Abstract
Background
Podocytes are essential components of the glomerular filtration barrier and essential for the proper filtration function of the glomerulus. Podocyte injury under various stress conditions is the primary pathogenesis and key determinant of focal segmental glomerulosclerosis (FSGS) with prominent clinical manifestations of proteinuria or nephrotic syndrome.
Summary
Under physiological conditions, a highly coordinated mitochondrial quality control system, including antioxidant defenses, mitochondrial dynamics (fusion, fission, and mitophagy), and mitochondrial biogenesis, guarantees the sophisticated structure and various functions of podocytes. However, under FSGS pathological conditions, mitochondria encounter oxidative stress, dynamics disturbances, and defective mitochondrial biogenesis. Moreover, mutations in mitochondrial DNA and mitochondria-related genes are also strongly associated with FSGS. Based on these pieces of evidence, bioactive agents that function to relieve mitochondrial oxidative stress and promote mitochondrial biogenesis have been proven effective in preclinical FSGS models. Targeting the mitochondrial network is expected to provide new therapeutic strategies for the treatment of FSGS and delay its progression to end-stage renal disease.
Key Messages
Mitochondrial dysfunction plays a key role in podocyte injury and FSGS progression. This review summarized recent advances in the study of mitochondrial homeostatic imbalance and dysfunction in FSGS and discussed the potential of mitochondria-targeted therapeutics in improving FSGS and retarding its progression to end-stage renal disease.
Keywords: Mitochondria, Podocyte, Focal segmental glomerulosclerosis
Introduction
Focal segmental glomerulosclerosis (FSGS) is a common clinicopathological syndrome with prominent clinical manifestations of proteinuria or nephrotic syndrome. The pathology is characterized by the obstruction of glomerular capillary loops by sclerotic material, and the glomerular sclerosis lesions are typically focal (less than 50% glomerular involvement) and segmental (less than 50% glomerular tuft involvement) [1]. It is also accompanied by effacement or loss of foot processes due to podocyte degeneration, as seen under electron microscopy [2]. As an important cause of end-stage renal disease worldwide, the incidence of FSGS is gradually increasing; however, treatments using steroids and immunosuppressive agents remain unsatisfactory. Moreover, even after kidney transplantation, FSGS can still recur in some cases [3]. Therefore, it is urgent to explore novel therapeutic targets and effective treatment strategies to attenuate renal injury in FSGS.
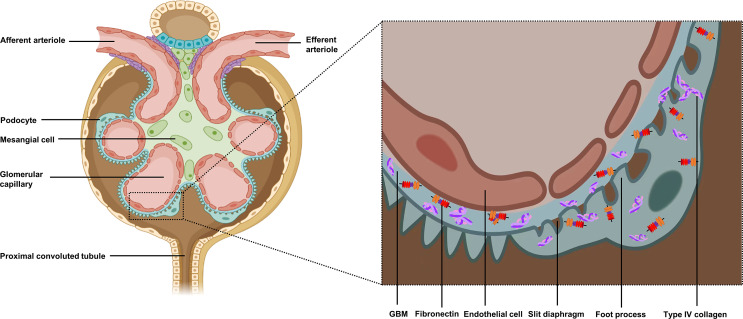
Regardless of the etiology of FSGS, a common feature is that the initial event occurs in podocytes [4]. Podocytes are highly differentiated epithelial cells with limited regenerative capacity. Under physiological conditions, the interdigitated foot processes of adjacent podocytes, connected by slit diaphragms, are essential for the proper filtration function of the glomerulus. Podocytes also play an important role in the metabolic balance of the glomerular basement membrane (GBM) by secreting type IV collagen and fibronectin for GBM formation, as well as matrix metalloproteinases and histone proteases for GBM degradation [5] (shown in Fig. 1). However, in the face of genetic defects, immune factors, infection, metabolic stress, and hemodynamic damage, irreversible loss of podocytes occurs [5]. Critical data suggest that podocyte depletion above 20% mediated the development of FSGS, and when depletion exceeded 40%, further development of glomerulosclerosis was triggered [6]. On the basis of this, both classical FSGS animal models using renal ablation or direct podocyte toxins, such as puromycin aminonucleoside (PAN) or adriamycin (ADR), and newly developed genetic animal models, such as PDSS2kd/kd mice, have been specially constructed by directly and indirectly, causing podocyte damage [7].
Fig. 1.
Basic structure and function of podocytes. Podocytes, together with capillary endothelial cells and GBM, form the basic structure of the glomerular filtration barrier. The crisscrossing foot processes of the podocytes and the slit diaphragm connection between adjacent foot processes are essential for the normal filtration function of the glomerulus. Moreover, podocytes secrete type IV collagen and fibronectin to form the GBM and perform an important role in the metabolic homeostasis of the GBM.
As a type of cell with a sophisticated structure and various functions, a podocyte relies on a substantial energy supply to maintain its function [8]. Podocytes rely on both glycolysis and mitochondrial metabolism to produce energy [9, 10]. In addition to supplying energy, mitochondria also play a pivotal role in regulating reactive oxygen species (ROS), intracellular calcium homeostasis, cell proliferation, and various forms of cell death (apoptosis, necrosis, necroptosis, pyroptosis, and ferroptosis) [11–16]. This review focuses on the recent advances in the study of mitochondrial abnormalities in podocyte injury and their contribution to FSGS. Based on this, we discussed the potential of mitochondria-targeted therapeutics in FSGS treatment.
Mitochondrial Abnormalities in FSGS
The sophisticated structure of podocytes and the maintenance of various cellular functions, including regulation and organization of the actin cytoskeleton and extracellular matrix proteins, depend on a high energy supply provided by a sufficient number of properly functioning mitochondria [17]. Under physiological conditions, a highly coordinated quality control system, including antioxidant defenses, mitochondrial dynamics (fusion, fission, and mitophagy), mitochondrial biogenesis, protein quality control, and mitochondrial DNA (mtDNA) repair, guarantees the structural and functional homeostasis of mitochondria in podocytes and counteracts stress to a certain extent so that cells can avoid mitochondrial damage. However, under severe stress conditions, the dysregulation of mitochondrial quality control mechanisms may lead to structural damage and dysfunction of mitochondria, triggering podocyte injury. Due to the limited repair and regeneration capacity of podocytes, the damage is usually irreversible, resulting in permanent podocyte loss and ultimately causing irreversible renal damage [5, 18].
Mitochondrial Oxidative Stress
In podocytes, ROS are produced mainly through two pathways – the mitochondrial respiration chain and NADPH oxidase (NOX) [10, 16]. The mitochondrial respiration chain consists of four protein complexes embedded in the inner mitochondrial membrane (complex I–IV) as well as cytochrome c (Cyt C) and quinone [16]. Mitochondrial ROS production is a tightly controlled process. Classical enzymatic antioxidants, including glutathione peroxidase (GPX), catalase (CAT), superoxide dismutase, thioredoxin reductase, and non-enzymatic antioxidants, including glutathione, glucose autoxidation, glycation products, ascorbic acid/vitamin C, α-tocopherol/vitamin E, flavonoids, and carotenoids, which together form an antioxidant defense system in vivo to restrain the excessive generation of ROS [19, 20]. Under physiological conditions, the mitochondrial antioxidant system can effectively maintain ROS at a low level, thus avoiding oxidative stress (OS)-induced damages in podocytes [16]. However, under pathological conditions or when an inherent defect occurs in the podocyte, the imbalance between increased levels of ROS production and decreased capacity of the cellular antioxidant system leads to OS, contributing to podocyte oxidative damage and cell death [12, 21].
