Abstract
Childhood emotional abuse (CEA) and childhood emotional neglect (CEN) are the least well-studied forms of childhood maltreatment due to challenges in their definition and in detection. However, the available evidence suggests associations with multiple adulthood mental health problems in clinical and non-clinical populations. This systematic review and meta-analysis (PROSPERO registration number CRD42020197833) explored the associations between CEA and CEN and a range of adulthood mental health problems based on systematic searches of eight databases. In total, 79 English and 11 Chinese studies met our inclusion criteria. Results suggested that CEA and CEN had positive associations with various adulthood mental health problems (d = 0.02–1.84), including depression, anxiety, substance abuse, suicidal ideation or attempts, personality disorders, eating disorders, and other psychological symptoms in the general population and across different geographic regions. Furthermore, findings suggested that compared with the non-clinical population, individuals in clinical populations were more likely to have experienced emotional abuse and neglect during childhood. The review highlights the need for more research on emotional abuse and emotional neglect. Furthermore, future research should include more populations from non-western countries and non-college populations. They further underline the importance of addressing issues related to CEA/CEN experiences in the prevention and treatment of mental health issues in adulthood.
Keywords: childhood psychological maltreatment, childhood emotional abuse, childhood emotional neglect, depression, anxiety, substance abuse, suicidal ideation, meta-analysis
Introduction
It is well established that different forms of childhood abuse are significantly associated with mental health problems and emotional, cognitive, behavioral, and social outcomes in childhood (Maguire et al., 2015) and that these difficulties frequently continue into adulthood (Hughes et al., 2017). A recent umbrella review, for example, suggested that the negative impacts of child sexual abuse included self-injury, somatization, schizophrenia, depression, anxiety, and psychosis (Hailes et al., 2019). Another systematic review suggested that long-term consequences of child physical abuse included substance abuse, suicidality, eating disorders, depression, and anxiety (Norman et al., 2012). Moody et al. (2018) reviewed the rates of childhood maltreatment worldwide in females and males based on self-reported measurements. They found that the prevalence of physical abuse ranges from 5.0% to 40.2%; sexual abuse ranges from 2.5% to 29.8%; emotional abuse ranges from 6.5% to 53.8%, and neglect (both physical and emotional) ranges from 1.6% to 67.3%. The large variation in the estimate of self-reported childhood maltreatment likely reflects the fact that the review covered different regions such as Africa, Asia, Australia, Europe, and South and North America, combined with possible recall and self-report biases (Moody et al., 2018). The reason of large variation may be because different regions have different definitions and boundaries regarding childhood maltreatment, as well as true differences in their prevalence rates. Given the prevalence and evidence for the negative outcomes of childhood maltreatment, there is a strong need for studies that can illuminate the full range and severity of its impacts. However, not all forms of childhood maltreatment have received equal attention in research. In particular, research exploring psychological maltreatment lags behind that of other forms of maltreatment. Psychological maltreatment can be sub-divided into emotional abuse (sometimes termed “psychological abuse”) and emotional neglect (sometimes termed “psychological neglect”) (McGee & Wolfe, 1991).
The term “emotional abuse” refers to the commission of hostile acts by the caregivers toward the child (McGee & Wolfe, 1991) (for example behaviors, see Table 1). While it often occurs alongside other forms of abuse, it can also be inflicted on its own (Baker & Festinger, 2011). Previous literature has suggested negative impacts of childhood emotional abuse (CEA) on adult mental health. For instance, in one study, CEA was significantly associated with major depression, anxiety disorder, and substance abuse disorder in a nationally representative adult sample from the United States (MAge = 48.1 years) (Taillieu et al., 2016).
Table 1.
Example Behaviors of CEA and CEN.
| Childhood Psychological Abuse | Childhood Psychological Neglect |
|---|---|
| ● Belittling, denigrating, or other rejection | ● Failing to provide necessary care for children |
| ● Singling out or humiliating in public | ● Providing little or no warmth, nurturing, praise during any developmental period in childhood |
| ● Intentionally trying to scare, humiliate, ignore, or isolate a child | ● Being detached or uninvolved; interact only when necessary |
| ● Confining within environment | ● Refusing to provide serious emotional health |
| ● Having rigid/unrealistic expectations accompanied by threats if not meet | |
| ● Restricting social interaction in community |
Source. Adapted from Hibbard et al. (2012) and Dubowitz (2013).
Note. CEA = childhood emotional abuse; CEN = childhood emotional neglect.
“Emotional neglect” refers to a caregiver’s acts of omission in failing to provide necessary care for children, which may include meeting their basic needs (Dubowitz, 2013) (for example behaviors see Table 1). Unlike CEA, childhood emotional neglect (CEN) may be unintentional, and caregivers are sometimes unaware that they are emotionally neglecting their child (Iwaniec, 2006). Research by Salokangas et al. (2019) suggested that CEA was significantly associated with depression, anxiety, and substance abuse. Finally, CEA and CEN may occur in different forms, which may be verbal or non-verbal, with intention or without intention, and active or passive.
Taken together, psychological maltreatment refers to a repeated pattern of caregivers’ behaviors that are likely to be interpreted by a child as being unwanted or unloved, and that undermine the child’s healthy development and socialization (Glaser, 2002). Psychological maltreatment describes a relationship between the parents and child rather than an event or series of repeated events occurring within the parent–child relationship. In this type of relationship the parent–child interactions are actually or potentially harmful by causing impairments in the child’s psychological/emotional health and development. Furthermore, psychological maltreatment may lead to impairment both by omission of care and commission of harm, and without physical contact (Glaser, 2002).
In line with research on other forms of maltreatment, psychological maltreatment has been shown to negatively affect children’s social, cognitive, emotional, and/or physical development (Hibbard et al., 2012), with difficulties continuing into adulthood (Hughes et al., 2017; Grummit et al., 2021). Indeed, previous evidence suggests that the negative impacts of psychological maltreatment during childhood may manifest in numerous ways, such as impaired emotional, cognitive, or social development, and lead to mental health outcomes such as depression (Christ et al., 2019), suicide attempts (Falgares et al., 2018), emotional dysregulation (Burns et al., 2010), or personality disorder (PD; Goodman et al., 2014) in the general population. Moreover, several studies have suggested links between childhood psychological maltreatment and mental health problems in clinical populations (Xie et al., 2018), for instance, those with eating disorders (Kent et al., 1999), alcohol dependency (Evren et al., 2011), or depressive disorders (Neumann, 2017). Besides this, mental health problems resulting from childhood psychological maltreatment can have multiple secondary effects in terms of social impairment (Armijo, 2017), lost productivity (Doran & Kinchin, 2019), and increased treatment/support needs (Dixon et al., 2016). However, no previous research has provided a systematic overview of associations between childhood psychological maltreatment and adult mental health.
There have been numerous systematic reviews and meta-analyses on the associations between childhood abuse and negative consequences, but none have focused exclusively on psychological maltreatment and adult mental health. For instance, Norman et al. (2012) found that CEA and CEN in the general population were associated with depression, drug use, suicide attempts, sexually transmitted infection, and risky sexual behaviors. Maguire et al. (2015) demonstrated the social, emotional, and behavioral features in children who experienced CEN or CEA. The results showed that these children were more likely to exhibit poor academic achievement, were more prone to suicidality and low self-esteem, and were less likely to develop friendships. Gardner et al. (2019) demonstrated that child abuse (i.e., sexual, physical, and emotional abuse and neglect) was associated with depressive disorder. Green et al. (2019) found that individuals with psychotic illness who experienced child abuse (i.e., sexual, sexual, physical, and emotional abuse and neglect) were at approximately twice the risk of perpetrating violence than individuals who did not experience child abuse. Angelakis et al. (2020a) found that core types of childhood abuse (physical, sexual, and emotional abuse and neglect) are associated with a higher rate of suicidal behaviors in young people. In addition, Angelakis et al. (2020b) also explored the association between childhood abuse and suicide attempt in prisoners. They found that childhood abuse (i.e., sexual, physical, and emotional abuse and physical and emotional neglect) was strongly associated with suicide attempts in this population.
As such, numerous reviews have explored the associations between different forms of child abuse and mental health in children, young adults, general populations, and the prisoner population. However, those reviews are limited with respect to identifying the effects of psychological maltreatment. For instance, Maguire et al. (2015) looked at neglect as a whole instead of only focusing on emotional neglect. Norman et al. (2012) examined the effects of CEA but only focused on a limited set of psychosocial outcomes. Furthermore, given the rate at which research is published in this area, an updated review of the links between CEA and mental health outcomes capturing research published in the decade since the searches of the Norman et al. (2012) systematic review is merited. Moreover, some existing literature has proposed that psychological maltreatment has a greater deleterious effect on mental health outcomes than physical abuse. For instance, Claussen and Crittenden (1991) found that psychological maltreatment was a stronger predicter of subsequence impairment than physical abuse. Theses findings highlight the needs for a systematic review of the literature that examine the links between psychological maltreatment and adult mental health.
