Abstract
Cardiac rhabdomyoma is a rare benign tumor of the pediatric age group which usually regresses by the age of 2 years. Cardiac rhabdomyoma in adults is still a rarer disease. It is usually associated with tuberous sclerosis. Patients with cardiac rhabdomyoma will usually be asymptomatic and detected incidentally, or in suspicion to the signs and symptoms of tuberous sclerosis. Symptomatic patients present with palpitations or failure to thrive due to obstructive symptoms leading to cardiac failure. The authors present a rare case of right ventricular rhabdomyoma in an adult without tuberous sclerosis treated surgically.
Keywords: Rhabdomyoma, Tuberous sclerosis, Transesophageal echocardiography
Introduction
Rhabdomyomas are benign mesenchymal tumors commonly involving the extremities, head, and neck [1]. Cardiac rhabdomyoma is a type of hamartoma of striated muscle origin. Primary cardiac tumors are extremely rare, and the reported prevalence is between 0.0017 and 0.028% [2]. Cardiac rhabdomyomas are the most common cardiac tumor in children (45%) [3]. They occur in 70 to 90% of children with tuberous sclerosis (TSC). Cardiac rhabdomyoma commonly regresses spontaneously within 2 years of age and is thus extremely rare in adults [4].
Case report
A 23-year-old male presented with complaints of chest pain and palpitations and with occasional syncopal attacks (4–5 episodes) of less than a minute duration on exertion, which were relieved by taking rest, for the last 2 years. He had normal mentation with no history of epilepsy. There was no family history of skin-related complaints or malignancy-related death. His physical examination was unremarkable except for tachycardia of 160 beats/min, regular, normal volume pulse with no radio-radial or radio-femoral delay. Blood investigations were normal except for raised C-reactive protein (CRP) levels > 20 mg/l on many occasions. Chest X-ray was unremarkable with a normal cardiothoracic (CT) ratio. Electrocardiogram (ECG) showed sinus tachycardia with a heart rate of 146/min with occasional ventricular ectopic. Screening thoracic echocardiography (TTE) suggested a space-occupying lesion in the right ventricle without any obstruction to the right ventricular outflow tract (RVOT) or tricuspid valve (TV) leaflet motion. Cardiac magnetic resonance imaging (MRI) showed a well-defined mass of size 7 × 7 cm seen in the lateral wall protruding into the right ventricular (RV) cavity (Fig. 1). The patient was planned for resection of the mass with the support of cardiopulmonary bypass (CPB) with adequate blood reserve.
Fig. 1.
Hypodense globular mass embedded in the right ventricular myocardium
With standard monitoring, under general anaesthesia, intraoperative transesophageal echocardiography (TEE) was done which showed well-defined nodular homogenous hyperechoic mass present in the anterolateral wall of RV, embedded in the myocardium, and protruding into the RV cavity, almost obliterating the RV cavity during systole without causing intracavitary obstruction during diastole. The RVOT was spared (Fig. 2).
Fig. 2.
Mid oesophagal 4 chamber and mid oesophagal right ventricular inflow-outflow views showing hyperechoic mass present in the anterolateral wall of the right ventricle with sparing of the outflow tract
After median sternotomy, followed by pericardiotomy, aortic cannulation and single-stage venous cannulation were done for both the superior vena cava and inferior vena cava. Cardiopulmonary bypass was initiated with moderate hypothermia and cold antegrade cardioplegia was given in the aortic root and diastolic cardiac arrest was achieved. The heart was enlarged with a bosselated appearance of an RV anterolateral wall (Fig. 3). The mass was approached through the incision on the RV epicardium directly above it. It was a sessile well-circumscribed multiple nodular mass without any capsule present, embedded in the myocardium and adhered to the surrounding tissues up to the endocardium. The tumor was resected from the surrounding myocardium with fine dissection and by maintaining gentle traction. Myocardial incision was closed using Poly Tetra Fluro Ethylene (PTFE) felt patches to prevent the tearing of the heart tissue and to provide additional seal and protection (Fig. 4). Intraoperative period was uneventful and safe de-cannulation was done. Post CPB, the patient did not have any conduction blocks but had occasional ventricular ectopics.
