Abstract
Aims: This study aimed to compare COVID-19 health policy and programme responses in 16 Northern and Indigenous regions in Canada. The goal was to summarise strategies used to mitigate the initial spread of the pandemic while highlighting aspects that reflect Indigenous values. Methods: A scoping review of grey literature was completed, focusing on territorial, regional health authority, and community level websites. Further media analysis was conducted to reach saturation regarding policy changes and programmes implemented to prevent transmission, improve health communication, access testing, provide health services effectively, secure borders, and provide financial assistance. Common responses were mapped on the Women’s College Hospital’s Wholistic Framework for Safe Wellness to identify aspects that reflected Indigenous values. This framework utilises the medicine wheel to discuss physical health (body), ceremony (spirit), community health (heart), and assessment (mind). Results: The Women’s College Hospital’s Wholistic Framework for Safe Wellness quadrants of the body, spirit and heart were covered by most regions via health communication efforts, adaptations to traditional practices, and continuation of care during the pandemic, respectively. It was found that 13 regions had pandemic responses adapted for Indigenous populations. Conclusions: The responses in each Northern region show that protecting each community was a priority; however, policies and programmes were developed as a kaleidoscope of what can be done quickly and evaluated later. Assessment, risk, and prevention, covered by the mind quadrant of the Women’s College Hospital’s Wholistic Framework for Safe Wellness, were missing in initial emergency responses. Increasing capacity for emergency management in Northern and Indigenous regions will require contingency planning that acknowledges and builds off traditional knowledge.
Keywords: COVID-19, health policy, Indigenous health services
Background
The quick onset of COVID-19 left countries and communities worldwide in need of emergency management procedures. The Canadian Institute of Health Research (CIHR)’s Institute of Health Services and Policy Research (IHSPR) and local leaders from northern regional health authorities identified the need to document and compare health policy responses to COVID-19. One area recognised was the need for rapid synthesis and comparative policy analysis of the COVID-19 response and outcomes [1]. Moreover, the need to support the health of Indigenous peoples and inform culturally safe healthcare policies was identified [1]. The need to compare responses in Northern and Indigenous regions was deemed a priority as health systems in these areas have unique features to which they must adapt, including remote geographies and harsh climates, while also striving to reflect Indigenous values.
Segments of the population vulnerable to complications from COVID-19 include older individuals, those with underlying medical conditions including but not limited to heart disease, hypertension, obesity, diabetes, certain chronic respiratory diseases, cancer, and those with compromised immune systems [2]. Due, in part, to historical sociopolitical exclusion and colonial practices, Indigenous populations experience health inequities resulting in a high prevalence of underlying chronic diseases [3–6]. The disproportionate effect of pandemics on Indigenous peoples is not new; historically, Indigenous peoples have suffered higher infection rates and traumatic loss during pandemics. For example, during the 1918 influenza, Canadian First Nations people were eight times more likely to die than non-First Nations, and during the 2009 H1N1 pandemic, First Nations people were three times more likely to be hospitalised and six and a half times more likely to be admitted to an intensive care unit [7].
Problems can arise when indigeneity is communicated as the leading motive for increased health services, such as vaccine distribution, as it exacerbates the feeling of being treated like a ‘guinea pig’ or a problem that needs to be solved [8]. Vaccine hesitancy has been described and, in some cases, attributed to mistrust due to limited and late information about their efficacy and why Indigenous populations are being prioritised for distribution [9]. One solution to this issue is to discuss risk attributes at an individual level and increase health communication from local leaders [9]. With increasing land claims, self-government, and health policy reformations, Indigenous communities in Canada have taken greater control over their health systems [10]. Indigenous-led health systems are more likely than western systems to improve the health of Indigenous communities due to their incorporation of community values and principles and their holistic approach to health and treatment [11]. Within Canada, there are three models of Indigenous health governance: (a) a public government model; (b) a tripartite agreement model; and (c) systems emerging from federal agreements [12]. Comparing COVID-19 responses in Northern and Indigenous health regions, some of which encompass self-governing communities, will provide insight into the most effective policies and programmes. At the same time, the analysis will allow for a better understanding of which health indicators were considered in programme development and implementation. Many Northern communities fared very well during the first wave of COVID-19 (approximately March 2020 to June 2020); great policy lessons can be learned from listening to those who have had historically dire relationships with pandemics. The capacity to provide culturally safe, responsive care is pertinent in a time when cultural practices and physical community connections have been limited.
