Abstract
Orbital varices typically present with symptoms related to dilation or thrombosis. We describe a rare presentation of an orbital varix with pain caused by hemodynamic collapse of the varix. A woman in the third decade presented with position-dependent orbital pain and enophthalmos. She was found to have an intraorbital varix and a separate pterygoid varix. The patient underwent endovascular treatment of the pterygoid varix using coils and sclerosing agents which altered the venous outflow from the orbital varix. The patient had immediate resolution of symptoms after the procedure. Our findings suggest that extraorbital venous outflow abnormalities may be the cause of symptoms in selected cases of orbital varices. By understanding the venous structures on cerebral angiography and treating the extraorbital component, orbital intervention may be avoided, reducing the risk of complications.
Keywords: Orbital varix, Orbital pain, Endovascular treatment
Introduction
Orbital varices are an uncommon entity composed of dilated venous channels in the orbit that communicate with the normal venous system. Patients with orbital varices commonly present with intermittent proptosis, diplopia, exophthalmos, or pain induced by Valsalva maneuver, coughing, or change in position [1, 2]. We describe a patient with an orbital varix presenting with intermittent orbital pain and enophthalmos associated with head movement. The pain was successfully treated by altering the hemodynamic pathway utilizing endovascular techniques. The CARE Checklist has been completed by the authors for this case report, attached as online supplementary material (for all online suppl. material, see https://doi.org/10.1159/000531601).
Case Report
A woman in her early twenties with a history of right facial venous malformations presented with intermittent, severe right orbital pain during anterior-posterior head movement in the sagittal plane. The patient also complained of pain in the V1 and V2 distributions. The patient rated the pain as 9/10 on a pain scale, which affected daily activity. The patient described a sensation of the eyeball being pulled backward. The Valsalva maneuver induced swelling of the right buccal venous malformation without any ocular symptoms. The only abnormality during ophthalmological exam was mild right enophthalmos, with Hertel exophthalmometry measuring 13.5 mm in the right eye and 15 mm in the left eye with a base of 100 mm.
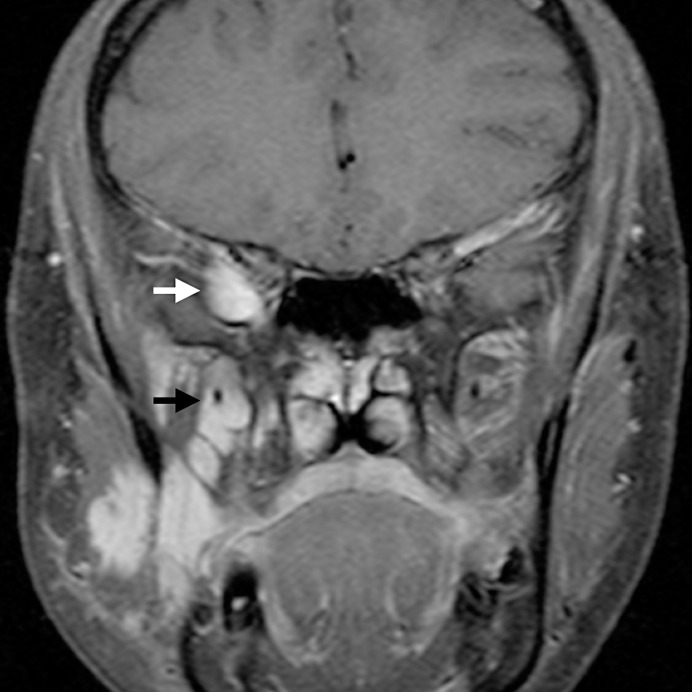
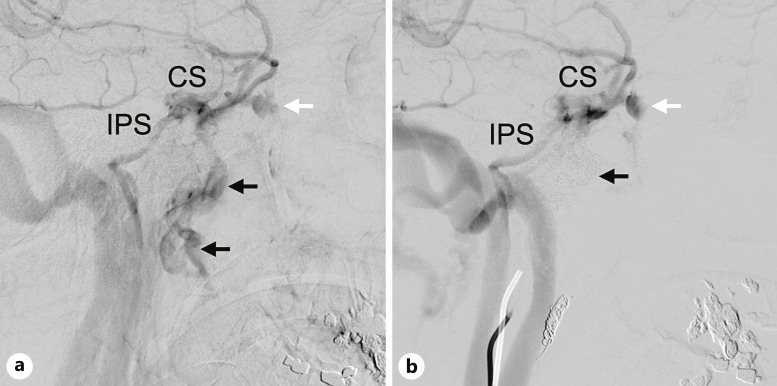
Magnetic resonance imaging demonstrated an orbital varix in the posterolateral extraconal space and a pterygoid plexus varix which was associated with the known facial venous malformation in the buccal region (Fig. 1). Right carotid angiogram revealed a 1.2-cm venous varix at the orbital apex draining into the cavernous sinus, and a separate 3.5-cm irregularly shaped varix in the pterygoid plexus and inferior petrosal sinus (Fig. 2a).
