Abstract
Background
The advantages and disadvantages of retrograde intrarenal surgery (RIRS) and minimally invasive percutaneous nephrolithotomy (mPCNL) for treatment of upper urinary tract calculi have not been conclusively determined.
Methods
In this meta-analysis, We comprehensively evaluated the performance of the two surgical approaches in treatment of upper urinary calculi. We searched the Pubmed, Embase, Cochrane and Web of science databases for randomized controlled trial (RCT) articles on RIRS and mPCNL upto December 2022. Data were extracted by two independent reviewers and subjected to the meta-analysis using the Stata 15.1 software (StataSE, USA).
Results
A total of 18 eligible RCTs involving 1733 patients were included in this study. The meta-analysis revealed that mPCNL of 1–2 cm or 2–3 cm stones had a higher stone clearance rate (RR:1.08, 95%CI (1.03, 1.14), p = 0.002) and shorter operation time (WMD : -10.85 min, 95%CI (-16.76, -4.94), p<0.001). However, it was associated with more hospital stay time (WMD :1.01 day, 95%CI(0.53, 1.5), p<0.001), hemoglobin drops (WMD :0.27 g/dl, 95%CI (0.14, 0.41), p<0.001), blood transfusion rate (RR:5.04, 95%CI(1.62, 15.65), p = 0.005), pain visual analogue score (WMD:0.75, 95%CI (0.04, 1.46), p = 0.037), hospital costs (SMD :-0.97, 95%CI (-1.19, -0.76), p<0.001) and major complications (RR:1.89, 95%CI(1.01, 3.53), p = 0.045).
Conclusion
Therefore, in terms of surgical effects and operation time, mPCNL is superior to RIRS, but is inferior with regards to other perioperative parameters. These factors should be fully considered in clinical decision making.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12894-023-01341-3.
Keywords: mPCNL, RIRS, Urinary tract stones, Stone free rate, Urolithiasis, Complications
Introduction
Globally, the incidences and recurrence rates of kidney stones are [1–3], resulting in a significant increase in treatment costs and substantial health challenges. Regarding treatment, most patients with stones < 1 cm will pass the stones automatically after analgesia and oral stone lysis, but patients with stones > 1 cm usually require urological interventions [4, 5]. The current mainstream methods of surgical interventions include retrograde intrarenal surgery (RIRS), standard percutaneous nephrolithotomy (sPCNL) and minimally invasive or Micro or Ultra-mini or super-mini percutaneous nephrolithotomy (mPCNL). Retrograde intrarenal surgery is suitable for stones less than 2 cm while percutaneous nephrolithotomy is suitable for stones more than 2 cm [6, 7]. Due to advances in laser and surgical technologies, minimally invasive percutaneous nephrolithotomy has attracted people’s attention because of its lower complications and higher stone clearance rate when compared with standard percutaneous nephrolithotomy [8–11].
Previously, meta-analyses have compared the outcomes of the two procedural approaches, asserting that mPCNL yields superior surgical outcomes compared to RIRS [12–16]. However, their conclusions regarding postoperative complications and related aspects are conflicting. Constrained by the quality and sample size of the included studies, prior research findings necessitate validation through prospective large-scale investigations. In recent years, a plethora of well-designed Randomized Controlled Trials (RCTs) addressing this subject have been published; nevertheless, a consensus on the conclusions has yet to be reached [17–21].
Henceforth, we aim to incorporate and synthesize the most recent RCT publications, with the intention of furnishing a higher level of evidence for the comparative efficacy and safety of mPCNL and RIRS interventions in the treatment of renal stones exceeding 1 cm. This endeavor seeks to underpin clinical decision-making processes.
Methods
This systematic review and meta-analysis was conducted following the methods recommended by the Preferred Reporting Project for Systematic Reviews and Meta-analyses (PRISMA) statement [22] and registered on the Prospero website (CRD42023387706).
Literature search, inclusion, and exclusion criteria
The Pubmed, Cochrane Library, Web of Science, and Embase databases were searched for published articles until December 20, 2022. The search was carried out using a combination of subject headings and free words. The following search strategy was developed on the basis of Intervention and patient-related characteristics: ((Kidney Calculi OR Upper Ureter stone* OR urolithiasis OR kidney stone*) AND (retrograde intrarenal surgery OR RIRS OR flexible ureteroscopy OR flexible Ureterscopy Surgeries) AND (minimally invasive percutaneous nephrolithotomy OR ultra-mini percutaneous nephrolithotomy OR miniaturized percutaneous nephrolithotomy OR miniaturized PCNL)).
To avoid omissions, we manually searched the English references of the included articles.
The inclusion criteria were define using the PICOS approach : P(patients): All adult patients diagnosed with upper urinary tract stones (>1 cm); I(intervention): patients who underwent mPCNL lithotripsy; C (comparator): patients who underwent RIRS lithotripsy; O (outcome): at least one of the following outcomes; SFR, operation duration, hospitalization time, pain visual analogue score, blood transfusion, hemoglobin drop, postoperative complications and hospitalization expense; S(study type): Only RCTs in English language were included. The exclusion criteria were: I: Non-comparative or non-randomized studies; III: Editorial comments, meeting abstracts, case reports, or reviews; III: Tract sizes of mPCNL<20 F or>11 F; IV: Other studies that did not meet the inclusion criteria.
Result parameters and data collection
Data extraction was independently performed by two reviewers as follows: I: General information: first author name, year of publication and country; II: Population characteristics: number of patients, age, body mass index (BMI), stone size, nephroscope size, lithotripsy; III: Perioperative outcomes: operative time, hemoglobin drop, transfusion rates, length of hospital stay, stone-free rate; IV: Overall complications rate, minor complications (defined as Clavien grade 1–2), major complications (defined as Clavien grade ≥ 3); and V: Pain visual analogue score, hospitalization expense. Any differences were resolved by consensus or by consultations with the third reviewer.
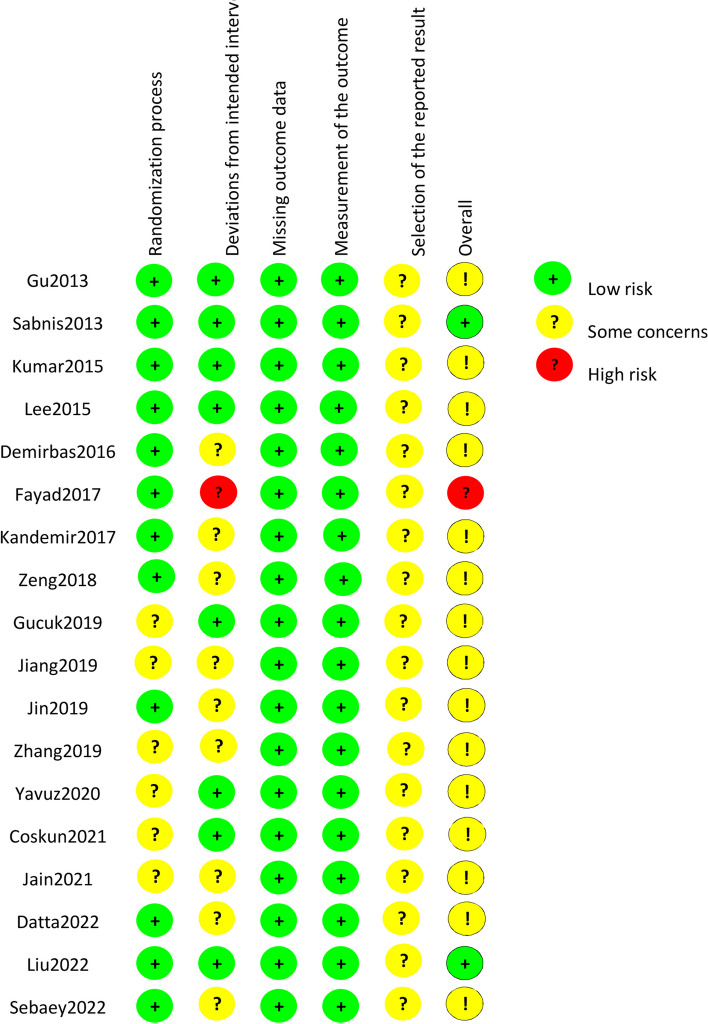
Quality assessment and statistical analysis
The qualities of all included RCTs were assessed using the Cochrane Collaboration’s tool for randomized trials(ROB 2) [23], including randomization process, deviations from intended interventions, missing outcome data, measurement of the outcome, selection of the reported result, and overall bias. Meta-analysis was conducted using the Stata 15.1 software (StataSE, USA). Risk ratio (RR) was used for dichotomous variables, whereas continuous variables were pooled as weighted mean difference (WMD). Statistical heterogeneity was evaluated using I2 statistics; When I2 ≥ 50% (p ≤ 0.1), it indicated significant heterogeneity, and a random effects model was employed; when I2 < 50%, a fixed effects model was employed (p > 0.1); p ≤ 0.05 was the threshold for statistical significance [24]. Subgroup and sensitivity analyses were performed when necessary to explore the sources and sizes of heterogeneity among studies. Publication bias was screened by using the funnel plot.
Results
Baseline characteristics
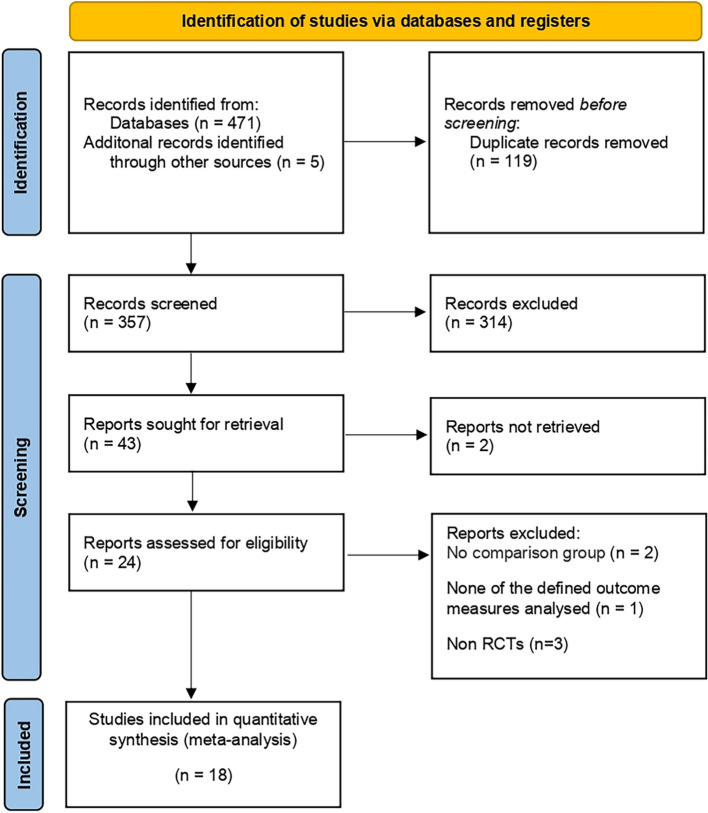
According to the literature screening process in Fig. 1, 18 [17–21, 25–37] qualified RCTs were included in this Meta-analysis Table 1; Fig. 2 summarizes the risk bias in the included studies. These trials included 887 mini-PCNL cases (52%) and 846 RIRS cases (48%). Table 2 summarizes the baseline characteristics and the associated preoperative variables (sample size, age, BMI, stone size, and lithotripsy) of the included patients. Outcome parameters or all included studies and the results after Meta-analysis are summarized in Tables 3 and 4.