Aims
The purpose of this work was to describe and summarise the changes to health policy and programming in Canadian Northern and Indigenous regions that were implemented in response to the pandemic. It is hoped that this work can be used as a base to understand better effective health communication strategies, policies and programme implementation approaches in areas with similar values.
Methods
A scoping review of grey literature following the method of Arksey and O’Malley [13] was conducted to understand better health policy and programme responses in Canada’s north. This project focused on the 18 Northern health regions defined by Young et al. (2019), with one modification (Table I) [14]. The ‘Northern health’ website supplies information for Northern British Columbia (BC) residents in three service delivery areas, the North West Health Service Delivery Area, the Northern Interior Health Service Delivery Area, and the Northeast Health Service Delivery Area [15]. Thus the three health regions were combined to understand the response to COVID-19 in northern BC. With this coalescence, analysis was completed on 16 regions in total. The review looked at policy and programme adaptations relating to preventing viral transmission, ensuring workforce capacity, providing health services effectively, health financing, economic protections, and other measures. Areas of focus were adapted from the North American Observatory (NAO) COVID-19 Policy Response Monitor [16].
Table I.
Northern health regions in Canada included in scoping review. a
| Province/territory | Health region | Shorthand | Total population | % Indigenous |
|---|---|---|---|---|
| Newfoundland and Labrador | Labrador-Grenfell Regional Health Authority | NL | 36,233 | 34 |
| Quebec | Region du Saguenay-Lac-Saint-Jean | Saguenay [QC] | 275,625 | 5 |
| Région de la Côte-Nord | Côte-Nord [QC] | 93,640 | 16 | |
| Région du Nord-du-Québec | Nord [QC] | 14,185 | 6 | |
| Région du Nunavik | Nunavik [QC] | 12,638 | 91 | |
| Région des Terres-Cries-de-la-BaieJames | Baie-James [QC] | 16,748 | 96 | |
| Ontario | Northwestern Health Unit | Northwestern [ON] | 75,598 | 34 |
| Porcupine Health Unit | Porcupine [ON] | 84,220 | 15 | |
| Thunder Bay District Health Unit | Thunder Bay [ON] | 149,618 | 16 | |
| Manitoba | Northern Regional Health Authority | Northern [MB] | 71,158 | 71 |
| Saskatchewan | Mamawetan/Keewatin/Athabasca (Saskatchewan regional health authorities) | Ma-Ke-At [SK] | 35,065 | 87 |
| Alberta | Alberta North Zone | North Zone [AB] | 429,455 | 17 |
| British Columbia | North West Health Service Delivery Area | BC | 71,960 | 32 |
| Northern Interior Health Service Delivery Area | 139,725 | 16 | ||
| Northeast Health Service Delivery Area | 66,678 | 15 | ||
| Yukon | Yukon | Yukon | 34,885 | 23 |
| Northwest Territories | NWT | NWT | 41,623 | 51 |
| Nunavut | Nunavut | Nunavut | 34,885 | 86 |
Data adapted from Young et al. (2019) [14].
Original data from Statistics Canada.
BC: British Columbia; NWT: Northwest Territories.
Data were compiled from territorial, regional health authority (RHA), and community level websites. Peer-reviewed academic literature was excluded in the data collection and analysis. This was due to the timing and focus of the scan; during the first wave of COVID-19, limited peer-reviewed information was available as it pertained to the impact COVID-19 was having on Northern regions specifically. Moreover, the goal of the project was to highlight regional level responses which were more readily available from virtual community bulletins. General web searches on the Google search engine were also utilised. Search terms for each Northern region included but were not limited to ‘COVID’, ‘ventilators’, ‘ICU capacity’, ‘PPE calls’, ‘travel restrictions’, and ‘health workforce’ as necessary to reach data saturation. The search strategy is highlighted in Table II. These sources were valuable to explore government documents, news blasts, and practice guidelines. Data for the Northwest Territories (NWT) was extracted from the North American COVID-19 Policy Response Monitor, completed by the NAO [16].
