Abstract
Background:
Epidermoid and dermoid cysts are benign developmental anomalies that can form anywhere in the body. Despite the rarity of incidence in the head and neck, they can arise at a variety of craniofacial locations. The purpose of this study was to analyze the clinical features of epidermoid and dermoid cysts arising in the craniofacial region with a literature review.
Methods:
A retrospective study was designed, and clinical features and surgical considerations were investigated from a literature review. Cases of epidermoid cysts in the scalp, temporal area, glabellar area, mouth floor, and buccal mucosa were described.
Results:
Dermoid cysts in more lateral regions of the scalp are rarely associated with intracranial extension. Because temporal dermoid cysts have a high rate of intracranial extension, radiological evaluation of the lesions in the temporal area is imperative. Epidermoid cysts in the glabellar area are usually superficial. Consideration of the surgical approach for an epidermoid cyst of the mouth floor is important. Because epidermoid cysts in the buccal mucosa are extremely rare, differential diagnosis was emphasized. Epidermoid cysts in the scalp, in the temporal intradiploic area, on the glabellar area in the periorbital region, in the mouth floor, and in the buccal mucosa were surgically excised considering the depth and location. Ten cases of epidermoid cysts in the buccal mucosa were retrieved from the literature review.
Conclusions:
Consideration of the anatomic locations of epidermoid and dermoid cysts in the craniofacial region might help facilitate accurate diagnosis and treatment.
Key Words: Buccal mucosa, craniofacial area, dermoid cyst, epidermoid cyst, mouth floor
Epidermoid and dermoid cysts are benign developmental anomalies that can form anywhere in the body, particularly in areas of embryonic element fusion.1,2 Epidermoid cysts are derived from the epidermis and lined with simple squamous epithelium. Dermoid cysts contain skin adnexa, such as hair follicles and sebaceous and sweat glands in the cyst wall, as well as epidermoid cyst characteristics. Epidermoid and dermoid cysts rarely occur in the head and neck, with an incidence ranging from 1.6%–6.9%.3,4 Although these conditions are rare, they occur in varied craniofacial locations. Classification by location can help guide diagnosis and treatment.5,6 Epidermoid and dermoid cysts are frequent lesions of the scalp in the pediatric population, and early excision is recommended because they can erode the cranial bone.7 Epidermoid cysts account for about 1% of intracranial tumors,8 and temporal dermoid cysts have a high rate of intracranial extension.9,10 The periorbital area is the most common site for head and neck dermoid cysts.11 Epidermoid and dermoid cysts are the most common cystic lesions in the orbital region.12 Dermoid cysts of the glabella in the periorbital area are uncommon13 and have low rates of intracranial extension.9 The mouth floor is the second most common location of dermoid cysts in the head and neck after the periorbital area.14,15 Epidermoid and dermoid cysts account for <0.1% of all cysts of the oral cavity.16,17 They can cause dyspnea or dysphagia.18–20 In the buccal mucosa, epidermoid cysts are extremely rare,21 and dermoid cysts have not been reported.
The purpose of this study is to analyze the clinical features of epidermoid and dermoid cysts arising in 5 locations in the craniofacial region with a literature review. Cases of epidermoid cysts in the scalp, temporal area, glabellar area, mouth floor, and buccal mucosa were delineated.
METHODS
The investigators performed a retrospective study of patients diagnosed with epidermoid cysts in the craniofacial area who were treated at Brong Ahafo Regional Hospital, Sunyani, Ghana, and Seoul National University Dental Hospital, Seoul, Korea. Epidermoid cysts in 5 anatomic locations, including the scalp, temporal area, glabellar area, mouth floor, and buccal mucosa, were surgically excised and pathologically confirmed. The literature search was carried out in PubMed using the keywords “[(epidermoid cyst) OR (dermoid cyst)] AND (scalp OR temporal OR orbital OR mouth floor OR buccal mucosa).”
RESULTS
Clinical features and surgical considerations of epidermoid and dermoid cysts in the craniofacial region were described according to anatomic location in clinical cases.
