Abstract
Cardiomyopathies represent a diverse group of heart muscle diseases with varying etiologies, presenting a diagnostic challenge due to their heterogeneous manifestations. Regular evaluation using cardiac imaging techniques is imperative as symptoms can evolve over time. These imaging approaches are pivotal for accurate diagnosis, treatment planning, and optimizing prognostic outcomes. Among these, cardiovascular magnetic resonance (CMR) stands out for its ability to provide precise anatomical and functional assessments. This manuscript explores the significant contributions of CMR in the diagnosis and management of patients with cardiomyopathies, with special attention to risk stratification. CMR’s high spatial resolution and tissue characterization capabilities enable early detection and differentiation of various cardiomyopathy subtypes. Additionally, it offers valuable insights into myocardial fibrosis, tissue viability, and left ventricular function, crucial parameters for risk stratification and predicting adverse cardiac events. By integrating CMR into clinical practice, clinicians can tailor patient-specific treatment plans, implement timely interventions, and optimize long-term prognosis. The non-invasive nature of CMR reduces the need for invasive procedures, minimizing patient discomfort. This review highlights the vital role of CMR in monitoring disease progression, guiding treatment decisions, and identifying potential complications in patients with cardiomyopathies. The utilization of CMR has significantly advanced our understanding and management of these complex cardiac conditions, leading to improved patient outcomes and a more personalized approach to care.
Keywords: Cardiac magnetic resonance, Cardiomyopathies, Prognosis, Dilated cardiomyopathy, Hypertrophic cardiomyopathy, Restrictive cardiomyopathy
Core Tip: Cardiomyopathies encompass a diverse range of diseases affecting the heart muscle, each with varied causes. Symptoms of cardiomyopathies can manifest differently and change over time, necessitating regular evaluation through cardiac imaging techniques. These approaches play a crucial role in diagnosis, treatment guidance, and prognosis optimization. To enhance the precision of anatomical and functional evaluation and obtain valuable prognostic insights, cardiovascular magnetic resonance (CMR) is typically employed. By integrating CMR into clinical practice, clinicians can tailor patient-specific treatment plans, implement timely interventions, and optimize long-term prognosis This manuscript aims to explore how the CMR contribute to the diagnosis and management of patients with cardiomyopathies specially focus on the risk stratification.
INTRODUCTION
Cardiomyopathies encompass a diverse range of diseases affecting the heart muscle, each with varied causes. The European Society of Cardiology (ESC) traditionally categorizes them into hypertrophic, dilated, arrhythmogenic, restrictive, or other forms[1]. Moreover, they are further classified as either familial/genetic or non-familial/non-genetic. We must highlight that this classification is highly discussed[2].
Symptoms of cardiomyopathies can manifest differently and change over time, necessitating regular evaluation through cardiac imaging techniques. These approaches play a crucial role in diagnosis, treatment guidance, and prognosis optimization.
Patient evaluation involves gathering medical history, conducting a physical examination, and performing an electrocardiogram (ECG). Transthoracic echocardiography (TTE) can raise suspicions of cardiomyopathy. To enhance the precision of anatomical and functional evaluation and obtain valuable prognostic insights, cardiovascular magnetic resonance (CMR) is typically employed. In some cases, nuclear medicine tests or cardiovascular computed tomography may also be necessary.
This manuscript aims to explore how the CMR contribute to the diagnosis and management of patients with cardiomyopathies.
CARDIOMYOPATHIES WITH DILATED PHENOTYPE
CMR plays a crucial role in the diagnosis and evaluation of dilated cardiomyopathies (DCM). We usually distinguish the DCM on the basis of the etiology between two groups, the non-ischemic DCM (NIDCM) and ischemic DCM (IDCM).
Non-ischemic dilated cardiomyopathy
CMR plays a crucial role in the diagnosis and management of NIDCM. NIDCM is characterized by left ventricular (LV) enlargement, systolic dysfunction, and myocardial fibrosis without significant coronary artery disease[3] and absence of other abnormal loading conditions like hypertension, valvular heart disease or congenital heart disease. CMR provides a noninvasive and accurate assessment of LV morphology, function, and remodeling[3]. It allows for the quantification of myocardial fibrosis, which is useful in assessing viability in ischemic cardiomyopathy[4]. CMR can also provide detailed and clinically useful information about the type and severity of cardiac damage by characterizing tissue changes in the myocardium[5].
One important application of CMR in NIDCM is the identification and characterization of fibrosis microstructure. Late gadolinium enhancement (LGE) imaging, a technique used in CMR, can detect enhancement patterns associated with fibrosis in NIDCM patients[6]. Fibrosis microstructure has been found to modulate reentry in NIDCM, and understanding these variations can improve risk stratification and guide treatment decision[6]. Computational modeling based on CMR images has been used to examine variations in fibrosis microstructure and quantify their effect on reentry inducibility and mechanism[6]. This information can help identify patients at high risk of sudden cardiac death (SCD) and guide the selection of appropriate interventions[6]. CMR is also valuable in differentiating NIDCM from other cardiomyopathies. CMR-derived myocardial parameters, such as total LV myocardial mass index and percentage of non-compacted myocardium, have been found to be discriminators between patients with LV non-compaction cardiomyopathy, other cardiomyopathies, and healthy controls[6]. This differentiation is important for accurate diagnosis and appropriate management of patients with NIDCM[7].
Furthermore, CMR can provide prognostic information in NIDCM. Global longitudinal strain (GLS) of the left ventricle measured by CMR feature tracking (FT) analysis has revealed enhanced prognostic utility when compared to conventional parameters in NIDCM[8]. Moreover, researchers have investigated the prognostic significance of right ventricular (RV) GLS through CMR-FT analysis has been evaluated in a cohort of individuals with NIDCM[8]. These investigations collectively highlight the promising ability of CMR to predict significant cardiac events and events related to heart failure in patients with NIDCM[8].
In relation with sequences like T2-STIR, T1, T2 and Extracellular volume (ECV) mapping there is controversial data some experts state that T1 and ECV have limited value that is explained by the reduced precision in NIDCM due to thinning of the myocardium[9]. Other authors have claimed some potential value of T1 and ECV, elevated ECV and T1 measurements have demonstrated prognostic significance regardless of LV ejection fraction (LVEF) and the presence of LGE[10]. Moreover, an elevated native T2 value suggests the potential existence of myocardial edema, potentially indicating the presence of inflammatory cardiomyopathy[11]. These methods present encouraging novel approaches for risk assessment; nevertheless, additional validation remains necessary.
In summary, CMR is playing a crucial role in the diagnosis, risk stratification, and prognostication of NIDCM. It provides valuable information about LV morphology, function, and remodeling, as well as the presence and characteristics of myocardial fibrosis. CMR can differentiate NIDCM from other cardiomyopathies and help guide treatment decisions. Additionally, CMR-derived parameters, such as GLS, have shown prognostic value in NIDCM. Overall, CMR is a valuable tool in the comprehensive evaluation and management of NIDCM patients.
Ischemic dilated cardiomyopathy
CMR plays a crucial role in the diagnosis and evaluation of IDCM. IDCM is a type of DCM that is caused by ischemic heart disease (IHD)[12]. Approximately 70% of heart failure cases have been attributed to IHD[13]. From the SOLVD study, IHD tended to have a greater impact than NIDCM, with double the risk of hospitalization and quadruple the risk of death[14].
CMR as we shown before this technique can aid in the differentiation of ischemic from non-ischemic cardiomyopathy subtypes. Currently, CMR-derived cardiac imaging is effective for both definition of IHD and for ischemia detection, with important diagnostic and prognostic implications[15].
The “function-perfusion-tissue characterization” triad should be studied in IHD for an adequate evaluation of cardiac viability and ischemic burden. As mentioned, the subendocardial distribution of LGE identifies an ischemic injury as opposed to fibrosis with meso- or subepicardial distribution, typical of non-ischemic alterations[16] CMR is also effective in defining myocardial viability through discrimination of LGE extension and segmental kinesis[4,17].
From the SPINS registry, extensive ischemic burden was related to a higher risk of major cardiac event, including hospitalization for congestive heart failure (HF), and revascularization was associated with a protective effect only in the extensive ischemia subset[18-21].
CARDIOMYOPATHIES WITH HYPERTROPHIC PHENOTYPE
LV hypertrophy (LVH) is most frequently caused by pressure overload. However, in cardiomyopathies, LVH occurs in the absence of abnormal loading conditions – hypertrophic cardiomyopathy (HCM) accounts for the majority of these cases.
CMR imaging has consolidated its role among the multimodality evaluation of myocardial disease, mostly due to high spatial resolution and unique ability for tissue characterization[22,23]. Non-invasive tissue characterization is crucial for differential diagnosis of LVH, identification of HCM phenocopies and risk stratification. This distinctive feature of CMR has led to a decrease in the use of endomyocardial biopsy (EMB) in cardiomyopathies with LVH, that is now restricted to few indications[24,25]. A recent position statement limited EMB use to patients with LVH in whom non-invasive evaluation produces inconclusive or discordant results, and there is clinical suspicion of phenocopies, particularly infiltrative or storage disease for which target treatment is available[25].
An Integrative CMR approach, Incorporating morphofunctional assessment with tissue characterization, including identification of the presence, location, and pattern of LGE, and combined with parametric mapping findings (particularly, native T1 and ECV), can be of value for differential diagnosis of hypertrophic phenotypes of cardiomyopathy (Table 1).
Table 1.