Fig. 1.
PRISMA flow diagram for the systematic review
Table 1.
Summary of RCTs studies included in Meta-analysis
| Study | Country | Study period | Study design | Sample size | mPCNL category | Definition of stone free rate | LE | |
|---|---|---|---|---|---|---|---|---|
| MPCNL | RIRS | |||||||
| Gu 2013 [25] | 2010.9-2011.11 | RCT | 30 | 29 | Mini-PCNL |
Fragments < 4 mm at 3 mo on NCCT |
Fragments<4 mm at 3 mo on NCCT | 2a |
| Sabnis 2013 [26] | India | 2011.2-2012.8 | RCT | 35 | 35 | Micro-PCNL |
Fragments < 4 mm at 3 mo on NCCT |
2a |
| Kumar 2015 [27] | India | 2012.1-2013.5 | RCT | 41 | 43 | Mini-PCNL |
Fragments < 4 mm at 3 mo on NCCT |
2a |
| Lee 2015 [28] | Korea | 2014.6-2015.2 | RCT | 35 | 33 | Mini-PCNL | Fragments < 2 mm at 3 mo on NCCT | 2a |
| Demirbas 2016 [29] | Turkey | 2015.3-2015.9 | RCT | 30 | 43 | Ultra-mini PCNL | Fragments < 3 mm at 1 mo on NCCT | 2a |
| Fayad 2017 [30] | Egypt | 2012.7-2015.12 | RCT | 60 | 60 | Mini-PCNL | Fragments < 3 mm at 3 mo on NCCT | 2a |
| Kandemir 2017 [31] | Turkey | 2013.3-2015.12 | RCT | 30 | 30 | Micro-PCNL |
Fragments < 4 mm at 3 mo on NCCT |
2a |
| Zeng 2018 [32] | China | 2015.8-2017.7 | RCT | 80 | 80 | Super-Mini PCNL | NA | 2a |
| Gucuk 2019 [33] | Turkey | 2016.4-2017.5 | RCT | 30 | 30 | Mini-PCNL | No fragments at 3 mo on low dose NCCT | 2a |
| Jiang 2019 [17] | China | 2013.1-2017.3 | RCT | 57 | 56 | Micro-PCNL | Fragments < 3 mm at 3 mo on NCCT | 2a |
| Jin 2019 [18] | China | 2017.5-2019.7 | RCT | 110 | 110 | Mini-PCNL | Fragments < 3 mm at 3 mo on NCCT | 2a |
| Zhang 2019 [19] | China | 2015.3-2017.3 | RCT | 60 | 60 | Ultra-mini PCNL | Fragments < 3 mm at 3 mo on NCCT | 2a |
| Yavuz 2020 [34] | Turkey | 2017.1-2017.12 | RCT | 33 | 34 | Ultra-mini PCNL + Micro-PCNL + Mini-PCNL | Fragments < 3 mm at 3 mo on NCCT | 2a |
| Coskun 2021 [35] | Turkey | 2016.6-2016.12 | RCT | 25 | 25 | Mini-PCNL | Fragments < 3 mm at 3 mo on NCCT | 2a |
| Jain 2021 [36] | India | 2016.12-2018.10 | RCT | 40 | 40 | Mini-PCNL | Fragments < 4 mm at 1 mo on NCCT | 2a |
| Datta 2022 [20] | England | 2015.5-2016.12 | RCT | 98 | 46 | Ultra-mini PCNL | Fragments < 2 mm at 1 mo on low dose NCCT | 2a |
| Liu 2022 [21] | China | 2018.7-2020.7 | RCT | 58 | 57 | Mini-PCNL | Fragments < 3 mm at 3 mo on NCCT | 2a |
| Sebaey 2022 [37] | Egypt | 2017.9-2019.9 | RCT | 35 | 35 | Mini-PCNL | Fragments < 4 mm on NCCT | 2a |
LE Eevel of evidece, mPCNL minimally invasive percutaneous nephrolithotomy, RIRS Retrograde intrarenal surgery; NA not available
Fig. 2.
Risk of bias assessment
Table 2.
Characters of patients and calculus
| Study | Treatments | Age(year) | BMI(kg/m2) | Male/Female | Stone size(mm) | Lithotripsy | Dilator | Access sheath size, Fr | Nephroscope size |
|---|---|---|---|---|---|---|---|---|---|
| Gu 2013 [25] | mPCNL | 42.5 ± 10.1 | NA | NA | 17.27(15–25) | Laser | FD | 12-18 F | 8.5 F/9.8 F |
| RIRS | 44.22 ± 13 | NA | NA | 16.23(15–25) | Laser | UAS | NA | 8.5 F/9.8 F | |
| Sabnis 2013 [26] | mPCNL | 38.6 ± 14.6 | 23.9 ± 4.9 | 22/13 | 11 ± 2.3 | Laser | NA | NA | NA |
| RIRS | 43.7 ± 12.1 | 24.9 ± 4.3 | 24/11 | 10.4 ± 2.5 | Laser | FD | 12 F | 7.5 F | |
| Kumar 2015 [27] | mPCNL | 33.7 ± 1.6 | 23.5 ± 1.2 | 20/21 | 13.3 ± 1.3 | Pneumatic | NA | 18 F | 15 F |
| RIRS | 33.4 ± 1.4 | 23.6 ± 1.1 | 20/23 | 13.1 ± 1.1 | Laser | UAS | 12 F | 8/9.8 F | |
| Lee 2015 [28] | mPCNL | 59.3 ± 13.3 | 26.3 ± 3.9 | 28/7 | 39.1 ± 30.7 | Laser | Balloon dilator | 18 F | 15 F |
| RIRS | 55.8 ± 11.2 | 25.6 ± 5.1 | 28/5 | 28.9 ± 17.5 | Laser | UAS | 12/14/16F | 7.5 F | |
| Demirbas 2016 [29] | mPCNL | 47.7 ± 14.6 | NA | 21/9 | 185.9 ± 88.3 | Laser | Amplatz dilators | 14 F | 6/7.5 F |
| RIRS | 48.7 ± 16.9 | NA | 20/23 | 181.7 ± 114.18a | Laser | UAS | 11.5 F | 7.5 F | |
| Fayad 2017 [30] | mPCNL | 37.2 ± 9.2 | NA | 38/22 | 14.7 ± 3 | Laser | Alkan dilators | 16 F | 10 F |
| RIRS | 37.7 ± 9.8 | NA | 34/26 | 14.1 ± 3 | Laser | UAS | 12/14F | 7.5 F | |
| Kandemir 2017 [31] | mPCNL | 49.7(1–78) | NA | 16/14 | 10.6(5–15) | Laser | NA | 16 F | NA |
| RIRS | 51.8(21–81) | NA | 19/11 | 11.5(7–15) | Laser | UAS | NA | NA | |
| Zeng 2018 [32] | mPCNL | 49.4 ± 12.8 | 23.26 ± 3.41 | 36/17 | 15 ± 2.9 | Laser | FD | 14 F | NA |
| RIRS | 47.1 ± 13.9 | 23.63 ± 3.83 | 39/14 | 14.3 ± 3.4 | Laser | UAS | 12/14F | NA | |
| Gucuk 2019 [33] | mPCNL | 46.1 ± 17.5 | 26.4 ± 3.3 | 21/9 | 275.5 ± 75.1 | Laser | One step dilator | 16.5 F | 12 F |
| RIRS | 46.6 ± 13.5 | 27.2 ± 3.7 | 23/7 | 259.1 ± 65.2b | Laser | UAS | 9.5/11.5 F | 7.5 F | |
| Jiang 2019 [17] | mPCNL | 43.4 ± 11.6 | 23.9 ± 4.5 | 39/19 | 16.1 ± 3.0 | Laser | NA | 16 F | NA |
| RIRS | 45.4 ± 11.2 | 24.1 ± 4.3 | 42/16 | 15.2 ± 3.2 | Laser | UAS | 14 F | 7.5 F | |
| Jin 2019 [18] | mPCNL | 53.2 ± 13.7 | 24.8 ± 3.8 | 79/31 | 14.9 ± 3.9 | Laser | FD | 16 F | NA |
| RIRS | 51.4 ± 11.9 | 25.3 ± 4.2 | 72/38 | 16.4 ± 3.3 | Laser | UAS | 12/14F | 8/9.8 F | |
| Zhang 2019 [19] | mPCNL | 48.9 ± 11.1 | 24.31 ± 3.01 | 37/23 | 15.48 ± 2.45 | Laser | UMP | 13 F | 4.5 F |
| RIRS | 50 ± 11.9 | 24.33 ± 3.14 | 34/26 | 14.63 ± 2.67 | Laser | UAS | 12/14F | NA | |
| Yavuz 2020 [34] | mPCNL | 42.3 ± 12.7 | 24.6 ± 3.7 | 18/16 | 415 ± 82 | Laser | NA | 12 F | 4.5 F |
| RIRS | 48.1 ± 13.1 | 25.4 ± 2.8 | 20/13 | 401 ± 85a | Laser | UAS | 12 F | 6/7.5 F | |
| Coskun 2021 [35] | mPCNL | 44 ± 14 | NA | 15/10 | 15.7 ± 2.5 | Pneumatic | Amplatz dilators | NA | NA |
| RIRS | 48 ± 13.9 | NA | 13/12 | 13.6 ± 2.2 | Laser | UAS | NA | 5.5 F | |
| Jain 2021 [36] | mPCNL | 35.6 | 23 | 25/15 | 12.35 | Laser/Pneumatic | FD | 16.5/17.5 | 16 F |
| RIRS | 40.45 | 25.09 | 32/8 | 12.9 | Laser | URF | 11 F | NA | |
| Datta 2022 [20] | mPCNL | 39.08 | 23.59 | 59/39 | 16.31 | Laser | NA | 13 F | NA |
| RIRS | 40.54 | 24.27 | 29/17 | 16.02 | Laser | NA | NA | NA | |
| Liu 2022 [21] | mPCNL | 47.59 ± 10.9 | 32.62 ± 1.94 | 39/19 | 585.39 ± 131.06a | Laser | FD | 18 F | 12 F |
| RIRS | 49.19 ± 13.3 | 31.19 ± 2.04 | 40/17 | 548.64 ± 123.55a | Laser | UAS | 12/14F | NA | |
| Sebaey 2022 [37] | mPCNL | 36.11 ± 11.91 | 41.76 ± 9.34 | 25/10 | 20.43 ± 2.2 | Laser | Teflon dilators | 14 F | 12 F |
| RIRS | 34.0 ± 10.69 | 42.21 ± 10.22 | 17/18 | 20.5 ± 2.1 | Laser | USA | 12/14F | 7.5 F |
aStone size is presented in terms of length (mm) unless indicated otherwise: mm3; b Stone size is presented in terms of length (mm) unless indicated otherwise: mm2 ; mPCNL minimally invasive percutaneous nephrolithotomy, RIRS Retrograde intrarenal surgery, UAS Ureteral access sheath placement, FD Fascial dilators, NA Not available;
Table 3.