Scalp
Because epidermoid and dermoid cysts in the scalp can erode cranial bone, early excision is recommended.7 Dermoid cysts are usually confined to an extracranial location and can be treated with simple surgical enucleation.22 However, computed tomography (CT) or magnetic resonance imaging (MRI) might be needed to rule out the possibility of intracranial extension. The risk of invasion into deeper structures is variable and depends on the anatomic location.6 Dermoid cysts located in more lateral areas are rarely associated with intracranial extension, but lesions along the midline of the scalp have a higher potential to extend intracranially.23
A 37-year-old man presented at the Outpatient Department of Brong Ahafo Regional Hospital, Sunyani, Ghana, with superficial swelling on the right parietal area of the scalp. The cystic mass was excised en bloc with preservation of the overlying skin (Fig. 1A, B). Histopathology of the surgical specimen revealed the cyst was lined with thin squamous epithelium and involved no atypical cellular change (Fig. 1C). The pathologic diagnosis was consistent with an epidermoid cyst.
FIGURE 1.
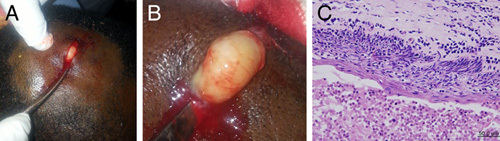
Epidermoid cyst in the scalp. (A and B) Intraoperative clinical images. (C) The cyst was lined with thin squamous epithelium and showed no atypical cellular change.
Temporal Area
Although dermoid cysts located in the lateral skull region are rarely associated with intracranial extension,23 temporal dermoid cysts have a high rate of intracranial extension.9,10 An association between frontotemporal location and bone erosion was reported.7 Preoperative imaging evaluation with CT or MRI was recommended for congenital mass in a sinus in the temporal area.10
A 17-year-old man presented at Brong Ahafo Regional Hospital with a recurrent facial mass of about 8 months duration. One year before the presentation, the patient had reported to a district hospital with a similar mass, which was excised but not histopathologically diagnosed. Two months after the surgical procedure, the patient noticed a recurrence of the mass, which was not completely removed, had gradually increased in size and had no known associated symptoms. A clinical examination revealed a well-defined elliptical facial mass with scarification marks extending from the mastoid of the temporal bone to the anterio-superior aspect of the left postauricular region (Fig. 2A, B). The edges and surface of the mass were smooth with no ulceration, and the mass was not mobile, with attachment to both underlying and overlying tissue. The mass was dark in color, similar to the patient’s facial skin, and no palpable facial or cervical lymph nodes were observed. Contrast CT revealed a predominantly hypodense fluid attenuation and an expansile intradiploic lesion in the left temporal bone and mastoid region involving the inner table of the diploic space, as shown in Figure 2C. The patient underwent surgical removal of the lesion. The scalp flap exposed an encapsulated whitish intradiploic tumor. The tumor was resected from apparently normal bone and was overlaid by scarified skin (Fig. 2D).
FIGURE 2.

Intradiploic epidermoid cyst in the temporal area. (A and B) Preoperative clinical images. (C) CT revealed a predominantly hypodense fluid attenuation, expansile, intradiploic lesion in the left temporal bone of the mastoid region involving the inner table of the diploic space. (D) The cystic mass was excised with scarified skin. CT indicates computed tomography.
Glabellar Region in the Periorbital Area
The periorbital area is the most common site for head and neck dermoid cysts.11 Epidermoid and dermoid cysts are the most common cystic lesions in the orbital region.12 Dermoid cysts at the glabellar region in the periorbital area are uncommon13 and have low rates of intracranial extension.9 Nasoglabellar dermoid cysts above the nasofrontal suture are usually superficial.10
A 36-year-old man presented at Brong Ahafo Regional Hospital with an ovoid-shape mass in the glabella in the vicinity of the medial canthus in the periorbital area (Fig. 3A). Mass excision was performed (Fig. 3B), and microscopic examination revealed that the cyst wall was lined with a thin squamous epithelium on the luminal side. The cyst contained numerous keratin plugs but no skin appendage tissue (Fig. 3C). The pathologic diagnosis was an epidermoid cyst.