Cardiac magnetic resonance findings in hypertrophic cardiomyopathy and phenocopies
|
|
Morphologic features
|
Tissue characterization
|
||
|
LGE
|
Mapping
|
ECV
|
||
| Athlete’s heart | Balanced increase in wall thickness and cavity size | Absent or in RV insertion points | Normal or decreased T1 | Normal or decreased |
| Hypertrophic cardiomyopathy (sarcomeric) | Typically asymmetric LVH, with septal predominance | Mid-mural, patchy, affecting most hypertrophied segments; transmural in advanced stages | Increased native T1, regardless of LGE presence, reflecting interstitial fibrosis | Increased ECV attributed to fibrosis |
| Amyloidosis | Symmetric or asymmetric LVH | Subendocardial, global, diffuse; transmural in advanced stages. LGE reflects infiltration, not fibrosis; abnormal gadolinium kinetics | Marked increase in native T1 value (AL > ATTR) due to protein accumulation | Markedly increased ECV reflecting protein accumulation |
| Fabry disease | Concentric LVH, prominent papillary muscles, RV hypertrophy | Mid-mural, basal inferolateral segment | Decreased native T1 values (lipid storage); pseudonormalization in advance stages due to fibrosis. Elevated T2 levels due to inflammation | Normal ECV |
ECV: Extracellular volume; LGE: Late gadolinium enhancement; LVH: Left ventricular hypertrophy; RV: Right ventricle.
Athlete’s heart
CMR is also useful for distinguishing pathological LVH from physiological adaption to exercise. The “athlete’s heart” is characterized by biventricular, symmetrical remodelling, and is associated to a concomitant and proportional increase in cavity size[26,27]. Specific reference values of ventricular size and function for athletes have been reported by D’Ascenzi et al[27] In athletes, the degree of hypertrophy is usually mild, and LV wall thickness rarely exceeds 12 mm[28]. Moreover, reversal of adaptative LVH can be achieved with detraining[29]. When present, in athletes, LGE is usually confined to the RV insertion points (mostly the inferior), and its presence has been correlated with training load and intensity[30]. This pattern of fibrosis does not affect prognosis nor requires further evaluation in otherwise healthy athletes[30]. Mapping data may further differentiate “athlete’s heart” from HCM: While the latter is usually associated with increased native T1 and ECV (reflecting interstitial fibrosis)[28,30], these parameters are normal, or even decreased, in athletes. Although echocardiography remains the major imaging tool for athlete pre-participation screening, CMR can be paramount in situations where suspicious of myocardial disease persists based on symptoms, family history, electrocardiographic or echocardiographic data.
HCM
HCM is defined by unexplained LVH in a non-dilated LV with wall thickness ≥ 15 mm or, alternatively, ≥ 13 mm, in the presence of positive family history or a disease-causing gene variant[22]. HCM, the most common genetic cardiovascular disease, with a prevalence of 1:200-1:500, is caused by sarcomeric gene mutations, that are inherited as an autosomal dominant trait[31]. There is marked phenotypic heterogeneity among HCM probands, even among individuals from the same family, that occasionally poses a challenge in terms of diagnosis and risk stratification.
Morphofunctional evaluation: The “classical” HCM phenotype consists of asymmetrical, septal-predominant hypertrophy, that may be associated to dynamic LV tract obstruction (LVOTO)[31]. In hypertrophied hearts, CMR enables precise measurement of maximal wall thickness and an accurate portrayal of LVH pattern, extent and distribution[28]. This is of particular importance in the presence of midventricular or apical variants of HCM, in which echocardiographic evaluation encounters limitations[23].
The presence of apical aneurysms is associated to higher rates of ventricular arrhythmias (VA), SCD, thromboembolic events, and heart failure in patients with HCM[32,33]. CMR has enabled more frequent identification of this high-risk subset of patients, by detecting small aneurysms that may remain unnoticed during non-contrast echocardiographic evaluation[23] but are still relevant for risk stratification. Accordingly, the presence of an apical aneurysm, regardless of size, has been considered a major risk factor by the American College of Cardiology/American Heart Association (ACC/AHA) guidelines, assigning it a class IIa (level of evidence B) recommendation for implantable cardioverter-defibrillator (ICD) implantation for primary prevention of SCD[34]. The ESC guidelines on SCD prevention have recently included LV apical aneurysm as an additional factor for consideration of an ICD (class IIb recommendation, level of evidence B)[35], even in patients with a low estimated risk according to the HCM Risk-SCD score[36].
Detection of thrombi within the scared LV apex also carries meaningful management considerations. In a recent study, Lee et al[37] found a linear relationship between aneurysm size and the risk of adverse events, including apical thrombus formation and thromboembolic stroke. Moreover, patients with an aneurysm size ≥ 2 cm showed a significant increase in 5-year SCD risk (9.7% vs 2.9%, P = 0.037)[37].
Other morphologic abnormalities related to HCM can be further demonstrated by CMR, including mitral subvalvular apparatus abnormalities or myocardial crypts. Maron et al reported the presence of myocardial crypts – narrow, deep blood-filled invaginations within LV myocardium – in 61% of genotype positive/phenotype negative (G+P-) patients without overt LV hypertrophy, suggesting this morphologic feature to be part of the phenotypic expression of HCM[38]. Contrastingly, in a large Danish cohort assessed by computed tomography, LV crypts were frequent among the general population, and were not associated with a composite endpoint of death, myocardial infarction, heart failure, or stroke[39]. However, among family members of patients with HCM, the presence of crypts may prompt careful follow-up to monitor progression to an overt phenotype.
Another subclinical marker of HCM observed by CMR has been proposed by the same group – LV apical-basal muscle bundles. LV muscle bundles were suggested as a latent marker in G+/P- individuals, and were related to HCM phenotypic expression, irrespective of LV wall thickness[40].
CMR is useful for depicting papillary muscle (PM) architecture and functional abnormalities. PM hypertrophy (minor axis diameter > 11 mm or combined mass > 7 g/m2) is present in more than half of HCM cases, and my contribute to mid-ventricular obstruction[41,42]. Additional abnormalities that contribute to LVOTO, such as accessory, bifid or displaced PM, can be adequately demonstrated by CMR[41].
Tissue characterization: The presence of LGE in HCM reflects replacement fibrosis, and its prognostic value is well-established[43]. LGE is found in more than half of HCM patients, usually presenting an mid-mural pattern within the most hypertrophied segments[43,44]. In advanced stages of the disease, LGE with transmural extension can be observed and carries a worse prognosis[44].
LGE has been consistently associated increased SCD incidence, and its presence and extent was included as a major risk factor in the ACC/AHA risk stratification algorithm[34] and, more recently, in the 2022 ESC Guidelines for prevention of SCD[35]. In a landmark multicenter study, LGE exceeding 15% of the LV mass was associated with a > 2-fold risk of SCD in patients who were deemed low risk by conventional tools, compared with patients in whom LGE was absent[43]. Therefore, presence of “extensive LGE” (≥ 15% of total LV mass) is regarded as a high-risk parameter, and in HCM patients without a defibrillator, CMR should be repeated every 3-5 years to monitor LGE progression and reconsider SCD prevention strategies[23,34].
T1 mapping and ECV (derived from native and post-contrast T1) allow for identification of diffuse, interstitial fibrosis[23]. Native T1 and ECV may be elevated in segments without LGE, and even in variant carriers without overt LVH[28]. Mapping techniques allow differentiation of HCM from phenocopies (Table 1).
Edema with abnormal T2 findings (T2-Stir) could be observed in HCM patients often indicative of an acute myocardial injury (i.e., ischemic extravascular damage) and associated with electrical instability[45].
Perfusion: Microvascular dysfunction is part of the pathophysiology of HCM and can be evaluated by means of CMR perfusion imaging. In HCM, reduced myocardial blood flow correlates with increased LV wall thickness and mass, presence of LGE, and increased ECV[23,28]. Aguiar Rosa et al[46] showed that increased ischemia severity, assessed by CMR, was associated with higher values of native T1 and greater LGE extension. Patients with severe ischemia demonstrated higher incidence of atrial arrhythmias and performed poorer in cardiopulmonary stress testing[46].
HCM phenocopies
CMR has an increasing role in the evaluation of rare forms of myocardial disease that also manifest with LVH, otherwise known as phenocopies of HCM. In such cases, family history, electrocardiographic patterns and extracardiac manifestations may raise diagnostic suspicion, that may be corroborated by imaging findings.
Amyloidosis: Cardiac amyloidosis (CA) produces LV “pseudo-hypertrophy”, resulting from interstitial expansion due to amyloid fibrils deposition, rather than from myocyte proliferation[47]. Transthyretin (ATTR), both hereditary and wild-type, and immunoglobulin-derived light chain amyloidosis are responsible for most cases of amyloid-related myocardial disease[48]. Extracellular expansion in CA is depicted in CMR parametric mapping findings by a marked increase in native T1 Levels and ECV[28]. Patients with CA show global, diffuse subendocardial LGE, that may become transmural in more advanced stages of the disease. This pattern of LGE, in the adequate setting, is very specific for CA[49]. LGE not rarely extends to the RV and the atria, particularly in ATTR[28]. Another characteristic CMR feature in CA is the abnormal gadolinium kinetics, with myocardial nulling preceding with the blood pool, or an equalization of these points[48,49]. More detailed information will be provided in the section entitled cardiomyopathies with restrictive phenotype.
Fabry disease: Fabry disease (FD), an X-linked lysosomal storage disorder, usually leads to concentric LVH, due to both glycosphingolipid accumulation and myocyte hypertrophy[50]. Prominent PM s are a typical feature of FD, as is concomitant RV hypertrophy[28,44].
Parametric mapping is of particular utility for the differential diagnosis of FD. Native T1 decreases with lipid deposition[22]; accordingly, in early stages of FD, native T1 values are low, when compared to normal reference values and other forms of LVH[28,50]. However, as disease progresses and replacement fibrosis becomes evident, pseudo-normalization of native T1 relaxation times occurs[28,50]. ECV remains within normal range in LGE-free areas[50], since FD leads to intracellular storage of glycosphingolipids. T2 values can be elevated due inflammatory response triggered by lipid accumulation.
LGE is present in > 50% of FD patients, and is usually located in the LV basal inferolateral segment, with a mid-mural or subepicardial pattern[22,44,49]. Presence of LGE has been reported in female mutation carriers without LVH[49]. Similar to HCM, presence of LGE in FD is associated to adverse outcomes and poor response to replacement therapy[50].
