Abstract
Introduction
Optic nerve (ON) enhancement alone without ON thickening on contrast-enhanced magnetic resonance imaging (CE-MRI) can be associated with post-laminar optic nerve invasion (PLONI) in eyes with group E retinoblastoma. A few case reports and retrospective studies in the literature show a poor correlation between ON enhancement on MRI and ON invasion on histopathological examination (HPE). There is no universal consensus on the management of such cases. It is desirable that the presence and extent of a true ON invasion be reliably picked up before planning upfront enucleation in order to avoid stage II disease.
Methods
In a prospective study conducted at a tertiary eye care center in North India, all retinoblastoma patients presenting with ON enhancement on imaging were evaluated. Demographic and imaging details, histopathological findings, and treatment details were recorded. The length and pattern of enhancement noted on MRI were correlated with histopathology. Follow-up was done till the end of the study period.
Results
Six group E retinoblastoma eyes were evaluated. 3 eyes (50%) showed solid enhancement, 2 eyes (33.33%) had tram track pattern and 1 eye (16.66%) showed punctate enhancement pattern on CE-MRI. On histopathology, 5 (83.33%) cases showed PLONI and all 6 (100%) had ON head infiltration. The cut end of the ON was free in all cases. On correlating MRI and HPE, all eyes with solid enhancement pattern showed PLONI, of which 2/3 (66.6%) had diffuse ON infiltration. Only 50% of eyes with tram track patterns showed PLONI. The case which showed a punctate enhancement pattern showed focal infiltration by tumor cells with vacuolated cytoplasm on HPE. At the last follow-up, all patients were alive and free of disease.
Conclusion
ON enhancement patterns may make it more predictive for PLONI on HPE. Solid enhancement pattern appears to correlate better with the extent of ON invasion on HPE, and longer lengths of solid ON enhancement may be considered for neoadjuvant chemotherapy rather than upfront enucleation.
Keywords: Extraocular retinoblastoma, Optic nerve enhancement, Ocular oncology, Ocular pathology, Ocular radiology
Introduction
The diagnosis of extraocular retinoblastoma (International Retinoblastoma Staging System, IRSS stage III) is based on baseline contrast-enhanced magnetic resonance imaging (CE-MRI) of orbit. Preoperative prediction of optic nerve (ON) invasion is important because ON involvement alters treatment and prognosis. ON thickening with enhancement on MRI is considered a definite sign of ON invasion and is treated with neoadjuvant chemotherapy, enucleation, adjuvant chemotherapy, and external beam radiotherapy. On the other hand, ON enhancement alone without ON thickening can be associated with post-laminar optic nerve invasion (PLONI). ON enhancement may also be seen in cases of retinoblastoma with aseptic orbital cellulitis. There are a few case reports and retrospective studies in the literature that show a poor correlation between ON enhancement and ON invasion on histopathological examination (HPE) [1–4]. There is no clear consensus on the treatment of such cases, while some authors advocate upfront enucleation and adjuvant chemotherapy after confirmation on HPE, others have preferred neoadjuvant chemotherapy, thus considering them an extraocular disease [5]. While it is important not to overtreat these patients as both chemotherapy and radiotherapy are associated with serious side effects and complications, it is desirable that the extent of ON invasion be picked up before planning upfront enucleation, thus avoiding stage II disease, which is known to have a grim prognosis. Hence, findings of preoperative ON enhancement need to be evaluated further to see if defining patterns of enhancement could make this finding more predictive of ON invasion. Herein, we report the radiological patterns of enhancement in 6 cases of retinoblastoma with ON enhancement only and correlate them with histopathology findings.