FIGURE 3.
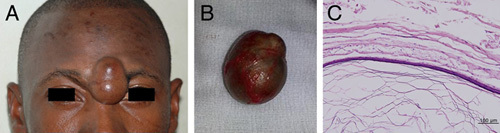
Epidermoid cyst in the glabellar area. (A) Preoperative clinical image. (B) Excised mass. (C) The cyst wall was lined with thin squamous epithelium on the luminal side. The cyst contained many keratin plugs but no growth of skin appendage tissue.
Mouth Floor
The sublingual spaces are separated from the submental and submandibular spaces by the mylohyoid muscle on the mouth floor. The surgical approach is determined according to the relative location of epidermoid and dermoid cysts to the mylohyoid muscle. A cystic lesion above the mylohyoid muscle, appearing as an intraoral mass, can be removed intraorally, while a lesion below the muscle, where chin swelling may occur, can be approached extraorally.14,24–26
A 16-year-old boy presented at Brong Ahafo Regional Hospital with submental swelling. A cystic mass was noted on the mouth floor. The cyst was enucleated without rupture through a submental incision using an extraoral approach (Fig. 4A, B). Histopathology of the surgical specimen revealed a flattened and nonproliferative epithelium lining and no features of hair follicles or sebaceous gland (Fig. 4C). The pathologic diagnosis was an epidermoid cyst.
FIGURE 4.

Epidermoid cyst in the mouth floor. (A) Preoperative clinical image. (B) Intraoperative clinical image. (C) The lining epithelium was flattened and nonproliferative, and there were no features consistent with hair follicles and sebaceous glands.
Buccal Mucosa
Epidermoid cysts are extremely rare in the buccal mucosa.21 Ten cases of epidermoid cysts arising in the buccal mucosa have been reported from 9 articles,21,27–34 and 11 cases, including those that are summarized in Supplemental Table 1 (Supplemental Digital Content 1, http://links.lww.com/SCS/F271). Patient ages ranged from 2 to 56 years, and most patients were in their 20s to 30s. Five patients were females and 6 were males. Three of the 11 cases had a trauma history. All lesions were surgically enucleated.
A 47-year-old man presented at the Department of Oral and Maxillofacial Surgery at Seoul National University Dental Hospital, Seoul, Korea, with swelling in the right lower cheek inside the oral cavity, just behind the commissure (Fig. 5A, B). Intraoral examination revealed a sessile, nonulcerated, smooth-surfaced, and normal-colored mass with well-defined margins. A CT scan revealed an ovoid, fluid-attenuated lesion surrounded by the orbicularis oris musculature and the buccinator muscle at the right mouth corner (Fig. 5D). The cystic mass was enucleated under local anesthesia (Fig. 5C). Upon microscopic examination, a cystic structure lined by a stratified squamous epithelium was identified in the muscle tissue. The epithelial lining contained a well-developed stratum granulosum, and the stratum corneum consisted of orthokeratin. Because skin appendages, such as sebaceous glands, sweat glands, or hair follicles, were not observed, the final histologic diagnosis was an intraoral epidermoid cyst (Fig. 6).
FIGURE 5.

Epidermoid cyst in the buccal mucosa. (A and B) Preoperative clinical images. (C) Intraoperative clinical image. (D) An axial CT image with a soft tissue window reveals an ovoid, fluid-attenuated lesion elevating the orbicularis oris musculature at the right mouth corner. CT indicates computed tomography.
FIGURE 6.