To the best of the authors’ knowledge, to date, no research has been carried out with a specific focus on synthesizing current evidence on the relations between childhood psychological maltreatment by caregivers (i.e., parents or another caregiving adult living in the same household) and adult mental health. According to the Flatley (2016), the perpetrators of psychological maltreatment are most likely to be the primary female caregivers (40%) (i.e., biological/step/adoptive father) and the primary male caregivers (35%) (i.e., biological/step/adoptive mother). Indeed, in the nuclear family model, parents are among the caregivers who spend most of the time with their children and are the primary disciplinarians. They tend to be the most common perpetrators of most types of child maltreatment (Devries et al., 2018). Therefore, a systematic review and meta-analysis of associations are needed to clarify how psychological maltreatment perpetrated by an adult living in the same household during childhood is associated with different mental health outcomes in adulthood.
The goal of the current study was to address this gap and provide an improved understanding of the consistency and strength of the link between childhood psychological maltreatment and a range of adult mental health outcomes at both the clinical and sub-clinical levels. The current systematic review and meta-analyses can provide more precise estimates of the associations with various mental health outcomes than have been provided by any primary study to date. This is important because it provides a clearer picture of which mental health issues are potentially most affected by psychological maltreatment, informing prevention and intervention that is more tailored to the anticipated psychological impacts of psychological maltreatment. It also allows us to examine the factors that moderate the magnitude of these associations and to evaluate whether the field is affected by publication bias. By including studies both published in English and Chinese, we can also start exploring the question of any potential differences in the links between childhood maltreatment and mental health outcomes across country and cultural contexts. Previous research has suggested that there are potential cultural differences between Western contexts and China in accepted and expected parenting behaviors (Xiao et al., 2022) and this may have implications for the associations between psychological maltreatment and mental health outcomes. In addition, previous reviews on any maltreatment have only included English-speaking studies which could have some limits. Hence, we here undertake a systematic review and meta-analyses of the relations between psychological maltreatment and a range of mental health outcomes in studies published in both Chinese and English. There are four primary review questions:
What are the long-term associations of childhood psychological maltreatment (CEA and CEN) on adult mental health.
What are the unique effects of childhood psychological maltreatment (CEA and CEN) by caregivers on adult mental health after adjusting for other forms of abuse and relevant confounders?
How do study-level moderators such as years of publication, study methodological quality, and study location affect these associations?
Are there differences in these associations between English language and Chinese language papers?
Method
This review is reported following the Preferred Reporting Items for Systematic Review and Meta-Analysis (Page et al., 2021). The protocol for this systematic review was registered in the International Prospective Register of Systematic Reviews (PROSPERO) with registration number CRD42020197833 and published in the journal Systematic Reviews (Xiao et al., 2021).
Search Strategy
The selection of search terms was based on the keywords used in the previous literature examining the impact of childhood psychological maltreatment on adult mental health problems. Table 2 provides an overview of the search terms. The Boolean operators “OR” and “AND” were used to combine terms with specific syntax adapted for individual databases (an example is provided in Supplemental Material 1). As well as linking mental health and maltreatment terms together, the maltreatment terms were combined with child* and the mental health terms with adult* to link the concepts to the relevant developmental stages. We searched the Web of Science, Medline, PubMed, PsycINFO, Applied Social Science Index and Abstract, ERIC and EMBASE databases, and ZhiWang for literature written in Chinese. The exclusion of studies other than those published in English may have potential biases because they do not represent all of the evidence (Morrison et al., 2012). Therefore, studies written in both English and Chinese will be reviewed, reflecting the language capabilities of the team.
Table 2.
Overview of Search Terms.
| CEA and CEN | Adult Mental Health |
|---|---|
| Child abuse | Mental health |
| Childhood psychological maltreatment | Generalized anxiety disorder |
| CEA | Depression |
| CEN | Major depression disorder |
| Psychological aggression | PTSD |
| Psychological violence | PD |
| Psychological domestic violence | Eating disorder |
| Childhood psychological victimization | Bipolar disorder |
| Schizophrenia | |
| Panic disorder | |
| Psychosis | |
| Social anxiety disorder | |
| Suicide attempt | |
| Suicidal ideation | |
| Non-suicidal self-injury | |
| Substance abuse |
Note. CEA = childhood emotional abuse; CEN = childhood emotional neglect; PD = personality disorder; PTSD = post-traumatic stress disorder.
Eligibility Criteria
We only included studies that met the following criteria: (a) participants aged over 18 at the assessment of the mental health problem, (b) studies that measured CEA and/or CEN before age 18 using prospective longitudinal and retrospective methods, using self-or-other-reported questionnaires, interviews, or police or social work records, (c) studies that measured mental health problems (standard diagnoses as listed in Diagnostic and Statistical Manual of Mental Disorders, Fifth Edintion (DSM-V) or International Classification of Disesases 10th Revision (ICD-10) or using mental health scores based on validated measures) using self-or-other-reported questionnaires or clinical interviews, (d) studies that only assessed childhood psychological maltreatment, CEA and/or CEN or studies that assessed both CEA and CEN and other types of abuse (e.g., physical or sexual), (e) studies where the perpetrators were the primary caregivers or an adult living in the same household, and (f) studies published in English or Chinese language.
We excluded the following types of studies: (1) any book chapters, case studies, letters, opinions, and editorials that did not present new data, (b) qualitative investigations, (c) review papers (e.g., narrative reviews, systematic reviews, or meta-analysis), (d) studies that did not provide an analysis of CEA/CEN linked to different mental health outcomes separately, (e) studies that focus on non-parental others (e.g., in institutional care) or where data from primary caregivers or adults in the household could not be disaggregated from the data on abuse perpetrated by others, (f) studies where different types of abuse were combined and not separately reported so that it was not possible to obtain an effect for CEA/CEN, and (g) studies where the outcomes were physical rather than mental conditions.
Study Selection
First, the titles and abstracts were assessed, followed by full-text screening conducted on those that met inclusion criteria. All articles identified in the searches were screened by two reviewers, co-authors of this paper. Reviewer one (ZX) and reviewer two (MMB) screened the English language articles, while reviewer one and reviewer three (WSC) screened the Chinese articles. All reviewers hold at least masters-level degrees in Psychology and have specialist knowledge of mental health. In addition, reviewers one and three have specialist knowledge of the topic of abuse. Disagreements between the reviewers were resolved by a fourth reviewer (ALM) who holds a doctorate in Psychology and has specialist knowledge of the topics of abuse and mental health. The reviewers then independently conducted data extraction and studies’ methodological quality assessment. It was possible to arrive at consensus for all studies, with 10 English language studies and 8 Chinese language studies first requiring discussion between reviewers.
Data Extraction
Data from each selected study were extracted and recorded in the form presented in Supplemental Materials. The form has fields “Population Data” that include information regarding (1) authors’ names, (2) publication year, (3) sample size, (4) location, (5) sample population, (6) sample population demographics, and (7) setting. “Study Data” includes information regarding (1) study methodology, (2) types of abuse assessed, (3) measurement of CEA/CEN, (4) measurement of mental health outcomes, (5) perpetrator of maltreatment, and (6) age at exposure to maltreatment. “Result” includes information regarding (1) study findings, (2) odds ratio or adjusted odds ratio (aOR) if available, and (3) other statistical information as relevant.
Assessment of Methodological Quality
Classification of risk of bias was based on the Newcastle–Ottawa Quality Assessment Scale (see Supplemental Materials 10, 11, and 12) was used to assess both case–control studies (e.g., non-longitudinal studies) and cohort studies (e.g., longitudinal studies) (Wells et al., 2014). Three main domains with eight sub-domains were included in this assessment: selection (adequateness of case definition, representativeness of the cases, and selection of controls and definition of controls), comparability (comparability of cases and controls based on the design or analysis), and exposure (ascertainment of exposure, same method of ascertainment for cases and control, and non-response rate). Each study was awarded stars (i.e., if the study met the criteria for sub-domains, a star would be awarded.) from zero to eight based on these criteria, with more stars representing a lower risk of bias.
Data Synthesis and Analysis
We used a narrative synthesis to analyze the main characteristics of each study (i.e., study location, sample size and characteristic, abuse types, abuse measurement, mental health measurement, perpetrators, and study effect size). Studies were organized based on mental health outcomes and population types (i.e., PD, eating disorder, psychological symptoms, suicidal ideation, depression and anxiety, substance abuse and clinical population studies).