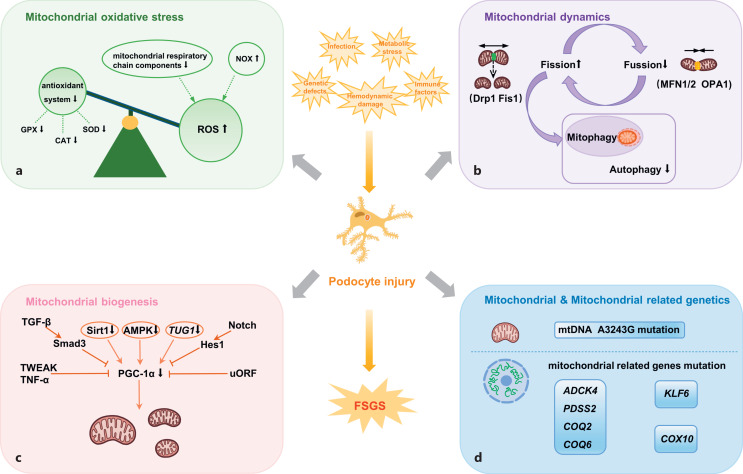
Mitochondrial respiratory chain dysfunction leads to an increased mitochondrial ROS level. In both PAN and ADR nephropathy animal models, decreased levels of mitochondrial respiratory chain components were observed [22–24]. In addition to mitochondrial respiratory chain dysfunction, high activity of NOX also accounts for increased ROS levels. Recently, a study in FSGS patients showed that steroid-resistant FSGS patients had higher NOX4 levels as well as higher ROS levels in isolated glomeruli compared to steroid-sensitive nephrotic syndrome patients [25]. By antagonizing the upregulation of NOX expression and downregulation of nuclear factor erythroid 2-related factor 2 (Nrf2) expression, angiotensin II receptor blockers exhibited a therapeutic effect, improving OS and inflammation in spontaneous FSGS Imai rats [26] (shown in Fig. 2).
Fig. 2.
Mitochondrial homeostatic imbalance and dysfunction of podocytes in FSGS. While under physiological conditions, well-balanced mitochondrial homeostasis is essential for the maintenance of podocyte structure and function. In the face of various deleterious stimuli, such as infection, genetic defects, immune factors, metabolic stress, and hemodynamic damage, irreversible loss of podocytes occurs which in turn further mediates the development of FSGS. a In FSGS, the balance between ROS production and clearance in podocytes is disrupted. Impaired mitochondrial respiratory chain and high levels of NOX lead to elevated ROS production. Meanwhile, reduced levels/activities of key antioxidant enzymes system (GPX, CAT, and SOD) represent a decreased ROS clearance ability. b In FSGS, the balance of mitochondrial dynamics in podocytes is also disrupted, which includes increased mitochondrial fission mediated by Drp1, Fis1, inhibited mitochondrial fusion mediated by MFN1/2, OPA1, and impaired autophagy. c PGC-1α is a master regulator of mitochondrial biogenesis in podocytes and can be positively regulated by Sirt1, AMPK, TUG1 and negatively regulated by two pro-fibrotic pathways (TGF-β/Smad3, Notch/Hes1), inflammatory factors (TWEAK and TNF-α), and uORF in the 5′ untranslated region of PPARGC1A gene. In FSGS, the expressions of PGC-1α, Sirt1, AMPK, and TUG1 were significantly suppressed, leading to impaired mitochondrial biogenesis. d Mutations in mtDNA and mitochondria-related genes also mediated the development of FSGS. SOD, superoxide dismutase.
Evidence of an impaired antioxidant defense system in FSGS has also been demonstrated. Deman et al. [27] captured key evidence of reduced activities of key enzymes of the antioxidant defense system, GPX, CAT, and superoxide dismutase, in an ADR-induced FSGS mouse model. Another similar study found that plasma, urine, and glomerular GPX levels were significantly lower in FSGS patients compared with minimal change disease patients and healthy controls [28]. Intriguingly, others have further demonstrated in ADR-induced FSGS mouse models that CAT knockout mice exhibited more severe pathological changes and clinical manifestations of FSGS and accelerated the progression of glomerulosclerosis compared to wild-type mice [29] (shown in Fig. 2).
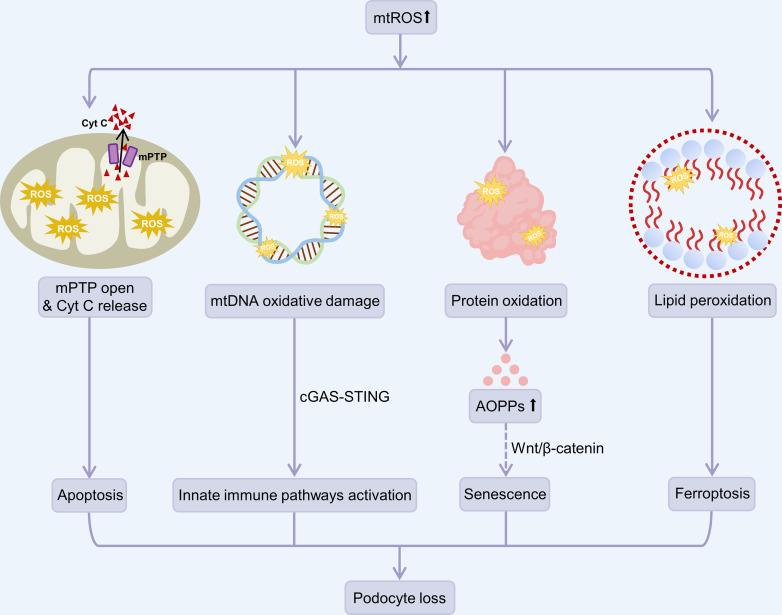
The unbalanced OS and antioxidant defense system lead to OS within podocytes. High levels of ROS were shown to induce mitochondrial permeability transition pore opening and increase Cyt C release, leading to mitochondrial dysfunction, organelle swelling, and cell apoptosis and death [13, 30]. Mitochondrial damage also leads to mtDNA leakage, which in turn overactivates the cyclic GMP-AMP synthase-stimulator of interferon genes pathway to cause podocyte injury [31]. Sustained high mtROS levels also damage macromolecules, such as DNA, proteins, and lipids. Due to the lack of histone protection and incomplete repair, mtDNA is extremely vulnerable to ROS damage, which may result in mtDNA mutations or invoke more ROS generation [30]. Oxidative alteration of proteins results in an increase of advanced oxidation protein products (AOPPs) [32]. Zhou et al. [33] demonstrated that increased AOPPs in the serum of patients with chronic kidney disease perform a pivotal role in the mobilization of the Wnt/β-catenin pathway, which in turn is engaged in OS-induced podocyte injury. Since activating Wnt/β-catenin pathway promoted cellular senescence in kidney tubular epithelial cells and lung epithelial cells, we might confer that AOPPs-induced Wnt/β-catenin pathway may also induce podocyte loss via inducing cellular senescence [34–37]. ROS also targets lipids, leading to lipid peroxidation and ferroptosis [14]. Recently, Wu and colleagues demonstrated that lipid peroxidation and ferroptosis accounted for high fructose-induced glomerular podocyte injury [38]. These studies suggest that a mitochondrial oxidant and antioxidant imbalance plays an important role in podocyte injury and the pathogenesis of FSGS, and use of mitochondria-targeted antioxidants may exert podocyte protective effects (shown in Fig. 3).
Fig. 3.
High levels of mtROS mediate podocyte loss. High levels of mtROS induce mPTP opening and Cyt C release from the mitochondria intermembrane space to the cytosol, ultimately leading to podocyte apoptosis. Sustained high mtROS levels also damage macromolecules, such as DNA, proteins, and lipids. Damaged mtDNA due to oxidation mediates podocyte loss by stimulating the cGAS-STING pathway, which in turn activates a series of innate immune pathways. AOPPs, the products of oxidative proteins, possibly induce podocyte senescence by activating the Wnt/β-catenin pathway. mtROS also targets lipids, resulting in lipid peroxidation and ferroptosis. mPTP, mitochondrial permeability transition pore.