Outcome parameters of MPCNL and RIRS
| Study | Treatments | SFR(%) | Hospitalization time(day) | Operation | Postoperative | Hb drop(g/dl) | Transfusion,n(%) | cost | Complications(%) | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| duration(min) | pain score | Overall n(%) | Grade I n(%) | Grade II n(%) | Grade III n(%) | |||||||
| Gu 2013 [25] | mPCNL | 100 | 4.6 ± 1.8 | 50–135(96.2) | - | - | - | - | - | - | - | - |
| RIRS | 89.7 | 1.9 ± 1.3 | 45–100(66.8) | - | - | - | - | - | - | - | - | |
| Sabnis 2013 [26] | mPCNL | 97.1 | 2.4 ± 0.9 | 51.6 ± 18.5 | 1.9 ± 1.2 | 0.96 ± 0.41 | - | - | 9(25.7) | 8(22.9) | 1(2.8) | 0 |
| RIRS | 94.3 | 2.1 ± 0.75 | 47.1 ± 17.5 | 1.6 ± 0.8 | 0.56 ± 0.31 | - | - | 4(11.4) | 4(11.4) | 0 | 0 | |
| Kumar 2015 [27] | mPCNL | 95.1 | 3.1 | 61.1 ± 1.3 | - | - | 12.9 | - | 10(24.9) | 8(20) | 2(4.9) | - |
| RIRS | 86.1 | 1.3 | 47.5 ± 1.1 | - | - | 0 | - | 4(9.4) | 2(4.7) | 2(4.7) | - | |
| Lee 2015 [28] | mPCNL | 85.7 | 1.6 ± 1.1 | 76.1 ± 70.6 | 4.2 ± 2.6 | 0.69 ± 0.98 | - | - | 15(42.9) | 11(31.4) | 4(11.4) | 0 |
| RIRS | 97 | 1.5 ± 0.9 | 99.6 ± 60.8 | 5.7 ± 3.0 | 0.38 ± 0.97 | - | - | 22(62.9) | 19(54.3) | 3(9.1) | 0 | |
| Demirbas 2016 [29] | mPCNL | 80 | 2.46 ± 3.02 | 54.53 ± 23.09 | 4.73 ± 1.25 | - | - | 665 | 7(23.4) | 2(6.7)a | 5(16.7) | |
| RIRS | 74.4 | 1.37 ± 1.48 | 59.41 ± 15.78 | 2.30 ± 1.12 | - | - | 1160 | 6(14) | 3(7)a | 3(7) | ||
| Fayad 2017 [30] | mPCNL | 92.72 | 71.66 ± 10.36 | - | 0.28 | 0 | - | 5(8.33) | 5(8.33) | - | - | |
| RIRS | 84.31 | 109.66 ± 20.75 | - | 0.13 | 0 | - | 5(8.33) | 5(8.33) | - | - | ||
| Kandemir 2017 [31] | mPCNL | 93.7 | 54.2 | 59.04 | - | 1.06(0.1–28) | 3.3 | - | 5(16.6) | 4(13.3) | 1(3.3) | 0 |
| RIRS | 86.7 | 19 | 51.05 | - | 0.75(0.1–21) | 0 | - | 6(19.9) | 4(13.3) | 2(6.6) | 0 | |
| Zeng 2018 [32] | mPCNL | 93.8 | 2.5 ± 1.1 | 58.6 ± 21.6 | 2.7 ± 1.7 | 1.02 ± 0.89 | 0 | - | 6(7) | 9(11.7) | 2(2.6) | - |
| RIRS | 82.5 | 2.5 ± 1.1 | 52.3 ± 22.4 | 2.0 ± 1.5 | 0.43 ± 0.88 | 0 | - | 6(7) | 12(14.5) | 2(2.6) | - | |
| Gucuk 2019 [33] | mPCNL | 86.7 | 2.1 ± 2.03 | 98.3 ± 18.8 | 3.1 ± 1.4 | - | 3.3 | - | 12(40) | 9(30) | 3(10) | 0 |
| RIRS | 83.3 | 1.6 ± 1.34 | 109.0 ± 33.8 | 3.0 ± 1.4 | - | 0 | - | 9(30) | 6(20) | 1(3.3) | 2(6.6) | |
| Jiang 2019 [17] | mPCNL | 94.7 | 3.2 ± 0.5 | 54.0 ± 8.2 | - | 3.0 ± 2.3 | - | - | 4(6.9) | 3(5.2) | 1(1.7) | 0 |
| RIRS | 92.9 | 3.2 ± 0.6 | 60.3 ± 8.5 | - | 2.3 ± 1.5 | - | - | 6(5.2) | 0 | 4(3.4) | 2(1.7) | |
| Jin 2019 [18] | mPCNL | 99.1 | 5.59 ± 0.82 | 79.6 ± 14.86 | 3.42 ± 1.24 | 1.14 ± 0.76 | - | - | 12(11) | 0 | 12(11) | 0 |
| RIRS | 97.3 | 3.15 ± 0.72 | 87.2 ± 13.34 | 1.62 ± 0.86 | 0.98 ± 0.68 | - | - | 6(5.5) | 0 | 6(5.5) | 0 | |
| Zhang 2019 [19] | mPCNL | 98 | 5.3 ± 1.2 | 68.58 ± 15.82 | - | 0.89 | 1.6 | 4085.51 ± 416.69 | 10(16.7) | 2(3.3) | 5(8.3) | 3(5) |
| RIRS | 92 | 3.2 ± 0.5 | 93.35 ± 21.64 | - | 0.44 | 0 | 4657.28 ± 679.28 | 6(10) | 2(3.3) | 3(5) | 1(1.7) | |
| Yavuz 2020 [34] | mPCNL | 94.1 | 2 (1–14) | 61.6 ± 18.5 | - | - | - | 632 ± 314 | 3(8.8) | - | 3(8.8) | 0 |
| RIRS | 76 | 1 (0.5-3) | 60.7 ± 13 | - | - | - | 1250 ± 505 | 2(6) | - | 2(6) | 0 | |
| Coskun 2021 [35] | mPCNL | 4.6 ± 3,5 | 71.7 ± 24.4 | - | - | 8 | - | - | 7(28) | 9(36) | 9(36) | |
| RIRS | 1.2 ± 0.59 | 72.8 ± 24.2 | - | - | 0 | - | - | 20(78) | 3(12) | 0 | ||
| Jain 2021 [36] | mPCNL | 92.5 | 2.85 | 51.58 | - | 0.88 | - | - | 9(22.5) | 2(5) | 3(7.5) | 4(10) |
| RIRS | 87.5 | 2.45 | 69.75 | - | 0.42 | - | - | 16(40) | 4(10) | 7(17.5) | 5(12.5) | |
| Datta 2022 [20] | mPCNL | 100 | 39.21 | 41.17 | - | 0.46 | - | 45.61 | 10(10.3) | 6(6.2) | 4(4.1) | 0 |
| RIRS | 73 | 39.08 | 73.58 | - | 0.31 | - | 423.02 | 16(35) | 16(35) | 0 | 0 | |
| Liu 2022 [21] | mPCNL | 86.2 | 3.5 ± 1.58 | 48.2 ± 24.25 | 4.6 ± 1.34 | 0.98 ± 0.55 | 5.2 | - | 13(22.4) | 13(22.4) | - | - |
| RIRS | 61.4 | 2.5 ± 1.24 | 43.5 ± 17.23 | 3.9 ± 1.07 | 0.76 ± 0.58 | 0 | - | 4(7) | 4(7) | - | - | |
| Sebaey 2022 [37] | mPCNL | 88.6 | 1.41 ± 0.46 | 59.71 ± 19.44 | - | 1.27 ± 0.1 | 2.9 | - | 3(8.6) | 3(8.6) | - | - |
| RIRS | 82.9 | 1.29 ± 0.44 | 80.43 ± 14.79 | - | 1.29 ± 0.1 | 0 | - | 1(2.9) | 1(2.9) | - | - | |
aoverall number of Grade I and Grade II; mPCNL minimally invasive percutaneous nephrolithotomy, RIRS Retrograde intrarenal surgery, Hb Hemoglobin, SFR Stone free rate
Table 4.
