Abstract
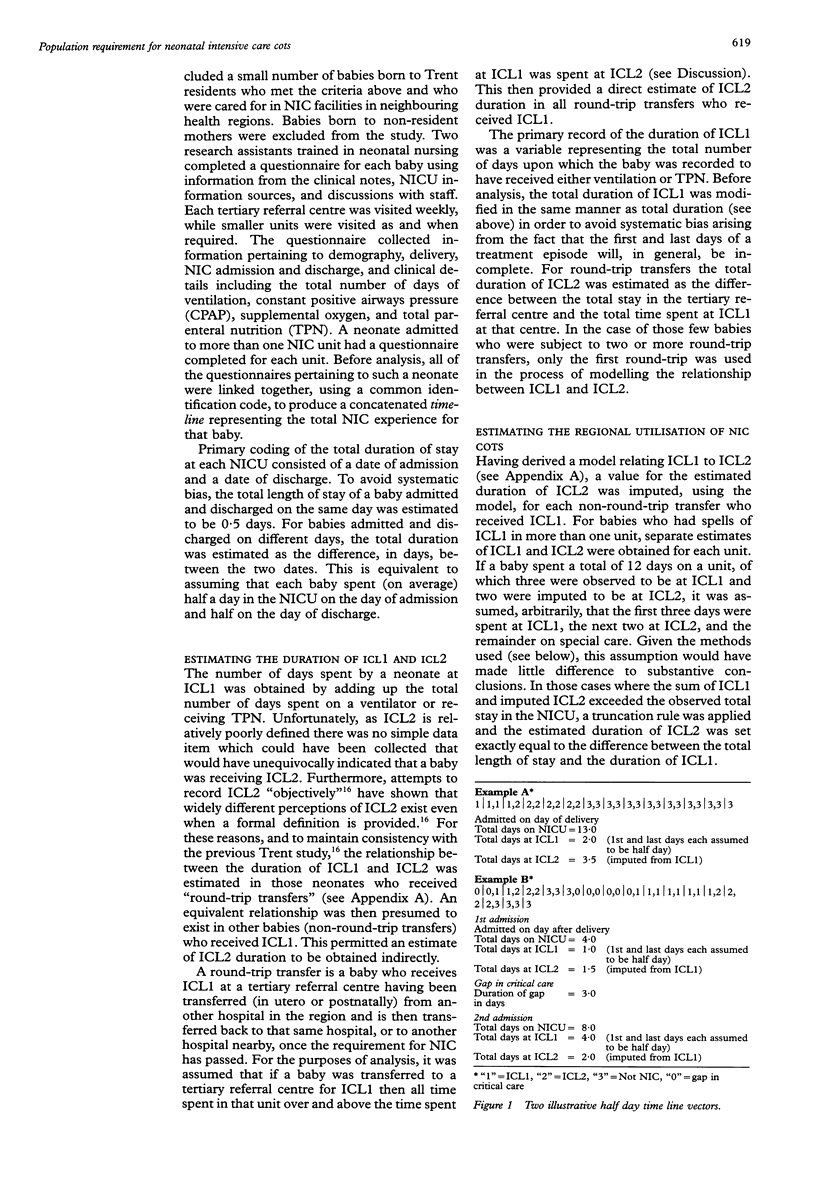
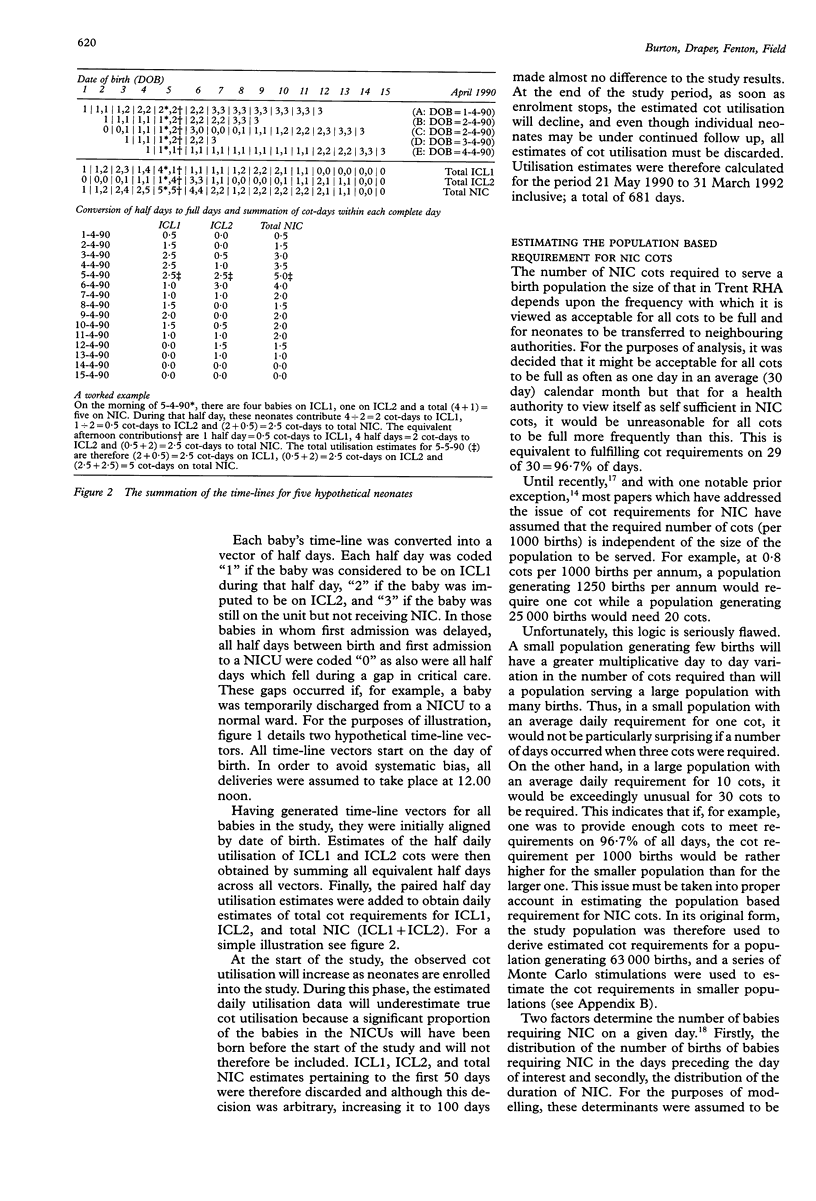
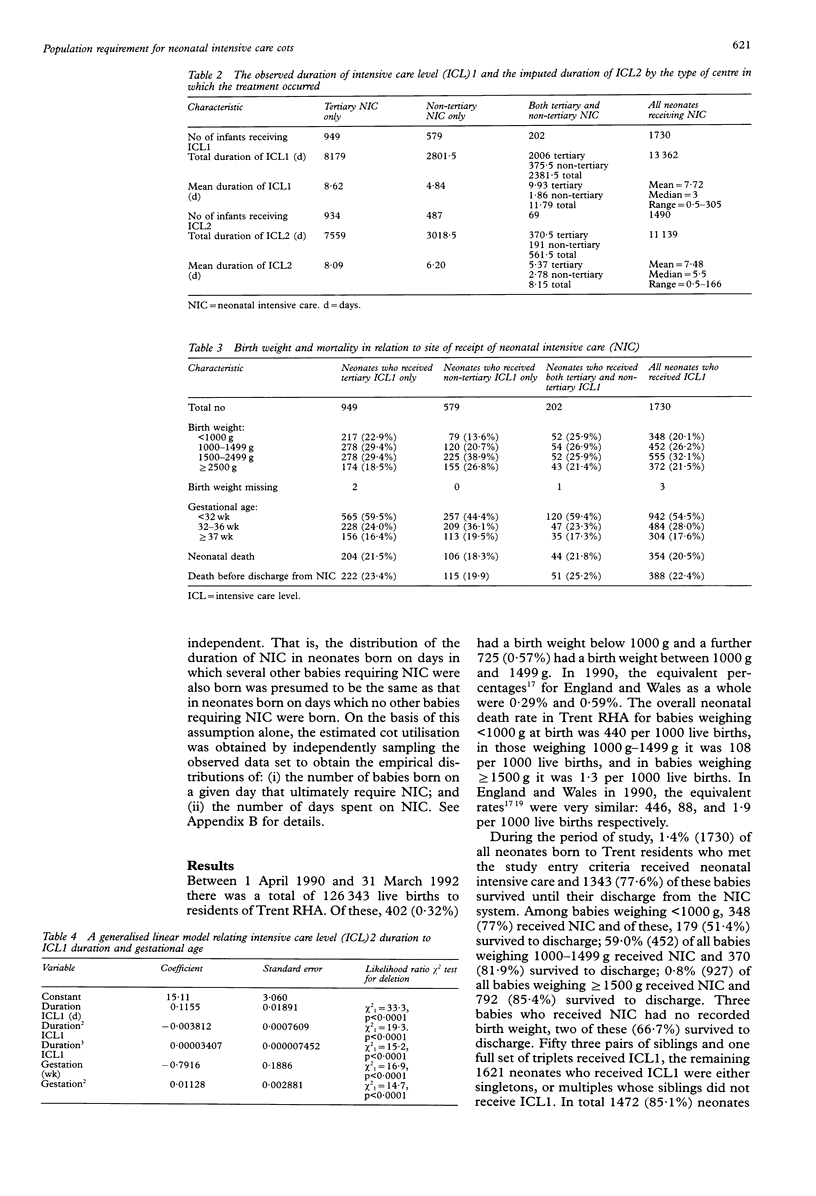
STUDY OBJECTIVES--To estimate the population based requirement for neonatal intensive care (NIC) cots by investigating NIC utilisation in a large population based study. DESIGN AND SETTING--This was a two year, non-randomised, prospective cohort study of neonates receiving NIC in hospitals in the Trent Regional Health Authority (RHA). PARTICIPANTS--The main study considered the 2979 neonates born to Trent RHA residents who had begun high dependency care in Trent RHA or neighbouring health authorities between 1 April 1990 and 31 March 1992 and met any of the following criteria: (i) birth weight < 1500 g; (ii) gestation < 32 weeks; (iii) need for active respiratory support other than initial resuscitation; (iv) need for in utero or neonatal transfer to receive high dependency care; (v) severe asphyxial brain insult after delivery : and (vi) death. The analysis here is restricted to the 1730 neonates who received total parenteral nutrition or assisted ventilation, or both; that is, those who received NIC level 1 (ICL1) on at least one day. MEASUREMENT AND ANALYSIS--The treatment history of each neonate was converted into a time-line detailing the dates of beginning and stopping NIC, the dates of any transfers between units, and any gaps in NIC treatment. The duration of ICL1 was observed directly and that of intensive care level 2 (ICL20 was imputed from a model based upon round trip transfers. These