CARDIOMYOPATHIES WITH RESTRICTIVE PHENOTYPE
Less than 5% of all cardiomyopathy cases are attributed to restrictive cardiomyopathies (RCM), which have a diverse range of causes[51].
RCM is characterized by a significant alteration in myocardial compliance, presenting severe diastolic dysfunction while maintaining preserved systolic function, especially in the early stages. The initial diagnosis typically involves a TTE that reveals normal or increased LV wall thickness, often with a concentric or symmetric distribution, along with a restrictive pattern observed through Doppler analysis. It also shows the absence of LV dilation, preserved LVEF, and significant biatrial enlargement[52]. However, while TTE plays a crucial role in the initial assessment and raising diagnostic suspicions, its utility becomes limited when establishing a differential diagnosis. In such cases, CMR imaging becomes highly relevant.
Two of the most common entities where CMR is essential are the endomyocardial fibrosis (EMF) and CA.
EMF
EMF represents a rare subtype of RCM. It is characterized by an unusual thickening of the endocardium, resulting from the deposition of fibrous tissue[53]. This condition is typically secondary to various factors, including infections (often found in tropical regions), inflammation, exposure to toxic agents, among others. Echocardiographic observations in EMF include apical obliteration due to thickening of the endocardium, a reduction in ventricular cavity size, and a pronounced restrictive diastolic pattern. EMF can primarily affect the left ventricle, both the left and right ventricles (in approximately 50% of cases), or predominantly the right ventricle[54]. The presence of apical thrombus is also a frequently encountered feature.
CMR is the gold standard for EMF evaluation and specifically for localization, characterization, and quantification of fibrous tissue by LGE sequences. LGE strongly correlates with histopathological findings and its extension is associated with increased mortality risk[55]. CMR may also identify apical thrombus or calcifications.
CA
In patients with CA, cine sequences or functional assessment methods provide a means to observe the structural characteristics of the infiltrated myocardium. These characteristics encompass biventricular hypertrophy, thickening of cardiac valves, interatrial septum, pericardial effusion, and biatrial dilation. Additionally, these techniques enable the precise evaluation of both systolic and diastolic function[56]. It is essential to not only focus on the assessment of the LV but also on the other cardiac chambers. Notably, the involvement of RV has been identified as a predictor of mortality in CMR, consistent with findings from TTE[57]. As the disease advances into later stages, there is a notable increase in atrial volume and dysfunction. This phenomenon is attributed to the direct infiltration of amyloid fibrils into the atria and indirectly to elevated filling pressures due to diastolic dysfunction.
The Table 2 summarizes the main cardiac magnetic resonance (CMR) findings in CA with an explanation of the prognostic and diagnostic implications.
Table 2.
Cardiac magnetic resonance findings in cardiac amyloidosis. Prognostic and diagnostic implications
|
Parameter
|
Implications
|
Ref.
|
| Reduction of the total left atrial emptying fraction in AL-CA patients | + Related to more advanced stages of the disease and with a worse functional class; + Increase in 2 years-mortality if its value < 16% | Mohty et al[79] |
| MCF and LAS in AL-CA patients | + If LAS > -7% and MCF < 52.6% greatest risk of death and heart transplantation | Arenja et al[80] |
| Anterior aortic plane systolic excursion in AL-CA patients | + Best predictive value for transplant-free survival | Ochs et al[81] |
| Strain | + Correlates well with the level of LGE uptake an alternative to LGE where contrast should not be used; + GLS impaired robust predictor of all-cause mortality in AL-CA patients | Wan et al[82] |
| Look-Locker sequence (T1 sequence with different inversion times) | + Increased risk of death if it is impossible to obtain a normal myocardial signal on LGE using this sequence with inversion time over than 300 ms | Mekinian et al[83] |
| LGE | + Typical pattern is a diffuse subendocardial uptake and also it was described a transmural pattern enhancement and less frequently a focal patchy one; + Controversy exists regarding the prognostic implication | Maceira et al[84], Fontana et al[85], Raina et al[86] |
| The difference in the intramyocardial T1 value post-gadolinium between subepicardium and subendocardium | + Worse survival when that difference was lower than 23 ms | Maceira et al[84] |
| Diffuse subendocardial uptake detected using a modified LGE-CMR protocol with visual T1 assessment | + High diagnostic precision (PPV 93%, NPV 90%); + Significantly associated with 2 yr mortality | Austin et al[87], White et al[88] |
| RV gadolinium uptake in AL-CA patients | + Independent predictor of survival during a period of 6 mo follow up | Wan et al[89] |
| QALE | + Score > 9 predicted worse survival, especially useful in patients with a subendocardial LGE pattern | Wan et al[90] |
| Noncontrast T1-mapping | + A cut-off value of 1020 ms had high sensitivity and specificity (around 90%) for identifying amyloid patients with possible or definite cardiac involvement | Karamitsos et al[91] |
| T1 mapping with native T1 and extracellular volume | + Patients with AL-CA and suspected cardiac involvement had increased values; + Only ECV had a significant prognostic implication with greater mortality if its value was > 44%; + Basal ECV had the best prognostic value amongst myocardial T1 mapping parameters | Karamitsos et al[91], Lin et al[92], Wan et al[93] |
| T2-weighted imaging | + No gadolinium administration is needed; + A decreased myocardial signal intensity compared with skeletal muscle was associated with shortened survival; + T2 ratio value < 1.36 had a weak sensitivity and specificity (63% and 73% respectively) to predict cardiac involvement | Wassmuth et al[94], Legou et al[95] |
AL-CA: Light chain cardiac amyloidosis; CMR: Cardiovascular magnetic resonance; ECV: Extracellular volume; GLS: Global longitudinal strain; LAS: Long axis strain; LGE: Late gadolinium enhancement; MCF: Myocardial contraction fraction; NPV: Negative predictive value; PPV: Positive predictive value; QALE: Query amyloid late enhancement score; RV: Right ventricle.
To sum up, CMR represents a complementary diagnostic step in the evaluation of patients suspected of having CA. This imaging method is not widely accessible in numerous medical facilities, and its lengthy duration per study restricts the total number of examinations feasible in a day.
ARRHYTHMOGENIC CARDIOMYOPATHY
Arrhythmogenic cardiomyopathy (ACM) is an inherited cardiomyopathy characterized by replacement of myocardium by fatty and fibrous tissue. Historically named Arrhythmogenic Right Ventricular Cardiomyopathy (ARVC) because of the RV involvement, the late recognition of left and biventricular forms led to the new term ACM, encompassing both phenotypes. VA through macro-reentry mechanism related to the fibrofatty involvement is one of the main clinical presentations, manifesting in the worst case by SCD. In the advanced stages, the disease is characterized by heart failure[58,59].
Diagnosis criteria established by the International Task Force (ITF) included morphological (dysfunction and structural alteration) and anatomopathological characterization, ECG abnormalities, history of arrhythmias and family history[60]. CMR role was limited to evaluation of regional RV motion wall, RV ejection fraction (RVEF) and RV end-diastolic volume. Critics have been raised about the absence of LV involvement and the limited role of CMR. In 2020, the Padua Criteria was proposed, revisiting the ITF criteria by including tissue characterization provided by CMR. Functional or structural abnormality is enough for the diagnosis[61]. Pathogenic mutations, ECG abnormalities, or VA are no longer sufficient. This highlights the role of CMR, which has become one of the preferred non-invasive imaging techniques, allowing an increase of diagnostic sensitivity for ACM. CMR offers an advanced evaluation of the heart, including ventricular morphology, volume, thickness, ejection fraction, regional motion, myocardial fibrous, adipose content, edema, flow, LGE, as well as new emerging and promising feature as global longitudinal and circumferential strain (assessed by using feature-tracking CMR). Despite its complete evaluation, CMR has some limitations: fatty infiltration is nonspecific and does not preclude the diagnosis.
Prognosis in ACM is mostly related to VA. ICD being the only intervention improving survival[62], risk stratification is vital to identify the high-risk patients benefiting the most from primary prevention ICD implantation. RV dysfunction and syncope history are strong predictor for arrhythmia event and have been both included in the guidelines. CMR is not included in the risk stratification recommendations, neither in the 2019 Heart Rhythm Society guidelines[63], nor the 2022 ESC guidelines for the management of patients with VA and the prevention of SCD[35]. In this context, CMR role is only limited to diagnosis. A 2019 consensus expert developed the ARVC 5-year Risk-VAs calculator: A prediction model for VA risk to guide decision regarding primary prevention ICD (www.arvcrisk.com)[64]. CMR is included only to assess RVEF. CMR parameters of tissue characterization and regional wall motion of both ventricles were not included. The role of CMR in risk stratification remains to be determined. Lack of consistent studies explains the absence of CMR from the risk stratification recommendation, even though some emerging data shows the potential prognosis information provided by CMR.
Different CMR phenotype of ACM are associated with different prognoses. Normal CMR has an excellent negative predictive value for major clinical events[65-67]. Tandri et al[68] showed that delayed gadolinium enhancement of RV correlates with inducible VT during electrophysiology testing. Lie et al[69] confirm that CMR findings, as low RVEF, RV wall-contraction abnormalities, or RV aneurysms are predictors of life-threatening ventricular arrhythmia. Evaluation of longitudinal strain by feature-tracking CMR could also bring risk stratification information, as reduced strain seems to be associated with sustained VA[70].
Regarding the LV involvement, its association with adverse outcomes is inconsistent[71]. Presence of LV dysfunction is associated with arrhythmic adverse outcomes as reported by a small European registry[72]. Some studies have suggested that CMR imaging features of LV phenotypes, as fat infiltration and LGE, in ACM may be associated with adverse outcomes. Aquaro et al[66] highlight that the different CMR presentations of ACM are associated with different prognoses, LV involvement (LV dominant and biventricular) being the worst prognosis. Zhang et al[73] confirm the bad prognosis of LV LGE, being associated with an increased risk of ICD therapy and cardiac death, independently of LVEF. LV myocardial assessment by CMR could also predict the HF-related event risk as reported by Chun et al[74]. On the contrary LV dysfunction was not a predictor of arrhythmic risk in two meta-analysis[75,76]. Zghaib et al[77] showed that LV fibrofatty infiltration in CMR was not associated with arrhythmic outcomes. The role of identification of LV involvement by CMR and its prognosis significance remains to be established.
