Abstract
The nutritional needs already increased by adolescent growth, activity, and stress are further exacerbated by the physical, physiological, and psychological stress that orthodontic treatment causes. Hence, the main objective of this systematic review was to analyze the relationship between adequate nutrition and its impact on orthodontic treatment success rates. Using relevant keywords, reference searches, and citation searches, the databases such as PubMed–Medical Literature Analysis and Retrieval System Online, Web of Science, Cochrane, and Scopus were all searched. “Diet,” “Minerals,” “Nutrition,” “Orthodontics,” and “Vitamins” were the search terms used to scour the database. The 10 studies selected for the systematic review and subsequent meta-analysis could not conclusively establish the correlation between proper nutrition and its impact on orthodontic treatment of the patient. There was virtually little connection between patients' dietary intake and the effectiveness of their orthodontic treatment. Additionally, a direct causal link between the two could not be established legitimately because the majority of the studies reviewed only noted an impact during the early stages of the treatment.
PROSPERO Registration Number: CRD42022380828
Keywords: Diet, minerals, nutrition, orthodontics, vitamins
Introduction
The science of food, the nutrients, and other substances within, their action, interaction, and balance in connection to health and diseases, and the processes by which the organism ingests, digests, absorbs, transports, utilizes, and excretes food substances[1] are all included in nutrition. The right amount of nourishment consumed determines the person's optimal growth and development. Any nutritional deficiency causes severe and long-lasting deformity when tissues and organs are still developing. Additionally, diet affects the time of sexual development, delaying menarche in cases of starvation and preponing it in cases of obesity.[2] Hippocrates stressed the significance of nutrition, saying “There are many additional maladies coming from inadequacy of diet, different from those of repletion, but no less awful”.[3] The scope of orthodontic therapy includes everything from addressing craniofacial complex growth and development to moving teeth through the medium of adjacent periodontal tissues. As a result, diet and orthodontic therapy interact strongly. This is so because orthodontic treatment has an impact on food consumption, quality, and consistency, while nutrition impacts periodontal condition, oral flora, healing potential, immune response, and growth of the individual.[4] The orthodontic treatment causes physical, physiological, and psychological stress, which increases nutritional needs already raised by adolescent growth, activity, and stress.[4] The lack of literature on the subject makes clear how neglected diet is, despite its crucial significance in orthodontic therapy.
Nutritional deficits can have a substantial impact on how well the body's endocrine glands work, which can affect both the dentition and the growth and development of the entire body.[5] The likelihood of cleft lip and palate in the progeny of animals fed a diet deficient in folic acid, riboflavin, and zinc is increased.[6] Malnutrition has been linked to retarded growth and the formation of face bones.[7,8] Reduced skull base length, jaw height, maxillomandibular width, and reduced facial height[8] are all possible effects of malnutrition. The use of attachments and force elements during orthodontic treatment might have a negative impact on dietary intake and jeopardize the patient's nutrition. However, a balanced diet is necessary for orthodontic treatment to be successful. As a result, it enters a vicious cycle that both the patient and the orthodontist should be aware of. The connection between nutrition and orthodontic therapy is discussed in this essay. Orofacial structure development is also influenced by the method of obtaining nourishment. Breastfeeding is essential for the growth of dentofacial structures and the development and synchronization of the orofacial muscles, which in turn help with the maturation of numerous key functions as a whole.[9] In contrast to subjects on a hard diet, subjects on a soft diet had narrow arches caused by underdeveloped muscles and supporting structures.[10] The incidence of class II malocclusion increased when coarse and fibrous meals were avoided, according to research.[11] Vitamins and minerals are a crucial part of a balanced diet and play a crucial role in promoting healthy development and growth. While vitamin A excess and vitamin D shortage produce skull softening as a result of decreased calcium deposition and also enhance the susceptibility for cleft lip and palate, vitamin A insufficiency and protein deficit result in inadequate bone growth concurrent with malocclusion of teeth.[5,12] Calcium and phosphorus metabolism, which is necessary for the development of the skeleton and teeth, is aided by vitamin D.[12] Lack of vitamin D results in rickets, maxillary dysplasia, difficulty closing facial sutures, an open bite, transverse hypodimension, and a malformed palate.[5]
To prevent appliance breakage and bracket debonding, orthodontists advise their patients to stay away from chewy, sticky, sticky–gummy, or very hard foods.[13] Choosing a soft diet over a hard one during orthodontic treatment causes dietary modifications that enhance fat intake while decreasing fiber and carbohydrate intake. During orthodontic treatment, copper and manganese levels decreased, according to Strause and Saltzmann.[14] It was attributed to avoiding nuts, whole grains, and eating fewer fruits and vegetables. Copper is necessary for the synthesis of hemoglobin and red blood cells, as well as for collagen cross-linking, redox system enzymes, and proper pigmentation.[13,15,16] Manganese is essential for glucose metabolism and bone remodeling.[14]
Hence, our primary objective in conducting this systematic review and meta-analysis was to examine research that had been written about the impact of nutrition and other dietary habits on various orthodontic treatment techniques. Additionally, we looked at whether nutrition played a role in the success or failure of orthodontic therapy.