Table II.
Grey literature search strategy.
| Method | Tools | Used to find |
|---|---|---|
| Grey literature repositories | Government websites RHA websites Indigenous and regional websites |
Government policies, regional news updates Programme and health service changes Health financing information |
| Targeted and general web searches | Google search engine | Health infrastructure and workforce capacity Regional restrictions Media platforms/health communication |
RHA: regional health authority.
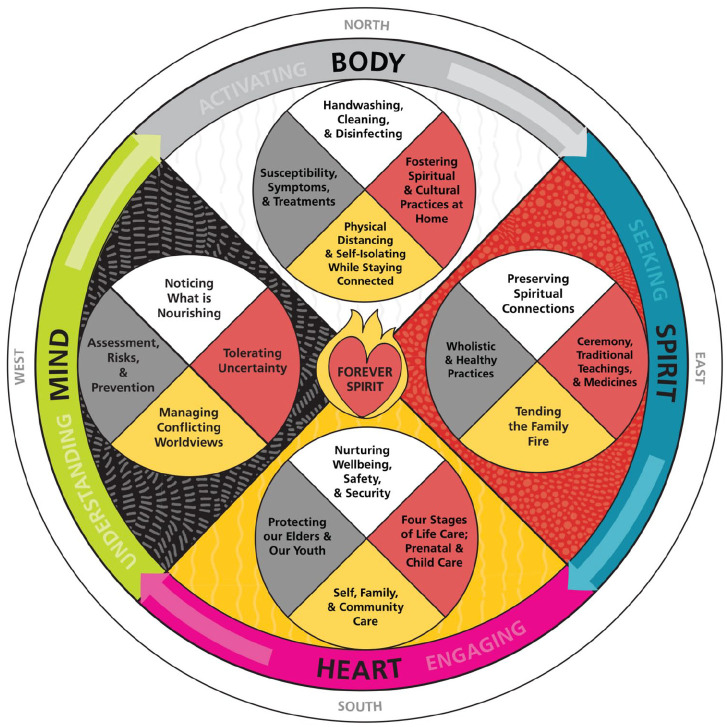
In total, 391 different sources were accessed and summarised. A breakdown of each source type can be seen in Table III. Following data charting, common responses were mapped onto the Women’s College Hospital’s Wholistic Framework for Safe Wellness (WFSW) developed by the Women’s College Hospital in Toronto to code responses related to Indigenous values deductively. The WFSW has been highlighted as a recommended COVID-19 resource that builds on the guidelines set out by public health institutions but is grounded in traditional and Elder knowledge [17]. This First Nation’s framework includes areas relating to the body, mind, heart, and spirit (Figure 1).
Table III.
Source type included in scoping review.
| Source | Government websites | Regional health authority websites and news updates | News articles/other web search hits | Total |
|---|---|---|---|---|
| Region | ||||
| Federal | 1 | 0 | 0 | 1 |
| NL | 4 | 16 | 2 | 22 |
| Quebec | 1 | 0 | 1 | 2 |
| Saguenay [QC] | 0 | 13 | 0 | 13 |
| Côte-Nord [QC] | 0 | 9 | 1 | 10 |
| Nord [QC] | 1 | 8 | 0 | 9 |
| Nunavik [QC] | 1 | 27 | 0 | 28 |
| Baie-James [QC] | 11 | 16 | 1 | 28 |
| Northwestern [ON] | 0 | 17 | 8 | 25 |
| Thunder Bay [ON] | 0 | 8 | 1 | 9 |
| Porcupine [ON] | 1 | 15 | 4 | 20 |
| Northern [MB] | 4 | 3 | 8 | 15 |
| Ma-Ke-At [SK] | 10 | 7 | 12 | 29 |
| North Zone [AB] | 3 | 6 | 4 | 13 |
| BC includes FNHA sources | 10 | 35 | 6 | 51 |
| Yukon | 26 | 0 | 4 | 30 |
| NWT | 2 | 33 | 3 | 38 |
| Nunavut | 40 | 0 | 8 | 48 |
| 115 | 213 | 63 | 391 |
BC: British Columbia; FNHA: First Nations Health Authority; NWT: Northwest Territories.