Mitochondrial Dynamics Disturbances
Mitochondria are highly dynamic organelles that combine damaged parts with healthy mitochondria through fusion, and they also separate and eliminate damaged parts of organelles through fission, thus continuously remodeling to meet cellular energy requirements, which is essential to initiate rapid repair of damaged mitochondria [32]. Mitochondrial fission and fusion are also accompanied by mitophagy. Specifically, mitochondrial fission has a surveillance role of identifying malfunctioning daughter organelles that exhibit reduced mitochondrial membrane potential, and they are then restored by fusion or degraded by mitophagy [39]. Research has shown that mitochondrial fission is considered a central process required for mitophagy to occur, while mitochondrial fusion inhibits mitophagy [40]. As a consequence, a network-like mode of action exists between the three processes, which facilitates the maintenance of cellular function and survival under physiological and pathological conditions. Imbalance between mitochondrial fusion, fission, and mitophagy leads to disruption of mitochondrial dynamics, which in turn leads to mitochondrial dysfunction.
Mitochondrial dynamics are regulated by specific proteins: the members of the dynamin superfamily GTPases, in which dynamin-related protein 1 (Drp1) and mitochondrial fission protein 1 (Fis1) are the main mediators of mitochondrial fission; mitofusin 1 (MFN1) and mitofusin 2 (MFN2), which regulate mitochondrial outer membrane fusion; and optic atrophy 1 (OPA1), which regulates mitochondrial inner membrane fusion. In PAN- and ADR-induced podocyte injury models, PAN and ADR were found to induce mitochondrial fission in podocytes by inhibiting MFN1, while the use of the mitochondrial fission inhibitor Mdivi inhibited the production of caspase-3 in podocytes, thereby preventing PAN-induced podocyte apoptosis [41]. Analogously, knockdown of Drp1 in vitro reduced aldosterone-induced mitochondrial fragmentation and podocyte damage [42] (shown in Fig. 2).
Autophagy is a lysosomal degradation pathway that not only removes and reuses disintegrated cytoplasmic components through massive degradation of cytosol in a non-selective manner but also selectively removes specific organelles [43]. It is reported that podocytes maintain high basal levels of autophagy to preserve the normal function of long-lived podocytes [44]. Mitophagy is one of the classic representatives of selective autophagy, and it maintains the stability of the intracellular environment and is relatively active in podocytes. Through ubiquitin-dependent (PINK1-Parkin) and ubiquitin-independent (receptor mediated) pathways, damaged mitochondria are selectively phagocytized and cleared by autophagosomes and then degraded by lysosomes [45]. Knockout of the key autophagy genes Atg5 and Atg7 in mice resulted in disruption of normal autophagic pathways, leading to typical FSGS pathology in 4-month-old mice and renal failure in 6-month-old mice [46]. Research showed that glomeruli, especially podocytes, had lower levels of Beclin 1-mediated autophagic activity in FSGS patients compared to minimal change disease patients [47]. Moreover, downregulation of signal regulatory protein α (SIRPα), which is strongly expressed in podocytes and promotes autophagy, was observed in FSGS patients and experimental mice models induced by PAN, and ADR, and the level of SIRPα in podocytes was negatively correlated with the severity of podocyte damage and proteinuria [48]. Recently, Yildirim et al. [49] also found critical evidence of impaired FSGS autophagy in the 5/6 nephrectomy and ADR-induced FSGS rat models (shown in Fig. 2).
Defective Mitochondrial Biogenesis
Mitochondrial biogenesis is a complex and multi-step process referring to the coordinated synthesis of proteins (which are encoded by nuclear and mitochondrial genomes), mitochondrial membranes, and the replication of mtDNA [50]. New functional mitochondria are produced through mitochondrial biogenesis, which helps replace defective mitochondria and provide reserves for increased ATP production [51, 52]. Peroxisome proliferator-activated receptor γ coactivator 1α (PGC-1α) is a transcriptional coactivator that acts as a primary regulator of mitochondrial biogenesis in a variety of cells, including podocytes. One of the principal downstream effects of PGC-1α is the activation of transcription factors Nrf1 and Nrf2, followed by direct transcription of mitochondrial proteins encoded by the nucleus, as well as regulatory factors required for mtDNA transcription and translation, primarily mitochondrial transcription factor A (TFAM), thereby promoting mitochondrial biogenesis [10].
Sirtuin 1 (Sirt1) and AMP-activated protein kinase (AMPK) are the main positive regulators of PGC-1α, which activate PGC-1α by deacetylation and phosphorylation, respectively [10, 50, 53]. We and other researchers have previously demonstrated repressed PGC-1α, Sirt1, and AMPK activation in ADR-induced FSGS models [54–56]. Overexpression of PGC-1α provided a protective effect against ADR-induced podocyte injury [54]. Similarly, 14 days of continuous treatment with nicotinamide mononucleotide attenuated ADR-induced proteinuria and glomerulosclerosis in mice by upregulating kidney expression of Sirt1 [56]. Conversely, podocyte-specific knockdown of Sirt1 decreased PGC-1α expression and increased susceptibility to ADR nephropathy and glomerular injury [57]. Activating AMPK also restricted podocyte loss and decelerated the progression to FSGS in unilateral and 5/6 nephrectomy mice models [55]. In addition to Sirt1 and AMPK, long non-coding RNA taurine upregulated gene 1 (TUG1) was also found to be a positive regulator of mitochondrial biogenesis [58]. A more recent study innovatively found significantly reduced or absent expression of TUG1 in the urine of FSGS patients, highlighting the potential diagnostic potential of this long non-coding RNA for assessing podocytopathy [59] (shown in Fig. 2).
In contrast, some studies demonstrated that several pro-fibrotic and inflammatory mediators inhibited PGC-1α expression. Transforming growth factor β (TGF-β), a well-known pro-fibrotic cytokine, negatively regulated PGC-1α levels through epigenetic downregulation of Smad3 [60]. Another pro-fibrotic transcription factor, hairy and enhancer of split 1 (Hes1), a target gene of Notch signaling that also has an indispensable role in the development of renal fibrosis, was found to directly bind to the promoter region of PGC-1α and repress the expression of PGC-1α [61]. At the same time, inflammatory mediators such as tumor necrosis factor-like weak inducer of apoptosis (TWEAK) or TNF-α rely on the activation of nuclear factor-κB (NF-κB) and epigenetic regulation to negatively regulate PGC-1α [50, 62]. In a recent published paper, PGC-1α translation was also found to be negatively regulated by an upstream open reading frame in the 5′ untranslated region of its gene (PPARGC1A) [63]. The current research on the negative regulatory factors of PGC-1α in FSGS is still in its infancy, and further exploration is urgently needed (shown in Fig. 2).
However, a surprising study showed that podocyte-specific overexpression of PGC-1α in mice contributed to the formation of giant mitochondria and induced proliferation and dedifferentiation of podocytes, exhibiting histological damage similar to collapsing FSGS [64]. This led us to ponder strategies that cause overexpression of PGC-1α or target its upstream and downstream molecules and consider that within a safe range, these strategies may exert a protective effect against podocyte injury in FSGS. Importantly, the degree of podocyte tolerance to PGC-1α still needs to be taken into account, and exceeding its safety limit may have irreparable consequences. Therefore, future investigations are still needed to iteratively validate and explore this potentially narrow therapeutic window of safety in different in vitro and in vivo models.
Mutations in mtDNA and Mitochondria-Related Genes
Owing to the advances in medical science, more than 50 genes have been identified relating to podocytopathies and nephrotic syndrome (mainly FSGS) [65]. The pathogenic gene mutations that have been widely reported to be present in hereditary FSGS include WT1, NPHS1, NPHS2, TRPC6, ACTN4, and INF2[65–67]. In addition to these well-known gene mutations, mutations in mtDNA and mitochondria-related genes are also reported to mediate the development of FSGS. Numerous clinical cases have revealed that an A to G transition mutation at position 3243 (A3243G) of the mtDNA is strongly related to FSGS and proteinuria in patients with mitochondrial cell disease [68, 69]. Intriguingly, Hall et al. [70] conducted a urinary proteomic analysis in 117 adult patients with mitochondrial disease and identified that this mutation occurred in 75 of them (64.1%). These data support the idea that adult patients with mitochondrial disease are prone to kidney involvement (shown in Fig. 2).