Fig. 1.
Magnetic resonance imaging. Contrast-enhanced T1-weighted coronal image of the head demonstrates dilated veins in the posterior-lateral orbit (white arrow) and in the pterygoid muscles (black arrow).
Fig. 2.
Cerebral angiogram. a Pre-treatment angiogram. Right internal carotid angiogram shows a venous varix at the posterior portion of the ophthalmic vein (white arrow) and a venous varix in the pterygoid plexus (black arrow). The cavernous sinus drains both through the inferior petrosal sinus and the pterygoid venous varix. b Post-treatment angiogram. Following the embolization, there is no flow of contrast through the pterygoid venous varix (black arrow). Note that the orbital varix (white arrow) remains and the venous flow drains only through the cavernous sinus and then the inferior petrosal sinus. CS: cavernous sinus. IPS: inferior petrosal sinus.
The decision was made to treat the pterygoid varix given that this was likely responsible for the patient’s recurrent pain in the V2 and V3 distributions. Additionally, the patient’s complaint was enophthalmos rather than proptosis, suggesting that the symptoms were unlikely to be due to engorgement of the orbital varix as in typical cases. After the selective carotid angiogram was performed, femoral vein access was obtained, followed by advancement of a 6 French guiding catheter into the right internal jugular vein under venous roadmapping. A microcatheter and a microguidewire were navigated into the venous varix through the guiding catheter. A total of 10 electrodetachable coils were deployed, effectively disconnecting the pterygoid varix from the cavernous sinus. A right ICA angiogram demonstrated a significant decrease in the varix’s opacification. Next, a sclerosing agent, 70% sodium tetradecyl sulfate (Sotradechol), mixed with 30% contrast and Avitene powder, was injected into the near-stagnant venous varix via the microcatheter (Fig. 2b). Sotradechol works by inducing inflammation and damage to the varix’s inner lining, leading to its shrinkage. Avitene, a microfibrillar collagen hemostat, was added to the mix to stimulate clot formation, augmenting the effectiveness of Sotradechol in obliterating the varix. Finally, two additional coils were deployed inferior to the venous varix to ensure complete trapping of the Sotradechol. After embolization, there was immediate redistribution of venous outflow from the orbital varix to the cavernous sinus and inferior petrosal sinus. During the same session, sodium tetradecyl sulfate and Avitene were injected percutaneously into the superficial components of the facial venous malformation under fluoroscopic guidance. Postoperatively, the orbital pain resolved and there was no recurrence for over 5 years. Informed consent for publication was provided from the patient.
Discussion
Symptoms from orbital varices typically occur due to distension during bending or the Valsalva maneuver and can also have acute onset of symptoms due to thrombosis or hemorrhage [3, 4]. Classically, patients have marked proptosis when leaning forward, but occasionally also have mild enophthalmos when upright or leaning backward due to fat atrophy caused by chronic venous engorgement [2, 5] Pulsating enophthalmos has also been reported as a result of associated orbital wall defects [6]. Pain and enophthalmos due to position-dependent collapse of an orbital varix, however, is exceedingly rare. The management of this pain, as we have described, may differ from the treatments for dilated or thrombosed varices.
Orbital varices are often managed with expectant observation. Intervention for orbital varices is reserved for symptomatic cases with intractable pain, severe proptosis, vision loss, or cosmetic disfigurement [7, 8]. Treatment options include surgical ligation, percutaneous sclerotherapy, endovascular treatment, and preoperative or intraoperative sclerotherapy followed by open surgery [9–11]. The literature on treatment of orbital varices is limited, and treatment guidelines are yet to be established. Open surgery is challenging because of the thin-walled vessels, the tendency to hemorrhage, and the lack of defined surgical margins [3]. Percutaneous sclerotherapy has the potential to cause orbital compartment syndrome due to the limited space in the orbit, where the pressure is increased within the orbit and lead to reduced perfusion and potential ischemia [4]. Transvenous embolization of orbital varices may lead to worsening of symptoms due to thrombosis, including pain and functional deficits [9, 12].
In our patient, we achieved hemodynamic alteration by transvenous obliteration of the pterygoid varix rather than attempting the relatively invasive orbital varix embolization. Prior to treatment, head movement likely led to an increase in venous outflow to the pterygoid varix and subsequent collapse of the orbital varix, causing enophthalmos and pain. Embolization and exclusion of the pterygoid varix from the venous outflow pathway then led to resolution of the patient’s symptoms. The patient’s severe pain (rated as 9/10 on the pain scale), its clear relationship with head movement, and its immediate and long-lasting resolution following our intervention strongly suggest a primary physiological cause. However, we recognize that psychosomatic factors may contribute to the symptom profile and must be considered in the overall assessment and management of such cases.