Figure 1.
Women’s College Hospital’s Wholistic Framework for Safe Wellness: body, mind, heart, and spirit. Four direction concept application: Banakonda Kennedy Kish (Bell), ShoShona Kish. Overall collaboration: Diane Longboat, Dr. Chase Everett McMurren, Elisa Levi, Lindsey Fechtig, Dr. Lisa Richardson, Rosary (Spence) Pavica, Selena Mills, Bryn Ludlow (graphic design).See https://www.womenscollegehospital.ca/research,-education-and-innovation/indigenous-wellbeing-in-the-times-of-covid-19.
Inclusion/ exclusion criteria for policy and programme changes
Inclusion criteria:
specific to the region;
current at time of review (from World Health Organization announcement to phased re-opening of the region);
described a policy or programme change relevant to preventing viral transmission, ensuring workforce capacity, providing health services effectively, health financing, economic protections, or other health communication measures.
Exclusion criteria:
general provincial measures;
changes to specific working environments;
changes occurring after July 2020 (exception exists for Tłı̨chǫ region due to concurrent research project).
Results
Common responses shared by most regional health authorities included health communication efforts specific to the region and a focus on the continuation of care despite restrictions. For example, 15 out of 16 RHAs had dedicated web pages for information about COVID-19 in the region, including where to get tested and how to stay safe. Twelve out of 16 of the regions had travel restrictions in place, and all had suspension of health services and/or visitations within care centres. Urgent care was not suspended in any region, and many services, while disrupted, continued with COVID-19 safe adaptations.
Importantly, 13 out of 16 regions, with the exceptions being Region du Saguenay-Lac-Saint-Jean, Région de la Côte-Nord, and Région du Nord-du-Québec, had information specific to Indigenous populations. The most common efforts were translating public health messaging into Indigenous languages, Indigenous-focused health information, and information regarding how to participate in traditional practices, including ceremony and harvest, safely. Both the government of the NWT and the government of Nunavut provided funding for on-the-land practices, along with the Tłı̨chǫ government, a self-governing body within the NWT. The inclusion of Indigenous-specific responses highlights the applicability of an Indigenous framework to embed policy analysis within.
This review highlighted a lack of tailored information regarding the susceptibility, symptoms, and treatment of COVID-19. While the world was still learning about the impact of the disease during the first wave, the scarcity of information could be detrimental to Indigenous populations at an increased risk of severe and lethal complications from COVID-19. Another gap noted from the review process was any type of assessment of policy and programme implementation processes. This will be a vital step moving forward for emergency preparedness in these regions.
Discussion
Each health system within Canada’s north adapted national and provincial/territorial responses to fit their geography and demographic to varying degrees. Public health communication is the clearest example of this. Most Northern RHAs also included aspects of (traditional) culture in their COVID-19 responses. Analysed with the WFSW, health communication efforts covered factors relating to the body although information regarding susceptibility was missing. Bi-cultural approaches, such as going on the land, addressed spirituality. The adaptations to health service provision ensured that communities stayed safe and healthy during the pandemic, addressing the factors grouped in the heart quadrant. Communities in Canada’s Northern health regions worked to provide relevant support for their population. Still, the fast-paced nature of COVID-19 crisis management meant that even jurisdictions with the ability to implement their own responses had to work with what they already had. Health policy development in response to COVID-19 in Canada’s Northern and Indigenous regions utilised a top-down approach, with implementation being altered to ensure cultural relevancy. Moving forward, it must be ensured that Indigenous traditions are acknowledged and respected as health policies and programmes are developed. Although acting quickly was a requirement for these RHAs, policy and decision-makers must strengthen their emergency management procedures and develop contingency frameworks to employ in the future. This will require planned and understood communication strategies among governments at all levels [18]. The development of such frameworks can be mapped to the fourth and final quadrant of the WFSW framework: the mind. This theme mentions the concepts of managing conflicting world views and assessment, risk, and prevention. By analysing the crisis management policy that was implemented and giving space to hear different perspectives, Northern RHAs can ensure holistic approaches to future emergencies are developed.
