Abstract
Background
Exercise-induced compartment syndrome is a condition characterized by elevated pressure within a muscle compartment, resulting from repetitive loading or participation in sports activities. Primarily affecting the medial compartment of the foot, this rare condition manifests as sudden-onset pain in the medial aspect of the foot, without a discernible history of trauma, occurring during or after physical exertion. Diagnosis is primarily clinical in nature, as diagnostic imaging techniques provide limited utility.
Conclusions
Exercise-induced compartment syndrome is a rare syndrome with prolonged implications such as contractures, claw toes, muscle weakness, and sensory neuropathy. Hence, it is imperative for orthopedic surgeons to be familiar with this condition in order to facilitate timely diagnosis and treatment.
Keywords: Compartment syndrome, Foot, Exercise-induced, Surgical management
Introduction
Foot compartment syndrome is an infrequent condition primarily attributed to crush injuries, although it can also arise from other less common causes such as burns, vascular injuries, vigorous exercise, surgical procedures, and fractures. It occurs when there is an elevation in pressure within a muscle compartment, leading to reduced vascular perfusion and subsequent tissue ischemia, ultimately resulting in irreversible muscle damage. In exercise-induced compartment syndrome, the medial plantar compartment is typically the most affected. This compartment comprises the abductor hallucis muscles, flexor hallucis brevis muscle, large flexor tendon of the digits, long peroneal tendon, as well as the medial plantar vein, nerve, and artery [1].
The clinical presentation of foot compartment syndrome typically includes moderate to severe pain, accompanied by an inability to bear weight or walk. In more severe cases, symptoms may be accompanied by paresthesias, pallor, and absence of pulses. Differential diagnoses encompass plantar fasciitis, tarsal tunnel syndrome, and adult flatfoot. The diagnostic utility of radiological imaging is limited, thus emphasizing the primary reliance on clinical assessment for diagnosis. Measurement of pressure within the affected compartment can aid in confirming the diagnosis. Initially, plain X-ray imaging is valuable for ruling out associated fractures. Magnetic resonance imaging (MRI) can identify soft tissue edema and is particularly useful when trauma is not evident [2]. Acute cases typically require surgical intervention, such as fasciotomy of the affected compartment. This condition commonly affects young athletes, and failure to promptly address it can result in significant functional consequences. Therefore, we present the case of a 30-year-old patient who developed this condition following physical activity.
Statement of informed consent
The patient consented the use of his medical records, as well as diagnostic images, for this case report.
Case report
A 30-year-old male patient presented to the emergency department with a 24-h history of pain in the medial aspect of his left foot, which commenced following a basketball game. The patient denied any evident trauma to the affected area. The pain was constant and did not alleviate with oral analgesics or rest. Physical examination revealed edema and swelling on the medial aspect of the foot, accompanied by tenderness upon palpation, although no signs of inflammation were observed (Fig. 1). The patient experienced pain during flexion, extension, and abduction of the hallux, while the neurovascular examination demonstrated normal findings, including symmetrical pulses and intact sensation.
Fig. 1.
Patient's foot in the ER.
The foot X-ray revealed soft tissue edema on the medial aspect of the foot, without any fractures or other abnormalities. Given the severity of the pain and the absence of a definitive diagnosis, a plain MRI of the left foot was performed, which revealed diffuse edema of the abductor hallucis muscle without any disruption in its continuity (Fig. 2). By that time, the patient had experienced pain relief with intravenous analgesics, and he was discharged with a diagnosis of traumatic myositis. The treatment plan included restricted weight-bearing, utilization of a Walker boot, oral analgesics, and a scheduled outpatient follow-up appointment in one week.
Fig. 2.
a) Sagittal, b) coronal, and c) axial MRI image where the hallux abductor muscle can be seen with changes in its intensity.
Six hours after being discharged, the patient returned to the emergency room reporting severe pain rated at 10/10 on the visual analogue scale, despite following the previous recommendations. Subsequently, a medical consultation was conducted, and the MRI images were reviewed by a specialized radiologist in musculoskeletal imaging. The updated radiology report revealed an increase in volume and signal intensity of the abductor hallucis muscle, along with indistinct, slightly hyperintense areas on T1-weighted images suggestive of edema or hematoma. Additionally, a small muscle hernia measuring 6.7 mm was observed at the lower margin of the muscle. An orthopedic department meeting, involving both a trauma specialist and a foot and ankle specialist, was convened, leading to the consideration of compartment syndrome in the medial compartment of the foot. Urgent surgical intervention in the form of fasciotomy was performed.