Due to the restricted number of the reported effect sizes in other areas, only the effects related to three mental health problems/populations (i.e., suicidal ideation, depression and anxiety, and clinical population) were meta-analyzed. A random-effects model was used as it was assumed that effect sizes were sampled from a heterogeneous population, that is, studies were expected to represent fairly substantial differences in method (i.e., types of participants, measurements) and were thus not anticipated to reflect a single underlying effect size. The “metafor” package for R statistical software was used to carry out the meta-analyses (Viechtbauer, 2010). Due to different statistical information provided in the included papers, we extracted all “r” statistics and converted them into Cohen’s d. If a paper did not provide “r,” we extracted the odds ratio and converted it to “r” in an additional step.
Study heterogeneity was assessed qualitatively by examining the characteristics of the studies. Statistical heterogeneity was assessed by calculating I2. Publication bias was explored using a funnel plot (Higgins & Green, 2011). A trim and fill method (Duval, 2005) was used to statistically test for its potential impacts. A moderator analysis assessed study-level moderators such as year of publication, quality of the study, and location of the study.
Overview of Studies
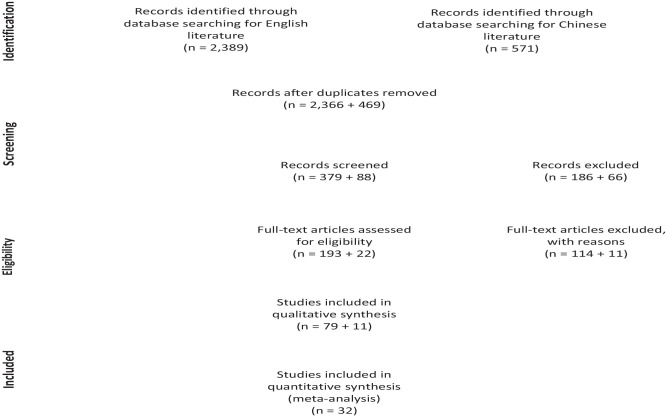
Based on the English literature search, 2,389 studies were found. Of these, 23 were duplicates, leaving 2,366 studies (see Figure 1). Screening by title left 379 and after screening the abstract, 193 studies remained eligible for full-text screening. In the full-text screening, phase studies were excluded because (1) mental health outcomes were assessed before the age of 18 (n = 48); (2) psychological maltreatment was not analyzed separately (n = 47); (3) abuse was not perpetrated by primary caregivers (n = 4); and (4) there was no mental health outcome variable (n = 15). In total, 79 studies were included in the systematic review.
Figure 1.
Flow chart of the systematic review based on PRISMA guidelines.
Note. PRISMA = Preferred Reporting Items for Systematic Review and Meta-Analysis.
Based on the Chinese literature search, 571 studies were found. Of these, 102 were duplicates, leaving 469 (see Figure 1). After screening by title, 88 studies remained, and 11 studies were eligible for the full-text screening after abstract screening. Studies were excluded in the full-text screening phase because (1) mental health outcomes were assessed before the age of 18 (n = 5); (2) CEA and CEN were not measured (n = 2); and (3) mental health outcome variables were not assessed (n = 4). In total, 11 Chinese studies were included in the systematic review.
For the English language studies (n = 79; 38 studies measured both CEA and CEN, 30 studies measured CEA and 1 study measured CEN only), Supplemental Material 2 shows the main characteristics of all the included studies organized by theme. The 79 studies were published between 1997 and 2020. In all, 14 studies conducted longitudinal research or used secondary datasets; four studies (Afifi et al., 2012; Harford et al., 2014; Taillieu et al., 2016; Waxman et al., 2014) used the same secondary dataset for different outcomes. The rest of the studies (n = 65) used a case–control study design and were cross-sectional studies. The sample size of the studies ranged from 75 to 34,653. In studies based on non-clinical settings (n = 48), most were conducted in the general population (n = 21) or in college student populations (n = 11). In the clinical settings (n = 23), studies were conducted relating to various mental health problems in patient populations (i.e., depression, bipolar disorder, schizophrenia, mood disorder, substance abuse disorder). Of these, 13 studies compared non-clinical and clinical populations. Four studies included only females (Christ et al., 2019; Haferkamp et al., 2015; Kent et al., 1997; Thompson et al., 2000), and two studies only included male participants (Can et al., 2019; Evren et al., 2016). Most of the studies (n = 57) measured all abuse types (physical abuse, physical neglect, sexual abuse, emotional abuse and emotional neglect and most (n = 59) used the Childhood Trauma Questionnaire (CTQ) or CTQ-Short Form (CTQ-SF). These two questionnaires measure traumatic incidents including physical abuse, sexual abuse, EA, EN, and physical neglect. The included studies used various measures for mental health outcomes. These ranged from general mental health measurements (e.g., Centre for Epidemiological Studies Depression Scale [CES-DS]); to those that corresponded with the DSM-IV classification (e.g., Structured Clinical Interview for DSM-IV Axis I Disorder); few developed their own questions. The perpetrators of the CEA or CEN were mainly primary caregivers (n = 65); some (n = 13) were parents or adults living in the same household, while only one study examined multiple perpetrators (Kruger & Fletcher, 2017).
For the literature written in Chinese (n = 11), Supplemental Material 3 provides the main characteristics of the included studies. Meta-analysis was not possible due to the small number of studies in each outcome group. The 11 studies were published between 2001 and 2018. All the studies used a case–control study design. The sample size of the studies ranged from 110 to 1,502; however, most of the studies (n = 9) were of college students. The measures were well-established in the Chinese context with acceptable internal consistency (α > .70). All studies used measurements that assessed CEA and CEN (i.e., Child Psychological Abuse and Neglect Scale, Childhood Emotional Abuse Scale, Parent–Child Conflict Tactics Scales). The perpetrators of the maltreatment were all parents or caregivers. Measures for mental health outcomes covered various mental health problems, for instance, depression (i.e., Self-Rating Depression Scale, CES-DS), PD (i.e., Symptoms Checklist 90), and suicidal ideation (i.e., Positive and Negative Suicide Ideation).
Supplemental Materials 4, 5, and 6 and Supplemental Materials 7, 8, and 9 provide the available information on the extraction forms mentioned above for English and Chinese studies, respectively.
Results
CEA and CEN and Adult Mental Health Outcomes in the English Language Publications
CEA and CEN and adult PD
Across six studies (three in a clinical setting), CEA and CEN were risk factors for the development of PDs later in life, even when controlling for other types of abuse, basic demographic characteristics, parental psychopathology, and comorbid PDs. Specifically, Waxman et al. (2014) found that CEN predicted avoidant, paranoid, and schizoid PD and CEA predicted borderline, narcissistic, and schizotypal PD. Goodman et al. (2014) reported that both CEA and CEN were associated with borderline PD symptoms. A more recent study by Fung et al. (2020) also had similar results. Bernstein et al. (1998) explored the associations in substance abuse patients and found that CEA and CEN predicted personality pathology (all clusters). Cohen et al. (2013, 2014) studied nonpsychotic psychiatric patients and found CEA predicted Cluster C (DSM-5, 2013) (Obsessive-Compulsive, Passive-aggressive, and Self-Defeating) PD traits. The effect size (Cohen’s d) of these five studies for CEA ranged from 0.16 to 0.95; and for CEN, ranged from 0.16 to 0.59.
CEA and adult eating disorder
In one study (non-clinical setting), CEA was the only form of abuse that predicted unhealthy eating attitudes in adulthood when controlling for other types of abuse. Age of exposure to CEA did not moderate this association (Kent et al., 1997).
CEA and CEN and adult suicidal ideation/attempts and non-suicidal self-injury behaviors
Across 11 studies (all non-clinical settings), there were positive associations between CEA/CEN and suicidal ideation/attempts, even when adjusting for gender, age, race, or marital status (Harford et al., 2014). Gibb et al. (2001) conducted a 2.5-year follow-up study and found the associations between suicidal ideation and greater CEN in childhood remained significant. Briere et al. (2016) reported that CEA was associated with both recent suicide attempts and recent suicidal ideation without attempts. Similarly, Harford et al. (2014), Thompson et al. (2000), and Saracli et al. (2016) reported the associations between CEN and suicidal ideation and attempts, with CEN was significantly related to suicidality. However, only one study (Smith et al., 2018) reported a non-significant link between CEA and suicidality. Besides suicidal ideation or attempts, Buser and Hackney (2012) found CEA to be significantly related to non-suicidal self-injury behaviors. The effect sizes (Cohen’s d) in these 11 studies for CEA ranged from 0.11 to 1.28 and for CEN ranged from 0.30 to 1.28.