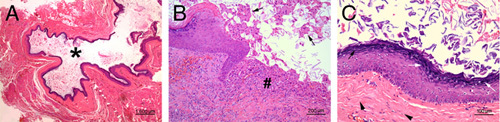
Representative histopathologic findings. (A) Epidermoid cyst denoting a keratin-filled cystic space (*) lined with thin epithelium in low magnification. (B) A portion of cyst epithelium was detached and ulcerated, producing many keratin plugs (arrows) and a subsequent granulomatous foreign body reaction (#). (C) In high magnification, the cyst epithelium was hyperkeratinized, and many superficial keratinocytes were exfoliated. The epithelium also showed similar features to the skin epithelium, exhibiting a thick granular cell layer (arrows) and cuboidal to columnar basal cells. Thick collagenous fibrous connective tissue (arrowheads) was found beneath the cyst epithelium where there was no lamina propria.
DISCUSSION
Epidermoid and dermoid cysts are benign developmental lesions that can be formed anywhere in the body. Although the lesions are rare in the head and neck area, they can occur at various craniofacial locations. Because the rarity of craniofacial epidermoid and dermoid cysts can cause diagnostic delays, clinicians should understand their features in their varied locations. Classification by anatomic location is helpful for diagnosis and treatment.5,6
Dermoid cysts at the midline area of the scalp are more likely to extend intracranially because they are located on a line of embryonic fusion. Due to their proximity to the sagittal suture, they have the capacity for intracranial or intradural extension.22,23 Extension into deeper tissue should be identified before surgical intervention, and preoperative imaging, such as CT or MRI, might be needed to rule out intracranial extension.6 However, dermoid cysts located in more lateral areas are rarely associated with intracranial extension.23
Epidermoid cysts in the temporal region have been rarely reported,35 and intradiploic epidermoid cysts of the temporal bone are uncommon.36 In rare cases, intradiploic epidermoid cysts in the temporal area can cause neurological symptoms and perforation of the skull.8 When an intracranial epithelial cyst is observed in the skull, an accurate radiological evaluation and complete removal of the cystic capsule are essential to obtain favorable results and avoid recurrence.8,11 Intradiploic epidermoid and dermoid cysts are observed as well-defined lytic lesions centered in the diploic space with or without sclerotic margins in the CT scan. To prevent intracranial complications after surgery, it is imperative to carefully dissect intradiploic epidermoid cysts from surrounding cranial bones and dura mater.36
Among 280 evaluated epidermoid and dermoid cysts in the periorbital and orbital area, 71% were periorbital and superficial, whereas 29% were orbital and deep.37 Approximately 3% of orbital dermoid cysts occur deep inside the orbit.38 Thus, it is necessary to determine whether the cystic mass is superficial or deep. Imaging studies are important to rule out both intracranial and intraorbital extension.11 Early operations are recommended to improve overall outcomes by restricting adjacent bone erosion and inflammatory response and to avoid complications.13,37
The mouth floor is the most common location for epidermoid and dermoid cysts in the oral cavity.34 As epidermoid and dermoid cysts of the mouth floor can displace the tongue, they can cause dyspnea or dysphagia.18–20 When the submental space inferior to the mylohyoid muscle is involved, a double chin may appear.25,39 Anatomic classification according to epidermoid and dermoid cyst relation to the muscles of the mouth floor helps surgeons to determine the surgical approach.14,24–26 In particular, the cyst’s relationship to the muscular planes is a decisive factor. Because epidermoid and dermoid cysts do not involve the sublingual gland, gland extirpation should be avoided, unlike that with ranula.39,40
Epidermoid cysts arising in the buccal mucosa are extremely rare, and they should be considered in differential diagnoses of swellings in the buccal mucosa. Surgical excision of epidermoid and dermoid cysts after pathologic confirmation is the treatment of choice.1,4,8,21 Caution should be taken not to rupture the cyst because contents act as irritants to fibrovascular tissues, causing postoperative inflammation.
Epidermoid and dermoid cysts rarely undergo malignant transformation. However, transformation potential should not be ignored because malignant changes of epidermoid and dermoid cysts in the craniofacial area have been reported in the cranium,41–43 orbital area,44 and mouth floor,45 and all had bad prognoses.