Materials and Methods
Protocol employed
This systematic review was performed as per the Preferred Reporting Items for Systematic Review and Meta-analysis (PRISMA) strategy and rules from the Cochrane group and the book Orderly Reviews in Health Care: Meta-Examination.[17]
Review hypotheses
Through this systematic review, our primary objective was to review studies that were published in the orthodontic literature about the effects of nutrition and other dietary patterns on the various orthodontic treatment modalities. Also, we sought to identify if nutrition was critical in the success/failure of orthodontic treatment.
Study selection
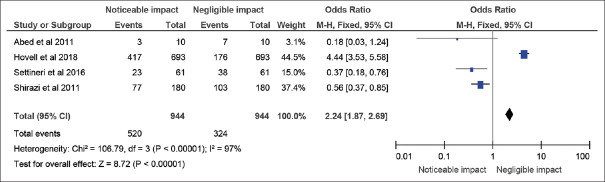
There were a total of 484 documents discovered after an extensive search on online journals, and 231 of the papers were selected initially. Following that, 164 similar/duplicate articles were eliminated, which resultantly made 67 separate papers available at first. The abstracts and titles of submissions were then reviewed, and a further 57 papers were eliminated. Finally, 10 documents that met the requisite inclusion and exclusion criteria were chosen, which primarily included in vitro studies, literature reviews, and comparative assessments [Figure 1].
Figure 1.
Representation of the selection of articles through PRISMA framework
Inclusion criterion
Articles that contained relevant data for our review objectives were selected for full-text screening. Studies that reported clinical trials, in vitro studies, randomized/non-randomized studies, systematic/literature reviews containing substantial sample volume, and detailed case reports were considered for inclusion in our review [Table 1]. We also monitored studies that possessed higher methodological quality.
Table 1.
AMSTAR-2 16-point checklist of risk-of-bias assessment in studies selected for the systematic review
| Studies selected | Question and inclusion | Protocol | Study design | Comprehensive search | Study selection | Data extraction | Excluded studies’ justification | Included study details |
|---|---|---|---|---|---|---|---|---|
| Abed et al. 2011[19] | Yes | Yes | Yes | Yes | Yes | No | No | No |
| Ashish et al. 2017[20] | Yes | Yes | Yes | Yes | Yes | No | No | No |
| Hovell et al. 2018[21] | Yes | Yes | Yes | Yes | Yes | No | No | No |
| Ibraheem et al. 2021[22] | Yes | Yes | Yes | Yes | Yes | No | No | No |
| Maheshwari et al. 2017[23] | Yes | Yes | Yes | Yes | Yes | No | No | No |
| Mehta et al. 2020[24] | Yes | Yes | Yes | Yes | Yes | No | No | No |
| Bose et al. 2021[25] | Yes | Yes | Yes | Yes | Yes | No | No | No |
| Settineri et al. 2016[26] | Yes | Yes | Yes | Yes | Yes | No | No | No |
| Shirazi et al. 2011[27] | Yes | Yes | Yes | Yes | Yes | No | No | No |
| Singh et al. 2017[28] | Yes | Yes | Yes | Yes | Yes | No | No | No |
|
| ||||||||
| Studies selected | Risk of bias | Funding sources | Statistical methods | Risk of bias in meta-analysis | Risk of bias in individual studies | Explanation of heterogeneity | Publication bias | Conflict of interest |
|
| ||||||||
| Abed et al. 2011[19] | Yes | N/A | Yes | Yes | Yes | Yes | Yes | Yes |
| Ashish et al. 2017[20] | Yes | N/A | Yes | Yes | Yes | Yes | Yes | Yes |
| Hovell et al. 2018[21] | Yes | N/A | Yes | N/A | Yes | Yes | Yes | Yes |
| Ibraheem et al. 2021[22] | Yes | N/A | Yes | Yes | Yes | Yes | Yes | Yes |
| Maheshwari et al. 2017[23] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Mehta et al. 2020[24] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Bose et al. 2021[25] | Yes | N/A | Yes | Yes | Yes | Yes | Yes | Yes |
| Settineri et al. 2016[26] | Yes | N/A | Yes | Yes | Yes | Yes | Yes | Yes |
| Shirazi et al. 2011[27] | Yes | N/A | Yes | N/A | Yes | Yes | Yes | Yes |
| Singh et al. 2017[28] | Yes | N/A | Yes | Yes | Yes | Yes | Yes | |
Exclusion criteria
The following were excluded from the scope of our systematic review: incomplete data, seminar presentations, scholarly articles, placebo-controlled studies, and opinion articles.