Fig. 3.
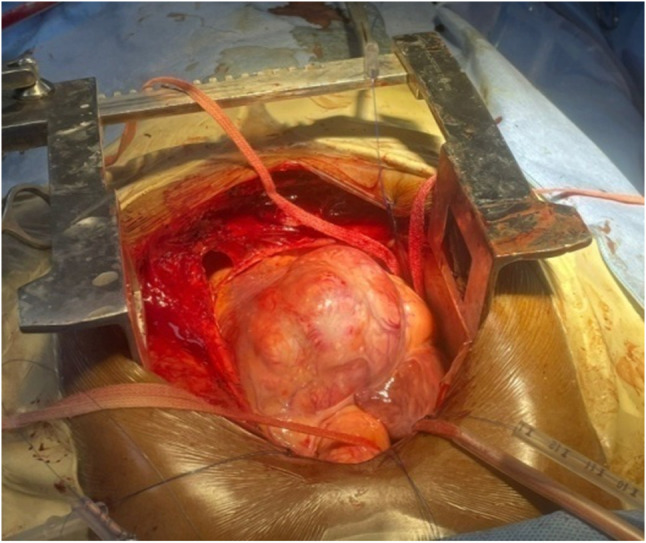
Bosselated appearance of the right ventricular surface due to underlying tumor
Fig. 4.
(From left to right) Delivering the tumor en masse with controlled traction, repair done with Poly Tetra Fluro Ethylene felt patches
Histopathological examination showed a mixture of spindle-shaped cells with abundant cytoplasm with scattered cytoplasmic vacuoles with no atypia, myofibrils radiating to the cell wall and occasional myocytes observed in the periphery of the tumor, features suggestive of benign rhabdomyoma (Fig. 5).
Fig. 5.
a Cross section of the resected right ventricular mass. b Microscopic: Large vacuolated cells with abundant glycogen
In the postoperative period, patient developed ventricular arrhythmias, which were not controlled by pharmacological means; hence, there was a need for an automatic implantable cardiac defibrillator (AICD) (Fortify Assura™ ICD with Durata™ defibrillator lead). No other postoperative complications were observed. The patient was followed for 1 year postoperatively and was found to have no syncopal attacks or palpitations.
Discussion
Rhabdomyomas are rare benign cardiac masses arising from striated muscle. Anatomically, they come under hamartomas and may be present in any cardiac chamber. Most of the tumors present within 1st year of age with an association with tuberous sclerosis. The incidence of tuberous sclerosis is 1/5000–10,000 live births [5]. 70–90% of tuberous sclerosis patients will have cardiac rhabdomyoma. Tuberous sclerosis is an autosomal dominant neurocutaneous disorder with associated tumors in the brain, heart, kidneys, and skin. TSC is usually presented as intractable epilepsy, mental retardation, adenoma sebaceum (Vogt triad), Shagreen patches, etc. [6]. They are usually well-circumscribed multiple nodules present within the myocardium. Pedunculation and myocardial embedding are occasional features of rhabdomyoma.
Cardiac rhabdomyomas are usually asymptomatic which are found incidentally or found in suspicion when other signs and symptoms of TSC are present. Symptoms when present are usually palpitations (arrhythmias) or heart failure (due to obstruction of chambers) which may lead to sudden death. The rhabdomyomas regress spontaneously, and hence, the outcome is usually favorable. Serial echocardiographic follow-up is warranted. The association of rhabdomyoma with TSC makes the outcome unfavorable, and it depends on several factors such as the extent of the organs involved and response to the treatment. Of the diagnosed cases of tuberous sclerosis, 30% of patients die before the age of 5 years [7]. Surgery is reserved for symptomatic patients [8].
Sporadic adult cardiac rhabdomyoma is extremely rare. There are few case reports of adult cardiac rhabdomyoma associated with TSC [4]. This patient had palpitations and chest discomfort without any signs, symptoms, and family history suggestive of TSC or other genetical perturbation. The occurrence of palpitations and syncope may be due to the involvement of the cardiac conducting system. Echocardiography is a good modality of diagnosis and provides temporal resolution, but is observer-dependent, while MRI is best for tumor characterization [9]. This patient was taken for upfront surgical management as the symptomatic rhabdomyoma, in the form of arrhythmias or congestive cardiac failure, has a proclivity for sudden death [10].