Results of meta-analysis comparing mPCNL and RIRS
| Outcomes | No.of studies | SamPle size | Heterogeneity(Total) | W(S)MD/RR(95%CI) | P value(Total) | ||||
|---|---|---|---|---|---|---|---|---|---|
| mPCNL | RIRS | chi2 | df | I2% | P value | ||||
| Overall SFR | 17 | 862 | 821 | 42.3 | 16 | 62.1 | 0.01 | 1.08(1.03–1.14) | P = 0.002 |
| SFR(stone 1–2 cm) | 11 | 571 | 573 | 28.34 | 10 | 64.7 | 0.002 | 1.09(1.03–1.15) | P = 0.003 |
| SFR(stone 2–3 cm) | 3 | 123 | 122 | 4.78 | 2 | 58.2 | 0.092 | 1.19(1.05–1.36) | P = 0.007 |
| Operation time | 18 | 887 | 846 | 836.6 | 17 | 98.00% | 0 | -6.82(-15.45, 1.81) | P = 0.122 |
| Operation time(2013–2019) | 8 | 341 | 353 | 322.5 | 7 | 97.80% | 0 | -0.65(-16.56, 15.26) | p = 0.936 |
| Operation time(2019–2022) | 10 | 546 | 493 | 62.9 | 9 | 85.70% | 0 | -10.85(-16.76,-4.94) | p<0.001 |
| Transfusion | 9 | 419 | 420 | 0.78 | 6 | 0 | 0.993 | 5.04(1.62–15.65) | P = 0.005 |
| Hospitalization time | 17 | 827 | 786 | 810.5 | 16 | 98 | 0 | 1.01(0.53,1.5) | P<0.001 |
| Pain visual analogue score | 7 | 378 | 388 | 81.65 | 6 | 92.7 | 0 | 0.75(0.04–1.46) | P = 0.037 |
| Hb drop | 11 | 723 | 667 | 56.4 | 10 | 82.3 | 0 | 0.27(0.14–0.41) | P<0.001 |
| Complication ratio | 16 | 832 | 792 | 38.29 | 15 | 60.8 | 0.001 | 1.17(0.82–1.68) | P = 0.39 |
| Clavien-Dindo(I-II) | 17 | 857 | 817 | 40.47 | 16 | 60.5 | 0.001 | 1.03(0.74–1.42) | P = 0.88 |
| Clavien-Dindo(III) | 12 | 583 | 542 | 8.25 | 7 | 15.2 | 0.311 | 1.89(1.014–3.53) | P = 0.045 |
| Cost | 4 | 221 | 183 | 5.18 | 3 | 42 | 0.159 | -0.97(-1.19, -0.76) | P<0.001 |
CI Confidence interval, WMD Weighted mean difference, SMD Standardized mean difference, mPCNL Minimally invasive percutaneous nephrolithotomy, RIRS Retrograde intrarenal surgery, RR Risk ratio, SFR Stone free rate;
Outcome analysis
Overall stone free rate
Seventeen studies reported on SFR. Due to heterogeneity (> 50%), a random effects model was employed for analysis. The SFR was found to be significantly higher in the mPCNL group, relative to the RIRS group (RR: 1.08, 95%CI 1.03, 1.14 p = 0.002) (Fig. 3A). Moreover, significant outcomes were obtained in subgroups with stone sizes of 1–2 cm (RR: 1.09, 95%CI 1.03, 1.15 p = 0.003) (Fig. 3B) and 2–3 cm (RR: 1.19, 95%CI 1.05, 1.36 p = 0.007) (Fig. 3C).
Fig. 3.
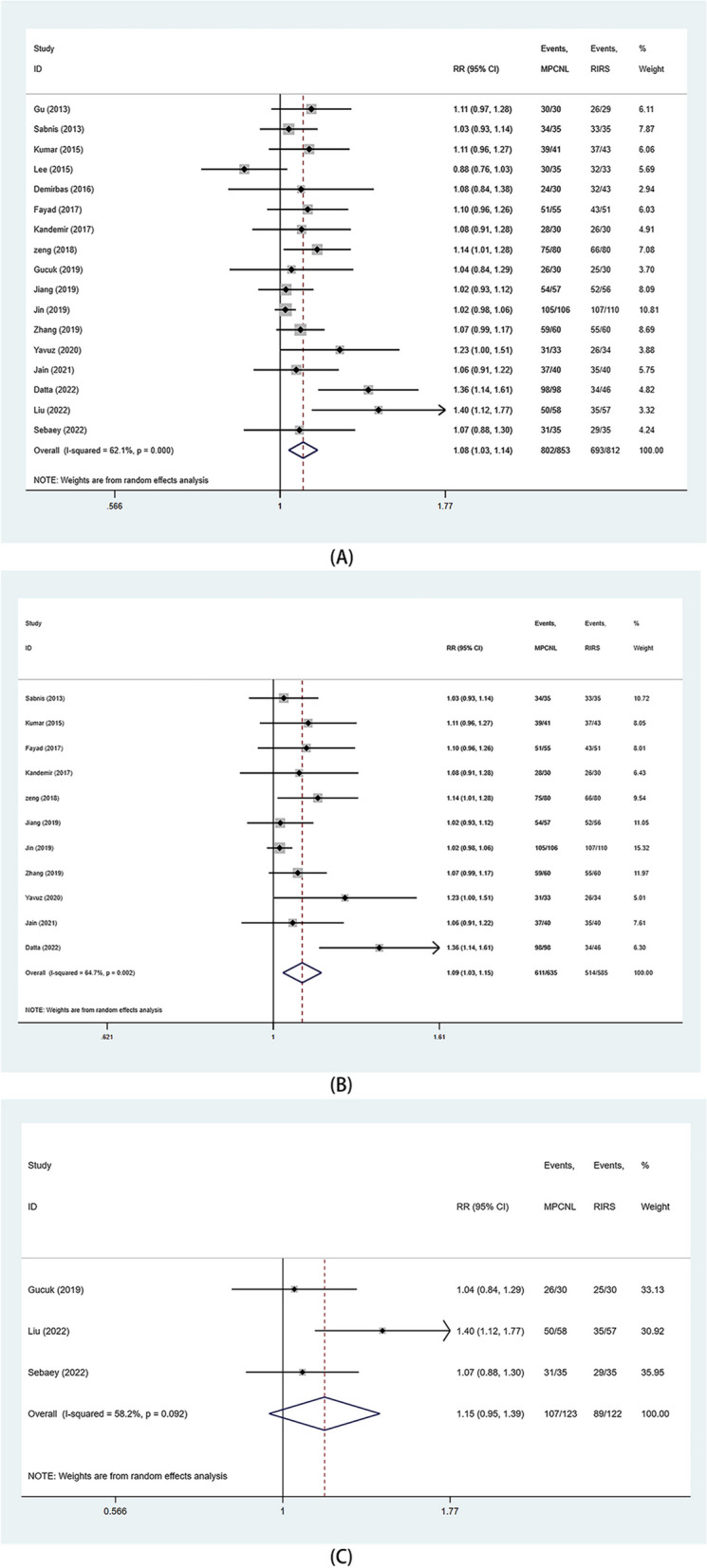
Forest plots of SFR. A overall SFR; B SFR (stone 1-2 cm); C. SFR (stone>2 cm)
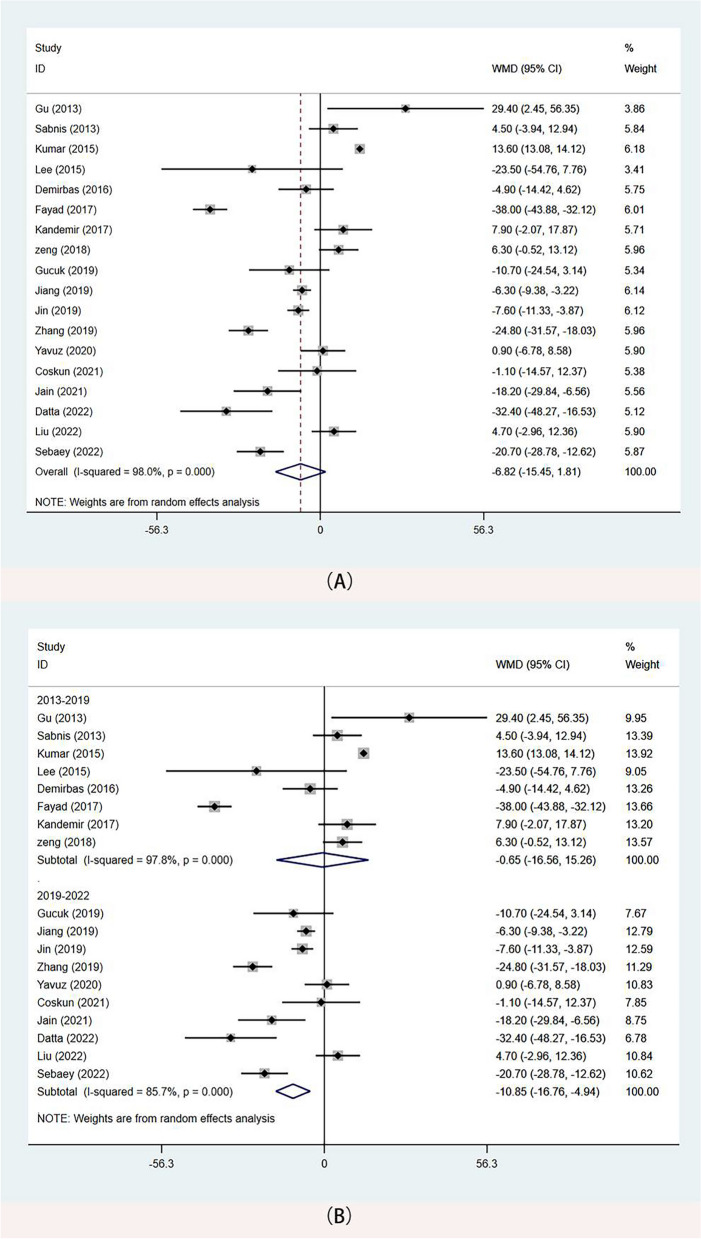
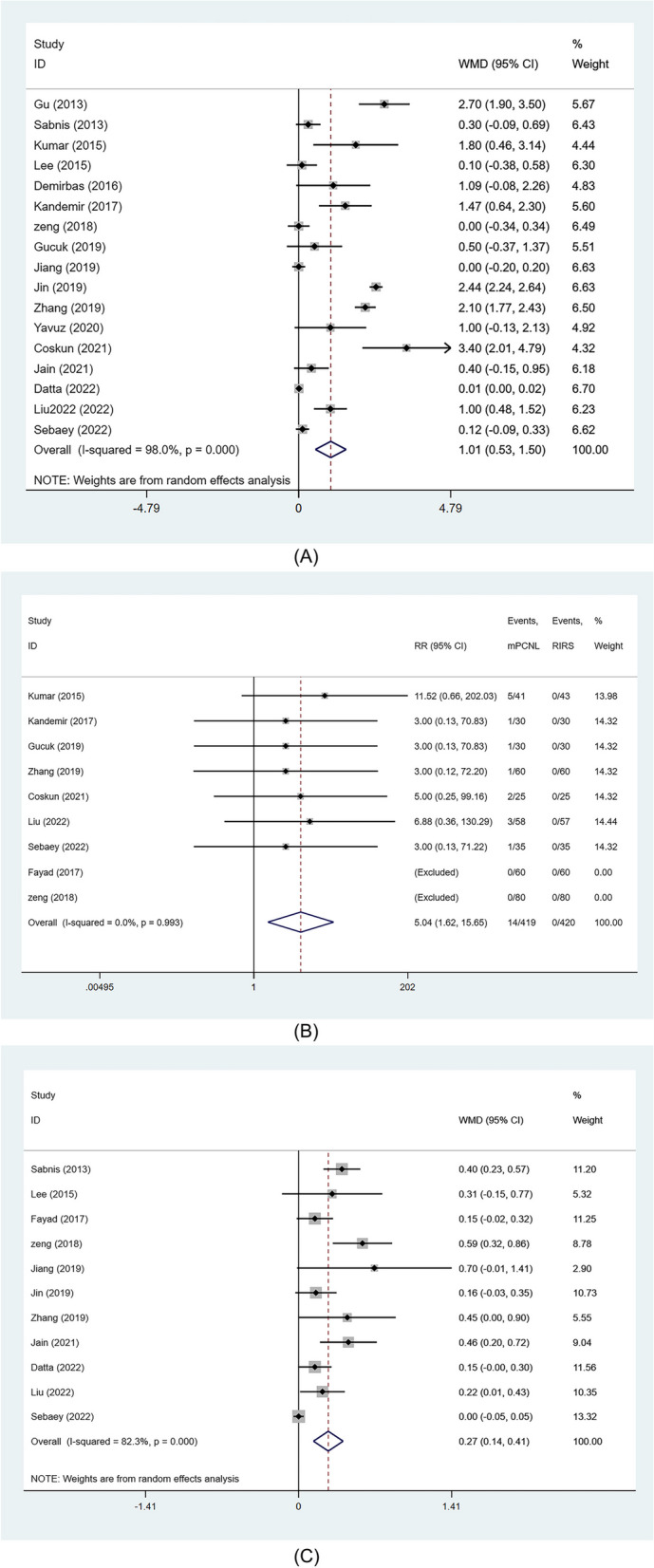
Operation duration
The operative time was reported in all included studies, and analyses were conducted using the random-effects model. The meta-analysis did not reveal any differences between the two surgical methods (WMD: -6.82 min, 95%CI -15.45, 1.81 p = 0.122) (Fig. 4A). However, subgroup analysis according to publication time showed that for studies published after 2019, procedure time was better in the mPCNL group than in the RIRS group (WMD: -10.85 min, 95%CI -16.76, -4.94 p<0.001) (Fig. 4B).
Fig. 4.
Forest plots of operative time. A operative time(Overall); B operative time (2019–2022)
Length of hospital stay