were also recorded on the timeline. The time-lines were first used to derived the observed distribution of the utilisation of NIC cots in Trent RHA during the study. An extensive series of Monte Carlo simulations was then carried out in order; (i) to estimate cot requirements in smaller populations; (ii) to determine whether Trent RHA utilised its NIC cots in a manner that was clinically appropriate at the population based level; (iii) to perform a series of sensitivity analyses; and (iv) to compare results with an equivalent study carried out in the Northern RHA. MAIN RESULTS AND CONCLUSIONS--Trent RHA is reasonably representative of the greater population of England and Wales in terms of both the distribution of birth weight and of birth weight-specific neonatal mortality. Trent RHA did not seen to be underprovided for NIC cots or to be overusing these cots inappropriately. It therefore seems reasonable, if the assumptions of the analysis are borne carefully in mind, to treat these utilisation data as a rough guide to true population based need. NIC cot requirements depend critically upon the size of the served population - small populations are subject to greater random variability and require relatively more cots to ensure cot availability on an equivalent proportion of days. A neonatal unit should not therefore serve a population generating fewer than 5000 and 25 000 births per annum, the estimated population based provision which would ensure free cots on 29 out of 30 days falls gradually from 1.20 to 0.88 NIC cots per 1000 births per annum. A cooperative network of NICUs offers the opportunity to provide fewer cots per head of population while maintaining good access for most neonates referred to the service.