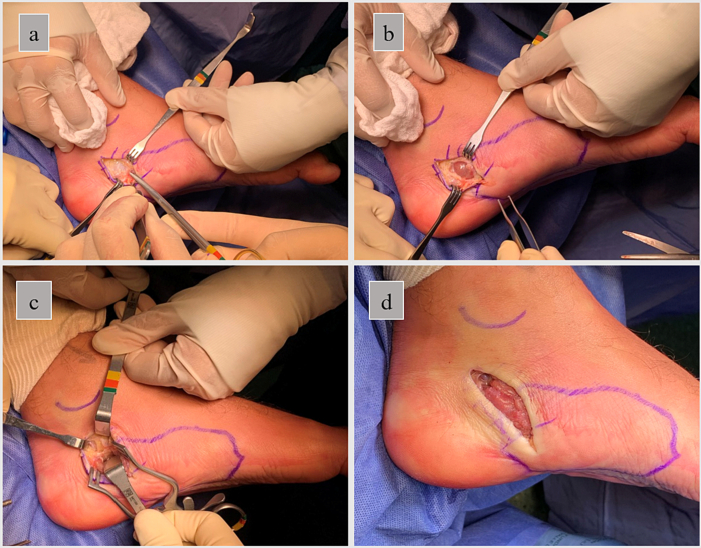
Under general anesthesia and in the supine position, a 5 cm oblique incision was made over the most proximal region of the medial compartment of the foot. The dissection proceeded through the appropriate planes until reaching the superficial fascia, which was incised along the same line as the skin incision. Subsequently, the abductor hallucis muscle, which appeared significantly pale but still retained contractility, was visualized and mobilized towards the plantar aspect of the foot. The deep fascia was also incised using the same approach. By the conclusion of the surgery, the muscle had regained its normal coloration, and the wound was closed using individual prolene sutures (Fig. 3). Following the fasciotomy, the patient experienced complete resolution of pain and was discharged with the utilization of a Walker boot one day later. Weekly follow-up appointments were conducted for the next two weeks, during which adequate wound healing and pain-free gait with gradually increasing weight bearing were observed. Three months post-surgery, the patient resumed his sports activities without any residual symptoms.
Fig. 3.
a) Surgical approach and exposition of the superficial fascia. b) Exposition of the hallux abductor muscle. c) Access and identification of the Deep fascia. d) End result.
Discussion
Exercise-induced compartment syndrome in the foot is a rare condition, and the available literature documenting such cases is limited. As of the writing of this article, few case reports have been identified [[1], [2], [3], [4], [5], [6], [7], [8], [9], [10]]. This report represents the first documented case of exercise-induced compartment syndrome in Colombia. In our case, the time elapsed between the initial visit to the emergency department and the surgical intervention was 48 h, which falls within the range reported in other studies, ranging from 19 h to 8 months [2,3,5]. It is worth noting that the latter study described a patient with a chronic presentation of this condition.
The diagnosis of exercise-induced compartment syndrome in the foot is challenging due to the variability in clinical presentations, ranging from acute pain to chronic and intermittent pain associated with exercise. Furthermore, unlike traumatic compartment syndrome, there is typically no neurovascular compromise evident during physical examination. The characteristic sign is the presence of tense and painful edema over the medial compartment of the foot. The gold standard for diagnosis is the measurement of intracompartmental pressure exceeding 30 mmHg. Unfortunately, intracompartmental pressure (ICP) measuring devices are not readily available in Colombia, and thus the diagnosis relies on clinical presentation and imaging findings.
One of the first methods of ICP measurement consists of a needle introduced into the compartment and connected to a column filled partly with saline and partly with air. ICP is measured with an attached manometer to inject air into the tubing and flatten the meniscus between saline and the air. Other methods of non-invasive pressure measurement of the compartment are being developed; the most researched methods include quantitative measurement of tissue hardness, measurement of local oxygenation by reflection of radiation in the near part of the infrared spectrum, and the use of ultrasound [11].