CEA and CEN and adult substance abuse
Across nine studies (one clinical setting) individuals who experienced CEA were more likely than individuals who did not experience CEA to engage in different kinds of substance abuse, for instance, alcohol (Crouch et al., 2018; Elliott et al., 2014; Mandavia et al., 2016; Yuan et al., 2014), cannabis (Aas et al., 2014), heroin (Afifi et al., 2012), or nicotine (Elliott et al., 2014) abuse. Even when adjusting for demographic factors (age group, race/ethnicity, educational attainment, income, and rurality), most studies still found significant associations. Aas et al. (2014) found that cannabis abuse was significantly associated with CEA in bipolar disorder. However, Yuan et al. (2014) only found associations in females but not in males. Contrary to the above, one study (Florez et al., 2020) found that CEA was not directly associated with alcohol misuse. Only two studies (Afifi et al., 2012; Elliott et al., 2014) explored the associations between CEN and substance abuse and reported significant findings. The effect size (Cohen’s d) of these nine studies for CEA ranged from 0.30 to 0.85 and for CEN ranged from 0.15 to 0.66.
CEA and CEN and adult depression and anxiety
Across 14 studies (all non-clinical settings), there were significant associations between CEA or CEN and adult depression and anxiety. Some studies explored the relations between CEN and adult depression and anxiety and found these associations were positive and significant (Balsam et al., 2010; Brown et al., 2016; Crow et al., 2014; Gong & Chan, 2018; Novelo et al., 2018; Sunley et al., 2020; Wright et al., 2009). Many of the included studies examined mediators such as behavioral activation (O’Mahen et al., 2015), self-compassion and gratitude (Wu et al., 2018), or moderators such as emotional dysregulation (Crow et al., 2014). The effect size (Cohen’s d) of these 14 studies for CEA ranged from 0.56 to 1.40; for CEN ranged from .01 to 0.70.
CEA and CEN and other psychological symptoms
Across seven studies (all non-clinical settings), there were positive relations between CEA and CEN and other mental health issues defined and measured with different levels of specificity. The included studies assessed various mental health issues, for instance, auditory and visual hallucination (Abajobir et al., 2017), internalizing problems (van Duin et al., 2019), and general psychological symptoms (Dias et al., 2015; Fung et al., 2020; Laoide, 2018; Sheikh et al., 2016; Taillieu et al., 2016). Taillieu et al. (2016) found that experiencing CEA and CEN increased the likelihood of mental health problems—CEN was associated with increased odds (aOR = 1.3) of depression, dysthymia, and social phobia, while CEA was associated with increased odds (aOR = 1.6) for lifetime diagnosis for borderline PD. Fung et al. (2020) found when controlling for other types of abuse, individuals who experienced both emotional abuse and emotional neglect scored the highest for mental health problems (e.g., depression, anxiety, borderline PD, post-traumatic stress disorder [PTSD], and somatoform dissociation), while individuals who experienced only emotional abuse or emotional neglect scored higher than individuals who had not experienced abuse. The effect size (Cohen’s d) of these seven studies for CEA ranged from .032 to 0.554 and for CEN ranged from 0.101 to 0.787.
CEA and CEN reported in clinical populations
Participants in a total of 32 retrospective studies based on adult clinical populations from a range of countries (e.g., USA, UK, China, Turkey, France, Italy, Germany, Brazil, Istanbul, Korea, Norway, Poland, Iran, South Africa, Geneva, New Zealand) reported having experienced more CEA and CEN during their childhood compared to non-clinical populations. Except for the Bruni et al. (2018) study, which only measured CEA, all other studies measured both CEA and CEN. All mental health problems were diagnosed based on the DSM-IV or ICD-10 classification. Mental health problems included eating disorders (Amianto et al., 2018), PTSD (Evren et al., 2010, 2016; Haferkamp et al., 2015), major depression disorder (de Mattos Souza et al., 2016), bipolar disorder (Janiri et al., 2015; Etain et al., 2010; Fowke et al., 2012; Hariri et al., 2015; Kefeli et al., 2018; Ostefjells et al., 2017; Pavlova et al., 2016; Russo et al., 2014; Watson et al., 2014), alcohol use disorder (Can et al., 2019; Potthast et al., 2014), depression (Arnow et al., 2011; Huh et al., 2017; Kounou et al., 2013; Neumann, 2017; Schulz et al., 2017), PD (Zhang et al., 2013), mood disorder (Ventimiglia et al., 2020), schizophrenia (Bruni et al., 2018), substance abuse (Khosravani et al., 2019; Mirhashem et al., 2017; Price et al., 2017), and other psychological symptoms (Kruger & Fletcher, 2017; Sar et al., 2009; Xie et al., 2018). None of the studies explored gender differences, except Russo et al. (2014), who found no gender differences in childhood CEA in bipolar disorder patients. Amianto et al. (2018) found that patients with eating disorders experienced more CEA and CEN than the healthy control group. Can et al. (2019) and Potthast et al. (2014) found that CEA scores were higher in alcohol use disorder patients. Haferkamp et al. (2015) suggested that women who had PTSD scored higher in CEA when controlling for other types of abuse. These findings suggested that clinical populations have a higher prevalence of CEA and CEN than non-clinical populations. The effect size (Cohen’s d) of these 32 studies for CEA ranged from .02 to 1.84; for CEN, they ranged from .08 to 0.73.
CEA and CEN and adult mental health outcomes in the Chinese Language Publications
Across 11 studies (one clinical setting), CEA, CEN, or psychological maltreatment was associated with various mental health outcomes in the Chinese population, mainly undergraduates. Only one study (Zhang et al., 2018) explored the differences between obsessive-compulsive disorder (OCD) patients and the general population and suggested that people with an OCD diagnosis were more likely to report having experienced psychological abuse during childhood. The retrospective studies drawing their samples from community settings showed significant correlations between childhood psychological maltreatment and self-injury behaviors (Dai et al., 2016; Zhang et al., 2017), suicidal ideation (Yang et al., 2019), aggression (Han et al., 2018), depression and anxiety (Chang & Wang, 2008; Deng et al., 2018; Guo, 2018; Wang & Liu, 2017; Zeng, 2016), and general mental health (Xie et al., 2008). Apart from these associations, some studies also explored the moderators and mediators of these links. For instance, Deng et al. (2018) found resilience played an important mediating role between college students’ depression and childhood CEA; those students who experienced CEA and had higher resilience skills could reduce the chance of suffering depression symptoms. Wang and Liu (2017) suggested that cognitive flexibility played a mediating role in adult depression and CEA. Yang et al. (2019) found that rumination was a significant mediator between adult suicidal ideation and CEA. One study (Xie et al., 2008) examined gender differences in the occurrence rate of CEA and found that males had higher occurrence rates on both CEA and CEN than females.
Meta-analyses
A random-effect model (restricted maximum-likelihood estimator) was used to carry out each meta-analysis.
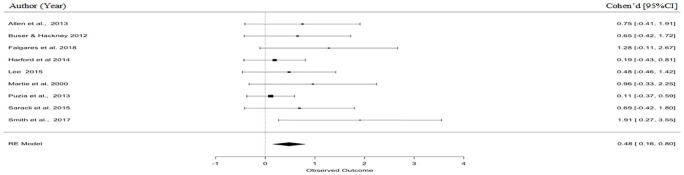
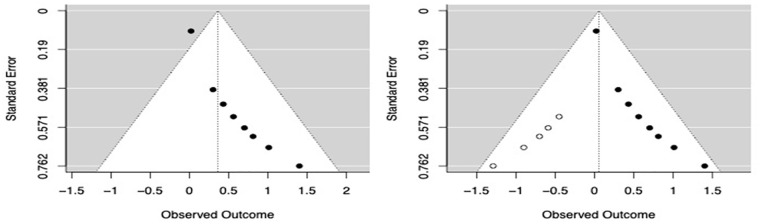
Suicidal ideation/attempts
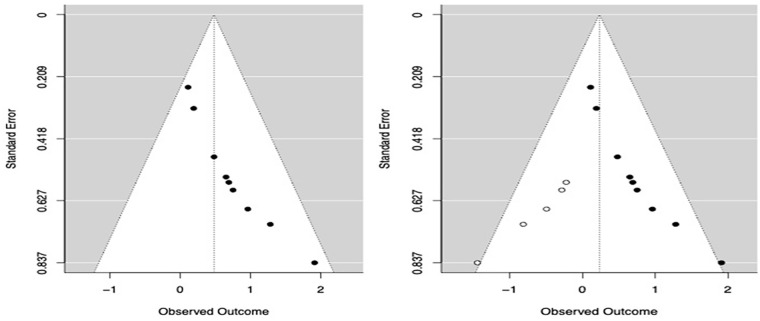
Based on nine studies (included studies are present in Table 3) that examined suicidal ideation/attempts as an adult outcome of CEA. The pooled estimate for the associations between CEA and adult suicidal ideation was 0.479 (95% confidence interval [CI: 0.156, 0.803], p < .001, τ2 = .030, H2 = 1.14) suggesting a medium effect size (Figure 2). The heterogeneity test suggested that the variance between the included studies was not significant (Q (8) = 8.186, p = .416, I2 = 11.94%). Using the trim and fill method (Duval, 2005) to test potential publication bias, it was estimated that five studies were potentially missing (standard error [SE] = 1.796). After adjustment for potential publication bias, the pooled estimated were 0.233 (95% CI [−.025, 0.490], p = .077). The test for heterogeneity suggested Q (13) = 18.844, p = .128, I2 = 0, suggesting that the effect size was smaller after adjustment. Funnel plots are provided in Figure 3.