Data on length of hospital stay were extracted from 17 studies. The random-effects model showed that the length of hospital stay was significantly longer in the mPCNL group than in the RIRS group (WMD: 1.01 day, 95%CI 0.53, 1.5 p<0.001) (Fig. 5A).
Fig. 5.
Forest plots of Los, transfusion rate and hemoglobin drop. A Length of stay; B transfusion rate; C. hemoglobin drop
Transfusion rate
Nine studies reported on the occurrence of transfusion events. The meta-analysis using a fixed-effects model showed that the probability of blood transfusion was significantly higher in the mPCNL group relative to the RIRS group (RR: 5.04, 95%CI 1.62, 15.65, p = 0.005) (Fig. 5B).
Hemoglobin drop
Data were obtained from 11 studies. The random-effects model revealed a greater decrease in hemoglobin levels in the mPCNL group than in the RIRS group (WMD 0.27 g/dl, 95%CI 0.14–0.41, p<0.001) (Fig. 5C).
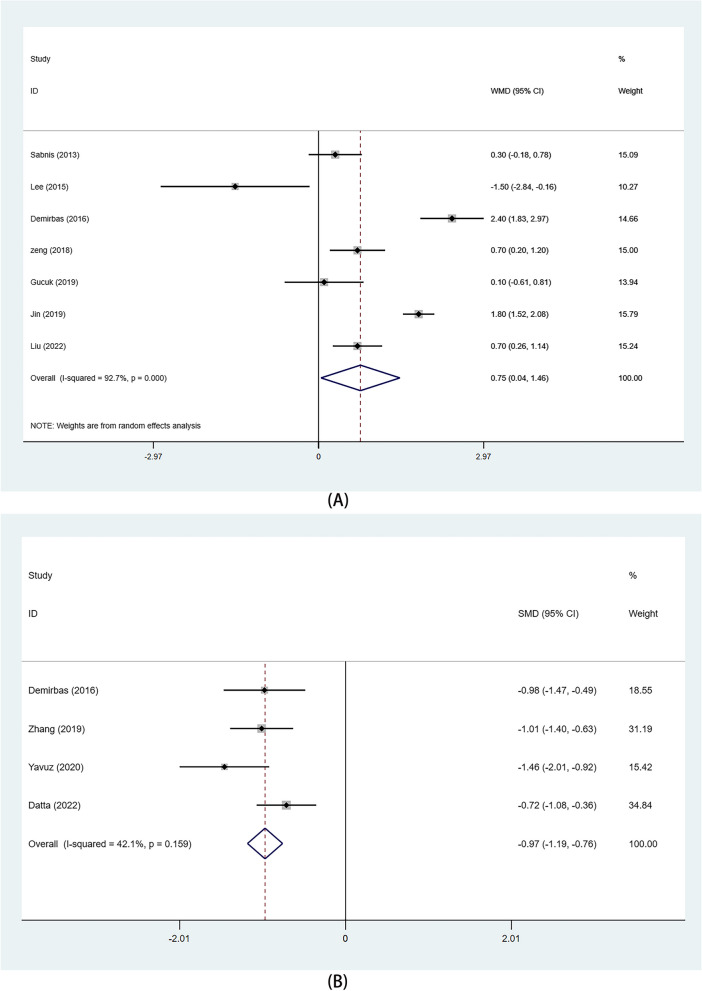
Pain visual analogue score
Data were derived from 7 studies. The random-effects model showed that patients in the mPCNL group had higher scores than those in the RIRS group (WMD: 0.75, 95%CI 0.04, 1.46, p = 0.037)(Fig. 6A).
Fig. 6.
Forest plots of pain visual analogue score and Hospitalization expense. A pain visual analogue score; B Hospitalization expense
Hospitalization expense
Among the studies, only four reported hospital costs. In the fixed-effects analysis, patient costs were generally lower in the mPCNL group than in the RIRS group (SMD: -0.97, 95%CI (-1.19, -0.76), p<0.001)(Fig. 6B).
Postoperative Complications
Postoperative complications were classified as follows: overall complications rate, minor complications (defined as Clavien grade 1–2), major complications (defined as Clavien grade ≥ 3) using the Clavien-Dindo classification system. In the random-effects model, we did not find differences in overall complications between the two surgical procedures (RR: 1.07 95%CI 0.87, 1.33 p = 0.51) (Fig. 7A). Data from 17 studies also showed no difference in the rate of minor complications between the groups (RR: 0.95 95%CI 0.78, 1.15 p = 0.58) (Fig. 7B). However, results of the fixed-effects model showed that the rate of severe complications was higher for mPCNL than for RIRS (RR: 1.89 95%CI 1.01–3.53 P = 0.045) (Fig. 7C).
Fig. 7.
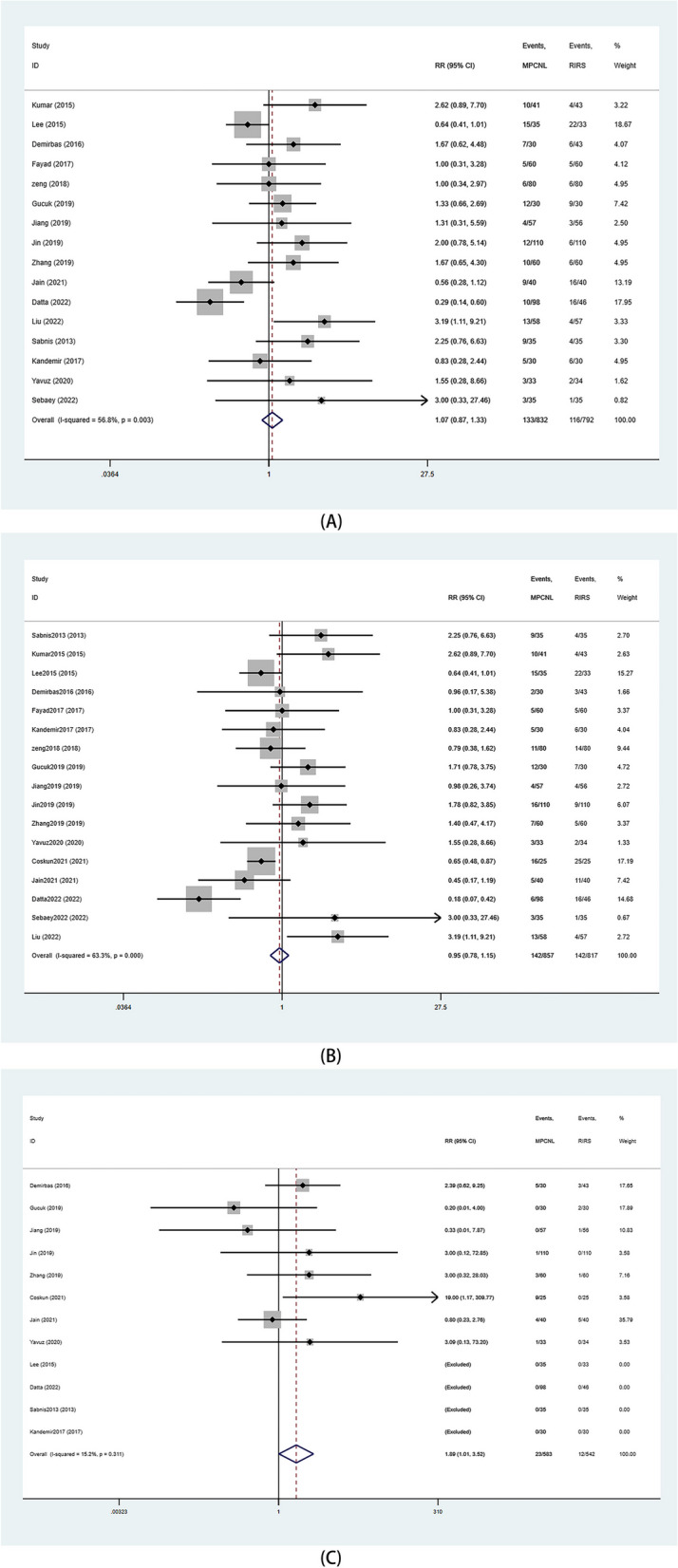
Forest plots of complication. A overall complication; B minor complication; C major complication
Heterogeneity
The majority of outcomes showed moderate to high heterogeneity, with only transfusion rates, major complications, and hospitalization costs having low heterogeneity outcomes. However, the reported low or moderate heterogeneity may be misleading because I2 is highly biased in a small number of studies [38]. Certain outcome measures (OT, LOS, and Hb drop) exhibit substantial heterogeneity. We endeavored to mitigate confounding factors such as country, publication year, and mPCNL type through meta-regression analysis. No discernible sources of heterogeneity were identified (p > 0.05) (Supplementary File 1). Furthermore, we conducted subgroup analyses for each outcome measure based on mPCNL type. The results indicate statistical significance only in terms of operative time, with no discernible differences observed in the remaining metrics (Supplementary File 2).