Methods
This was a prospective study conducted from January 2020 to August 2022 at a tertiary eye care center in North India. Institute Ethics Committee approval was obtained for the study (IECPG-80/February 27, 2020). All retinoblastoma patients showing ON enhancement on imaging were evaluated. Patients who had received prior treatment or presented with features of orbital cellulitis were excluded. Written informed consent from LAR was taken. Clinical data including age, sex, familial disease, lag time, the first sign, and presenting signs were noted. CE-MRI films of the orbit which were performed with a 1.5 T MRI scanner using a standard head coil were read by a single radiologist. The ON enhancement was evaluated on post-gadolinium T1-weighted images. It was compared with the contralateral ON in unilateral disease or age-matched controls in a patient with bilateral disease. Signs of orbital cellulitis were ruled out in all patients clinically and radiologically. The length and pattern of enhancement, tumor morphology, location, and size were also noted. All patients underwent upfront enucleation within 3 weeks of the MRI. Patients undergoing enucleation more than 3 weeks from the time of MRI were excluded.
Histopathological evaluation of the enucleated eyes was done by a single ocular pathologist. The presence and extent of ON invasion were noted [6]. Other high-risk features including choroidal, scleral, and anterior chamber invasion were also noted where present. Tumor differentiation, amount of necrosis, and presence of microscopic residual disease were noted if present. Adjuvant treatment, if any was given, was noted. Death, systemic metastasis, or local recurrence, if found, were noted. Follow-up was updated till August 2022.
Results
Demographic Data
Six eyes of consecutive patients with ICRB group E retinoblastoma showing an ON enhancement without any ON thickening were recruited during the study period. The mean age of the cohort was 24.66 months (range: 4 months–48 months). All were males. There was no history of consanguinity or familial disease. Two cases were bilateral (n = 2/6, 33.33%). The presenting complaint was leukocoria in all cases. The mean lag time was 2.41 months (15 days–5 months).
Imaging Findings (Table 1)
The length of ON enhancement ranged from 1 mm to 26 mm. Additionally, choroidal invasion was present on MRI in 5/6 cases. There was no scleral breach or anterior segment involvement in any of the eyes (Table 1).
Table 1.
Clinical, Imaging, histopathology details, and outcome
| Pt | Age (m) | Sex | Laterality | Lag time (m) | Group | MRI findings | HPE findings | Outcome (months of follow-up) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OD | OS | ONH | pattern | length | TV | other HRF | RLONI | length | diff. | HRF | ||||||
| 1 | 4 | M | BL | 2 | E | A | + | S | 2 mm | 2/3 | Choroidal invasion | Present | 5 mm | WD | FCI | Alive, FOD (22) |
| 2 | 24 | M | UL | 3 | E | + | T | 26 mm | 2/3 | Choroidal invasion | Present | 1.5 mm | PD | MCI SI, ESI |
Alive, FOD (21) | |
| 3 | 12 | M | BL | 3 | C | E | + | T | 5 mm | 2/3 | Choroidal invasion | Absent | none | WD | MCI | Alive, FOD (26) |
| 4 | 36 | M | UL | 5 | E | + | P | 1 mm | 1/2 | Choroidal invasion | Present | 4 mm | PD | – | Alive, FOD (28) | |
| 5 | 24 | M | UL | 1 | E | + | S | 2 mm | 1/3 | Absent | Present | 5.5 mm | PD | FCI | Alive, FOD (25) | |
| 6 | 48 | M | UL | 0.5 | E | + | S | 2 mm | 1/3 | Choroidal invasion | Present | 1.5 mm | PD | MCI | Alive, FOD (21) | |