Coenzyme Q10 (CoQ10) not only serves as two crucial electron carriers in the respiratory chain together with Cyt C but also has antioxidant activity. Mutations in the aarF domain-containing kinase 4 (ADCK4) gene, which encodes a mitochondrial respiratory chain protein expressed in podocytes and participates in CoQ10 biosynthesis, have been reported in patients with steroid-resistant nephrotic syndrome, which is characterized by FSGS and mitochondrial abnormalities in podocytes [71, 72]. Likewise, Saiki et al. [73] found that homozygous mice with mutations in the prenyl diphosphate synthase subunit 2 (PDSS2), which is also indispensable for the synthesis of CoQ10, developed proteinuria and interstitial nephritis and eventually died of end-stage renal disease. Gasser et al. [74] further showed that PDSS2 mutations led to a significantly increased risk of FSGS and collapsing glomerulopathy in humans. Other genes critical for CoQ10 biosynthesis, such as COQ2 and COQ6, are also correlated with steroid-resistant FSGS and collapsing glomerulopathy [75–80]. In patients and animal models with CoQ10 biosynthesis-related gene mutations, supplementation with CoQ10 or its precursor analogs showed prominent therapeutic efficiency [71, 72, 73, 77, 79, 80, 81, 82, 83] (shown in Fig. 2).
Krüppel-like factor 6 (KLF6) is a zinc finger domain transcription factor that also works as an early inducible damage response gene that regulates complex IV expression. Decreased KLF6 expression was discovered in renal biopsies from FSGS patients and HIV-associated nephropathy, and podocyte-specific KLF6 gene deletion exacerbated ADR-induced FSGS and podocyte injury in mice [84]. Also, mice with a loss-of-function deletion mutation in the mitochondrial complex IV cofactor heme A: farnesyltransferase (COX10) developed severe early onset FSGS and died prematurely owing to renal exhaustion [85] (shown in Fig. 2).
Mitochondria-Targeted Therapy
In recent years, with the progressive understanding of mitochondria in FSGS, several mitochondria-targeted strategies have been found beneficial in treating FSGS and other models of podocyte injury in vitro and in vivo. Mitoquinone, a mitochondria-targeted antioxidant, has been confirmed to diminish podocyte dysfunction and OS in podocytes, alleviate glomerulosclerosis, and minimize podocyte injury and apoptosis in a mouse model of angiotensin II-induced podocyte damage [86]. Two clinical trials evaluating the effect of mitoquinone in chronic kidney disease (NCT02364648, NCT03960073) are currently underway. Exogenous dietary supplementation with the antioxidant vitamin E exhibited a level of protective efficacy in an ADR-induced kidney impairment model in rats [87]. In parallel, MitoTEMPO, taurine, and SS-31 (a mitochondria-targeted antioxidant peptide) also displayed positive efficacy in reducing podocyte damage in PAN-induced minimal-change nephrotic syndrome and renal ischemia-reperfusion injury rat models due to their powerful antioxidant effects [88–90].
It has also been demonstrated that in rats with ADR-induced nephropathy, the administration of the mitochondrial permeability transition pore inhibitor cyclosporine reduced OS and exerted a sufficient podocyte protective function [91]. Nevertheless, the safe range of the drug must be closely monitored and controlled during clinical application since it has already been reported that high doses of cyclosporine may excert nephrotoxicity [92]. Resveratrol, a natural polyphenol found to be a Sirt1 activator, also attenuated aldosterone-induced podocyte injury and mitochondrial dysfunction through upregulation of PGC-1α both in vitro and in vivo [93]. Formoterol, an FDA-approved, classic, long-acting, and specific β2-adrenoceptor agonist, has been reported to promote mitochondrial biogenesis [94]. The mechanism is that formoterol first promotes Akt phosphorylation in a Gβγ-PI3K-dependent manner, leading to increased phosphorylation of its downstream target eNOS, which in turn further activates sGC to increase cGMP production, thereby promoting PGC-1α expression [95]. In ADR-induced FSGS and acute nephrotoxic serum nephritis mice models, treatment with formoterol agonized β2-adrenergic receptors on podocyte membranes and improved renal pathology, diminished proteinuria, and hastened glomerular functional recovery by promoting PGC-1α-dependent mitochondrial biogenesis [96]. Excitingly, novel polymeric nanoparticles that efficiently encapsulate and target formoterol to the kidney have been successfully designed and developed to promote renal mitochondrial biogenesis and reduce cardiovascular side effects, providing a promising therapeutic platform for future treatment in FSGS [97]. Recently, GDC-0879, a novel compound targeting Braf/Mapk, has been reported to ameliorate renal damage associated with global CoQ10 deficiency in PDSS2kd/kd mice [98].
The benefit of bioactive components of traditional Chinese medicine in ameliorating podocyte injury has gained increasing attention in recent years. Previous studies in our group have demonstrated that Huaier reversed mitochondrial dysfunction by upregulating PGC-1α expression and relieved ADR-induced podocyte toxicity in animal and in vitro models [99]. Hyperoside, an integral component of the Chinese herb forsythia, was also shown to inhibit mitochondrial fission, promote restoration of mitochondrial function, and improve proteinuria and podocyte damage in an ADR-induced FSGS mouse model [100]. Additionally, it has been suggested that apigenin (a bioactive plant flavone that is widely distributed in vegetables and fruits) and Shenkangning exerted nephroprotective effects by inhibiting OS injury in an ADR-induced FSGS mouse model [101, 102].
Conclusion
As an important component of the glomerular filtration barrier, damage and loss of podocytes under various stresses can lead to proteinuria, and they are important determinants in the progression of FSGS. Podocytes are highly differentiated epithelial cells packed with mitochondria. Under physiological conditions, a fine-tune balance between mitochondrial oxidants and antioxidants, fusion and fission, mitophagy and mitochondrial biogenesis maintains normal podocyte homeostasis and function, whereas under pathological conditions of FSGS, mitochondrial injury and dysfunction occurs, which mediates podocyte lesions and renal dysfunction. Favorable preclinical data have been achieved by targeting mitochondria and the key molecules of mitochondria-related signaling pathways in retarding FSGS development. However, there is still a long way to go for the clinical approval of mitochondria-targeted therapeutics in FSGS.
Although the current findings are promising, many issues remain to be further explored. First, the exact role and mechanisms of mitochondria in FSGS have not been fully elucidated; for example, studies on mitochondrial dynamics disorders in FSGS are still in the preliminary phase. More diverse and improved models of FSGS and more adequate individual studies are required to discover more specific and novel therapeutic targets targeting mitochondria in the future. Second, the pathogenesis of FSGS and podocyte injury is complex and multifactorial, with a variety of immune, infectious, metabolic, hemodynamic, and genetic elements that can be involved. For example, the activation of the Janus kinase-signal transducer/activator of transcription protein pathway, a major transducer of inflammatory signaling, was recently identified in the kidney of FSGS patients [103]. This undoubtedly adds more complexity to future studies. Third, the mechanisms of synergy and crosstalk between podocytes and other cells (such as renal tubular epithelial cells), mitochondria and other organelles (e.g., endoplasmic reticulum), and various links in the mitochondrial network warrant further exploration. Finally, future studies on the heritability of FSGS should be conducted with attention to the possible variability of mitochondrial genes and inheritance patterns between the different age groups of children and adults.
Conflict of Interest Statement
The authors declare that they have no competing interests.
Funding Sources
This work was supported by National Natural Science Foundation Grants (82090022; 81830020); Medical Research Project from Jiangsu Health and Health Commission (Z2022071); and Outstanding Youth Project from Nanjing Health and Health Commission (JQX22010).
Author Contributions
Y.L. and J.F. organized and wrote the first draft of the manuscript. W.Z. and Y.N. wrote sections of the manuscript. M.W. designed the study, revised the manuscript, and provided financial support for this work. A.Z. contributed to the conception and design of the study and provided financial support for this work. All authors approved the submitted version.