The development of intractable ventricular arrhythmia in the postoperative period may also be due to the disruption of the conducting system while excising the tumor. As there was an absence of a reversible cause for the development of intractable post-cardiac surgery ventricular arrhythmia, AICD was placed.
Conclusion
Cardiac rhabdomyomas are usually present in childhood and are associated with tuberous sclerosis. They usually regress. When asymptomatic, serial ECG and echocardiography should be done to know the progression of the disease. A thorough search for the signs and symptoms of tuberous sclerosis should be made. Sporadic cases of rhabdomyoma presenting in adulthood without tuberous sclerosis are extremely rare. Surgery is recommended for symptomatic patients only.
Funding
None.
Data Availability
All data underlying the results are available as a part of the article and no additional source data are required.
Declarations
Ethics committee approval
Not applicable.
Informed consent
Taken.
Conflict of interest
None.
Human and animal rights statement
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Akash, Email: akki2015om@gmail.com.
Pavan Kumar Dammalapati, Email: heartdrpavan@gmail.com.
References
- 1.Hansen T, Katenkamp D. Rhabdomyoma of the head and neck: morphology and differential diagnosis. Virchows Arch. 2005;447:849–854. doi: 10.1007/s00428-005-0038-8. [DOI] [PubMed] [Google Scholar]
- 2.Patel J, Sheppard MN. Pathological study of primary cardiac and pericardial tumours in a specialist UK Centre: surgical and autopsy series. Cardiovasc Pathol. 2010;19:343–352. doi: 10.1016/j.carpath.2009.07.005. [DOI] [PubMed] [Google Scholar]
- 3.Freedom RM, Lee KJ, MacDonald C, Taylor G. Selected aspects of cardiac tumors in infancy and childhood. Pediatr Cardiol. 2000;21:299–316. doi: 10.1007/s002460010070. [DOI] [PubMed] [Google Scholar]
- 4.Ghosh S, Milunski MR. Cardiac rhabdomyoma in adult. Cureus. 2021;13:e14565. doi: 10.7759/cureus.14565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mahadevappa M, Patil V, Poornima KS, Velamala S, Guruprasad BV. Two cases of tuberous sclerosis with multiple rhabdomyoma succumbing to sudden cardiac death. Indian J Clin Cardiol. 2021;2:151–157. doi: 10.1177/26324636211012485. [DOI] [Google Scholar]
- 6.Sciacca P, Giacchi V, Mattia C, Greco F, Smilari P, Betta P, et al. Rhabdomyomas and tuberous sclerosis complex: our experience in 33 cases. BMC Cardiovasc Disord. 2014;14:66. doi: 10.1186/1471-2261-14-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ajay V, Singhal V, Venkateshwarlu V, Rajesh SM. Tuberous sclerosis with rhabdomyoma. Indian J Hum Genet. 2013;19:93–95. doi: 10.4103/0971-6866.112912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tyebally S, Chen D, Bhattacharyya S, Mughrabi A, Hussain Z, Manisty C, et al. Cardiac tumors: JACC CardioOncology state-of-the-art review. JACC CardioOncol. 2020;2:293–311. doi: 10.1016/j.jaccao.2020.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Travis WD, Brambilla E, Nicholson AG, Yatabe Y, Austin JHM, Beasley MB, et al. The 2015 World Health Organization classification of lung tumors: impact of genetic, clinical and radiologic advances since the 2004 Classification. J Thorac Oncol. 2015;10:1243–1260. doi: 10.1097/JTO.0000000000000630. [DOI] [PubMed] [Google Scholar]
- 10.Yinon Y, Chitayat D, Blaser S, Seed M, Amsalem H, Yoo SJ, et al. Fetal cardiac tumors: a single-center experience of 40 cases. Prenat Diagn. 2010;30:941–949. doi: 10.1002/pd.2590. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data underlying the results are available as a part of the article and no additional source data are required.