There is some potential speculation on some cases of ACM that could be explained by an inflammatory activity or hot phase, if the diagnosis it is in a very early-stage sequences like T2-STIR for oedema detection could help[78], this hot phase could be related with arrhythmias during the disease.
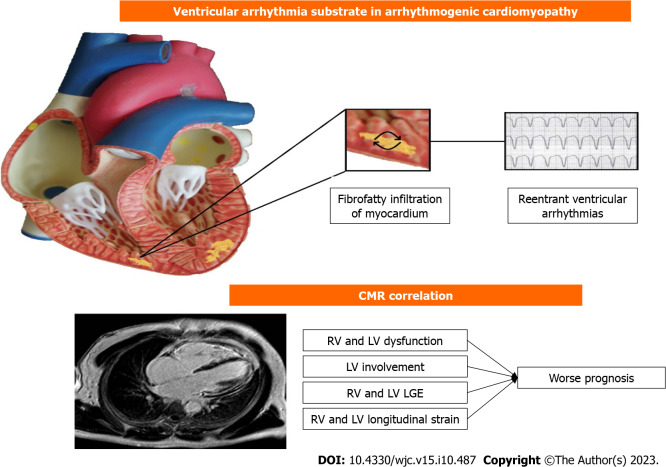
To finalise, CMR role in diagnosis is well established (Figure 1). Regarding the risk stratification, only RV function is validated in international guidelines and risk calculator. Lack of consistent data about correlation between CMR characterization and adverse outcomes could explain the absence of CMR role from guidelines, but a few emerging studies show new evidence about CMR imaging, Indicating that the presence of structural abnormalities in the RV as observed through CMR plays a crucial role in evaluating the risk of arrhythmias. : RV dilatation, dysfunction and LGE are among the strongest predictors. Regarding the LV involvement, the few data are contradictory, but may trend towards an association with high-risk event. CMR may have a promising role in association with classical clinical feature, but further studies are needed to better define CMR place in risk stratification.
Figure 1.
Correlation between cardiac magnetic resonance and ventricular arrythmia in arrhythmogenic cardiomyopathy. CMR: Cardiac magnetic resonance; RV: Right ventricle; LV: Left ventricle; LGE: Late gadolinium enhancement.
CONCLUSION
Cardiovascular imaging methods play a vital role in investigating cardiomyopathies, furnishing valuable diagnostic and prognostic insights. The inclusion of CMR in the evaluation of all patients is highly recommended, owing to its ability to offer comprehensive anatomical, functional, and tissue-specific data, which holds significant prognostic value. While other imaging techniques might be employed selectively, the integration of multiple modalities of cardiac imaging assumes a crucial role in clinical decision-making, leading to enhanced patient management and care outcomes.
Footnotes
Conflict-of-interest statement: All the authors report no relevant conflicts of interest for this article.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: July 30, 2023
First decision: September 4, 2023
Article in press: September 27, 2023
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: Spain
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Barison A, Italy; Yang YQ, China S-Editor: Lin C L-Editor: A P-Editor: Yuan YY
Contributor Information
Rafael Vidal-Perez, Servicio de Cardiología, Unidad de Imagen y Función Cardíaca, Complexo Hospitalario Universitario A Coruña Centro de Investigación Biomédica en Red de Enfermedades Cardiovasculares (CIBERCV), A Coruña 15006, Galicia, Spain. rafavidal@hotmail.com.
Mariana Brandão, Department of Cardiology, Centro Hospitalar de Vila Nova de Gaia/Espinho, Vila Nova de Gaia 4434-502, Portugal.
Wael Zaher, Department of Cardiology, Hôpital Erasme, Université Libre de Bruxelles, Brussels 1070, Brussels, Belgium.
Ruben Casado-Arroyo, Department of Cardiology, Hôpital Erasme, Université Libre de Bruxelles, Brussels 1070, Brussels, Belgium.
Alberto Bouzas-Mosquera, Servicio de Cardiología, Unidad de Imagen y Función Cardíaca, Complexo Hospitalario Universitario A Coruña Centro de Investigación Biomédica en Red de Enfermedades Cardiovasculares (CIBERCV), A Coruña 15006, Galicia, Spain.
Ricardo Fontes-Carvalho, Department of Cardiology, Centro Hospitalar de Vila Nova de Gaia/Espinho, Vila Nova de Gaia 4434-502, Portugal; Cardiovascular R&D Centre - UnIC@RISE, Department of Surgery and Physiology, Faculty of Medicine of the University of Porto, Porto 4200-319, Portugal.
Jose Manuel Vazquez-Rodriguez, Servicio de Cardiología, Complexo Hospitalario Universitario A Coruña, A Coruña 15006, A Coruña, Spain.
References
- 1.Elliott P, Andersson B, Arbustini E, Bilinska Z, Cecchi F, Charron P, Dubourg O, Kühl U, Maisch B, McKenna WJ, Monserrat L, Pankuweit S, Rapezzi C, Seferovic P, Tavazzi L, Keren A. Classification of the cardiomyopathies: a position statement from the European Society Of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2008;29:270–276. doi: 10.1093/eurheartj/ehm342. [DOI] [PubMed] [Google Scholar]
- 2.Rapezzi C, Aimo A, Barison A, Emdin M, Porcari A, Linhart A, Keren A, Merlo M, Sinagra G. Restrictive cardiomyopathy: definition and diagnosis. Eur Heart J. 2022;43:4679–4693. doi: 10.1093/eurheartj/ehac543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yang Z, Huang L. Editorial for "The Impact of Hypertension on Left Ventricular Function and Remodeling in Non-Ischemic Dilated Cardiomyopathy Patients: A 3.0 T MRI Study". J Magn Reson Imaging. 2023;58:172–173. doi: 10.1002/jmri.28480. [DOI] [PubMed] [Google Scholar]
- 4.Singh T, Joshi S, Meah MN, Spath NB, Papanastasiou G, Kershaw LE, Baker AH, Dweck MR, Newby DE, Semple SI. Repeatability and reproducibility of cardiac manganese-enhanced magnetic resonance imaging. Sci Rep. 2023;13:3366. doi: 10.1038/s41598-023-29591-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Patel AR, Kramer CM. Role of Cardiac Magnetic Resonance in the Diagnosis and Prognosis of Nonischemic Cardiomyopathy. JACC Cardiovasc Imaging. 2017;10:1180–1193. doi: 10.1016/j.jcmg.2017.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Balaban G, Halliday BP, Mendonca Costa C, Bai W, Porter B, Rinaldi CA, Plank G, Rueckert D, Prasad SK, Bishop MJ. Fibrosis Microstructure Modulates Reentry in Non-ischemic Dilated Cardiomyopathy: Insights From Imaged Guided 2D Computational Modeling. Front Physiol. 2018;9:1832. doi: 10.3389/fphys.2018.01832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grothoff M, Pachowsky M, Hoffmann J, Posch M, Klaassen S, Lehmkuhl L, Gutberlet M. Value of cardiovascular MR in diagnosing left ventricular non-compaction cardiomyopathy and in discriminating between other cardiomyopathies. Eur Radiol. 2012;22:2699–2709. doi: 10.1007/s00330-012-2554-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cittar M, Cipriani A, Merlo M, Vitrella G, Masè M, Carrer A, Barbati G, Belgrano M, Pagnan L, De Lazzari M, Giorgi B, Cova MA, Iliceto S, Basso C, Stolfo D, Sinagra G, Perazzolo Marra M. Prognostic Significance of Feature-Tracking Right Ventricular Global Longitudinal Strain in Non-ischemic Dilated Cardiomyopathy. Front Cardiovasc Med. 2021;8:765274. doi: 10.3389/fcvm.2021.765274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Halliday BP. State of the art: multimodality imaging in dilated cardiomyopathy. Heart. 2022;108:1910–1917. doi: 10.1136/heartjnl-2022-321116. [DOI] [PubMed] [Google Scholar]
- 10.Puntmann VO, Carr-White G, Jabbour A, Yu CY, Gebker R, Kelle S, Hinojar R, Doltra A, Varma N, Child N, Rogers T, Suna G, Arroyo Ucar E, Goodman B, Khan S, Dabir D, Herrmann E, Zeiher AM, Nagel E International T1 Multicentre CMR Outcome Study. T1-Mapping and Outcome in Nonischemic Cardiomyopathy: All-Cause Mortality and Heart Failure. JACC Cardiovasc Imaging. 2016;9:40–50. doi: 10.1016/j.jcmg.2015.12.001. [DOI] [PubMed] [Google Scholar]
- 11.Thavendiranathan P, Walls M, Giri S, Verhaert D, Rajagopalan S, Moore S, Simonetti OP, Raman SV. Improved detection of myocardial involvement in acute inflammatory cardiomyopathies using T2 mapping. Circ Cardiovasc Imaging. 2012;5:102–110. doi: 10.1161/CIRCIMAGING.111.967836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Damasceno A, Mayosi BM, Sani M, Ogah OS, Mondo C, Ojji D, Dzudie A, Kouam CK, Suliman A, Schrueder N, Yonga G, Ba SA, Maru F, Alemayehu B, Edwards C, Davison BA, Cotter G, Sliwa K. The causes, treatment, and outcome of acute heart failure in 1006 Africans from 9 countries. Arch Intern Med. 2012;172:1386–1394. doi: 10.1001/archinternmed.2012.3310. [DOI] [PubMed] [Google Scholar]