Funding Statement
This work was supported by National Natural Science Foundation Grants (82090022; 81830020); Medical Research Project from Jiangsu Health and Health Commission (Z2022071); and Outstanding Youth Project from Nanjing Health and Health Commission (JQX22010).
References
- 1. Musiała A, Donizy P, Augustyniak-Bartosik H, Jakuszko K, Banasik M, Kościelska-Kasprzak K, et al. Biomarkers in primary focal segmental glomerulosclerosis in optimal diagnostic-therapeutic strategy. J Clin Med. 2022 Jun 8;11(12):3292. 10.3390/jcm11123292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sobh MM, El Kannishy G, Moustafa F, Eid R, Hamdy N, Tharwat S. Role of detached podocytes in differentiating between minimal change disease and early focal segmental glomerulosclerosis, can we rely on routine light microscopy? J Nephrol. 2022 Nov 9;35(9):2313–24. 10.1007/s40620-022-01456-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Harshman LA, Bartosh S, Engen RM. Focal segmental glomerulosclerosis: risk for recurrence and interventions to optimize outcomes following recurrence. Pediatr Transplant. 2022 Sep;26(6):e14307. 10.1111/petr.14307. [DOI] [PubMed] [Google Scholar]
- 4. Ravaglia F, Melica ME, Angelotti ML, De Chiara L, Romagnani P, Lasagni L. The pathology lesion patterns of podocytopathies: how and why? Front Cell Dev Biol. 2022;10:838272. 10.3389/fcell.2022.838272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kopp JB, Anders HJ, Susztak K, Podestà MA, Remuzzi G, Hildebrandt F, et al. Podocytopathies. Nat Rev Dis Primers. 2020 Aug 13;6(1):68. 10.1038/s41572-020-0196-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wharram BL, Goyal M, Wiggins JE, Sanden SK, Hussain S, Filipiak WE, et al. Podocyte depletion causes glomerulosclerosis: diphtheria toxin-induced podocyte depletion in rats expressing human diphtheria toxin receptor transgene. J Am Soc Nephrol. 2005 Oct;16(10):2941–52. 10.1681/ASN.2005010055. [DOI] [PubMed] [Google Scholar]
- 7. Yang JW, Dettmar AK, Kronbichler A, Gee HY, Saleem M, Kim SH, et al. Recent advances of animal model of focal segmental glomerulosclerosis. Clin Exp Nephrol. 2018 Aug;22(4):752–63. 10.1007/s10157-018-1552-8. [DOI] [PubMed] [Google Scholar]
- 8. Yuan Q, Miao J, Yang Q, Fang L, Fang Y, Ding H, et al. Role of pyruvate kinase M2-mediated metabolic reprogramming during podocyte differentiation. Cell Death Dis. 2020 May 11;11(5):355. 10.1038/s41419-020-2481-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ahmad AA, Draves SO, Rosca M. Mitochondria in diabetic kidney disease. Cells. 2021 Oct 29;10(11):2945. 10.3390/cells10112945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Audzeyenka I, Bierżyńska A, Lay AC. Podocyte bioenergetics in the development of diabetic nephropathy: the role of mitochondria. Endocrinology. 2022 Jan 1;163(1):bqab234. 10.1210/endocr/bqab234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Zhang Y, Su SS, Zhao S, Yang Z, Zhong CQ, Chen X, et al. RIP1 autophosphorylation is promoted by mitochondrial ROS and is essential for RIP3 recruitment into necrosome. Nat Commun. 2017 Feb 8;8:14329. 10.1038/ncomms14329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Liu T, Chen XM, Sun JY, Jiang XS, Wu Y, Yang S, et al. Palmitic acid-induced podocyte apoptosis via the reactive oxygen species-dependent mitochondrial pathway. Kidney Blood Press Res. 2018;43(1):206–19. 10.1159/000487673. [DOI] [PubMed] [Google Scholar]
- 13. Tang C, Cai J, Yin XM, Weinberg JM, Venkatachalam MA, Dong Z. Mitochondrial quality control in kidney injury and repair. Nat Rev Nephrol. 2021 May;17(5):299–318. 10.1038/s41581-020-00369-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Fan J, Xu X, Li Y, Zhang L, Miao M, Niu Y, et al. A novel 3-phenylglutaric acid derivative (84-B10) alleviates cisplatin-induced acute kidney injury by inhibiting mitochondrial oxidative stress-mediated ferroptosis. Free Radic Biol Med. 2023;194:84–98. 10.1016/j.freeradbiomed.2022.11.029. [DOI] [PubMed] [Google Scholar]
- 15. Wang H, Lv D, Jiang S, Hou Q, Zhang L, Li S, et al. Complement induces podocyte pyroptosis in membranous nephropathy by mediating mitochondrial dysfunction. Cell Death Dis. 2022 Mar 29;13(3):281. 10.1038/s41419-022-04737-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Zhu YT, Wan C, Lin JH, Hammes HP, Zhang C. Mitochondrial oxidative stress and cell death in podocytopathies. Biomolecules. 2022 Mar 4;12(3):403. 10.3390/biom12030403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Giardino L, Armelloni S, Corbelli A, Mattinzoli D, Zennaro C, Guerrot D, et al. Podocyte glutamatergic signaling contributes to the function of the glomerular filtration barrier. J Am Soc Nephrol. 2009 Sep;20(9):1929–40. 10.1681/ASN.2008121286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Yin L, Yu L, He JC, Chen A. Controversies in podocyte loss: death or detachment? Front Cell Dev Biol. 2021;9:771931. 10.3389/fcell.2021.771931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Forman HJ, Davies KJ, Ursini F. How do nutritional antioxidants really work: nucleophilic tone and para-hormesis versus free radical scavenging in vivo. Free Radic Biol Med. 2014 Jan;66:24–35. 10.1016/j.freeradbiomed.2013.05.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Braga PC, Alves MG, Rodrigues AS, Oliveira PF. Mitochondrial pathophysiology on chronic kidney disease. Int J Mol Sci. 2022 Feb 4;23(3):1776. 10.3390/ijms23031776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Zhang Q, Hu Y, Hu JE, Ding Y, Shen Y, Xu H, et al. Sp1-mediated upregulation of Prdx6 expression prevents podocyte injury in diabetic nephropathy via mitigation of oxidative stress and ferroptosis. Life Sci. 2021 Aug 1;278:119529. 10.1016/j.lfs.2021.119529. [DOI] [PubMed] [Google Scholar]
- 22. Hagiwara M, Yamagata K, Capaldi RA, Koyama A. Mitochondrial dysfunction in focal segmental glomerulosclerosis of puromycin aminonucleoside nephrosis. Kidney Int. 2006 Apr;69(7):1146–52. 10.1038/sj.ki.5000207. [DOI] [PubMed] [Google Scholar]
- 23. Yu L, Liu Y, Wu Y, Liu Q, Feng J, Gu X, et al. Smad3/Nox4-mediated mitochondrial dysfunction plays a crucial role in puromycin aminonucleoside-induced podocyte damage. Cell Signal. 2014 Dec;26(12):2979–91. 10.1016/j.cellsig.2014.08.030. [DOI] [PubMed] [Google Scholar]
- 24. Xie K, Zhu M, Xiang P, Chen X, Kasimumali A, Lu R, et al. Protein kinase A/CREB signaling prevents adriamycin-induced podocyte apoptosis via upregulation of mitochondrial respiratory chain complexes. Mol Cell Biol. 2018 Jan 1;38(1):e00181–17. 10.1128/MCB.00181-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Tong J, Jin Y, Weng Q, Yu S, Jafar Hussain HM, Ren H, et al. Glomerular transcriptome profiles in focal glomerulosclerosis: new genes and pathways for steroid resistance. Am J Nephrol. 2020;51(6):442–52. 10.1159/000505956. [DOI] [PubMed] [Google Scholar]
