Abstract
Introduction:
Revision total hip arthroplasty requires meticulous planning and execution to achieve the desired outcome. Pelvic vessel injury following total hip arthroplasty is rare, but a well-known and serious complication, having a very high morbidity (15%) and mortality (7%). This case demonstrates the rare occurrence of acetabular screw abutment to the external iliac vessels, which if removed during revision hip surgery without releasing the adhesions around it, will lead to avulsion injury of the vessels and a catastrophic event.
Case Report:
We present this challenging and unique case of a 64-year-old female patient where the acetabular component screw was found to be adherent to the external iliac vessels, with vascular injury imminent. During revision surgery, the iliac vessels were first released free of all adhesions with the intrapelvis screw using an ilioinguinal incision and retroperitoneal approach. The prosthesis was removed using a posterior approach to the hip joint. Definitive surgery was performed after 2 weeks.
Conclusion:
Surgeons should be cognizant of the possibility of an avulsion vascular injury in revision cases having intrapelvic screws or implants. The proximity of such an implant with the intrapelvic vasculature must be confirmed preoperatively. Management should be individualized. Dual approach and staged procedure help in a favorable outcome. Vascular injury, revision total hip arthroplasty, screw abutting iliac vessel, external iliac vessel, computed tomographic angiography.
Keywords: Vascular injury, revision total hip arthroplasty, screw abutting iliac vessel, external iliac vessel, computed tomographic angiography
Learning Point of the Article:
Awareness of vascular avulsion injury can prevent potentially life-threatening situations in Total Hip Arthroplasty.
Introduction
The incidence of vascular injury following total hip arthroplasty (THA) ranges from 0.04% to 0.1% [1]. The incidence increases to 0.2% in revision THA (RTHA) cases, with the external iliac and the common femoral vessels being the most injured [1]. The associated 15% morbidity and 7% mortality [2] require surgeons to understand how to recognize, confirm, and effectively manage such injuries to prevent life-threatening situations.
Identifiable risk factors for vascular injury around the hip can be patient related like vascular atherosclerosis, altered vascular anatomy, impaired hip anatomy due to multiple previous surgeries, skin scarring, etc. or surgeon related like misplacement of Hohmann retractors or its excessive retraction, medial acetabulum wall breach while reaming, direct perforation of the artery with drills bits or screws, thermal injury from bone cement extravasation, etc. [3]. The external iliac, gluteal, obturator, and femoral vessels are at a higher risk of injury due to proximity to the acetabulum [2].
Wasielewski et al. described the acetabular quadrants for secure placement of the acetabular screws during primary THA. The posterior upper quadrant followed by the posterior lower quadrant is considered to be relatively safe [4]. Here, we present a case explaining the caution to be kept in mind when approaching RTHA with intrapelvic screws during index surgery.
Case Report
A 64-year-old female patient complaining of progressive shortening of the left lower limb for the past 1 year was admitted to our hospital. She was operated for left THA 3 years ago in some other hospital. The clinical examination of the left hip showed restricted flexion range, abduction range, and external rotation of the hip with a true shortening of 3 cm. Surgical scars from previous surgery had healed well. There was no fever, local warmth, local redness, or tenderness present. A plain anteroposterior radiograph of the pelvis with both hips showed acetabular component loosening and superior migration. Screws used for acetabular shell fixation were found to be protruding into the pelvis, medial to Kohler’s line (Ilioischial line) in the unsafe zone (Fig. 1). Unfortunately, we did not have access to radiographs before and after primary surgery and during follow-ups for detailed assessment. Obturator and iliac views of the pelvis (Fig. 2) were taken, which revealed all acetabular screws to be intrapelvic, far beyond the safe zone. One screw had broken due to prosthetic migration. Three dimensional computed tomography (Fig. 3) confirmed our findings. Acetabular bone loss was classified by Paprosky classification as Type 3A that is, superior and lateral migration ≥3 cm with intact medial support (Kohler’s line). To assess the proximity of these screws with the intrapelvic vasculature, a computed tomographic (CT) angiography of the pelvis with the lower limb was performed which, to our surprise, revealed one screw tip being interposed between the external iliac artery and vein (Fig. 4 and 5) and a catastrophic vascular injury waiting to happen. Normal blood flow was noted through these vessels without any evidence of pseudoaneurysm formation.