- 13.Cleland JG, McGowan J. Heart failure due to ischaemic heart disease: epidemiology, pathophysiology and progression. J Cardiovasc Pharmacol. 1999;33 Suppl 3:S17–S29. doi: 10.1097/00005344-199906003-00003. [DOI] [PubMed] [Google Scholar]
- 14.Bowling CB, Sanders PW, Allman RM, Rogers WJ, Patel K, Aban IB, Rich MW, Pitt B, White M, Bakris GC, Fonarow GC, Ahmed A. Effects of enalapril in systolic heart failure patients with and without chronic kidney disease: insights from the SOLVD Treatment trial. Int J Cardiol. 2013;167:151–156. doi: 10.1016/j.ijcard.2011.12.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Palumbo P, Cannizzaro E, Di Cesare A, Bruno F, Arrigoni F, Splendiani A, Barile A, Masciocchi C, Di Cesare E. Stress Perfusion Cardiac Magnetic Resonance in Long-Standing Non-Infarcted Chronic Coronary Syndrome with Preserved Systolic Function. Diagnostics (Basel) 2022;12 doi: 10.3390/diagnostics12040786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Palmisano A, Vignale D, Benedetti G, Del Maschio A, De Cobelli F, Esposito A. Late iodine enhancement cardiac computed tomography for detection of myocardial scars: impact of experience in the clinical practice. Radiol Med. 2020;125:128–136. doi: 10.1007/s11547-019-01108-7. [DOI] [PubMed] [Google Scholar]
- 17.Kim RJ, Wu E, Rafael A, Chen EL, Parker MA, Simonetti O, Klocke FJ, Bonow RO, Judd RM. The use of contrast-enhanced magnetic resonance imaging to identify reversible myocardial dysfunction. N Engl J Med. 2000;343:1445–1453. doi: 10.1056/NEJM200011163432003. [DOI] [PubMed] [Google Scholar]
- 18.Ge Y, Antiochos P, Steel K, Bingham S, Abdullah S, Chen YY, Mikolich JR, Arai AE, Bandettini WP, Shanbhag SM, Patel AR, Farzaneh-Far A, Heitner JF, Shenoy C, Leung SW, Gonzalez JA, Shah DJ, Raman SV, Ferrari VA, Schulz-Menger J, Stuber M, Simonetti OP, Kwong RY. Prognostic Value of Stress CMR Perfusion Imaging in Patients With Reduced Left Ventricular Function. JACC Cardiovasc Imaging. 2020;13:2132–2145. doi: 10.1016/j.jcmg.2020.05.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schwitter J. The SPINS Trial: Building Evidence and a Consequence? J Am Coll Cardiol. 2019;74:1756–1759. doi: 10.1016/j.jacc.2019.07.075. [DOI] [PubMed] [Google Scholar]
- 20.Patel AR, Salerno M, Kwong RY, Singh A, Heydari B, Kramer CM. Stress Cardiac Magnetic Resonance Myocardial Perfusion Imaging: JACC Review Topic of the Week. J Am Coll Cardiol. 2021;78:1655–1668. doi: 10.1016/j.jacc.2021.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ge Y, Steel K, Antiochos P, Bingham S, Abdullah S, Mikolich JR, Arai AE, Bandettini WP, Shanbhag SM, Patel AR, Farzaneh-Far A, Heitner JF, Shenoy C, Leung SW, Gonzalez JA, Shah DJ, Raman SV, Nawaz H, Ferrari VA, Schulz-Menger J, Stuber M, Simonetti OP, Kwong RY. Stress CMR in patients with obesity: insights from the Stress CMR Perfusion Imaging in the United States (SPINS) registry. Eur Heart J Cardiovasc Imaging. 2021;22:518–527. doi: 10.1093/ehjci/jeaa281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Menghoum N, Vos JL, Pouleur AC, Nijveldt R, Gerber BL. How to evaluate cardiomyopathies by cardiovascular magnetic resonance parametric mapping and late gadolinium enhancement. Eur Heart J Cardiovasc Imaging. 2022;23:587–589. doi: 10.1093/ehjci/jeac051. [DOI] [PubMed] [Google Scholar]
- 23.Nagueh SF, Phelan D, Abraham T, Armour A, Desai MY, Dragulescu A, Gilliland Y, Lester SJ, Maldonado Y, Mohiddin S, Nieman K, Sperry BW, Woo A. Recommendations for Multimodality Cardiovascular Imaging of Patients with Hypertrophic Cardiomyopathy: An Update from the American Society of Echocardiography, in Collaboration with the American Society of Nuclear Cardiology, the Society for Cardiovascular Magnetic Resonance, and the Society of Cardiovascular Computed Tomography. J Am Soc Echocardiogr. 2022;35:533–569. doi: 10.1016/j.echo.2022.03.012. [DOI] [PubMed] [Google Scholar]
- 24.Porcari A, Baggio C, Fabris E, Merlo M, Bussani R, Perkan A, Sinagra G. Endomyocardial biopsy in the clinical context: current indications and challenging scenarios. Heart Fail Rev. 2023;28:123–135. doi: 10.1007/s10741-022-10247-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Seferović PM, Tsutsui H, McNamara DM, Ristić AD, Basso C, Bozkurt B, Cooper LT Jr, Filippatos G, Ide T, Inomata T, Klingel K, Linhart A, Lyon AR, Mehra MR, Polovina M, Milinković I, Nakamura K, Anker SD, Veljić I, Ohtani T, Okumura T, Thum T, Tschöpe C, Rosano G, Coats AJS, Starling RC. Heart Failure Association of the ESC, Heart Failure Society of America and Japanese Heart Failure Society Position statement on endomyocardial biopsy. Eur J Heart Fail. 2021;23:854–871. doi: 10.1002/ejhf.2190. [DOI] [PubMed] [Google Scholar]
- 26.Pluim BM, Zwinderman AH, van der Laarse A, van der Wall EE. The athlete's heart. A meta-analysis of cardiac structure and function. Circulation. 2000;101:336–344. doi: 10.1161/01.cir.101.3.336. [DOI] [PubMed] [Google Scholar]
- 27.D'Ascenzi F, Anselmi F, Piu P, Fiorentini C, Carbone SF, Volterrani L, Focardi M, Bonifazi M, Mondillo S. Cardiac Magnetic Resonance Normal Reference Values of Biventricular Size and Function in Male Athlete's Heart. JACC Cardiovasc Imaging. 2019;12:1755–1765. doi: 10.1016/j.jcmg.2018.09.021. [DOI] [PubMed] [Google Scholar]
- 28.Aguiar Rosa S, Thomas B, Pieroni M, Maurizi N, Zampieri M, Cappelli F, Marchi A, Pradella S, Cardim N, Bogaert J, Olivotto I. Role of cardiovascular magnetic resonance in the clinical evaluation of left ventricular hypertrophy: a 360° panorama. Int J Cardiovasc Imaging. 2023;39:793–809. doi: 10.1007/s10554-022-02774-x. [DOI] [PubMed] [Google Scholar]
- 29.Pelliccia A, Maron BJ, De Luca R, Di Paolo FM, Spataro A, Culasso F. Remodeling of left ventricular hypertrophy in elite athletes after long-term deconditioning. Circulation. 2002;105:944–949. doi: 10.1161/hc0802.104534. [DOI] [PubMed] [Google Scholar]
- 30.Małek ŁA, Bucciarelli-Ducci C. Myocardial fibrosis in athletes-Current perspective. Clin Cardiol. 2020;43:882–888. doi: 10.1002/clc.23360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Maron BJ, Desai MY, Nishimura RA, Spirito P, Rakowski H, Towbin JA, Rowin EJ, Maron MS, Sherrid MV. Diagnosis and Evaluation of Hypertrophic Cardiomyopathy: JACC State-of-the-Art Review. J Am Coll Cardiol. 2022;79:372–389. doi: 10.1016/j.jacc.2021.12.002. [DOI] [PubMed] [Google Scholar]
- 32.Rowin EJ, Maron BJ, Haas TS, Garberich RF, Wang W, Link MS, Maron MS. Hypertrophic Cardiomyopathy With Left Ventricular Apical Aneurysm: Implications for Risk Stratification and Management. J Am Coll Cardiol. 2017;69:761–773. doi: 10.1016/j.jacc.2016.11.063. [DOI] [PubMed] [Google Scholar]
- 33.Strachinaru M, Huurman R, Bowen DJ, Schinkel AFL, Hirsch A, Michels M. Relation Between Early Diastolic Mid-Ventricular Flow and Elastic Forces Indicating Aneurysm Formation in Hypertrophic Cardiomyopathy. J Am Soc Echocardiogr. 2022;35:846–856.e2. doi: 10.1016/j.echo.2022.04.010. [DOI] [PubMed] [Google Scholar]
- 34.Writing Committee Members; Ommen SR, Mital S, Burke MA, Day SM, Deswal A, Elliott P, Evanovich LL, Hung J, Joglar JA, Kantor P, Kimmelstiel C, Kittleson M, Link MS, Maron MS, Martinez MW, Miyake CY, Schaff HV, Semsarian C, Sorajja P ACC/AHA Joint Committee Members, O'Gara PT, Beckman JA, Levine GN, Al-Khatib SM, Armbruster A, Birtcher KK, Ciggaroa J, Dixon DL, de Las Fuentes L, Deswal A, Fleisher LA, Gentile F, Goldberger ZD, Gorenek B, Haynes N, Hernandez AF, Hlatky MA, Joglar JA, Jones WS, Marine JE, Mark D, Palaniappan L, Piano MR, Tamis-Holland J, Wijeysundera DN, Woo YJ. 2020 AHA/ACC guideline for the diagnosis and treatment of patients with hypertrophic cardiomyopathy: A report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Thorac Cardiovasc Surg. 2021;162:e23–e106. doi: 10.1016/j.jtcvs.2021.04.001. [DOI] [PubMed] [Google Scholar]