- 26. Kim HJ, Sato T, Rodríguez-Iturbe B, Vaziri ND. Role of intrarenal angiotensin system activation, oxidative stress, inflammation, and impaired nuclear factor-erythroid-2-related factor 2 activity in the progression of focal glomerulosclerosis. J Pharmacol Exp Ther. 2011 Jun;337(3):583–90. 10.1124/jpet.110.175828. [DOI] [PubMed] [Google Scholar]
- 27. Deman A, Ceyssens B, Pauwels M, Zhang J, Houte KV, Verbeelen D, et al. Altered antioxidant defence in a mouse adriamycin model of glomerulosclerosis. Nephrol Dial Transplant. 2001 Jan;16(1):147–50. 10.1093/ndt/16.1.147. [DOI] [PubMed] [Google Scholar]
- 28. Chen HC, Guh JY, Lai YH. Alterations of glomerular and extracellular glutathione peroxidase levels in patients and rats with focal segmental glomerulosclerosis. J Lab Clin Med. 2001 Apr;137(4):279–83. 10.1067/mlc.2001.113231. [DOI] [PubMed] [Google Scholar]
- 29. Takiue K, Sugiyama H, Inoue T, Morinaga H, Kikumoto Y, Kitagawa M, et al. Acatalasemic mice are mildly susceptible to adriamycin nephropathy and exhibit increased albuminuria and glomerulosclerosis. BMC Nephrol. 2012 Mar 25;13:14. 10.1186/1471-2369-13-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Gujarati NA, Vasquez JM, Bogenhagen DF, Mallipattu SK. The complicated role of mitochondria in the podocyte. Am J Physiol Renal Physiol. 2020 Dec 1;319(6):F955–65. 10.1152/ajprenal.00393.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Zang N, Cui C, Guo X, Song J, Hu H, Yang M, et al. cGAS-STING activation contributes to podocyte injury in diabetic kidney disease. iScience. 2022 Oct 21;25(10):105145. 10.1016/j.isci.2022.105145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Barutta F, Bellini S, Gruden G. Mechanisms of podocyte injury and implications for diabetic nephropathy. Clin Sci. 2022 Apr 14;136(7):493–520. 10.1042/cs20210625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Zhou L, Chen X, Lu M, Wu Q, Yuan Q, Hu C, et al. Wnt/β-catenin links oxidative stress to podocyte injury and proteinuria. Kidney Int. 2019 Apr;95(4):830–45. 10.1016/j.kint.2018.10.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Luo C, Zhou S, Zhou Z, Liu Y, Yang L, Liu J, et al. Wnt9a promotes renal fibrosis by accelerating cellular senescence in tubular epithelial cells. J Am Soc Nephrol. 2018 Apr;29(4):1238–56. 10.1681/ASN.2017050574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Xiong Y, Zhou L. The signaling of cellular senescence in diabetic nephropathy. Oxid Med Cell Longev. 2019;2019:7495629. 10.1155/2019/7495629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Lehmann M, Hu Q, Hu Y, Hafner K, Costa R, van den Berg A, et al. Chronic WNT/β-catenin signaling induces cellular senescence in lung epithelial cells. Cell Signal. 2020 Jun;70:109588. 10.1016/j.cellsig.2020.109588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Gong W, Luo C, Peng F, Xiao J, Zeng Y, Yin B, et al. Brahma-related gene-1 promotes tubular senescence and renal fibrosis through Wnt/β-catenin/autophagy axis. Clin Sci. 2021 Aug 13;135(15):1873–95. 10.1042/CS20210447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Wu WY, Wang ZX, Li TS, Ding XQ, Liu ZH, Yang J, et al. SSBP1 drives high fructose-induced glomerular podocyte ferroptosis via activating DNA-PK/p53 pathway. Redox Biol. 2022 Jun;52:102303. 10.1016/j.redox.2022.102303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kraus F, Roy K, Pucadyil TJ, Ryan MT. Function and regulation of the divisome for mitochondrial fission. Nature. 2021 Feb;590(7844):57–66. 10.1038/s41586-021-03214-x. [DOI] [PubMed] [Google Scholar]
- 40. Liu S, Yuan Y, Xue Y, Xing C, Zhang B. Podocyte Injury in diabetic kidney disease: a focus on mitochondrial dysfunction. Front Cell Dev Biol. 2022;10:832887. 10.3389/fcell.2022.832887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Li X, Tao H, Xie K, Ni Z, Yan Y, Wei K, et al. cAMP signaling prevents podocyte apoptosis via activation of protein kinase A and mitochondrial fusion. PLoS One. 2014;9(3):e92003. 10.1371/journal.pone.0092003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Yuan Y, Zhang A, Qi J, Wang H, Liu X, Zhao M, et al. p53/Drp1-dependent mitochondrial fission mediates aldosterone-induced podocyte injury and mitochondrial dysfunction. Am J Physiol Renal Physiol. 2018 May 1;314(5):F798–808. 10.1152/ajprenal.00055.2017. [DOI] [PubMed] [Google Scholar]
- 43. Tang C, Livingston MJ, Liu Z, Dong Z. Autophagy in kidney homeostasis and disease. Nat Rev Nephrol. 2020 Sep;16(9):489–508. 10.1038/s41581-020-0309-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Bork T, Liang W, Yamahara K, Lee P, Tian Z, Liu S, et al. Podocytes maintain high basal levels of autophagy independent of mtor signaling. Autophagy. 2020 Nov;16(11):1932–48. 10.1080/15548627.2019.1705007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Ng MYW, Wai T, Simonsen A. Quality control of the mitochondrion. Dev Cell. 2021 Apr 5;56(7):881–905. 10.1016/j.devcel.2021.02.009. [DOI] [PubMed] [Google Scholar]
- 46. Kawakami T, Gomez IG, Ren S, Hudkins K, Roach A, Alpers CE, et al. Deficient autophagy results in mitochondrial dysfunction and FSGS. J Am Soc Nephrol. 2015 May;26(5):1040–52. 10.1681/ASN.2013111202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Zeng C, Fan Y, Wu J, Shi S, Chen Z, Zhong Y, et al. Podocyte autophagic activity plays a protective role in renal injury and delays the progression of podocytopathies. J Pathol. 2014 Oct;234(2):203–13. 10.1002/path.4382. [DOI] [PubMed] [Google Scholar]
- 48. Li L, Liu Y, Li S, Yang R, Zeng C, Rong W, et al. Signal regulatory protein α protects podocytes through promoting autophagic activity. JCI Insight. 2019 Mar 19;5(9):e124747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Yildirim D, Bender O, Karagoz ZF, Helvacioglu F, Bilgic MA, Akcay A, et al. Role of autophagy and evaluation the effects of microRNAs 214, 132, 34c and prorenin receptor in a rat model of focal segmental glomerulosclerosis. Life Sci. 2021 Sep 1;280:119671. 10.1016/j.lfs.2021.119671. [DOI] [PubMed] [Google Scholar]
- 50. Fontecha-Barriuso M, Martin-Sanchez D, Martinez-Moreno JM, Monsalve M, Ramos AM, Sanchez-Niño MD, et al. The role of PGC-1α and mitochondrial biogenesis in kidney diseases. Biomolecules. 2020 Feb 24;10(2):347. 10.3390/biom10020347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Zhu J, Wang KZ, Chu CT. After the banquet: mitochondrial biogenesis, mitophagy, and cell survival. Autophagy. 2013 Nov 1;9(11):1663–76. 10.4161/auto.24135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Jiang M, Bai M, Lei J, Xie Y, Xu S, Jia Z, et al. Mitochondrial dysfunction and the AKI-to-CKD transition. Am J Physiol Renal Physiol. 2020 Dec 1;319(6):F1105–16. 10.1152/ajprenal.00285.2020. [DOI] [PubMed] [Google Scholar]
- 53. Liu T, Yang L, Mao H, Ma F, Wang Y, Li S, et al. Sirtuins as novel pharmacological targets in podocyte injury and related glomerular diseases. Biomed Pharmacother. 2022 Nov;155:113620. 10.1016/j.biopha.2022.113620. [DOI] [PubMed] [Google Scholar]