Full text
PDF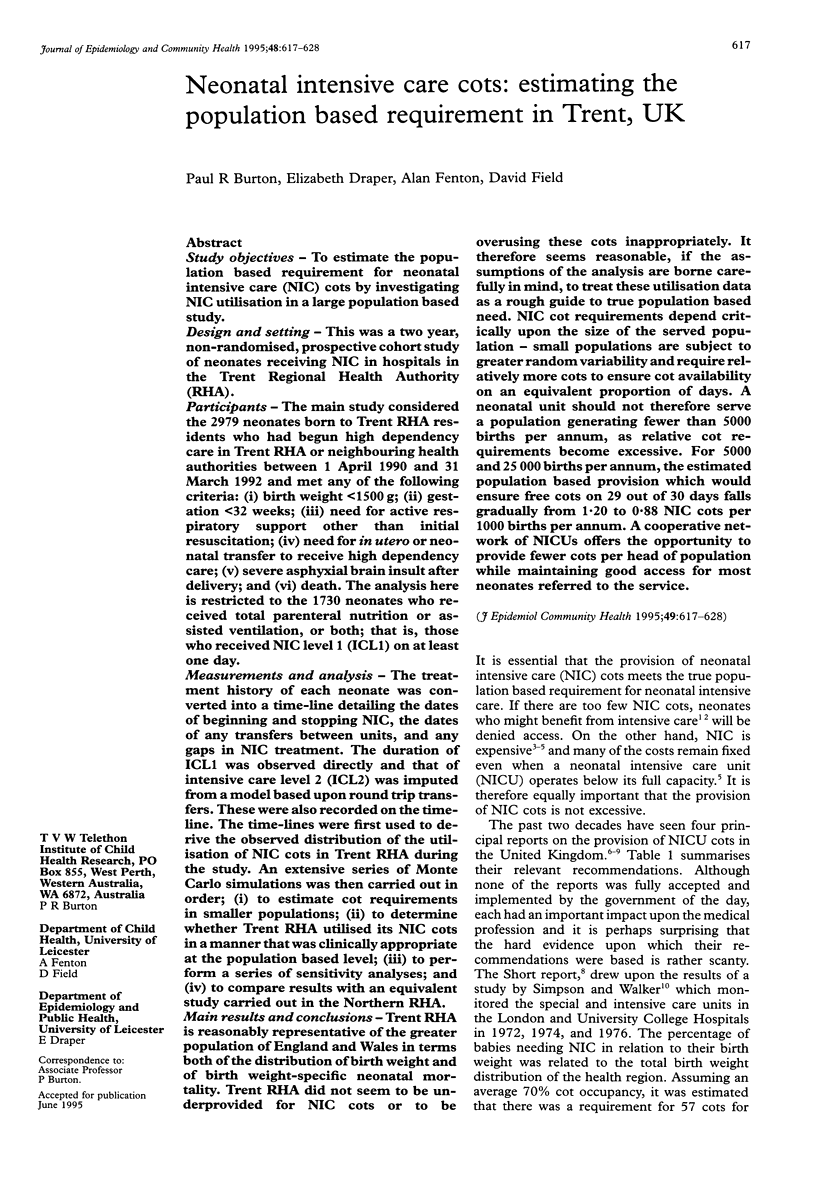

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Alberman E., Botting B. Trends in prevalence and survival of very low birthweight infants, England and Wales: 1983-7. Arch Dis Child. 1991 Nov;66(11):1304–1308. doi: 10.1136/adc.66.11.1304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Field D. J., Hodges S., Mason E., Burton P., Yates J., Wale S. The demand for neonatal intensive care. BMJ. 1989 Nov 25;299(6711):1305–1308. doi: 10.1136/bmj.299.6711.1305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fordham R., Field D. J., Hodges S., Normand C., Mason E., Burton P., Yates J., Male S. Cost of neonatal care across a regional health authority. J Public Health Med. 1992 Jun;14(2):127–130. [PubMed] [Google Scholar]
- Morris D., Handyside A. J. Effects of methods of admitting emergencies on use of hospital beds. Br J Prev Soc Med. 1971 Feb;25(1):1–11. doi: 10.1136/jech.25.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morriss F. H., Jr, Adcock E. W., 3rd, Denson S. E., Stoerner J. W., Malloy M. H., Johnson C. A., Decker M. Determination of newborn special care bed requirements by application of queuing theory to 1975-1976 morbidity experience. J Pediatr. 1978 Apr;92(4):668–671. doi: 10.1016/s0022-3476(78)80319-9. [DOI] [PubMed] [Google Scholar]