Pt, patient code; m, months; M, male; BL, bilateral; UL, unilateral; OD, oculus dextrus; OS, oculus sinister; group, Intraocular Classification of Retinoblastoma; MRI, magnetic resonance imaging; ONH, optic nerve head; S, solid; T, tram track; P, punctate; mm, millimeter; TV, tumor volume (in fraction of globe); HPE, histopathological examination; RLONI, retrolaminar optic nerve invasion; HRF, high-risk features; diff., differentiation; PD, poorly differentiated; WD, well differentiated; FCI, focal choroidal invasion; MCI, massive choroidal invasion; SI, scleral invasion; ESI, extrascleral invasion; FOD, free of disease;
Patterns of Enhancement
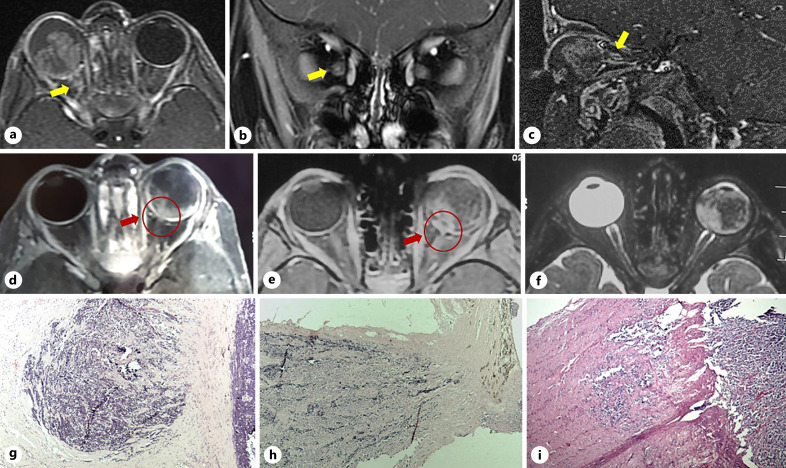
We observed 3 types of ON enhancement patterns on CE-MRI: solid, tram track, and punctate (Fig. 1). Solid pattern was defined as full thickness enhancement of the involved length of the ON. Tram track pattern showed only ON sheath enhancement. Punctate enhancement appeared as patchy contrast enhancement of ON. Three patients (3/6, 50%) showed solid enhancement, 2 patients (2/6, 33.33%) had tram track pattern, and 1 patient (1/6, 16.66%) showed punctate pattern of enhancement on MRI imaging.
Fig. 1.
CE-MRI scan of the orbit. a–c Axial, coronal, and sagittal sections showing tram track pattern of enhancement in the eye with retinoblastoma (yellow arrow). d, e Axial section showing solid enhancement of 2 mm and punctate enhancement pattern, respectively, as illustrated by red arrow. f T2w axial scan of orbit showing normal-sized ON in a case with punctate enhancement of the ON. g–i Microphotograph of histopathological sections (hematoxylin and eosin stain, 4x) of cases with tram-track, solid, and punctate enhancement showing focal and diffuse infiltration of the ON by tumor cells and focal infiltration with tumor cells with vacuolated cytoplasm, respectively.
Histopathology Findings (Table 2)
On HPE of enucleated eyes, the tumor was well differentiated in 2 and poorly differentiated in 4 cases. All eyes showed extensive areas of tumor necrosis (grade 3+) and calcification. Five cases showed retrolaminar tumor invasion of the ON, and all 6 (100%) patients had ON head infiltration. Massive choroidal invasion was noted in 3 eyes, one of which also showed extrascleral tumor invasion. The cut end of the ON was free in all cases (Table 2).
Table 2.
Histopathology details of eyes with ON enhancement
| SL No. | Grading of necrosis | Differentiation | Tumor dimensions (height × base diameter in mm) | ON invasion | Other HRF | MRD | |||
|---|---|---|---|---|---|---|---|---|---|
| Length of PLONI | Pattern of on invasion | Choroidal invasion | Iris/CB invasion | Scleral invasion | |||||
| 1 | 3+ | Well differentiated | 7.63 × 9.24 | 5 mm | Diffuse | Focal | Absent | Absent | Absent |
| 2 | 3+ | Poorly differentiated | 18 × 21 | 1.5 mm | Focal | Massive | Absent | Present | Extrasceral invasion |
| 3 | 3+ | Well differentiated | 21 × 19 | none | Not applicable | Massive | Absent | Absent | Absent |
| 4 | 3+ | Poorly differentiated | 18 × 15 | 4 mm | Focal, with vacuolated cytoplasm | Absent | Absent | Absent | Absent |
| 5 | 3+ | Poorly differentiated | 21 × 16 | 5.5 mm | Diffuse | Focal | Absent | Absent | Absent |
| 6 | 3+ | Poorly differentiated | 10 × 15 | 1.5 mm | Focal | Massive | Absent | Absent | Absent |
PLONI, post-laminar optic nerve invasion; CB, ciliary body; HRF, high-risk features; MRD, microscopic residual disease.