CONCLUSIONS
Although epidermoid and dermoid cysts are rare, they can present in a variety of craniofacial locations. Classification by location is helpful for diagnosis and treatment. Despite benign pathology, epidermoid and dermoid cysts can invade adjacent structures. Clinical features of the cysts according to anatomic location should be considered. Epidermoid and dermoid cysts should be included in the differential diagnosis of cystic lesions in the craniofacial region.
Supplementary Material
ACKNOWLEDGMENTS
The authors thank Professor Suk Keun Lee in the Institute of Hydrogen Magnetic Reaction Gene Regulation for his pathologic diagnosis and consultations.
Footnotes
This study was supported by grant no 03-2019-0043 from the SNUDH Research Fund and the National Research Foundation of Korea grant funded by the Korean government (2022R1F1A1069624).
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional Review Board (S-D20200022) at Seoul National University and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Written informed consent was obtained from all individual participants included in the study for publication of this manuscript and any accompanying images.
H.J.O.: analyzed the literature and wrote the manuscript. M.Y.E.: collected the literature data. B.S.I.: drafted the article. E.K.A.: described the case in the buccal mucosa. P.F.: described the case in the temporal intradiploic area. H.M.: designed the article. S.M.K.: prepared the figures and wrote the manuscript.
The authors report no conflicts of interest.
Supplemental Digital Content is available for this article. Direct URL citations are provided in the HTML and PDF versions of this article on the journal's website, www.jcraniofacialsurgery.com.
Contributor Information
Hyun Jun Oh, Email: victor.oh@snu.ac.kr.
Mi Young Eo, Email: miyoungeo@snu.ac.kr.
Buyanbileg Sodnom-Ish, Email: buyanbilegso@gmail.com.
Emmanuel Kofi Amponsah, Email: ampek2003@yahoo.co.uk.
Paul Frimpong, Email: frimpongpaul@ymail.com.
Hoon Myoung, Email: myoungh@snu.ac.kr.
Soung Min Kim, Email: smin5@snu.ac.kr.
REFERENCES
- 1. Santos HB, Rolim LS, Barros CC, et al. Dermoid and epidermoid cysts of the oral cavity: a 48-year retrospective study with focus on clinical and morphological features and review of main topics. Med Oral Patol Oral Cir Bucal 2020;25:e364–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Dutta M, Saha J, Biswas G, et al. Epidermoid cysts in head and neck: our experiences, with review of literature. Indian J Otolaryngol Head Neck Surg 2013;65:14–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Al-Khateeb TH, Al-Masri NM, Al-Zoubi F. Cutaneous cysts of the head and neck. J Oral Maxillofac Surg 2009;67:52–7 [DOI] [PubMed] [Google Scholar]
- 4. Pupic-Bakrac J, Pupic-Bakrac A, Bacic I, et al. Epidermoid and dermoid cysts of the head and neck. J Craniofac Surg 2021;32:e25–7 [DOI] [PubMed] [Google Scholar]
- 5. Vega RA, Hidlay DT, Tye GW, et al. Intradiploic dermoid cyst of the lateral frontotemporal skull: case report and review of the literature. Pediatr Neurosurg 2013;49:232–5 [DOI] [PubMed] [Google Scholar]
- 6. Golden BA, Jaskolka MS, Ruiz RL. Craniofacial and orbital dermoids in children. Oral Maxillofac Surg Clin North Am 2012;24:417–25 [DOI] [PubMed] [Google Scholar]
- 7. Prior A, Anania P, Pacetti M, et al. Dermoid and epidermoid cysts of scalp: case series of 234 consecutive patients. World Neurosurg 2018;120:119–24 [DOI] [PubMed] [Google Scholar]