Figure 1.
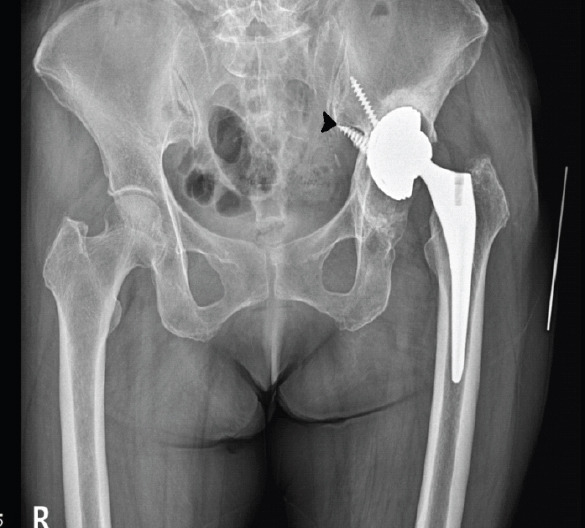
Anteroposterior view of pelvis with both hips at the time of presentation – Shows left hip acetabular component loosening with superior migration and two screws protruding into the pelvic cavity (Arrowhead).
Figure 2.
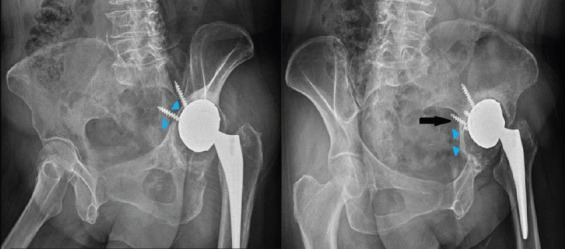
Special views of the pelvis – obturator view (left) showing excessively long screws pointing into the pelvic cavity. Furthermore, note the thinned-out anterior column of the acetabulum (arrowheads) and iliac view (right) showing a broken screw (arrow). Note the posterior intact but thinned out acetabulum column (arrowheads).
Figure 3.
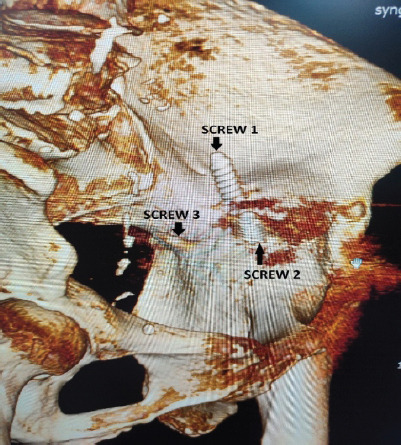
3D CT of the pelvis showing the three screws when seen from the inner aspect of the pelvis. They have been arbitrarily labeled as Screw 1 for the superior most screw, Screw 2 for the anterior screw, and Screw 3 for the posterior most screw (Broken Screw).
Figure 4.
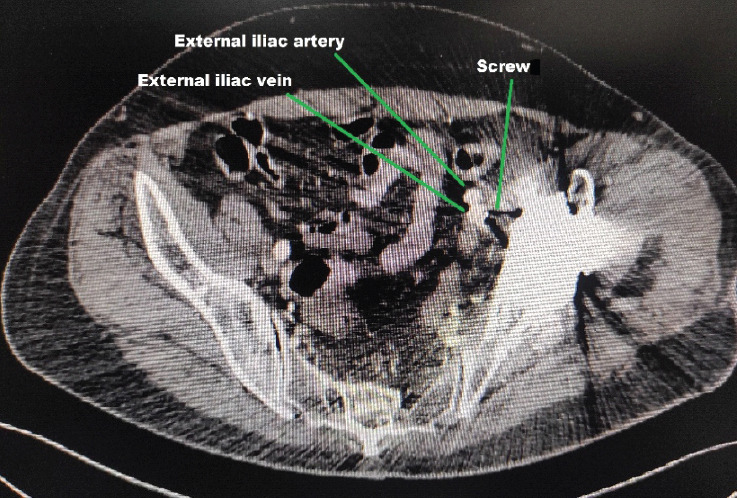
Axial cut of CT Angiography of the pelvis – The screw tip in extreme proximity to the external iliac vessels can be seen.