Future studies evaluating programme effectiveness will prove vital. Understanding what changes have occurred is just the first step; as climate crises and zoonotic diseases become more prevalent, communities, regions, and nations will need strong emergency preparedness and management plans. An estimated 60% of emerging human infections are zoonotic in origin and are influenced by factors such as climate change and urbanisation [19]. Thus COVID-19 responses can act as a case study to evaluate what kept communities safe as well as what did not work and what received pushback from the public. There are different types of evaluation studies that will be required; process evaluation will be needed to look at how programmes and public health guidelines were developed, while summative/outcome evaluations will be required to look at the efficacy of said programmes and guidelines [20].
Limitations
Scoping review methodology is strongest when multiple people select sources and extract data [21]. In this review, all steps were completed by one individual; the potential impact this may have had on consistency and bias is unknown. Moreover, the use of the review conducted by the NAO on health systems and policies on the NWT as opposed to independent data extraction may have resulted in inconsistent data selection; although the same categories for policy and programme adaptations were used to summarise each jurisdiction, the difference in authorship could result in data discrepancies. In addition, programme changes may have been overlooked as experts were not consulted from any of the regions. In the future, a team approach, systemic documentation of search strings, and community consultation should be included to improve coverage uniformity.
Conclusions
This study set out to describe and summarise the changes in health policy and programming that resulted due to the COVID-19 pandemic in Canadian Northern and Indigenous regions. The scoping review of grey literature allowed for the successful completion of this goal; with dramatic differences in testing, treatment, and health service staff capacity within these regions, the response to COVID-19 was a patchwork of policy, programmes, and altered health service provisions. The strongest and most common response was seen in tailored health communication efforts, while the assessment of implemented policy and programmes was lacking. This review can be used to understand better effective approaches to health programme implementation for subsequent crises.
In the future, individual communities must engage with community members of all ages and roles to determine what programmes will work best for them. When discussing Indigenous health, the role of knowledge of past pandemics should be highlighted and used to develop programme changes that consider community values. Traditional knowledge must be represented in health policies that are developed to ensure both cultural relevancy and efficacy. Understanding, respecting, and embedding culture into emergency management will allow for safe practice with minimal unintended consequences.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Canadian Institute of Health Research’s Canadian Graduate Scholarship (Master’s) and the Alberta Graduate Excellence Scholarship (Indigenous).
Data availability: Data are available online: https://docs.google.com/document/d/1MPXwuYx8IYkaaVQMyTkSz7f5z5swKrmd-hUUYHd8Ol0/edit?usp=sharing.
ORCID iD: Katherine Fleury  https://orcid.org/0000-0003-1135-9759
https://orcid.org/0000-0003-1135-9759
References
- [1]. McMahon M, Nadigel J, Thompson E, et al. Informing Canada’s Health System Response to COVID-19: Priorities for Health Services and Policy Research. Healthcare Policy. June 2020. [cited 27 July 2020];16(1). https://www.longwoods.com/content/26249//informing-canada-s-health-system-response-to-covid-19-priorities-for-health-services-and-policy-r (accessed 27 July 2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2]. Public Health Agency of Canada. Vulnerable populations and COVID-19. aem. 2020. [cited 8 September 2020]. https://www.canada.ca/en/public-health/services/publications/diseases-conditions/vulnerable-populations-covid-19.html (accessed 8 September 2020).