Publication bias
Analysis of the funnel plot revealed no significant asymmetry, indicating that there was no significant publication bias in our results (Fig. 8).
Fig. 8.
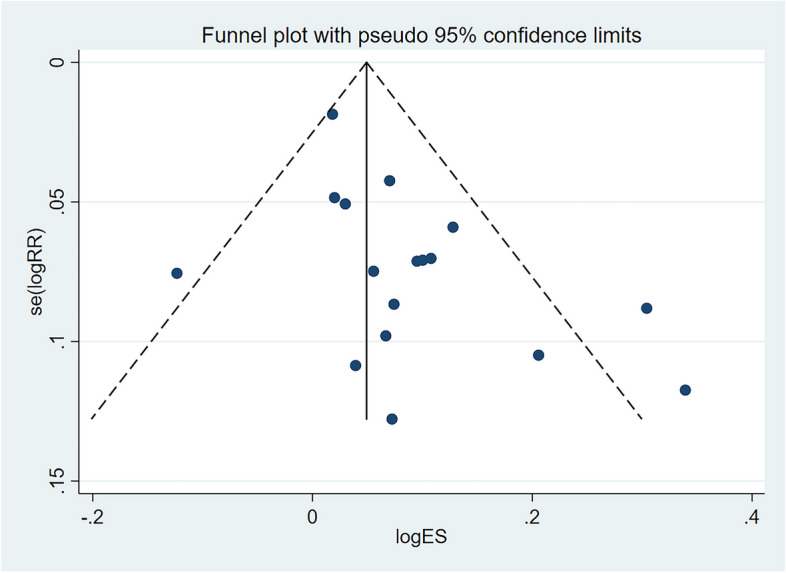
Funnel plot of operative time for publication bias
Discussion
This is a meta-analysis incorporating the latest research. Our study reveals that, compared to RIRS, mPCNL exhibits advantages such as shorter operation time and higher stone free rate. However, in terms of hospital stay time, transfusion rate, pain visual analogue score, and major complications, mPCNL performance falls short of that of RIRS. These findings warrant further discussion.
In recent years, minimally invasive surgery has increasingly been applied in the treatment of upper urinary tract calculi. According to the guidelines of European Association of Urology, both pcnl and RIRS are recommended for the treatment of upper urinary tract stones with diameter < 2 cm, and PCNL is the first-line treatment for upper urinary tract stones with diameter > 2 cm [39]. With the rapid development of minimally invasive technology and endoscopic instruments, traditional PCNL has been constructed from Mini-PCNL, Ultra-mini PCNL, Super-mini PCNL, Micro-pcnl and other minimally invasive PCNL procedures. Such improvements have substantially decreased the access and size of the puncture sheath of the previous 20 F [40]. Compared to conventional PCNL, miniaturized PCNL (mPCNL) has demonstrated a distinct advantage in reducing postoperative complications [41–43]. Over the years, traditional RIRS has also evolved to become today’s dual-channel flexible ureteroscope, disposable flexible ureteroscope, robot-assisted flexible ureteroscope and other new flexible ureteroscope [44, 45]. In the comparison of advantages and disadvantages of mPCNL and RIRS, it is not only necessary to pay attention to the stone clearance rate, but also to the quality of life during the perioperative period. In this paper, we analyzed the most recent RCT study to comprehensively compare the advantages and disadvantages of the two surgical methods in the treatment of upper urinary calculi.
The efficacy of the two treatments is based on total stone-free rate. This study found that mPCNL had a better summary stone-free rate compared with RIRS, which was consistent with results of a previous meta-analysis [46]. However, for stones measuring 2 to 3 centimeters, there is no significant difference in the effectiveness between the two surgical procedures. In this study, subgroup analyses revealed that for stones measuring 1–2 centimeters and 2–3 centimeters, mPCNL demonstrated superiority over RIRS. This observation may be attributed to the steeper funnel-pelvic angle and longer funnel calyx, which pose challenges for RIRS in accessing the lower pole, thus limiting complete stone extraction [47]. In the study conducted by Datta et al. [20] approximately 46% of patients in the RIRS group presented with preoperative lower pole renal calyx stones, indicative of residual stones postoperatively. Ripple et al. [48] posit that patients with preoperative renal calculi larger than 1 cm, following Retrograde Intrarenal Surgery (RIRS), exhibit residual fragments in approximately 50% of cases. Furthermore, Ghan and colleagues along with WOLF et al. [49] employing rigorous CT imaging as a follow-up modality, have derived a post-RIRS average stone clearance rate of 77%. Therefore, for renal lower pole calculi that present challenges in accessibility via RIRS or are constrained by ureteral stenosis, mPCNL emerges as an impeccable alternative. In terms of operation time, there seemed to be no significant advantage or disadvantage between the two surgical methods. However, subgroup analysis reported that 10 RCTS published after 2019 showed that the operation time of mPCNL was significantly shorter compared with that of RIRS. RIRS entails a segmented surgical approach, where flexible ureteroscopy necessitates manipulation and flexion for stone fragmentation. Concurrently, mPCNL is also a multi-step procedure, involving an initial ultrasound or fluoroscopy-guided entry, placement of a guidewire within the system, removal of the initial puncture needle from the guidewire, continuous or stepwise dilation of the urethra during the procedure, resulting in urethral bleeding, and ultimately the placement of a sheath onto the urethral dilator [50]. These discrete maneuvers are time-consuming. Although mPCNL represents a relatively newer surgical modality, it is readily graspable by any urologist who has undergone PCNL training. We hypothesize that due to the accumulated experience in these procedures, contemporary practitioners exhibit greater proficiency compared to their initial application of mPCNL. The reduction in hemoglobin matched with a significant difference in blood transfusion, and the study by Kumar [27] included five patients who required blood transfusion, possibly for reasons related to the surgical technique. The magnitude of blood loss during PCNL is contingent upon the caliber of the tract [51, 52]. Employing a single-step procedure along with the use of minimally sized tracts serves to mitigate hemorrhagic tendencies and associated complications in PCNL. Notably, Desai et al. have successfully implemented the microperc technique to accomplish PCNL in a singular procedural step [53].
According to the CLAVIEN-Dindo classification, there was no significant difference in the total complications and mild complications between the two groups, but the probability of severe complications was higher in mPCNL. The principal operative-related complications associated with PCNL encompass significant hemorrhage (7.8%), renal pelvis perforation (3.4%), pleural effusion (1.8%), and transfusion (5.7%) [54]. RIRS constitutes an endoscopic procedure conducted via natural orifices, thereby minimizing trauma to the renal parenchyma and reducing intraoperative blood loss. The primary complications of RIRS involve ureteral avulsion or perforation [55]. Deployment of a ureteral access sheath may potentially result in ureteral wall injury [56]. In the study by COSKUN et al [35], the number of major complications which affected the balance were reported but no explanation was given. One possible reason could be the surgical management procedures at local hospitals. Postoperative complications of RIRS, which the authors attributed to catheter detachment, catheter displacement or calcification due to bipolar catheters, increased the risk of readmission.
RIRS typically entails the placement of stents, resulting in associated discomfort for patients and necessitating subsequent stent removal [57]. Additionally, flexible ureteroscopy is prone to wear and tear, potentially requiring significant refurbishment after 4–14 uses [58]. Disposable components like baskets can also escalate the overall procedural expenses, whereas mPCNL, characterized by lower wear rates, can yield cost-effectiveness benefits.
Previous meta-analyses
In recent years, several studies have compared the treatment of renal stones using mPCNL and RIRS. Several studies predominantly encompassed cohort designs, potentially introducing bias in their conclusions due to the absence of randomized controlled trials [12, 59]. Moreover, despite the inclusion of RCTs, subgroup analyses based on stone size and mPCNL were not conducted due to insufficient data volume [13–15, 46].
Strengths and limitations
Firstly, this study encompassed 18 randomized controlled trials characterized by high methodological quality and substantial sample sizes. Secondly, in contrast to previous investigations, novel findings emerged, demonstrating that mPCNL exhibited superior surgical duration and clearance rates for upper urinary tract stones measuring 2 to 3 centimeters, as compared to the RIRS group. However, mPCNL demonstrated higher levels of bleeding, transfusion rates, costs, and postoperative discomfort when compared to the RIRS group. Thirdly, we conducted relevant subgroup analyses to minimize outcome heterogeneity. Nonetheless, this study is not without limitations. Firstly, certain included studies lacked descriptions regarding blinding and randomization concealment, potentially introducing biases into the conclusions. Furthermore, variations in outcome definitions and measurement methods may contribute to outcome heterogeneity. Consequently, caution is advised when interpreting our research findings.