- 35.Zeppenfeld K, Tfelt-Hansen J, de Riva M, Winkel BG, Behr ER, Blom NA, Charron P, Corrado D, Dagres N, de Chillou C, Eckardt L, Friede T, Haugaa KH, Hocini M, Lambiase PD, Marijon E, Merino JL, Peichl P, Priori SG, Reichlin T, Schulz-Menger J, Sticherling C, Tzeis S, Verstrael A, Volterrani M ESC Scientific Document Group. 2022 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Eur Heart J. 2022;43:3997–4126. doi: 10.1093/eurheartj/ehac262. [DOI] [PubMed] [Google Scholar]
- 36.O'Mahony C, Jichi F, Pavlou M, Monserrat L, Anastasakis A, Rapezzi C, Biagini E, Gimeno JR, Limongelli G, McKenna WJ, Omar RZ, Elliott PM Hypertrophic Cardiomyopathy Outcomes Investigators. A novel clinical risk prediction model for sudden cardiac death in hypertrophic cardiomyopathy (HCM risk-SCD) Eur Heart J. 2014;35:2010–2020. doi: 10.1093/eurheartj/eht439. [DOI] [PubMed] [Google Scholar]
- 37.Lee DZJ, Montazeri M, Bataiosu R, Hoss S, Adler A, Nguyen ET, Rakowski H, Chan RH. Clinical Characteristics and Prognostic Importance of Left Ventricular Apical Aneurysms in Hypertrophic Cardiomyopathy. JACC Cardiovasc Imaging. 2022;15:1696–1711. doi: 10.1016/j.jcmg.2022.03.029. [DOI] [PubMed] [Google Scholar]
- 38.Maron MS, Rowin EJ, Lin D, Appelbaum E, Chan RH, Gibson CM, Lesser JR, Lindberg J, Haas TS, Udelson JE, Manning WJ, Maron BJ. Prevalence and clinical profile of myocardial crypts in hypertrophic cardiomyopathy. Circ Cardiovasc Imaging. 2012;5:441–447. doi: 10.1161/CIRCIMAGING.112.972760. [DOI] [PubMed] [Google Scholar]
- 39.Sigvardsen PE, Pham MHC, Kühl JT, Fuchs A, Afzal S, Møgelvang R, Nordestgaard BG, Køber L, Kofoed KF. Left ventricular myocardial crypts: morphological patterns and prognostic implications. Eur Heart J Cardiovasc Imaging. 2021;22:75–81. doi: 10.1093/ehjci/jeaa020. [DOI] [PubMed] [Google Scholar]
- 40.Gruner C, Chan RH, Crean A, Rakowski H, Rowin EJ, Care M, Deva D, Williams L, Appelbaum E, Gibson CM, Lesser JR, Haas TS, Udelson JE, Manning WJ, Siminovitch K, Ralph-Edwards AC, Rastegar H, Maron BJ, Maron MS. Significance of left ventricular apical-basal muscle bundle identified by cardiovascular magnetic resonance imaging in patients with hypertrophic cardiomyopathy. Eur Heart J. 2014;35:2706–2713. doi: 10.1093/eurheartj/ehu154. [DOI] [PubMed] [Google Scholar]
- 41.Tao J, Duan F, Long J, Meng Q, Zhang B, Zhu Z, Wang H. The Role of the Submitral Apparatus in Hypertrophic Obstructive Cardiomyopathy. J Am Soc Echocardiogr. 2023;36:133–145. doi: 10.1016/j.echo.2022.09.018. [DOI] [PubMed] [Google Scholar]
- 42.Brandão M, Marchi A, Olivotto I. Mid-ventricular obstruction in hypertrophic cardiomyopathy: a signal void. Rev Esp Cardiol (Engl Ed) 2023;76:749. doi: 10.1016/j.rec.2022.12.009. [DOI] [PubMed] [Google Scholar]
- 43.Chan RH, Maron BJ, Olivotto I, Pencina MJ, Assenza GE, Haas T, Lesser JR, Gruner C, Crean AM, Rakowski H, Udelson JE, Rowin E, Lombardi M, Cecchi F, Tomberli B, Spirito P, Formisano F, Biagini E, Rapezzi C, De Cecco CN, Autore C, Cook EF, Hong SN, Gibson CM, Manning WJ, Appelbaum E, Maron MS. Prognostic value of quantitative contrast-enhanced cardiovascular magnetic resonance for the evaluation of sudden death risk in patients with hypertrophic cardiomyopathy. Circulation. 2014;130:484–495. doi: 10.1161/CIRCULATIONAHA.113.007094. [DOI] [PubMed] [Google Scholar]
- 44.Casas G, Rodríguez-Palomares JF. Multimodality Cardiac Imaging in Cardiomyopathies: From Diagnosis to Prognosis. J Clin Med. 2022;11 doi: 10.3390/jcm11030578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Todiere G, Pisciella L, Barison A, Del Franco A, Zachara E, Piaggi P, Re F, Pingitore A, Emdin M, Lombardi M, Aquaro GD. Abnormal T2-STIR magnetic resonance in hypertrophic cardiomyopathy: a marker of advanced disease and electrical myocardial instability. PLoS One. 2014;9:e111366. doi: 10.1371/journal.pone.0111366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Aguiar Rosa S, Thomas B, Fiarresga A, Papoila AL, Alves M, Pereira R, Branco G, Cruz I, Rio P, Baquero L, Ferreira RC, Mota Carmo M, Lopes LR. The Impact of Ischemia Assessed by Magnetic Resonance on Functional, Arrhythmic, and Imaging Features of Hypertrophic Cardiomyopathy. Front Cardiovasc Med. 2021;8:761860. doi: 10.3389/fcvm.2021.761860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Maurer MS, Elliott P, Comenzo R, Semigran M, Rapezzi C. Addressing Common Questions Encountered in the Diagnosis and Management of Cardiac Amyloidosis. Circulation. 2017;135:1357–1377. doi: 10.1161/CIRCULATIONAHA.116.024438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Garcia-Pavia P, Rapezzi C, Adler Y, Arad M, Basso C, Brucato A, Burazor I, Caforio ALP, Damy T, Eriksson U, Fontana M, Gillmore JD, Gonzalez-Lopez E, Grogan M, Heymans S, Imazio M, Kindermann I, Kristen AV, Maurer MS, Merlini G, Pantazis A, Pankuweit S, Rigopoulos AG, Linhart A. Diagnosis and treatment of cardiac amyloidosis: a position statement of the ESC Working Group on Myocardial and Pericardial Diseases. Eur Heart J. 2021;42:1554–1568. doi: 10.1093/eurheartj/ehab072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Merlo M, Gagno G, Baritussio A, Bauce B, Biagini E, Canepa M, Cipriani A, Castelletti S, Dellegrottaglie S, Guaricci AI, Imazio M, Limongelli G, Musumeci MB, Parisi V, Pica S, Pontone G, Todiere G, Torlasco C, Basso C, Sinagra G, Filardi PP, Indolfi C, Autore C, Barison A. Clinical application of CMR in cardiomyopathies: evolving concepts and techniques: A position paper of myocardial and pericardial diseases and cardiac magnetic resonance working groups of Italian society of cardiology. Heart Fail Rev. 2023;28:77–95. doi: 10.1007/s10741-022-10235-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pieroni M, Moon JC, Arbustini E, Barriales-Villa R, Camporeale A, Vujkovac AC, Elliott PM, Hagege A, Kuusisto J, Linhart A, Nordbeck P, Olivotto I, Pietilä-Effati P, Namdar M. Cardiac Involvement in Fabry Disease: JACC Review Topic of the Week. J Am Coll Cardiol. 2021;77:922–936. doi: 10.1016/j.jacc.2020.12.024. [DOI] [PubMed] [Google Scholar]
- 51.Muchtar E, Blauwet LA, Gertz MA. Restrictive Cardiomyopathy: Genetics, Pathogenesis, Clinical Manifestations, Diagnosis, and Therapy. Circ Res. 2017;121:819–837. doi: 10.1161/CIRCRESAHA.117.310982. [DOI] [PubMed] [Google Scholar]
- 52.Habib G, Bucciarelli-Ducci C, Caforio ALP, Cardim N, Charron P, Cosyns B, Dehaene A, Derumeaux G, Donal E, Dweck MR, Edvardsen T, Erba PA, Ernande L, Gaemperli O, Galderisi M, Grapsa J, Jacquier A, Klingel K, Lancellotti P, Neglia D, Pepe A, Perrone-Filardi P, Petersen SE, Plein S, Popescu BA, Reant P, Sade LE, Salaun E, Slart RHJA, Tribouilloy C, Zamorano J EACVI Scientific Documents Committee; Indian Academy of Echocardiography. Multimodality Imaging in Restrictive Cardiomyopathies: An EACVI expert consensus document In collaboration with the "Working Group on myocardial and pericardial diseases" of the European Society of Cardiology Endorsed by The Indian Academy of Echocardiography. Eur Heart J Cardiovasc Imaging. 2017;18:1090–1121. doi: 10.1093/ehjci/jex034. [DOI] [PubMed] [Google Scholar]
- 53.Mocumbi AO, Carrilho C, Sarathchandra P, Ferreira MB, Yacoub M, Burke M. Echocardiography accurately assesses the pathological abnormalities of chronic endomyocardial fibrosis. Int J Cardiovasc Imaging. 2011;27:955–964. doi: 10.1007/s10554-010-9753-6. [DOI] [PubMed] [Google Scholar]
- 54.Mocumbi AO, Ferreira MB, Sidi D, Yacoub MH. A population study of endomyocardial fibrosis in a rural area of Mozambique. N Engl J Med. 2008;359:43–49. doi: 10.1056/NEJMoa0708629. [DOI] [PubMed] [Google Scholar]