Table 3.
Pooled Effect Size from Random-Effects Meta-Analyses.
| Author (year) | Location | N | r | Effect Size [95% CI] |
|---|---|---|---|---|
| Suicide ideation | ||||
| Allen et al. (2013) | N/A | 260 | .35 | 0.75 [−0.41 to 1.91] |
| Buser and Hackney (2012) | USA | 390 | .30 | 0.65 [−0.42 to 1.72] |
| Falgares et al. (2018) | Italy | 293 | .54 | 1.28 [−0.11 to 2.67] |
| Harford et al. (2014) | USA | 34,653 | .10 | 0.19 [−0.43 to 0.81] |
| Lee (2015) | Korea | 1,396 | .23 | 0.48 [−0.46 to 1.42] |
| Thompson et al. (2000) | USA | 335 | .43 | 0.96 [−0.33 to 2.25] |
| Puzia et al. (2014) | USA | 189 | .06 | 0.11 [−0.37 to 0.59] |
| Saracli et al. (2016) | Turkey | 897 | .32 | 0.69 [−0.42 to 1.80] |
| Smith et al. (2018) | USA | 91 | .69 | 1.91 [0.27 to 3.55] |
| Suicide ideation total | 0.48 [0.16 to 0.80] | |||
| Depression and anxiety | ||||
| Balsam et al. (2010) | USA | 669 | .58 | 1.40 [−0.09 to 2.89] |
| Christ et al. (2019) | Netherland | 276 | .33 | 0.70 [−0.43 to 1.83] |
| Crow et al. (2014) | USA | 3,902 | .45 | 1.01 [−0.30 to 2.32] |
| Massing-Schaffer et al. (2015) | USA | 185 | .27 | 0.56 [−0.46 to 1.58] |
| McCabe et al. (2018) | Latinas | 548 | .21 | 0.43 [−0.47 to 1.33] |
| Novelo et al. (2018) | Brazil | 449 | .38 | 0.81 [−0.40 to 2.20] |
| Sunley et al. (2020) | Netherland | 22,551 | 1.48 | 0.30 [−0.18 to 0.22] |
| Depression and anxiety total | 0.80 [−0.46 to 1.06] | |||
| Clinical population | ||||
| Arnow et al. (2011) | USA | 5,673 | .68 | 1.84 [0.22 to 3.46] |
| Can et al. (2019) | Turkey | 328 | .45 | 0.45 [−0.47 to 1.37] |
| de Mattos Souza et al. (2016) | Brazil | 473 | .02 | 0.04 [−0.24 to 0.32] |
| Janiri et al. (2015) | Italy | 207 | .08 | 0.15 [−0.37 to 0.67] |
| Etain et al. (2010) | France | 300 | .21 | 0.42 [−0.48 to 1.32] |
| Evren et al. (2016) | Turkey | 190 | .39 | 0.84 [−0.38 to 2.06] |
| Jaworska-Andryszewska et al. (2018) | Poland | 52 | .04 | 0.07 [−0.32 to 0.46] |
| Kefeli et al. (2018) | Turkey | 80 | .01 | 0.02 [−0.18 to 0.22] |
| Kounou et al. (2013) | France | 181 | .34 | 0.72 [−0.42 to 1.86] |
| Neumann (2017) | Germany | 191 | .26 | 0.54 [−0.46 to 1.54] |
| Ostefjells et al. (2017) | Norway | 261 | .52 | 1.22 [−0.19 to 2.63] |
| Pavlova et al. (2016) | Geneva | 174 | .19 | 0.38 [−0.47 to 1.23] |
| Schulz et al. (2017) | Germany | 123 | .28 | 0.58 [−0.47 to 1.23] |
| Xie et al. (2018) | China | 679 | .54 | 1.27 [−0.17 to 2.71] |
| Zhang et al. (2013) | China | 2,090 | .20 | 0.41 [−0.47 to 1.29] |
| Clinical population total | 0.31 [0.03 to 0.37] | |||
Note . CI = confidence interval.
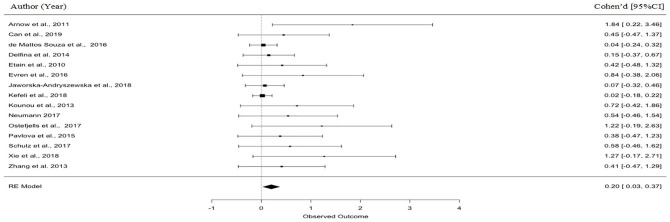
Figure 2.
Forest plot for CEA and suicide ideation.
Note. CEA = childhood emotional abuse.
Figure 3.
Funnel plots of the included. Studies of the associations between emotional abuse and suicide ideation (left). Studies of the associations between emotional abuse and suicide ideation used the trim and fill method (right).
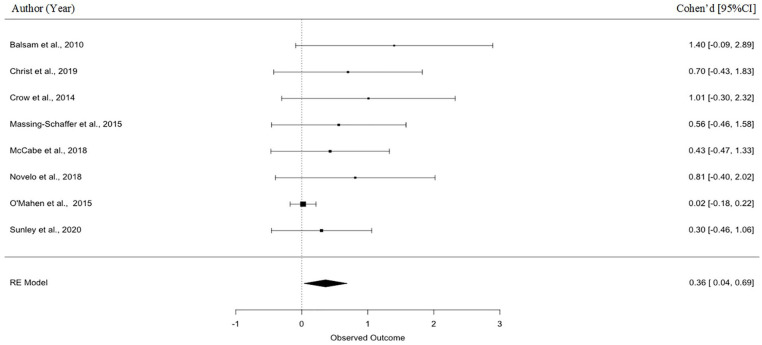
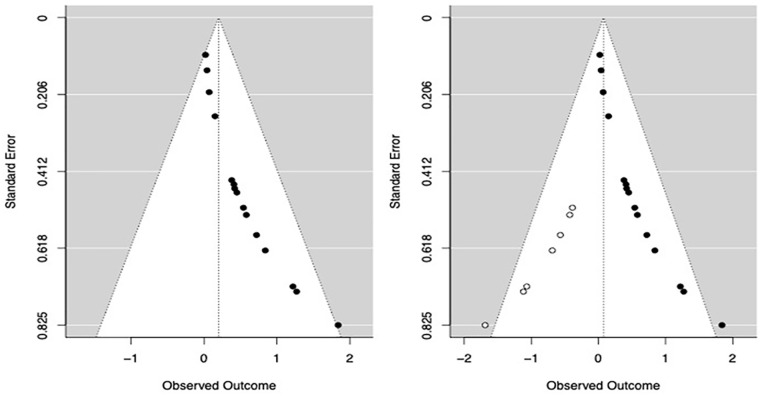
Depression and anxiety
Based on the eight included studies (see Table 3), the pooled estimates for the associations between CEA and adult depression and anxiety were 0.36 (95% CI [.036, 0.687], p = .030, τ2 = .053, H2 = 1.33) suggesting a small to medium effect size (Figure 4). The heterogeneity test suggested that the variance between the included studies was not significant (Q (7) = 9.214, p = .238, I2 = 24.82%), demonstrating that the studies were comparable. Using the trim and fill method (Duval, 2005), it was estimated that five studies were potentially missing (SE = 1.648). After adjusting for potential bias, the pooled estimates were .05 (95% CI [−0.113, 0.221], p = .524). The test for heterogeneity was Q (12) = 18.924, p = .090, I2 = 0 suggesting that the effect size was smaller after adjusting potential publication bias. Funnel plots are shown in Figure 5.
Figure 4.
Forest plot for CEA and depression and anxiety.
Note. CEA = childhood emotional abuse.
Figure 5.
Funnel plots of the included. Studies of the associations between emotional abuse and depression and anxiety (left). Studies of the associations between emotional abuse and depression and anxiety used the trim and fill method (right).
Clinical population
Based on the 15 included studies (see Table 3), the pooled estimates for the associations between CEA and having a clinical diagnosis of a mental health disorder were 0.2 (95% CI [.035, 0.365], p = .018, τ2 = .013, H2 = 1.16), suggesting a small to medium effect size. The heterogeneity test suggested that the variances between the included studies were not significant (Q (14) = 15.952, p = .316, I2 = 13.44%). Figure 6 depicts the forest plot of the included studies. Using the trim and fill method (Duval, 2005), it was estimated that seven studies were potentially missing (SE = 2.228). After adjusting for the potential bias, the pooled estimates were .07 (95% CI [−.049, 0.202], p = .23). The test for heterogeneity was Q (21) = 31.038, p = .073, I2 = 0, suggesting that effect size was smaller after adjusting the potential publication bias. Funnel plots are shown in Figure 7.