Figure 5.
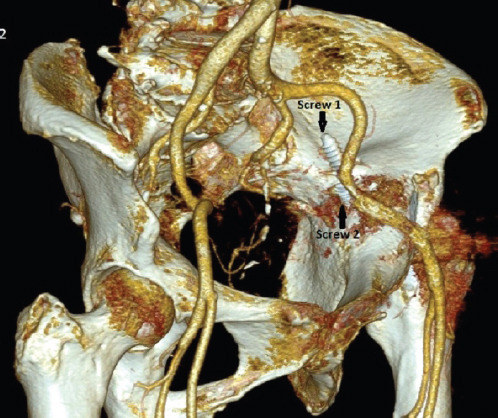
3D reconstructed CT Angiography of the pelvis – A better visualization of the screw previously labeled as Screw 2, abutting the external iliac artery.
Long-standing symptoms led us to believe that there will be adhesions all around the screw, entangling the surrounding vascular structure. After a detailed discussion with the patient, an early intervention was planned in two stages. Revision surgeries are extensive with longer surgical duration, more blood loss, and a prolonged rehabilitation period. This case, in particular, was more extensive as it required two approaches, one for releasing adhesions around the screw and freeing the vessels and the second for prosthesis removal and definitive surgery. Furthermore, early prosthesis loosening, just 3-year post-primary surgery, made us suspicious of prosthetic joint infection. It had to be ruled out even in the absence of any clinical signs of infection and hence we felt a two-staged intervention to be appropriate. Intraoperative cell salvage facilities were not available to us. Attempting to remove the screw without adhesiolysis will lead to vessel avulsion injury, having very high mortality.
Pre-operative total leukocyte counts (TLC), erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP) levels were found to be within normal limits. In the first stage, adhesions between the vessels and the intrapelvic screw were released using an ilioinguinal incision to prevent any possible injury to the vessels while removing the screw. This stage was performed in the presence and guidance of a vascular surgeon who was well-versed in dealing with vascular complications. During the procedure, it was found that the screw was strongly adhered to the vessel. The external iliac vessels had to be carefully dissected away from the screw by releasing the adhesions all around (Fig. 6). Once the adhesions were released, the external iliac vessels were protected with saline-soaked gauze, the incision was temporarily closed and the patient was carefully repositioned from supine to lateral decubitus position. The hip joint was exposed through the posterior approach. After removal of the femoral component and the acetabular polyethylene liner, the screws were gently removed to explant the acetabular shell. The broken screw was completely embedded in the pelvic bone and could not be removed. We decided to leave it behind as it was not abutting any important structure. Intraoperative frozen section was not available at our hospital and therefore tissue samples were collected and sent for bacterial cultures. Antibiotic-laden polymethylmethacrylate cement containing 80mg Gentamicin and 2g Vancomycin was used to fill the acetabular cavity and proximal femoral canal (Fig. 7). Incision was closed, keeping a negative suction drain. The integrity of the external iliac vessels was reconfirmed (Fig. 8) and then the anterior incision was finally closed.
Figure 6.
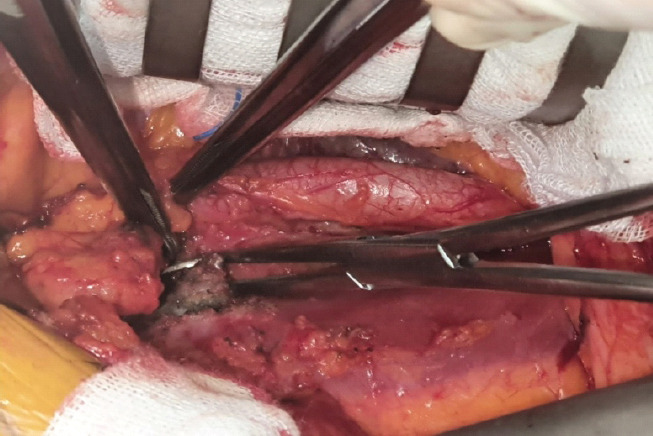
Intraoperative picture (First stage surgery) – Shows the screw tip which is separated away from the external iliac artery and vein through the ilioinguinal incision.
