A 64-year-old woman with a past medical history of poorly controlled diabetes, morbid obesity, hypertension, and status post-oncological treatment for metastatic sigmoid colon cancer was admitted to the surgery department due to a 50 × 40 × 43-mm abscess in the right kidney on computed tomography (CT) ( Fig. 1 ). The abscess penetrated the gallbladder, causing its perforation. It also penetrated the liver and was causing renal artery infiltration with pseudoaneurysm formation (21 mm and 16 mm in diameter) ( Fig. 2 ). The patient was clinically and biochemically septic. CT ruled out other sites of abscess. Due to significant associated co-morbidities, poor general status, and poor percutaneous access, neither a standard surgical intervention nor percutaneous drainage was feasible.
Fig. 1.
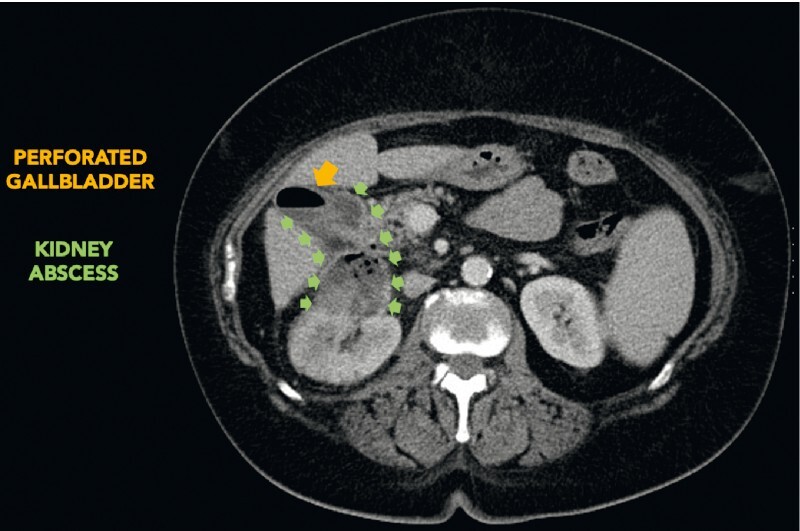
The 50 × 40 × 43-mm abscess in the right kidney, penetrating into the gallbladder causing its perforation.
Fig. 2.
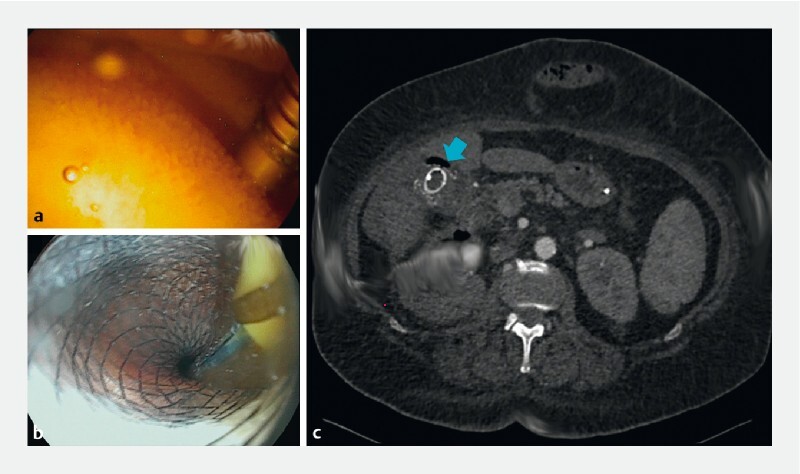
Endoscopic ultrasound-guided lumen-apposing metal stent (20 mm × 16 mm) placement for left kidney drainage through the gallbladder, followed by nasogastric tube placement.
As there was a connection between the kidney abscess and perforated gallbladder, endoscopic ultrasound (EUS)-guided drainage was performed under general anesthesia using a linear echoendoscope ( Video 1 ). Through transduodenal access after endosonographic visualization of the gallbladder, fine-needle aspiration (FNA) with a 19G FNA needle was performed. The aspired purulent content mixed with bile of the gallbladder confirmed the position. A 0.035-inch guidewire was advanced through the needle and looped in the abscess cavity under X-ray control. Then, the tract was dilated with a 10-Fr cystotome, followed by placement of a 20 × 16-mm cautery-enhanced lumen-apposing metal stent (LAMS). Immediately, purulent content outflow was observed from the stent lumen. The procedure was concluded with placement of a 7-Fr nasogastric tube through the LAMS lumen for active abscess lavage (50 ml of saline every 6 hours).