Since the literature available on this topic was quite scant in volume, we did not limit our search in terms of the time period when the studies were published, that is, we took into account all the papers that were published with context to our topic (where the number of papers itself was found to be quite sparse in number). Also, excluded were literature reviews and cases published in languages other than English.
Search strategy
The databases such as PubMed–Medical Literature Analysis and Retrieval System Online, Web of Science, Cochrane, and Scopus were all searched using pertinent keywords, reference searches, and citation searches. The search terms utilized to comb through the database were “Diet,” “Minerals,” “Nutrition,” “Orthodontics,” and “Vitamins.”
Data selection and coding
Two independent reviewers located the relevant papers using the right keywords in various databases and online search tools. The chosen articles were compared, and a third reviewer was brought in if there was a dispute.
After choosing the articles, the same two reviewers independently extracted the following data: author, year of publication, country, kind of publication, study topic, population demographics (n, age), outcome measure(s), relevant result(s), and conclusion(s). The data were compared, and any differences were discussed with the third reviewer.
Risk-of-bias assessment
The A Measurement Tool to Assess systematic Reviews (AMSTAR)-2 technique[18] was used to evaluate the risk of bias in the studies we chose. AMSTAR-2 joins many other instruments that have been released for this purpose as a critical evaluation tool for systematic reviews. As seen in Table 2, it is a 16-point checklist. Two instruments that have drawn a lot of attention served as the foundation for the creation of the original AMSTAR tool. The original AMSTAR was duplicated in two newly produced instruments. The AMSTAR-2 risk-of-bias items identify the domains specified in the Cochrane risk-of-bias instruments for systematic reviews. In each case, these indicate an agreement that was achieved after input from more than 30 methodology experts.
Table 2.
Description and outcomes as observed in the studies selected for the systematic review
| Author and year of study | Sample size | Study design | Study objective/description | Study inference/outcome |
|---|---|---|---|---|
| Abed et al. 2011[19] | 10 adolescents (mean age 13.21 years; 4 males) | Qualitative interview- based study | The purpose of this study was to evaluate how fixed orthodontic treatment affected dietary intake and behavior. By conducting semi-structured one-on-one interviews with 10 adolescent patients receiving fixed orthodontic treatment—with a mean age of 13.21 years—the study used a qualitative methodology. By applying framework principles to identify emerging themes and ideas, the interviews were transcribed and analyzed by two separate researchers. | The two primary themes arising in adolescent patients receiving fixed orthodontic treatment were pain experience and dietary change, according to framework analysis. During the first few days of treatment, all patients complained of varying degrees of pain; however, after that, it was observed to lessen. All patients acknowledged that their diets had changed as a result of pain, difficulty chewing and biting, and dietary recommendations made by their orthodontist. Patients believed that after receiving treatment, their eating habits had improved. The study made clear the need to investigate dietary modifications across a wider population base. |
| Ashish et al. 2017[20] | - | Literature review | By conducting this literature review, the authors hoped to shed light on the relationship between dietary habits and the orthodontic treatment the patient received, and how nutrition may play a crucial role in enhancing the likelihood that the orthodontic therapy will be successful. | The physicians remarked that it could have been advantageous to offer dietary assistance to orthodontic patients in selecting soft food diets to optimize patients’ physiologic response to orthodontic therapy. This involved gathering nutritional history, assessing the diet, enlightening the patient about diet elements crucial to dental health, inspiring the patient to improve diet, and providing follow-up to assist the patient in changing their eating habits. |