The mean height and base diameter of intraocular tumor on MRI were 17.54 (standard error ± 1.84) and 14.27 (standard error ± 1.92), respectively. There was no statistically significant difference (p: 0.263, 0.336) in the mean height or basal diameter between the cases with and without post-laminar ON and/or extrascleral tumor extension on histopathology. There was no correlation between the length of enhancement and histopathological length of involvement of the ON (Spearman’s rho −0.5643).
When we correlated the pattern of involvement on MRI and HPE, out of 3 patients with solid enhancement pattern, 2 showed diffuse infiltration of the ON (66.66%) and one showed focal infiltration in the retrolaminar area (33.33%). Diffuse infiltration was defined as full-thickness invasion of the post-laminar ON, while focal infiltration was defined as invasion limited to a few clusters of tumor cells.
Of the 2 eyes showing tram track pattern, one showed focal retrolaminar infiltration, and the other showed only prelaminar ON involvement without any retrolaminar infiltration. For the case which showed a punctate enhancement pattern, we observed focal infiltration of tumor cells with vacuolated cytoplasm on HPE. The data are summarized in Table 2.
Treatment Details and Follow-Up
All eyes were enucleated within an average of 1.66 weeks of the MRI (1–3 weeks). The mean ON stump obtained was 8.33 mm (6–10 mm). Adjuvant chemotherapy 6 cycles for high-risk histology was given in 5 cases. Adjuvant 12 cycles of chemotherapy and external beam radiotherapy were administered in 1 case with stage 2 disease (extrascleral invasion). At the last follow-up of 23.83 months (range: 21–28 months), all patients were alive and free of disease.
Discussion
The frequency of ON invasion, in eyes enucleated for retinoblastoma, on histopathology is reported to be 29–48% [7, 8]. Microscopic ON invasion is picked up on histopathology, while gross extraocular ON disease can be identified on baseline imaging as ON thickening. These represent the spectrum of ON invasion by the tumor. While microscopic PLONI not reaching the resected end of ON logically has no orbital residual disease, it still has a risk of CSF spreading through the CSF sleeve of ON. There are occasional case reports in the literature of CNS metastasis in cases with PLONI [9]. Stage II disease or histopathological invasion of resected margin of ON has a significantly poorer prognosis despite aggressive treatment with chemotherapy and radiotherapy. Preoperative identification of microscopic ON invasion thus becomes desirable, mainly in order to avoid stage II disease. Preoperative baseline staging of retinoblastoma is best done on MRI. 1.5 T is the most commonly used field strength in MRI evaluation of retinoblastoma. The main advantage of (higher field strength) 3 T versus 1.5 T MRI is the increased signal to noise and possibly an improved diagnostic accuracy with the use of multichannel head coils. But there is limited published literature to support this. Also, the cost of a 3 T MRI is higher as compared to 1.5 T MRI. According to published guidelines for evaluation of retinoblastoma, the field strength of the MR system should be at least 1.5 T [2]. There are few reports on the use of ultrahigh-field 7T MRI, reporting superior submillimeter resolution for ocular structures and intraocular tumors, but these are mostly experimental [10].
ON enhancement without thickening is considered to suggest PLONI. Several studies have been conducted to evaluate this imaging finding and its ability to predict the histopathological invasion of the ON. However, most studies report a poor correlation with histopathology. All studies were limited by a small number of patients with PLONI (4.8–11.1%), and this has precluded a detailed correlation between the MRI and histological findings of ON invasion [5]. Most studies have demonstrated high specificity of 93–100% but low sensitivity varying from 50 to 67% of ON enhancement for predicting histological ON invasion (PLONI). Also, there are several case reports reporting that an ON enhancement on MRI may not correlate with histological invasion [2, 4, 11]. The positive predictive value as reported by a few studies has ranged from 60 to 100% [1–4].