- 8. Kim CS, Yoon SH, Oh JW, et al. Epidermoid cyst in temple area with skull perforation. Arch Craniofac Surg 2020;21:137–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Overland J, Hall C, Holmes A, et al. Risk of intracranial extension of craniofacial dermoid cysts. Plast Reconstr Surg 2020;145:779e–87e [DOI] [PubMed] [Google Scholar]
- 10. Lacey M, Gear AJ, Lee A. Temporal dermoids: three cases and a modified treatment algorithm. Ann Plast Surg 2003;51:103–9 [DOI] [PubMed] [Google Scholar]
- 11. Pryor SG, Lewis JE, Weaver AL, et al. Pediatric dermoid cysts of the head and neck. Otolaryngol Head Neck Surg 2005;132:938–42 [DOI] [PubMed] [Google Scholar]
- 12. Bonavolonta G, Strianese D, Grassi P, et al. An analysis of 2,480 space-occupying lesions of the orbit from 1976 to 2011. Ophthalmic Plast Reconstr Surg 2013;29:79–86 [DOI] [PubMed] [Google Scholar]
- 13. Celik T. Glabellar dermoid cyst: a case presentation. Ophthalmic Genet 2016;37:331–2 [DOI] [PubMed] [Google Scholar]
- 14. Teszler CB, El-Naaj IA, Emodi O, et al. Dermoid cysts of the lateral floor of the mouth: a comprehensive anatomo-surgical classification of cysts of the oral floor. J Oral Maxillofac Surg 2007;65:327–32 [DOI] [PubMed] [Google Scholar]
- 15. Ohta N, Watanabe T, Ito T, et al. A case of sublingual dermoid cyst: extending the limits of the oral approach. Case Rep Otolaryngol 2012;2012:634949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mohta A, Sharma M. Congenital oral cysts in neonates: report of two cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006;102:e36–8 [DOI] [PubMed] [Google Scholar]
- 17. De Ponte FS, Brunelli A, Marchetti E, et al. Sublingual epidermoid cyst. J Craniofac Surg 2002;13:308–10 [DOI] [PubMed] [Google Scholar]
- 18. Derin S, Koseoglu S, Sahan L, et al. Giant dermoid cyst causing dysphagia and dyspnea. J Craniofac Surg 2016;27:e260–1 [DOI] [PubMed] [Google Scholar]
- 19. Pirgousis P, Fernandes R. Giant submental dermoid cysts with near total obstruction of the oral cavity: report of 2 cases. J Oral Maxillofac Surg 2011;69:532–5 [DOI] [PubMed] [Google Scholar]
- 20. Banerjee N, Padhiary SK, Chattopadhyay A, et al. A huge epidermoid cyst endangering life. J Maxillofac Oral Surg 2011;10:246–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Dammak N, Chokri A, Slim A, et al. Epidermoid cyst of the buccal mucosa-An uncommon entity: Case report and literature review. Clin Case Rep 2021;9:e04853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sorenson EP, Powel JE, Rozzelle CJ, et al. Scalp dermoids: a review of their anatomy, diagnosis, and treatment. Childs Nerv Syst 2013;29:375–80 [DOI] [PubMed] [Google Scholar]
- 23. Wood J, Couture D, David LR. Midline dermoid cyst resulting in frontal bone erosion. J Craniofac Surg 2012;23:131–4 [DOI] [PubMed] [Google Scholar]
- 24. Mirza S, Fadl S, Napaki S, et al. Case report of complicated epidermoid cyst of the floor of the mouth: Radiology-histopathology correlation. Qatar Med J 2014;2014:12–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Longo F, Maremonti P, Mangone GM, et al. Midline (dermoid) cysts of the floor of the mouth: report of 16 cases and review of surgical techniques. Plast Reconstr Surg 2003;112:1560–5 [DOI] [PubMed] [Google Scholar]
- 26. Fuchshuber S, Grevers G, Issing WJ. Dermoid cyst of the floor of the mouth—a case report. Eur Arch Otorhinolaryngol 2002;259:60–2 [DOI] [PubMed] [Google Scholar]
- 27. Schneider LC, Mesa ML. Epidermoid cysts of the buccal mucosa. Q Natl Dent Assoc 1978;36:39–42 [PubMed] [Google Scholar]