- 54. Zhu C, Xuan X, Che R, Ding G, Zhao M, Bai M, et al. Dysfunction of the PGC-1α-mitochondria axis confers adriamycin-induced podocyte injury. Am J Physiol Renal Physiol. 2014 Jun 15;306(12):F1410–7. 10.1152/ajprenal.00622.2013. [DOI] [PubMed] [Google Scholar]
- 55. Banu K, Lin Q, Basgen JM, Planoutene M, Wei C, Reghuvaran AC, et al. AMPK mediates regulation of glomerular volume and podocyte survival. JCI Insight. 2021 Oct 8;6(19):e150004. 10.1172/jci.insight.150004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Hasegawa K, Sakamaki Y, Tamaki M, Wakino S. Nicotinamide mononucleotide ameliorates adriamycin-induced renal damage by epigenetically suppressing the NMN/NAD consumers mediated by Twist2. Sci Rep. 2022 Aug 12;12(1):13712. 10.1038/s41598-022-18147-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Chuang PY, Xu J, Dai Y, Jia F, Mallipattu SK, Yacoub R, et al. In vivo RNA interference models of inducible and reversible Sirt1 knockdown in kidney cells. Am J Pathol. 2014 Jul;184(7):1940–56. 10.1016/j.ajpath.2014.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Long J, Badal SS, Ye Z, Wang Y, Ayanga BA, Galvan DL, et al. Long noncoding RNA TUG1 regulates mitochondrial bioenergetics in diabetic nephropathy. J Clin Invest. 2016 Nov 1;126(11):4205–18. 10.1172/JCI87927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Salazar-Torres FJ, Medina-Perez M, Melo Z, Mendoza-Cerpa C, Echavarria R. Urinary expression of long non-coding RNA TUG1 in non-diabetic patients with glomerulonephritides. Biomed Rep. 2021 Jan;14(1):17. 10.3892/br.2020.1393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Li SY, Susztak K. The role of peroxisome proliferator-activated receptor γ coactivator 1α (PGC-1α) in kidney disease. Semin Nephrol. 2018 Mar;38(2):121–6. 10.1016/j.semnephrol.2018.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Han SH, Wu MY, Nam BY, Park JT, Yoo TH, Kang SW, et al. PGC-1α protects from notch-induced kidney fibrosis development. J Am Soc Nephrol. 2017 Nov;28(11):3312–22. 10.1681/ASN.2017020130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Ruiz-Andres O, Suarez-Alvarez B, Sánchez-Ramos C, Monsalve M, Sanchez-Niño MD, Ruiz-Ortega M, et al. The inflammatory cytokine TWEAK decreases PGC-1α expression and mitochondrial function in acute kidney injury. Kidney Int. 2016 Feb;89(2):399–410. 10.1038/ki.2015.332. [DOI] [PubMed] [Google Scholar]
- 63. Dumesic PA, Egan DF, Gut P, Tran MT, Parisi A, Chatterjee N, et al. An evolutionarily conserved uORF regulates PGC1α and oxidative metabolism in mice, flies, and bluefin tuna. Cell Metab. 2019 Jul 2;30(1):190–200.e6. 10.1016/j.cmet.2019.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Li SY, Park J, Qiu C, Han SH, Palmer MB, Arany Z, et al. Increasing the level of peroxisome proliferator-activated receptor γ coactivator-1α in podocytes results in collapsing glomerulopathy. JCI Insight. 2017 Jul 20;2(14):e92930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Massengill S, Trachtman H. Genetic spectrum of nephrotic syndrome: impact of podocytopathy in adult life. Adv Chronic Kidney Dis. 2022 May;29(3):221–4. 10.1053/j.ackd.2022.04.005. [DOI] [PubMed] [Google Scholar]
- 66. Nandlal L, Winkler CA, Bhimma R, Cho S, Nelson GW, Haripershad S, et al. Causal and putative pathogenic mutations identified in 39% of children with primary steroid-resistant nephrotic syndrome in South Africa. Eur J Pediatr. 2022 Oct;181(10):3595–606. 10.1007/s00431-022-04581-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Zhu X, Zhang Y, Yu Z, Yu L, Huang W, Sun S, et al. The clinical and genetic features in Chinese children with steroid-resistant or early-onset nephrotic syndrome: a multicenter cohort study. Front Med. 2022;9:885178. 10.3389/fmed.2022.885178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Alcubilla-Prats P, Solé M, Botey A, Grau JM, Garrabou G, Poch E. Kidney involvement in MELAS syndrome: description of 2 cases. Med Clin. 2017 Apr 21;148(8):357–61. 10.1016/j.medcli.2017.01.029. [DOI] [PubMed] [Google Scholar]
- 69. Narumi K, Mishima E, Akiyama Y, Matsuhashi T, Nakamichi T, Kisu K, et al. Focal segmental glomerulosclerosis associated with chronic progressive external ophthalmoplegia and mitochondrial DNA A3243G mutation. Nephron. 2018;138(3):243–8. 10.1159/000485109. [DOI] [PubMed] [Google Scholar]
- 70. Hall AM, Vilasi A, Garcia-Perez I, Lapsley M, Alston CL, Pitceathly RD, et al. The urinary proteome and metabonome differ from normal in adults with mitochondrial disease. Kidney Int. 2015 Mar;87(3):610–22. 10.1038/ki.2014.297. [DOI] [PubMed] [Google Scholar]
- 71. Yang J, Yang Y, Hu Z. A novel ADCK4 mutation in a Chinese family with ADCK4-associated glomerulopathy. Biochem Biophys Res Commun. 2018 Nov 30;506(3):444–9. 10.1016/j.bbrc.2018.10.102. [DOI] [PubMed] [Google Scholar]
- 72. Widmeier E, Yu S, Nag A, Chung YW, Nakayama M, Fernández-Del-Río L, et al. ADCK4 deficiency destabilizes the coenzyme Q complex, which is rescued by 2,4-dihydroxybenzoic acid treatment. J Am Soc Nephrol. 2020 Jun;31(6):1191–211. 10.1681/ASN.2019070756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Saiki R, Lunceford AL, Shi Y, Marbois B, King R, Pachuski J, et al. Coenzyme Q10 supplementation rescues renal disease in PDSS2kd/kd mice with mutations in prenyl diphosphate synthase subunit 2. Am J Physiol Renal Physiol. 2008 Nov;295(5):F1535–44. 10.1152/ajprenal.90445.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Gasser DL, Winkler CA, Peng M, An P, McKenzie LM, Kirk GD, et al. Focal segmental glomerulosclerosis is associated with a PDSS2 haplotype and, independently, with a decreased content of coenzyme Q10. Am J Physiol Renal Physiol. 2013 Oct 15;305(8):F1228–38. 10.1152/ajprenal.00143.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Diomedi-Camassei F, Di Giandomenico S, Santorelli FM, Caridi G, Piemonte F, Montini G, et al. COQ2 nephropathy: a newly described inherited mitochondriopathy with primary renal involvement. J Am Soc Nephrol. 2007 Oct;18(10):2773–80. 10.1681/ASN.2006080833. [DOI] [PubMed] [Google Scholar]
- 76. O’Toole JF. Renal manifestations of genetic mitochondrial disease. Int J Nephrol Renovasc Dis. 2014;7:57–67. 10.2147/IJNRD.S37887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Park E, Ahn YH, Kang HG, Yoo KH, Won NH, Lee KB, et al. COQ6 mutations in children with steroid-resistant focal segmental glomerulosclerosis and sensorineural hearing loss. Am J Kidney Dis. 2017 Jul;70(1):139–44. 10.1053/j.ajkd.2016.10.040. [DOI] [PubMed] [Google Scholar]