Aseptic orbital cellulitis in cases of retinoblastoma can also present with ON enhancement on imaging. However, in such cases, there are additional signs including fat stranding, extraocular muscle enlargement, and lacrimal gland enlargement which help identify the cellulitis. The cause of aseptic cellulitis is believed to be either autoinfarction or immune-mediated tumor necrosis. ON enhancement in such cases is more likely to be due to associated inflammation of ocular coats and orbital contents. A recent study attempted to describe enhancement pattern likely to suggest inflammatory enhancement rather than tumor-related enhancement [12]. We excluded such cases in our study in order to eliminate inflammation-related enhancement and evaluate enhancement patterns likely to be due to tumor invasion.
Brisse et al. [4] studied 5 cases of retinoblastoma that were primarily enucleated and had abnormal ON enhancement on baseline CE-MRI and found 3 cases to have a true invasion on pathology. The meningeal enhancement found in one case was attributed to inflammatory changes. Two cases with false-positive MRI findings were ascribed to a posterior bulge of the ON lamina cribrosa. The authors discussed that the length of ON invasion was not underestimated by MRI in true positives and suggested that the length of ON enhancement could be a useful criterion to increase the specificity of MR for detecting ON invasion.
Song et al. [13] reported imaging and histopathology correlation for ON invasion in 41 eyes that underwent either primary or secondary enucleation; 10 of these had PLONI on histopathology. They have described two patterns of enhancement: focal strong and diffuse mild enhancement and found an excellent inter-observer agreement for identifying strong focal enhancement as compared to those with diffuse mild enhancement. Also, the authors reported that the extent of enhancement in cases with diffuse mild enhancement did not correlate with the length of tumor involvement on HPE or even the presence of tumor invasion in some cases as there was no tumor overlying ON head. They hypothesized that local hemodynamic mechanisms may be responsible for diffuse mild enhancement. They concluded that a focal strong pattern of enhancement may estimate the extent of ON invasion and hence the tumor burden in ON.
Some authors advocate routine use of NACT to reduce the risk of residual disease and CNS metastasis in cases with ON enhancement without thickening [5]. Armenian et al. [5] quoted 2 cases with ON enhancement who underwent upfront enucleation and were found to have ON cut end invasion on histopathology. They reported the use of NACT in a series of 9 cases with ON enhancement and advocated the use of NACT in cases with ON enhancement to reduce tumor burden at the time of enucleation in such cases. Radhakrishnan et al. [14] proposed a staging system for ON invasion on MRI. They reported treatment outcomes in 8 cases with ON enhancement alone of less than 5 mm (stage 1) that were treated with chemotherapy and radiotherapy, one of which died of CNS relapse at 9.8 months of follow-up, while 6 out of 8 cases were free of disease at a mean follow-up of 24 months (range 21.37–27.87 months). Therefore, the treatment for patients with ON enhancement with normal-sized ONs remains debatable.
In our study, we found 3 types of patterns of ON enhancement on MRI in 6 cases of RB that were enucleated primarily: solid, tram track, and punctate. A solid pattern of enhancement showed the greatest likelihood of PLONI on HPE. 2 of 3 cases with the solid pattern of enhancement showed diffuse, i.e., full thickness ON invasion, and one case showed focal infiltration in the retrolaminar area (Fig. 1). Other patterns, i.e., punctate (seen as specs of enhancement within the proximal ON) and tram track (enhancement of ON sheath), had no or focal invasion of the ON on HPE, and there was no correlation found with length of involvement. The mean ON stump length of the enucleated eye was 6 mm, and none showed cut-end positivity for tumor invasion. All the patients received adjuvant chemotherapy post-enucleation, and no event was observed in any patient till the last follow-up.