Figure 7.
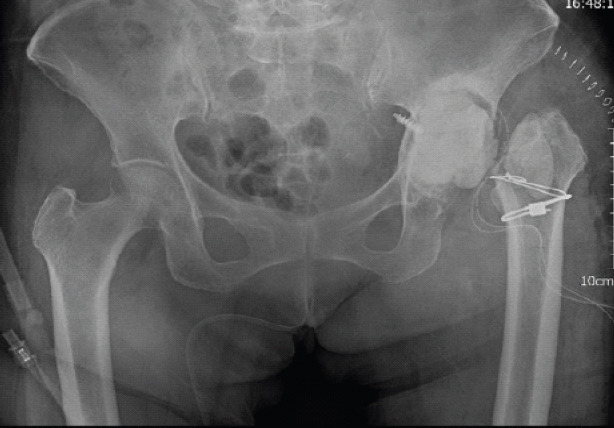
Post-operative radiograph of pelvis with both hips after Stage 1 surgery – Antibiotic laden cement filler in the left acetabulum and proximal femur seen. Prophylactic wiring of the proximal femur was done to prevent fracture during stem removal.
Figure 8.
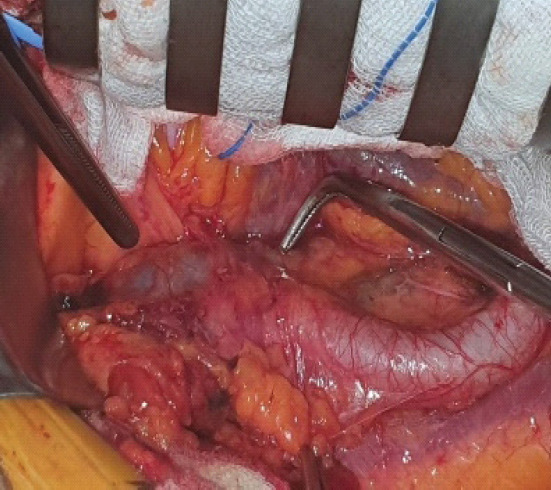
Intraoperative picture of the ilioinguinal incision (Before final Closure) – shows uninjured iliac artery and vein after screw and prosthesis removal.
Postoperatively, the patient was observed closely for any signs of internal bleeding and delayed injury to vessels. Infection assessment with parameters such as TLC, ESR, CRP levels, and daily drain output was done. Intraoperative samples for bacterial cultures turned out to be inconclusive, showing no bacterial growth after 2 weeks of incubation period.
Definitive surgery was then scheduled and during this surgery, the cement filler was extracted and the acetabular bone defect was reconstructed using trabecular metal augment in a flying buttress mode [5]. Impaction bone grafting using morselized allograft was done to build up the medial acetabular floor and a multi-hole uncemented acetabular shell was implanted. Acetabular screws were placed carefully according to the maximum bone available for fixation, the screw lengths were determined using the pre-operative CT scan. Screw insertion in the posterosuperior zone was not feasible due to the trabecular metal augment. A long hydroxyapatite-coated femoral stem was press-fitted. Post-operative radiograph shows correction of the limb length discrepancy (Fig. 9). In bed and bedside rehabilitation was started on the same evening. Toe-touch weight bearing, giving 20–30% of body weight was started on the third post-operative day with the help of a walker and full weight bearing was gradually allowed after 6 weeks.
Figure 9.