| Hovell et al. 2018[21] | 693 children (8-14 years old) | Randomized control trial | The authors enlisted orthodontic offices in Southern California and Tijuana, Mexico, and enlisted their patients aged 8 to 16 to participate in a two-year study to conduct a randomized controlled trial to determine whether brief exercise and dietary advice given during child patient visits their orthodontic office could improve diet, physical activity, and age- and gender-adjusted BMI. The staff gave the kids “prescriptions” for bettering their eating and activity habits at each visit to the office. | Although the authors highlighted that orthodontists might give non-dental preventative counsel to complement other health practitioners’ recommendations, the intervention, which was based on the Geoffrey Rose model, had minimal success in reaching its goals. To adequately examine the effectiveness of clinician-based brief counsel on preventing child obesity and/or reversing obesity, higher integrity to trial design was required. |
| Ibraheem et al. 2021[22] | - | Literature review | This review was created after searching and compiling articles from 1930 to July 2021. It emphasizes different food types that should be consumed during fixed orthodontic therapy and explains the impact of different foods and beverages on the growth and development of craniofacial structures, tooth surfaces, root resorption, tooth movement, retention, and stability after orthodontic treatment, as well as the impact on the components of fixed orthodontic appliances. | The authors noted that it might be helpful to offer dietary advice to the patient to optimize their physiological reactions to orthodontic treatments. This could be done by obtaining their nutritional history, assessing their diet, teaching them about the diet elements that are crucial for oral health, inspiring them to improve their diet, and then following up to support their efforts to alter their eating habits. |
| Maheshwari et al. 2017[23] | - | Literature review | The authors of this study believed that specific dietary considerations and recommendations were essential for the patient’s overall health and the success of the treatment, so they provided an overview of the relationship between diet and orthodontic treatment, including orthognathic surgeries. | According to the authors, it could have been advantageous to give the orthodontic patients proper food advice to maximize their physiologic response to the orthodontic therapy. To support patients’ efforts to alter their eating habits, practitioners needed to assume responsibility for gathering nutrition history, evaluating the diet, educating the patient about diet components and their significance for oral health, motivating the patient to improve their diet, and following up. |
| Mehta et al. 2020[24] | - | Literature review | The authors’ objective in performing this literature review was to establish a connection between dietary practices and the orthodontic therapy the patient underwent and how nutrition may be a key factor in increasing the likelihood that the orthodontic therapy would be effective. | It was advised that dietary advice be given to orthodontic patients in choosing soft food diets, which included obtaining nutrition history, evaluating the diet, and educating the patient about diet components important for oral health. Adequate nutrition allowed proper healing response during applied orthodontic forces that optimized the patient’s physiologic response to orthodontic treatment. |
| Bose et al. 2021[25] | - | Through this review, the authors sought to learn more about the role that dietary management plays in an orthodontic procedure that lessens the likelihood that the orthodontic appliance will be harmed. They thought it was advantageous for both the orthodontist and the patient undergoing treatment, as well as convenient for the orthodontist. | The authors noted that the key to successful orthodontic treatment was following an orthodontist’s recommended diet. Less breakage of orthodontic attachments, which was the most frequent mistake experienced by orthodontists, resulted from teaching a patient receiving orthodontic treatment about his or her diet. | |