This case suggests that venous structures surrounding the orbital lesion should be carefully assessed on cerebral angiography. In selected cases with symptoms caused by hemodynamic changes in associated extraorbital components, treatment of extraorbital components may resolve symptoms, eliminating the need for direct intervention within the orbit.
Statement of Ethics
This study complies with the Declaration of Helsinki and is compliant with the Health Insurance Portability and Accountability Act. Written informed consent was obtained from the patient for the publication of the details of their medical case and any accompanying images. This retrospective review of patient data did not require ethical approval in accordance with local/national guidelines.
Conflict of Interest Statement
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Funding Sources
There are no funding sources.
Author Contributions
Naoki Kaneko and Ariel Takayanagi wrote this manuscript and conducted the relevant literature search associated with it. Daniel B. Rootman participated in the care of this patient and wrote this manuscript. Robert Goldberg and Gary R. Duckwiler offered expert opinion and edits. Satoshi Tateshima is the senior author who was the primary operator of the endovascular procedure, composed the treatment strategy, and oversaw the manuscript.
Funding Statement
There are no funding sources.
Data Availability Statement
All data generated or analyzed during this study are included in this article and its online supplementary material. Further inquiries can be directed to the corresponding author.
Supplementary Material
References
- 1. Rootman J. Vascular malformations of the orbit: hemodynamic concepts. Orbit. 2003;22(2):103–20. 10.1076/orbi.22.2.103.14311. [DOI] [PubMed] [Google Scholar]
- 2. Mokhtarzadeh A, Garrity JA, Cloft HJ. Recurrent orbital varices after surgical excision with and without prior embolization with n-butyl cyanoacrylate. Am J Ophthalmol. 2014;157(2):447–50.e1. 10.1016/j.ajo.2013.10.011. [DOI] [PubMed] [Google Scholar]
- 3. Singh V, Phadke RV, Udiya A, Shetty GS, Sharma K, Kanaujia V. Inferior petrosal sinus route microcatheterization study and embolization for primary orbital varix. Interv Neuroradiol. 2016;22(1):108–15. 10.1177/1591019915617318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Vadlamudi V, Gemmete JJ, Chaudhary N, Pandey AS, Kahana A. Transvenous sclerotherapy of a large symptomatic orbital venous varix using a microcatheter balloon and bleomycin. J Neurointerv Surg. 2016;8(8):e30. 10.1136/neurintsurg-2015-011777.rep. [DOI] [PubMed] [Google Scholar]
- 5. Rivas JJ, Lobato RD, Cordobés F, Barcena A, Millán JM. Intermittent exophthalmos studied with computerized tomography. Report of two cases. J Neurosurg. 1982;57(2):290–4. 10.3171/jns.1982.57.2.0290. [DOI] [PubMed] [Google Scholar]
- 6. Prabhakaran VC, Selva D. Pulsating enophthalmos in association with an orbital varix. Indian J Ophthalmol. 2009;57(3):225–7. 10.4103/0301-4738.49399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mavilio N, Pau A, Pisani R, Casasco A, Rosa M. Embolisation of orbital varix via the superficial temporal vein. Interv Neuroradiol. 2000;6(2):137–40. 10.1177/159101990000600209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Takechi A, Uozumi T, Kiya K, Yano T, Sumida M, Yoshikawa S, et al. Embolisation of orbital varix. Neuroradiology. 1994;36(6):487–9. 10.1007/BF00593691. [DOI] [PubMed] [Google Scholar]
- 9. Couch SM, Garrity JA, Cameron JD, Cloft HJ. Embolization of orbital varices with N-butyl cyanoacrylate as an aid in surgical excision: results of 4 cases with histopathologic examination. Am J Ophthalmol. 2009;148(4):614–8.e1. 10.1016/j.ajo.2009.04.024. [DOI] [PubMed] [Google Scholar]
- 10. Strianese D, Bonavolontà G, Iuliano A, Mariniello G, Elefante A, Liuzzi R. Risks and benefits of surgical excision of orbital cavernous venous malformations (So-Called cavernous hemangioma): factors influencing the outcome. Ophthalmic Plast Reconstr Surg. 2021 May–Jun 01;37(3):248–54. 10.1097/IOP.0000000000001767. [DOI] [PubMed] [Google Scholar]
- 11. De Maria L, De Sanctis P, Tollefson M, Mardini S, Garrity JA, Morris PP, et al. Sclerotherapy for low-flow vascular malformations of the orbital and periocular regions: systematic review and meta-analysis. Surv Ophthalmol. 2020;65(1):41–7. 10.1016/j.survophthal.2019.08.003. [DOI] [PubMed] [Google Scholar]
- 12. Sia PI, Sia DI, Scroop R, Selva D. Orbital compartment syndrome following transvenous embolization of carotid-cavernous fistula. Orbit. 2014;33(1):52–4. 10.3109/01676830.2013.841717. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during this study are included in this article and its online supplementary material. Further inquiries can be directed to the corresponding author.