It is important to note that delayed treatment can lead to significant sequelae, as demonstrated in the case reported by Park et al., where an 8-day delay in surgical intervention resulted in hypoesthesia in the medial foot region and a flexion deformity of the hallux [2]. Therefore, this case report aims to raise awareness among orthopedic surgeons practicing in developing countries, emphasizing the importance of clinical and imaging-based diagnosis to reduce diagnostic delays and enable timely treatment. Additionally, we provide a detailed account of the surgical procedure as a guide for specialists performing this surgery for the first time.
Conclusion
Although exercise-induced foot compartment syndrome is considered a rare condition, it should always be considered in cases of acute or chronic foot pain. The typical clinical presentation involves tense and painful edema in the medial compartment of the foot. Diagnosis can be confirmed through measurement of compartment pressure, if measurement of the compartment pressure isn't available, diagnosis should be made clinically. Prompt management is crucial to prevent potential complications or sequelae.
Declaration of competing interest
Authors state no conflicts of interest.
References
- 1.Blacklidge D.K., Kurek J.B., Soto A.D., Kissel C.G. Acute exertional compartment syndrome of the medial foot. J. Foot Ankle Surg. 1996;35(1):19–22. doi: 10.1016/s1067-2516(96)80007-x. [DOI] [PubMed] [Google Scholar]
- 2.Jowett A., Birks C., Blackney M. Chronic exertional compartment syndrome in the medial compartment of the foot. Foot Ankle Int. 2008;29(8):838–841. doi: 10.3113/FAI.2008.0838. [DOI] [PubMed] [Google Scholar]
- 3.Park Y.H., Ahn J.H., Choi G.W., Kim H.J. Exertional medial compartment syndrome of the foot-referred pain and sequelae of delayed diagnosis: a case report. Clin. J. Sport Med. 2019;29(6):e83–e85. doi: 10.1097/JSM.0000000000000582. [DOI] [PubMed] [Google Scholar]
- 4.Myerson M.S., Berger B.I. Isolated medial compartment syndrome of the foot: a case report. Foot Ankle Int. 1996;17(3):183–185. doi: 10.1177/107110079601700313. [DOI] [PubMed] [Google Scholar]
- 5.Izadi F.E., Richie D.H., Jr. Exertional compartment syndrome of the medial foot compartment—diagnosis and treatment: a case report. J. Am. Podiatr. Med. Assoc. 2014;104(4):417–421. doi: 10.7547/0003-0538-104.4.417. [DOI] [PubMed] [Google Scholar]
- 6.Kelsey N.R., Edmonds L.D., Biko D.M. Acute exertional medial compartment syndrome of the foot in a teenager. Radiol. Case Rep. 2016;10(2):1092 doi: 10.2484/rcr.v10i2.1092. (Published 2016 Feb 17) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lokiec F., Siev-Ner I., Pritsch M. Chronic compartment syndrome of both feet. J. Bone Joint Surg. (Br.) 1991;73(1):178–179. doi: 10.1302/0301-620X.73B1.1991764. [DOI] [PubMed] [Google Scholar]
- 8.Seiler R., Guziec G. Chronic compartment syndrome of the feet. A case report. J. Am. Podiatr. Med. Assoc. 1994;84(2):91–94. doi: 10.7547/87507315-84-2-91. [DOI] [PubMed] [Google Scholar]
- 9.Muller G.P., Masquelet A.C. Le syndrome de loge chronique du pied. Description d’un cas [chronic compartment syndrome of the foot. A case report] Rev. Chir. Orthop. Reparatrice Appar. Mot. 1995;81(6):549–552. [PubMed] [Google Scholar]
- 10.Mollica M.B. Chronic exertional compartment syndrome of the foot. A case report. J. Am. Podiatr. Med. Assoc. 1998;88(1):21–24. doi: 10.7547/87507315-88-1-21. [DOI] [PubMed] [Google Scholar]
- 11.McQueen M.M., Duckworth A.D. The diagnosis of acute compartment syndrome: a review. Eur. J. Trauma Emerg. Surg. 2014;40:521–528. doi: 10.1007/s00068-014-0414-7. [DOI] [PubMed] [Google Scholar]