Figure 6.
Forest plot for CEA and clinical population.
Note. CEA = childhood emotional abuse.
Figure 7.
Funnel plots of the included. Studies of the associations between emotional abuse and clinical population (left). Studies of the associations between emotional abuse and clinical population used the Trim and Fill method (right).
Methodological quality assessment
The Newcastle–Ottawa Quality Assessment Scale (Well et al., 2017) was used to assess the quality (range = 0–8) of selected studies. For English studies, there were 61 case–control studies (M = 5.96, range = 4–8) (see Supplemental Material 10) and 14 cohort studies (M = 6.07, range = 4–8) (see Supplemental Material 11). For the Chinese literature, there were 11 case–control studies (M = 3.90, range = 3–5) (see Supplemental Material 12).
Moderator analysis
Moderation analysis was conducted to evaluate whether study-level moderators (year of publication, study quality, and study location) affected the associations between EA and adult mental health. We conducted a moderation analysis for suicidal ideation, depression, and anxiety and the clinical population studies. The results suggested that none of these moderators significantly impacted these associations (see Table 4).
Table 4.
Moderator Analyses.
| QM (df) | p | |
|---|---|---|
| Suicide ideation | ||
| Year | 0.000 (1) | .983 |
| Location | 2.072 (4) | .723 |
| QA | 8.168 (1) | .318 |
| Depression and anxiety | ||
| Year | 0.266 (1) | .606 |
| Location | 7.998 (4) | .092 |
| QA | 0.068 (1) | .795 |
| Clinical population | ||
| Year | 2.709 (1) | .100 |
| Location | 13.105 (10) | .218 |
| QA | 0.050 (1) | .822 |
Note. QA = Quality Assessment QM = Model Sum of Squares, df = degree of freedom.
Key findings are presented in Table 5.
Table 5.
Critical Findings.
| 1. This is the first systematic review and meta-analyses that looks at the long-term effects of CEA and CEN on adult mental health |
| 2. CEA and CEN are significantly associated with adult PD, eating disorder, depression, anxiety, suicidal ideation or attempts, substance abuse, and other psychological symptoms |
| 3. Clinical populations are more likely than non-clinical populations to have experienced CEA or CEN during childhood |
| 4. The associations between CEA/CEN and adult mental health remain significant after adjusting for other types of abuse |
| 5. Moderators such as publication year, region, and study methodological quality did not affect the associations between CEA/CEN and adult mental health problems |
| 6. There is a consistency of findings in associations between studies conducted in European countries, the United States, and Asia, suggesting that the impact of CEA/CEN on adult mental health is universal |
| 7. Studies conducted on the Chinese populations showed consistent results with English studies. |
Note. CEA = childhood emotional abuse; CEN = childhood emotional neglect; PD = personality disorder.
Discussion
Findings from 79 English and 11 Chinese papers using data from 132,082 participants aged over 18 years suggested that CEA and CEN are associated with poorer adult mental health. Our goals were to (1) review and synthesize evidence to illuminate the long-term effects of childhood psychological maltreatment on mental health; (2) assess whether there were unique effects of these forms of abuse after adjusting for others; (3) explore whether study-level moderators such as year of publication, study methodological quality, and study location affect these associations; and (4) explore whether there are differences in these associations between English language and Chinese language papers.
Our findings suggested that CEA and CEN are associated with mental health outcomes in adulthood in both English language and Chinese language papers, including the outcomes of suicidal ideation, depression, anxiety, eating disorders, PDs, and other psychological symptoms. Similarly, those belonging to clinical populations defined by adulthood mental health issues (e.g., major depression, bipolar disorder, PD, schizophrenia) were shown to have experienced more CEA and CEN. We conducted meta-analyses for the mental health outcomes with sufficient studies, namely, suicidal ideation, depression, and anxiety. The results showed that the pooled estimates suggested a small to medium effect in the expected direction. Moreover, the current review also found that the effects of CEA and CEN remained significant after adjusting for other forms of abuse.
We also found that the results from the included studies were not affected by the region where the studies were conducted. We also found in our descriptive comparison that the results in English language and Chinese language papers were consistent. That is, except for the different measurements and participants involved in English and Chinese languages, we found no differences between English and Chinese literature in the association between CEA and/or CEN and poorer adult mental health. Taken together, these findings suggest that the impacts of CEA and/or CEN on adult mental health are likely to be universal. Finally, the quality of the studies did not moderate the results of the included studies.
Completeness and Applicability of Evidence
This is the first systematic review focused on the long-term mental health correlation of experiencing CEN and CEA perpetrated by caregivers (parents or adults living in the same household) as victims. Our findings are consistent with previous systematic reviews that have focused on associations between other types of abuse and adult mental health (e.g., Norman et al., 2012; Leeb et al., 2011). For instance, Norman et al. (2012) reported an association between different forms of abuse (physical abuse, EA, and neglect) and various health consequences (e.g., drug use, suicide attempts, depression disorder, risky sexual behaviors); however, unlike in the present review, CEN was only considered as part of the broader concept of child neglect. Relative to this study, our findings provide updated results reflecting studies published in the last decade since the publication of that review, and also report additional associations between CEA and CEN and the outcomes of PDs, eating disorders, depression, and anxiety, suicidal ideation, self-injury, substance abuse, and other psychological symptoms. We also found that clinical populations reported more CEA and CEN in their childhood. Another recent systematic review (Petruccelli et al., 2019) explored different forms of childhood maltreatment and their impact on depressed mood, illicit drug use, suicidal ideation, obesity, and problematic alcohol or tobacco use. They found that the associations between childhood maltreatment and mental health outcomes were positive and significant. Finally, Liu et al. (2018) found that CEA and CEN were related to non-suicidal self-injury behaviors in their review. The findings from our review, in which we cover varying populations without limitations on gender, ethnicity, cultures, and socioeconomic status, are thus consistent with previous reviews suggesting long-term impacts of experiencing childhood abuse. We also reviewed the Chinese literature, which examined whether the associations between CEA/CEN and adult mental health generalized to different cultural contexts and found similar results.
However, there were some methodological differences worth highlighting. In the Chinese literature, researchers only measured CEA and CEN, not accompanied by measures of other types of abuse, which may have left the possibility of confounding with other types of abuse. Moreover, only Chang and Wang (2008) used a general population sample, other studies (n = 9) used college students, and one (Zhang et al., 2018) compared clinical populations and general populations.
Quality of Evidence
During the review process, some key limitations were identified. First, there was considerable variability in measurement methods for psychological maltreatment and mental health outcomes. Using different measures has both benefits and disadvantages. For example, similar results based on diverse measurement approaches increase confidence in the findings; however, measurement heterogeneity also makes it difficult to compare the results across studies. There were several ways in which the measurement approaches differed. First, some studies measured various types of abuse while some only measured CEA and CEN. In the latter case, there was no possibility to adjust for different forms of abuse. As such, these studies show that those experiencing CEA and CEN will be at risk of poorer adult mental health outcomes; however, they cannot identify the unique effects of CEA and/or CEN. This is a limitation given that different forms of abuse and adversity often co-occur and future studies on CEA and CEN are encouraged to measure these concepts in the context of other risk factors for mental health issues, especially other forms of abuse. Another difference among studies was that some aimed to measure only childhood abuse within the family setting (e.g., physical abuse, sexual abuse, emotional abuse, or neglect). In contrast, others aimed to capture more general surroundings such as peer relations or living environment. Third, the age of victimization varied widely, from 14 to 18. Finally, the perpetrators referred to in the measures differed. Some studies examined parents or caregivers as perpetrators; some were parents or another older adolescent or adult; some were parents or adults in the same household (e.g., this is often how the CTQ is used); some referred to multiple perpetrators. This was different from the Chinese studies where the perpetrators referred to in all the included studies were limited to only parents or primary caregivers.
The English language studies were mainly located in the United States (n = 32). There were another 26 studies conducted in high-income countries or regions (e.g., UK, France, Poland, Italy, Netherland, South Korea, Germany, Norway, Portugal, New Zealand, Hongkong, Australia, Geneva) and 21 studies conducted in low- or middle-income countries or regions (e.g., China, Brazil, Turkey, Iran, South Africa). Our review suggested that the associations between CEA and poor adult mental health are consistent worldwide, and this was confirmed by our moderation analysis which tested location as a moderator. The locations of the Chinese studies spanned the southern to the northern region of China; however, they were mainly from the regions with higher economic development. The lack of studies conducted in regions with lower economic development may be because there are many “left-behind children” (i.e., parents moved to other cities for work and left their children at home and asked other relatives or guardians to take care of them). The absence of parents may make the associations between CEA or CEN and adult mental health difficult to research. Studies were mainly conducted between 2010 and 2020, which suggested increasing attention to childhood psychological maltreatment and adult mental health. However, moderator analyses suggested that associations between CEA and adult mental health were not affected by the publication years. Finally, results suggested that most of the studies had a low risk of bias for English literature, while most studies had a higher risk of bias for Chinese literature. However, for both English and Chinese literature, the study quality did not affect the associations between CEA/CEN and adult mental health.