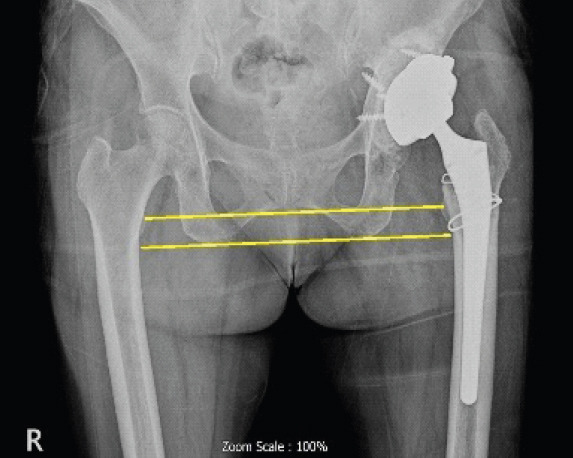
Post-operative radiograph of pelvis with both hips after the definitive surgery – Total hip arthroplasty performed using trabecular metal augment for tackling the acetabular bone loss. Note the correction of limb length discrepancy depicted by parallel interischial and intertrochanteric line.
Discussion
Identification and successful prevention of forthcoming external iliac vascular injury in an operated case of THA are illustrated in this case report.
Injury to pelvic vasculature due to an acetabular screw can have serious consequences, including death. Alshameeri et al., in their systemic review, found that major vascular injury during THA tolls to a mortality rate of about 7–9%, amputation in approximately 12–15%, and permanent disability in up to 17% [6].
About 40% of vascular injuries around the hip are reported to occur during RTHA [2]. The majority of them occurred during intrapelvic implant removal and were most commonly associated with metallosis, peri-implant fibrosis, and infection [2]. In addition, inflammatory response around the implants makes the vessel more adherent and non-resilient, making it prone to damage.
Lacerations or avulsion injuries of major vessels cause immediate heavy bleeding and are almost always recognized immediately. However, minute puncture injuries may be missed as they cause slow bleeding and result in false aneurysm formation. These are diagnosed later due to continuous slow occult bleeding, hematoma formation, or a pulsatile palpable mass [6]. Diagnosis of a pseudoaneurysm may be delayed for about a mean period of 9 months [6]. We were fortunate to not have any pseudoaneurysm formation in our case, in spite of the screw being so close to the vessels.
The first step in major vessel injury is to notify the anesthetist and operating room staff immediately. Anesthesiologists should ensure sufficient peripheral or central line access, start intravenous fluids, stabilize the patient and, if necessary, initiate cardiopulmonary resuscitation. Operating room personnel should call for assistance, arrange and open equipment needed for ancillary treatment, and make blood and blood products available immediately [7].
Meanwhile, the surgeon should try to identify the source of bleeding and aim to minimize it by applying local pressure whenever possible, making the patient supine (if not already) and giving a Trendelenburg position. If bleeding has occurred due to the drilling of a screw hole, a screw must be inserted immediately [8]. Unfortunately, intraoperative visualization and determination of the exact location of this vessel is impossible. If a vascular surgeon is available, an emergency exploratory laparotomy must be carried out. However, if facilities for vascular surgery are not available, the patient must be shifted on an emergency basis to a tertiary care center [7]. Pressure just above the umbilicus to compress the abdominal aorta and at the pelvic brim to compress the distal part of the external iliac vein may help to decrease bleeding while waiting for a vascular surgeon, especially when the patient is unstable or the facilities for transportation of the patient are not readily available [8]. The vascular surgeon may choose to do a vascular repair or bypass depending on the location and type of injury. The total duration of vessel compression must be noted as limb ischemia time. A vascular surgeon was available with us in the operating room and adhesiolysis was performed under his guidance. This precautionary step was necessary to circumvent any chance of vascular insult during the surgery and to tackle it immediately if it occurs.
In a RTHA, it, thus, becomes very crucial to assess these red flags preoperatively and plan accordingly. Screw projecting beyond ilioischial line has to be further evaluated with special radiographs of the pelvis and CT scans. The “Quad view” described by Wilson et al., projects an image that is parallel to the acetabular quadrilateral plate surface and is very useful for identifying medial wall breaches. The Quad view is nothing but an inlet obturator oblique view of the pelvis [9]. Diesel et al. recommended that every patient undergoing revision hip arthroplasty should ideally undergo a CT Angiography to look for the location of the vessels and their proximity to the prosthetic components if the screw or cement is migrated more than 5 mm beyond the ilioischial line [2].