| Settineri et al. 2016[26] | 61 adolescents (mean age 15.6 years) | Correlational study | The study’s objective was to examine the connection between the psychological effects of orthodontic treatment on adolescents’ levels of self-esteem and any potential relationships with their eating patterns. 61 teenagers between the ages of 12 and 22 took part in the study. The Eating Attitudes Test, the Rosenberg Self-Esteem Scale, and the Psychosocial Impact of Dental Aesthetics Questionnaire were used in interviews with each adolescent. | Although the data could not directly link eating disorders to dental aesthetics, adolescents undergoing orthodontic treatment, particularly in the early stages of donning braces, had odd eating habits and experienced a greater psychological impact of dental aesthetics. Eating habits and overall self-esteem were directly related. |
| Shirazi et al. 2011[27] | 180 individuals (15-17 years old) | Randomized control trial | 180 patients between the ages of 15 and 17 participated in this study, 90 of whom were in the study group and 90 of whom were controls. The primary goal of the study was to compare the nutrient intakes of adolescents wearing fixed orthodontic appliances and a control group matched for age and gender. A 24-hour recollection recall was used to evaluate nutritional intake, and demographic information was gathered using questionnaires. | Orthodontic patients consumed about the same total calories, protein, and carbohydrates as the control group did, but they consumed more total fat, saturated fat, monounsaturated fat, polyunsaturated fat, linolenic fat, linoleic fat, and cholesterol. They also consumed significantly less fiber, chromium, and beta-carotene. Other macro- and micronutrient intake did not vary considerably between the groups. |
| Singh et al. 2017[28] | - | Literature review | The authors of this research discussed the connection between nutrition and orthodontic therapy because they thought that a balanced diet was essential for successful orthodontic treatment and should be taken into account by both the patient and the orthodontist. | The authors pointed out that to improve the patient’s physiological responses to orthodontic treatments, it would be beneficial to provide nutritional recommendations. This could be achieved by learning about their nutritional background, evaluating their diet, educating them about the diet components that are important for dental health, motivating them to change their diet, and then following up to support their efforts to adjust their eating patterns. |
BMI: Body mass index
Statistical analysis
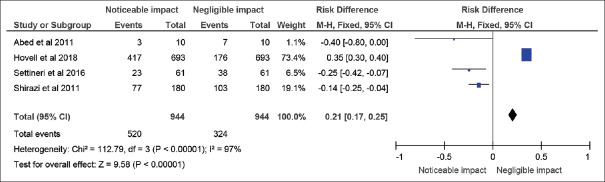
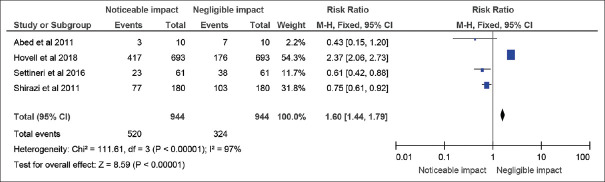
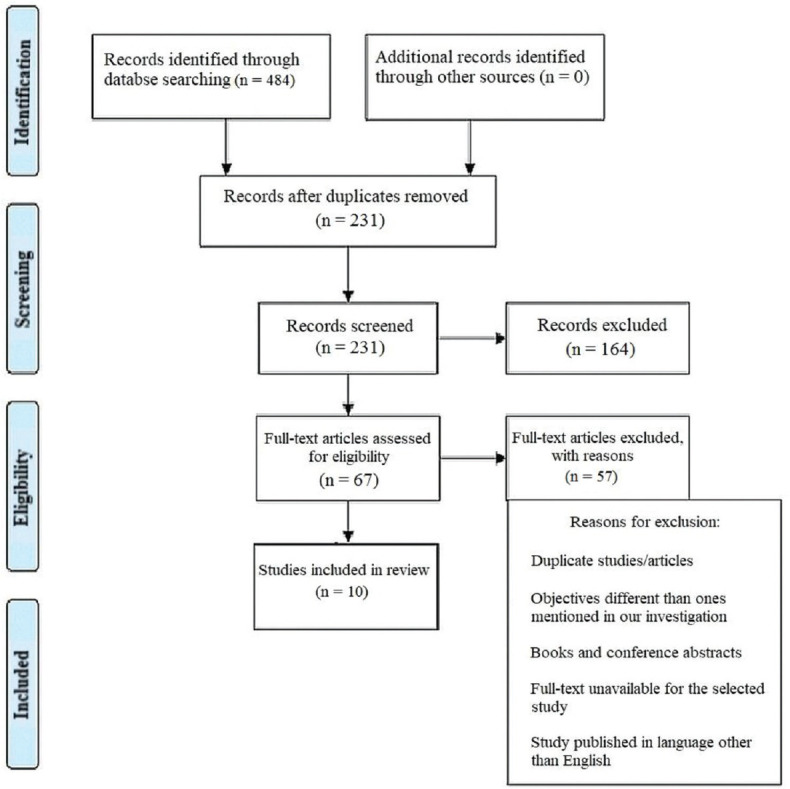
After selecting data on the sample size, variables analyzed, and various elements of the investigations, the data were then entered into the RevMan 5 program for meta-analysis. Forest plots illustrating the odds ratio for different study methodologies were obtained as part of the meta-analysis for our study as shown in Figures 2-4.
Figure 2.
Odds ratio of randomized control trials and qualitative studies selected in this systematic review that assessed the impact of dietary habits and nutrition on orthodontic treatment represented on a forest plot after meta-analysis
Figure 4.
Risk difference in randomized control trials and qualitative studies selected in this systematic review that assessed the impact of dietary habits and nutrition on orthodontic treatment represented on a forest plot after meta-analysis
Figure 3.
Risk ratio of randomized control trials and qualitative studies selected in this systematic review that assessed the impact of dietary habits and nutrition on orthodontic treatment represented on a forest plot after meta-analysis
Results
The study design, methodology employed, description, and outcome are mentioned in Table 2. The results of the meta-analysis are provided in Figures 2-4.
