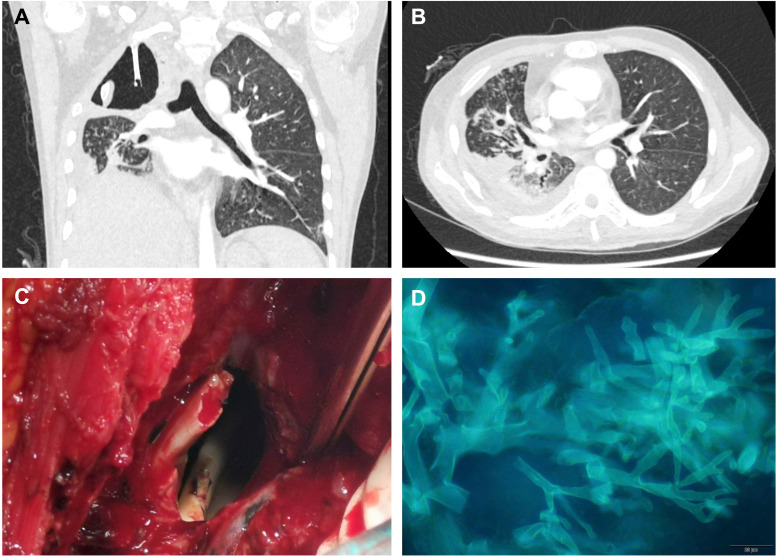
A 36-year-old man presented to the emergency department with chest pain, dyspnea, and hemoptysis of 4 months in duration. He had no fever. The patient had a history of acute lymphoblastic leukemia and was neutropenic after receiving two cycles of chemotherapy (vindesine, idarubicin, cyclophosphamide, aspartase, and dexamethasone and cyclophosphamide, vincristine, and prednisone regimens). He did not have diabetes. Physical examination was notable for decreased breath sounds on the right and low peripheral oxygen saturation. Computed tomography pulmonary angiography ruled out pulmonary embolism but showed a cavity in the right upper lung with a fractured rib hanging inside (Figure 1A). Tree-in-bud signs were present in the right middle and right lower lobes (Figure 1B). The patient denied a history of trauma. Airway fungal plugs were observed and partially removed through bronchoscopy. Metagenomic next-generation sequencing confirmed detection of Rhizomucor pusillus. A diagnosis of pulmonary mucormycosis was made, and treatment with intravenous amphotericin B and posaconazole was initiated. Right pneumonectomy was performed to remove damaged tissue after two-week antifungal therapy. The right first and second ribs (Figure 1C) were fractured, and mucor mycelium was found in the broken ends (Figure 1D). Recovery from surgery was uneventful, with continued intravenous posaconazole and amphotericin B. The patient was transferred to a local hematology center three weeks later. Another four-week antifungal treatment was given before the third cycle of chemotherapy. Informed consent was obtained from the patient’s legal representative.
Figure 1.
(A) Coronal reformatted chest computed tomography showing a cavitary lesion in the right upper lung with a fractured rib hanging inside. (B) Diffuse tree-in-bud signs were present in the right middle and lower lobes. A small cavity was seen in the right middle lobe. Pleural effusion was observed in the right lung. (C) Intraoperative photograph showing fractured end of the rib. (D) Fluorescent staining of the mycelium sample collected from the broken end of the rib, showing nonseptate hyphae branching at wide angles. Staining of sputum and airway plug sample produced similar findings. Scale bar, 20 µm.
Here we present a case of pulmonary mucormycosis with rib involvement in an immunocompromised host. Chest computed tomography showed a fractured rib hanging inside the chest cavity, resembling the “sword of Damocles,” which may lead to massive hemoptysis and may threaten survival if infection progresses. Pulmonary mucormycosis is very invasive, with a high fatality rate (1). Various tissues may be damaged by mucor infection, yet bone destruction has been rarely reported (2, 3). The rib involvement in this case was a vivid example of the high invasiveness of mucor infection. Early surgical debridement plus antifungal therapy is important for survival (4).
Footnotes
Supported by National High Level Hospital Clinical Research Funding and Elite Medical Professionals Project of China-Japan Friendship Hospital grant ZRJY2021-QM17.
Author Contributions: X.C. and B.C. were responsible for patient care. Y.L. and J.X. collected clinical information and wrote the manuscript. C.W. and B.L. conducted microbiological analysis. C.L. performed thoracic surgery. G.H. performed bronchoscopy. All authors have read and approved the manuscript.
Originally Published in Press as DOI: 10.1164/rccm.202207-1290IM on January 10, 2023
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1. Cornely OA, Alastruey-Izquierdo A, Arenz D, Chen SCA, Dannaoui E, Hochhegger B, et al. Mucormycosis ECMM MSG Global Guideline Writing Group Global guideline for the diagnosis and management of mucormycosis: an initiative of the European Confederation of Medical Mycology in cooperation with the Mycoses Study Group Education and Research Consortium. Lancet Infect Dis . 2019;19:e405–e421. doi: 10.1016/S1473-3099(19)30312-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Yang J, Zhang J, Feng Y, Peng F, Fu F. A case of pulmonary mucormycosis presented as Pancoast syndrome and bone destruction in an immunocompetent adult mimicking lung carcinoma. J Mycol Med . 2019;29:80–83. doi: 10.1016/j.mycmed.2018.10.005. [DOI] [PubMed] [Google Scholar]
- 3. Taj-Aldeen SJ, Gamaletsou MN, Rammaert B, Sipsas NV, Zeller V, Roilides E, et al. International Osteoarticular Mycoses Consortium Bone and joint infections caused by mucormycetes: a challenging osteoarticular mycosis of the twenty-first century. Med Mycol . 2017;55:691–704. doi: 10.1093/mmy/myw136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Shao W, Zhang J, Ma S, Feng H, Zhang Z, Liang C, et al. Characteristics of pulmonary mucormycosis and the experiences of surgical resection. J Thorac Dis . 2020;12:733–740. doi: 10.21037/jtd.2019.12.117. [DOI] [PMC free article] [PubMed] [Google Scholar]