- [3]. Power T, Wilson D, Best O, et al. COVID-19 and Indigenous peoples: an imperative for action. J Clin Nursing 2020;29:2737–2741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4]. Czyzewski K. Colonialism as a Broader Social Determinant of Health. Int Indigenous Policy J 16 May 2011. [cited 11 March 2022]; 2(1). https://ojs.lib.uwo.ca/index.php/iipj/article/view/7337 (accessed 29 March 2022). [Google Scholar]
- 5]. Kim PJ. Social determinants of health inequities in Indigenous Canadians through a life course approach to colonialism and the residential school system. Health Equity 2019;3:378–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6]. Committee on Economic, Social and Cultural Rights. The Right to the Highest Attainable Standard of Health. Geneva: Office of the High Commissioner for Human Rights, 2000. [Google Scholar]
- [7]. Boggild AK, Yuan L, Low DE, et al. The impact of influenza on the Canadian First Nations. Can J Public Health 2011;102:345–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8]. Driedger SM, Cooper E, Jardine C, et al. Communicating risk to Aboriginal peoples: First Nations and Metis responses to H1N1 risk messages. PLoS ONE 2013;8:e71106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9]. Mosby I, Swidrovich J. Medical experimentation and the roots of COVID-19 vaccine hesitancy among Indigenous Peoples in Canada. CMAJ 2021; 193: E381–E383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10]. Lavoie JG, Kornelsen D, Wylie L, et al. Responding to health inequities: Indigenous health system innovations. Global Health, Epidemiol Genom 2016. [cited 22 March 2020]; 1. https://www.cambridge.org/core/product/identifier/S2054420016000129/type/journal_article (accessed 29 March 2022). [DOI] [PMC free article] [PubMed]
- [11]. Harfield SG, Davy C, McArthur A, et al. Characteristics of Indigenous primary health care service delivery models: a systematic scoping review. Globaliz Health December 2018. [cited 22 March 2020]; 14(1). https://globalizationandhealth.biomedcentral.com/articles/10.1186/s12992-018-0332-2 (accessed 29 March 2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12]. Marchildon GP, Lavoie JG, Harrold J. Typology of Indigenous Health System Governance in Canada. Toronto: Institute of Public Administration of Canada, 2021. (accessed 15 November 2021). [Google Scholar]
- [13]. Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8:19–32. [Google Scholar]
- [14]. Young TK, Chatwood S, Ng C, et al. The north is not all the same: comparing health system performance in 18 northern regions of Canada. Int J Circumpol Health 2019;78:1697474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15]. Government of British Columbia. Health Boundaries – Province of British Columbia. [cited 12 June 2020]. https://www2.gov.bc.ca/gov/content/data/geographic-data-services/land-use/administrative-boundaries/health-boundaries (accessed 29 March 2022).
- [16]. NAO: North American Observatory on Health Systems and Policies. COVID-19 Policy Response Monitor. Institute of Health Policy, Management and Evaluation, University of Toronto. 2020. [cited September 2020]. https://ihpme.utoronto.ca/research/research-centres-initiatives/nao/covid19/ (accessed 29 March 2022). [Google Scholar]
- [17]. Richardson L, Crawford A. COVID-19 and the decolonization of Indigenous public health. CMAJ 2020;192:E1098–E1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18]. Hodder C, Corrigan S. Discovering the Path to Community Emergency Management Independence. 24 June 2020. https://attendee.gotowebinar.com/recording/6754072738334550288 (accessed 29 March 2022).
- [19]. Rahman MT, Sobur MA, Islam MS, et al. Zoonotic diseases: etiology, impact, and control. Microorganisms 2020;8:1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20]. Coyle SL, Boruch RF, Turner CF. Design and Implementation of Evaluation Research [Internet]. Evaluating AIDS Prevention Programs: Expanded Edition. National Academies Press (US); 1991. [cited 22 March 2021]. https://www.ncbi.nlm.nih.gov/books/NBK235374/ (accessed 22 March 2021). [PubMed] [Google Scholar]
- [21]. Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010;5:69. [DOI] [PMC free article] [PubMed] [Google Scholar]