Video 1 Endoscopic ultrasound-guided drainage of a complex kidney abscess through perforated gallbladder using lumen-apposing metal stent with double pigtail.
After 3 weeks of active transmural drainage, symptoms resolved and laboratory parameters normalized. CT showed a collection decrease to 3 mm, given that the nasogastric tube was replaced with a 7-Fr × 7-cm double-pigtail stent. The patient was discharged and followed up in outpatient settings. After 5 months, CT showed a collection size of 21 × 10 mm (decrease> 50 %) and a healed gallbladder wall during follow-up endoscopic assessment ( Fig. 3 ). One year after the procedure, the patient remains asymptomatic, without collection, on LAMS stent and permanent double-pigtail drainage to prevent recurrence ( Fig. 4 ).
Fig. 3.
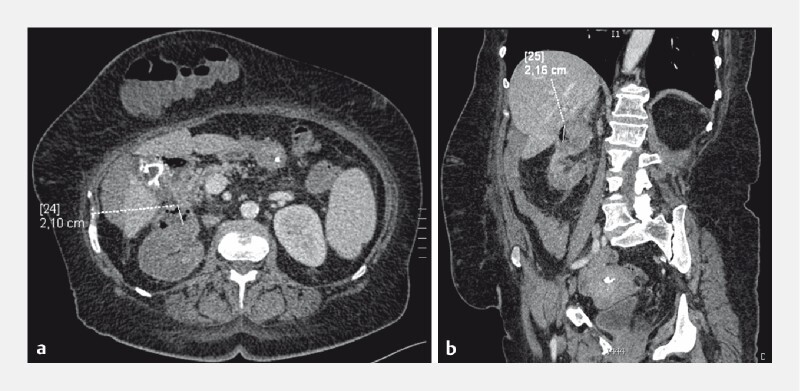
Computed tomography performed 5 months after the procedure: successful endoscopic treatment (collection size 21 × 10 mm; decrement > 50 %).
Fig. 4.
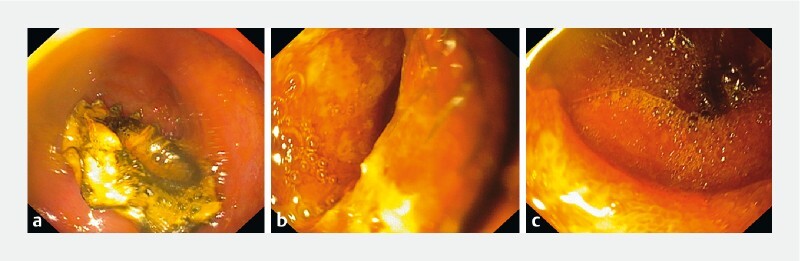
Surveillance esophagogastroduodenoscopy 12 months after the procedure: healed gallbladder wall; patient remains asymptomatic.
This case is important for three reasons. First, we show how a complex kidney abscess penetrating the gallbladder and liver can be successfully managed endoscopically. Second, EUS-guided drainage of a peritoneal cavity abscess might be an optimal alternative therapy for patients with multiple comorbidities, at high risk for life-threatening recurrent sepsis, and are poor surgical candidates. Lastly, similar to the management of other types of recurrent collections, long-term transmural drainage with an indwelling double-pigtail plastic stent seems to be an option for this group of patients 1 .
Endoscopy_UCTN_Code_CCL_1AF_2AZ_3AD
Footnotes
Competing interests The authors declare that they have no conflict of interest.
Endoscopy E-Videos : https://eref.thieme.de/e-videos .
E-Videos is an open access online section of the journal Endoscopy , reporting on interesting cases and new techniques in gastroenterological endoscopy. All papers include a high-quality video and are published with a Creative Commons CC-BY license. Endoscopy E-Videos qualify for HINARI discounts and waivers and eligibility is automatically checked during the submission process. We grant 100% waivers to articles whose corresponding authors are based in Group A countries and 50% waivers to those who are based in Group B countries as classified by Research4Life (see: https://www.research4life.org/access/eligibility/ ). This section has its own submission website at https://mc.manuscriptcentral.com/e-videos
Reference
- 1.Gkolfakis P, Bourguignon A, Arvanitakis M et al. Indwelling double-pigtail plastic stents for treating disconnected pancreatic duct syndrome-associated peripancreatic fluid collections: long-term safety and efficacy. Endoscopy. 2021;53:1141–1149. doi: 10.1055/a-1319-5093. [DOI] [PubMed] [Google Scholar]