- 55.Salemi VM, Rochitte CE, Shiozaki AA, Andrade JM, Parga JR, de Ávila LF, Benvenuti LA, Cestari IN, Picard MH, Kim RJ, Mady C. Late gadolinium enhancement magnetic resonance imaging in the diagnosis and prognosis of endomyocardial fibrosis patients. Circ Cardiovasc Imaging. 2011;4:304–311. doi: 10.1161/CIRCIMAGING.110.950675. [DOI] [PubMed] [Google Scholar]
- 56.White JA, Fine NM. Recent Advances in Cardiovascular Imaging Relevant to the Management of Patients with Suspected Cardiac Amyloidosis. Curr Cardiol Rep. 2016;18:77. doi: 10.1007/s11886-016-0752-7. [DOI] [PubMed] [Google Scholar]
- 57.Ruberg FL, Appelbaum E, Davidoff R, Ozonoff A, Kissinger KV, Harrigan C, Skinner M, Manning WJ. Diagnostic and prognostic utility of cardiovascular magnetic resonance imaging in light-chain cardiac amyloidosis. Am J Cardiol. 2009;103:544–549. doi: 10.1016/j.amjcard.2008.09.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.van der Voorn SM, Te Riele ASJM, Basso C, Calkins H, Remme CA, van Veen TAB. Arrhythmogenic cardiomyopathy: pathogenesis, pro-arrhythmic remodelling, and novel approaches for risk stratification and therapy. Cardiovasc Res. 2020;116:1571–1584. doi: 10.1093/cvr/cvaa084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Corrado D, Link MS, Calkins H. Arrhythmogenic Right Ventricular Cardiomyopathy. N Engl J Med. 2017;376:61–72. doi: 10.1056/NEJMra1509267. [DOI] [PubMed] [Google Scholar]
- 60.Corrado D, Wichter T, Link MS, Hauer R, Marchlinski F, Anastasakis A, Bauce B, Basso C, Brunckhorst C, Tsatsopoulou A, Tandri H, Paul M, Schmied C, Pelliccia A, Duru F, Protonotarios N, Estes NA 3rd, McKenna WJ, Thiene G, Marcus FI, Calkins H. Treatment of arrhythmogenic right ventricular cardiomyopathy/dysplasia: an international task force consensus statement. Eur Heart J. 2015;36:3227–3237. doi: 10.1093/eurheartj/ehv162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Corrado D, Perazzolo Marra M, Zorzi A, Beffagna G, Cipriani A, Lazzari M, Migliore F, Pilichou K, Rampazzo A, Rigato I, Rizzo S, Thiene G, Anastasakis A, Asimaki A, Bucciarelli-Ducci C, Haugaa KH, Marchlinski FE, Mazzanti A, McKenna WJ, Pantazis A, Pelliccia A, Schmied C, Sharma S, Wichter T, Bauce B, Basso C. Diagnosis of arrhythmogenic cardiomyopathy: The Padua criteria. Int J Cardiol. 2020;319:106–114. doi: 10.1016/j.ijcard.2020.06.005. [DOI] [PubMed] [Google Scholar]
- 62.Groeneweg JA, Bhonsale A, James CA, te Riele AS, Dooijes D, Tichnell C, Murray B, Wiesfeld AC, Sawant AC, Kassamali B, Atsma DE, Volders PG, de Groot NM, de Boer K, Zimmerman SL, Kamel IR, van der Heijden JF, Russell SD, Jan Cramer M, Tedford RJ, Doevendans PA, van Veen TA, Tandri H, Wilde AA, Judge DP, van Tintelen JP, Hauer RN, Calkins H. Clinical Presentation, Long-Term Follow-Up, and Outcomes of 1001 Arrhythmogenic Right Ventricular Dysplasia/Cardiomyopathy Patients and Family Members. Circ Cardiovasc Genet. 2015;8:437–446. doi: 10.1161/CIRCGENETICS.114.001003. [DOI] [PubMed] [Google Scholar]
- 63.Towbin JA, McKenna WJ, Abrams DJ, Ackerman MJ, Calkins H, Darrieux FCC, Daubert JP, de Chillou C, DePasquale EC, Desai MY, Estes NAM 3rd, Hua W, Indik JH, Ingles J, James CA, John RM, Judge DP, Keegan R, Krahn AD, Link MS, Marcus FI, McLeod CJ, Mestroni L, Priori SG, Saffitz JE, Sanatani S, Shimizu W, van Tintelen JP, Wilde AAM, Zareba W. 2019 HRS expert consensus statement on evaluation, risk stratification, and management of arrhythmogenic cardiomyopathy. Heart Rhythm. 2019;16:e301–e372. doi: 10.1016/j.hrthm.2019.05.007. [DOI] [PubMed] [Google Scholar]
- 64.Cadrin-Tourigny J, Bosman LP, Nozza A, Wang W, Tadros R, Bhonsale A, Bourfiss M, Fortier A, Lie ØH, Saguner AM, Svensson A, Andorin A, Tichnell C, Murray B, Zeppenfeld K, van den Berg MP, Asselbergs FW, Wilde AAM, Krahn AD, Talajic M, Rivard L, Chelko S, Zimmerman SL, Kamel IR, Crosson JE, Judge DP, Yap SC, van der Heijden JF, Tandri H, Jongbloed JDH, Guertin MC, van Tintelen JP, Platonov PG, Duru F, Haugaa KH, Khairy P, Hauer RNW, Calkins H, Te Riele ASJM, James CA. A new prediction model for ventricular arrhythmias in arrhythmogenic right ventricular cardiomyopathy. Eur Heart J. 2022;43:e1–e9. doi: 10.1093/eurheartj/ehac180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Aquaro GD, Pingitore A, Di Bella G, Piaggi P, Gaeta R, Grigoratos C, Altinier A, Pantano A, Strata E, De Caterina R, Sinagra G, Emdin M. Prognostic Role of Cardiac Magnetic Resonance in Arrhythmogenic Right Ventricular Cardiomyopathy. Am J Cardiol. 2018;122:1745–1753. doi: 10.1016/j.amjcard.2018.08.007. [DOI] [PubMed] [Google Scholar]
- 66.Aquaro GD, De Luca A, Cappelletto C, Raimondi F, Bianco F, Botto N, Lesizza P, Grigoratos C, Minati M, Dell'Omodarme M, Pingitore A, Stolfo D, Ferro MD, Merlo M, Di Bella G, Sinagra G. Prognostic Value of Magnetic Resonance Phenotype in Patients With Arrhythmogenic Right Ventricular Cardiomyopathy. J Am Coll Cardiol. 2020;75:2753–2765. doi: 10.1016/j.jacc.2020.04.023. [DOI] [PubMed] [Google Scholar]
- 67.Deac M, Alpendurada F, Fanaie F, Vimal R, Carpenter JP, Dawson A, Miller C, Roussin I, di Pietro E, Ismail TF, Roughton M, Wong J, Dawson D, Till JA, Sheppard MN, Mohiaddin RH, Kilner PJ, Pennell DJ, Prasad SK. Prognostic value of cardiovascular magnetic resonance in patients with suspected arrhythmogenic right ventricular cardiomyopathy. Int J Cardiol. 2013;168:3514–3521. doi: 10.1016/j.ijcard.2013.04.208. [DOI] [PubMed] [Google Scholar]
- 68.Tandri H, Saranathan M, Rodriguez ER, Martinez C, Bomma C, Nasir K, Rosen B, Lima JA, Calkins H, Bluemke DA. Noninvasive detection of myocardial fibrosis in arrhythmogenic right ventricular cardiomyopathy using delayed-enhancement magnetic resonance imaging. J Am Coll Cardiol. 2005;45:98–103. doi: 10.1016/j.jacc.2004.09.053. [DOI] [PubMed] [Google Scholar]
- 69.Lie ØH, Rootwelt-Norberg C, Dejgaard LA, Leren IS, Stokke MK, Edvardsen T, Haugaa KH. Prediction of Life-Threatening Ventricular Arrhythmia in Patients With Arrhythmogenic Cardiomyopathy: A Primary Prevention Cohort Study. JACC Cardiovasc Imaging. 2018;11:1377–1386. doi: 10.1016/j.jcmg.2018.05.017. [DOI] [PubMed] [Google Scholar]
- 70.Bourfiss M, Prakken NHJ, James CA, Planken RN, Boekholdt SM, Ahmetagic D, van den Berg MP, Tichnell C, Van der Heijden JF, Loh P, Murray B, Tandri H, Kamel I, Calkins H, Asselbergs FW, Zimmerman SL, Velthuis BK, Te Riele ASJM. Prognostic value of strain by feature-tracking cardiac magnetic resonance in arrhythmogenic right ventricular cardiomyopathy. Eur Heart J Cardiovasc Imaging. 2022;24:98–107. doi: 10.1093/ehjci/jeac030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Belhassen B, Laredo M, Roudijk RW, Peretto G, Zahavi G, Sen-Chowdhry S, Badenco N, Te Riele ASJM, Sala S, Duthoit G, van Tintelen JP, Paglino G, Sellal JM, Gasperetti A, Arbelo E, Andorin A, Ninni S, Rollin A, Peichl P, Waintraub X, Bosman LP, Pierre B, Nof E, Miles C, Tfelt-Hansen J, Protonotarios A, Giustetto C, Sacher F, Hermida JS, Havranek S, Calo L, Casado-Arroyo R, Conte G, Letsas KP, Zorio E, Bermúdez-Jiménez FJ, Behr ER, Beinart R, Fauchier L, Kautzner J, Maury P, Lacroix D, Probst V, Brugada J, Duru F, de Chillou C, Bella PD, Gandjbakhch E, Hauer R, Milman A. The prevalence of left and right bundle branch block morphology ventricular tachycardia amongst patients with arrhythmogenic cardiomyopathy and sustained ventricular tachycardia: insights from the European Survey on Arrhythmogenic Cardiomyopathy. Europace. 2022;24:285–295. doi: 10.1093/europace/euab190. [DOI] [PubMed] [Google Scholar]
- 72.Pinamonti B, Dragos AM, Pyxaras SA, Merlo M, Pivetta A, Barbati G, Di Lenarda A, Morgera T, Mestroni L, Sinagra G. Prognostic predictors in arrhythmogenic right ventricular cardiomyopathy: results from a 10-year registry. Eur Heart J. 2011;32:1105–1113. doi: 10.1093/eurheartj/ehr040. [DOI] [PubMed] [Google Scholar]