In our case, the position of the screws indicated that it was probably not placed in the recommended safe zone during the index surgery. The external iliac vein was particularly at a significant risk of rupture if screw removal was performed without releasing the adhesions all around the screw.
To the best of our knowledge, this is the first case report which demonstrates the successful prevention of vascular injury of external iliac vessels due to an adherent screw from the acetabular component.
Conclusion
An understanding of the osseous and neurovascular anatomy pertinent to individual cases is crucial in minimizing potentially catastrophic complications. Surgeons should be cognizant of the possibility of an avulsion vascular injury if intrapelvic implant removal is attempted without adhesiolysis. The vicinage of such an implant with the intrapelvic vasculature must be confirmed preoperatively. Management should be individualized to the case. Two-staged operation and dual approach helps in a favorable outcome.
Clinical Message.
Surgeons should be cognizant of the possibility of an avulsion vascular injury if intrapelvic implant removal is attempted without adhesiolysis, especially when the implant is more than 5 mm beyond Kohler’s line.
Biography


Footnotes
Conflict of Interest: Nil
Source of Support: Nil
Consent: The authors confirm that informed consent was obtained from the patient for publication of this case report
References
- 1.Street MW, Howard LC, Neufeld ME, Masri BA. Vascular injuries during hip and knee replacement. Orthop Clin North Am. 2022;53:1–12. doi: 10.1016/j.ocl.2021.08.009. [DOI] [PubMed] [Google Scholar]
- 2.Diesel CV, Guimarães MR, Menegotto SM, Pereira AH, Pereira AA, Bertolucci LH, et al. Strategy to avoid vascular injuries in revision total hip arthroplasty with intrapelvic implants. Bone Jt Open. 2022;3:859–66. doi: 10.1302/2633-1462.311.BJO-2021-0188.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Payapanon P, Ruangsomboon P, Narkbunnam R, Chareancholvanich K, Pornrattanamaneewong C. Delayed femoral artery occlusion after total hip arthroplasty via the posterior approach:A single-case report from Thailand. Arthroplast Today. 2021;11:38–40. doi: 10.1016/j.artd.2021.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wasielewski RC, Cooperstein LA, Kruger MP, Rubash HE. Acetabular anatomy and the transacetabular fixation of screws in total hip arthroplasty. J Bone Joint Surg Am. 1990;72:501–8. [PubMed] [Google Scholar]
- 5.Jenkins DR, Odland AN, Sierra RJ, Hanssen AD, Lewallen DG. Minimum five-year outcomes with porous tantalum acetabular cup and augment construct in complex revision total hip arthroplasty. J Bone Joint Surg Am. 2017;99:e49. doi: 10.2106/JBJS.16.00125. [DOI] [PubMed] [Google Scholar]
- 6.Alshameeri Z, Bajekal R, Varty K, Khanduja V. Iatrogenic vascular injuries during arthroplasty of the hip. Bone Joint J. 2015;97-B:1447–55. doi: 10.1302/0301-620X.97B11.35241. [DOI] [PubMed] [Google Scholar]
- 7.Sandadi S, Johannigman JA, Wong VL, Blebea J, Altose MD, Hurd WW. Recognition and management of major vessel injury during laparoscopy. J Minim Invasive Gynecol. 2010;17:692–702. doi: 10.1016/j.jmig.2010.06.005. [DOI] [PubMed] [Google Scholar]
- 8.Melnic CM, Heng M, Lozano-Calderon SA. Acute surgical management of vascular injuries in hip and knee arthroplasties. J Am Acad Orthop Surg. 2020;28:874–83. doi: 10.5435/JAAOS-D-19-00697. [DOI] [PubMed] [Google Scholar]
- 9.Wilson JM, Pflederer JA, Schwartz AM, Farley KX, Reimer NB. Intraoperative radiographic detection of intrapelvic acetabular screw penetration:Lessons learned from our trauma colleagues. Arthroplast Today. 2021;8:226–30. doi: 10.1016/j.artd.2021.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]