- PIKE M. C., PROCTOR D. M., WYLLIE J. M. ANALYSIS OF ADMISSIONS TO A CASUALTY WARD. Br J Prev Soc Med. 1963 Oct;17:172–176. doi: 10.1136/jech.17.4.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson C. J. Principles of organization of a neonatal intensive care unit from scratch. Clin Perinatol. 1976 Sep;3(2):329–335. [PubMed] [Google Scholar]
- Ryan S., Sics A., Congdon P. Cost of neonatal care. Arch Dis Child. 1988 Mar;63(3):303–306. doi: 10.1136/adc.63.3.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandhu B., Stevenson R. C., Cooke R. W., Pharoah P. O. Cost of neonatal intensive care for very-low-birthweight infants. Lancet. 1986 Mar 15;1(8481):600–603. doi: 10.1016/s0140-6736(86)92820-5. [DOI] [PubMed] [Google Scholar]
- Simpson H., Walker G. Estimating the cots required for neonatal intensive care. Arch Dis Child. 1981 Feb;56(2):90–93. doi: 10.1136/adc.56.2.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sims D. G., Wynn J., Chiswick M. L. Outcome for newborn babies declined admission to a regional neonatal intensive care unit. Arch Dis Child. 1982 May;57(5):334–337. doi: 10.1136/adc.57.5.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Speidel B. D. Skimping on care of the newborn is false economy. Br Med J (Clin Res Ed) 1986 Sep 6;293(6547):575–576. doi: 10.1136/bmj.293.6547.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swyer P. R. The regional organisation of special care for the neonate. Pediatr Clin North Am. 1970 Nov;17(4):761–776. doi: 10.1016/s0031-3955(16)32479-8. [DOI] [PubMed] [Google Scholar]