- 28. Gutmann J, Cifuentes C, Gandulfo P, et al. Intradermal nevus associated with epidermoid cyst in the mucous membrane of the cheek. Oral Surg Oral Med Oral Pathol 1978;45:76–82 [DOI] [PubMed] [Google Scholar]
- 29. Rajayogeswaran V, Eveson JW. Epidermoid cyst of the buccal mucosa. Oral Surg Oral Med Oral Pathol 1989;67:181–4 [DOI] [PubMed] [Google Scholar]
- 30. Ozan F, Polat HB, Ay S, et al. Epidermoid cyst of the buccal mucosa: a case report. J Contemp Dent Pract 2007;8:90–6 [PubMed] [Google Scholar]
- 31. Kini YK, Kharkar VR, Rudagi BM, et al. An unusual occurrence of epidermoid cyst in the buccal mucosa: a case report with review of literature. J Maxillofac Oral Surg 2013;12:90–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Costa FW, Carvalho FS, Chaves FN, et al. Epidermoid cyst arising in the buccal mucosa: case report and literature review. Acta Stomatol Croat 2015;49:65–73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Srivastava AN, Gupta P, Siddiqui A, et al. An unusual occurrence of multiple epidermoid cysts in both sides of buccal mucosa: a unique and rare first case report. Natl J Maxillofac Surg 2015;6:244–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Rohde RL, Costa DJ, Brinkmeier JV. Epidermoid Cyst of the buccal space in a pediatric patient-a rare clinic report. Ear Nose Throat J 2021;100:525S–7S [DOI] [PubMed] [Google Scholar]
- 35. Boffano P, Roccia F, Campisi P, et al. Epidermoid cyst of the temporal region. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2011;112:e113–6 [DOI] [PubMed] [Google Scholar]
- 36. Lee DH. Intradiploic epidermoid cyst of the temporal bone: is it the same as or different from cholesteatoma? J Craniofac Surg 2011;22:1973–5 [DOI] [PubMed] [Google Scholar]
- 37. Pushker N, Meel R, Kumar A, et al. Orbital and periorbital dermoid/epidermoid cyst: a series of 280 cases and a brief review. Can J Ophthalmol 2020;55:167–71 [DOI] [PubMed] [Google Scholar]
- 38. Wagh VK, Lam KC, Morley AMS. Orbital dermoid masquerading as allergic lid swelling. Can J Ophthalmol 2016;51:e143–7 [DOI] [PubMed] [Google Scholar]
- 39. Misch E, Kashiwazaki R, Lovell MA, et al. Pediatric sublingual dermoid and epidermoid cysts: a 20-year institutional review. Int J Pediatr Otorhinolaryngol 2020;138:110265 [DOI] [PubMed] [Google Scholar]
- 40. Gordon PE, Faquin WC, Lahey E, et al. Floor-of-mouth dermoid cysts: report of 3 variants and a suggested change in terminology. J Oral Maxillofac Surg 2013;71:1034–41 [DOI] [PubMed] [Google Scholar]
- 41. Faltaous AA, Leigh EC, Ray P, et al. A rare transformation of epidermoid cyst into squamous cell carcinoma: a case report with literature review. Am J Case Rep 2019;20:1141–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Solanki SP, Maccormac O, Dow GR, et al. Malignant transformation of residual posterior fossa epidermoid cyst to squamous cell carcinoma. Br J Neurosurg 2017;31:497–8 [DOI] [PubMed] [Google Scholar]
- 43. Chon KH, Lee JM, Koh EJ, et al. Malignant transformation of an epidermoid cyst in the cerebellopontine angle. J Korean Neurosurg Soc 2012;52:148–51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Concepcion-Torio K, Park JW, Woo KI, et al. Pilosebaceous malignant transformation of dermoid cyst in the orbit. Ophthalmic Plast Reconstr Surg 2020;36:e103–5 [DOI] [PubMed] [Google Scholar]
- 45. Devine JC, Jones DC. Carcinomatous transformation of a sublingual dermoid cyst. A case report. Int J Oral Maxillofac Surg 2000;29:126–7 [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


