, et al. Seroprevalence of rodent-borne viruses in Afro-descendent communities in Brazil. Rev Inst Med Trop Sao Paulo. 2019;61:e66. doi: 10.1590/S1678-9946201961066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Quaresma FRP, da Silva ME, Barasuol AM, Pontes-Silva A, Fonseca FLA, Adami F. Quality of primary health care for quilombolas’ Afro-descendant in Brazil: a cross-sectional study. Rev Assoc Med Bras. 2022;68:482–489. doi: 10.1590/1806-9282.20210994. [DOI] [PubMed] [Google Scholar]
- 44.Santos ENA, Magalhães PKA, Santos AM, Correia MS, Santos JCS, CarvalhoNeto APM, et al. Quality of life of women from a quilombola community in northeastern Brazil. Braz J Biol. 2022;84:e246463. doi: 10.1590/1519-6984.246463. [DOI] [PubMed] [Google Scholar]
- 45.Sardinha AHL, Aragão FBA, Silva CM, Rodrigues ZMR, Reis AD, van Varga ID. Quality of life of elderly quilombolas in the Brazilian northeast. Rev Bras Geriatr e Gerontol. 2019;22:190011. [Google Scholar]
- 46.Gubert MB, Segall-Corrêa AM, Spaniol AM, Pedroso J, Coelho SEDAC, Pérez-Escamilla R. Household food insecurity in black-slaves descendant communities in Brazil: Has the legacy of slavery truly ended? Public Health Nutr. 2017;20:1513–22. doi: 10.1017/S1368980016003414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Liu EW, Chastain HM, Shin SH, Wiegand RE, Kruszon-Moran D, Handali S, et al. Seroprevalence of antibodies to Toxocara species in the United States and associated risk factors, 2011–2014. Clin Infect Dis. 2018;66:206–212. doi: 10.1093/cid/cix784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rubinsky-Elefant G, da Silva-Nunes M, Malafronte RS, Muniz PT, Ferreira MU. Human toxocariasis in rural Brazilian Amazonia: seroprevalence, risk factors, and spatial distribution. Am J Trop Med Hyg. 2008;79:93–98. [PubMed] [Google Scholar]
- 49.Cook J, Hardie R, Bailey K, Tapper M, Vickers I, Calder D, et al. Seroprevalence of human toxocariasis. Jamaica Trop Biomed. 2016;33:88–94. [PubMed] [Google Scholar]
- 50.Thorkildsen K. Social-ecological changes in a Quilombola community in the Atlantic forest of southeastern Brazil. Hum Ecol Interdiscip J. 2014;42:913–927. doi: 10.1007/s10745-014-9691-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Berrett AN, Erickson LD, Gale SD, Stone A, Brown BL, Hedges DW. Toxocara seroprevalence and associated risk factors in the United States. Am J Trop Med Hyg. 2017;97:1846–1850. doi: 10.4269/ajtmh.17-0542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Farmer A, Beltran T, Choi YS. Prevalence of Toxocara species infection in the US: results from the National Health and nutrition examination survey, 2011–2014. PLoS Negl Trop Dis. 2017;11:e0005818. doi: 10.1371/journal.pntd.0005818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Santarém VA, do Couto AC, Lescano SZ, Roldán WH, Delai RR, Giuffrida R, et al. Serosurvey of anti-Toxocara canis antibodies in people experiencing homelessness and shelter workers from São Paulo Brazil. Parasit Vectors. 2022;15:1–9. doi: 10.1186/s13071-022-05499-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Adeel AA. Seroepidemiology of human toxocariasis in North Africa. Adv Parasitol. 2020;109:501–534. doi: 10.1016/bs.apar.2020.01.023. [DOI] [PubMed] [Google Scholar]
- 55.Abuseir S. A systematic review of frequency and geographic distribution of water-borne parasites in the Middle East and North Africa. East Mediterr Health J. 2023;29:151–161. doi: 10.26719/emhj.23.016. [DOI] [PubMed] [Google Scholar]
- 56.Merigueti Y, Giuffrida R, Silva R, Kmetiuk L, Santos A, Biondo A, et al. Dog and cat contact as risk factor for human toxocariasis: systematic review and meta-analysis. Front Public Heal. 2022;10:854468. doi: 10.3389/fpubh.2022.854468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mendoza Roldan JA, Otranto D. Zoonotic parasites associated with predation by dogs and cats. Parasit Vectors. 2023;16:1–14. doi: 10.1186/s13071-023-05670-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kong L, Peng H-J. Current epidemic situation of human toxocariasis in China. Adv Parasitol. 2020;109:433–448. doi: 10.1016/bs.apar.2020.01.016. [DOI] [PubMed] [Google Scholar]
- 59.Song HB, Lee D, Jin Y, Kang J, Cho S-H, Park MS, et al. Prevalence of toxocariasis and its risk factors in patients with eosinophilia in Korea. Korean J Parasitol. 2020;58:413–419. doi: 10.3347/kjp.2020.58.4.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Won EJ, Kim J, Shin M-G, Shin JH, Suh SP, Ryang DW. Seroepidemiology of toxocariasis and its clinical implications in Gwangju and Jeonnam-province. Korea Ann Lab Med. 2015;35:449–453. doi: 10.3343/alm.2015.35.4.449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Chou C-M, Fan C-K. Seroprevalence of Toxocara spp. infection in southeast Asia and Taiwan. Adv Parasitol. 2020;109:449–63. doi: 10.1016/bs.apar.2020.01.020. [DOI] [PubMed] [Google Scholar]
- 62.Fialho PMM, Correa CRS, Lescano SZ. Seroprevalence Brazil. Adv Parasitol. 2020;109:357–374. doi: 10.1016/bs.apar.2020.01.013. [DOI] [PubMed] [Google Scholar]
- 63.de Azevedo P, Lescano SZ, Giuffrida R, Kmetiuk LB, Dos Santos AP, Dangoudoubiyam S, et al. Serosurvey of anti-Toxocara antibodies and risk factors in adolescent and adult pregnant women of southeastern Brazil. PLoS Negl Trop Dis. 2021;15:1–13. doi: 10.1371/journal.pntd.0009571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Panazzolo GK, Kmetiuk LB, Domingues OJ, Farinhas JH, Doline FR, de França DA, et al. One Health approach in serosurvey of Toxoplasma gondii in former black slave (Quilombola) communities in southern Brazil and among their dogs. Trop Med Infect Dis. 2023;8:377. doi: 10.3390/tropicalmed8070377. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Figure S1. Receiver-operating characteristic (ROC) curve [evaluating the accuracy of the multivariate logistic regression model (AUC = 0.823, 95% CI = 0.739–0.907)] to predict seropositivity for anti-Toxocara spp. antibodies in individuals of quilombola communities of Paraná State, southern Brazil
Additional file 2: Raw data of associated risk factors of toxocariasis in quilombola communities of southern Brazil..
Data Availability Statement
All data generated or analysed during this study are included in this published article and its Additional file information.