- 78. Song CC, Hong Q, Geng XD, Wang X, Wang SQ, Cui SY, et al. New mutation of coenzyme Q(10) monooxygenase 6 causing podocyte injury in a focal segmental glomerulosclerosis patient. Chin Med J. 2018 Nov 20;131(22):2666–75. 10.4103/0366-6999.245158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Widmeier E, Airik M, Hugo H, Schapiro D, Wedel J, Ghosh CC, et al. Treatment with 2,4-dihydroxybenzoic acid prevents FSGS progression and renal fibrosis in podocyte-specific COQ6 knockout mice. J Am Soc Nephrol. 2019 Feb 8;30(3):393–405. 10.1681/ASN.2018060625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Li M, Yue Z, Lin H, Wang H, Chen H, Sun L. COQ2 mutation associated isolated nephropathy in two siblings from a Chinese pedigree. Ren Fail. 2021 Dec;43(1):97–101. 10.1080/0886022X.2020.1864402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Feng C, Wang Q, Wang J, Liu F, Shen H, Fu H, et al. Coenzyme Q10 supplementation therapy for 2 children with proteinuria renal disease and ADCK4 mutation: case reports and literature review. Medicine (Baltimore). 2017 Nov;96(47):e8880. 10.1097/MD.0000000000008880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Stańczyk M, Bałasz-Chmielewska I, Lipska-Ziętkiewicz B, Tkaczyk M. CoQ10-related sustained remission of proteinuria in a child with COQ6 glomerulopathy-a case report. Pediatr Nephrol. 2018 Dec;33(12):2383–7. 10.1007/s00467-018-4083-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Maeoka Y, Doi T, Aizawa M, Miyasako K, Hirashio S, Masuda Y, et al. A case report of adult-onset COQ8B nephropathy presenting focal segmental glomerulosclerosis with granular swollen podocytes. BMC Nephrol. 2020 Aug 28;21(1):376. 10.1186/s12882-020-02040-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Mallipattu SK, Horne SJ, D'Agati V, Narla G, Liu R, Frohman MA, et al. Krüppel-like factor 6 regulates mitochondrial function in the kidney. J Clin Invest. 2015 Mar 2;125(3):1347–61. 10.1172/JCI77084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Baek JH, Gomez IG, Wada Y, Roach A, Mahad D, Duffield JS. Deletion of the mitochondrial complex-IV cofactor heme A:farnesyltransferase causes focal segmental glomerulosclerosis and interferon response. Am J Pathol. 2018 Dec;188(12):2745–62. 10.1016/j.ajpath.2018.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Zhu Z, Liang W, Chen Z, Hu J, Feng J, Cao Y, et al. Mitoquinone protects podocytes from angiotensin II-induced mitochondrial dysfunction and injury via the Keap1-Nrf2 signaling pathway. Oxid Med Cell Longev. 2021;2021:1394486. 10.1155/2021/1394486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Van den Branden C, Deman A, Ceyssens B, Pauwels M, Empsen C, Verbeelen D. Vitamin E protects renal antioxidant enzymes and attenuates glomerulosclerosis in adriamycin-treated rats. Nephron. 2002 May;91(1):129–33. 10.1159/000057614. [DOI] [PubMed] [Google Scholar]
- 88. Szeto HH, Liu S, Soong Y, Seshan SV, Cohen-Gould L, Manichev V, et al. Mitochondria protection after acute ischemia prevents prolonged upregulation of IL-1β and IL-18 and arrests CKD. J Am Soc Nephrol. 2017 May;28(5):1437–49. 10.1681/ASN.2016070761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Stacchiotti A, Favero G, Lavazza A, Monsalve M, Rodella LF, Rezzani R. Taurine supplementation alleviates puromycin aminonucleoside damage by modulating endoplasmic reticulum stress and mitochondrial-related apoptosis in rat kidney. Nutrients. 2018 May 29;10(6):689. 10.3390/nu10060689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Fujii Y, Matsumura H, Yamazaki S, Shirasu A, Nakakura H, Ogihara T, et al. Efficacy of a mitochondrion-targeting agent for reducing the level of urinary protein in rats with puromycin aminonucleoside-induced minimal-change nephrotic syndrome. PLoS One. 2020;15(1):e0227414. 10.1371/journal.pone.0227414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Guan N, Ren YL, Liu XY, Zhang Y, Pei P, Zhu SN, et al. Protective role of cyclosporine A and minocycline on mitochondrial disequilibrium-related podocyte injury and proteinuria occurrence induced by adriamycin. Nephrol Dial Transplant. 2015 Jun;30(6):957–69. 10.1093/ndt/gfv015. [DOI] [PubMed] [Google Scholar]
- 92. de Arriba G, Calvino M, Benito S, Parra T. Cyclosporine A-induced apoptosis in renal tubular cells is related to oxidative damage and mitochondrial fission. Toxicol Lett. 2013 Mar 27;218(1):30–8. 10.1016/j.toxlet.2013.01.007. [DOI] [PubMed] [Google Scholar]
- 93. Yuan Y, Huang S, Wang W, Wang Y, Zhang P, Zhu C, et al. Activation of peroxisome proliferator-activated receptor-γ coactivator 1α ameliorates mitochondrial dysfunction and protects podocytes from aldosterone-induced injury. Kidney Int. 2012 Oct;82(7):771–89. 10.1038/ki.2012.188. [DOI] [PubMed] [Google Scholar]
- 94. Wills LP, Trager RE, Beeson GC, Lindsey CC, Peterson YK, Beeson CC, et al. The β2-adrenoceptor agonist formoterol stimulates mitochondrial biogenesis. J Pharmacol Exp Ther. 2012 Jul;342(1):106–18. 10.1124/jpet.112.191528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Cameron RB, Peterson YK, Beeson CC, Schnellmann RG. Structural and pharmacological basis for the induction of mitochondrial biogenesis by formoterol but not clenbuterol. Sci Rep. 2017 Sep 5;7(1):10578. 10.1038/s41598-017-11030-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Arif E, Solanki AK, Srivastava P, Rahman B, Fitzgibbon WR, Deng P, et al. Mitochondrial biogenesis induced by the β2-adrenergic receptor agonist formoterol accelerates podocyte recovery from glomerular injury. Kidney Int. 2019 Sep;96(3):656–73. 10.1016/j.kint.2019.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Vallorz EL, Blohm-Mangone K, Schnellmann RG, Mansour HM. Formoterol PLGA-PEG nanoparticles induce mitochondrial biogenesis in renal proximal tubules. Aaps j. 2021 Jun 24;23(4):88. 10.1208/s12248-021-00619-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Sidhom EH, Kim C, Kost-Alimova M, Ting MT, Keller K, Avila-Pacheco J, et al. Targeting a Braf/Mapk pathway rescues podocyte lipid peroxidation in CoQ-deficiency kidney disease. J Clin Invest. 2021 Mar 1;131(5):e141380. 10.1172/JCI141380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Che R, Zhu C, Ding G, Zhao M, Bai M, Jia Z, et al. Huaier cream protects against adriamycin-induced nephropathy by restoring mitochondrial function via PGC-1α upregulation. PPAR Res. 2015;2015:720383. 10.1155/2015/720383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Chen Z, An X, Liu X, Qi J, Ding D, Zhao M, et al. Hyperoside alleviates adriamycin-induced podocyte injury via inhibiting mitochondrial fission. Oncotarget. 2017 Oct 24;8(51):88792–803. 10.18632/oncotarget.21287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Wu Q, Li W, Zhao J, Sun W, Yang Q, Chen C, et al. Apigenin ameliorates doxorubicin-induced renal injury via inhibition of oxidative stress and inflammation. Biomed Pharmacother. 2021 May;137:111308. 10.1016/j.biopha.2021.111308. [DOI] [PubMed] [Google Scholar]
- 102. Wei M, Qiu Z, Li H, Lu B, Wang C, Ji L. Integrating network pharmacology approach and experimental validation to reveal the alleviation of shenkangning capsule on chronic nephritis. J Ethnopharmacol. 2022 Dec 5;299:115676. 10.1016/j.jep.2022.115676. [DOI] [PubMed] [Google Scholar]
- 103. Tao J, Mariani L, Eddy S, Maecker H, Kambham N, Mehta K, et al. JAK-STAT signaling is activated in the kidney and peripheral blood cells of patients with focal segmental glomerulosclerosis. Kidney Int. 2018 Oct;94(4):795–808. 10.1016/j.kint.2018.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]