Conclusions
MPCNL has a higher stone clearance rate and a shorter operation time in stones < 3 cm when both procedures are safe and effective. However, MPCNL has more hospital stay, more blood loss, more blood transfusion, more severe complications, more pain and more hospital costs than RIRS because of its invasive characteristics. Because of the high heterogeneity of some of the results, our results should be interpreted with caution, and clinicians should fully consider the advantages and disadvantages of the two surgical procedures to make the decision that is best for patients.
Supplementary Information
Acknowledgements
We would like to thank the researchers and study participants for their contributions. Thanks to Ms. Yu Jiang for her encouragement and support to YL in his medical career.
We would like to thank the researchers and study participants for their contributions. Thank Ms. Yu Jiang for her encouragement and love to me. Although the road is far away, the action will arrive.
Authors' contributions
LY: Protocol development, data collection and management, data analysis and manuscript writing. ZH: Protocol development, data collection and management, data analysis and manuscript writing. YX: Protocol development, data management, data analysis and manuscript writing. WZ: Data management, data analysis and manuscript writing. JY: Data management, data analysis and manuscript writing. HJ: Data management, data analysis and manuscript writing. CC: Data management and manuscript writing. WC: Data management and manuscript writing. WJ: Data management and manuscript writing. BE: Data management and manuscript writing.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Acknowledgments:
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yang Liu and Huimin Zhang contributed equally to this work.
References
- 1.Finger M, Finger E, Bellucci A, Malieckal DA. Medical management for the prevention of kidney stones. Postgrad Med J. 2023;99(1169):112–8. doi: 10.1136/postgradmedj-2021-140971. [DOI] [PubMed] [Google Scholar]
- 2.Thongprayoon C, Krambeck AE, Rule AD. Determining the true burden of kidney stone Disease. Nat Rev Nephrol. 2020;16(12):736–46. doi: 10.1038/s41581-020-0320-7. [DOI] [PubMed] [Google Scholar]
- 3.Mohebbi N. [Risk factors for urolithiasis] Therapeutische Umschau Revue Therapeutique. 2021;78(5):223–7. doi: 10.1024/0040-5930/a001264. [DOI] [PubMed] [Google Scholar]
- 4.Corbo J, Wang J. Kidney and Ureteral stones. Emerg Med Clin North Am. 2019;37(4):637–48. [DOI] [PubMed]
- 5.Fontenelle LF, Sarti TD. Kidney stones: treatment and Prevention. Am Fam Physician. 2019;99(8):490–6. [PubMed]
- 6.Assimos D, Krambeck A, Miller NL, Monga M, Murad MH, Nelson CP, Pace KT, Pais VM Jr., Pearle MS, Preminger GM et al. Surgical Management of stones: American Urological Association/Endouro logical Society Guideline, PART I. J Urol. 2016;196(4):1153–60. [DOI] [PubMed]
- 7.Sanguedolce F, Bozzini G, Chew B, Kallidonis P, de la Rosette J. The evolving role of Retrograde Intrarenal Surgery in the treatment of Urolithiasis. Eur Urol Focus. 2017;3(1):46–55. doi: 10.1016/j.euf.2017.04.007. [DOI] [PubMed] [Google Scholar]
- 8.DiBianco JM, Ghani KR. Precision Stone Surgery: current status of miniaturized percutaneous N ephrolithotomy. Curr Urol Rep. 2021;22(4):24. [DOI] [PubMed]
- 9.Zhu W, Liu Y, Liu L, Lei M, Yuan J, Wan SP, Zeng G. Minimally invasive versus standard percutaneous nephrolithotomy: a met a-analysis. Urolithiasis. 2015;43(6):563–70. [DOI] [PubMed]
- 10.Atassi N, Knoll T. Future of kidney stone management: surgical intervention miniaturizati on of PCNL: where is the limit? Curr Opin Urol. 2020;30(2):107–12. [DOI] [PubMed]
- 11.Proietti S, Giusti G, Desai M, Ganpule AP. A critical review of Miniaturised Percutaneous Nephrolithotomy: is Sma Ller Better? Eur Urol Focus. 2017;3(1):56–61. [DOI] [PubMed]
- 12.Cabrera JD, Manzo BO, Torres JE, Vicentini FC, Sánchez HM, Rojas EA, Lozada E. Mini-percutaneous nephrolithotomy versus retrograde intrarenal Surgery for the treatment of 10–20 mm lower Pole renal stones: a systematic review and meta-analysis. World J Urol. 2020;38(10):2621–8. doi: 10.1007/s00345-019-03043-8. [DOI] [PubMed] [Google Scholar]
- 13.Tsai SH, Chung HJ, Tseng PT, Wu YC, Tu YK, Hsu CW, Lei WT. Comparison of the efficacy and safety of shockwave lithotripsy, retrograde intrarenal Surgery, percutaneous nephrolithotomy, and minimally invasive percutaneous nephrolithotomy for lower-pole renal stones: a systematic review and network meta-analysis. Med (United States). 2020;99(10):e19403. [DOI] [PMC free article] [PubMed]
- 14.Awedew AF, Alemu CT, Yalew DZ. Efficacy and safety of various endosurgical procedures for management of large renal stone: a systemic review and network meta-analysis of randomised control trials. Urolithiasis. 2023;51(1):87. [DOI] [PubMed]
- 15.Hou J, Xu F, Du H, Liu J, Li N. Efficacy and safety of the surgical treatments for lower calyceal stones: a systematic review and network meta-analysis. Int J Surg. 2023;109(3):383–8. doi: 10.1097/JS9.0000000000000062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kallidonis P, Adamou C, Ntasiotis P, Pietropaolo A, Somani B, Özsoy M, Liourdi D, Sarica K, Liatsikos E, Tailly T. The best treatment approach for lower calyceal stones ≤ 20 mm in maximal diameter: mini percutaneous nephrolithotripsy, retrograde intrarenal Surgery or shock wave lithotripsy. A systematic review and meta-analysis of the literature conducted by the European section of Uro-Technology and Young Academic urologists. Minerva Urol Nephrol. 2021;73(6):711–23. doi: 10.23736/S2724-6051.21.04388-3. [DOI] [PubMed] [Google Scholar]
- 17.Jiang K, Chen H, Yu X, Chen Z, Ye Z, Yuan H. The all-seeing needle micro-PCNL versus flexible ureterorenoscopy for lower calyceal stones of ≤ 2 cm. Urolithiasis. 2019;47(2):201–6. doi: 10.1007/s00240-018-1049-7. [DOI] [PubMed] [Google Scholar]
- 18.Jin LC, Yang B, Zhou Z, Li NC. Comparative efficacy on flexible ureteroscopy lithotripsy and miniaturized percutaneous nephrolithotomy for the treatment of medium-sized Lower-Pole Renal Calculi. J Endourol. 2019;33(11):914–9. doi: 10.1089/end.2019.0504. [DOI] [PubMed] [Google Scholar]
- 19.Zhang H, Hong TY, Li G, Jiang N, Hu C, Cui X, Chu C, Zhao JL. Comparison of the efficacy of Ultra-mini PCNL, Flexible Ureteroscopy, and Shock Wave lithotripsy on the treatment of 1–2 cm lower Pole Renal Calculi. Urol Int. 2019;102(2):194–8. doi: 10.1159/000493508. [DOI] [PubMed] [Google Scholar]
- 20.Datta SN, Chalokia RS, Wing KW, Patel K, Solanki R, Desai J. Ultramini-percutaneous nephrolithotomy versus retrograde intrarenal Surgery in the treatment of 10–30 mm calculi: a randomized controlled trial. Urolithiasis. 2022;50(3):361–7. doi: 10.1007/s00240-022-01304-7. [DOI] [PubMed] [Google Scholar]
- 21.Liu X, Xia D, Peng E, Tong Y, Liu H, Wang X, He Y, Chen Z, Tang K. Comparison of two techniques for the management of 2–3 cm lower Pole renal calculi in obese patients. World J Urol. 2022;40(2):513–8. doi: 10.1007/s00345-021-03872-6. [DOI] [PubMed] [Google Scholar]
- 22.Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA, Group P-P. Preferred reporting items for systematic review and meta-analysis prot ocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;350:g7647. [DOI] [PubMed]
- 23.Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA. The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58. [DOI] [PubMed]
- 25.Gu XJ, Lu JL, Xu Y. Treatment of large impacted proximal ureteral stones: randomized comparison of minimally invasive percutaneous antegrade ureterolithotripsy versus retrograde ureterolithotripsy. World J Urol. 2013;31(6):1605–10. doi: 10.1007/s00345-013-1026-2. [DOI] [PubMed] [Google Scholar]
- 26.Sabnis RB, Ganesamoni R, Doshi A, Ganpule AP, Jagtap J, Desai MR. Micropercutaneous nephrolithotomy (microperc) vs retrograde intrarenal Surgery for the management of small renal calculi: a randomized controlled trial. BJU Int. 2013;112(3):355–61. doi: 10.1111/bju.12164. [DOI] [PubMed] [Google Scholar]
- 27.Kumar A, Kumar N, Vasudeva P, Kumar Jha S, Kumar R, Singh H. A prospective, randomized comparison of shock wave lithotripsy, retrograde intrarenal Surgery and miniperc for treatment of 1 to 2 cm radiolucent lower calyceal renal calculi: a single center experience. J Urol. 2015;193(1):160–4. doi: 10.1016/j.juro.2014.07.088. [DOI] [PubMed] [Google Scholar]
- 28.Lee JW, Park J, Lee SB, Son H, Cho SY, Jeong H. Mini-percutaneous nephrolithotomy vs Retrograde Intrarenal Surgery for Renal stones larger than 10 mm: a prospective Randomized Controlled Trial. Urology. 2015;86(5):873–7. doi: 10.1016/j.urology.2015.08.011. [DOI] [PubMed] [Google Scholar]
- 29.Demirbas A, Resorlu B, Sunay MM, Karakan T, Karagöz MA, Doluoglu OG. Which should be Preferred for moderate-size kidney stones? Ultramini Percutaneous Nephrolithotomy or Retrograde Intrarenal Surgery? J Endourol. 2016;30(12):1285–9. doi: 10.1089/end.2016.0370. [DOI] [PubMed] [Google Scholar]
- 30.Fayad AS, Elsheikh MG, Ghoneima W. Tubeless mini-percutaneous nephrolithotomy versus retrograde intrarenal Surgery for lower calyceal stones of ⩽2 cm: a prospective randomised controlled study. Arab J Urol. 2017;15(1):36–41. doi: 10.1016/j.aju.2016.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kandemir A, Guven S, Balasar M, Sonmez MG, Taskapu H, Gurbuz R. A prospective randomized comparison of micropercutaneous nephrolithotomy (Microperc) and retrograde intrarenal Surgery (RIRS) for the management of lower Pole kidney stones. World J Urol. 2017;35(11):1771–6. doi: 10.1007/s00345-017-2058-9. [DOI] [PubMed] [Google Scholar]
- 32.Zeng G, Zhang T, Agrawal M, He X, Zhang W, Xiao K, Li H, Li X, Xu C, Yang S, et al. Super-mini percutaneous nephrolithotomy (SMP) vs retrograde intrarenal Surgery for the treatment of 1–2 cm lower-pole renal calculi: an international multicentre randomised controlled trial. BJU Int. 2018;122(6):1034–40. doi: 10.1111/bju.14427. [DOI] [PubMed] [Google Scholar]
- 33.Gucuk A, Yilmaz B, Gucuk S, Uyeturk U. Are Stone Density and Location Useful Parameters That Can Determine th e Endourological Surgical Technique for Kidney Stones That are Smaller than 2 cm? A Prospective Randomized Controlled Trial. Urol J. 2019;16(3):236–41. [DOI] [PubMed]
- 34.Yavuz A, Kilinc MF, Bayar G. Outcomes of different minimally invasive techniques in lower calyceal stones of 1 to 2 centimeters: a prospective, randomized study. Arch Esp Urol. 2020;73(4):307–15. [PubMed]
- 35.Coskun A, Eryildirim B, Sarica K, Çamur E, Can U, Saglam E. Comparison of Mini Percutaneous Nephrolithotomy (Mini PCNL) and Retrograde Intrarenal Surgery (RIRS) for the minimal Invasive Management of Lower Caliceal stones. Urol J. 2021;18(5):485–90. doi: 10.22037/uj.v18i07.6443. [DOI] [PubMed] [Google Scholar]
- 36.Jain M, Manohar C, Nagabhushan M, Keshavamurthy R. A comparative study of minimally invasive percutaneous nephrolithotomy and retrograde intrarenal Surgery for solitary renal stone of 1–2 cm. Urol Annals. 2021;13(3):226–31. doi: 10.4103/UA.UA_10_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sebaey A, Taleb AA, Elbashir S, Gomaa R, Elshazli A, Saber W. Flexible ureterorenoscopy (RIRS) vs. Mini- percutaneous nephrolithotomy (MINI-PCNL) for renal stones 20–30 mm a prospective randomized study. Afr J Urol. 2022;28:13.