Discussion
According to the literature, a patient's dietary state may have an impact on how their tissues respond to orthodontic forces. For instance, the ascorbic acid shortage is thought to delay orthodontic tooth movement by reducing the body's capacity for healing. Too little ascorbic acid prevents collagen from breaking down and reforming, which is important for tooth movement.[4,29] Ascorbic acid levels in orthodontic patients range from 17% to 72% below ideal.[29,30] Although there is little literature on how orthodontic treatment affects a patient's diet and even fewer reports on specific diet guidelines for orthodontic patients, orthodontists frequently advise their patients to eat soft foods during treatment to accommodate pressure sensitivity experienced with tooth movement.[31] However, there is not much mention of how orthodontic treatment modalities are affected by the nutritional patterns of the patients using orthodontic appliances. To date, we discovered only three randomized clinical trials that discussed the direct correlation between orthodontic treatment and nutritional profile.[21,27,32]
Sean Beattie et al.[33] proposed that polymeric elastic bands serve as one of the foundations for orthodontic tooth movement by replicating the effects of daily diet and patient compliance with elastic band alteration. In contrast to using heavy force, using light force at the right rates allows for quick tooth movement during orthodontic therapy with the least amount of patient discomfort and mobility. Force degradation is influenced by lumen size, with smaller diameters requiring more frequent renewal to maintain the intended force application.[34] Studies have looked into the impacts of simulated saliva environments, pH, and thermocycling, in an effort to model different oral environments, on force degradation.[34,35,36,37] The simplest formulation of artificial saliva is 0.09% aqueous sodium chloride, which is frequently employed in experiments simulating the intraoral environment. In general, the data showed that after elastics were subjected to experimental circumstances, force significantly relaxed. During clinical use, orthodontic elastic bands are believed to degrade mostly as a result of mechanical forces.[37] Leachable moieties, however, have been isolated from a few orthodontic elastic bands, and their rising concentrations in solution correlated with a gradual loss of force.[38] The majority of the experiments on the deterioration of orthodontic elastic materials have been done in artificial saliva or air, although this topic has been studied.[36,37,38] However, dental polymeric restorative materials’ reactions to food-like oral environments have been researched. When polymeric restorative materials are exposed to ethanol/water, ethanol/artificial saliva, lactic acid, citric acid, and alcohol/water as simulated foods, several forms of degradation have been observed to be accelerated that include coffee, erythrosine, food colors, vinegar, Coca-Cola, whisky, and oranges.[39,40,41]
According to Gokhan Oncag et al.,[40] the study looked at how acidic soft beverages affected metal brackets’ resistance to shear stresses both in vitro and in vivo and discovered that there was no statistically significant difference between the in vivo and in vitro groups in terms of debonding resistance. In both the in vitro and in vivo groups, areas of enamel surface defect brought on by erosion were seen close to the brackets. Coca-Cola and Sprite are examples of acidic soft beverages that negatively affect bracket retention against shearing pressures and enamel erosion.
Shimizu et al.'s[41] investigation on changes in the upper and lower alveolar bones’ skeletal microstructure after masticatory loading brought on by feeding growing rats a soft diet. The findings show that in rats with modest masticatory stress throughout growth, alveolar osteopenia is more severe in the mandible than the maxilla.
The lack of randomized control trials can be attributed to being a major flaw in this systematic review of ours; however, the topic of nutrition and its correlation with orthodontic treatment/management modalities has been very poorly represented and quite under-researched in the literature as we observed. Also, a ton of literature/scoping reviews exist on this topic, which we believe do not paint an accurate picture since they lack evidence of a correlation between orthodontic treatment and dietary patterns. Hence, we believe that more studies are needed to ascertain the link between the two factors so that credible, fact-based recommendations can be devised that are beneficial for the patients undergoing treatment.
Conclusions