The punctate enhancement seen in our study appears similar to the “double dot” pattern described by Brisse et al. [15]. The authors reported that such a double dot pattern showed no correlation with ON invasion and was likely to be due to dilated vascular channels. However, in our study, no dilated vascular channels were identified, and interestingly, vacuolated tumor cells were identified in focal clusters. The solid enhancement pattern of our study perhaps may be similar to the strong focal enhancement pattern described by an earlier study and appears to have a stronger predictive potential for HPE invasion of ON [13]. Although our study is limited by the small number of patients, observations made in the study indicate the need of defining patterns of enhancement in cases with normal-sized ONs in retinoblastoma, in order to improve the sensitivity of this MRI finding.
On reviewing our previous records, we found 6 patients with ON contrast enhancement, two of whom were treated with upfront enucleation. One of the patients showed ON cut-end invasion by tumor cells, and on reviewing the MRI of this patient, found a solid enhancement pattern of 5 mm length.
Thus, the clinical application of the observations made in this study can be that if the enhancement pattern is solid with longer lengths, i.e., 5 mm or more, then probably neoadjuvant chemotherapy may be more advisable to reduce tumor burden in the ON, while if it is tram track (or diffuse mild enhancement), even longer lengths of invasion may be treated with upfront enucleation. Also, all cases in our study showed severe degrees of tumor necrosis, pointing toward a possible correlation between enhancement and tumor necrosis. This needs to be evaluated in further studies.
To conclude, ON enhancement patterns may make it more predictive for ON invasion on HPE. Solid enhancement patterns appear to correlate better with the extent of ON invasion on HPE, and longer lengths of solid ON enhancement may be considered for neoadjuvant chemotherapy rather than upfront enucleation.
Acknowledgment
The authors would like to thank Veena, Statistician, AIIMS, New Delhi.
Statement of Ethics
This study protocol was reviewed and approved by Ethics Committee, All India Institute of Medical Sciences, New Delhi, approval number IECPG-80/February 27, 2020. Written informed consent was obtained from the parent/legal guardian of the patients to participate in the study for all participants. Written informed consent was obtained from the parents/legal guardians of the patients for publication of the details of their medical case and any accompanying images.
Conflict of Interest Statement
The authors have no conflicts of interest to declare.
Funding Sources
No funding was received from any sources for the study.
Author Contributions
Madhu Chiranthan: drafting the work or revising it critically for important intellectual content. Rachna Meel: final approval of the version to be published. Sanjay Sharma, Neiwete Lomi, Seema Kashyap, and Mandeep S. Bajaj: substantial contributions to the acquisition, analysis, and interpretation of data for the work.
Funding Statement
No funding was received from any sources for the study.
Data Availability Statement
All data generated or analyzed during this study are included in this article. Further inquiries can be directed to the corresponding author.
References
- 1. Schueler AO, Hosten N, Bechrakis NE, Lemke AJ, Foerster P, Felix R, et al. High resolution magnetic resonance imaging of retinoblastoma. Br J Ophthalmol. 2003;87(3):330–5. 10.1136/bjo.87.3.330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. de Graaf P, Barkhof F, Moll AC, Imhof SM, Knol DL, van der Valk P, et al. Retinoblastoma: MR imaging parameters in detection of tumor extent. Radiology. 2005;235(1):197–207. 10.1148/radiol.2351031301. [DOI] [PubMed] [Google Scholar]