- 73.Zhang N, Song Y, Hua W, Hu Y, Chen L, Cai M, Niu H, Cai C, Gu M, Zhao S, Zhang S. Left ventricular involvement assessed by LGE-CMR in predicting the risk of adverse outcomes of arrhythmogenic cardiomyopathy with ICDs. Int J Cardiol. 2021;337:79–85. doi: 10.1016/j.ijcard.2021.04.015. [DOI] [PubMed] [Google Scholar]
- 74.Chun KH, Oh J, Hong YJ, Yu HT, Lee CJ, Kim TH, Joung B, Pak HN, Lee MH, Kim YJ, Kang SM. Prognostic Cardiac Magnetic Resonance Markers of Left Ventricular Involvement in Arrhythmogenic Cardiomyopathy for Predicting Heart Failure Outcomes. J Am Heart Assoc. 2022;11:e023167. doi: 10.1161/JAHA.121.023167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Agbaedeng TA, Roberts KA, Colley L, Noubiap JJ, Oxborough D. Incidence and predictors of sudden cardiac death in arrhythmogenic right ventricular cardiomyopathy: a pooled analysis. Europace. 2022;24:1665–1674. doi: 10.1093/europace/euac014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bosman LP, Sammani A, James CA, Cadrin-Tourigny J, Calkins H, van Tintelen JP, Hauer RNW, Asselbergs FW, Te Riele ASJM. Predicting arrhythmic risk in arrhythmogenic right ventricular cardiomyopathy: A systematic review and meta-analysis. Heart Rhythm. 2018;15:1097–1107. doi: 10.1016/j.hrthm.2018.01.031. [DOI] [PubMed] [Google Scholar]
- 77.Zghaib T, Te Riele ASJM, James CA, Rastegar N, Murray B, Tichnell C, Halushka MK, Bluemke DA, Tandri H, Calkins H, Kamel IR, Zimmerman SL. Left ventricular fibro-fatty replacement in arrhythmogenic right ventricular dysplasia/cardiomyopathy: prevalence, patterns, and association with arrhythmias. J Cardiovasc Magn Reson. 2021;23:58. doi: 10.1186/s12968-020-00702-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Asatryan B, Asimaki A, Landstrom AP, Khanji MY, Odening KE, Cooper LT, Marchlinski FE, Gelzer AR, Semsarian C, Reichlin T, Owens AT, Chahal CAA. Inflammation and Immune Response in Arrhythmogenic Cardiomyopathy: State-of-the-Art Review. Circulation. 2021;144:1646–1655. doi: 10.1161/CIRCULATIONAHA.121.055890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Mohty D, Boulogne C, Magne J, Varroud-Vial N, Martin S, Ettaif H, Fadel BM, Bridoux F, Aboyans V, Damy T, Jaccard A. Prognostic value of left atrial function in systemic light-chain amyloidosis: a cardiac magnetic resonance study. Eur Heart J Cardiovasc Imaging. 2016;17:961–969. doi: 10.1093/ehjci/jew100. [DOI] [PubMed] [Google Scholar]
- 80.Arenja N, Andre F, Riffel JH, Siepen FAD, Hegenbart U, Schönland S, Kristen AV, Katus HA, Buss SJ. Prognostic value of novel imaging parameters derived from standard cardiovascular magnetic resonance in high risk patients with systemic light chain amyloidosis. J Cardiovasc Magn Reson. 2019;21:53. doi: 10.1186/s12968-019-0564-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Ochs MM, Fritz T, Arenja N, Riffel J, Andre F, Mereles D, Siepen FAD, Hegenbart U, Schönland S, Katus HA, Friedrich MGW, Buss SJ. Regional differences in prognostic value of cardiac valve plane displacement in systemic light-chain amyloidosis. J Cardiovasc Magn Reson. 2017;19:87. doi: 10.1186/s12968-017-0402-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wan K, Sun J, Yang D, Liu H, Wang J, Cheng W, Zhang Q, Zeng Z, Zhang T, Greiser A, Jolly MP, Han Y, Chen Y. Left Ventricular Myocardial Deformation on Cine MR Images: Relationship to Severity of Disease and Prognosis in Light-Chain Amyloidosis. Radiology. 2018;288:73–80. doi: 10.1148/radiol.2018172435. [DOI] [PubMed] [Google Scholar]
- 83.Mekinian A, Lions C, Leleu X, Duhamel A, Lamblin N, Coiteux V, De Groote P, Hatron PY, Facon T, Beregi JP, Hachulla E, Launay D Lille Amyloidosis Study Group. Prognosis assessment of cardiac involvement in systemic AL amyloidosis by magnetic resonance imaging. Am J Med. 2010;123:864–868. doi: 10.1016/j.amjmed.2010.03.022. [DOI] [PubMed] [Google Scholar]
- 84.Maceira AM, Prasad SK, Hawkins PN, Roughton M, Pennell DJ. Cardiovascular magnetic resonance and prognosis in cardiac amyloidosis. J Cardiovasc Magn Reson. 2008;10:54. doi: 10.1186/1532-429X-10-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Fontana M, Pica S, Reant P, Abdel-Gadir A, Treibel TA, Banypersad SM, Maestrini V, Barcella W, Rosmini S, Bulluck H, Sayed RH, Patel K, Mamhood S, Bucciarelli-Ducci C, Whelan CJ, Herrey AS, Lachmann HJ, Wechalekar AD, Manisty CH, Schelbert EB, Kellman P, Gillmore JD, Hawkins PN, Moon JC. Prognostic Value of Late Gadolinium Enhancement Cardiovascular Magnetic Resonance in Cardiac Amyloidosis. Circulation. 2015;132:1570–1579. doi: 10.1161/CIRCULATIONAHA.115.016567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Raina S, Lensing SY, Nairooz RS, Pothineni NV, Hakeem A, Bhatti S, Pandey T. Prognostic Value of Late Gadolinium Enhancement CMR in Systemic Amyloidosis. JACC Cardiovasc Imaging. 2016;9:1267–1277. doi: 10.1016/j.jcmg.2016.01.036. [DOI] [PubMed] [Google Scholar]
- 87.Austin BA, Tang WH, Rodriguez ER, Tan C, Flamm SD, Taylor DO, Starling RC, Desai MY. Delayed hyper-enhancement magnetic resonance imaging provides incremental diagnostic and prognostic utility in suspected cardiac amyloidosis. JACC Cardiovasc Imaging. 2009;2:1369–1377. doi: 10.1016/j.jcmg.2009.08.008. [DOI] [PubMed] [Google Scholar]
- 88.White JA, Kim HW, Shah D, Fine N, Kim KY, Wendell DC, Al-Jaroudi W, Parker M, Patel M, Gwadry-Sridhar F, Judd RM, Kim RJ. CMR imaging with rapid visual T1 assessment predicts mortality in patients suspected of cardiac amyloidosis. JACC Cardiovasc Imaging. 2014;7:143–156. doi: 10.1016/j.jcmg.2013.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Wan K, Sun J, Han Y, Luo Y, Liu H, Yang D, Cheng W, Zhang Q, Zeng Z, Chen Y. Right ventricular involvement evaluated by cardiac magnetic resonance imaging predicts mortality in patients with light chain amyloidosis. Heart Vessels. 2018;33:170–179. doi: 10.1007/s00380-017-1043-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Wan K, Sun J, Han Y, Liu H, Yang D, Li W, Wang J, Cheng W, Zhang Q, Zeng Z, Chen Y. Increased Prognostic Value of Query Amyloid Late Enhancement Score in Light-Chain Cardiac Amyloidosis. Circ J. 2018;82:739–746. doi: 10.1253/circj.CJ-17-0464. [DOI] [PubMed] [Google Scholar]
- 91.Karamitsos TD, Piechnik SK, Banypersad SM, Fontana M, Ntusi NB, Ferreira VM, Whelan CJ, Myerson SG, Robson MD, Hawkins PN, Neubauer S, Moon JC. Noncontrast T1 mapping for the diagnosis of cardiac amyloidosis. JACC Cardiovasc Imaging. 2013;6:488–497. doi: 10.1016/j.jcmg.2012.11.013. [DOI] [PubMed] [Google Scholar]
- 92.Lin L, Li X, Feng J, Shen KN, Tian Z, Sun J, Mao YY, Cao J, Jin ZY, Li J, Selvanayagam JB, Wang YN. The prognostic value of T1 mapping and late gadolinium enhancement cardiovascular magnetic resonance imaging in patients with light chain amyloidosis. J Cardiovasc Magn Reson. 2018;20:2. doi: 10.1186/s12968-017-0419-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Wan K, Li W, Sun J, Xu Y, Wang J, Liu H, Dong Y, Cheng W, Zhang Q, Zeng Z, Zhou X, Han Y, Chen Y. Regional amyloid distribution and impact on mortality in light-chain amyloidosis: a T1 mapping cardiac magnetic resonance study. Amyloid. 2019;26:45–51. doi: 10.1080/13506129.2019.1578742. [DOI] [PubMed] [Google Scholar]
- 94.Wassmuth R, Abdel-Aty H, Bohl S, Schulz-Menger J. Prognostic impact of T2-weighted CMR imaging for cardiac amyloidosis. Eur Radiol. 2011;21:1643–1650. doi: 10.1007/s00330-011-2109-3. [DOI] [PubMed] [Google Scholar]
- 95.Legou F, Tacher V, Damy T, Planté-Bordeneuve V, Rappeneau S, Benhaiem N, Rosso J, Itti E, Luciani A, Kobeiter H, Rahmouni A, Deux JF. Usefulness of T2 ratio in the diagnosis and prognosis of cardiac amyloidosis using cardiac MR imaging. Diagn Interv Imaging. 2017;98:125–132. doi: 10.1016/j.diii.2016.08.007. [DOI] [PubMed] [Google Scholar]