Finally, our review highlighted that CEN was found to have received less research attention compared to CEA. Only 38 English language and 11 Chinese language studies assessed CEN in our review. There are four types of child abuse—physical, sexual, emotional abuse, and neglect. Emotional neglect is under the category of neglect; therefore, some studies investigated neglect as a whole instead of emotional neglect only. For future research and measurement development, it would be beneficial to focus on the measurements for CEN and its impacts on adult mental health.
Strengths and Limitations
The current systematic review and meta-analyses represent the first effort to synthesize the English and Chinese literatures on the impacts of childhood psychological maltreatment on adult mental health.
The inclusion of studies written in both English language and Chinese language may reduce generalizability issues as investigators in non-English-speaking countries tend to publish some work in local journals (Dickersin et al., 1994). In particular, researchers might be more likely to publish positive and significant results in an international English journal while reporting negative findings in the local journal (Egger & Smith, 1998). In the current review, we included a wide geographic reach and also included samples diverse in terms of languages, genders, ethnicity, cultures, race, nationality, and geography; however, some areas of the world, especially those less developed within and across countries were under-represented.
However, our study also has some limitations with respect to diversity. Although the current review covered a wide geographic range, information such as gender identity, sexual orientation, religion, and ability were not typically available and older age groups were generally under-represented. Further research will be needed to address these gaps. In addition, due to the limited number of studies on some mental health problems (i.e., eating disorders, PDs, substance abuse, and other psychological symptoms) and articles written in Chinese, it was only possible to carry out meta-analyses on a limited number of outcomes (i.e., suicidal ideation, depression, and anxiety, and more reported CEA and CEN in clinical population). The lack of studies conducted in non-Western countries also meant that we could not fully explore these associations and their differences across different regions such as Africa, India, or South Asia. Last, despite our research team using multiple strategies to screen and extract the literature, we might have missed or misinterpreted some details presented in the literature reviewed, given the inherent challenge of identifying all studies and the subjectivity of the review process.
Implications and Future Research
This review has implications for future research, policy, or practice related to childhood psychological maltreatment and adult mental health. First, it highlights that more research in general population samples beyond the United States and other developed countries and college student samples is needed to enhance the understanding of the impacts of childhood psychological maltreatment on adult mental health. More longitudinal studies are also needed to understand the longer-term impacts of these associations across the whole lifespan including into older adulthood. This understanding could help develop prevention and interventions or training programs across the lifespan that would aim to prevent and alleviate the impacts of childhood psychological maltreatment on individuals of different ages. For instance, parental training could benefit parents unaware that their behaviors are harmful to their children. Researchers could also compare the differences in childhood psychological maltreatment in different countries or regions to explore whether different psychological maltreatment behaviors are related to specific mental health problems. Finally, EA and EN are difficult to detect and quantify; therefore, it is essential to further define and develop measures and measurement approaches to assess psychological maltreatment for further research.
Policies that better address the issue of childhood psychological maltreatment are needed. There are policies and laws about sexual and physical abuse; however, written policies or legal guidance for emotional abuse and emotional neglect generally lag behind these. Parents need to be aware of their behaviors towards their children and implement strategies such as adaptive emotional regulation strategies when children misbehave to avoid behavior consistent with psychological maltreatment. Importantly, childhood psychological maltreatment needs to be acknowledged as a severe public health concern instead of a personal and social problem, as it is seen now. Implications for practice, policy, and research are summarized in Table 6.
Table 6.
Implications for Practice, Policy, and Research.
| 1. More research studying the associations between CEA/CEN and adult mental health outcomes is needed in elder populations, clinical populations, and contexts beyond the United States or other developed countries |
| 2. Interventions to reduce CEA and CEN may help reduce the burden of adult mental health problems. Parenting training programs could, for example, use the findings from our review as the foundation to engage in intervention or coping strategies |
| 3. For clinical populations, childhood experiences may merit exploration in treatment contexts |
| 4. This systematic review provided evidence suggesting possible long-term impacts of childhood psychological maltreatment on adult mental health. Therefore, more attention to CEA and CEN prevention and mitigation is needed. |
Note. CEA = childhood emotional abuse; CEN = childhood emotional neglect.
Supplemental Material
Supplemental material, sj-docx-1-tva-10.1177_15248380221122816 for The Impact of Childhood Psychological Maltreatment on Mental Health Outcomes in Adulthood: A Systematic Review and Meta-Analysis by Zhuoni Xiao, Mina Murat Baldwin, Siu Ching Wong, Ingrid Obsuth, Franziska Meinck and Aja Louise Murray in Trauma, Violence, & Abuse
Author Biographies
Zhuoni Xiao, PhD candidate at Department of Psychology, University of Edinburgh. Her research focuses on measurements that assess psychological maltreatment, adult mental health problems. She is interested in understanding the long-term impacts of childhood psychological maltreatment on adult mental health, as well as the moderators and mediators such as resilience, self-esteem in these associations.
Mina Murat Baldwin, Mina completed her Master’s degree in Human Cognitive Neuropsychology at the University of Edinburgh in 2020. She is currently training at the NHS to qualify as a Psychological Wellbeing Practitioner. Her research interests involve mental health, well-being, and autism.
Wong Siu Ching, MSc, is a Research Assistant at the Department of Psychology, University of Edinburgh. Her research focuses on domestic violence against women, child development, and mental health. She is interested in using quantitative tools to investigate multidisciplinary problems in the fields mentioned, especially in domestic violence during pregnancy and neurodevelopmental difficulties.
Aja Louise Murray, PhD, is a Lecturer in Psychological in the Department of Psychology, University of Edinburgh. Her research uses longitudinal designs to illuminate mental health issues from a developmental perspective.
Ingrid Obsuth, PhD, is a Lecturer in Clinical Psychology in School of Health in Social Science, University of Edinburgh. Her research focuses on adolescent mental health in the context of family and school.
Franziska Meinck, DPhil, is a Lecture in School of Social and Political Science at University of Edinburgh and Extraordinary Professor at North-West University. Her research focuses on the measurement of violence against children and on social determinants of violence and associated health outcomes. She is passionate about ending violence against children using evidence-based approaches.
Footnotes
The authors declared no potential conflict of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: FM received support from the European Research Council (ERC) under the European Union’s Horizon 2020 research and innovation program [Grant Agreement Number 852787] and the UK Research and Innovation Global Challenges Research Fund [ES/S008101/1].
ORCID iD: Zhuoni Xiao  https://orcid.org/0000-0002-2030-6045
https://orcid.org/0000-0002-2030-6045
Supplemental Material: Supplemental material for this article is available online.
References
*References for included studies are in the Supplemental Material.