- 3. Barkhof F, Smeets M, van der Valk P, Tan KE, Hoogenraad F, Peeters J, et al. MR imaging in retinoblastoma. Eur Radiol. 1997;7(5):726–31. 10.1007/BF02742934. [DOI] [PubMed] [Google Scholar]
- 4. Brisse HJ, Guesmi M, Aerts I, Sastre-Garau X, Savignoni A, Lumbroso-Le Rouic L, et al. Relevance of CT and MRI in retinoblastoma for the diagnosis of postlaminar invasion with normal-size optic nerve: a retrospective study of 150 patients with histological comparison. Pediatr Radiol. 2007;37(7):649–56. 10.1007/s00247-007-0491-4. [DOI] [PubMed] [Google Scholar]
- 5. Armenian SH, Panigrahy A, Murphree AL, Jubran RF. Management of retinoblastoma with proximal optic nerve enhancement on MRI at diagnosis. Pediatr Blood Cancer. 2008;51(4):479–84. 10.1002/pbc.21604. [DOI] [PubMed] [Google Scholar]
- 6. Sastre X, Chantada GL, Doz F, Wilson MW, de Davila MT, Rodríguez-Galindo C, et al. Proceedings of the consensus meetings from the International Retinoblastoma Staging Working Group on the pathology guidelines for the examination of enucleated eyes and evaluation of prognostic risk factors in retinoblastoma. Arch Pathol Lab Med. 2009;133(8):1199–202. 10.5858/133.8.1199. [DOI] [PubMed] [Google Scholar]
- 7. Kim U, Rathi G, Chowdhary G, Srinavasan KG, Shanthi R, Krishna RSP. Accuracy of preoperative imaging in predicting optic nerve invasion in retinoblastoma: a retrospective study. Indian J Ophthalmol. 2019;67(12):2019–22. 10.4103/ijo.IJO_1611_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wong FL, Boice JD Jr, Abramson DH, Tarone RE, Kleinerman RA, Stovall M, et al. Cancer incidence after retinoblastoma. Radiation dose and sarcoma risk. JAMA. 1997;278(15):1262–7. 10.1001/jama.278.15.1262. [DOI] [PubMed] [Google Scholar]
- 9. de Jong MC, Van Der Valk P, Jansen RW, Abbink F, Bosscha M, Castelijns JA, et al. Full-width postlaminar optic nerve tumor invasion of retinoblastoma as risk-factor for leptomeningeal spread of retinoblastoma. A case report and review of the literature. Ophthalmic Genet. 2020;41(1):69–72. 10.1080/13816810.2020.1727535. [DOI] [PubMed] [Google Scholar]
- 10. Singh AD, Platt S, Lystad L, Lowe M, Oh S, Jones SE, et al. Optic nerve assessment using 7-tesla magnetic resonance imaging. Ocul Oncol Pathol. 2016;2(3):178–80. 10.1159/000443650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. de Graaf P, Moll AC, Imhof SM, van der Valk P, Castelijns JA. Retinoblastoma and optic nerve enhancement on MRI: not always extraocular tumour extension. Br J Ophthalmol. 2006;90(6):800–1. 10.1136/bjo.2005.089383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jansen RW, van der Heide S, Cardoen L, Sirin S, de Bloeme CM, Galluzzi P, et al. Magnetic resonance imaging can reliably differentiate optic nerve inflammation from tumor invasion in retinoblastoma with orbital cellulitis. Ophthalmology. 2022;129(11):1275–86. 10.1016/j.ophtha.2022.06.013. [DOI] [PubMed] [Google Scholar]
- 13. Song KD, Eo H, Kim JH, Yoo SY, Jeon TY. Can preoperative MR imaging predict optic nerve invasion of retinoblastoma? Eur J Radiol. 2012;81(12):4041–5. 10.1016/j.ejrad.2012.03.034. [DOI] [PubMed] [Google Scholar]
- 14. Radhakrishnan V, Sharma S, Vishnubhatla S, Bakhshi S. MRI findings at baseline and after neoadjuvant chemotherapy in orbital retinoblastoma (IRSS stage III). Br J Ophthalmol. 2013;97(1):52–8. 10.1136/bjophthalmol-2012-301977. [DOI] [PubMed] [Google Scholar]
- 15. Brisse HJ, de Graaf P, Galluzzi P, Cosker K, Maeder P, Göricke S, et al. Assessment of early-stage optic nerve invasion in retinoblastoma using high-resolution 1.5 Tesla MRI with surface coils: a multicentre, prospective accuracy study with histopathological correlation. Eur Radiol. 2015;25(5):1443–52. 10.1007/s00330-014-3514-1. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this article. Further inquiries can be directed to the corresponding author.