This systematic review found a very weak correlation between the nutritional intake of patients and its impact on their orthodontic treatment. Also, since most of the studies mentioned only noticed an impact during the beginning phase of the treatment, a direct causal link between the two could not be established credibly. Hence, we believe more studies are needed in this regard and we believe orthodontic patients should receive nutritional counseling, and enlisting the assistance of a nutritionist may be beneficial.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Cuerda C, Muscaritoli M, Krznaric Z, Pirlich M, Van Gossum A, Schneider S, et al. Nutrition education in medical schools (NEMS) project: Joining ESPEN and university point of view. Clin Nutr. 2021;40:2754–61. doi: 10.1016/j.clnu.2021.03.010. [DOI] [PubMed] [Google Scholar]
- 2.Spinelli A, Buoncristiano M, Nardone P, Starc G, Hejgaard T, Júlíusson PB, et al. Thinness, overweight, and obesity in 6- to 9-year-old children from 36 countries: The World Health Organization European Childhood Obesity Surveillance Initiative—COSI 2015–2017. Obes Rev. 2021;22((Suppl 6)):e13214. doi: 10.1111/obr.13214. [DOI] [PubMed] [Google Scholar]
- 3.Giridhar VU. Role of nutrition in oral and maxillofacial surgery patients. Natl J Maxillofac Surg. 2016;7:3–9. doi: 10.4103/0975-5950.196146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Khatri JM, Kolhe VD. Nutrition and orthodontics. Int J Orthod Rehabil. 2018;9:163–7. [Google Scholar]
- 5.Jairam LS, Konde S, Raj NS, Kumar NC. Vitamin D deficiency as an etiological factor in delayed eruption of primary teeth: A cross-sectional study. J Indian Soc Pedod Prev Dent. 2020;38:211–5. doi: 10.4103/JISPPD.JISPPD_184_18. [DOI] [PubMed] [Google Scholar]
- 6.Nahas LD, Alzamel O, Dali MY, Alsawah R, Hamsho A, Sulman R, et al. Distribution and risk factors of cleft lip and palate on patients from a sample of Damascus hospitals-A case-control study. Heliyon. 2021;7:e07957. doi: 10.1016/j.heliyon.2021.e07957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jasim E, Garma N, Mohammed N. The Association between Malocclusion and Nutritional Status among 9-11 Years Old Children. Iraqi Orthod J. 2016;12:13–9. [Google Scholar]
- 8.Thomaz EB, Cangussu MC, da Silva AA, Assis AM. Is malnutrition associated with crowding in permanent dentition? Int J Environ Res Public Health. 2010;7:3531–44. doi: 10.3390/ijerph7093531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fisher J, Selikowitz HS, Mathur M, Varenne B. Strengthening oral health for universal health coverage. Lancet. 2018;392:899–901. doi: 10.1016/S0140-6736(18)31707-0. [DOI] [PubMed] [Google Scholar]
- 10.Kingsnorth J, Cushen SJ, Janiszewska K, Avery A. Health professionals’ knowledge, views and advice on diet and dental health: A survey of UK and Ireland dietitians and dentists. J Hum Nutr Diet. 2021;34:705–14. doi: 10.1111/jhn.12842. [DOI] [PubMed] [Google Scholar]
- 11.Zhang X, Yi J, Li Y. Effects of nutrition and hormones on functional appliance treatment outcome in patients with skeletal class II malocclusion. J World Fed Orthod. 2020;9:9–12. doi: 10.1016/j.ejwf.2020.01.004. [DOI] [PubMed] [Google Scholar]
- 12.Leszczyszyn A, Hnitecka S, Dominiak M. Could vitamin D3 deficiency influence malocclusion development? Nutrients. 2021;13:2122. doi: 10.3390/nu13062122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shirazi M, Tamadon M, Izadi M. Effect of addition of bioactive glass to resin modified glass ionomer cement on enamel demineralization under orthodontic brackets. J Clin Exp Dent. 2019;11:e521–6. doi: 10.4317/jced.55576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Strause L, Saltman P. Role of manganese in bone metabolism. Nutritional Bioavailability of Manganese. 1987;354:46–55. doi: 10.1021/bk-1987-0354.ch005. [Google Scholar]
- 15.Scribante A, Dermenaki Farahani MR, Marino G, Matera C, Rodriguez Y Baena R, Lanteri V, et al. Biomimetic effect of nano-hydroxyapatite in demineralized enamel before orthodontic bonding of brackets and attachments: Visual, adhesion strength, and hardness in in vitro tests. Biomed Res Int. 2020;2020:6747498. doi: 10.1155/2020/6747498. doi: 10.1155/2020/6747498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nam HJ, Kim YM, Kwon YH, Yoo KH, Yoon SY, Kim IR, et al. Fluorinated bioactive glass nanoparticles: Enamel demineralization prevention and antibacterial effect of orthodontic bonding resin. Materials (Basel) 2019;12:1813. doi: 10.3390/ma12111813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009;6:e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008. doi: 10.1136/bmj.j4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abed Al Jawad F, Cunningham SJ, Croft N, Johal A. A qualitative study of the early effects of fixed orthodontic treatment on dietary intake and behaviour in adolescent patients. Eur J Orthod. 2011;34:432–6. doi: 10.1093/ejo/cjr032. [DOI] [PubMed] [Google Scholar]