- Angelakis I., Austin J. L., Gooding P. (2020. a). Association of childhood maltreatment with suicide behaviors among young people: A systematic review and meta-analysis. JAMA Network Open, 3(8), e2012563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angelakis I., Austin J. L., Gooding P. (2020. b). Childhood maltreatment and suicide attempts in prisoners: A systematic meta-analytic review. Psychological Medicine, 50(1), 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armijo J. (2017). Social impairment and mental health. Annals of Behavioural Science, 3, 1. [Google Scholar]
- Baker A. J., Festinger T. (2011). Emotional abuse and emotional neglect subscales of the CTQ: Associations with each other, other measures of psychological maltreatment, and demographic variables. Children and Youth Services Review, 33(11), 2297–2302. [Google Scholar]
- Burns E. E., Jackson J. L., Harding H. G. (2010). Child maltreatment, emotion regulation, and posttraumatic stress: The impact of emotional abuse. Journal of Aggression, Maltreatment & Trauma, 19(8), 801–819. [Google Scholar]
- Claussen A. H., Crittenden P. M. (1991). Physical and psychological maltreatment: Relations among types of maltreatment. Child Abuse & Neglect, 15(1–2), 5–18. [DOI] [PubMed] [Google Scholar]
- Devries K., Knight L., Petzold M., Merrill K. G., Maxwell L., Williams A., Cappa C., Chan K. L., Garcia-Moreno C., Hollis N., Kress H., Peterman A., Walsh S. D., Kishor S., Guedes A., Bott S., Butron Riveros B. C., Watts C., Abrahams N. (2018). Who perpetrates violence against children? A systematic analysis of age-specific and sex-specific data. BMJ Paediatrics Open, 2(1). 10.1136/bmjpo-2017-000180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickersin K., Scherer R., Lefebvre C. (1994). Systematic reviews: Identifying relevant studies for systematic reviews. BMJ, 309(6964), 1286–1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon L. B., Holoshitz Y., Nossel I. (2016). Treatment engagement of individuals experiencing mental illness: Review and update. World Psychiatry, 15(1), 13–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doran C. M., Kinchin I. (2019). A review of the economic impact of mental illness. Australian Health Review, 43(1), 43–48. [DOI] [PubMed] [Google Scholar]
- Dubowitz H. (2013). Neglect in children. Pediatric Annals, 42(4), e72–e76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duval S. (2005). The trim and fill method. Publication Bias in Meta-Analysis: Prevention, Assessment and Adjustments, 127–144. [Google Scholar]
- Egger M., Smith G. D. (1998). Meta-analysis bias in location and selection of studies. BMJ, 316(7124), 61–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evren C., Dalbudak E., Cetin R., Durkaya M., Evren B. (2010). Relationship of alexithymia and temperament and character dimensions with lifetime post-traumatic stress disorder in male alcohol-dependent inpatients. Psychiatry and Clinical Neurosciences, 64(2), 111–119. [DOI] [PubMed] [Google Scholar]
- Flatley J. (2016). Abuse during childhood: Findings from the Crime Survey for England and Wales, year ending March 2016. Office for National Statistic. https://www.ons.gov.uk/peoplepopulationandcommunity/crimeandjustice/articles/abuseduringchildhood/findingsfromtheyearendingmarch2016crimesurveyforenglandandwales
- Gardner M. J., Thomas H. J., Erskine H. E. (2019). The association between five forms of child maltreatment and depressive and anxiety disorders: A systematic review and meta-analysis. Child Abuse & Neglect, 96, 104082. [DOI] [PubMed] [Google Scholar]
- Glaser D. (2002). Emotional abuse and neglect (psychological maltreatment): A conceptual framework. Child Abuse & Neglect, 26(6–7), 697–714. [DOI] [PubMed] [Google Scholar]
- Green K., Browne K., Chou S. (2019). The relationship between childhood maltreatment and violence to others in individuals with psychosis: A systematic review and meta-analysis. Trauma, Violence, & Abuse, 20(3), 358–373. [DOI] [PubMed] [Google Scholar]
- Guo J. (2018). The relationships between college students’ mental health and parental emotional abuse during childhood. Youth and Adolescent Studies, 3, 32–37. [Google Scholar]
- Grummitt L. R., Kreski N. T., Kim S. G., Platt J., Keyes K. M., McLaughlin K. A. (2021). Association of childhood adversity with morbidity and mortality in US adults: A systematic review. JAMA pediatrics, 175(12), 1269–1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hailes H. P., Yu R., Danese A., Fazel S. (2019). Long-term outcomes of childhood sexual abuse: an umbrella review. The Lancet Psychiatry, 6(10), 830–839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hibbard R., Barlow J., MacMillan H. Child Abuse and Neglect, American Academy of Child And Adolescent Psychiatry, & Child Maltreatment and Violence. (2012). Psychological maltreatment. Pediatrics, 130(2), 372–378. [DOI] [PubMed] [Google Scholar]
- Higgins J. P., Green S. (2011). Cochrane handbook for systematic reviews of interventions, version 5.1. The Cochrane Collaboration. www.cochrane-handbook.org [Google Scholar]
- Hughes K., Bellis M. A., Hardcastle K. A., Sethi D., Butchart A., Mikton C., Jones L., Dunne M. P. (2017). The effect of multiple adverse childhood experiences on health: a systematic review and meta-analysis. The Lancet Public Health, 2(8), e356–e366. [DOI] [PubMed] [Google Scholar]
- Iwaniec D. (2006). The emotionally abused and neglected child: Identification, assessment and intervention: A practice handbook. John Wiley & Sons. [Google Scholar]
- Kent A., Goddard K. L., Van Den Berk P. A. H., Raphael F. J., McCluskey S. E., Lacey J. H. (1997). Eating disorder in women admitted to hospital following deliberate self-poisoning. Acta Psychiatrica Scandinavica, 95(2), 140–144. [DOI] [PubMed] [Google Scholar]
- Leeb R. T., Lewis T., Zolotor A. J. (2011). A review of physical and mental health consequences of child abuse and neglect and implications for practice. American Journal of Lifestyle Medicine, 5(5), 454–468. [Google Scholar]
- Liu R. T., Scopelliti K. M., Pittman S. K., Zamora A. S. (2018). Childhood maltreatment and non-suicidal self-injury: a systematic review and meta-analysis. The Lancet Psychiatry, 5(1), 51–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maguire S. A., Williams B., Naughton A. M., Cowley L. E., Tempest V., Mann M. K., Teague M., Kemp A. M. (2015). A systematic review of the emotional, behavioural and cognitive features exhibited by school-aged children experiencing neglect or emotional abuse. Child: Care, Health and Development, 41(5), 641–653. [DOI] [PubMed] [Google Scholar]
- McGee R. A., Wolfe D. A. (1991). Psychological maltreatment: Toward an operational definition. Development and Psychopathology, 3(1), 3–18. [Google Scholar]
- Moody G., Cannings-John R., Hood K., Kemp A., Robling M. (2018). Establishing the international prevalence of self-reported child maltreatment: A systematic review by maltreatment type and gender. BMC Public Health, 18(1), 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrison A., Polisena J., Husereau D., Moulton K., Clark M., Fiander M., Mierzwinski-Urban M., Clifford T., Hutton B., Rabb D. (2012). The effect of English-language restriction on systematic review-based meta-analyses: A systematic review of empirical studies. International Journal of Technology Assessment in Health Care, 28(2), 138–144. [DOI] [PubMed] [Google Scholar]
- Norman R. E., Byambaa M., De R., Butchart A., Scott J., Vos T. (2012). The long-term health consequences of child physical abuse, emotional abuse, and neglect: A systematic review and meta-analysis. PLoS Medicine, 9(11), e1001349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page M. J., McKenzie J. E., Bossuyt P. M., Boutron I., Hoffmann T. C., Mulrow C. D., Shamseer L., Tetzlaff J. M., Akl E. A., Brennan S. E., Chou R., Glanville J., Grimshaw J. M., Hróbjartsson A., Lalu M. M., Li T., Loder E. W., Mayo-Wilson E., McDonald S., Moher D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. International Journal of Surgery, 88, 105906. [DOI] [PubMed] [Google Scholar]
- Petruccelli K., Davis J., Berman T. (2019). Adverse childhood experiences and associated health outcomes: A systematic review and meta-analysis. Child Abuse & Neglect, 97, 104127. [DOI] [PubMed] [Google Scholar]
- Salokangas R. K., Schultze-Lutter F., Schmidt S. J., Pesonen H., Luutonen S., Patterson P., von Reventlow H. G., Heinimaa M., From T., Hietala J. (2019). Childhood physical abuse and emotional neglect are specifically associated with adult mental disorders. Journal of Mental Health, 29(4), 376–384. [DOI] [PubMed] [Google Scholar]
- Viechtbauer W. (2010). Conducting meta-analyses in R with the metafor package. Journal of Statistical Software, 36(3), 1–48. [Google Scholar]
- Wells G., Shea B., O’Connell D., Peterson J., Welch V., Losos M., Tugwell P. (2014). Newcastle-Ottawa quality assessment scale cohort studies. University of Ottawa. [Google Scholar]
- Xiao Z., Baldwin M. M., Meinck F., Obsuth I., Murray A. L. (2021). The impact of childhood psychological maltreatment on mental health outcomes in adulthood: A protocol for a systematic review and meta-analysis. Systematic Reviews, 10(1), 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xiao Z., Obsuth I., Meinck F., Murray A. L. (2022). Validation of the Chinese version of the Psychological Maltreatment Review (PMR): A multidimensional measure of psychological maltreatment. PsyArXiv. [Google Scholar]
- Xie Z., Tang Q., Chang X., Deng Y. (2008). 457 college students’ experience of psychological abuse and neglect in childhood and mental health. Chinese Journal of Clinical Psychology, 16(1), 63–65. [Google Scholar]
- Zeng Q., Liu A., Zhong J. (2016). Mediating role of rumination between childhood psychological maltreatment and trait depression. Chinese Journal of Clinical Psychology, 24, 310–313. [Google Scholar]
- Zhang S., Zhang Y., Jin F. (2017). Mediating role of social support in the association among childdood psychological maltreatment neglect and self injury of local normal university students in Liaoning Province. Chinese Journal of School Health, 38, 1510–1512. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-tva-10.1177_15248380221122816 for The Impact of Childhood Psychological Maltreatment on Mental Health Outcomes in Adulthood: A Systematic Review and Meta-Analysis by Zhuoni Xiao, Mina Murat Baldwin, Siu Ching Wong, Ingrid Obsuth, Franziska Meinck and Aja Louise Murray in Trauma, Violence, & Abuse