- 38.von Hippel PT. The heterogeneity statistic I(2) can be biased in small meta-analyses. BMC Med Res Methodol. 2015;15:35. [DOI] [PMC free article] [PubMed]
- 39.Türk C, Petřík A, Sarica K, Seitz C, Skolarikos A, Straub M, Knoll T. EAU guidelines on Interventional Treatment for Urolithiasis. Eur Urol. 2016;69(3):475–82. [DOI] [PubMed]
- 40.Druskin SC, Ziemba JB. Minimally invasive (Mini) percutaneous nephrolithotomy: Classificati on, indications, and outcomes. Curr Urol Rep. 2016;17(4):30. [DOI] [PubMed]
- 41.Nagele U, Schilling D, Sievert KD, Stenzl A, Kuczyk M. Management of lower-pole stones of 0.8 to 1.5 cm maximal diameter by the minimally invasive percutaneous approach. J Endourol. 2008;22(9):1851–3. doi: 10.1089/end.2008.9791. [DOI] [PubMed] [Google Scholar]
- 42.Mishra S, Sharma R, Garg C, Kurien A, Sabnis R, Desai M. Prospective comparative study of miniperc and standard PNL for treatment of 1 to 2 cm size renal stone. BJU Int. 2011;108(6):896–9. doi: 10.1111/j.1464-410X.2010.09936.x. [DOI] [PubMed] [Google Scholar]
- 43.ElSheemy MS, Elmarakbi AA, Hytham M, Ibrahim H, Khadgi S, Al-Kandari AM. Mini vs standard percutaneous nephrolithotomy for renal stones: a comparative study. Urolithiasis. 2019;47(2):207–14. doi: 10.1007/s00240-018-1055-9. [DOI] [PubMed] [Google Scholar]
- 44.Falagario UG, Calò B, Auciello M, Carrieri G, Cormio L. Advanced ureteroscopic techniques for the management of kidney stones. Curr Opin Urol. 2021;31(1):58–65. [DOI] [PubMed]
- 45.Gauhar V, Somani BK, Heng CT, Gauhar V, Chew BH, Sarica K, Teoh JY-C, Castellani D, Saleem M, Traxer O. Technique, feasibility, Utility, limitations, and future perspectives of a new technique of applying direct In-Scope suction to Improve Outc omes of Retrograde Intrarenal Surgery for stones. J Clin Med. 2022;11(19):5710. [DOI] [PMC free article] [PubMed]
- 46.Jiao BB, Luo ZK, Xu X, Zhang M, Zhang G. Minimally invasive percutaneous nephrolithotomy versus retrograde intrarenal Surgery in surgical management of upper urinary stones - a systematic review with meta-analysis. Int J Surg. 2019;71:1–11. doi: 10.1016/j.ijsu.2019.09.005. [DOI] [PubMed] [Google Scholar]
- 47.Karim SS, Hanna L, Geraghty R, Somani BK. Role of pelvicalyceal anatomy in the outcomes of retrograde intrarenal Surgery (RIRS) for lower Pole stones: outcomes with a systematic revi ew of literature. Urolithiasis. 2020;48(3):263–70. [DOI] [PMC free article] [PubMed]
- 48.Rippel CA, Nikkel L, Lin YK, Danawala Z, Olorunnisomo V, Youssef RF, Pearle MS, Lotan Y, Raman JD. Residual fragments following ureteroscopic lithotripsy: incidence and predictors on postoperative computerized tomography. J Urol. 2012;188(6):2246–51. doi: 10.1016/j.juro.2012.08.040. [DOI] [PubMed] [Google Scholar]
- 49.Ghani KR, Wolf JS., Jr What is the stone-free rate following flexible ureteroscopy for kidney stones? Nat Reviews Urol. 2015;12(5):281–8. doi: 10.1038/nrurol.2015.74. [DOI] [PubMed] [Google Scholar]
- 50.Doré B. [Complications of percutaneous nephrolithotomy: risk factors and management] Ann Urol (Paris) 2006;40(3):149–60. doi: 10.1016/j.anuro.2006.01.006. [DOI] [PubMed] [Google Scholar]
- 51.Yamaguchi A, Skolarikos A, Buchholz NP, Chomón GB, Grasso M, Saba P, Nakada S, de la Rosette J. Operating times and bleeding Complications in percutaneous nephrolithotomy: a comparison of tract dilation methods in 5,537 patients in the Clinical Research Office of the Endourological Society Percutaneous Nephrolithotomy Global Study. J Endourol. 2011;25(6):933–9. doi: 10.1089/end.2010.0606. [DOI] [PubMed] [Google Scholar]
- 52.Kukreja R, Desai M, Patel S, Bapat S, Desai M. Factors affecting blood loss during percutaneous nephrolithotomy: prospective study. J Endourol. 2004;18(8):715–22. doi: 10.1089/end.2004.18.715. [DOI] [PubMed] [Google Scholar]
- 53.Desai MR, Sharma R, Mishra S, Sabnis RB, Stief C, Bader M. Single-step percutaneous nephrolithotomy (microperc): the initial clinical report. J Urol. 2011;186(1):140–5. doi: 10.1016/j.juro.2011.03.029. [DOI] [PubMed] [Google Scholar]
- 54.de la Rosette J, Assimos D, Desai M, Gutierrez J, Lingeman J, Scarpa R, Tefekli A. The Clinical Research Office of the Endourological Society Percutaneous Nephrolithotomy Global Study: indications, Complications, and outcomes in 5803 patients. J Endourol. 2011;25(1):11–7. doi: 10.1089/end.2010.0424. [DOI] [PubMed] [Google Scholar]
- 55.Kirac M, Bozkurt ÖF, Tunc L, Guneri C, Unsal A, Biri H. Comparison of retrograde intrarenal Surgery and mini-percutaneous nephrolithotomy in management of lower-pole renal stones with a diameter of smaller than 15 mm. Urolithiasis. 2013;41(3):241–6. doi: 10.1007/s00240-013-0552-0. [DOI] [PubMed] [Google Scholar]
- 56.Traxer O, Thomas A. Prospective evaluation and classification of ureteral wall injuries resulting from insertion of a ureteral access sheath during retrograde intrarenal Surgery. J Urol. 2013;189(2):580–4. doi: 10.1016/j.juro.2012.08.197. [DOI] [PubMed] [Google Scholar]
- 57.Nabi G, Cook J, N’Dow J, McClinton S. Outcomes of stenting after uncomplicated ureteroscopy: systematic review and meta-analysis. BMJ. 2007;334(7593):572. doi: 10.1136/bmj.39119.595081.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Monga M, Best S, Venkatesh R, Ames C, Lee C, Kuskowski M, Schwartz S, Vanlangendock R, Skenazy J, Landman J. Durability of flexible ureteroscopes: a randomized, prospective study. J Urol. 2006;176(1):137–41. doi: 10.1016/S0022-5347(06)00575-1. [DOI] [PubMed] [Google Scholar]
- 59.Jiang HY, Yu Z, Chen LP, Wang T, Liu Z, Liu JH, Wang SG, Ye ZQ. Minimally Invasive Percutaneous Nephrolithotomy versus Retrograde Intrarenal Surgery for Upper Urinary Stones: A Systematic Review and Meta-Analysis. Biomed Res Int. 2017;2017. 10.1155/2017/2035851. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.