- 20.Ashish A, Pradeep R, Utkarsh S, Abhimanyu K. Diet and nutrition: Conceptual importance in the speciality of orthodontics-a review. Int J Adv Res. 2017;5:2198–202. [Google Scholar]
- 21.Hovell MF, Schmitz KE, Liles S, Robusto K, Hofstetter CR, Nichols JF, et al. A randomized controlled trial of orthodontist-based brief advice to prevent child obesity. Contemp Clin Trials. 2018;70:53–61. doi: 10.1016/j.cct.2018.05.003. [DOI] [PubMed] [Google Scholar]
- 22.Ibraheem M, Nahidh M. Diet and orthodontics- A review. J Bagh Coll Dent. 2021;33:30–8. [Google Scholar]
- 23.Maheshwari S, Tariq M, Gaur A, Jiju M. A systematic nutritional and dietary guideline for orthodontic and orthognathic surgery patients. IP Indian J Orthod Dentofacial Res. 2017;3:136–40. [Google Scholar]
- 24.Mehta V, Bagga MK, Bhatti BK. “How diet affects an orthodontic treatment outcome”- A review. Int J Res Rev. 2018;5:46–51. [Google Scholar]
- 25.Bose M, Bagga DK, Agrawal P. Managing nutrition but not damaging the orthodontic attachments: A consideration. Ann Romanian Soc Cell Biol. 2021;25:586–90. [Google Scholar]
- 26.Settineri S, Rizzo A, Ottanà A, Liotta M, Mento C. Dental aesthetics perception and eating behavior in adolescence. Int J Adolesc Med Health. 2015;27:311–7. doi: 10.1515/ijamh-2014-0031. [DOI] [PubMed] [Google Scholar]
- 27.Shirazi AS, Mobarhan MG, Nik E, Kerayechian N, Ferns GA. Comparison of dietary intake between fixed orthodontic patients and control subjects. Aust Orthod J. 2011;27:17–22. [PubMed] [Google Scholar]
- 28.Singh N, Tripathi T, Rai P, Gupta P. Nutrition and orthodontics: Interdependence and interrelationship. Res Rev J Dent Sci. 2017:18–22. [Google Scholar]
- 29.Lomanto ML. Stability in orthodontics and their relation with myofunctional orthodontics and vitamin C. SVOA Dentistry. 2021;2:115–8. [Google Scholar]
- 30.Arqub SA, Gandhi V, Iverson MG, Ahmed M, Kuo CL, Mu J, et al. The effect of the local administration of biological substances on the rate of orthodontic tooth movement: A systematic review of human studies. Prog Orthod. 2021;22:5. doi: 10.1186/s40510-021-00349-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ozdemir M, Ilhan A, Gorucu-Coskuner H, Taner T, Bilgic P. Assessment of food consumption changes in adolescents during orthodontic treatment. Am J Orthod Dentofacial Orthop. 2021;159:604–12. doi: 10.1016/j.ajodo.2019.11.023. [DOI] [PubMed] [Google Scholar]
- 32.Riordan DJ. Effects of orthodontic treatment on nutrient intake. Am J Orthod Dentofacial Orthop. 1997;111:554–61. doi: 10.1016/s0889-5406(97)70292-0. [DOI] [PubMed] [Google Scholar]
- 33.Beattie S, Monaghan P. An in vitro study simulating effects of daily diet and patient elastic band change compliance on orthodontic latex elastics. Angle Orthod. 2004;74:234–9. doi: 10.1043/0003-3219(2004)074<0234:AIVSSE>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 34.Notaroberto DFC, Martins MME, Goldner MTA, Mendes AM, Quintão CCA. Force decay evaluation of latex and non-latex orthodontic intraoral elastics: In vivo study. Dental Press J Orthod. 2018;23:42–7. doi: 10.1590/2177-6709.23.6.042-047.oar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yang L, Lv C, Yan F, Feng J. Force degradation of orthodontic latex elastics analyzed in vivo and in vitro. Am J Orthod Dentofacial Orthop. 2020;157:313–9. doi: 10.1016/j.ajodo.2019.03.028. [DOI] [PubMed] [Google Scholar]
- 36.Klabunde R, Grünheid T. Dynamic force decay evaluation of latex and non-latex orthodontic elastics. J Orofac Orthop. 2022;83:318–24. doi: 10.1007/s00056-021-00319-w. [DOI] [PubMed] [Google Scholar]
- 37.Csekő K, Maróti P, Helyes Z, Told R, Riegler F, Szalma J, et al. The effect of extrinsic factors on the mechanical behavior and structure of elastic dental ligatures and chains. Polymers (Basel) 2021;14:38. doi: 10.3390/polym14010038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Huget EF, Patrick KS, Nunez LJ. Observations on the elastic behavior of a synthetic orthodontic elastomer. J Dent Res. 1990;69:496–501. doi: 10.1177/00220345900690021601. [DOI] [PubMed] [Google Scholar]
- 39.Farahat DS, El-Wassefy NA. Effects of food-simulating solutions on the surface properties of two CAD/CAM resin composites. J Clin Exp Dent. 2022;14:e782–90. doi: 10.4317/jced.59822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Oncag G, Tuncer AV, Tosun YS. Acidic soft drinks effects on the shear bond strength of orthodontic brackets and a scanning electron microscopy evaluation of the enamel. Angle Orthod. 2005;75:247–53. doi: 10.1043/0003-3219(2005)075<0243:ASDEOT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 41.Shimizu Y, Ishida T, Hosomichi J, Kaneko S, Hatano K, Ono T. Soft diet causes greater alveolar osteopenia in the mandible than in the maxilla. Arch Oral Biol. 2013;58:907–11. doi: 10.1016/j.archoralbio.2013.02.003. [DOI] [PubMed] [Google Scholar]